Abstract
Objective
To enhance the survival rate of atraumatic restorative treatment (ART) restorations using (class I and class II) bilayer technique of placing glass ionomer cement (GIC) along with nanofilled coating (NC) over the restorations, thereby improving longevity.
Study design
A total of 178 primary molars in 67 children were selected and randomly divided into four groups. Group IA was treated with a single layer of GIC, followed by a protective layer of petroleum jelly in class I restoration. Group IB was treated with a single layer of GIC, followed by a protective layer of petroleum jelly in class II restoration. Group IIA was treated with bilayer GIC restoration followed by NC of GC-Coat Plus in class I, whereas group IIB was treated with bilayer GIC restoration followed by GC-Coat Plus in class II. Clinical analysis of all three groups was performed at 1, 3, 6, 9, and 12 months to evaluate the success of treatment procedures using predetermined criteria. Pearson's Chi-square and Kaplan–Meier estimates were utilized to evaluate the success of all four treatment procedures (p < 0.05).
Results
Out of 178 teeth, 33 teeth were in group IA, 36 teeth were in group IB, 43 teeth were in group IIA, and 40 teeth were available for evaluation at the end of the 12-month follow-up period. The overall success was determined to be 81% for group IA, 79.2% for group IB, 79.5% for group IIA, and 88.6% for IIB. At 6th-month follow-up, one clinical failure was observed in groups IA and IB. At 9 months follow-up, two clinical failures were observed in both group IA and group IB and three failures were observed in group IIB. At 12 months follow-up, four clinical failures were observed in group IA, three in group IB and one clinical failure was observed in group IIB. There was no statistically significant difference observed between the success of the four groups, suggesting that either of the techniques can be utilized for ART.
Conclusion
No statistically significant difference was observed between the survival of class I and class II restorations of both the groups, indicating that either single-layer or bilayer technique along with NC can be adopted for the management of dental caries in primary molars using the ART approach.
How to cite this article
Khan N, Garg N, Garg N, et al. Comparative Evaluation of the Survival Rates of Atraumatic Restorative Treatment Restorations Using Bilayer Technique along with Nanofilled Coating in Primary Molars: A Clinical Study. Int J Clin Pediatr Dent 2024;17(S-1):S55–S60.
Keywords: Atraumatic restorative treatment, Bilayer technique, Glass ionomer cement
Introduction
The World Health Organization (WHO) promotes atraumatic restorative treatment (ART) as a feasible approach to meet the requirements for the management of caries. This treatment protocol integrates both the restorative aspect and the preventive element, leading to maximum preservation of the tooth structure.1,3
In ART, by using hand instruments, demineralized tissue is removed, followed by restoring the cavity with a restorative material,4,5 which binds to the dental structure, releases fluoride, and stimulates remineralization. Over the years, numerous studies have been conducted to view the various aspects of the technique, which have concentrated on the properties of adhesive restorative material and their survival rates.6,8 These studies have led to improvement of the technique9 and properties of newly introduced glass ionomer cement (GIC), especially for ART.
Currently, the material of choice is high viscosity GIC because of its well-known properties (physical and chemical), such as anticariogenic potential, its ability to be dimensionally stable and illustrating enhanced marginal integrity in high humidity. The material also brings a viscous consistency, making this cement consist of compound manipulation.10,12 The problem in dealing with high viscosity GIC usually results in improper adherence to the tooth surface. Furthermore, open marginal and cervical gaps may result in failures of ART proximal restorations.13,15
Recent laboratory studies16,17 revealed that in class II cavities of deciduous teeth, the placement of a thin layer of GIC prior to the introduction of a thick layer, that is, bilayer technique, high viscosity GICs, can enhance the adaptation of material to the tooth surface, which helps to reduce microleakage, decreased stress concentration and higher bond strength values to sound dentine.
Although high viscosity GIC provides improved mechanical properties when compared to the earlier generation of conventional restorative GICs, some adverse characteristics may inflict their limits on clinical use. GICs have a long setting time, that is, 24 hours, and during this period, they are highly sensitive to humidity and dehydration, which leads to easy wear resistance. In order to obtain the highest mechanical properties of this material, several authors have recommended the use of surface protecting agents,18,20 especially in the initial stage of jellification like petroleum jelly. It is economical, easy to use, safe for the patients, more effective than copal varnish and adhesive systems, and low-cost. As long as the protective material remains in contact with the restorations, there are less chances that the mechanical properties of this material will reduce.
In recent years, a new light-cured protective type of coating has been introduced for GIC, that is, G-Coat Plus, GC Europe, Leuven, Belgium, which contains uniformly dispersed nanofillers to enhance the properties of GIC on its application. Few authors have concluded that the application of this material reduces wear in permanent first molars.21,23 Its major advantages are superb polish, excellent esthetics, and improved wear resistance.
