Abstract
Tobacco smoking, a significant public health concern globally, is associated with a rise in noncommunicable diseases (NCDs) and preventable deaths, with pronounced impacts in conflict zones like Gaza. A cross-sectional study, conducted in 2020, in Gaza focused on individuals over 40 years of age, aiming to identify predictors of tobacco use and its links to diseases like coronary artery disease (CAD), chronic lung disease (CLD), and stroke using regression analysis. The research, based on the Gaza NCD study data with 4576 participants and a 96.6% response rate, found an overall tobacco smoking prevalence of 19.4%, with higher rates among men. After adjusting for various factors, the study identified significant associations between cigarette smoking in men and adverse health outcomes, such as CAD and CLD, with adjusted odds ratios (OR) of 1.67, 95% CI (1.22–2.29) and 1.68, 95% CI (1.21–2.33) respectively. However, after adjusting for independent variables, shisha smoking in men showed no association with these health outcomes. The findings of this study could assist other researchers in designing interventions aimed at reducing smoking prevalence by utilizing the associated factors identified in our analysis, such as age, education level, physical activity, and body mass index among men in Gaza.
Keywords: Smoking, Tobacco, Cigarette, Shisha, NCDs, Gaza
Subject terms: Public health, Epidemiology
Introduction
Tobacco smoking is considered a global public health concern that is associated with significant morbidity and premature mortality1,2. The number of smokers worldwide increased to 1.1 billion in 2019, with tobacco smoking leading to 7.7 million deaths3. The prevalence of tobacco smoking, including cigarette and shisha smoking, is particularly increasing in the Middle East and has been alarming in some Arab countries4. Tobacco smoking remains one of the leading causes of preventable deaths and is a primary risk factor for the increase in noncommunicable diseases (NCDs) and tobacco-specific morbidities affecting mainly the cardiovascular and respiratory systems5. In fact, the adverse health effects of smoking include but are not limited to coronary artery disease (CAD), chronic lung disease (CLD) and lung cancer6. The burden of treating these smoking-related diseases contributes to a substantial economic strain on the healthcare system. This is evident in the increased costs for medical treatments, hospitalizations, medications, and the necessary care for addressing these chronic medical conditions7.
Smoking is also driven by various socioeconomic and psychological factors. In fact, tobacco smoking has been found to be more prevalent among those with lower socioeconomic status (SES)8. The high prevalence of smoking among disadvantaged groups is suggested to be influenced by low social support, low levels of awareness and education, reduced motivation to quit, a stronger addiction to tobacco use, lack of self-efficacy, and the impact of tobacco industry marketing, particularly due to low tobacco prices9.
Tobacco smoking in the Arab region has also been a significant concern for public health officials, health professionals, and policy makers4. In fact, the prevalence of tobacco smoking has been particularly high in Arab men compared to women10. However, there has been very little global research addressing the use of tobacco and nicotine dependence among civilians in conflict-affected areas, despite key vulnerabilities such as the presence of various socioeconomic stressors. Most studies have addressed this topic within adolescent and young adult populations. Indeed, a study performed in the Republic of Georgia revealed that nicotine dependence was significantly associated with multiple mental health disorders in older conflict-affected men11. Moreover, the Palestinian Central Bureau of Statistics (PCBS), in its preliminary results of the “Smoking and Tobacco Consumption Survey, 2021”, reported an obvious increase in the prevalence of smoking among individuals aged 18 and above in the West Bank12.
As such, many efforts have been made to address the predictors of smoking, given its association with the challenging burden of disease, disability, and death. Among these predictors, we mention SES, cultural norms, age, and gender13,14.
Past studies have examined the prevalence of smoking and awareness of smoking-associated health risks among young people in Gaza, specifically focusing on university students. These studies were relatively small in size15,16.
In the Gaza Strip, tobacco smoking remains a significant public health challenge, particularly among men. Given the near absence of smoking among women in the population of Gaza, as evidenced by local and regional surveys, our study focused its analysis exclusively on men17. This gender-specific approach allows us to address the substantial health impacts and the sociocultural dynamics of smoking in this demographic, which is most affected by tobacco use. Understanding these patterns is crucial for developing targeted public health interventions and for providing a foundation for gender-specific health policies in regions with similar cultural and social norms.
Methods
Study design
This was a secondary data analysis of the Gaza NCD study database. The 2020 cross-sectional study collected data on a representative sample of 4576 individuals aged 40 years and above selected from 2493 households across Gaza’s five governorates through an interviewer-administered household survey. Details about study design including sampling and Sample size justification, have been published previously17. Interviewers visited each household for the study, obtained verbal informed consent, and then proceeded with data collection during the same visit. One eligible male and one eligible female were selected from each household using the Kish selection grid method, as detailed in the initial publication from this dataset. The original aim of collecting this dataset was to assess and identify potential solutions for NCDs in a densely populated area affected by prolonged armed conflict, such as Gaza17.
Measures used
Our primary objective was to identify predictors of both cigarette and shisha smoking. The selection of these predictors was based on known risk factors for smoking documented in the literature, as well as the availability of relevant data within the Gaza dataset.
Variables
Dependent variables
For smoking prediction: The dependent variables were cigarette and shisha smoking statuses. Current cigarette smoking status was defined according to the definition used by Centers for Disease Control and Prevention (CDC) and the National Health Interview Survey (NHIS)18. This definition encompasses individuals who have smoked 100 or more cigarettes over their lifetime and currently engage in daily smoking or smoking on some days. Current shisha smoking was defined as smoking Shisha either daily or on some days.
