Abstract
Introduction
Otoscopes and otomicroscopes are the most commonly used instruments for visualizing the ear. Digital otoscopy (DO) could be used to improve diagnostics in primary health care by utilizing image enlargement. The aim of the study was to explore the possibilities of DO in remote consultations.
Materials and Methods
Based on real‐life referrals, 45 otologic outpatients were recruited. DO was performed followed by an attending otologist's appointment, serving as the gold standard. Twenty‐four patient cases were analyzed on a digital platform as remote consultation cases containing the given referral information supplemented with DO videos (DOVs). A total of 71 evaluations were performed by five otologists. The quality of the DOVs, their suitability for remote consultations, the accuracy of diagnoses and the usefulness of remote consultations were determined.
Results
The average DOV quality was judged to be 7.4 ± 0.3 (mean ± standard error of the mean; scale of 1–10). The diagnosis was correct in 79% of the cases. In 59% of the patients, the otologists considered that remote consultation could have replaced an in‐person visit.
Conclusions
In our simulated remote consultation setup, DOV quality was sufficient for diagnostic purposes, DO improved diagnostics and treatment planning in most cases and could be used to reduce the need for in‐person visits. DO‐aided remote consultation may improve diagnostics and access to care.
Level of evidence: 3.
Keywords: digital otoscope, digital otoscopy, otology, remote consultation, telemedicine
Digital otoscopy (DO) videos for remote consultations were studied in a simulated setting. DO improved diagnostics and treatment planning and could be used to reduce in‐person visits. In future, DO‐aided remote consultation may improve diagnostics and access to care also in real‐life setting.
1. INTRODUCTION
Telemedicine is defined as the use of electronic information and communications technologies to provide and support health care when distance separates the participants. 1 The advantage of telemedicine is that it provides health care to more patients at a lower cost. Telemedicine has been most widely utilized in fields such as radiology, dermatology, and pathology. 2 , 3 , 4 , 5 The applications of telemedicine in otology have been limited, likely due to the high dependence of visual evaluation of the ear by experienced otologists, but there has been an increasing trend in since the COVID‐19 pandemic. 6
The most commonly used instrument for ear examination is an otoscope. When the examination is performed by an otologist, an otomicroscope is often used. Traditional otoscopes provide poor possibility for teleconsultation, as there is no possibility of image capture or video recording. On the other hand, otomicroscopy can be considered too expensive and requires extensive learning for use by primary health care physicians (PHPs).
Advances in technology have made digital otoscopy (DO) a possible solution for these problems. DOs are more affordable than otomicroscopes and require less learning than both otoscopy and otomicroscopy. 7 , 8 Furthermore, the possibility of video recording and postexamination evaluation of the videos provides a possibility for remote consultations.
There are some studies on the diagnostic accuracy of digital otoscopes. Morberly et al. 9 compared DO still images to otomicroscopy combined with audiometry and/or tympanometry. Neurotologists were able to obtain a correct diagnosis using DO for different ear pathologies in 49%–100% of the cases, depending on the type of pathology. Confidence in diagnosis varied substantially among types of pathology and among participants. In the study tympanic membrane (TM) perforations were often misdiagnosed as retractions, which could be caused by the lack of three‐dimensional features in still images. Moshtagi et al. 10 compared smartphone‐enabled otoscopy with otomicroscopy. With smartphone‐enabled otoscopy, abnormal ears were identified in 100% of the cases, and the correct diagnosis was made in 82% of the cases.
Compared with still images, video recordings provide an improved three‐dimensional view, which could increase diagnostic accuracy. Kleinman et al. 11 compared findings obtained with traditional otoscopy to digital otoscope video (DOV) recordings made by trainees and their supervisors in the pediatric emergency department and primary care clinic patients. They found that DO improved the agreement between the trainee and the supervisor and reduced the need for repeated confirmatory examinations by the supervisor.
