Abstract
Background
American and European guidelines define hypertension differently and are sex agnostic. Our aim was to assess the impact of different hypertension thresholds at the age of 40 on 30-year stroke risk and to examine sex differences.
Methods
We included 2608 stroke-free individuals from the Akershus Cardiac Examination 1950 Study, a Norwegian regional study conducted in 2012–2015 of the 1950 birth cohort, who had previously participated in the Age 40 Program, a nationwide health examination study conducted in 1990–1993. We categorised participants by systolic blood pressure (SBP) at age 40 (<120 mm Hg (reference), 120–129 mm Hg, 130–139 mm Hg and ≥140 mm Hg) and compared stroke risk using Cox proportional hazard regressions adjusted for age, sex, smoking, cholesterol, physical activity, obesity and education. Fatal and non-fatal strokes were obtained from the Norwegian Cardiovascular Disease Registry from 1 January 2012 to 31 December 2020, in addition to self-reported strokes.
Results
The mean age was 40.1±0.3 years (50.4% women) and mean SBP was 128.3±13.5 mm Hg (mean±SD). Stroke occurred in 115 (4.4%) individuals (32 (28%) women and 83 (72%) men) during 29.4±2.9 years of follow-up. SBP between 130 and 139 mm Hg was not associated with stroke (adjusted HR 1.71, 95% CI 0.87 to 3.36) while SBP ≥140 mm Hg was associated with increased stroke risk (adjusted HR 3.11, 95% CI 1.62 to 6.00). The adjusted HR of stroke was 4.32 (95% CI 1.66 to 11.26) for women and 2.66 (95% CI 1.03 to 6.89) for men, with non-significant sex interactions.
Conclusions
SBP ≥140 mm Hg was significantly associated with 30-year stroke risk in both sexes. A small subgroup of women had SBP ≥140 mm Hg and systolic hypertension was a strong risk factor for stroke in these women.
Trial registration number
Keywords: STROKE, Hypertension, Epidemiology
WHAT IS ALREADY KNOWN ON THIS TOPIC
Hypertension is the most important modifiable risk factor for stroke, but the optimal blood pressure to prevent stroke remains debated. Current guidelines use different thresholds for defining hypertension and are sex agnostic.
WHAT THIS STUDY ADDS
We found a steep incline in stroke risk above the threshold of 140 mm Hg for both sexes. A small subgroup of women had systolic hypertension (≥140 mm Hg) at age 40 and systolic hypertension was associated with a fourfold increased risk of stroke compared with women with optimal systolic blood pressure (<120 mm Hg).
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our results support previous studies showing that a hypertension threshold of 140 mm Hg is clinically relevant for stroke prevention, and systolic blood pressure ≥140 mm Hg at age 40 was a strong risk factor in women for incident cerebrovascular events.
Introduction
Stroke is a serious condition with a large impact on quality of life.1 Preventive measures at the population level are needed to delay the onset of stroke and reduce its disease burden.
Several modifiable risk factors for stroke are identified, the most prominent being hypertension.2 3 The causal link between hypertension and stroke has been established through scientific literature over decades.4 The consequence has been a shift towards stricter definitions and treatment targets for hypertension, but there is still uncertainty about how low targets should be and whether they should be age-specific and sex-specific.5,8
Today, there are two widely accepted definitions of hypertension. The 2018 European Society of Cardiology/European Society of Hypertension guideline9 defines hypertension as a blood pressure of at least 140/90 mm Hg while the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline defines hypertension as a blood pressure of at least 130/80 mm Hg, with systolic blood pressure (SBP) less than 120 mm Hg considered normal.10 Although these definitions are independent of age and sex, lifetime blood pressure trajectories differ between the sexes, and women seem to be at higher risk of adverse cardiovascular outcomes at lower blood pressure thresholds.11 12
After the publication of the 2017 ACC/AHA guideline, questions were raised about the cardiovascular risk posed by blood pressure in the category of 130–139/80–89 mm Hg among otherwise healthy young adults, as they would be defined as having hypertension in one guideline, but not the other.13 Supplementary statements based on expert opinions and observational studies were published to aid clinicians,14 but there is still a lack of data to support risk assessment for this population. Studies that compare the long-term risk of cardiovascular events by different hypertension thresholds, preferably also investigating sex differences, are therefore needed. Moreover, studies that solely focus on stroke risk are needed to supplement studies where stroke is part of a composite endpoint.