-
For health outcomes: The health outcomes considered as dependent variables included CAD, CLD, and stroke. The presence of CAD was assessed if participants reported a history of heart attack or angina. It was dichotomized as yes/no.
CLD was assessed by determining whether participants had a history of chronic obstructive pulmonary disease (COPD), asthma, or respiratory allergies and was dichotomized as yes/no.
Stroke was assessed by determining whether participants had a history of stroke and was dichotomized as yes/no.
Hypercholesterolemia and hypertension were assessed by determining if participants had previously received a diagnosis of high cholesterol or high blood pressure (or systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg), and they were dichotomized as yes/no.
Independent variables
-
For Smoking Prediction: The independent variables included age, education level, start or do more physical activity over the past year, body mass index (BMI), marital status, working within the past 30 days, presence of health insurance, and receipt of cash assistance.
Age in years was categorized into four categories: 40–50, 50–60, 60–70, and > 70 years.
Educational levels were classified into four groups: illiterate, basic education (able to read and write, elementary, preparatory), intermediate education (secondary, associate diploma, bachelor’s degree), and higher education (higher diploma, master’s degree, PhD).
We defined physical activity as the initiation or increase in physical activity within the past year and categorized it as “yes” or “no.” Participants were asked to report both the frequency and duration of their engagement in three categories of physical activity: vigorous, moderate, and light. Vigorous physical activity was defined as activities that require hard physical effort and make one breathe much harder than normal. Moderate physical activity included activities that make one breathe somewhat harder than normal. Light physical activity encompassed activities that do not cause a significant increase in breathing rate. Participants reported how often (frequency) and how long (duration) they engaged in each type of activity during a typical week. This allowed us to categorize their overall physical activity levels as ‘yes’ or ‘no’ based on whether they initiated or increased physical activity in the past year.
BMI was initially classified into six categories: underweight, normal, overweight, obese class I, obese class II, and obese class III. Subsequently, we recategorized the data into three categories: normal/underweight, overweight, and obese. During the survey, the research team directly measured the height and weight of each participant. These measurements were then used to calculate the BMI according to the standard formula: BMI = weight (kg)/[height (m2).
Marital status was categorized into two groups: married and unmarried. Other predictors, such as having worked during the past 30 days, having health insurance and receiving cash assistance, were all dichotomized as yes/no.
For Health Outcomes: In addition to the above variables used for smoking prediction, we also included cigarette and shisha smoking statuses, hypercholesterolemia, and hypertension as independent variables to analyze their association with the specified health outcomes.
Statistical analysis
Demographics and other variables of the study were summarized using frequency distributions. The prevalence of cigarette and shisha smoking were computed along with their 95% confidence intervals. Univariable and multivariable logistic regressions were used to identify the predictors of cigarette smoking and shisha smoking. Unadjusted and adjusted odds ratios (OR) were presented along with their 95% confidence intervals. Hosmer and Lemeshow tests were used to assess the goodness-of-fit of the models, and the predictive power of the models was assessed using receiver operating characteristic (ROC) curves. Similar analyses were performed to assess the potential association between tobacco smoking and NCDs. IBM-SPSS (version 29, Armonk, NY, USA) was used for the data analysis. Statistical significance was set at the 5% level.
The study received approval from the Imperial College Research Ethics Committee (reference 20IC5733), the American University of Beirut Institutional Review Board, and the Gaza Helsinki Committee (reference PHRC/HC/483/19). All methods conducted for the manuscript adhered to applicable guidelines and regulations.
Results
A total of 4576 participants were included in the cross-sectional study, resulting in a response rate of 96.6%. Of the participants, 46% were males, and 38% were above 60 years of age. For more details, Abu Hamad et al. provided a description of this sample17.
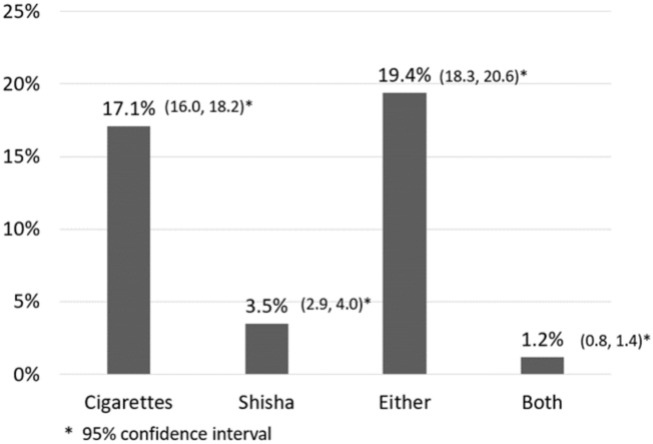
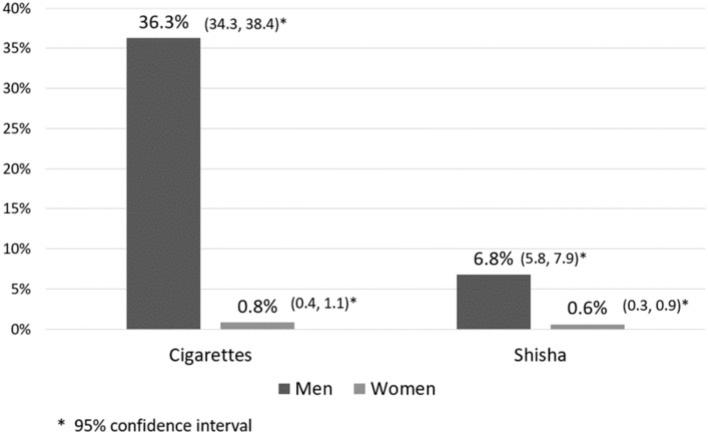
The prevalence of current cigarette smoking was 17.1% (95% CI: 16.0–18.2%), and for shisha smoking, it was 3.5% (95% CI: 2.9–4.0%). Among the participants, 783 individuals (19.4%) were identified as current cigarette or shisha smokers, with only 1.2% reported as users of both (refer to Fig. 1), but there was a marked sex difference. Given the higher prevalence rates among men (36.6% for cigarettes and 6.8% for shisha) than among women (0.8% for cigarettes and 0.6% for shisha), our analysis focused exclusively on male participants (see Fig. 2). The unadjusted and adjusted OR of cigarette and shisha smoking are shown in Tables 1 and 2.