Considering the diagnostic accuracy of DO, it is tempting to speculate that it could be used in a remote consultation setting. In a recent study, 12 DO still images were used in hearing loss patient screening. The patients were examined by an audiology assistant with DO, audiological tests and by collecting medical history focused on the ears and hearing. The data collected by the audiology assistant were then analyzed remotely by an otologist or audiologist, who established a diagnosis. Remote consultation was found to be effective in screening patients for more severe pathologies. The capability of patients to perform otoscopy has been studied by Shomorony et al. 13 and found that patients could perform ear endoscopy well when guided by a medical professional.
In this study, we aimed to determine whether DOVs are applicable in a simulated remote consultation (SRC) setting to diagnose common external and middle ear pathologies. We were interested in how otologists perceive DOV quality and in the diagnostic accuracy of remote consultations using DOVs. Furthermore, we wanted to determine whether DOV‐aided remote consultations could replace in‐person visits.
2. MATERIALS AND METHODS
2.1. Ethics
This was a prospective observational study approved by the Helsinki University Hospital Ethics Committee. The research permit was obtained from the Institutional Review Board (No. §43/3.4.2023, HUS/279/2023). Patients were outpatients from the Helsinki University Hospital Head and Neck Center, Department of Otorhinolaryngology – Head and Neck Surgery.
2.2. Patient enrollment
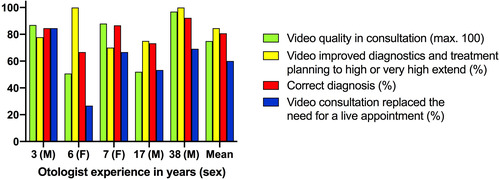
The study design is provided in Figure 1. First, 120 referrals to our tertiary otologic outpatient clinic were screened. The majority (16/22) of the original referrals were made by general practitioners working in local primary health care centers. Four referrals were made by ear‐, nose‐ and throat (ENT) specialists from the private sector or central hospitals in southern Finland. The inclusion criteria were adult, fluent in Finnish or Swedish and based on the referral had an abnormal otoscopy or otomicroscopy finding, or conductive hearing loss. We only included patients with exostoses, external otitis, TM perforations, secretory otitis media (SOM), cholesteatoma, or normal looking ears based on the otologist's otomicroscopy. Of the 120 patients, 48 met the inclusion criteria and were contacted by phone prior to their otologic appointment. At the hospital, 45/48 patients were willing to participate in the study and gave their informed consent. The patients were recruited in November 2022. The study population represented typical outpatients treated in our outpatient department.
FIGURE 1.
Study design. Ca of EAC, epidermoid carcinoma of external auditory canal; COE, chronic otitis externa; ENT, ear, nose and throat; SRC, simulated remote consultation. The three patients were excluded from the study, as the gold standard diagnosis could not be established on the otologist's appointment.
2.3. DO and otologist's appointment
Prior to the attending otologist (AO) appointment, the first author (E.A., ENT resident) recorded DOVs on patients' both ears. The digital otoscope was provided by Sibbo Medical Devices Ltd. (Helsinki, Finland). The Ear Penguin prototype model comprises a high‐quality digital camera, a mobile monitor and a user interface enabling video recordings. Obstructed ear canals needed cleaning before recordings in 4/45 cases. After the video recordings, the patient moved to the AO appointment. This otologic examination always included otomicroscopy. The patients had completed the Ear Outcome Survey‐16 14 for ear symptoms and quality of life. Prior audiometry was performed by the referring institute or by our institute if necessary. The diagnosis and treatment decisions made during the AO appointment served as the gold standards for the study.
2.4. Simulated remote consultations
After the AO appointments, 45 cases were reviewed by the first and last authors, and 21/45 cases were excluded because the study included enough cases with the same pathology. Three cases were excluded because the gold standard diagnosis could not be established during the otologist appointment.
The remaining 21 patients (24 ears) were reconstructed on a digital platform (Microsoft Forms, Microsoft, Redmond, WA, USA) as SRC cases. The pathologies diagnosed by the AO included in the SRCs were chronic otitis externa (COE [n = 4]), exostoses (n = 6), TM perforations (n = 8), of which six were dry and two were wet perforations, SOM (n = 2), and cholesteatoma (n = 2). Two patients had no pathology. Each SRC contained a referral letter from the PHP, the DOV, the Ear Outcome Survey‐16 symptom questionnaire and possible audiogram and imaging findings. Both ears were included in the study if they were affected. In contrast to the otologists who reviewed the SRC patients (SRC otologists, SRCOs), the AO had the benefit of interviewing the patient during regular appointments. The SRCOs were then asked to evaluate the DOV quality, establish a diagnosis and evaluate whether the SRC with or without a phone conversation with the patient could have substituted an in‐person visit to the otologist. An example of an SRC case is presented in Data S1. The full‐length DOV is found in Video S2.
