Abstract
Abstract
Purpose
The Aboriginal Families Study is a prospective, intergenerational cohort study with well-established Aboriginal governance arrangements and community partnerships to support all research processes including data collection, interpretation and knowledge translation.
Participants
344 Aboriginal and Torres Strait Islander children born in South Australia between July 2011 and June 2013 and their mothers and other primary caregivers. Two waves of survey data collection have been undertaken: early in the first year postpartum and when the study children were aged 5–8 years. Children participated in direct developmental assessments of their cognitive, speech and language development at 5–8 years of age. Social and cultural determinants of health and well-being have been assessed at each wave of data collection.
Findings to date
Publications and policy briefs to date focus on social determinants of women’s and children’s physical and mental health; identifying gaps in access to pregnancy, postnatal, primary, specialist and allied healthcare; and evidence that Aboriginal-led services in South Australia have improved women’s experiences and access to antenatal care.
Future plans
Wave 3 follow-up is planned as the study children reach 14–16 years of age. Longitudinal follow-up of women and children in the cohort will generate new knowledge about factors promoting children and young people’s social and emotional well-being. Our goal is to build a stronger understanding of the potential for key domains of social and emotional well-being (eg, connection to community, family and kin, country and spirituality) to buffer the impacts of social determinants of health, including intergenerational trauma and social inequity.
Keywords: Community-Based Participatory Research, EPIDEMIOLOGY, Health Services, MENTAL HEALTH, PUBLIC HEALTH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Research team respected time needed to consult Aboriginal communities prior to designing the study.
Strong community, research and policy partnerships and Aboriginal governance arrangements.
Largely representative sample in terms of maternal age, infant birth weight and gestation.
Lack of culturally validated measures or reference values for Aboriginal and Torres Strait Islander children for some outcomes of interest.
Relatively small sample offset by limited initial selection bias and selective attrition.
Introduction
In 2007, the Australian Government committed to ‘close the gap in Aboriginal and Torres Strait Islander life expectancy within a generation’.1 While progress is being made (eg, improvements in infant birth weight, participation in preschool), Aboriginal and Torres Strait Islander children and young people continue to experience rates of out-of-home care, involvement with youth justice and youth suicide that are markedly higher than non-Aboriginal young people.2 In the states of South Australia and Victoria, the proportions of Aboriginal children in out-of-home care and rates of youth suicide are rising.2 3 Historically, policy responses have been dominated by a deficit discourse that defines Aboriginal and Torres Strait Islander people as ‘a problem’ needing to be solved, rather than recognising the strengths, aspirations and resilience of Aboriginal and Torres Strait Islander people as the foundation for system reform.4
For some time, Aboriginal and Torres Strait Islander people have been calling for policy-makers to move away from deficit-based thinking, and adopt strengths-based approaches grounded in Aboriginal knowledge and culture.4,7 The lack of robust evidence foregrounding the strengths of Aboriginal and Torres Strait Islander families and communities remains a significant obstacle to implementation of strengths-based approaches.8,12 Few longitudinal cohort studies have focused in detail on the way in which family, community and cultural strengths of Aboriginal and Torres Strait Islander children and young people may mitigate impacts of intergenerational and collective trauma.13,17 There is an urgent need to strengthen understanding of social, cultural and political determinants of good health,5 in particular focusing on factors promoting the social and emotional well-being of Aboriginal and Torres Strait Islander children, young people and families.
The Aboriginal Families Study was developed in partnership with the Aboriginal Health Council of South Australia and has had a commitment to benefiting Aboriginal and Torres Strait Islander communities right from the start.18 Initially, the study had a primary focus on hearing from women about their experiences during and after pregnancy, including experiences of accessing new Aboriginal Family Birthing Programme (AFBP) Services in metropolitan, regional and remote areas of South Australia. A second wave of follow-up timed when the children were in early primary school has enabled us to examine a broader range of issues. Importantly, this includes the role of family, community and cultural strengths and access to Aboriginal-led services in promoting positive maternal and child health outcomes. The purpose of this paper is to provide an overview of the study, including the rationale, aims of the first two waves of data collection and study measures incorporated in surveys and direct assessments of children’s cognitive, speech and language development. We also describe study governance arrangements, summarise key findings to date and outline plans for future follow-up of the cohort. Further information about the establishment of the study is summarised in earlier publications.18 19
Methods
Study design and approach
The Aboriginal Families Study is a population-based intergenerational cohort initially established to investigate the views and experiences of mothers having an Aboriginal baby in South Australia between July 2011 and June 2013. Funding to undertake community consultation with urban, regional and remote Aboriginal communities in South Australia to inform development of the study was obtained in 2007. Further funding was received in 2011 to establish the cohort and undertake interviews with women in the first 12 months postpartum (wave 1). A subsequent grant has enabled follow-up of the study children and their mothers/other primary caregivers when the children were aged 5–8 years (wave 2).
The research design and approach to community engagement, choice of study methods, selection of study measures, analysis methods and processes for interpreting and reporting findings were informed by and consistent with values and ethics for Aboriginal and Torres Strait Islander health research outlined by the Australian National Health and Medical Research Council (NHMRC) and the South Australian Aboriginal Health Research Accord.20,22 This included a commitment to community consultation to inform the study protocol; detailed pretesting of study procedures and study designed measures (undertaken prior to each wave of the study) and an overarching commitment to ensuring that the study would benefit Aboriginal communities in South Australia.
Development of the study protocol was informed by an 18-month period of community consultation respecting Aboriginal time and ways of working.18 Issues raised during these early consultations included the impact of life stresses and social health issues on women’s health during pregnancy and early parenting, lack of access to culturally safe and affordable health services, and concerns about the limited provision of support for Aboriginal and Torres Strait Islander fathers. There was strong support for the study to focus on social determinants of health and for Aboriginal researchers to undertake structured interviews so that all women would be asked the same questions. The research team was encouraged to talk to women about family violence, housing stress, grief and loss, legal problems and cannabis use. We were told that the way that questions were asked, how the study was explained and the language used would matter; that it would be important for Aboriginal researchers to lead community engagement; that communities would want to be kept informed about study progress and findings and that the findings ‘must be used to benefit Aboriginal families and communities’.18 To align with this guidance, the study employed only Aboriginal researchers to undertake fieldwork and undertook extensive pilot testing of study procedures and all study measures prior to both waves of data collection. Pilot testing was undertaken using a variety of methods, including yarning circles and one-to-one interviews. Interviews and yarning circles—held in urban, regional and remote communities—were used to seek verbal feedback about ways of asking about potentially sensitive issues in culturally acceptable and safe ways. Iterative testing of study procedures and potential study measures and approaches was undertaken, with each stage of testing integrating feedback from the previous stage. In wave 1, this phase of work took over 12 months and included development of a study designed measure of stressful events and social health issues. In wave 2, the pilot phase focused on development of a culturally adapted measure of Aboriginal women’s experiences of partner violence and development of study designed measures of Aboriginal ways of parenting, again taking over 12 months.