Accordingly, in this study, we aimed to examine the longitudinal association between different hypertension thresholds at the age of 40 and 30-year stroke risk, including sex differences, in a well-described cohort from the general Norwegian population.
Methods
Study design
The present study included 2608 stroke-free individuals participating in the Akershus Cardiac Examination (ACE) 1950 Study, a prospective 1950 birth cohort study within the general Norwegian population, with the first visit conducted in 2012–2015.
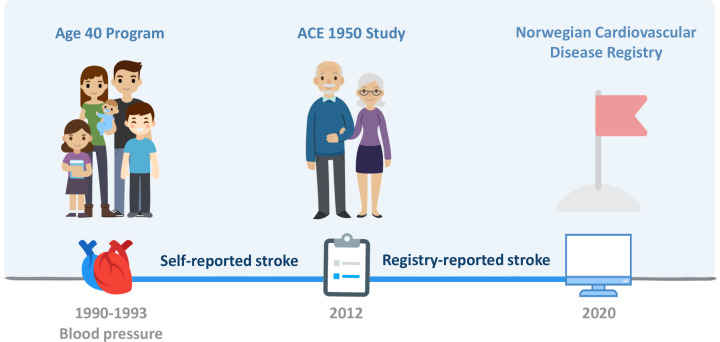
The exposure, SBP at age 40, was obtained via linkage from the ACE 1950 Study to the Age 40 Program, a nationwide health examination study conducted in 1990–1993. The endpoint stroke, was obtained by self-report for events between 1990–1993 and 31 December 2011, and from the Norwegian Cardiovascular Disease Registry (NCDR) for events from 1 January 2012 to 31 December 2020. Data from the ACE 1950 Study, the Age 40 Program and NCDR were linked using the national identification number. Figure 1 illustrates the studies and registries included in the present study.
Figure 1. Studies and registries included in the present study. Figure developed by the authors using venngage.com with a licence to use, reproduce and distribute worldwide. ACE, Akershus Cardiac Examination.
The ACE 1950 Study
The ACE 1950 Study is a cohort study of the cardiovascular health of men and women born in 1950 living in Akershus County, Norway. All individuals born in 1950 who were permanent residents of Akershus County at the time of 1 November 2011 were invited to participate in the study. The first visit was conducted at two study sites (Akershus University Hospital and Bærum Hospital, Vestre Viken Hospital Trust) between 2012 and 2015. The study protocol included a cardiovascular examination, a self-reported questionnaire and a fasting blood sample. The questionnaire contained marital status, educational level, ethnicity, medical history and current medications. The clinical examination included measurements of blood pressure in the sitting and supine position after 10 min of rest, height and weight, hip and waist circumference, vital parameters, and ECG. Details on the study protocol and population characteristics have been described previously.15
The Age 40 Program
In total, 74% of the ACE 1950 Study participants had previously participated in the Age 40 Program.16 The Age 40 Program was a national cardiovascular health screening survey conducted by Norwegian health authorities in the 1990s. The survey included a clinical examination, a non-fasting blood sample and a self-reported questionnaire on lifestyle habits and medical history.
Blood pressure measurements and categorisation
The main exposure variable, SBP at age 40, was measured after 2 min of seated rest by a trained study nurse using an automated blood pressure measurer (DINAMAP; Criticon, Tampa, Florida, USA). Three measurements with 1 min intervals were obtained, and the mean of the second and third readings were used in the analyses. SBP was categorised into four groups: <120 mm Hg, 120–129 mm Hg, 130–139 mm Hg and ≥140 mm Hg, with <120 mm Hg as the reference group.
Incident stroke
The outcome variable, incident stroke, was based on self-reported and registry-reported events. For the time period between the Age 40 Program (1990–1993) and 31 December 2011, strokes were obtained from the self-reported questionnaire in the first visit of the ACE 1950 Study. In the case of a self-reported stroke, participants also reported the respective year of occurrence. For the time period between 1 January 2012 (on which day the NCDR was established) and 31 December 2020, fatal and non-fatal strokes were obtained from the NCDR and the National Cause of Death Registry. The NCDR is a mandatory national registry that contains information on all Norwegian citizens with cardiovascular disease, including diagnostic codes (International Classification of Diseases Version 10) and dates of inpatient hospitalisations. The National Cause of Death Registry is a mandatory registry that contains information on the time and cause of death for all Norwegian citizens. Incident stroke was defined as the participant’s first inpatient hospitalisation with diagnostic codes I61.x or I63.x as the main diagnosis. For self-reported strokes, the event date was set to 1 June of the year the stroke was reported.
