Abstract
Introduction: Pediatric Early Warning Score (PEWS), also known as Brighton PEWS or Monaghan PEWS, was developed to identify children at risk for clinical deterioration in hospitals. We designed this study to describe the epidemiology of unintentional injuries in children admitted to the critical care unit in a tertiary healthcare setting, and to determine the predictive properties of PEWS in these injuries.
Methods: This is a cross-sectional study. Injury-related data were based on Haddon’s matrix of agent, host, and environment factors. Each child was evaluated using PEWS on admission. We noted the following outcomes: duration of stay in the intensive unit; major intervention required; and death.
Results: We analyzed data from 157 children. Most of the children were in the age group of one to five years (57.7%), followed by more than five to 12 years old (37.6%). The most common injuries were bites (35.7%), falls (24.2%), and poisoning (21.7%). These injuries occurred at home (52.7%) and in the presence of a caretaker (40.0%). On admission, 11% of children were classified as green, 40% as yellow, 36% as orange, and 13% as red by PEWS. Classification of red versus the rest (orange/yellow/green) had a high sensitivity (100%), specificity (88.3%), and negative predictive value (100%) for “death” as an outcome.
Conclusion: Most of the injuries occurred at home and at a time when the caretaker was around. Thus, it will be useful to develop “safe home interventions” and train parents in first aid to take care of these injuries on-site. Baseline PEWS was a good predictor of “poor” as well as “positive” outcomes. It may be worthwhile to implement this score regularly in the management of childhood injuries in hospitals.
Keywords: positive predictive value (ppv), adverse clinical outcomes, pediatric early warning score (pews), epidemiology study, unintentional childhood injuries
Introduction
Globally, injuries account for nearly 8% of total deaths and are among the top five leading causes of death [1]. Unintentional and transport-related injuries were responsible for 25% of the deaths in adolescents and 14% of disability-adjusted life years (DALYs) globally; it was higher in males compared with females [2]. Injuries account for about 6% of total deaths in children under the age of five years in India, and a recent study reported that the prevalence of unintentional injuries in children was 4.7% (95% confidence intervals 4.4% to 4.9%); falls were the most common and drowning-related injuries were the least common injuries [3,4]. Furthermore, even though the prevalence of injuries was higher in male children, burn-related injuries and poisonings were more common in females [5]. Thus, there appear to be epidemiological differences according to age and gender [6]. Furthermore, childhood injuries may also increase mental health illness, substance abuse, and social issues in these children [1].
Thus, it is important to manage these critical injuries appropriately in healthcare settings. One of the components of management is the early assessment of children admitted to emergency units and intensive care units. Pediatric Early Warning Score (PEWS) also known as Brighton PEWS or Monaghan PEWS was developed to identify children at risk for clinical deterioration in hospitals [7,8]. It also helps to identify children who may require intensive care or consultation [9]. The use of PEWS has increased in hospital settings from 2005 onward [10]. However, some authors argue that even though there is an increase in the use of PEWS, there is limited evidence of its effectiveness [10]. Other authors have, however, found that PEWS had a good predictive value for identifying poor outcomes (respiratory or cardiac arrest or unexpected deaths) [11]. Another recent systematic review found that even though PEWS is useful in the improvement of clinical and process outcomes, there was limited evidence of its role as a healthcare intervention [12]. There are other scores such as the pediatric index of mortality (PIM), the pediatric risk of mortality score (PRISM), and the pediatric logistic organ dysfunction-2 (PELOD-2); these scores have been used as predictors of mortality in intensive care units [13-15]. These scores usually require calculators and include many more parameters compared with PEWS. PRISM uses 14 parameters, the PIM-2 score has 10 variables, and the PELOD-2 uses 10 variables from five organ dysfunctions; these are clinical and biochemical parameters [13,16,17]. PEWS, however, is easy to score using three parameters (behavior, cardiovascular, and respiratory), and its implementation is associated with a reduction in clinical deterioration and hospital mortality - even in resource-limited settings [7,18,19]. Hence, if proven to be useful, it may be easy to replicate and use in rural and resource-limited settings.
With this background, we designed the present study with these specific objectives: 1) to describe the epidemiological profile of unintentional injuries in children admitted to the critical care unit in teaching hospital located in resource-limited settings and 2) to evaluate the test properties (sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and area under the curve (AUC)) of PEWS for clinical outcomes of these injuries.
Materials and methods
The present study is a cross-sectional analysis of data collected from children who presented with unintentional injuries and were admitted to the critical care unit over a period of 17 months from February 2017 to July 2018.
Study site and population
The study was conducted in the Pediatric Intensive Care Unit (PICU) of the Department of Pediatrics of MGM Hospital, Navi Mumbai, India. This is a teaching hospital located about 50 km from Mumbai. The hospital has an eight-bed PICU, with 45-50 admissions per month. A consecutive sample of children aged one month to twelve years of age who presented with unintentional injuries in the emergency department and were admitted to the PICU were included in the present analysis. The cases which were proven or suspected of intentional injuries were excluded.