Study aims
At wave 1, the aims of the study were to (1) investigate the views and experiences of women having an Aboriginal and/or Torres Strait Islander baby in South Australia regarding pregnancy, birthing and postnatal services; (2) compare the experiences of women attending standard models of public antenatal care (eg, public clinic care) with those of women accessing antenatal care via Aboriginal Family Birthing Programme (AFBP) Services; (3) assess factors associated with early and continued engagement of Aboriginal and Torres Strait Islander families with antenatal care and (4) use information gathered in the study to inform early intervention strategies and appropriate care pathways for Aboriginal and Torres Strait Islander women and families.18
At wave 2, the study aims were extended to (5) investigate the longer-term consequences of stressful events and social health issues during pregnancy and postpartum for women’s health and well-being; (6) determine the extent to which maternal psychological distress, substance use and exposure to stressful events and social health issues in pregnancy and postpartum predict child health, development and well-being and (7) investigate whether there are social or cultural factors (eg, strong family and community connections, engagement with Aboriginal-led services) that promote resilience reflected in positive maternal and child outcomes despite experiencing adversity.
Sample size
The original sample size was determined based on the primary study hypothesis for wave 1. Our primary hypothesis was that compared with mothers of Aboriginal infants attending standard public models of antenatal care, mothers of Aboriginal babies who attended AFBP Services would be more likely to have their first antenatal visit in the first trimester of pregnancy and to attend five or more antenatal appointments. We estimated that a sample of 330 women with alpha of 0.05 would provide 80% power to detect a 20% absolute increase in the proportion of women attending their first visit in the first 13 weeks of pregnancy, and a 15% increase in the proportion of women attending five or more visits. Further details regarding the original study hypotheses and sample size calculations are available in an earlier paper.18
Aboriginal governance
An Aboriginal Governance Group comprising Aboriginal community leaders with expertise in Aboriginal women’s and children’s health policy and services has guided the study since 2007. The original 10-member Aboriginal Governance Group comprised community leaders with knowledge of South Australian Aboriginal communities and expertise in policy, government and community-controlled health services and included a member of the South Australian Council of Aboriginal Elders. Initially, the Aboriginal Governance Group provided advice and direction to the research team undertaking community consultations and interpreting community feedback. Since 2007, they have worked collaboratively with the research team to develop the study protocol, implement the research, analyse and interpret research findings, and disseminate results. They have guided and approved all decisions regarding recruitment procedures, conduct of the study, interpretation and release of findings and processes for ongoing community engagement and community feedback.
Over time, the terms of reference and composition of the group have evolved to address gaps in expertise in areas such as child health and well-being, child development and education. The inaugural chair of the Aboriginal Governance Group (KG) was a study investigator on the original NHMRC grant awarded in 2011, and several other Governance Group members were associate investigators. Over time, Aboriginal study staff and Governance Group members have increasingly taken on roles as members of the study investigator team. Aboriginal Governance Group members participate as coauthors on all study publications. The priority order for publications is set by the Aboriginal Governance Group and no publications are released without their approval.
Capacity building and knowledge exchange
The study investigator team is co-led by KG and SJB and includes both Aboriginal and non-Aboriginal investigators. Building capacity for working in ways that strengthen Aboriginal communities has been a constant focus since commencement of the study. Knowledge exchange between Aboriginal Governance Group members, study investigators and members of the research team has been key. Aboriginal investigators (KG, CL, YC and GG) and Aboriginal Governance Group members (CL, KG, AN, YC, TF and AC-C) bring community and policy knowledge, clinical experience in psychology and research experience using Indigenous methodologies. Non-Aboriginal investigators and researchers (SJB, DG, FKM, RG, SR, PM, MM and PC) bring experience in Aboriginal health research, epidemiological methods, biostatistics, psychology, child development, speech pathology, linguistics and nutrition. Capacity strengthening for study staff occurred via recruitment and training of Aboriginal researchers; knowledge exchange between Aboriginal and non-Aboriginal researchers; support for Aboriginal researchers to obtain research qualifications (eg, Certificate IV in Indigenous Research Capacity Building, Masters of Public Health, PhD). Ongoing two-way learning involved Aboriginal and non-Aboriginal team members sharing knowledge in their respective areas of expertise. Aboriginal team members shared their knowledge of culture and Aboriginal ways of knowing, being and doing in their communities. Non-Aboriginal researchers shared their knowledge of longitudinal study methods, analytical techniques and study strengths and limitations within the framework of western concepts of epidemiology.
Patient and public involvement
The study’s Aboriginal Governance Group has been involved in all phases of the research. Aboriginal communities in urban, regional and remote areas of South Australia have been consulted at key points in the study and have been kept informed regarding study progress and findings through community forums and newsletters. Community feedback informed the design of the study; research aims; selection of study measures; approaches to recruitment and follow-up of study participants and ongoing approaches to community engagement and feedback.
Cohort description
Who is in the cohort?
A total of 344 women enrolled in the study and completed the wave 1 questionnaire at around 7 months postpartum. To be eligible to take part, women needed to have given birth to an Aboriginal and/or Torres Strait Islander baby in South Australia between July 2011 and June 2013 and to be aged ≥14 years. Women were recruited via a range of organisations including Aboriginal Health Services, AFBP services and early childhood services. Staff from these agencies passed on information to eligible women and obtained women’s consent for a member of the research team to contact them. In addition, Aboriginal community researchers recruited women via the postnatal ward of a large metropolitan tertiary hospital; attended playgroups and community events to promote the study and recruited women via their own community networks.19
In waves 1 and 2, women completed a structured questionnaire with an Aboriginal community researcher or self-completed the questionnaire if preferred. At wave 2, women were asked to consent to participation of the study children in activities designed to assess cognitive and language development. If the study child was not living with their mother, the child’s primary caregiver (eg, father, another family member, foster carer) was asked to complete a modified version of the wave 2 questionnaire and to consent to the study child’s participation in wave 2. Figure 1 shows participant numbers for each wave of follow-up.