Other covariates
Body mass index (BMI) was calculated as the weight in kilograms divided by the square of height in metres. Obesity was defined as a BMI of at least 30 kg/m2. Higher education was defined as at least 4 years of college or university training.
Statistical analysis
Continuous data are presented as mean±SD for normally distributed variables and median with IQR for skewed variables, with comparisons made using the Student’s t-test or one-way analysis of variance. Categorical data are presented as numbers with percentages, and comparisons were made using the χ2 test.
The total stroke incidence per 100 000 person-years was calculated for the total population and separately for men and women. Cox proportional hazard regressions were used to estimate HRs with 95% CIs for stroke, with SBP both as a continuous and categorical exposure variable.
In all Cox regressions, the start date was defined as the examination date in the Age 40 Program, and participants were censored at the time of stroke, death or end of follow-up, whichever occurred first. Separate Cox regressions were performed for men and women, and we tested for interactions between sex and SBP on stroke risk.
In all analyses, the crude model presents unadjusted data. In the adjusted models, we adjusted for the following predefined covariates from the Age 40 Program: age, sex, smoking, total cholesterol, physical activity and obesity. In addition, we adjusted for education as reported at the time of the ACE 1950 Study’s first visit. All statistical analyses were performed by using the Stata software V.17 (StataCorp). Two-sided p values below 0.05 were considered statistically significant.
Patient and public involvement
An ACE 1950 Study ‘User Panel’ has been formed, consisting of four study cohort members born in 1950 (two women and two men), two user organisation representatives and two general practitioners. This User Panel serves in an advisory capacity, working alongside the steering committee to guide the ongoing study. The User Panel members participated in the practical planning phase of the ACE 1950 Study and are actively involved in the current conduct of the 10-year follow-up study visits.
Results
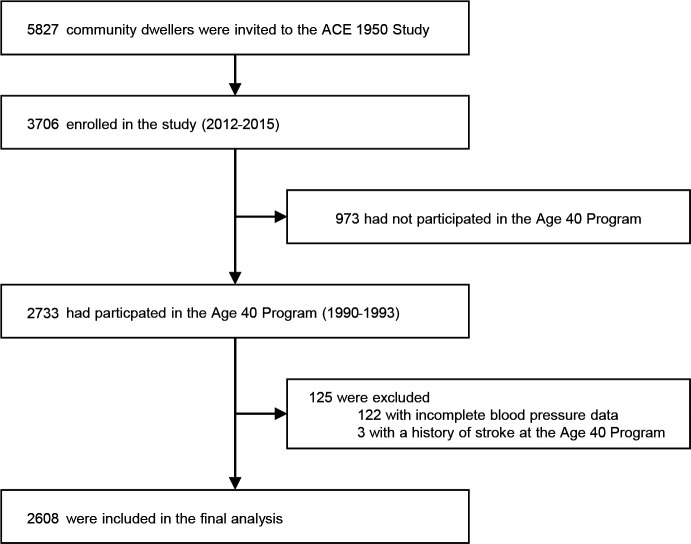
A total of 5827 individuals were invited to participate in the ACE 1950 Study (2012–2015), and 3706 (attendance rate 64%) were enrolled in the study. Of these, 2733 (74%) individuals had previously participated in the Age 40 Program and were available for the analysis. We excluded individuals with incomplete blood pressure readings (n=122) or a self-reported history of stroke (n=3) before the age of 40, resulting in a final analytical cohort of 2608 individuals (figure 2).
Figure 2. Inclusion of participants to the study. ACE, Akershus Cardiac Examination.
The mean age of participants was 40.1±0.3 years and 50.4% were women. The mean SBP and diastolic blood pressure values were 128.3±13.5 and 78.2±9.4 mm Hg (123.2±12.6 and 75.9±8.9 mm Hg for women and 133.4±12.4 and 80.6±9.2 mm Hg for men). Only 36 (1%) individuals reported being under treatment for hypertension while 488 (19%) had a mean SBP of at least 140 mm Hg. Study population characteristics at age 40 for the total cohort are provided in table 1 while characteristics separate for men and women are provided in online supplemental table S1. Population characteristics of the ACE 1950 Study’s first visit (2012–2015) by SBP at age 40 are provided in online supplemental table S2, and characteristics at the ACE 1950 Study’s first visit among participants versus non-participants in the Age 40 Program are provided in online supplemental table S3.