Study procedure and variables
Detailed information was recorded in a pre-designed form. The variables in the data collection sheet were based on Haddon’s matrix [20] of host, environment, and agent factors. The host factors were age; sex; and socio-economic class based on the Kuppuswamy scale (divided into five groups - upper, upper middle, lower middle, upper lower, and lower) [21]. The environmental factors were time of injury (morning 8 am to 4 pm, evening 4 pm to 10 pm, night 10 pm to 8 am); day of injury (weekday and weekend); place of injury (road, home, school, playground, others); presence of caretaker (nobody, parent or other); and time to hospitalization (up to one hour, one hour to <6 hours, >=6 hours). At the time of presentation, the injuries were classified into the following types: accidental poisoning; foreign body injuries; drowning; bites; burns; falls; and road traffic accidents (RTAs). For analysis in the tables, we have grouped these into poisoning, bites, falls, RTAs, and others (due to small numbers in these categories). We classified age into three categories: up to 12 months of age (neonates and infants); more than 12 months to five years of age (toddlers and preschool children), and more than five years to 12 years of age (school-going children). The care of the child and movement within and outside the house may differ in these groups. We also recorded details on agent factors: poisoning (such as kerosene, insect repellant, rat poison, camphor, turpentine oil, diesel, gas cleaner, or any other agent), type of foreign body ingestion, drowning (such as fresh water, seawater, bucket, or bathtub), bites (cause of bites and the body part affected), burns (thermal or electric), fall (fall from height, fall from stairs, fall from the level ground; and the body parts injured), and road traffic accidents (type of injury - abrasion, contusion, laceration, or fracture, body part affected, and whether the injured child was the pedestrian or the passenger).
At the time of admission to the PICU, each child was evaluated using the PEWS [7,19]. Three parameters were considered for allocating scores: behavior; cardiovascular; and respiratory. They were scored on a scale of 0-3. The components included the following parameters: 1) behavior including patient’s level of consciousness (playing/appropriate, sleeping, irritable, and lethargic/reduced response to pain); 2) cardiovascular parameters such as color or capillary refill time and heart rate (based on age-appropriate cut-offs); and 3) respiratory parameters included respiratory rate (age-specific mean respiratory rates), use of accessory muscles, sternal recession, tracheal tug and grunting, liters of O2 needed for maintaining saturation of 98%-100%. An additional score of 2 was added for ¼ hourly nebulizers or persistent vomiting following surgery [7, 19]. PEWS were graded as Green (0-2), Yellow (3), Orange (4), or Red (5+) indicating low(green), medium (yellow or orange), and high (red) risk for deterioration. We also recorded the clinical course of the child in the PICU. We recorded the following outcomes in the PICU: duration of stay in the PICU, any major intervention (defined as ventilation or surgical procedure) required during the stay in the PICU, and death.
Statistical analysis
With a sample size of 157, we had >90% power and alpha of 0.05, to detect an AUC of 0.86 from the receiver operating characteristics (ROC) curve for ICU admission for PEWS score (based on a previous study by Gold and colleagues [19]). This also included a 5% inflation of sample size to account for missing data. The sample size was estimated using the formula for “Sample Size for Single ROC curve.” This sample size also had enough power for epidemiological data of 35% of road traffic accidents (also reported previously [22]). The sample size of 157 had 90% power, with an alpha of 0.05 and a delta of 0.125. The sample size was estimated using Stata version 17 (StataCorp, College Station, TX, USA).
Data were entered in MS Excel (Microsoft, Washington, DC, USA) and analyzed using Stata version 15.1 (Stata Corp.). We estimated the mean and standard deviation (SD) for the linear variable. We estimated the proportions for categorical variables; these proportions across various groups were compared using the chi-square test or Fisher’s exact test for low expected cell counts. The means were compared using the t-test for two groups or analysis of variance for more than two groups. We then used the logistic regression models for multivariate analysis and estimated the odds ratio (OR) and their 95% confidence intervals (CI). These models were used to study the factors (host and environment factors) associated with different types of injuries. We also estimated the diagnostic test properties of the PEWS for clinical outcomes (stay for more than one day, major intervention required, and death) in these children. We plotted the receiver operating characteristics curve (ROC). We estimated the AUC from these ROC curves, sensitivity, specificity, PPV, and NPV for these diagnostic test properties. A “p” value of <0.05 was considered statistically significant. The study was approved by the Ethics Committee at Mahatma Gandhi Missions (MGM) Medical College, Navi Mumbai, India (Reference No. 2017/04/SC/76, date: May 2, 2017).
Results
We present the results from 157 children admitted to the intensive care unit. The majority of the children admitted with unintentional injuries to the critical care unit were in the age group of one to five years (57.7% (n=91)), followed by more than five years to 12 years (37.6% (n=59)); the proportion of males was higher (58.6% (n=92)) compared with females (41.4% (n=65)). The children were in the lower (26.1% (n=41)) and upper lower (69.4% (n=109)) socio-economic status. The most common injuries were bites (35.7% (n=56)), falls (24.2% (n=38)), and poisoning (21.7% (n=34)). The majority of the injuries occurred in the evenings (53.5% (n=84)) and weekdays (73.9% (n=116)). Most of the injuries were at home (52.7% (n=83)), on the playground (19.7% (n=31)), and on roads (17.9% (n=28)). Though a caretaker (mother) was present at the time of injury in about 40% (n=62) of the cases, no caretaker was present in 26% (n=41) of these cases. We have presented detailed descriptive data in Table 1.
Table 1. Number and proportions (%) according to host and environment factors in 157 children with injuries admitted to the critical care unit, Navi Mumbai, India.