Figure 1. Flow diagram—participation in the Aboriginal Families Study. Denominator for percentages is the number of families participating at wave 1 (n=344).
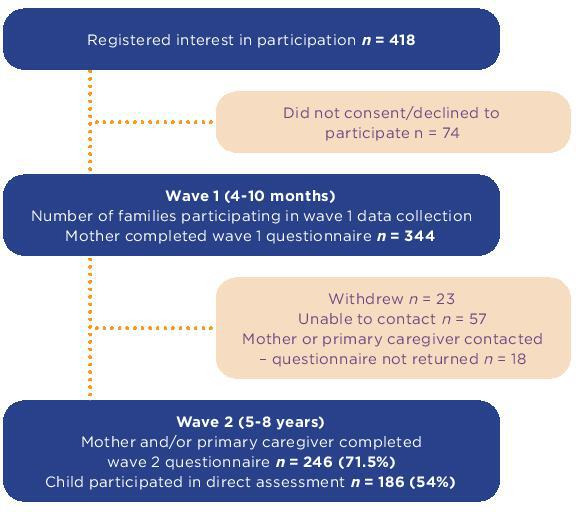
As shown in figure 1, 227 mothers and 24 other primary caregivers of the study children completed the wave 2 questionnaire providing data on 246 children (71.5% of original sample). Reasons for non-participation in wave 2 were mother and child withdrew, mostly because there was ‘too much happening at the time’ (n=23); mother/primary caregiver of the study child unable to be contacted (n=57); mother consented to wave 2 follow-up but did not complete the questionnaire (n=18).
A total of 186 children (54% of original sample) participated in direct developmental assessments. Numbers vary due to non-consent, ineligibility for direct assessments (eg, child with intellectual disability) and scheduling difficulties (including the need to pause school visits during 2020 because of the COVID-19 pandemic).
What has been measured?
Online supplemental table 1 summarises key domains assessed in wave 1 and wave 2. The wave 1 questionnaire asked women to report on experiences during pregnancy, pregnancy care, health behaviours, birth outcomes, postpartum health and well-being and experiences of using health and social care services. The wave 2 questionnaire asked about women’s health and well-being, health behaviours, stressful events and social health issues, health and well-being of the study child and about use of health services. The modified wave 2 questionnaire completed by other caregivers included a brief section focusing on living arrangements and the social context of the study child, and a longer section focusing on the health and well-being of the study child and their contacts with health services.
Family and social context
Data were gathered on mothers’ and fathers’ Aboriginal and Torres Strait Islander status and community/cultural connections; educational qualifications; participation in paid work and training/study; fathers’ involvement in pregnancy care and parenting; and the involvement of other people, including extended family members in caring for the study children in waves 1 and 2. In addition, women provided information on other adults and children living in the household, housing stability, health insurance status and access to a healthcare card (providing access to bulk billed medical care and subsidised pharmaceuticals).
Women were also asked to provide information regarding stressful events (eg, family member passing away) and social health issues (eg, housing problems) experienced during pregnancy and in the 12 months prior to wave 2 follow-up. These questions were study-designed and piloted to determine their acceptability and face validity before inclusion in the wave 1 questionnaire.
At wave 2, exposure to partner violence was assessed using a modified version of the Composite Abuse Scale.23 The modified scale included 30 items asking about different types of behaviours or actions by a current or former partner. Women were asked to indicate how often these actions had happened in the last 12 months: ‘never’, ‘once’, ‘several times’ or ‘a lot’ (scored 0–3). Women were categorised as experiencing physical IPV if they scored ≥1 for physical abuse items (eg, ‘pushed, grabbed or shoved you’); financial IPV if they scored ≥2 for financial abuse items (eg, ‘took money you needed for something else’) and emotional IPV if they scored ≥3 for emotional abuse items (eg, ‘tried to turn family, friends and children against you’). Further information about the development, acceptability and construct validity of this scale is available elsewhere.24
Maternal health and well-being
At wave 1, women reported on their health and well-being during the index pregnancy, and at the time of enrolment. At wave 2, women reported on their health and well-being in the previous 12 months. Physical health was assessed using single-item questions that covered pregnancy complications (eg, high blood pressure, gestational diabetes); medical conditions (eg, asthma, heart disease) and common postpartum physical health problems (eg, back pain). A range of measures were included to assess maternal mental health and well-being. The Kessler-5 (K-5), a modified version of the original Kessler-10 scale and shortened Kessler-6 scale for assessing psychological distress, was included in both the wave 1 and wave 2 questionnaires.25 The K-5 incorporates five items from the six-item version of the Kessler scale, with minor changes to item wording to improve acceptability among Aboriginal and Torres Strait Islander people.26 At wave 2, we also included the adapted Aboriginal version of the 9-item Patient Health Questionnaire (aPHQ-9, assessing depressive symptoms)27 and the Generalised Anxiety Disorder scale (GAD-7, assessing anxiety symptoms).28 29 The aPHQ-9 has demonstrated sensitivity, specificity and acceptability as a screening tool for depression in Aboriginal and Torres Strait Islander people.27 30 The GAD-7 was selected as a short screening measure for anxiety and pretested for cultural acceptability in the pilot study for wave 2. The wave 2 questionnaire also included the Aboriginal Resilience and Recovery Questionnaire, a 60-item multi-dimensional strengths questionnaire designed to assess strengths and resources associated with resilience, healing and recovery among Aboriginal and Torres Strait Islander help-seeking populations.31 Study designed questions on maternal cigarette smoking and use of cannabis were included in both questionnaires.32 At wave 2, this was supplemented by additional questions on prescription medications, use of alcohol and other drugs.33 34
Child health and well-being
At wave 1, mothers reported on infant birth weight and gestation, admission to special care nursery/neonatal intensive care, and initiation and duration of breastfeeding in the year after birth. At wave 2, mothers and caregivers provided information on childhood health conditions (eg, respiratory conditions, hearing problems) and developmental conditions (eg, autism, learning difficulties). Children’s strengths and resources were assessed in wave 2 using the parent/caregiver version of the Childhood Resilience Questionnaire (CRQ-PC).35 The CRQ-PC comprises 10 scales across the socioecological domains most important to children (personal, family, school and culture). The CRQ-PC has demonstrated content validity and cultural acceptability for assessing resilience in Aboriginal and Torres Strait Islander children.35 In addition, mothers and caregivers were asked to report on children’s peer relationships and emotional and behavioural difficulties using the Strengths and Difficulties Questionnaire (SDQ).36
Contacts with health and social care services
Mothers reported on health service use related to their own health and the health of the study child in both wave 1 and 2 questionnaires. At wave 1, this included carefully structured questions asking about experiences of using primary healthcare services and hospital-based care during pregnancy and birthing, and the early postnatal period. At wave 2, mothers were asked to report on experiences of primary healthcare, specialist health services, allied health services and hospital-based care when the study child was 5–8 years of age. Both questionnaires included questions designed to identify visits to Aboriginal community controlled health services and other Aboriginal-led programmes, such as AFBP services.37 Mothers were also asked to report on contacts with social care and advocacy services (eg, legal services, housing services, financial counselling). The caregivers’ version of the wave 2 questionnaire included questions asking about contacts with health services related to the study child.