Table 1. Study population characteristics at age 40 years, n=2608.
| Systolic blood pressure at age 40 years (mm Hg) | P value | ||||
| <120 | 120–129 | 130–139 | ≥140 | ||
| N | 711 (27%) | 792 (30%) | 617 (24%) | 488 (19%) | <0.001 |
| Female sex | 551 (78%) | 410 (52%) | 228 (37%) | 124 (25%) | <0.001 |
| Age, years, mean±SD | 40.1±0.3 | 40.1±0.3 | 40.0±0.3 | 40.0±0.3 | 0.887 |
| Body mass index, kg/m2, mean±SD | 23.1±2.8 | 24.3±3.2 | 25.1±3.3 | 25.8±3.5 | <0.001 |
| Obesity* | 17 (2%) | 46 (6%) | 45 (7%) | 48 (10%) | <0.001 |
| Systolic blood pressure, mm Hg, mean±SD | 112.8±5.5 | 124.8±2.8 | 134.4±2.8 | 148.9±8.2 | <0.001 |
| Diastolic blood pressure, mm Hg, mean±SD | 70.5±6.1 | 76.1±6.2 | 81.5±6.6 | 88.9±8.8 | <0.001 |
| Non-caucasian | 13 (2%) | 9 (1%) | 8 (1%) | 6 (1%) | 0.680 |
| Higher education† | 320 (45%) | 357 (45%) | 274 (44%) | 209 (43%) | 0.886 |
| Physical activity | <0.001 | ||||
| Sedentary activity | 143 (20%) | 130 (17%) | 122 (20%) | 89 (18%) | – |
| Walking or cycling at least 4 hours/week | 464 (65%) | 485 (61%) | 338 (55%) | 289 (59%) | – |
| Recreational sports at least 4 hours/week | 95 (14%) | 159 (20%) | 140 (22%) | 101 (21%) | – |
| Hard training several times per week | 9 (1%) | 18 (2%) | 17 (3%) | 9 (2%) | – |
| Smoking‡ | 0.906 | ||||
| Never | 276 (39%) | 311 (40%) | 251 (41%) | 193 (40%) | – |
| Current or previous | 430 (61%) | 472 (60%) | 360 (59%) | 290 (60%) | – |
| Cardiovascular comorbidity | |||||
| Myocardial infarction or angina | 3 (0.4%) | 4 (0.5%) | 3 (0.5%) | 3 (0.6%) | 0.974 |
| Hypertension§ | 3 (0.4%) | 5 (0.6%) | 2 (0.3%) | 26 (5.3%) | <0.001 |
| Diabetes¶ | 1 (0.1%) | 2 (0.3%) | 0 (0%) | 4 (0.8%) | 0.054 |
| Biomarkers | |||||
| Cholesterol, mmol/L, mean±SD | 5.2±0.9 | 5.4±1.0 | 5.6±1.0 | 5.8±1.1 | <0.001 |
| Triglycerides, mmol/L, mean±SD | 1.4±0.9 | 1.6±1.1 | 1.9±1.3 | 2.2±1.8 | <0.001 |
Obesity: body mass index ≥30 kg/m2, higher education: at least 4 years of college or university training.
1 missing value.
8 missing values.
25 missing values.
3 missing values.
2 missing values.
A total of 115 strokes occurred during a mean follow-up of 29.4±2.9 years. Of these, 70 (61%) were self-reported and 45 (39%) were registry reported. The median age of stroke victims was 60.1 (IQR 54.5–64.9) years, and the total incidence of stroke per 100 000 person-years was 149.
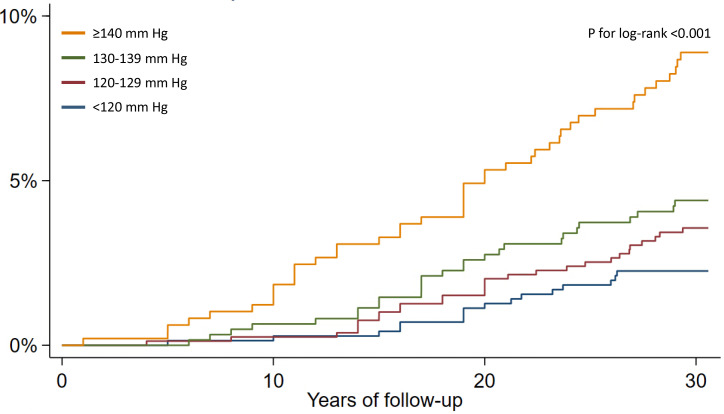
Figure 3 shows the cumulative incidence of stroke by SBP categories at age 40. In the crude analysis, SBP between 130 and 139 mm Hg was associated with stroke (HR 1.97, 95% CI 1.06 to 3.66) when compared with the category of <120 mm Hg (table 2). This association was attenuated by adjustment for covariates (HR 1.71, 95% CI 0.87 to 3.36). For the category of SBP ≥140 mm Hg, associations were significant in both the crude (HR 4.07, 95% CI 2.29 to 7.22) and adjusted analysis (HR 3.11, 95% CI 1.62 to 6.00).