The total column uses 157 as the denominator and the other % are for row total except for total (which is column percentage)
| Characteristics | Total | Poisoning | Bites | Falls | Road traffic accidents | Others | P-value |
| N (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| All children | 157 (100) | 34 (21.7) | 56 (35.7) | 38 (24.2) | 19 (12.1) | 10 (6.4) | |
| Host factors | |||||||
| 1 month - 12 months | 7 (4.5) | 1 (14.3) | 3 (42.9) | 3 (42.9) | 0 (0) | 0 (0) | <0.001 |
| >12 months - 5 years | 91 (57.7) | 28 (30.8) | 18 (19.8) | 25 (27.5) | 11 (12.1) | 9 (9.9) | |
| >5 years - 12 years | 59 (37.6) | 5 (8.5) | 35 (59.3) | 10 (16.9) | 8 (13.6) | 1 (1.7) | |
| Sex | |||||||
| Female | 65 (41.4) | 18 (27.7) | 18 (27.7) | 14 (21.5) | 9 (13.8) | 6 (9.2) | 0.21 |
| Male | 92 (58.6) | 16 (17.4) | 38 (41.3) | 24 (26.1) | 10 (10.9) | 4 (4.4) | |
| Socio-economic class | |||||||
| Lower middle | 7 (4.5) | 4 (57.1) | 1 (14.3) | 1 (14.3) | 0 (0) | 1 (14.3) | 0.001 |
| Upper lower | 109 (69.4) | 18 (16.5) | 32 (29.4) | 34 (31.2) | 17 (15.6) | 8 (7.3) | |
| Lower | 41 (26.1) | 12 (29.3) | 23 (56.1) | 3 (7.3) | 2 (4.9) | 4 (9.1) | |
| Environment factors | |||||||
| Time of injury | |||||||
| Morning | 59 (37.6) | 18 (30.5) | 15 (25.4) | 19 (32.2) | 3 (5.1) | 4 (6.8) | 0.031 |
| Evening | 84 (53.5) | 14 (16.7) | 32 (38.1) | 18 (21.4) | 14 (16.7) | 6 (7.1) | |
| Night | 14 (9.0) | 2 (14.3) | 9 (64.3) | 1 (7.1) | 2 (14.3) | 0 (0) | |
| Day of week | |||||||
| Weekday | 116 (73.9) | 27 (23.3) | 40 (34.5) | 27 (23.3) | 16 (13.8) | 6 (5.2) | 0.58 |
| Weekend | 41 (26.1) | 7 (17.1) | 16 (39.0) | 11 (26.8) | 3 (7.3) | 4 (9.8) | |
| Time to hospitalization | |||||||
| Up to 1 hour | 92 (58.6) | 25 (27.2) | 18 (19.6) | 30 (32.6) | 12 (13) | 7 (7.6) | <0.001 |
| >1 hour to <6 hours | 62 (39.5) | 8 (12.9) | 37 (59.7) | 8 (12.9) | 6 (9.7) | 3 (4.8) | |
| >=6 hours | 3 (1.9) | 1 (33.3) | 1 (33.3) | 0 (0) | 1 (33.3) | 0 (0.0) | |
| Place of injury | |||||||
| Road | 28 (17.9) | 0 (0) | 7 (25.0) | 2 (7.1) | 19 (67.9) | 0 (0) | <0.001 |
| Home | 83 (52.7) | 30 (36.1) | 21 (25.3) | 26 (31.3) | 0 (0) | 6 (7.2) | |
| School | 5 (3.2) | 0 (0) | 1 (20.0) | 3 (60.0) | 0 (0) | 1 (20.0) | |
| Playground | 31 (19.7) | 4 (12.9) | 20 (64.5) | 6 (19.4) | 0 (0) | 1 (3.2) | |
| Others | 10 (6.4) | 0 (0) | 7 (70.0) | 1 (10.0) | 0 (0) | 2 (20.0) | |
| Caretaker at time of injury | |||||||
| Father | 18 (11.5) | 2 (11.1) | 10 (55.6) | 1 (5.6) | 5 (27.8) | 0 (0) | <0.001 |
| Mother | 62 (39.5) | 21 (33.9) | 9 (14.5) | 18 (29.0) | 9 (14.5) | 5 (8.1) | |
| Both parents | 24 (15.3) | 3 (12.5) | 4 (16.7) | 12 (50.0) | 4 (16.7) | 1 (4.2) | |
| Relatives | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Neighbor | 2 (1.3) | 0 (0) | 2 (100.0) | 0 (0) | 0 (0) | 0 (0) | |
| Others | 10 (6.4) | 0 (0) | 5 (50.0) | 3 (30.0) | 0 (0) | 2 (20.0) | |
| None | 41 (26.1) | 8 (19.5) | 26 (63.4) | 4 (9.8) | 1 (2.4) | 2 (4.9) |
In the multivariate analysis, we found that poisoning was significantly more common at home than in other places (OR: 8.34, 95% CI: 2.46, 28.29; p < 0.001). Bites were less likely in children aged one to five years compared with those up to 12 months (OR: 0.13, 95% CI: 0.02, 0.94; p < 0.05) (reference category up to 12 months). Bites were also significantly less likely when parents were present (OR: 0.19, 95% CI: 0.07, 0.48; p < 0.01); however, they were significantly more likely in the night (OR: 10.42, 95% CI: 2.23, 48.71; p < 0.05). Falls were significantly less likely at night compared with morning (OR: 0.11, 95% CI: 0.01, 0.99; p < 0.05) (reference category - “morning”). Road traffic accidents were significantly more common when children were with parents compared with when parents were not present (OR: 12.51, OR: 1.53, >100.0; p < 0.01) (reference category - “parents not present”). We have presented ORs and their 95% confidence intervals for these multivariate models in Table 2.
Table 2. Odds ratios (ORs) and 95% confidence intervals (CIs) of association between host and environment factors and the type of injury.