Five independent SRCOs evaluated the SCRs. Each case was reviewed by three different SRCOs (except for one cholesteatoma case, which was reviewed by two). In total, 71 evaluations of the 24 cases were made. The SRCOs were blinded to the AO examination. The average time for analysis of a case varied between 3.6 and 5.5 min depending on the SRCO and case. Case demographics and diagnoses are presented in Table 1.
TABLE 1.
Case demographics and diagnoses.
| All | Exostoses | COE | TM perforation | TM perf., dry | TM perf., wet | SOM | Cholesteatoma | Healthy | |
|---|---|---|---|---|---|---|---|---|---|
| Ears, n | 24 | 6 | 4 | 8 | 6 | 2 | 2 | 2 | 2 |
| Age, year (mean ± SD) | 56 ± 18 | 72 ± 7 | 47 ± 19 | 54 ± 13 | 52 ± 14 | 58 ± 10 | 34 ± 13 | 52 ± 34 | 56 ± 16 |
| Gender, male (%) | 58 | 100 | 25 | 38 | 50 | 0 | 50 | 50 | 100 |
| Evaluations, n | 71 | 18 | 12 | 24 | 18 | 6 | 6 | 5 | 6 |
Note: TM perforation includes both dry and wet perforations.
Abbreviations: COE, chronic otitis externa; n, evaluations per diagnosis group; SOM, secretory otitis media; TM, tympanic membrane.
2.5. Statistics
All the statistical analyses were performed using IBM SPSS Statistics for Macintosh version 28.0 (Armonk, NY, USA). Graphs were generated using Prism 8 (GraphPad, San Diego, CA, USA). For statistical tests, one‐way ANOVA followed by Tukey's multiple comparison test was used for quantitative variables, chi‐square test was used for qualitative variables of different diagnosis groups, and unpaired t‐test was used for quantitative variables between the external auditory canal (EAC) and TM views. The significance level was set at p ≤ .05.
3. RESULTS
SRCOs judged the overall subjective quality of the DOVs in a remote consultation (from 1, useless to 10, very good) as 7.4 ± 0.3 (mean ± standard error of the mean; Table 2). The overall video quality was considered good across different diagnostic groups. In exostosis cases the video quality was considered better than in COE (8.2 ± 0.4 vs. 5.3 ± 0.9, respectively; p < .05). The scores were the lowest for COE (5.3 ± 0.9) cases.
TABLE 2.
Simulated remote consultation (SRC) results.
| All | Exostoses | COE | TM perforation | TM perf., dry | TM perf., wet | SOM | Cholesteatoma | Healthy | |
|---|---|---|---|---|---|---|---|---|---|
| Evaluations, n | 71 | 18 | 12 | 24 | 18 | 6 | 6 | 5 | 6 |
| Overall video quality (1–10) | 7.4 ± 0.3 | 8.2 ± 0.4a | 5.3 ± 0.9a | 7.8 ± 0.5 | 7.6 ± 0.6 | 8.3 ± 0.9 | 7.5 ± 1.2 | 9.0 ± 0.8 | 6.2 ± 1.5 |
| View to EAC (1–10) | 7.4 ± 0.3* | 7.8 ± 0.4 | 6.1 ± 0.8 | 7.4 ± 0.5 | 7.2 ± 0.6 | 7.8 ± 1.1 | 8.0 ± 1.1 | 9.2 ± 0.4 | 6.3 ± 1.4 |
| View to TM (1–10) | 5.7 ± 0.4* | 3.4 ± 0.7bcde | 3.8 ± 0.8fghi | 7.4 ± 0.5bf | 7.3 ± 0.6cg | 7.8 ± 0.9dh | 6.8 ± 1.0d | 8.6 ± 0.5eei | 5.8 ± 1.2 |
| Correct diagnosis (%) | 79 | 100 | 75 | 83 | 56 | 100 | 50 | 80 | 33 |
| Remote consultation replaces otologist visit (%) | 59 | 89 | 58 | 58 | 61 | 50 | 0 | 40 | 50 |
| Diagnosis incorrect, but no need for otologist visit was seen as necessary (%) | 3% (n = 2) | 0 | 0 | 4% (n = 1) | 6% (n = 1) | 0 | 0 | 0 | 17% (n = 1) |
Note: Table of key results in SRCs. Average score of recordings, view of EAC and TM. Percentage of correct diagnosis. In TM perforations, both dry and wet perforations were accepted as the correct diagnosis. In the dry and wet subcategories, the specific diagnosis was required. TM perforation includes data from both dry and wet perforations. For correct diagnosis identification of any kind of TM perforation was accepted. Correct diagnosis Data are mean ± standard error of the mean unless otherwise stated.