Figure 3. Cumulative incidence of stroke by systolic blood pressure categories at age 40 years, n=2608.
Table 2. HRs of incident stroke by SBP categories at age 40 years, n=2608.
| N | Crude | Adjusted* | Strokes, n | |||
| HR (95% CI) | P value | HR (95% CI) | P value | |||
| SBP, mm Hg | ||||||
| <120 | 711 (27%) | 1 (reference) | – | 1 (reference) | – | 17 (15%) |
| 120–129 | 792 (30%) | 1.58 (0.86 to 2.92) | 0.144 | 1.47 (0.76 to 2.85) | 0.252 | 28 (24%) |
| 130–139 | 617 (24%) | 1.97 (1.06 to 3.66) | 0.032 | 1.71 (0.87 to 3.36) | 0.118 | 27 (24%) |
| ≥140 | 488 (19%) | 4.07 (2.29 to 7.22) | <0.001 | 3.11 (1.62 to 6.00) | 0.001 | 43 (37%) |
Adjusted for age, sex, smoking, total cholesterol, physical activity, obesity, education.
SBP, systolic blood pressure
When exploring SBP as a continuous exposure variable, each 1 mm Hg higher SBP at age 40 increased the crude HR of incident stroke by 1.03 (HR 1.03, 95% CI 1.02 to 1.05). Adjustment for covariates did not attenuate this association (adjusted HR 1.03, 95% CI 1.01 to 1.04). In subgroup analyses, SBP as a continuous variable was associated with stroke among women (adjusted HR 1.04, 95% CI 1.02 to 1.07) and men (adjusted HR 1.02, 95% CI 1.00 to 1.04).
Out of 115 strokes, 83 (72%) occurred in men. Stroke incidence was 82 per 100 000 person-years for women and 218 per 100 000 person-years for men. Median age of stroke was 60.4 (95% CI 56.4 to 66.6) years for women and 59.1 (95% CI 54.1 to 64.1) years for men. Online supplemental table S4 shows the distribution of strokes per SBP categories at age 40 in women and men.
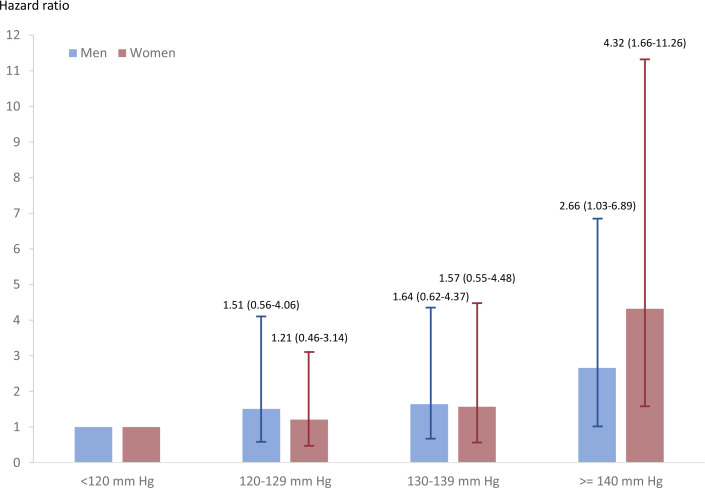
In sex-specific Cox regressions, the results were comparable to that of the total cohort (online supplemental table S5). SBP between 130 and 139 mm Hg was not associated with an increased stroke risk compared with the reference group in either of the sexes (adjusted HR 1.57, 95% CI 0.55 to 4.48 for women and 1.64, 95% CI 0.62 to 4.37 for men). However, an SBP of at least 140 mm Hg was significantly associated with stroke in both women (adjusted HR 4.32, 95% CI 1.66 to 11.26) and men (adjusted HR 2.66, 95% CI 1.03 to 6.89) (figure 4). There was no interaction between sex and SBP on the risk of stroke (P for interaction=0.146). Among adjustment covariates, smoking and sex were significantly associated with stroke risk (online supplemental table S6).