School experiences
At wave 2, mothers and caregivers reported on children’s participation in preschool, childcare and school and experiences that the children had in the school setting.
Child cognitive and language development
At wave 2, children completed six developmental assessments with an Aboriginal community researcher. Assessments measured non-verbal skills (Matrices subtest of the Kaufman Brief Intelligence Test second edition),38 executive function (National Institutes of Health (NIH) Toolbox Dimensional Change Card Sort and Flanker Inhibitory Control and Attention Test),39 receptive vocabulary (NIH Toolbox Picture Vocabulary Test)40 and phonological memory (Children’s Test of Nonword Repetition).41 Assessments of language development were selected (and in some cases adapted) to minimise the potential for cultural and linguistic bias. For example, we selected a non-word repetition task because stimuli are novel and not dependent on culturally dependent knowledge. In addition, audio recordings of test stimulus items were re-recorded with a speaker of Australian Aboriginal English. Children were also invited to tell a story using a textless picture book as stimulus to assess oral narrative abilities (producing language) independent of dialect use. All measures were age appropriate for children aged 5–8 years and administered following standard instructions. In most cases, assessments were undertaken at school.
Parenting and activities with family
The final section of the wave 2 questionnaire included a series of study-designed questions that asked about parenting and activities the study children did with family, including extended family members. Questions on parenting asked mothers and caregivers to describe the strengths and values that they brought to parenting, how they encouraged children to learn about family and the world around them and how they prepared and supported children to deal with racism.
Collaboration
The study was designed with a view to providing evidence to inform policy and practice. Conditions of ethics approval preclude data sharing via a public repository. However, the investigator team and Aboriginal Governance Group welcome inquiries about the data and proposals for collaboration. For example, approval was granted for early release of findings from wave 2 to inform the development of Aboriginal and Torres Strait Islander maternal and child health continuity of care protocols in South Australia.42
Findings to date
How representative is the cohort?
Women ranged in age from 15 to 43 years at the time of giving birth to the study child and had connections with more than 35 Aboriginal and Torres Strait Islander language and community groups across Australia. At enrolment, 39% were living in Adelaide (a major metropolitan city), 36% in regional and 25% in remote areas of South Australia. Participant characteristics were compared with data collected by the South Australian Pregnancy Outcome Unit for all births to Aboriginal women in 2011. This showed that the original cohort was largely representative of Aboriginal women giving birth in South Australia during the study period in terms of maternal age, infant birth weight and length of gestation. Women having their first baby were slightly over-represented (42% of participants vs 34.3% of recorded births to Aboriginal and Torres Strait Islander mothers in 2011 data) and women giving birth at metropolitan hospitals were slightly under-represented (54% of participants vs 59% of recorded births to Aboriginal and Torres Strait Islander mothers in 2011 data).18 43
At wave 2, 44.0% of the study children were living in Adelaide (a major metropolitan city), 36.7% were living in regional and 19.2% were living in in remote areas. The average age of the study children at the time that mothers/caregivers completed the wave 2 questionnaire was 6.5 years (SD=1.0, range 5–8 years). Comparisons with the original cohort (see table 1) demonstrate that families participating in wave 2 are largely representative of the original cohort in terms of maternal place of residence and education at the time of recruitment, maternal age at first birth and birth outcomes of the infants.
Table 1. Characteristics of families participating in waves 1 and 2 of the Aboriginal Families Study.
| Wave 1(n=344) | Wave 2(n=246) | |
| n (%) | n (%) | |
| Mothers’ age at birth of study child | ||
| 15–19 years | 55 (16.0) | 36 (14.6) |
| 20–24 years | 140 (40.7) | 99 (40.2) |
| 25–29 years | 91 (26.5) | 67 (27.2) |
| 30–35 years | 33 (9.6) | 27 (11.0) |
| > 35 years | 25 (7.3) | 17 (6.9) |
| Mothers’ Indigenous status | ||
| Aboriginal and/or Torres Strait Islander | 319 (92.7) | 226 (91.9) |
| Not Aboriginal or Torres Strait Islander* | 25 (7.3) | 20 (8.1) |
| Birth weight of study child | ||
| <2500 g | 49 (15.0) | 31 (13.4) |
| ≥2500 g | 278 (85.0) | 201 (86.6) |
| Gestation at birth of study child | ||
| ≥37 weeks | 278 (86.9) | 198 (86.1) |
| <37 weeks | 42 (13.1) | 32 (13.9) |
| Study child born small for gestational age | ||
| ≥10th percentile | 240 (79.7) | 174 (80.9) |
| <10th percentile | 61 (20.3) | 41 (19.1) |
| Mothers’ place of residence at wave 1 | ||
| Metropolitan area | 134 (39.0) | 99 (40.2) |
| Regional | 123 (35.8) | 90 (36.6) |
| Remote | 87 (25.3) | 57 (23.2) |
| Mothers’ highest educational qualification at wave 1 | ||
| University degree | 22 (6.4) | 19 (7.7) |
| Diploma/certificate | 155 (45.1) | 119 (48.4) |
| Year 12 | 33 (9.6) | 23 (9.3) |
| Less than year 12 | 134 (39.0) | 85 (34.6) |
| Mothers’ participation in paid employment at wave 1 | ||
| Full-time job | 60 (17.4) | 50 (20.3) |
| Part-time job | 39 (11.3) | 32 (13.0) |
| Not in paid employment | 245 (71.2) | 164 (66.7) |
| Stressful events/social health issues during pregnancy | ||
| None | 45 (13.1) | 30 (12.2) |
| 1–2 | 105 (30.6) | 77 (31.3) |
| 3 or more | 193 (56.3) | 139 (56.5) |
| Total | 344 (100.0) | 246 (100.0) |
Non-Aboriginal mothers are mothers of Aboriginal children.