Abbreviations: COE, chronic otitis externa; EAC, external auditory canal; n, evaluations per diagnosis group; SOM, secretory otitis media; TM, tympanic membrane.
p = .0008 for statistical significance of difference (unpaired t‐test). For statistical significance of difference between diagnostic groups p < .05 (ahi), p < .01 (defg), p < .001 (c) and, p < .0001 (b), one‐way ANOVA followed by Tukey's multiple comparison test.
The subjective view of the EAC was generally considered better than the view of the TM (7.5 ± 0.3 vs. 5.7 ± 0.4, respectively; p = .0008). However, when looking at the different diagnostic groups, it was evident that the difference was mainly due to the low TM view scores in the exostosis (3.4 ± 0.7) and COE (3.8 ± 0.8) groups. The mean score for the TM view was 7.5 ± 1.3 when exostosis and COE cases were excluded. There were no differences in the EAC view scores between the different diagnostic groups.
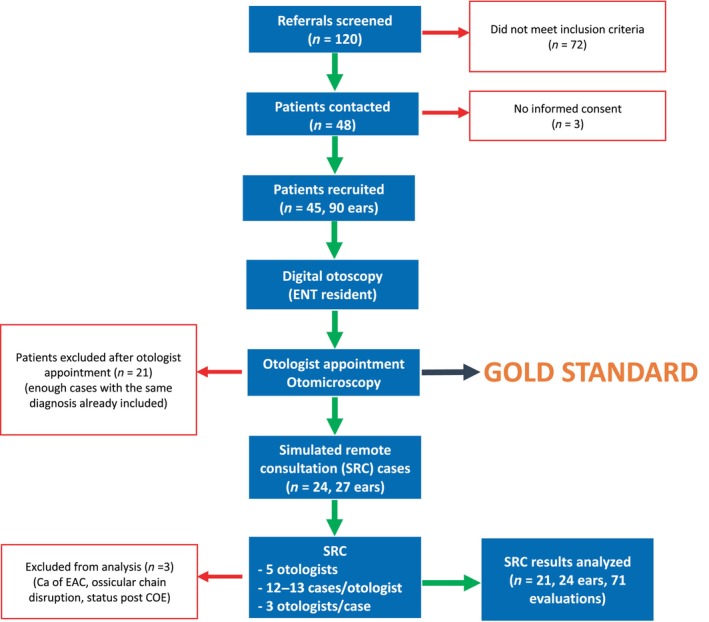
Next, the SRCOs were asked to diagnose the SRC cases based on the available information. Their diagnoses were compared with the gold standard diagnoses made during the AO appointment. In 79% of the SRC cases, the diagnosis was correct (Table 2). A positive correlation was found between correct diagnosis and overall quality of the DOV (p < .01), (Figure 2). Exostoses were identified in all 18 cases, and COE was identified in 9/12 (75%) cases. TM perforations in general were correctly diagnosed in 83% of the cases, dry perforations in 10/18 (56%) and wet perforations in 6/6. Cholesteatoma was identified in 4/5 (80%) cases. SOM was correctly diagnosed in 3/6 (50%) cases. Healthy ears were correctly diagnosed in 2/6 (33%) cases. No statistically significant differences were found between the different diagnosis groups.