Significance *p<0.05, **p<0.01
| Variables | Poisoning | Bites | Falls | Road traffic accidents |
| OR (95% CIs) | OR (95% CIs) | OR (95% CIs) | OR (95% CIs) | |
| Age group | ||||
| 1 month - 12 months | Reference | Reference | Reference | Reference |
| >12 months - 5 years | 6.16 (0.63, 59.92) | 0.13 (0.02, 0.94)* | 0.56 (0.09, 3.40) | Reference |
| >5 years - 12 years | 2.85 (0.24, 33.86) | 0.72 (0.10, 5.42) | 0.38 (0.05, 2.67) | 1.57 (0.52, 4.76) |
| Sex | ||||
| Female | Reference | Reference | Reference | Reference |
| Male | 0.48 (0.20, 1.18) | 2.25 (0.94, 5.37) | 1.57 (0.68, 3.63) | 0.71 (0.25, 2.01) |
| Socioeconomic class | ||||
| Lower middle | Reference | Reference | Reference | Reference |
| Upper Lower | 0.32 (0.05, 1.90) | 1.29 (0.11, 14.64) | 6.22 (0.66, 58.26) | Reference |
| Lower | 0.67 (0.10, 4.40) | 5.86 (0.48, 70.88) | 0.95 (0.08, 11.34) | 0.35 (0.07, 1.74) |
| Caretaker | ||||
| No parents | Reference | Reference | Reference | Reference |
| Parents present | 1.07 (0.35, 3.27) | 0.19 (0.07, 0.48)** | 1.64 (0.59, 4.56) | 12.51 (1.53, >100)* |
| Time of day | ||||
| Morning | Reference | Reference | Reference | Reference |
| Evening | 0.64 (0.25, 1.67) | 1.98 (0.76, 5.18) | 0.61 (0.26, 1.44) | 3.77 (0.98, 14.67) |
| Night | -- | 10.42 (2.23, 48.71)* | 0.11 (0.01, 0.99)* | 2.10 (0.28, 15.67) |
| Day of week | ||||
| Weekday | Reference | Reference | Reference | Reference |
| Weekend | 0.52 (0.17, 1.54) | 1.04 (0.39, 2.79) | 1.40 (0.56, 3.53) | 0.47 (0.12, 1.89) |
| Place of injury | ||||
| Not home | Reference | Reference | Reference | -- |
| At home | 8.34 (2.46, 28.29)** | 0.88 (0.33, 2.32) | 2.02 (0.80, 5.09) | -- |
The mean (SD) PEWS on admission was 3.48 (1.23). The mean (SD) PEWS was significantly higher in children who died compared with those who did not (6.33 (1.15) vs 3.42 (1.18); p<0.001). Similarly, the mean (SD) PEWS values were significantly higher in those who had any “major intervention” compared with those who did not (5.33 (1.53) vs 3.44 (1.21); p=0.01). We have presented the means and SDs in Table 3. On admission, 11% (n=17) of children were classified as green, 40% (n=62) as yellow, 36% (n=57) as orange, and 13% (n=21) as red by PEWS. There was no association between age and category of PEWS (p=0.08). There was a significant association between the type of injury and PEWS scoring (p<0.001). A higher proportion of burns and road traffic accidents were classified as orange or red on the PEWS score (Table 4). Among those who were admitted to the PICU for only one day (n=68), 4% (n=3) were classified as red on admission; the proportion was 15% (n=8) in those who were admitted to the PICU for two days (n=53), and it was 28% (n=10) in those who were admitted to the PICU for more than two days (n=36). There appeared to be a significant association between the duration of stay in the PICU and PEWS classification on admission (p < 0.01). We also found that all the deaths were classified as red on admission. All children who required major intervention were classified as orange or red on PEWS. We have presented detailed proportions for PEWS categories in Table 4.
Table 3. Means and standard deviations (SDs) of Pediatric Early Warning System (PEWS) score according to demographic and injury-related characteristics, Navi Mumbai, India.
The total row shows column percentage, and the PEWS value column shows mean and standard deviation in parentheses
| Characteristics | All | PEWS value | P-value |
| N (%) | Mean (SD) | ||
| Total | 157 (100.0) | 3.48 (1.24) | |
| Age | |||
| 1 month - 12 months | 7 (4.5) | 3.71 (1.11) | 0.21 |
| >12 months - 5 years | 91 (58.0) | 3.33 (1.07) | |
| >5 years - 12 years | 59 (37.6) | 3.68 (1.47) | |
| Type of injury | |||
| Poisoning | 34 (21.7) | 3.29 (0.68) | 0.04 |
| Bites | 56 (35.7) | 3.75 (1.70) | |
| Falls | 38 (24.2) | 3.05 (0.73) | |
| Road traffic accidents | 19 (12.1) | 3.89 (0.99) | |
| Others | 10 (6.4) | 3.40 (1.17) | |
| Time to hospitalization | |||
| < 1 hour | 92 (58.6) | 3.30 (0.90) | 0.01 |
| > 1 hour to < 6 hours | 62 (39.5) | 3.79 (1.54) | |
| >= 6 hours | 3 (1.9) | 2.33 (2.08) | |
| Outcome | |||
| Discharge | 0 (0) | -- | <0.001 |
| Transfer to ward | 154 (98.1) | 3.42 (1.18) | |
| Death | 3 (1.9) | 6.33 (1.15) | |
| Duration of stay in PICU | |||
| 1 day | 68 (43.3) | 2.71 (1.23) | <0.001 |
| 2 days | 53 (33.8) | 3.96 (0.88) | |
| > 2 days | 36 (22.9) | 4.22 (0.83) | |
| Major intervention required | |||
| No | 154 (98.1) | 3.44 (1.21) | 0.01 |
| Yes | 3 (1.9) | 5.33 (1.53) |
Table 4. Number and proportions (%) of distribution of Pediatric Early Warning System (PEWS) score according to demographic and injury-related characteristics, Navi Mumbai, India.