Experiences of pregnancy and pregnancy care (aims 1–3)
The mean age of women in the study at the time of giving birth to the study child was 25 years (SD 6, range 15–43 years). Just over half of women (51%) reported serious medical conditions and/or adverse events in a previous pregnancy.44 Most women (78%) had their first pregnancy visit during the first trimester, 18% attended their first visit between 14 and 26 weeks, 1.6% attended after 26 weeks and 1.7% had no antenatal care. Just over half of women (52%) attended AFBP services. Around one-third (34%) attended standard public antenatal care, and relatively small groups of women attended midwifery group practice (6%) or an Aboriginal Health Service (7%). Women who attended metropolitan or regional AFBP services or received care from an Aboriginal Health Service were more likely to (1) attend their first visit in the first trimester of pregnancy; (2) attend a minimum of five pregnancy check-ups and (3) report positive experiences of care, compared with women attending standard public antenatal care services.43
The AFBP was operating in three metropolitan and five regional sites in South Australia during the period of recruitment to the study.37 Most women in the study who attended AFBP Services saw Aboriginal Maternal Infant Care (AMIC) worker/s for at least some of their visits. In other models of care, women only occasionally saw Aboriginal health workers. Two-thirds of women attending AFBP services (68%) used transport arranged by the service to get to antenatal visits, compared with around 23% of women attending standard public antenatal care. One in four women attending AFBP services had a home visit from a midwife and/or AMIC worker, compared with 2% of women attending standard public care. Overall, women attending AFBP services and Aboriginal Health Services reported more positive experiences of interactions with health professionals.43 They also more commonly reported receiving support with social health issues, such as housing problems and financial difficulties.43
Despite the more positive experiences reported by women attending AFBP services, over half of women in the study perceived that they had experienced discrimination or unfair treatment by hospitals and health services providing perinatal care. Experiences of discrimination and unfair treatment were more common among women experiencing a greater number of stressful events and social health issues and among those who had a baby with a low birth weight (<2500 g) or infant born small for gestational age.45
Experiences of postnatal care (aims 1–3)
The majority of women saw a primary care practitioner at least once after leaving hospital: 86% saw a child and family health service nurse, 81% saw a general practitioner and 61% an Aboriginal health worker.46 Overall, women living in regional areas were more likely to have seen a primary care practitioner since the birth than women living in metropolitan areas. Women who attended AFBP services or Aboriginal health services in pregnancy were also more likely to see an AMIC worker or Aboriginal health worker after the birth.46 Gaps in service provision were evident in a small proportion of women who did not receive primary care follow-up despite experiencing serious medical conditions during pregnancy. Around 16% of women with gestational diabetes and 10% with hypertension in pregnancy had not seen a general practitioner since the birth.46
About women’s lives (aim 5)
Just over half of women in the study (56%) experienced three or more stressful events or social health issues during pregnancy.44 47 The six most common issues were being upset by family arguments (55%), housing problems (43%), family member/friend passing away (41%), being scared by other people’s behaviour (31%), being pestered for money (31%) and having to leave home because of a family argument (27%). There were no differences in exposure to stressful events and social health issues related to maternal age, number of children or adults in the household or place of residence. Women who had completed a degree or diploma reported fewer issues compared with women who did not have these educational qualifications. Women who had a healthcare concession card (an indicator of low income), reported smoking and/or use of cannabis during pregnancy experienced a greater number of issues.32 47
More than one-third of women (37%) experiencing three or more stressful events and social health issues during pregnancy reported high to very high postpartum psychological distress (Kessler-5 ≥12) compared with 11% of women experiencing no issues.47 Other factors associated with high/very high postpartum psychological distress were living in a remote area, having a healthcare concession card, having more than three children, not completing year 12 and smoking and/or using cannabis during pregnancy.47
Similar patterns of exposure to stressful events and social health issues were apparent at wave 2 follow-up.48 One in three women and children in the study had moved their place of residence three or more times in the 5 years prior to wave 2 follow-up and one in three women was on a waiting list for public housing. More than half of women (69%) reported some degree of financial stress. This affected families in many ways. The most common were not being able to pay bills on time (48%), putting off going to the doctor (19%) and going without meals (14%).48 Our more detailed inquiry about experiences of partner violence at wave 2 follow-up identified that 39% of women had experienced physical, financial or emotional abuse by a current or former partner in the previous 12 months.24 The majority of women in the study (82%) felt connected to a particular place or community, and 63% named family connections as one of the things that kept them strong.48
Wave 2 follow-up enabled exploration of social determinants of women’s and children’s health in greater depth. Drawing on findings from both waves has allowed us to look longitudinally at patterns of exposure to social determinants of health. In particular, we are examining the relationship between maternal and child mental health and well-being, and exposure to cannabis use, high residential mobility, partner violence and other social health issues.49
What keeps women and children strong and resilient (aim 8)
Another major focus of current work is what enables mothers and children to stay strong. This work draws on strengths-based measures of resilience specifically designed to be culturally relevant to Aboriginal and Torres Strait Islander adults and children.31 35 A series of papers will examine ways in which cultural, community and family strengths and resources support Aboriginal and Torres Strait Islander children and families to experience positive health and well-being. The role of inner strengths and supportive school environments is also being explored.
Strengths and limitations
Major strengths of the study include the strong community, research and policy partnerships underpinning the study; the time taken to consult with Aboriginal communities prior to designing the study; engagement of communities in pretesting study measures and procedures for wave 1 and wave 2 follow-up; the achievement of a sample largely representative in terms of maternal age, infant birth weight and gestation; and high level of participation of women and families living in urban, regional and remote areas of South Australia in both waves of data collection. The global COVID-19 pandemic impacted the final year of follow-up and participation would have been higher without the disruption to regional visits and face-to-face contact with families that this entailed. Despite this, 72% of families took part in wave 2 follow-up providing a strong platform for future follow-up of the cohort.