To the best of my knowledge, there are limited studies22,24 available in the literature showing the combined efficacy of the bilayered technique and the use of nanofilled coating (NC) in the longevity of ART restorations. Hence, this study was undertaken to investigate the rate of ART restoration survival (class I and class II) in deciduous molars using two different insertion techniques (single layer and bilayer) and with two different materials for surface protection (petroleum jelly and G-Coat Plus).
Materials and Methods
Prior approval of the study design was taken by the Ethics Committee of the Institution. After screening 216 children who reported to the outpatient department of pedodontics and preventive dentistry, 67 children who fulfilled the inclusion criteria were chosen for the study. The sampling method used was the stratified sampling method. A total of 178 primary molars from the selected participants were assigned to two groups—group I, 86 teeth (42 in class I/ 44 in class II) and group II, 92 teeth (48 allotted to class I and 44 to class II) based on the randomization protocol.25 Sample size calculation was done following the power analysis, which was >85% for this study with a minimum sample size of 132. For this study, both boys and girls belonging to the age-group of 5–11 years and having at least one occlusal carious lesion in deciduous molar involving dentin, extending not >2 mm mesiodistally and 2.5 mm buccolingually or occluso-cervically were selected. Patients having profound behavioral or medical problems and pulpal involvement, including pain, swelling, fistula, or pathological mobility of the tooth, were not considered for the study.
The treatment was performed as per the ART guidelines, and no local anesthesia or radiographic examination was performed.26 Isolation was done using cotton wool rolls. Caries excavation in both groups was carried out using hand instruments. The prepared cavities were conditioned with the diluted polyelectrolytic liquid of GIC for 10 seconds, followed by rinsing and drying with wet and dry cotton balls, respectively. A metallic matrix band and wedge were placed for all class II cavities prior to restoration.
Clinical procedure in group I (conventional single layer ART restoration) GIC mixture was prepared as per the manufacturer's guidelines. After inserting the GIC into the cavity, the press finger technique was applied, and extra material was cleared off with the help of an explorer. Using an applicator tip, a fine layer of petroleum jelly was placed to shield the restoration.
Clinical procedure in group II (bilayer technique ART restoration). The first layer of flowable consistency GIC with aa powder/liquid ratio of 0.5:1 was applied at the bottom of the cavity and cavity walls as a liner. For the second layer, GIC was mixed using a powder/liquid ratio of 1:1 and placed while the first layer was partially set.16 After inserting the GIC into the cavity, the press finger technique was applied, and excess material was removed. For shielding the restoration, the NC for GIC (G-Coat Plus) was applied with a microbrush on the restoration's occlusal surface, and the coat was photopolymerized for 20 seconds.
To assess the success of the treatment, clinical evaluation of all the teeth in all the groups was carried out at 1, 3, 6, 9, and 12 months, respectively, as described by Hesse et al.22
Results
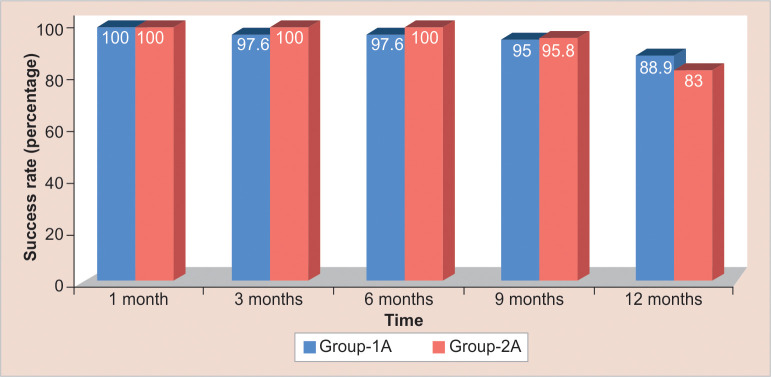
A total of 39 males and 28 females received treatment in either group, with a mean age of 6.67 ± 1.61 years. At the end of the 1-month follow-up, 42 (100%) restorations were intact in group IA and 48 (100%) were intact in group IIA (score 0). At the end of the 3-month follow-up, one (2.1%) restoration in group IIA showed a slight defect at the margin (score 10), but no repair was needed. One (2.4%) restoration in group IA showed a defect at the margin >0.5 mm in depth (score 11), needing repair. At the end of the 6th-month follow-up, four (9.8%) restorations in group IA and group IIA showed a slight defect at the margin (score 10), but no repair was needed. One (2.4%) restoration in group IA showed a defect at the margin >0.5 mm in depth (score 11) needing repair. At the end of the 9th month's follow-up, 11 (27.5%) restorations in group IA and nine (18.8%) restorations showed a slight defect at the margin (score 10), but no repair was needed. One restoration in group IIA showed a defect at the margin >0.5 mm in depth (score 11), needing repair. One (2.5%) restoration in group IA showed secondary caries (score 21), needing repair. The restoration was not present—a bulk fracture in one tooth in group IA. At the end of 12 months of follow-up, 13 (36.1%) restorations in group IA and 17 (36.2%) restorations in group IIA showed a slight defect at the margin (score 10), but no repair was needed. One (2.8%) restoration in both group IA and group IIA showed a defect at the margin >0.5 mm in depth (score 11), needing repair. One (2.8%) restoration in group IA and two (4.3%) restoration in group IIA showed no gap underfilled >0.5 mm. needing repair. One (2.1%) restoration in group IIA showed secondary caries (score 21), needing repair. Restoration was not present: bulk fracture in one (2.1%) tooth in group IIA. A significant difference was not seen between group IA and group IIA (p > 0.05) at the various time intervals.