FIGURE 2.
Correlation between digital otoscope video overall quality and correct diagnosis.
The SRCOs considered that altogether 59% of the cases could be diagnosed and treated as remote consultations, but there seemed to be great variation between the different diagnosis categories (Table 2). According to the SRCOs, treatment recommendations could be given for 16/18 (89%) exostosis cases based on remote consultation, whereas all six SOM cases would have needed an appointment. In the other diagnostic categories, remote consultation was considered sufficient in 40%–61% of the patients. No statistically significant differences were found between the different diagnosis groups.
In 41% (n = 29) of the cases, the SRCOs considered that an in‐person otologist visit was necessary after the remote consultation (Table 3). The most common reason was that a treatment recommendation could not be made (66%), followed by inability to establish a diagnosis (45%) and the feeling that patient findings would require treatment at an ENT appointment (28%). Of the 29 cases in which an in‐person otologist visit was considered necessary, two could have been substituted with a phone conversation with the patient. In these cases, the reason for the phone conversation was to give treatment recommendations.
TABLE 3.
Reasons why simulated remote consultation was insufficient to replace an ear, nose and throat (ENT) specialist visit.
| All | Exostoses | COE | TM perforation | TM perf., dry | TM perf., wet | SOM | Cholesteatoma | Healthy | |
|---|---|---|---|---|---|---|---|---|---|
| Evaluations, n | 71 | 18 | 12 | 24 | 18 | 6 | 6 | 5 | 6 |
| Cases in which ENT visit is necessary (%) | 41 | 11 | 42 | 42 | 39 | 50 | 100 | 60 | 50 |
| Given information not sufficient for diagnosis (%) | 45 | 0 | 80 | 30 | 43 | 0 | 33 | 33 | 100 |
| Given information insufficient for treatment recommendation (%) | 66 | 100 | 40 | 70 | 57 | 100 | 83 | 100 | 0 |
| Patient findings require treatment at ENT appointment (%) | 28 | 0 | 40 | 10 | 14 | 0 | 33 | 33 | 67 |
Note: TM perforation includes data from both dry and wet perforation subcategories.
Abbreviations: COE, chronic otitis externa; n, evaluations per diagnosis group; SOM, secretory otitis media; TM, tympanic membrane.
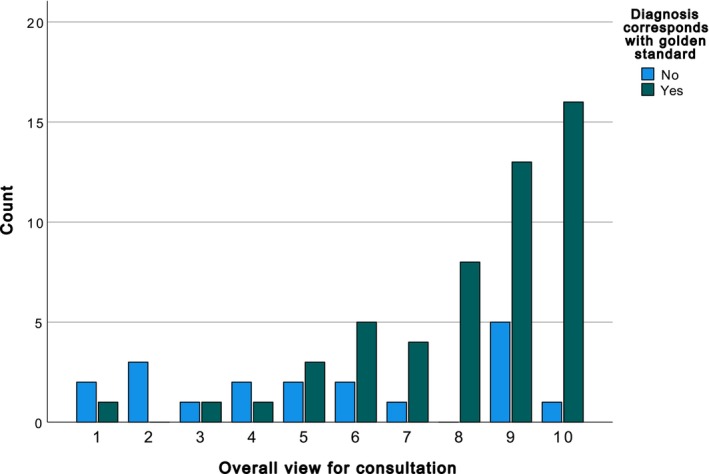
When looking at the individual SRCOs' responses (Figure 3), the perceived overall video quality (max. 100) ranged between 51 and 97 depending on the SRCO. Video improved diagnostics and treatment planning to a high or very high extent in 70%–100% of the cases. Correct diagnosis of SRC was achieved by different SRCOs in 67%–92% of the cases. The SRCOs concluded that the SRC replaced the need for in‐person appointments in 27%–85% of the cases. There seemed to be a correlation between the perceived video quality and the rate of correct diagnosis. SRCO experience in years (as an ENT specialist) or sex did not seem to correlate with SRC results.
FIGURE 3.