The Aboriginal Governance Group has guided the study from conception and has provided significant direction with regard to all stages of the study. The research team has endeavoured to combine Aboriginal ways of knowing, being and doing with epidemiological methods and approaches requiring multiway capacity exchange between the Aboriginal Governance Group, Aboriginal research team members and non-Aboriginal members of the research team. The decision to incorporate codesigned measures of adult and childhood resilience31 35 in wave 2 follow-up positions the study to make an important contribution to knowledge about ways in which connections to family, community and culture, as well as inner strengths and resources may act to support children and families in contexts of intergenerational trauma and social inequity.
Where possible, the study has used Aboriginal designed study measures and/or measures that have been validated with Aboriginal and Torres Strait Islander people (eg, Aboriginal Resilience and Recovery Questionnaire, adapted PHQ-9, Alcohol Use Disorders Identification Test (AUDIT) 3).27 31 33 35 When no culturally validated measures were available, we selected measures that had been used previously with Aboriginal and Torres Strait Islander people (eg, SDQ)36 50 and/or adapted measures to reduce the likelihood of cultural and linguistic bias. For example, child language measures were selected and adapted to improve linguistic appropriateness and cultural acceptability (eg, the non-word repetition task was modified to be administered as a play-based task).51 Nonetheless, we are conscious that interpretation of these measures must still be undertaken with caution.
Data are also limited by the relatively small number of families in the original cohort. This is partially offset by the high rate of participation among women approached to take part. We estimate that 83% of eligible women approached by the research team agreed to take part.47 Importantly, the original cohort participants were representative in terms of maternal age, infant birth weight and gestation. At wave 2, there was limited evidence of selective attrition in relation to key covariates, such as maternal age, education, place of residence or birth outcomes of the infants. The impacts of missing data are considered in all analyses and statistical techniques to account for missing data used where applicable.
The Aboriginal Families Study’s long-standing partnerships with the Aboriginal Health Council of South Australia and policy-makers in South Australia Health have facilitated rapid translation of the study findings and knowledge gained. For example, the findings from wave 1 were used to advocate for ongoing funding of the AFBP and expansion of multidisciplinary teams to provide greater support to families experiencing social health issues during pregnancy.37 More recently, findings from wave 2 reporting child health and health service use were included in a report commissioned by the South Australian Government to inform systems-level change to improve continuity of care for Aboriginal women and children in South Australia.42
Future plans
We are continuing to analyse data from wave 2 and simultaneously undertaking community feedback and consultations in preparation for wave 3 follow-up. This has included the release of a community report summarising key findings from the study to date.52 We hope to undertake wave 3 follow-up as the study children reach 14–16 years of age (in 2026–28). Wave 3 follow-up will involve yarning circles and a further wave of survey data collection with young people and their mothers/other primary caregivers. Our aim is to generate new knowledge about the potential for key domains of social and emotional well-being (eg, body, mind and emotions, connection to community, family and kin, country and spirituality) to buffer the impacts of social, political and historical determinants of mental health, health behaviours, educational and social pathways. We also aim to use data linkage with health and administrative data sets to examine health service use and pathways in education, child protection and youth justice to contextualise the experiences of women and young people in the cohort.
supplementary material
Acknowledgements
The authors respectfully acknowledge the Aboriginal and Torres Strait Islander Custodians of the Lands and Waters of Australia. We would like to acknowledge members of the Aboriginal Governance Group who guided all stages of the study, including interpretation of findings, and members of the research team (additional to the authors) who contributed to data collection, all women and families taking part in the study, and the many agencies that assisted us to connect with families.
Footnotes
Funding: This study was supported by two National Health and Medical Research Council (NHMRC) project grants (#1004395 and #1105561) and by funds awarded to the study by SA Health. SJB and MM hold NHMRC Leadership Investigator Grants. PM, GG and YC hold NHMRC Emerging Leadership Investigator Grants. Research at the Murdoch Children’s Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-082337).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by South Australian Aboriginal Health Research Ethics Committee (04.09.290) and Royal Children’s Hospital Human Research Ethics Committee (29076). Participants gave informed consent to participate in the study before taking part.
Data availability free text: The Intergenerational Health group at Murdoch Children’s Research Institute, Melbourne, Australia has been the co-ordinating unit for the study since 2007. Under the conditions of ethics approval, the principal investigator (SJB) acts as the custodian for study data. This includes data contained in study questionnaires, observational assessments of the study children and transcripts of discussion groups. Study participants retain ownership of data contributed to the study and are able to withdraw consent for use of these data prior to inclusion in study outputs, such as publications and policy briefs. The conditions of ethics approval preclude data sharing via a public repository. However, the Investigator Team and Aboriginal Governance Group welcome inquiries about the data and proposals for collaboration. Interested parties are invited to contact the lead investigators, KG (karen.glover@sahmri.com) and SJB (stephanie.brown@mcri.edu.au).
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
Karen Glover, Email: karen.glover@sahmri.com.
Cathy Leane, Email: cathy.leane2@sa.gov.au.
Arwen Nikolof, Email: arwen.nikolof@mcri.edu.au.
Deirdre Gartland, Email: deirdre.gartland@mcri.edu.au.
Petrea Cahir, Email: petrea.cahir@mcri.edu.au.
Fiona K Mensah, Email: fiona.mensah@mcri.edu.au.
Rebecca Giallo, Email: rebecca.giallo@mcri.edu.au.
Sheena Reilly, Email: s.reilly@griffith.edu.au.
Philippa Middleton, Email: philippa.middleton@adelaide.edu.au.
Maria Makrides, Email: Maria.Makrides@sahmri.com.
Theresa Francis, Email: theresa.francis@sa.gov.au.
Amanda Collins-Clinch, Email: amanda.collins-clinch@ahcwa.org.
Yvonne Clark, Email: yvonne.clark@sahmri.com.
Graham Gee, Email: graham.gee@mcri.edu.au.
Stephanie Janne Brown, Email: stephanie.brown@mcri.edu.au.
Data availability statement
Data may be obtained from a third party and are not publicly available.