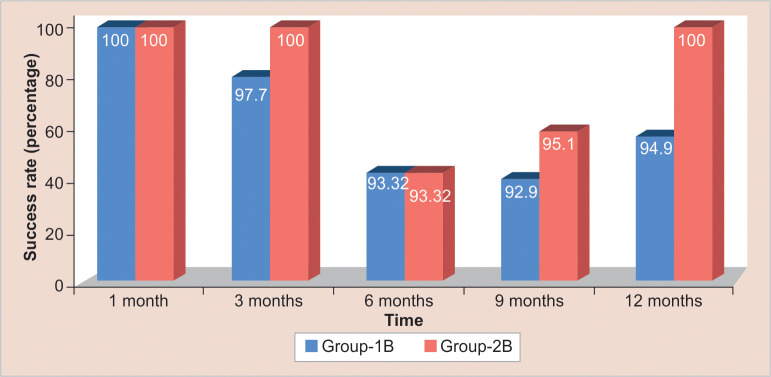
At the end of the 1-month follow-up, 44 (100%) restorations were intact in group IB, and 44 (100%) were intact in group IIB (score 0) (p > 0.05). At the end of the 3-month follow-up, one restoration (2.3%) in group IB showed a slight defect at the margin (score 10), but no repair was needed. One (2.3%) restoration in group IB showed a defect at the margin >0.5 mm in depth (score 11), needing repair (p > 0.05). At the end of 6-month follow-up, four (9.1%) restorations in group IB and three (6.8%) in group IIB showed a slight defect at the margin (score 10), but no repair was needed. Restoration was not present—bulk fracture in two (4.5%) teeth in group IB and three (6.8%) teeth in group IIB (score 30) (p > 0.05). At the end of the 9-month follow-up, 10 (23.8%) restorations in group IB and six (14.6%) restorations in group IIB showed a slight defect at the margin (score 10), but no repair was needed. One restoration (2.4%) in group IB showed a defect at the margin >0.5 mm in depth (score 11) needing repair. One (2.4%) restoration in group IIB showed no gap, was underfilled, and needed repair (score 12). Restoration was not present—bulk fracture in two (4.8%) teeth in group IB (score 30) (p > 0.05). At the end of 12 months follow-up, 22 (56.4%) restorations were intact in group IB and 30 (76.9%) in group IIB (score 0). Around 15 (38.5%) restorations in group IB and nine (23.1%) restorations in group IIB showed slight defects at the margin (score 10), but no repair was needed. One (2.6%) restoration in group IB showed a defect at the margin >0.5 mm in depth (score 11), needing repair (p > 0.05). Table 1 represents the overall success rate observed between group I (single surface + petroleum jelly) and group II (bilayer + nanofilled coating) at various follow-up periods. Figure 1 represents success rates observed between group IA and group IIA in class I restoration at various follow-up periods. Figure 2 represents success rates observed between group IB and group IIB in class II restorations at various follow-up periods.