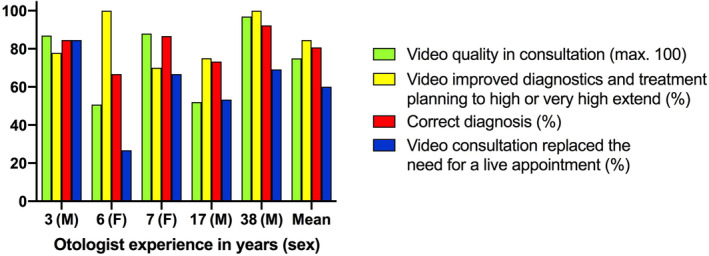
Otologist demographics and key results. F, female; M, male.
There were two SRC cases (3%) where the otologist did not see a need for an ENT appointment, but the diagnosis was incorrect. One patient had no pathology but was misdiagnosed as having a TM perforation. The other patient had a TM perforation, but the SRCO was unable to establish a diagnosis at all (Table 2).
4. DISCUSSION
Our study was designed to investigate how well DOVs are suited for diagnosing ear pathologies and to evaluate whether remote consultations with DOVs could be used to replace in‐person visits. We found that DOVs were effective at visualizing common ear pathologies. The diagnosis was correct in most cases, and an in‐person visit was often not necessary when DOVs were combined with a typical written otologic referral.
In a study by Tötterman et al., 15 four different digital otoscope devices were compared. The average image quality ranged between 363 and 672 (scale 1–1000) depending on the device. In the present study, the average video quality was 7.4 (scale 1–10), which might suggest that videos are superior to still images. In our study, DOVs provided a good quality view of the EAC and, in most cases, a good view of the TM if there was no pathology in the EAC that blocked the view of the TM. The same limitation applies to the otology diagnostic gold standard, otomicroscopy.
Overall, the correct diagnosis was reached in 79% of the SRC cases. TM perforations were correctly diagnosed in 83% of the cases in our study, which was greater than the 49% reported by Moberly et al. 9 using still images. In contrast to our study, Moberly et al. did not differentiate between dry and wet perforations, where dry and wet perforations were identified with 56% and 100% accuracy, respectively. These results support the idea that videos are superior to still images.
Some technologies have been developed with the aim of combining the best aspects of both still images and video recordings. One such technology is SelectStitch. 16 , 17 They used a computer‐aided otoscopic frame selection and stitching framework to select meaningful frames and remove irrelevant frames from DOVs to create a single image. They found that computer‐assisted composite images originating from DOVs can have diagnostic accuracy similar to that of video recordings in selected eardrum conditions. In a remote consultation setting, the use of, e.g., the SelectStitch method could have the advantage of less media transfer and arguably better integration in patient file systems.
In an earlier study comparing DO still images to an otomicroscopy view with no additional information given to the reviewer, the healthy ears were correctly diagnosed in 72% of the cases. 9 In our study, the healthy ears were identified with a low accuracy of 33%. The reason could be the inability of the otologist to interview the patient during the SRC when the findings of the video were not in accordance with the information given in the referral. The AO at the in‐person appointment had the benefit of adjusting their questions and judgment based on their interaction with the patient. In our study also overall quality was considered quite low (6.2) in the healthy ears. This might reflect that the otologists look for pathology and if it is not visible, the video quality is considered inadequate. Altogether it is possible, that judging the healthy ear poses a special problem in a remote consultation setting.
Overall, in 59% of the cases, the SRCOs judged that remote consultation was sufficient for making diagnoses and giving treatment recommendations. This is a surprisingly high figure given that, to our knowledge, remote consultations are very rarely used in clinical otology practice. Recent studies in the field of audiology have shown promising results for remote digital solutions in the diagnosis and rehabilitation of hearing‐impaired patients. 12 , 18 , 19 , 20 , 21 , 22 DO‐aided remote consultations could save time of health care professionals. At present, in Finland, the referring PHP examines patients during a 20–30 min appointment, followed by an ENT specialist at a 20–30 min appointment. In a remote consultation, the PHP could spend the same amount of time examining the patient with a digital otoscope and some minutes attaching the recording to the consultation. As in our study, the time needed to evaluate the SRCs was on average four to 6 min, the time saved by medical doctors would be ~15–25 min for each patient. Our calculation does not include the time for a possible further patient interview or treatment discussion, beyond that of the referring MD. Furthermore, the travel time saved by the patient and absence from work were not included, as these vary greatly depending on the geographical distances among other factors. With improved remote consultation systems, it could be possible to substantially speed up diagnostic workups and save money and resources both for patients and for the health care system. At least, remote consultations could be used as a first‐line evaluation tool to guide further diagnostics and treatments.