Figure 1.
Prevalence of cigarette smoking, shisha smoking, and use of both among individuals aged 40 years and older in the Gaza population.
Figure 2.
Prevalence of smoking cigarettes and shisha among men and women in Gaza, aged ≥ 40 years.
Table 1.
Cigarette smoking model in men.
| Men | Nonsmoker (Cigarettes) N(%) | Cigarette smoker N(%) | Unadjusted OR (95% CI) | p-value | Adjusted OR (95%CI) | p-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| 40–50 | 215 (51.3) | 204 (48.7) | 1 | 1 | ||
| 50–60 | 452 (57.9) | 329 (42.1) | 0.767 (0.60, 0.97) | 0.029 | 0.750 (0.58, 0.97) | 0.03 |
| 60–70 | 389 (69.3) | 172 (30.7) | 0.466 (0.36, 0.61) | < 0.001 | 0.448 (0.33, 0.60) | < .001 |
| > 70 | 283 (82.7) | 59 (17.3) | 0.220 (0.16, 0.31) | < 0.001 | 0.161 (0.11, 0.24) | < .001 |
| Education | ||||||
| Illiterate | 55 (64.7) | 30 (35.3) | 1 | 1 | ||
| Basic education | 610 (57.5) | 451(42.5) | 1.355 (0.86, 2.15) | 0.196 | 0.911 (0.54, 1.54) | 0.727 |
| Intermediate education | 638 (71.1) | 259 (28.9) | 0.744 (0.466, 1.188) | 0.216 | 0.528 (0.31, 0.90) | 0.020 |
| Higher education | 367 (60.0) | 24 (40.0) | 1.222 (0.618, 2.417) | 0.564 | 1.098 (0.51, 2.38) | 0.812 |
| Start/do more physical activity in past year | ||||||
| No | 715 (62.8) | 423 (37.2) | 1 | 1 | ||
| Yes | 624 (64.7) | 341 (35.3) | 0.924 (0.77, 1.10) | 0.384 | 0.762 (0.62, 0.93) | 0.008 |
| BMI | ||||||
| Normal/underweight | 181 (40.5) | 266 (59.5) | 1 | 1 | ||
| Overweight | 520 (64.8) | 282 (35.2) | 0.369 (0.29, 0.47) | < 0.001 | 0.324 (0.25, 0.42) | < .001 |
| Obese | 584 (74.8) | 197 (25.2) | 0.230 (0.18, 0.29) | < 0.001 | 0.199 (0.15, 0.26) | < .001 |
| Marital status | ||||||
| Unmarried | 25 (78.1) | 7 (21.9) | 1 | 1 | ||
| Married | 1314 (63.4) | 757 (36.6) | 2.058 (0.89, 4.78) | 0.093 | 1.491 (0.58, 3.81) | 0.405 |
| Did you work during the past 30 days? | ||||||
| No | 925 (65.0) | 499 (35.0) | 1 | 1 | ||
| Yes | 414 (61.13) | 264 (38.9) | 1.182 (0.98, 1.43) | 0.083 | 0.909 (0.72, 1.15) | 0.428 |
| Health insurance | ||||||
| No | 193 (56.3) | 150 (43.78) | 1 | 1 | ||
| Yes | 1146 (65.2) | 612 (34.8) | 0.687 (0.54, 0.87) | 0.002 | 0.764 (0.59, 0.99) | 0.039 |
| Cash assistance | ||||||
| No | 748 (65.2) | 400 (34.8) | 1 | 1 | ||
| Yes | 591 (61.9) | 364 (38.1) | 1.152 (0.96, 1.38) | 0.12 | 0.818 (0.66, 1.02) | 0.068 |
Table 2.