The total column uses 157 as the denominator and the other %s are for row total except for total (which is column percentage) (significance * p<0.001)
| Characteristics | All | PEWS-Green | PEWS-Yellow | PEWS-Orange | PEWS-Red |
| N (%) | n (%) | n (%) | n (%) | n (%) | |
| Total | 157 (100.0) | 17 (10.8) | 62 (39.5) | 57 (36.3) | 21 (13.4) |
| Age | |||||
| 1 month - 12 months | 7 (4.5) | 0 (0) | 4 (57.1) | 2 (28.6) | 1 (14.3) |
| >12 months - 5 years | 91 (58.0) | 12 (13.2) | 36 (39.6) | 37 (40.7) | 6 (6.6) |
| >5 years - 12 years | 59 (37.6) | 5 (8.5) | 22 (37.3) | 18 (30.5) | 14 (23.7) |
| Type of injury* | |||||
| Poisoning | 34 (21.7) | 2 (5.9) | 19 (55.9) | 13 (38.2) | 0 (0) |
| Bites | 56 (35.7) | 8 (14.3) | 10 (17.9) | 21 (37.5) | 17 (30.4) |
| Falls | 38 (24.2) | 5 (13.2) | 24 (63.2) | 9 (23.7) | 0 (0) |
| Road traffic accidents | 19 (12.1) | 0 (0) | 7 (36.8) | 9 (47.4) | 3 (15.8) |
| Others | 10 (6.4) | 2 (20.0) | 2 (20.0) | 5 (50.0) | 1 (10.0) |
| Time to hospitalization* | |||||
| Up to 1 hour | 92 (58.6) | 9 (9.8) | 44 (47.8) | 36 (39.1) | 3 (3.3) |
| > 1 hour to < 6 hours | 62 (39.5) | 7 (11.3) | 17 (27.4) | 20 (32.3) | 18 (29) |
| >= 6 hours | 3 (1.9) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 0 (0) |
| Outcome* | |||||
| Discharge | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Transfer to ward | 154 (98.1) | 17 (11.0) | 62 (40.3) | 57 (37.0) | 18 (11.7) |
| Death | 3 (1.9) | 0 (0) | 0 (0) | 0 (0) | 3 (100.0) |
| Duration of stay in PICU* | |||||
| 1 day | 68 (43.3) | 17 (25) | 42 (61.8) | 6 (8.8) | 3 (4.4) |
| 2 days | 53 (33.8) | 0 (0) | 15 (28.3) | 30 (56.6) | 8 (15.1) |
| >2 days | 36 (22.9) | 0 (0) | 5 (13.9) | 21 (58.3) | 10 (27.8) |
| Major Intervention required | |||||
| No | 154 (98.1) | 17 (11.0) | 62 (40.3) | 56 (36.4) | 19 (12.3) |
| Yes | 3 (1.9) | 0 (0) | 0 (0) | 1 (33.3) | 2 (66.6) |
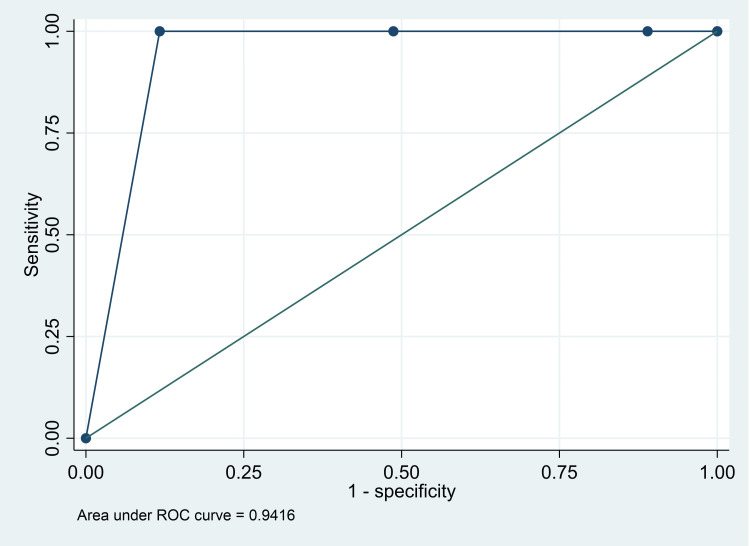
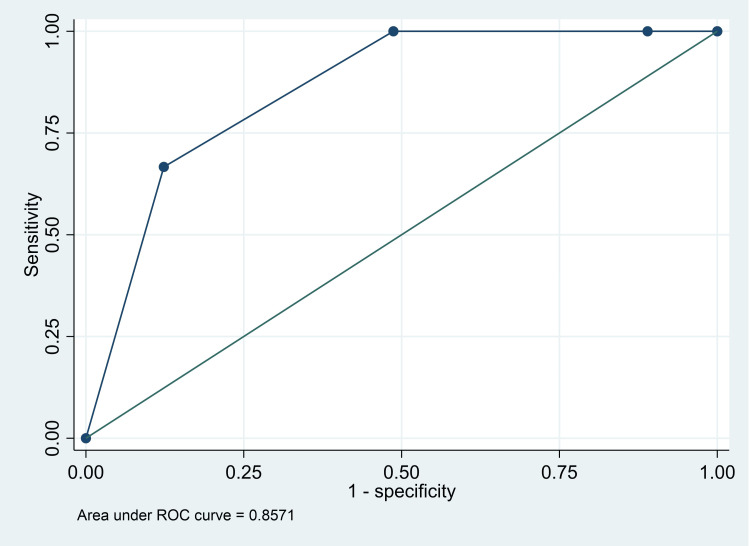
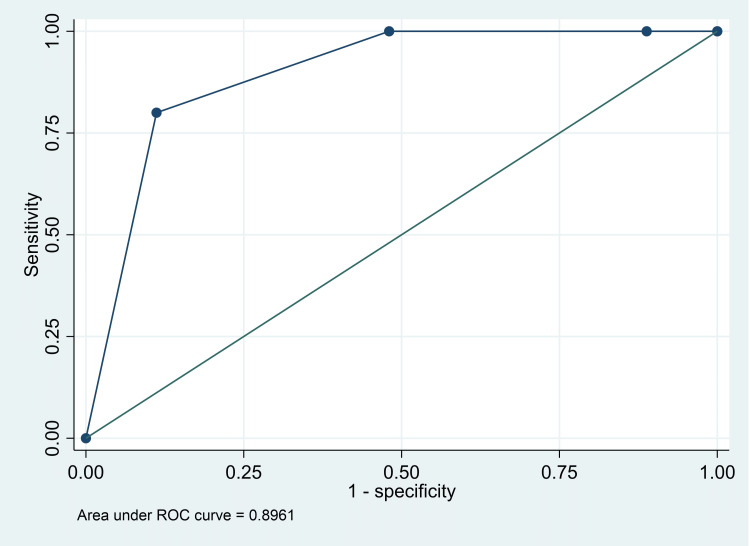
The AUC for death was 0.94 (95% CI: 0.92, 0.97), for major intervention was 0.86 (95% CI: 0.69, 1.00), and for either death or major intervention was 0.90 (95% CI: 80, 0.99) (Figures 1-3). The Classification of red versus the rest (orange/yellow/green) had a high sensitivity (100%; 95% CI: 29.2%, 100%), specificity (88.3%; 95% CI: 82.2%, 92.9%), and NPV (100%; 95% CI: 97.3%, 100%) for “death” as an outcome. However, the classification of red and orange versus yellow and green had good sensitivity (100%; 95% CI: 29.2%, 100%) and NPV (100%, 95% CI: 95.4%, 100%) for “major intervention required” as an outcome. Finally, classification of yellow and green versus orange and red had good sensitivity (86.8%; 95% CI: 76.4%, 93.8%), specificity (77.5%; 95% CI: 67.4%, 85.7%), PPV (74.7%; 95% CI: 63.6%, 83.8%), and NPV (88.5%; 95% CI: 79.2%, 94.6%) for “admission in the PICU for only one day” - considered as a good outcome (Table 5).
Table 5. Sensitivity, specificity, positive predictive value, negative predictive value, area under the curve (AUC) and their 95% confidence intervals (95% CI) of Pediatric Early Warning Score (PEWS) score in select clinical outcomes in children who presented with critical injuries, Navi Mumbai, India.
The data are presented as the estimate of measure along with its 95% confidence interval