The SRCOs were asked if the SRC could replace an in‐person appointment. If the answer was negative, they were asked why. In 41% of the cases where ENT visits were considered necessary, the most common reason was the need for treatment recommendations (66%). This percentage was especially high in exostoses, TM perforations, SOM and cholesteatoma patients. These pathologies typically require surgical procedures, and given the more invasive nature of the treatment, the desire for an in‐person visit is understandable. In the exostosis group, an otologist visit was not necessary in 89% of the patients, and in the remaining exostosis patients, the reason for the visit was to make a proper treatment plan. The highest rate of need for ENT visits was in the SOM group, in which the correct diagnosis was also made in only 50% of the cases. The apparent issues with SOM might be due to the lack of pneumatic otoscopy during the DO in our study.
Overall, there was great individual variation in how SRCOs perceived DO and the SRC setting. There seemed to be no correlation between experience or sex and SRC results. However, there seemed to be a correlation between perceived video quality and the rate of correct diagnoses. The SRCOs were experienced in otology; however, their previous experience with DO was not recorded in our study. It is possible that their experience/inexperience could affect the results.
In terms of the limitations of the study, the number of cases in each diagnosis group was relatively small, limiting the statistical strength of the study. Including fewer different pathologies would have addressed this problem; however, the decision to include many common otologic pathologies was made to reflect the heterogeneous group of patients examined by otologists. When considering the analysis of the video quality, the results are based on the subjective evaluation by the SRCOs. The number of SRCOs was relatively small (n = 5), but the SRCOs had much experience handling referrals. In our study, the clearing of the EAC of obstructions was performed when needed. The instruments we used are not often accessible to PHPs. However, in 41/45 (91%) cases, no clearing was needed.
5. CONCLUSION
Our study with a simulated setting suggests that remote consultations might be useful in first‐line treatment for many otologic patients. Further studies where DO would be used in a real‐life setting by PHPs for remote consultations would give more information of its usefulness, benefits, and limitations in otology.
FUNDING INFORMATION
This research was supported by the Helsinki University Hospital Research Funds, the Tauno Palva Foundation, and The Finnish ORL‐HNS Foundation.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
Data S1. Supporting information.
Video S2. Digital otoscopy performed on patient's left ear prior to the otologist's appointment (0:01–0:05 External ear canal with normal findings 0:05–0:12 Tympanic membrane with myringosclerosis inferiorly. Atticus cholesteatoma).