References
- 1.Australian Institute of Health and Welfare . Canberra: AIHW; 2023. Aboriginal and Torres Strait Islander Health Performance Framework. [Google Scholar]
- 2.Productivity Commission Closing the gap: annual data compilation report Canberra: Australian Government. 2023. https://www.pc.gov.au/closing-the-gap-data/annual-data-report/report Available.
- 3.Cripps K. Australian Government: Australian Institute of Health and Welfare; 2023. Indigenous domestic and family violence, mental health and suicide. [Google Scholar]
- 4.Dodson M. The End in the Beginning: Re(de)Finding Aboriginality. Canberra: Australian Institute of Aboriginal Studies; 1994. [Google Scholar]
- 5.Fogarty W, Lovell M, Langenberg J, et al. Deficit Discourse and Strengths-Based Approaches: Changing the Narrative of Aboriginal and Torres Strait Islander Health and Wellbeing. Melbourne: The Lowitja Institute; 2018. [Google Scholar]
- 6.Dudgeon P, Bray A, D’costa B, et al. Decolonising Psychology: Validating Social and Emotional Wellbeing. Aust Psychol. 2017;52:316–25. doi: 10.1111/ap.12294. [DOI] [Google Scholar]
- 7.Laird P, Chang AB, Jacky J, et al. Conducting decolonizing research and practice with Australian First Nations to close the health gap. Health Res Policy Syst. 2021;19:127. doi: 10.1186/s12961-021-00773-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Usher K, Jackson D, Walker R, et al. Indigenous Resilience in Australia: A Scoping Review Using A Reflective Decolonizing Collective Dialogue. Front Public Health. 2021;9:630601. doi: 10.3389/fpubh.2021.630601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verbunt E, Luke J, Paradies Y, et al. Cultural determinants of health for Aboriginal and Torres Strait Islander people - a narrative overview of reviews. Int J Equity Health. 2021;20:181. doi: 10.1186/s12939-021-01514-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grove N, Brough M, Canuto C, et al. Aboriginal and Torres Strait Islander health research and the conduct of longitudinal studies: issues for debate. Aust N Z J Public Health. 2003;27:637–41. doi: 10.1111/j.1467-842x.2003.tb00612.x. [DOI] [PubMed] [Google Scholar]
- 11.Westhead S, Appleby Q, Andrews B, et al. The need for a roadmap to guide actions for Aboriginal and Torres Strait Islander adolescent health: youth governance as an essential foundation. Med J Aust. 2022;217:13–5. doi: 10.5694/mja2.51592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azzopardi P, Blow N, Purcell T, et al. Investing in the health of Aboriginal and Torres Strait Islander adolescents: a foundation for achieving health equity. Med J Aust. 2020;212:202. doi: 10.5694/mja2.50500. [DOI] [PubMed] [Google Scholar]
- 13.Study of Environment on Aboriginal Resilience and Child HealthInvestigators The Study of Environment on Aboriginal Resilience and Child Health (SEARCH): study protocol. BMC Public Health. 2010;10:287. doi: 10.1186/1471-2458-10-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones R, Thurber KA, Chapman J, et al. Study protocol: Our Cultures Count, the Mayi Kuwayu Study, a national longitudinal study of Aboriginal and Torres Strait Islander wellbeing. BMJ Open. 2018;8:e023861. doi: 10.1136/bmjopen-2018-023861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gubhaju L, Banks E, Ward J, et al. “Next Generation Youth Well-being Study:” understanding the health and social well-being trajectories of Australian Aboriginal adolescents aged 10-24 years: study protocol. BMJ Open. 2019;9:e028734. doi: 10.1136/bmjopen-2018-028734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bourke SC, Chapman J, Jones R, et al. Developing Aboriginal and Torres Strait Islander cultural indicators: an overview from Mayi Kuwayu, the National Study of Aboriginal and Torres Strait Islander Wellbeing. Int J Equity Health. 2022;21:109. doi: 10.1186/s12939-022-01710-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thurber KA, Thandrayen J, Banks E, et al. Strengths-based approaches for quantitative data analysis: A case study using the Australian Longitudinal Study of Indigenous Children. SSM Popul Health. 2020;12:100637. doi: 10.1016/j.ssmph.2020.100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buckskin M, Ah Kit J, Glover K, et al. Aboriginal Families Study: a population-based study keeping community and policy goals in mind right from the start. Int J Equity Health. 2013;12:41. doi: 10.1186/1475-9276-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weetra D, Glover K, Miller R, et al. Community engagement in the Aboriginal Families Study: Strategies to promote participation. Women Birth. 2019;32:72–9. doi: 10.1016/j.wombi.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 20.National Health and Medical Research Council . Commonwealth of Australia: Canberra; 2003. Values and ethics: guidelines for ethical conduct in Aboriginal and Torres Strait Islander research. [Google Scholar]
- 21.National Health and Medical Research Council . Canberra: Commonwealth of Australia; 2018. Ethical conduct in research with Aboriginal and Torres Strait Islander Peoples and communities: guidelines for researchers and stakeholders. [Google Scholar]
- 22.Morey K on behalf of the Wardliparingga Aboriginal Health Equity Research Theme South Australian Aboriginal Health Research Accord: companion document. SAHMRI, Adelaide, South Australia. 2017
- 23.Hegarty K, Bush R, Sheehan M, et al. The composite abuse scale: further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Vict . 2005;20:529–47. [PubMed] [Google Scholar]