Figure 4. Adjusted HRs for stroke for men and women by systolic blood pressure at age 40 years, with 95% CIs (mean follow-up 29.4±2.9 years), n=2608. Adjusted for age, sex, smoking, total cholesterol, physical activity, obesity and education.
Discussion
In this population-based cohort study, we examined the association between different systolic hypertension thresholds at age 40 and incident stroke risk over a 30-year period. We did not find an increased stroke risk among individuals with SBP between 130 and 139 mm Hg. However, the risk of stroke increased gradually with increasing SBP, suggesting a positive dose–response relationship. For SBP ≥140 mm Hg, we found significant associations, with an almost threefold stroke risk in the total population. The small subgroup of women with SBP ≥140 mm Hg at age 40 had fourfold risk of stroke compared with women with SBP <120 mm Hg in multivariable analysis.
These findings are consistent with those reported in the Coronary Artery Risk Development in Young Adults study, which found no significant association between blood pressure in the range of 130–139/80–89 mm Hg and incident stroke over a 28-year period.17 In line with our results, blood pressure ≥140/≥90 mm Hg exhibited a significant increase in stroke hazard, with HRs of similar magnitude to ours.
Although available data suggest a graded increase in the risk of major cardiovascular events with rising blood pressure,4 18 and correspondingly a reduced risk when blood pressure is lowered,19 20 previous studies have primarily used composite endpoints, where the proportion of stroke cases tends to be small, rather than exclusively focusing on stroke risk.21,25 Further, few studies have specifically investigated the sex-specific risk of SBP on long-term stroke risk.
We found significant associations for both men and women for SBP ≥140 mm Hg, with hypertensive women having approximately fourfold risk of stroke in multivariable analysis that adjusted for other clinical risk factors, while HR was two for hypertensive men at age 40 compared with men with SBP <120 mm Hg. These findings are supported by recently published sex-stratified data from ten cycles of the National Health and Nutrition Examination Survey suggesting that women are at higher risk of death from cardiovascular disease at lower levels of SBP compared with men.26 Confirmatory studies on sex-specific risk cut points in defining and treating hypertension are warranted.
The present study reports a slightly lower stroke incidence (approximately 25% lower) compared with estimates from The Norwegian National Patient Registry and the National Cause of Death Registry.27 This discrepancy can be explained by the fact that the mean age of stroke is significantly higher nationally, with a mean age of 72 years for men and 76 years for women in Norway, whereas our participants were only followed until the age of 70 years.28 Moreover, our participants reported a higher level of education and socioeconomic status compared with the national average. Additionally, survivorship bias may contribute to the lower stroke incidence observed in our cohort.
Our study has several strengths. These include a long follow-up period and a substantial sample size comprising healthy individuals from the general population. Furthermore, our study builds on prior population-based studies by reporting HRs for stroke by categories of SBP, thereby offering insights valuable for clinical practice. Additionally, we present data separately for men and women within an already extensively described Norwegian cohort.29 30 Blood pressure was measured according to protocol in a controlled research environment. Few individuals were treated for hypertension at baseline, and the general cardiovascular risk burden was low in our population.
However, the findings of this study must be interpreted in light of certain limitations. First, our main exposure variable was obtained at age 40, and we cannot exclude confounding factors related to blood pressure changes in the follow-up period. Second, participants in the ACE 1950 Study were invited from the general population, but those who chose to participate may have had systematically differing traits compared with non-participants. This selection may have been exaggerated by the further subgrouping of participants who had also enrolled in the Age 40 Program (45% of individuals invited to the ACE 1950 Study were included in the final analysis). Third, even though we have controlled for covariates, we cannot exclude residual confounding. Fourth, the use of self-reported stroke may have introduced recall bias, as participants may misclassify stroke events. Still, previous studies have demonstrated acceptable validity of self-reported events such as stroke with positive predictive values ranging from 0.67 to 0.79.31,33 Finally, information on stroke severity would have enhanced the clinical relevance of our findings.