Table 1:
Overall success rate observed between group I (single surface + petroleum jelly) and group II (bilayer + NC)
| Group IA | Group IB | Group IIA | Group IIB | ||
|---|---|---|---|---|---|
| 1 month | Failure | 0/42 | 0/48 | 0/44 | 0/44 |
| Survival | 100% | 100% | 100% | 100% | |
| 3 months | Failure | 1/42 | 0/48 | 1/44 | 0/44 |
| Survival | 97.6% | 100% | 97.7% | 100% | |
| 6 months | Failure | 2/42 | 0/48 | 4/44 | 3/44 |
| Survival | 95.2% | 100% | 91% | 93.2% | |
| 9 months | Failure | 4/42 | 2/48 | 7/44 | 5/44 |
| Survival | 90.5% | 95.8% | 84.1% | 88.6% | |
| 12 months | Failure | 8/42 | 10/48 | 9/44 | 5/44 |
| Survival | 81% | 79.2% | 79.5% | 88.6% | |
Fig. 1:
Represents the success rates observed between group IA and group IIA in class I restorations at various follow-up periods
Fig. 2:
Success rates observed between group IB and group IIB in class II restorations at various follow-up periods
Discussion
Atraumatic restorative treatment technique is one of the existing minimal intervention approaches, which mainly depends on the removal of the soft carious lesion using the hand equipment, followed by restoration of the tooth with the help of an adhesive material, usually GIC.27 This technique is patient-friendly as it reduces both the phobia of pain and anxiety when compared with that of traditional procedure, as no vibrating drills or noisy suction machines are used in this method of treating dental caries28 and this is not only engaged for field area but can also be used for dental clinic settings.8
High viscosity GIC has been traditionally used as a treatment option for ART due to its fluoride releasing property, and it is also convenient to use. Raggio et al.29 suggested that high viscosity GIC restoration showed similar success to the conventional approach by using composite resin for both the occluso-proximal and occlusal restoration in deciduous molars after a follow-up of 24 months. Although this material has the advantage of enhancing the mechanical properties compared to its forerunners, to date, it has few imperfections. The high viscosity of GIC results mainly in poor adaptation, particularly in class II cavities, leading to failure of restorations.11,12 Therefore, in order to overcome this difficulty, the bilayer method of GIC restoration has been used. The technique encompasses penetrating a thin layer of flowable GIC in a class II cavity prior to the introduction of a conventional GIC layer and has shown satisfactory material adaptation to dental structures.16 In addition, it also helps in reducing the stress from the occlusal load,30 and this results in longer-lasting restorations.
The restoration done using a thin flowable layer of GIC showed less microleakage, and no voids were observed on the tooth surface. The lower powder/liquid ratio plays an important role in tooth structure adhesion. The higher polyacrylic acid increases the number of cross-links and thus improves the enhanced wettability. This verity describes the lower microleakage, and no voids were observed in the bilayer technique (two-layered group). The principle of adhesion states that fluid materials inserted in a satisfactory manner in the substrate facilitate the micromechanical adhesion,31 which in turn increases microleakage resistance.32 Both the mechanisms (chemical and micromechanical adhesion) are enhanced by the thin layer of GIC. Apparently, the presence of a flowable GIC layer provides satisfactory adherence to the whole material in the cavity. In the present study, the bilayer technique was used because of its numerous advantages.
Clinical trials are usually made with the most expensive GIC brands, which may be very high for the people of developing countries.33 Bonifacio et al.34 investigated the success rate of three brands of GIC, applied to proximal restorations and concluded that there were no differences present among the various GIC brands. Their results indicate that GIC itself cannot be considered the major reason for the success of ART restoration, as it mainly results in a high failure rate; therefore, in the present study, glass ionomer restorative material (Gold Label, GC Corporation, Tokyo Japan) brand was used as it is easily available and less costing without compromising the physical and mechanical properties.
Longitudinal research data have highlighted enhanced success rates for the ART technique in class I cavities.3,35,36 However, the same success rates are not reported when the cavities were prepared involving multiple surfaces, even with the use of high viscosity GICs.37 The numbers presented by a meta-analysis showed that longevity rates of class I restorations are 95, 93, and 66% after 1, 2, and 3 years, respectively. In the present study, the success rate of class I restorations was 85.5%. The available literature has revealed that the ART protocol is important for the treatment of one surface cavities in both primary and permanent teeth.38,39 Honkala et al.,8 in their research found that ART restorations in deciduous teeth were highly successful.
Several clinical studies with short follow-up periods have observed a high survival rate of one surface ART restorations in primary molars but poorer results for multiple surface restorations.40
Frencken et al.14 stated that when the dental cavities were prepared by using hand instruments, it mainly resulted in insufficient removal of caries and hand fatigue. Consequently, this results in a shorter survival rate expectation. In addition to this, incorrect matrix band placement, poor manipulation of GIC, and restorative material lead to poor success rate of ART restoration. These are all operator/assistant-dependent factors.