Shisha smoking model in men.
| Men | Nonsmoker (Shisha) N(%) | Shisha smoker N(%) | Unadjusted OR (95% CI) | p-value | Adjusted OR (95%CI) | p-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| 40–50 | 368 (87.8) | 51 (12.2) | 1 | 1 | ||
| 50–60 | 716 (91.7) | 65 (8.3) | 0.655 (0.45, 0.97) | < 0.032 | 0.738 (0.49, 1.11) | 0.148 |
| 60–70 | 537 (95.7) | 24 (4.3) | 0.322 (0.20, 0.53) | < 0.001 | 0.412 (0.24, 0.71) | 0.002 |
| > 70 | 338 (98.8) | 4 (1.2) | 0.085 (0.03, 0.24) | < 0.001 | 0.084 (0.03, 0.28) | < .001 |
| Education | ||||||
| Illiterate | 81 (95.3) | 4 (4.7) | 1 | 1 | ||
| Basic education | 998 (94.1) | 63 (5.9) | 1.278 (0.45, 3.60) | 0.642 | 0.991 (0.30, 3.31) | 0.988 |
| Intermediate education | 827 (92.2) | 70 (7.8) | 1.714 (0.61, 4.82) | 0.307 | 1.152 (0.34, 3.87) | 0.819 |
| Higher education | 53 (88.3) | 7 (11.7) | 2.675 (0.75, 9.58) | 0.131 | 1.689 (0.40, 7.18) | 0.478 |
| Start/do more physical activity in past year | ||||||
| No | 1061 (93.2) | 77 (6.8) | 1 | 1 | ||
| Yes | 898 (93.1) | 67 (6.9) | 1.028 (0.73, 5.11) | 0.873 | 0.848 (0.59, 1.22) | 0.372 |
| BMI | ||||||
| Normal/Underweight | 425 (95.1) | 22 (4.9) | 1 | 1 | ||
| Overweight | 743 (92.6) | 59 (7.4) | 1.534 (0.93, 2.54) | 0.096 | 1.340 (0.80, 2.24) | 0.266 |
| Obese | 728 (93.2) | 53 (6.8) | 1.406 (0.84, 2.35) | 0.191 | 1.277 (0.76, 2.16) | 0.361 |
| Marital status | ||||||
| Unmarried | 30 (93.8) | 2 (6.3) | 1 | 1 | ||
| Married | 1929 (93.1) | 142(6.9) | 1.104 (0.26, 4.667) | 0.893 | 0.59 (0.13, 2.67) | 0.494 |
| Did you work during the past 30 days? | ||||||
| No | 1354 (95.1) | 70 (4.9) | 1 | 1 | ||
| Yes | 604 (89.1) | 74 (10.9) | 2.370 (1.69, 3.33) | 0.001 | 1.296 (0.87, 1.94) | 0.207 |
| Health insurance | ||||||
| No | 314 (91.5) | 29 (8.5) | 1 | 1 | ||
| Yes | 1643 (93.5) | 115 (6.5) | 0.758 (0.50, 1.16) | 0.201 | 0.845 (0.54, 1.32) | 0.461 |
| Cash assistance | ||||||
| No | 1047 (91.2) | 101 (8.8) | 1 | 1 | ||
| Yes | 912 (95.5) | 43 (4.5) | 0.489 (0.34, 0.71) | < 0.001 | 0.566 (0.37, 0.86) | 0.008 |
Cigarette smoking
Bivariate analysis: For men, older age (> 70 years) compared to those between 40–50 years, having obese status versus normal weight or underweight, and having health insurance versus not having it were all significantly associated with decreased odds of current cigarette smoking. The OR were 0.220, 95% CI (0.16, 0.31), 0.230, 95% CI (0.18, 0.29) and 0.687, 95% CI (0.54, 0.87) respectively (Table 1).
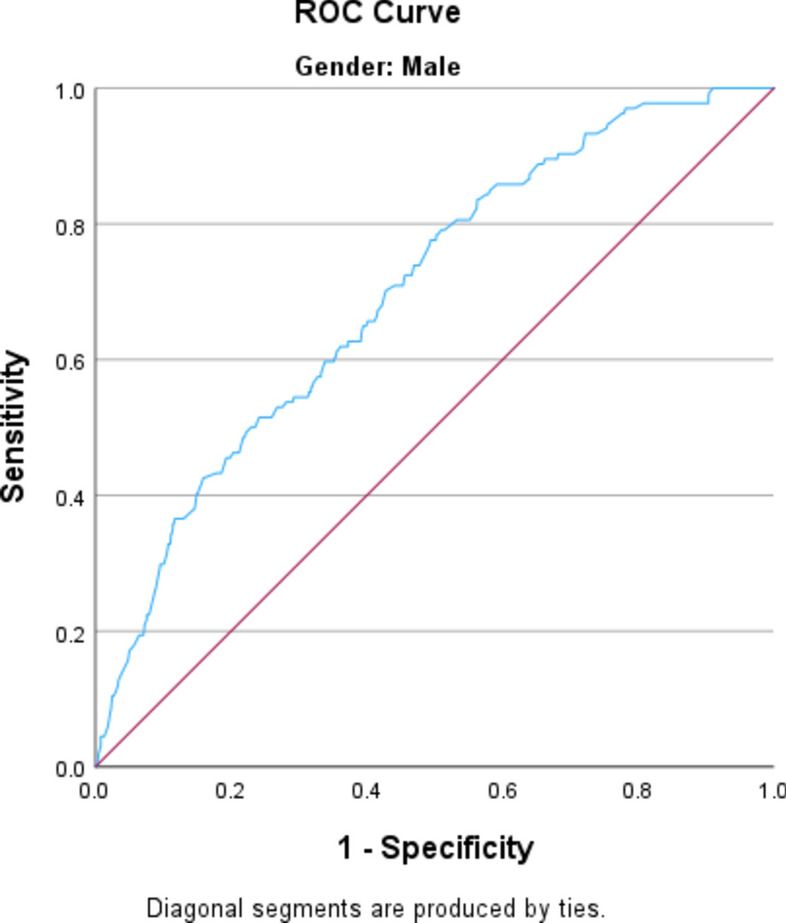
Multivariable analysis: Men over 70 years old were less likely to smoke compared to those aged 40–50, with an OR of 0.161, 95% CI (0.11, 0.24). Additionally, individuals who increased their physical activity over the past year were less likely to smoke compared to those who did not increase their activity, with an OR of 0.762, 95% CI (0.62, 0.93). Moreover, having obese status versus normal weight or underweight, and having health insurance versus not having it were significantly associated with decreased odds of current cigarette smoking. The OR were 0.199, 95% CI (0.15, 0.26) and 0.764, 95% CI (0.59, 0.99) respectively. Individuals with intermediate education, in contrast to those who are illiterate, exhibited a lower likelihood of smoking with an OR of 0.528, 95% CI (0.31, 0.90) (Table 1). The goodness-of-fit of the model using the Hosmer‒Lemeshow test showed a good fit (p-value of 0.394) and the ability to predict smokers and nonsmokers correctly in 71.7% of the participants (Fig. 3).