| Outcomes | Sensitivity (95% CI) | Specificity (95% CI) | Positive predictive value (95% CI) | Negative predictive value (95% CI) | AUC (95% CI) |
| Death | |||||
| Orange & red/yellow & green | 100% (29.2%, 100%) | 51.3% (43.1%, 59.4%) | 3.9% (0.8%, 10.8%) | 100% (95.4%, 100%) | 0.76 (0.72, 0.80) |
| Red/orange & yellow & green | 100% (29.2%, 100%) | 88.3% (82.2%, 92.9%) | 14.3% (3.1%, 36.3%) | 100% (97.3%, 100%) | 0.94 (0.92, 0.97) |
| Major intervention required | |||||
| Orange & red/yellow & green | 100% (29.2%, 100%) | 51.3% (43.1%, 59.4%) | 3.9% (0.8%, 10.8%) | 100% (95.4%, 100%) | 0.76 (0.72, 0.80) |
| Red/orange & yellow & green | 66.7% (9.4%, 99.2%) | 87.7% (81.4%, 92.4%) | 9.5% (1.2%, 30.4%) | 99.3% (96.0%, 100%) | 0.77 (0.44, 1.00) |
| Admitted for only 1 day in PICU | |||||
| Yellow & green/orange & red | 86.8% (76.4%, 93.8%) | 77.5% (67.4%, 85.7%) | 74.7% (63.6%, 83.8%) | 88.5% (79.2%, 94.6%) | 0.82 (0.76, 0.88) |
| Green/yellow & orange & red | 25% (15.3%, 37%) | 100% (95.9%, 100%) | 100% (80.5%, 100%) | 73.6%, (55%, 71.5%) | 0.63 (0.57, 0.68) |
Figure 1. Receiver operating characteristics curve for PEWS score and “death” as an outcome.
PEWS: Pediatric Early Warning Score
Figure 2. Receiver operating characteristics curve for PEWS score and “major intervention” as an outcome.
PEWS: Pediatric Early Warning Score
Figure 3. Receiver operating characteristics curve for PEWS score and “death or major intervention” as an outcome.
PEWS: Pediatric Early Warning Score
Discussion
Thus, we found that the majority of the children admitted with critical injuries to the intensive care unit were in the age group of one to five years. The most common injuries were bites, falls, and poisoning (21.7%). In our study nearly half the children with critical injuries were classified as orange or red, and the other half as green or yellow. PEWS classification “red” had good sensitivity and specificity for “death” as an outcome; whereas PEWS classification “orange/red” had good sensitivity and specificity for “major intervention required.” However, the yellow/green classification on PEWS had good sensitivity for better outcomes - admission in the PICU for only one day.
The Global Burden of Disease dataset reported that unintentional injuries were responsible for about 686.49 DALYs per 100,000 population in children globally and 862.27 per 100,000 in India; it is the third cause of DALYs in India [23]. The important contributors to DALYs globally were road injuries (3.97%), drowning (2.50%), falls (1.31%), animal bites (0.82%), and foreign bodies (0.44%). In India, drowning (2.8%), road injuries (2.26%), animal bites (2.04%), and falls (1.5%) were the four important contributors to total DALYs [22]. In our study, bites and falls were the common injuries admitted to the PICU. Another study from Nigeria found that road traffic accidents, foreign bodies, and injuries were common childhood injuries [24]. However, another study from North India reported that falls (35%) were the most common childhood injuries [22]. We may have seen a lot of bites and falls compared with other Indian and international studies because the area covered by our hospital is largely rural and tribal with a hilly terrain. Thus, children are more likely to be exposed to animals (including wild animals), and due to the terrain, they are more likely to experience falls.