The results of the present study, after 6 months and 1 year, show high success in occlusal and proximal surface ART restorations. No significant statistical difference was observed in the success of single and bilayered techniques. For class I, the success rate at 12 months follow-up for group IA was 81% and group IIA, 79.5% and for class II, the success rate at 12-month follow-up period for group IB was 79.2% and for group IIB, 88.6%. In the survival rate of class II restorations in deciduous molars, it was observed that the medium-sized cavities showed better success rates. The major reason for restoration failure in the present study was “bulk fracture and gross marginal defect.” Careful removal of carious dentin, especially at the enamel–dentin junction, may have been a reason for the high success rates observed in the present study. The criteria applied for observing the success of restorations for the present study were in accordance with previous ART studies.41,42 The criteria are well-defined for evaluating the success or failure of restorations in a field setting.1,39
Another crucial mass for the GICs is surface protection. The water sensitivity and longer setting time result in decreased mechanical properties, therefore restricting the use of GIC in day-to-day practice.18,43,44 Kamatham and Reddy45 conducted a study to assess the effect of surface protection material on the release of fluoride from conventional GICs. They observed that varnish application over GIC critically disrupts fluoride release, whereas petroleum jelly also delays the fluoride release but to a lesser extent. They concluded that petroleum jelly may be used in cases where the fluoride-releasing property cannot be compromised.
G-Coat Plus (GC-Co, Tokyo, Japan) is a nanofilled material with low viscosity, mainly placed on top of glass ionomers cement restorations. Available literature shows that the use of this coating enhances the restoration's flexural strength and wear resistance.46,47 Consequently, in the present study, it was decided to test the recently developed nanofilled coating for GIC.
The reported consequence of this nanofilled material on mechanical properties of FIX is, however, contradictory; whereas some of the studies demonstrated the results of improvement in some properties,46,47 other parameters presented no improvement after association of this surface protection and GIC in laboratory tests.48,49 A few studies have compared the clinical performance of Fuji IX GP Extra with and without NC, but the results are controversial. Diem et al.50 verified after a 2-year follow-up period that the coated group showed significantly less wear; on the contrary, by the 3rd year, there was no statistical difference between the groups. Fried et al.51 evaluated the presentation of FIX with NC restorations and concluded that it can be used as a permanent restorative material for class I cavities of varying sizes and small class II cavities.
Fraji et al.52 conducted an in vitro study to evaluate the effect of aging and the type of NC material used on the microhardness of GIC. They observed that low microhardness in the G-Coat Plus group could be due to the weakness of a thick layer of unfilled resin, which undergoes hydrolysis over a period of time and is inexpensive. They also mentioned that the manufacturer guarantees the 3 months effectiveness of G-Coat Plus protective coating. This could be the reason why G-Coat Plus did not show significant differences when compared to the petroleum jelly group after a 12-month follow-up.
G-Coat Plus, consisting of single-phase nanofillers, develop “microlamination effect,” which leads to the formation of a protective coating of about 35–40 µm. This final lamination hereby forms the smooth and glossy surface, which in turn enhances the hardness of all GIC restoration. It also protects the GIC from excessive water contamination and binds in a good manner to both the cement and tooth surface, therefore packing the voids. Thus, the stress is scattered by the laminating layer. It was also observed that the sample coated with the NC, that is, G-Coat Plus, provides higher mechanical strength than the unprotected ones. With the help of dispersion nanofiller technology, GC Coat Plus increases the wear resistance of the material as it helps to uniformly disperse nanofillers. This also provides protection against any acid attack, which helps in the slow and steady release of fluoride. These properties improve the quality of glass ionomer restoration for use in pediatric dentistry.
At the end of the 1, 3, 6, 9, 12 months period of follow-up, no significant differences were noticed between the two groups of class I restorations, that is, group IA (single layer of GIC followed by petroleum jelly) and group IIA (bilayer GIC technique followed by G-Coat Plus) p > 0.05. There were also no significant differences seen between group IB and group IIB (p > 0.05).
One limiting factor in the present study is that the restorations were protected by either petroleum jelly or NC (G-Coat Plus) for GIC. Therefore, there was no group included that did not have some type of protective coating, which made it unfeasible to ascertain the effects of temperature in the material without some kind of protection. The deductions of the present study are similar to Hesse et al.,22 who reported that the coated GIC had no influence on the SR of approximal restorations in primary teeth. Hence, further studies with larger sample sizes and an increased follow-up period are required to prove the efficacy of the same.
Conclusion
The conclusions drawn from this study are:
The survival rate of ART restorations using single layer technique in class I was 81%, and in class II restoration was 79.5%. The survival rate of ART restorations using bilayer technique in class I was 79.2%, and in class II restoration, it was 88.6%.
Failures were observed in both groups irrespective of the technique used, and the differences were statistically not significant.
No statistically significant difference was observed between the survival of class I and class II restoration of both the groups, indicating that either of the techniques can be utilized for ART.
Further studies utilizing longer follow-up periods should be undertaken to arrive at a final conclusion.