Figure 3.
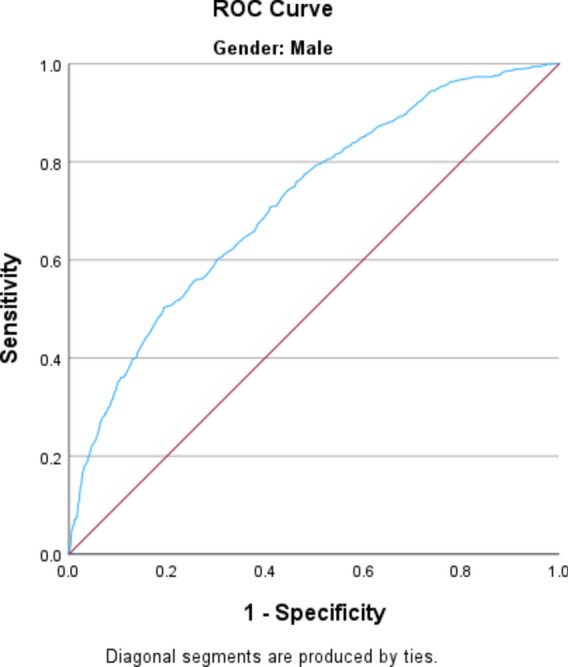
ROC curve of the cigarette smoking model for men. Area under the curve = 0.717.
Shisha smoking
Bivariate analysis: Older men (> 70 years) compared to younger than 70 years, and receiving cash assistance as compared to those who didn’t receive cash assistance were associated with less odds of current shisha smoking. The OR were 0.085, 95% CI (0.03, 0.024), and 0.489, 95% CI (0.34, 0.71) respectively. Those who worked during the past 30 days compared to those who didn’t work were associated with greater odds of current shisha smoking OR 2.370, 95% CI (1.69, 3.33) (Table 2).
Multivariable analysis: After adjusting for all variables in the model, only a few variables exhibited a significant association. Men over 70 years old, compared to those aged 40–50 years, were less likely to smoke shisha, with an OR of 0.084, 95% CI (0.03, 0.28). Similarly, individuals who received cash assistance were less likely to smoke shisha compared to those who did not receive such assistance, with an OR of 0.566, 95% CI (0.37, 0.86) (Table 2). The goodness-of-fit of the model using the Hosmer‒Lemeshow test showed a good fit (p-value of 0.269) and the ability to predict smokers and nonsmokers correctly in 69.9% of the participants (Fig. 4).
Figure 4.
ROC curve for men in the Shisha smoking model. Area under the curve = 0.699.
Noncommunicable diseases
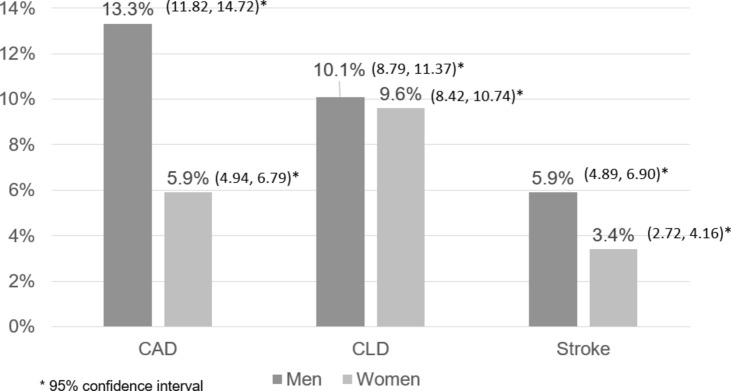
CAD: The prevalence of CAD was 13.3% among men and 5.9% among women (Fig. 5). Cigarette smoking was significantly associated with a history of CAD in men, with an adjusted OR of 1.67, 95% CI (1.22–2.29). No significant association was found for shisha smoking (Table 3).
CLD: The prevalence of CLD was 10.1% among men and 9.6% among women (Fig. 5). Among men, cigarette smoking showed a significant association with CLD, with an adjusted OR of 1.68, 95% CI (1.21–2.33). Shisha smoking did not show a significant link with CLD (Table 3).
Stroke: The prevalence of stroke was 5.9% among men and 3.4% among women (Fig. 5). Neither cigarette nor shisha smoking was significantly associated with stroke incidence among men (Table 3).
Figure 5.
Prevalence of NCDs in Gaza among men and women, age ≥ 40 years.
Table 3.