Conclusions
In this cohort, there was no significant association between SBP between 130 and 139 mm Hg at the age of 40 and stroke during 30 years of follow-up. However, long-term stroke risk increased with rising SBP, and above the threshold of 140 mm Hg, stroke risk was significantly increased in both sexes. A small subgroup of women had SBP ≥140 mm Hg at age 40 and these women had a fourfold increased risk of stroke compared with women with SBP <120 mm Hg in an analysis that adjusted for other clinical risk factors.
supplementary material
Acknowledgements
We are thankful for the study participants in the ACE 1950 Study, as well as the engaged and dedicated research team conducting the study, located both at Bærum Hospital, Vestre Viken Hospital Trust and the Clinical Trial Unit, Division of Medicine, Akershus University Hospital.
Footnotes
Funding: MMW-H was funded by a PhD grant from the South-Eastern Norway Regional Health Authority. The ACE 1950 Study was funded by Vestre Viken Hospital Trust, Akershus University Hospital Trust, the South-Eastern Norway Regional Health Authority, the University of Oslo and the Norwegian Health Association.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: All participants signed an informed consent before participating in the ACE 1950 Study. The study is approved by the Regional Committee for Medical and Health Research Ethics in Norway (reference number 2011/1475) and is in accordance with the Declaration of Helsinki. The written consent included the linkage of data from the ACE 1950 Study to national surveys and mandatory registries.
Contributor Information
Marte Meyer Walle-Hansen, Email: marte.meyer.walle-hansen@vestreviken.no.
Guri Hagberg, Email: guri.hagberg@gmail.com.
Marius Myrstad, Email: marium@vestreviken.no.
Trygve Berge, Email: trygveberge@gmail.com.
Thea Vigen, Email: theavigen@gmail.com.
Hege Ihle-Hansen, Email: hmihle@ous-hf.no.
Bente Thommessen, Email: bthommessen@yahoo.no.
Inger Ariansen, Email: inger.ariansen@fhi.no.
Magnus Nakrem Lyngbakken, Email: m.n.lyngbakken@medisin.uio.no.
Helge Røsjø, Email: h.r.rosjo@medisin.uio.no.
Ole Morten Rønning, Email: Ole.Morten.Ronning@ahus.no.
Arnljot Tveit, Email: arnljot.tveit@vestreviken.no.
Håkon Ihle-Hansen, Email: HAAIHL@vestreviken.no.
Data availability statement
The data set used in this study is not publicly available; the Data Protection Authority approval and patient consent do not allow for such publication. However, data access may be granted on application.
References
- 1.Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245–54. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA. 1996;275:1571–6. doi: 10.1001/jama.1996.03530440051036. [DOI] [PubMed] [Google Scholar]
- 3.O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–23. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 4.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 5.Diao D, Wright JM, Cundiff DK, et al. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012;2012:CD006742. doi: 10.1002/14651858.CD006742.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sundström J, Arima H, Jackson R, et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann Intern Med. 2015;162:184–91. doi: 10.7326/M14-0773. [DOI] [PubMed] [Google Scholar]
- 7.Musini VM, Tejani AM, Bassett K, et al. Pharmacotherapy for hypertension in adults 60 years or older. Cochrane Database Syst Rev. 2019;6:CD000028. doi: 10.1002/14651858.CD000028.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allen N, Berry JD, Ning H, et al. Impact of blood pressure and blood pressure change during middle age on the remaining lifetime risk for cardiovascular disease: the cardiovascular lifetime risk pooling project. Circulation. 2012;125:37–44. doi: 10.1161/CIRCULATIONAHA.110.002774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) Eur Heart J. 2018;39:3021–104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 10.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 11.Connelly PJ, Currie G, Delles C. Sex Differences in the Prevalence, Outcomes and Management of Hypertension. Curr Hypertens Rep. 2022;24:185–92. doi: 10.1007/s11906-022-01183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ji H, Niiranen TJ, Rader F, et al. Sex Differences in Blood Pressure Associations With Cardiovascular Outcomes. Circulation. 2021;143:761–3. doi: 10.1161/CIRCULATIONAHA.120.049360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark D, Hall ME, Jones DW. Dilemma of Blood Pressure Management in Older and Younger Adults. Hypertension. 2020;75:35–7. doi: 10.1161/HYPERTENSIONAHA.119.14125. [DOI] [PubMed] [Google Scholar]