Orcid
Nishita Garg https://orcid.org/0000-0001-6594-9098
Ramakrishna Yeluri https://orcid.org/0000-0002-0320-2105
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Frencken JE, Holmgren CJ. ART: a minimal intervention approach to manage dental caries. Dent Update. 2004;31(5):295–298. doi: 10.12968/denu.2004.31.5.295. [DOI] [PubMed] [Google Scholar]
- 2.Molina GF, Cabral RJ, Frencken JE. The ART approach: clinical aspects reviewed. J Appl Oral Sci. 2009;17:89–98. doi: 10.1590/s1678-77572009000700016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frencken JE, Leal SC, Navarro MF. Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig. 2012;16(5):1337–1346. doi: 10.1007/s00784-012-0783-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frencken JE, Holmgren CJ. Atraumatic Restorative Treatment (ART) for Dental Caries. 1st edition. Nijmegen: STI Book bv; 1999. pp. 39–54. [Google Scholar]
- 5.Frencken JE, Pilot T, Songpaisan Y, et al. Atraumatic restorative treatment (ART) rationale, technique and development. J Public Health Dent. 1996;56(3):135–140. doi: 10.1111/j.1752-7325.1996.tb02423.x. [DOI] [PubMed] [Google Scholar]
- 6.Lo ECM, Luo Y, Fan MW, et al. Clinical investigation of two glass-ionomer restoratives used with the atraumatic restorative treatment approach in China: two-year results. Caries Res. 2001;35(6):458–563. doi: 10.1159/000047490. [DOI] [PubMed] [Google Scholar]
- 7.Lo ECM, Holmgren CJ. Provision of atraumatic restorative treatment (ART) restorations to Chinese pre-school children—a 30-month evaluation. Int J Paediatr Dent. 2001;11(1):3–10. doi: 10.1046/j.1365-263x.2001.00232.x. [DOI] [PubMed] [Google Scholar]
- 8.Honkala E, Behbehani J, Inbricevic H, et al. The atraumatic restorative treatment (ART) approach to restoring primary teeth in a standard dental clinic. Int J Paediatr Dent. 2003;13(3):172–179. doi: 10.1046/j.1365-263x.2003.00455.x. [DOI] [PubMed] [Google Scholar]
- 9.Phantumvanit P, Songpaisan Y, Pilot T, et al. Atraumatic restorative treatment (ART): a three-year community field trial in Thailand-survival of one-surface restorations in the permanent dentition. J Public Health Dent. 1996;56(3):141–145. doi: 10.1111/j.1752-7325.1996.tb02424.x. [DOI] [PubMed] [Google Scholar]
- 10.Salama FS, Riad MI, Abdel Megid FY. Microleakage and marginal gap formation of glass ionomer resin restorations. J Clin Pediatr Dent. 1995;20(1):31–36. [PubMed] [Google Scholar]
- 11.Mhaville RJ, Amerongen WE, Mandari GJ. Residual caries and marginal integrity in relation to class II glass ionomer restorations in primary molars. Eur Arch Peadiatr Dent. 2006;7(2):81–84. doi: 10.1007/BF03320819. [DOI] [PubMed] [Google Scholar]
- 12.Roeleveld AC, Amerongen WE, Mandari GJ. Influence of residual caries and survival gaps on the survival rate of the class II glass ionomer restorations. Eur Arch Paediatr Dent. 2006;7(2):85–91. doi: 10.1007/BF03320820. [DOI] [PubMed] [Google Scholar]
- 13.Frencken JE, Hof MA, Amerongen WE, et al. Effectiveness of single –surface ART restorations in the permanent dentition: a meta-analysis. J Dent Res. 2004;83(2):120–123. doi: 10.1177/154405910408300207. [DOI] [PubMed] [Google Scholar]
- 14.Frencken JE, Helderman WH, Holmgren CJ, et al. The atraumatic restorative treatment (ART) approach for managing dental caries: a meta-analysis. Int Dent J. 2006;56(6):345–351. doi: 10.1111/j.1875-595x.2006.tb00339.x. [DOI] [PubMed] [Google Scholar]
- 15.Frencken JE, Taifour D, van 't Hof MA. Survival of ART and amalgam restorations in permanent teeth of children after 6.3 years. J Dent Res. 2006;85(7):622–626. doi: 10.1177/154405910608500708. [DOI] [PubMed] [Google Scholar]
- 16.Bonifacio CC, Amerongen WE, Meschini TG, et al. Flowable glass ionomer cement as a liner: improving marginal adaptation of atraumatic restorative treatment restorations. J Dent Child. 2010;77(1):12–16. [PubMed] [Google Scholar]
- 17.Lenzi TL, Bonifácio CC, Bönecker M, et al. Flowable glass ionomer cement layer bonding to sound and carious primary dentin. J Dent Child. 2013;80(1):20–24. [PubMed] [Google Scholar]