As seen in our study, the proportion of males presenting with injuries is higher compared with females [6,23]. A study from South India reported that the occurrence of road traffic accidents was nearly the same in males and females [25]; we found that the proportion was slightly higher in females compared with males. We had indicated earlier that the terrain covered by our hospital was hilly and tribal. Thus, girls who help their mothers in household work may be exposed to injuries as they try to negotiate the roads in this terrain. As seen in our population, most of the childhood injuries occurred at home [3]. Thus, it is important to create intervention programs aimed at increasing the safety of children at home (such as child-safe kitchens and water-holding areas) and train parents (particularly mothers) in first aid.
PEWS is an important early warning system in critical situations in children and is useful in identifying children at risk of deterioration in the ICU and monitoring the severity of clinical conditions [26,27]. In our study population - unintentional injuries admitted to the critical care unit - we did find that PEWS has good test properties not only in identifying children who may have poor outcomes but also those children who may have good outcomes (stayed in the ICU for one day only). The AUC was best for death followed by major intervention required in these children with injuries. Authors have also found that regular use of PEWS helped in improving interdisciplinary dynamics and emphasized the role of patient safety in healthcare settings [28]. Thus, it will be useful to include this bedside score in the triage of pediatric patients in the emergency unit, as well as in clinical management and decision-making for pediatric patients admitted to the hospital intensive care units or wards.
The study had its limitations. For instance, we monitored PEWS only at baseline (at the time of admission) to the intensive care unit. Though we did find baseline PEWS has good NPV for poor clinical outcomes in these children, repeated PEWS would probably be useful to monitor the progress of the child during the hospital stay. In addition, we did not include the facilitators and barriers to the administration of PEWS in clinical settings. Agulnik and colleagues have reported that beneficial outcomes in patients and support by supervisors/leaders were facilitators for its implementation, whereas staff turnover and COVID-19 hampered the regular administration of PEWS in hospital settings [29,30].
Conclusions
Nonetheless, the study provides useful evidence on unintentional childhood injuries admitted to the critical care units and the role of PEWS for clinical outcomes of injuries in resource-limited healthcare settings. The most common injuries were bites, falls, and poisonings. Most of these injuries occurred at home and at a time when the caretaker (usually one or both parents) was around. Thus, we should develop “safe home interventions” to prevent injuries at home and parents should be trained in first aid to take care of these injuries on-site. Baseline PEWS had good NPV for “poor” and good PPV for “positive” outcomes in children who present with unintentional injuries. Easily administered, it may be worthwhile to implement PEWS regularly in the management of childhood injuries in hospitals in rural and resource-limited settings. Children who score green or yellow on the PEWS score may be managed in high-dependency units, and not overburden the intensive care units in resource-limited settings.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Ethics Committee at Mahatma Gandhi Missions (MGM) Medical College, Navi Mumbai, India issued approval Reference No. 2017/04/SC/76.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Acquisition, analysis, or interpretation of data: Maninder S. Setia, Sagar Malde, Prajvi Jain
Drafting of the manuscript: Maninder S. Setia, Sagar Malde, Prajvi Jain, Bageshree Seth
Concept and design: Sagar Malde, Natesan Revathi, Bageshree Seth
Critical review of the manuscript for important intellectual content: Natesan Revathi
Supervision: Natesan Revathi, Bageshree Seth
References
- 1.Injuries and violence. [ Jan; 2023 ]. 2021. https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence
- 2.Adolescent transport and unintentional injuries: a systematic analysis using the Global Burden of Disease Study 2019. Global Burden of Disease Adolescent Transport Unintentional Injuries Collaborators. Lancet Public Health. 2022;7:0–69. doi: 10.1016/S2468-2667(22)00134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.A review of Epidemiology of unintentional injuries among children in India. Jospeh A, Kumar D, Edward KD. Indian J Public Health Res Development. 2019;10:114–118. [Google Scholar]
- 4.Descriptive epidemiology of unintentional childhood injuries in India: an ICMR taskforce multisite study. Nooyi SC, Sonaliya KN, Dhingra B, et al. Indian Pediatr. 2021;58:517–524. [PubMed] [Google Scholar]
- 5.A study on epidemiology of unintentional childhood injury at one of the districts of Gujarat state: an Indian Council of Medical Research task force study. Dave VR, Rana BM, Shah VR, Sonaliya KN. Indian J Community Med. 2022;47:187–191. doi: 10.4103/ijcm.ijcm_1275_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Profile and risk factor analysis of unintentional injuries in children. Bhamkar R, Seth B, Setia MS. Indian J Pediatr. 2016;83:1114–1120. doi: 10.1007/s12098-016-2159-2. [DOI] [PubMed] [Google Scholar]
- 7.Detecting and managing deterioration in children. Monaghan A. Paediatr Nurs. 2005;17:32–35. doi: 10.7748/paed2005.02.17.1.32.c964. [DOI] [PubMed] [Google Scholar]