Association between noncommunicable diseases (CAD, CLD and stroke) and smoking in men.
| Model | Cigarette smoking/No | Shisha smoking/No | Hosmer & Lemeshow test | Area under the curve | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadj. odds ratio | CI 95% | p-value | Adj. odds ratio | CI 95% | p-value | Unadj. odds ratio | CI 95% | p-value | Adj. odds ratio | CI 95% | p-value | |||
| CAD | 1.03 | 0.79–1.34 | 0.826 | 1.67 | 1.22–2.29 | 0.001 | 0.576 | 0.32–1.06 | 0.074 | 0.75 | 0.39–1.44 | 0.38 | 0.134 | 0.785 |
| CLD | 1.55 | 1.16–2.06 | 0.003 | 1.68 | 1.21–2.33 | 0.002 | 0.8 | 0.44–1.36 | 1.47 | 0.96 | 0.50–1.86 | 0.9 | 0.523 | 0.657 |
| Stroke | 0.646 | 0.43–0.97 | 0.96 | 0.82 | 0.52–1.32 | 0.415 | 0.438 | 0.16–1.20 | 0.109 | 0.667 | 0.23–1.91 | 0.451 | 0.591 | 0.769 |
We adjusted for age, education, physical activity, BMI, marital status, work during the past month, health insurance, cash assistance, hypercholesterolemia, hypertension, cigarette smoking, and shisha smoking in each of the 3 models.
Discussion
This study identified significant predictors of tobacco smoking (including cigarettes and shisha) in the Gaza Strip. This study with a representative sample aimed to assess the burden of smoking among adults aged above 40 years in Gaza.
In the context of cigarette smoking, a greater likelihood of smoking was associated with being male. Historically, smoking has been more socially accepted among men than among women19. Furthermore, findings from neuroimaging data indicate that smoking triggers reward pathways in men more than in women20. Additionally, advertising agencies have traditionally targeted male consumers using role models such as actors and athletes. Given the near absence of smoking among women in the population of Gaza, we focused our analysis exclusively on men. Smoking is nearly nonexistent among women in Gaza, and if it does occur, it is not openly reported due to societal taboos. Women might also be more aware of the negative impact of smoking, especially its impact on pregnancy21.
In our study, smoking was also found to be less prevalent among older adults. This can be explained by the fact that older individuals might have quit smoking due to health conditions that make it inadvisable or due to its negative impact on their overall wellbeing. Another plausible explanation is that individuals aged 70 years and above are more likely to be healthy and are initially nonsmokers22.
Our study found that individuals who increased their physical activity over the past year were more likely to abstain from smoking. Relying on physical activity is an excellent stress relief mechanism that can be adopted rather than resorting to tobacco smoking23. Recent studies have shown that physical activity is an effective mechanism used in many smoking cessation programs24.
Furthermore, our study revealed a negative correlation between intermediate education and cigarette smoking. Educated individuals are better equipped to understand the detrimental effects of smoking and may have a higher SES, granting them improved access to healthcare services and the means to participate in smoking cessation programs. Conversely, individuals with intermediate education may face limitations in resources and healthcare access compared to their higher-educated counterparts, potentially resulting in lower smoking rates among this group8,25.
Regarding BMI, individuals who were overweight or obese had a lower likelihood of being smokers. Smoking has the potential to curb appetite and increase metabolism, leading to smokers often having a reduced BMI. Conversely, individuals with a higher BMI are at increased risk of developing several NCDs26.
Having health insurance was associated with a lower risk of smoking. Health insurance is a marker of higher SES in Gaza. People with health insurance generally have better access to healthcare services. Furthermore, smokers are less likely to purchase insurance deals, which contradicts theoretical expectations given the serious complications that can arise from smoking27.
In our study, we found that working in the past 30 days, having cash assistance or being married were not associated with cigarette smoking.
Moreover, being elderly or receiving cash assistance was negatively associated with smoking.
In relation to the study’s secondary outcomes in men, these data are limited by the fact that they are self-reported and elicited at the same time as the smoking questionnaire. Therefore, they are looking for associations, and no causal implications can be drawn.
Cigarette smoking was found to be significantly associated with a history of CAD and CLD. Conversely, no association was found between smoking shisha and a history of these NCDs. In fact, studies have shown that the number of cigarettes smoked is associated with the number of damaged vessels and the severity of CAD27. Moreover, according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, approximately 50% of smokers will eventually develop COPD28. In our study, no significant association was noted between cigarette smoking and the risk of developing stroke. Indeed, it was demonstrated in the literature that up to one-quarter of all strokes are directly attributed to cigarette smoking. No association was noted between shisha smoking and the risk of developing NCDs such as CAD, CLD and stroke. This might be related to the small population size of people who smoke shisha, which may negatively impact the study’s power to detect a significant difference.
Limitations/strengths
The data were collected three years prior to the beginning of the Gaza War on October 7, 2023. The insights derived from these data may remain pertinent for the population and could offer valuable understanding of the risk factors for NCDs associated with smoking, particularly in a population currently contending with a healthcare system that has completely collapsed. Despite war-related destruction, preconflict data remain a vital resource for informing public health strategies, shaping policies, and guiding long-term health planning and interventions during the reconstruction of Gaza’s healthcare system29.
The current study provides valuable insights into the predictors of cigarette and shisha smoking in the Gaza population. Although this is one of the largest reports on the prevalence of smoking in Gaza, there are several limitations to consider. First, the study’s cross-sectional design prevents us from establishing temporality and determining whether subjects were exposed to smoking before or after contracting diseases30.