- 18.McLean JW, Wilson AD. The clinical development of the glass-ionomer cement II. Some clinical applications. Aust Dent J. 1977;22(2):120–127. doi: 10.1111/j.1834-7819.1977.tb04463.x. [DOI] [PubMed] [Google Scholar]
- 19.Nicholson JW, Czarneka B. Kinetic studies of the effect of varnish on water loss by glass-ionomer cements. Dent Mater. 2007;23(12):1549–1552. doi: 10.1016/j.dental.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Brito CR, Velasco LG, Bonini GA, et al. Glass ionomer cement hardness after different materials for surface protection. J Biomed Mater Res. 2010;93(1):243–246. doi: 10.1002/jbm.a.32524. [DOI] [PubMed] [Google Scholar]
- 21.Moshaverinia A, Ansari S, Movasaghi Z, et al. Modification of conventional glass-ionomer cements with N-vinylpyrrolidone containing polyacids, nano-hydroxy and fluoroapatite to improve mechanical properties. Dent Mater. 2008;24(10):1381–1390. doi: 10.1016/j.dental.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 22.Hesse D, Bonifacio C, Bonecker M, et al. Survival rate of atraumatic restorative treatment (ART) restorations using a glass ionomer bilayer technique with a nanofilled coating: a bi–center randomized clinical trial. Pediatr Dent. 2016;38(1):18–24. [PubMed] [Google Scholar]
- 23.Lyapina M, Tzekova M, Dencheva M, et al. Nano glass ionomer cements in modern restorative dentistry. J Int Med Assoc Bulgaria. 2016;22(2):116–165. doi: 10.5272/jimab.2016222.1160. [DOI] [Google Scholar]
- 24.Hesse D, Bonifacio C, Bonecker M, et al. Bilayer technique and Nanofilled coating increases success of approximal ART restorations: a randomized clinical trial. Int J Paediatr Dent. 2016;26(3):231–239. doi: 10.1111/ipd.12194. [DOI] [PubMed] [Google Scholar]
- 25.Pukallus ML, Ploka KA, Holcombe TF, et al. A randomized controlled trial of a 10% CPP-ACP cream to reduce mutans streptococci colonization. Pediatr Dent. 2013;35(7):550–555. [PubMed] [Google Scholar]
- 26.Frencken J, Pilot T, Amerongen E, et al. Manual for the Atraumatic Restorative Treatment Approach to Control Dental Caries. 3rd edition. Groningen: Who Collaborating Centre for Oral Health Services Research; 1997. pp. 103–120. [Google Scholar]
- 27.Chkir AF, Salem KB, Volu KA. Atraumatic restorative treatment and glass ionomer sealants in Tunisian children: survival after 3 years. East Mediter Health J. 2002;23:200–204. [PubMed] [Google Scholar]
- 28.Anusavice KJ. Does ART have a place in preservative dentistry? Community Dent Oral Epidemiol. 1997;27(6):442–448. doi: 10.1111/j.1600-0528.1999.tb02046.x. [DOI] [PubMed] [Google Scholar]
- 29.Raggio DP, Hesse D, Lenzi TL, et al. Is ART an option for restoring occlusoproximal caries in primary teeth? A systematic review and meta-analysis. Int J Pediatr Dent. 2013;23(6):435–443. doi: 10.1111/ipd.12013. [DOI] [PubMed] [Google Scholar]
- 30.Bonifacio CC, de Jager N, Kleverlaan CJ. Mechanical behavior of a bi-layer glass ionomer. Dent Mater. 2013;29(10):1020–1025. doi: 10.1016/j.dental.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 31.Swiftr E, Perdigao J, Heymann HO. Bonding to enamel and dentin: a brief history and state of the art. Quintessence Int. 1995;26(2):95–110. [PubMed] [Google Scholar]
- 32.Ngo H, Mount G, Peters Me. A study of glass ionomer cement and its interface with enamel and dentin using a low-temperature, high-resolution scanning electron microscopic technique. Quintessence Int. 1997;28(1):63–69. [PubMed] [Google Scholar]
- 33.da Franca C, Colares V, Van Amerongen E. Two years evaluation of ART approach in primary molars class I and II restorations. Int J Peadiatr dent. 2011;21(4):249–253. doi: 10.1111/j.1365-263X.2011.01125.x. [DOI] [PubMed] [Google Scholar]
- 34.Bonifacio C, Hesse D, Raggio D, et al. The effect of GIC brand on the survival rate of proximal ART restorations. Int J. Pediatr Dent. 2013;23(4):251–258. doi: 10.1111/j.1365-263X.2012.01259.x. [DOI] [PubMed] [Google Scholar]
- 35.Deepa G, Shobha T. A clinical evaluation of two glass ionomer cements in primary molars using atraumatic restorative treatment technique in India: 1-year follow-up. Int J Paediatr Dent. 2010;20(6):410–418. doi: 10.1111/j.1365-263X.2010.01067.x. [DOI] [PubMed] [Google Scholar]