- 8.Calculated decisions: pediatric early warning score (PEWS) Kwon R. https://www.ebmedicine.net/media_library/files/mHealth_in_Emergency_Medicine_and_Nick's_Picks_Calculated_Decisions.pdf. Emerg Med Pract. 2017;Suppl 2017B:12–13. [PubMed] [Google Scholar]
- 9.Paediatric early warning systems (PEWS and Trigger systems) for the hospitalised child: time to focus on the evidence. Lillitos PJ, Maconochie IK. Arch Dis Child. 2017;102:479–480. doi: 10.1136/archdischild-2016-312136. [DOI] [PubMed] [Google Scholar]
- 10.Use of paediatric early warning systems in Great Britain: has there been a change of practice in the last 7 years? Roland D, Oliver A, Edwards ED, Mason BW, Powell CV. Arch Dis Child. 2014;99:26–29. doi: 10.1136/archdischild-2012-302783. [DOI] [PubMed] [Google Scholar]
- 11.'The Score Matters': wide variations in predictive performance of 18 paediatric track and trigger systems. Chapman SM, Wray J, Oulton K, Pagel C, Ray S, Peters MJ. Arch Dis Child. 2017;102:487–495. doi: 10.1136/archdischild-2016-311088. [DOI] [PubMed] [Google Scholar]
- 12.Paediatric early warning systems for detecting and responding to clinical deterioration in children: a systematic review. Lambert V, Matthews A, MacDonell R, Fitzsimons J. BMJ Open. 2017;7:0. doi: 10.1136/bmjopen-2016-014497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pediatric logistic organ dysfunction-2 (PELOD-2) score as a model for predicting mortality in pediatric burn injury. Dewi W, Christie CD, Wardhana A, Fadhilah R, Pardede SO. https://www.ncbi.nlm.nih.gov/pubmed/31528154. Ann Burns Fire Disasters. 2019;32:135–142. [PMC free article] [PubMed] [Google Scholar]
- 14.Comparison of outcomes using pediatric index of mortality (PIM) -3 and Pim-2 models in a pediatric intensive care unit. Sankar J, Gulla KM, Kumar UV, Lodha R, Kabra SK. https://www.ncbi.nlm.nih.gov/pubmed/30587646. Indian Pediatr. 2018;55:972–974. [PubMed] [Google Scholar]
- 15.Reliability of PRISM and PIM scores in paediatric intensive care. van Keulen JG, Polderman KH, Gemke RJ. Arch Dis Child. 2005;90:211–214. doi: 10.1136/adc.2003.046722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Application of the pediatric risk of mortality (PRISM) score and determination of mortality risk factors in a tertiary pediatric intensive care unit. Costa GA, Delgado AF, Ferraro A, Okay TS. Clinics (Sao Paulo) 2010;65:1087–1092. doi: 10.1590/S1807-59322010001100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pediatric index of mortality 2 score as an outcome predictor in pediatric intensive care unit in India. Gandhi J, Sangareddi S, Varadarajan P, Suresh S. Indian J Crit Care Med. 2013;17:288–291. doi: 10.4103/0972-5229.120320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scoping review of pediatric early warning systems (PEWS) in resource-limited and humanitarian settings. Brown SR, Martinez Garcia D, Agulnik A. Front Pediatr. 2018;6:410. doi: 10.3389/fped.2018.00410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evaluating the pediatric early warning score (PEWS) system for admitted patients in the pediatric emergency department. Gold DL, Mihalov LK, Cohen DM. Acad Emerg Med. 2014;21:1249–1256. doi: 10.1111/acem.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Advances in the epidemiology of injuries as a basis for public policy. Haddon W Jr. https://www.ncbi.nlm.nih.gov/pubmed/7422807 . Public Health Rep. 1980;95:411–421. [PMC free article] [PubMed] [Google Scholar]
- 21.An updated Kuppuswamy’s socio-economic classification for 2017. Tabassum N, Rao RLL. Indian J Health Sci Res. 2017;7:365–367. [Google Scholar]
- 22.Childhood injuries in rural north India. Mohan D, Kumar A, Varghese M. Int J Inj Contr Saf Promot. 2010;17:45–52. doi: 10.1080/17457300903524862. [DOI] [PubMed] [Google Scholar]
- 23.Global Burden of Disease. GBD Compare. GBD Compare. [ Dec; 2022 ]. 2019. https://vizhub.healthdata.org/gbd-compare/ https://vizhub.healthdata.org/gbd-compare/
- 24.Epidemiology of childhood injury. Adesunkanmi AR, Oginni LM, Oyelami AO, Badru OS. J Trauma. 1998;44:506–512. doi: 10.1097/00005373-199803000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Epidemiological study of road traffic accident cases: a study from South India. Jha N, Srinivasa D, Roy G, Jagdish S. Indian J Community Med. 2004;XXIX:20–24. [Google Scholar]
- 26.Comparison of PEWS to physician opinion to identify deteriorating pediatric patients. Fenix J, Gillespie C, Levin A, Dean N. Critical Care Med. 2013;41:159. [Google Scholar]
- 27.Pediatric Early Warning Systems (PEWS) improve provider-family communication from the provider perspective in pediatric cancer patients experiencing clinical deterioration. Gillipelli SR, Kaye EC, Garza M, et al. Cancer Med. 2023;12:3634–3643. doi: 10.1002/cam4.5210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Multilevel impacts of a pediatric Early Warning System (PEWS) in resource-limited pediatric oncology settings. Mirochnick E, Graetz DE, Ferrara G, et al. Pediatr Critical Care Med. 2022;23:11. doi: 10.3389/fonc.2022.1018224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Challenge implementing pediatric early warning systems to improve early identification of clinical deterioration in hospitalized children with cancer: is it the score? Agulnik A. Pediatr Blood Cancer. 2023;70:0. doi: 10.1002/pbc.30105. [DOI] [PubMed] [Google Scholar]
- 30.Impact of Implementing a pediatric early warning system (PEWS) in a pediatric oncology hospital. Agulnik A, Johnson S, Wilkes R, et al. Critical Care Med. 2018;46:631. [Google Scholar]