- 14.Jones DW, Whelton PK, Allen N, et al. Management of Stage 1 Hypertension in Adults With A Low 10-Year Risk for Cardiovascular Disease: Filling A Guidance Gap: A Scientific Statement From the American Heart Association. Hypertension. 2021;77:e58–67. doi: 10.1161/HYP.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 15.Berge T, Vigen T, Pervez MO, et al. Heart and Brain Interactions--the Akershus Cardiac Examination (ACE) 1950 Study Design. Scand Cardiovasc J. 2015;49:308–15. doi: 10.3109/14017431.2015.1086813. [DOI] [PubMed] [Google Scholar]
- 16.Tverdal A, Hjellvik V, Selmer R. Heart rate and mortality from cardiovascular causes: a 12 year follow-up study of 379,843 men and women aged 40-45 years. Eur Heart J. 2008;29:2772–81. doi: 10.1093/eurheartj/ehn435. [DOI] [PubMed] [Google Scholar]
- 17.Gerber Y, Rana JS, Jacobs DR, Jr, et al. Blood Pressure Levels in Young Adulthood and Midlife Stroke Incidence in a Diverse Cohort. Hypertension. 2021;77:1683–93. doi: 10.1161/HYPERTENSIONAHA.120.16535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lacey B, Lewington S, Clarke R, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Glob Health. 2018;6:e641–9. doi: 10.1016/S2214-109X(18)30217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ACCORD Study Group. Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–7. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 22.Liszka HA, Mainous AG, King DE, et al. Prehypertension and cardiovascular morbidity. Ann Fam Med. 2005;3:294–9. doi: 10.1370/afm.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal N, St John J, Van Iterson EH, et al. Association of pulse pressure with death, myocardial infarction, and stroke among cardiovascular outcome trial participants. Am J Prev Cardiol . 2024;17:100623. doi: 10.1016/j.ajpc.2023.100623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kario K, Okawara Y, Kanegae H, et al. Potential Long-Term Benefit of Home Systolic Blood Pressure Below 125 mm Hg for Cardiovascular Risk Reduction: The J-HOP Study Extended. Hypertension. 2024;81:282–90. doi: 10.1161/HYPERTENSIONAHA.123.22122. [DOI] [PubMed] [Google Scholar]
- 25.Mainous AG, III, Everett CJ, Liszka H, et al. Prehypertension and mortality in a nationally representative cohort. Am J Cardiol. 2004;94:1496–500. doi: 10.1016/j.amjcard.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 26.Elfassy T, German CA, Muntner P, et al. Blood Pressure and Cardiovascular Disease Mortality Among US Adults: A Sex-Stratified Analysis, 1999-2019. Hypertension. 2023;80:1452–62. doi: 10.1161/HYPERTENSIONAHA.123.21228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rand K, Dahl FA, Viana J, et al. Fewer ischemic strokes, despite an ageing population: stroke models from observed incidence in Norway 2010-2015. BMC Health Serv Res. 2019;19:705. doi: 10.1186/s12913-019-4538-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The Norwegian Stroke Register; 2022. The Norwegian stroke register stroke in Norway in 2022 - report for patients and next-of-kin. [Google Scholar]
- 29.Berge T, Lyngbakken MN, Ihle-Hansen H, et al. Prevalence of atrial fibrillation and cardiovascular risk factors in a 63-65 years old general population cohort: the Akershus Cardiac Examination (ACE) 1950 Study. BMJ Open. 2018;8:e021704. doi: 10.1136/bmjopen-2018-021704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lyngbakken MN, Kvisvik B, Berge T, et al. Serial blood pressure measurements, left ventricular remodelling and cardiovascular outcomes. Eur J Clin Invest. 2023;53:e13876. doi: 10.1111/eci.13876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Engstad T, Bonaa KH, Viitanen M. Validity of self-reported stroke: The Tromso Study. Stroke. 2000;31:1602–7. doi: 10.1161/01.str.31.7.1602. [DOI] [PubMed] [Google Scholar]
- 32.Bots ML, Looman SJ, Koudstaal PJ, et al. Prevalence of stroke in the general population. The Rotterdam Study. Stroke . 1996;27:1499–501. doi: 10.1161/01.str.27.9.1499. [DOI] [PubMed] [Google Scholar]
- 33.Bergmann MM, Byers T, Freedman DS, et al. Validity of self-reported diagnoses leading to hospitalization: A comparison of self-reports with hospital records in A prospective study of American adults. Am J Epidemiol. 1998;147:969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data set used in this study is not publicly available; the Data Protection Authority approval and patient consent do not allow for such publication. However, data access may be granted on application.