Another limitation of the study is that all variables, including smoking and reporting NCDs, relied on self-reported data. This introduces the possibility of information bias or recall bias, potentially leading to overestimation or underestimation in some cases, thereby affecting the accuracy of the findings31. Additionally, due to the low prevalence of shisha smoking, the statistical models employed may lack power or may not fit the data well.
Another important limitation is that the analysis was performed exclusively on male participants, who comprised 46% of the study sample. This focus was due to the significantly higher prevalence rates of smoking among men compared to women in our study population. While this approach allowed for a detailed analysis of smoking patterns among the more affected group, it limits the generalizability of our findings across the entire demographic.
Moreover, as this study was not primarily designed to investigate smoking as the main outcome, there may be additional predictors of smoking that were not included in the analysis, such as family history of smoking, peer pressure, advertising and media32.
It is important to acknowledge these limitations, as they provide context for the findings and emphasize the need for further research to overcome these challenges and gain a more comprehensive understanding of smoking behavior in the Gaza population.
The current study on the predictors of cigarette and shisha smoking in the Gaza population is a significant contribution to the literature. This study not only provides important information on smoking patterns in the Gaza population but also sheds light on the risk of developing NCDs such as CAD and CLD. Several key strengths of the study can be highlighted. First, the study boasts a reasonably large sample size, ensuring that the findings are based on a substantial number of participants. This approach enhances the statistical power and reliability of the results33. A notable strength is the representative nature of the sample, which ensures that the prevalence rates of smoking and associated risk factors accurately reflect the population of interest34. Another strength of the study lies in its ability to assess multiple outcomes and predictors. By examining the relationship between smoking and various diseases, this study provides a comprehensive understanding of the risks associated with smoking35.
Conclusion
In conclusion, our study reinforces the established association between cigarette smoking and both CAD and CLD, consistent with the broader literature. Importantly, unlike general findings, our study did not identify a significant association between smoking and stroke within the Gaza population. This deviation from expected outcomes may provide new insights into population-specific health dynamics influenced by the unique socio-economic and healthcare contexts in Gaza.
Moreover, by documenting these associations within a conflict-affected area, our research adds valuable localized evidence that can inform tailored public health strategies and healthcare interventions. This study is particularly significant for healthcare professionals in Gaza, as it reinforces the critical need to address smoking as a key factor in the management and prevention of NCDs in challenging environments.
We believe this study serves as a crucial resource for researchers, policymakers, and healthcare providers working to mitigate the impacts of smoking in regions with similar geopolitical and health landscapes.
Acknowledgements
We would like to thank the tremendous efforts of the data collectors and field supervisors in the Gaza Strip who showed courage, resilience, and dedication to conducting this survey in the most challenging circumstances. The original study was funded by the UK’s Department for International Development (DFID), the Medical Research Council (MRC), the Economic and Social Research Council (ESRC) and Welcome Trust’s Health Systems Research Initiative (HSRI) (MR/S012877/1). AI, LH, HD, MK, and IS would like to acknowledge the training received under the Scholars in HeAlth Research Program (SHARP) that was in part supported by the Fogarty International Center and Office of Dietary Supplements of the National Institutes of Health (Award Number D43 TW009118). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The publication of this article was funded by the Weill Cornell Medicine – Qatar Health Sciences Library.
Author contributions
A.I., L.H, H.D., M.K., and I.S. contributed to the research question, methodology, analysis, writing and editing. Z.M. and H.T. provided supervision and guidance. B.A.H., Z.J., G.S., E.V., S.B., J.Y., M.J., C.M., and H.G. conceptualized implemented the original Gaza NCD study. All authors reviewed and edited the draft and agreed to submit the manuscript for publication.
Data availability
The data supporting the findings of this study are available upon request from the Gaza NCD study dataset, in accordance with data sharing policies established by the UK’s Department for International Development (DFID), the Medical Research Council (MRC), the Economic and Social Research Council (ESRC), and Welcome Trust’s Health Systems Research Initiative (HSRI) (Grant Number: MR/S012877/1).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Ziyad Mahfoud, Email: zrm2001@qatar-med.cornell.edu.
Gaza NCD Study Group:
Bassam Abu Hamad, Zeina Jamaluddine, Gloria Safadi, Eszter Vamos, Sanjay Basu, John Yudkin, Mohammed Jawad, Christopher Millet, and Hala Ghattas
References
- 1.Bonnie, R. J. et al. The effects of tobacco use on health. In Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products (National Academies Press, 2015). [PubMed] [Google Scholar]
- 2.Nagi, M., Riewpaiboon, A. & Thavorncharoensap, M. Cost of premature mortality attributable to smoking in the Middle East and North Africa. East. Mediterr. Health J.27, 974–983 (2021). [DOI] [PubMed] [Google Scholar]
- 3.Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the global burden of disease study 2019. The Lancet397, 2337–2360 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nasser, A. M. A., Geng, Y. & Al-Wesabi, S. A. The prevalence of smoking (cigarette and waterpipe) among university students in some Arab countries: A systematic review. Asian Pac. J. Cancer Prev. APJCP21, 583 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. (2008). WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. World Health Organization. https://Apps.Who.Int/Iris/Handle/10665/43818.
- 6.El-Zaatari, Z. M., Chami, H. A. & Zaatari, G. S. Health effects associated with waterpipe smoking. Tob. Control24, i31–i43 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costs and Expenditures. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/cost-and-expenditures.html (2022).