- 36.Amorim RG, Leal SC, Frencken JE. Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta-analysis. Clin Oral Investig. 2012;16(2):429–441. doi: 10.1007/s00784-011-0513-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frencken JE. Atraumatic restorative treatment and minimal intervention dentistry. Br Dent J. 2017;223(3):183–189. doi: 10.1038/sj.bdj.2017.664. [DOI] [PubMed] [Google Scholar]
- 38.Frencken JE, Makoni F, Sithole WD, et al. Three-year survival of one-surface ART restorations and glass-ionomer sealants in a school oral health programme in Zimbabwe. Caries Res. 1998;32(2):119–126. doi: 10.1159/000016441. [DOI] [PubMed] [Google Scholar]
- 39.Holmgren CJ, Lo EC, Hu D, et al. ART restorations and sealants placed in Chinese school children – results after three years. Community Dent Oral Epidemiol. 2000;28(4):314–320. doi: 10.1034/j.1600-0528.2000.280410.x. [DOI] [PubMed] [Google Scholar]
- 40.Ersin NK, Candan U, Aykut A, et al. A clinical evaluation of resin-based composite and glass ionomer cement restorations placed in primary teeth using the ART approach: results at 24 months. J Am Dent Assoc. 2006;137(11):1529–1536. doi: 10.14219/jada.archive.2006.0087. [DOI] [PubMed] [Google Scholar]
- 41.Cefaly DF, Barata Tde J, Tapety CM, et al. Clinical evaluation of multisurface ART restorations. J Appl Oral Sci. 2005;13(1):159. doi: 10.1590/s1678-77572005000100004. [DOI] [PubMed] [Google Scholar]
- 42.Mallow PK, Durward CS, Klaipo M. Restoration of permanent teeth in young rural children in Cambodia using the atraumatic restorative treatment (ART) thechnique and Fuji II glass ionomer cement. Int J Paediatr Dent. 1998;8(1):35–40. doi: 10.1046/j.1365-263x.1998.00058.x. [DOI] [PubMed] [Google Scholar]
- 43.De Gee AJ, van Duinen RN, Werner A, et al. Early and long-term wear of conventional and resin-modified glass ionomers. J Dent Res. 2006;75(8):1613–1619. doi: 10.1177/00220345960750081401. [DOI] [PubMed] [Google Scholar]
- 44.Mount GJ. Longevity in glass-ionomer restorations: review of a successful technique. Quintessence Int. 1997;28(10):643–650. [PubMed] [Google Scholar]
- 45.Kamatham R, Reddy J. Surface coatings on glass ionomer restorations in pediatric dentistry-Worthy or not? J Ind Soc Pedod Prev Dent. 2013;31(4):229–233. doi: 10.4103/0970-4388.121818. [DOI] [PubMed] [Google Scholar]
- 46.Lohbauer U, Krämer N, Siedschlag G, et al. Strength and wear resistance of a dental glass-ionomer cement with a novel nanofilled resin coating. Am J Dent. 2011;24(2):124–128. [PubMed] [Google Scholar]
- 47.Bonifacio CC, Werner A, Kleverlaan CJ. Coating glass-ionomer cements with a nanofilled resin. Acta Odontol Scand. 2012;70(6):471–477. doi: 10.3109/00016357.2011.639307. [DOI] [PubMed] [Google Scholar]
- 48.Bonifacio C, Kleverlaan CJ, Raggio DP, et al. Physical-mechanical properties of glass ionomer cements indicated for atraumatic restorative treatment. Aust Dent J. 2009;54(3):233–237. doi: 10.1111/j.1834-7819.2009.01125.x. [DOI] [PubMed] [Google Scholar]
- 49.Kikwilu E, Frencken J, Mulder J. Impact of atraumatic restorative treatment (ART) on the treatment profile in pilot government dental clinics in Tanzania. BMC Oral Health. 2009;9:1–7. doi: 10.1186/1472-6831-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Diem VT, Tyas MJ, Ngo HC, et al. The effect of a nano-filled resin coating on the 3-year clinical performance of a conventional high-viscosity glass ionomer cement. Clin Oral Investig. 2014;18(3):753–759. doi: 10.1007/s00784-013-1026-z. [DOI] [PubMed] [Google Scholar]
- 51.Fried K, Hiller KA, Friedl KH. Clinical performance of a new glass-ionomer based restoration system: a retrospective cohort study. Dent Mater. 2011;27(10):1031–1037. doi: 10.1016/j.dental.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 52.Fraji F, Heshmat H, Banava S. Effect of protective coating on microhardness of a new glasss ionomer cement: nanofilled coating versus unfilled resin: J Conserv Dent. 2017;20(4):260–263. doi: 10.4103/JCD.JCD_83_16. [DOI] [PMC free article] [PubMed] [Google Scholar]