- 24.Glover K, Gartland D, Leane C, et al. Development, acceptability and construct validity of the Aboriginal Women’s Experiences of Partner Violence Scale (AEPVS): a co-designed, multiphase study nested within an Australian Aboriginal and Torres Strait Islander birth cohort. BMJ Open. 2022;12:e059576. doi: 10.1136/bmjopen-2021-059576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–76. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- 26.Page IS, Ferrari AJ, Slade T, et al. Estimating the difference in prevalence of common mental disorder diagnoses for Aboriginal and Torres Strait Islander peoples compared to the general Australian population. Epidemiol Psychiatr Sci. 2022;31:e44. doi: 10.1017/S2045796022000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hackett ML, Teixeira‐Pinto A, Farnbach S, et al. Getting it Right: validating a culturally specific screening tool for depression (aPHQ‐9) in Aboriginal and Torres Strait Islander Australians. Med J Aust. 2019;211:24–30. doi: 10.5694/mja2.50212. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 29.Plummer F, Manea L, Trepel D, et al. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Farnbach S, Gee G, Eades A-M, et al. Process evaluation of the Getting it Right study and acceptability and feasibility of screening for depression with the aPHQ-9. BMC Public Health. 2019;19:1270. doi: 10.1186/s12889-019-7569-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gee G, Hulbert C, Kennedy H, et al. Development of an Aboriginal Resilience and Recovery Questionnaire - a collaboration between practitioners and help-seeking clients of a Victorian Aboriginal community controlled health service. BMC Med Res Methodol. 2023;23:290. doi: 10.1186/s12874-023-02091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown SJ, Mensah FK, Ah Kit J, et al. Use of cannabis during pregnancy and birth outcomes in an Aboriginal birth cohort: a cross-sectional, population-based study. BMJ Open. 2016;6:e010286. doi: 10.1136/bmjopen-2015-010286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Calabria B, Clifford A, Shakeshaft AP, et al. Identifying Aboriginal-specific AUDIT-C and AUDIT-3 cutoff scores for at-risk, high-risk, and likely dependent drinkers using measures of agreement with the 10-item Alcohol Use Disorders Identification Test. Addict Sci Clin Pract . 2014;9:17. doi: 10.1186/1940-0640-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wand H, Ward J, Bryant J, et al. Individual and population level impacts of illicit drug use, sexual risk behaviours on sexually transmitted infections among young Aboriginal and Torres Strait Islander people: results from the GOANNA survey. BMC Public Health. 2016;16:600. doi: 10.1186/s12889-016-3195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gartland D, Riggs E, Giallo R, et al. Development and validation of a multidimensional, culturally and socially inclusive Child Resilience Questionnaire (parent/caregiver report) to measure factors that support resilience: a community-based participatory research and psychometric testing study in Australia. BMJ Open. 2022;12:e061129. doi: 10.1136/bmjopen-2022-061129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawes DJ, Dadds MR. Australian data and psychometric properties of the Strengths and Difficulties Questionnaire. Aust N Z J Psychiatry. 2004;38:644–51. doi: 10.1080/j.1440-1614.2004.01427.x. [DOI] [PubMed] [Google Scholar]
- 37.Middleton P, Bubner T, Glover K, et al. “Partnerships are crucial”: an evaluation of the Aboriginal Family Birthing Program in South Australia. Aust N Z J Public Health. 2017;41:21–6. doi: 10.1111/1753-6405.12599. [DOI] [PubMed] [Google Scholar]
- 38.Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test, Second Edition. Pearson; 2004. [Google Scholar]
- 39.Zelazo PD, Anderson JE, Richler J, et al. II. NIH Toolbox Cognition Battery (CB): measuring executive function and attention. Monogr Soc Res Child Dev. 2013;78:16–33. doi: 10.1111/mono.12032. [DOI] [PubMed] [Google Scholar]
- 40.Gershon RC, Slotkin J, Manly JJ, et al. IV. NIH Toolbox Cognition Battery (CB): measuring language (vocabulary comprehension and reading decoding) Monogr Soc Res Child Dev. 2013;78:49–69. doi: 10.1111/mono.12034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gathercole SE, Willis CS, Baddeley AD, et al. The children’s test of nonword repetition: A test of phonological working memory. Memory. 1994;2:103–27. doi: 10.1080/09658219408258940. [DOI] [PubMed] [Google Scholar]
- 42.Glover K, Morey K, Rumbold A, et al. Systems change to improve Aboriginal and Torres Strait Islander maternal and child health continuity of care in South Australia. 2022
- 43.Brown SJ, Weetra D, Glover K, et al. Improving Aboriginal Women’s Experiences of Antenatal Care: Findings from the Aboriginal Families Study in South Australia. Birth. 2015;42:27–37. doi: 10.1111/birt.12143. [DOI] [PubMed] [Google Scholar]
- 44.Brown S, Glover K, Weetra D, et al. Improving Access to Antenatal Care for Aboriginal Women in South Australia: Evidence from a Population‐Based Study. Birth. 2016;43:134–43. doi: 10.1111/birt.12214. [DOI] [PubMed] [Google Scholar]
- 45.Brown SJ, Gartland D, Weetra D, et al. Health care experiences and birth outcomes: Results of an Aboriginal birth cohort. Women Birth. 2019;32:404–11. doi: 10.1016/j.wombi.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 46.Yelland J, Weetra D, Stuart-Butler D, et al. Primary health care for Aboriginal women and children in the year after birth: findings from a population-based study in South Australia. Aust N Z J Public Health. 2016;40:418–23. doi: 10.1111/1753-6405.12581. [DOI] [PubMed] [Google Scholar]
- 47.Weetra D, Glover K, Buckskin M, et al. Stressful events, social health issues and psychological distress in Aboriginal women having a baby in South Australia: implications for antenatal care. BMC Pregnancy Childbirth. 2016;16:88. doi: 10.1186/s12884-016-0867-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brown S, Glover K, Lean C, et al. Melbourne: Murdoch Children’s Research Institute; 2021. Aboriginal families study policy brief no 6: social health issues - time for action. [Google Scholar]
- 49.Mensah FK, Glover K, Leane C, et al. Understanding cannabis use and mental health difficulties in context with women’s experiences of stressful events and social health issues in pregnancy: The Aboriginal Families Study. Compr Psychiatry. 2024;131:152455. doi: 10.1016/j.comppsych.2024.152455. [DOI] [PubMed] [Google Scholar]
- 50.Williamson A, Redman S, Dadds M, et al. Acceptability of an emotional and behavioural screening tool for children in Aboriginal Community Controlled Health Services in urban NSW. Aust N Z J Psychiatry. 2010;44:894–900. doi: 10.3109/00048674.2010.489505. [DOI] [PubMed] [Google Scholar]
- 51.Gould J. Non-standard assessment practices in the evaluation of communication in Australian Aboriginal children. Clin Ling Phon. 2008;22:643–57. doi: 10.1080/02699200802222206. [DOI] [PubMed] [Google Scholar]
- 52.Glover K, Leane C, Nikolof A, et al. Murdoch Children’s Research Institute and South Australian Health and Medical Research Institute; 2023. Aboriginal families study community report. [Google Scholar]