- 8.World Health Organization & Ciapponi, A. Systematic Review of the Link between Tobacco and Poverty. (World Health Organization, 2014).
- 9.Hiscock, R., Bauld, L., Amos, A., Fidler, J. A. & Munafò, M. Socioeconomic status and smoking: A review. Ann. N. Y. Acad. Sci.1248, 107–123 (2012). [DOI] [PubMed] [Google Scholar]
- 10.Khattab, A. et al. Smoking habits in the middle East and North Africa: Results of the BREATHE study. Respir. Med.106, S16–S24 (2012). [DOI] [PubMed] [Google Scholar]
- 11.Roberts, B., Chikovani, I., Makhashvili, N., Patel, V. & McKee, M. Tobacco use and nicotine dependence among conflict-affected men in the Republic of Georgia. Int. J. Environ. Res. Public. Health10, 2185–2197 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.PCBS | Announces the preliminary results of the Smoking and Tobacco Consumption Survey, 2021.
- 13.Sommer, I. et al. Socioeconomic inequalities in non-communicable diseases and their risk factors: An overview of systematic reviews. BMC Public Health15, 1–12 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garrett, B. E. Socioeconomic differences in cigarette smoking among sociodemographic groups. Prev. Chronic. Dis.16, (2019). [DOI] [PMC free article] [PubMed]
- 15.Abu Shomar, R. T., Lubbad, I. K., El Ansari, W., Al-Khatib, I. A. & Alharazin, H. J. Smoking, awareness of smoking-associated health risks, and knowledge of national tobacco legislation in Gaza, Palestine. Cent. Eur. J. Public Health22, 80–89 (2014). [DOI] [PubMed] [Google Scholar]
- 16.Tucktuck, M., Ghandour, R. & Abu-Rmeileh, N. M. E. Waterpipe and cigarette tobacco smoking among Palestinian university students: A cross-sectional study. BMC Public Health18, 1 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abu Hamad, B. A. et al. The hypertension cascade of care in the midst of conflict: The case of the Gaza strip. J. Hum. Hypertens.10.1038/s41371-022-00783-w (2022). 10.1038/s41371-022-00783-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.NHIS-Adult Tobacco Use-Glossary. https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm (2019).
- 19.Hirokawa, K., Yamazawa, K. & Shimizu, H. An examination of sex and masculinity/femininity as related to the taste sensitivity of Japanese students. Sex Roles55, 429–433 (2006). [Google Scholar]
- 20.Chang, P.-H. et al. Combination therapy of varenicline with nicotine replacement therapy is better than varenicline alone: A systematic review and meta-analysis of randomized controlled trials. BMC Public Health15, 689 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grard, A. et al. Smoking beliefs across genders, a comparative analysis of seven European countries. BMC Public Health19, 1321 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kleykamp, B. A. & Heishman, S. J. The Older Smoker. JAMA306, (2011). [DOI] [PMC free article] [PubMed]
- 23.Charilaou, M., Karekla, M., Constantinou, M. & Price, S. Relationship between physical activity and type of smoking behavior among adolescents and young adults in Cyprus. Nicotine Tob. Res.11, 969–976 (2009). [DOI] [PubMed] [Google Scholar]
- 24.Chen, H., Yang, Y., Miyai, H., Yi, C. & Oliver, B. G. The effects of exercise with nicotine replacement therapy for smoking cessation in adults: A systematic review. Front. Psychiatry13, 1053937 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tomioka, K., Kurumatani, N. & Saeki, K. The association between education and smoking prevalence, independent of occupation: A nationally representative survey in Japan. J. Epidemiol.30, 136–142 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dare, S., Mackay, D. F. & Pell, J. P. Relationship between smoking and obesity: A cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS ONE10, e0123579 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rezayatmand, R., Groot, W. & Pavlova, M. Smoking behaviour and health care costs coverage: A European cross-country comparison. Int. J. Health Econ. Manag.17, 453–471 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramsey, M. W., Chen-Sankey, J. C., Reese-Smith, J. & Choi, K. Association between marital status and cigarette smoking: Variation by race and ethnicity. Prev. Med.119, 48–51 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rutherford, S. & Saleh, S. Rebuilding health post-conflict: Case studies, reflections and a revised framework. Health Policy Plan.34, 230–245 (2019). [DOI] [PubMed] [Google Scholar]
- 30.Cross Sectional Study - an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/cross-sectional-study.
- 31.Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc.9, 211–217 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baheiraei, A., Soltani, F., Ebadi, A., Cheraghi, M. A. & Foroushani, A. R. Family and peer risk factors as predictors of lifetime tobacco use among Iranian adolescents: Gender similarities and differences. Glob. J. Health Sci.6, 63–75 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Madjarova, S. J. et al. Fragility part I: A guide to understanding statistical power. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA30, 3924–3928 (2022). [DOI] [PubMed] [Google Scholar]
- 34.Rudolph, J. E., Zhong, Y., Duggal, P., Mehta, S. H. & Lau, B. Defining representativeness of study samples in medical and population health research. BMJ Med.2, e000399 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolff, R. F. et al. PROBAST: A tool to assess the risk of bias and applicability of prediction model studies. Ann. Intern. Med.170, 51–58 (2019). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are available upon request from the Gaza NCD study dataset, in accordance with data sharing policies established by the UK’s Department for International Development (DFID), the Medical Research Council (MRC), the Economic and Social Research Council (ESRC), and Welcome Trust’s Health Systems Research Initiative (HSRI) (Grant Number: MR/S012877/1).