Appelberg E, Viitasalo S, Hafrén L, et al. Digital otoscopy in remote consultations. Laryngoscope Investigative Otolaryngology. 2024;9(4):e70003. doi: 10.1002/lio2.70003
REFERENCES
- 1. Crump WJ, Driscoll B. An application of telemedicine technology for otorhinolaryngology diagnosis. Laryngoscope. 1996;106:595‐598. [DOI] [PubMed] [Google Scholar]
- 2. Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA. 1995;273:483‐488. [PubMed] [Google Scholar]
- 3. Chan S, Li L, Torous J, Gratzer D, Yellowlees PM. Review of use of asynchronous technologies incorporated in mental health care. Curr Psychiatry Rep. 2018;20:85. [DOI] [PubMed] [Google Scholar]
- 4. Thrall JH. Teleradiology. Part I. History and clinical applications. Radiology. 2007;243:613‐617. [DOI] [PubMed] [Google Scholar]
- 5. High WA, Houston MS, Calobrisi SD, Drage LA, McEvoy MT. Assessment of the accuracy of low‐cost store‐and‐forward teledermatology consultation. J Am Acad Dermatol. 2000;42:776‐783. [DOI] [PubMed] [Google Scholar]
- 6. Yang A, Kim D, Hwang PH, Lechner M. Telemedicine and telementoring in rhinology, otology, and laryngology: a scoping review. OTO Open. 2022;6:2473974X211072791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Niermeyer WL, Philips RHW, Essig GF Jr, Moberly AC. Diagnostic accuracy and confidence for otoscopy: are medical students receiving sufficient training? Laryngoscope. 2019;129:1891‐1897. [DOI] [PubMed] [Google Scholar]
- 8. Soares C, Clifton W, Freeman WD. Use of handheld video otoscopy for the diagnosis of acute otitis media: technical note. Cureus. 2019;11:e5547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moberly AC, Zhang M, Yu L, et al. Digital otoscopy versus microscopy: how correct and confident are ear experts in their diagnoses? J Telemed Telecare. 2018;24:453‐459. [DOI] [PubMed] [Google Scholar]
- 10. Moshtaghi O, Sahyouni R, Haidar YM, et al. Smartphone‐enabled otoscopy in neurotology/otology. Otolaryngol Head Neck Surg. 2017;156:554‐558. [DOI] [PubMed] [Google Scholar]
- 11. Kleinman K, Psoter KJ, Nyhan A, Solomon BS, Kim JM, Canares T. Evaluation of digital otoscopy in pediatric patients: a prospective randomized controlled clinical trial. Am J Emerg Med. 2021;46:150‐155. [DOI] [PubMed] [Google Scholar]
- 12. Siggaard LD, Jacobsen H, Hougaard DD, Hogsbro M. Digital vs. physical ear‐nose‐and‐throat specialist assessment screening for complicated hearing loss and serious ear disorders in hearing‐impaired adults prior to hearing aid treatment: a randomized controlled trial. Front digit. Health. 2023;5:1182421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shomorony A, Weitzman R, Chen H, Sclafani AP. Augmented otorhinologic evaluation in telemedical visits. Am J Otolaryngol. 2023;45:104088. [DOI] [PubMed] [Google Scholar]
- 14. Laakso JT, Silvola J, Hirvonen T, et al. Development of otology specific outcome measure: ear outcome survey‐16 (EOS‐16). J Otol. 2021;16:150‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Totterman M, Jukarainen S, Sinkkonen ST, Klockars T. A comparison of four digital otoscopes in a teleconsultation setting. Laryngoscope. 2020;130:1572‐1576. [DOI] [PubMed] [Google Scholar]
- 16. Binol H, Moberly AC, Niazi MKK, et al. SelectStitch: automated frame segmentation and stitching to create composite images from otoscope video clips. Appl Sci. 2020;10:5894. [Google Scholar]
- 17. Binol H, Niazi MKK, Essig G, et al. Digital otoscopy videos versus composite images: a reader study to compare the accuracy of ENT physicians. Laryngoscope. 2021;131:E1668‐E1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Almufarrij I, Dillon H, Dawes P, et al. Web‐ and app‐based tools for remote hearing assessment: a scoping review. Int J Audiol. 2023;62:699‐712. [DOI] [PubMed] [Google Scholar]
- 19. De Sousa KC, Moore DR, Smits C, Swanepoel DW. Digital technology for remote hearing assessment—current status and future directions for consumers. Sustainability. 2021;13:10124. [Google Scholar]
- 20. Corona AP, Ferrite S, Bright T, Polack S. Validity of hearing screening using hearTest smartphone‐based audiometry: performance evaluation of different response modes. Int J Audiol. 2020;59:666‐673. [DOI] [PubMed] [Google Scholar]
- 21. Bright T, Pallawela D. Validated smartphone‐based apps for ear and hearing assessments: a review. JMIR Rehabil Assist Technol. 2016;3:e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. D'Onofrio KL, Zeng F‐G. Tele‐audiology: current state and future directions. Front Digit Health. 2022;3:788103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.
Video S2. Digital otoscopy performed on patient's left ear prior to the otologist's appointment (0:01–0:05 External ear canal with normal findings 0:05–0:12 Tympanic membrane with myringosclerosis inferiorly. Atticus cholesteatoma).


