Abstract
Background
Acute pain due to rib fractures causes significant in-hospital morbidity and impacts patients’ quality of life after discharge. Intraoperative transthoracic cryoneurolysis of the intercostal nerves can improve postoperative pain; however, non-surgical patients are provided limited analgesia options. Here, we describe our experience with a bedside cryoanalgesia technique for management of acute rib fracture pain.
Methods
Five patients at a single level I trauma center completed bedside intercostal nerve cryoneurolysis (INC) using a handheld cryotherapy device and ultrasound guidance. Relative pain ratings (scale 0–10/10) and maximal incentive spirometry (ISmax) volumes were taken prior to the procedure as a baseline. Patients were observed for 24 hours after procedure, with relative pain ratings and ISmax recorded at 1, 8, 16, and 24 hours after procedure.
Results
Our patients were 29–88 years old and had one to five single-sided rib fractures. At baseline, they had high pre-procedure pain ratings (7–10/10) and ISmax volumes of 800–2000 mL. Many had improvements in their pain rating but little change in their ISmax at 1 hour (1–5/10 and 1000–2000 mL, respectively) and 8 hours (1–5/10 and 1250–2400 mL, respectively). ISmax volumes improved by 16 hours (1500–2400 mL) with comparable pain ratings (0–5/10). At 24 hours, pain ratings and ISmax ranged from 0 to 8/10 and from 1500 mL to 2400 mL, respectively. Each patient had improved pain control and ISmax volumes compared with their pre-procedure values. All patients reported the procedure as an asset to their recovery at discharge.
Conclusions
Our study demonstrates patients with rib fractures may experience improved pain ratings and ISmax values after INC. Percutaneous INC appears to be a viable adjunct to multimodal pain control for patients with rib fractures and should be considered in patients with difficult pain control. Further studies are required to fully assess INC safety, efficacy, post-discharge outcomes, and utility in patients with altered mental status or on mechanical ventilation.
Level of evidence
Level V, case series.
Keywords: pain management, rib fractures
WHAT IS ALREADY KNOWN ON THIS TOPIC.
WHAT THIS STUDY ADDS
Bedside percutaneous cryoneurolysis has several advantages over other methods of procedural pain control, is feasible and improves patient-reported pain and incentive spirometry in this case series.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Bedside percutaneous cryoneurolysis may prove to be a useful adjunct in the treatment of non-operative acute rib fracture pain.
Background
Rib fractures affect 10–20% of trauma patients and pose significant challenges in management.1,3 Approximately 59% of trauma patients with rib injuries report severe chest wall pain and impairment extending to 8 weeks after injury.4 Sequelae of poor pain management are most often insufficient respiratory function with increased risk for complications like atelectasis and pneumonia, all contributing to significant morbidity and mortality.4,6 Continuous intercostal nerve block (CINB) has been shown to decrease pain scores and hospital length of stay.7 Despite this, CINB requires maintenance of local anesthetic infusion through a foreign body and can be cumbersome.7 Ultrasound (US)-guided percutaneous intercostal cryoneurolysis (IC) offers potential benefits over CINB. It offers long-acting pain control without the need for catheters, pumps, or medications.8 9 Intraoperative IC combined with rib fracture fixation has shown promising early results.10 However, US-guided percutaneous IC at the bedside has only recently been introduced and there are limited data available regarding efficacy in this patient population.10 11 This technique aims to provide non-opioid, long-term pain relief in patients with rib fractures who are not surgical candidates.2 12 We present a case series of six patients at our institution, highlighting their pain ratings and incentive spirometry (IS) volumes before and after procedure.
Methods
Refinement of technique
Prior to patient enrollment, we conducted an iovera° acute rib fracture pain management training workshop in collaboration with a representative from Pacira and under the guidance of remote subject matter experts. The training event used a cadaveric model and all study team members attended the training event. The cadavers were placed in prone, supine, and lateral recumbent positions to establish the ideal access to each rib level, both posteriorly and anteriorly.
For all patients, each rib and corresponding fracture was identified using a phased array US probe (Venue Point of Care Ultrasound, GE Healthcare, Dallas, TX). A local anesthetic was administered at the treatment site for patient comfort. Once local anesthesia was achieved, the iovera° cryoneurolysis device (Pacira BioSciences Inc., Tampa, FL) was carefully guided under US visualization at a 45-degree angle targeting the neurovascular bundle of each affected rib (figure 1A). The device includes a long closed end needle and requires no incision to insert. Additional rib levels would then be treated sequentially. For most patients with multiple rib fractures our preference was to use a seated upright position with the patient leaning forward supporting their arms on a table. On some patients lateral decubitus positioning was used. We found it beneficial to treat each rib along the same vertical axis approximately 6 cm from the spine, given the fractures were all distal to the treatment area (figure 1B). On identification of the targeted neurovascular bundle, a 106-second freeze-thaw cycle was initiated via the device to achieve cryoneurolysis. In certain instances, if patients had ineffective or incomplete relief one or two additional treatments were administered at the same rib level.
Figure 1. Bedside intercostal nerve cryoneurolysis using the iovera° system instrumentation. Illustration of instrument and patient positioning with unobstructed view. (A) Cryoneurolysis device (1) positioned under ultrasound (2) guidance to target intervention location as determined by physician. (B) For most patients with multiple rib fractures the preference was to use a seated upright position with the patient leaning forward supporting their arms on a table. Each affected rib was treated along the same vertical axis approximately 6 cm from the spine, given the fractures were all distal to the treatment area.

Study design
All patients signed a written informed consent for the US-guided percutaneous IC procedure, follow-up, and publication of relevant non-identifiable information related to the study. The study team collected informed consent and baseline metrics on the morning of the procedure according to our protocol (online supplemental file 1). Patients were informed about possible risks of procedure including infections, bleeding, and pneumothorax. All patients were evaluated for baseline IS and status of rib-associated pain using adaptations from the Numeric Rating Scale (NRS), McGill Pain Questionnaire (MPQ), and Brief Pain Inventory (BPI). Sleep quality was assessed using the Medical Outcomes Study (MOS)-Sleep Interference and Sleep Quality (Pittsburgh Sleep Quality Index, PSQI), functionality by Quality of Life Scale (QOLS), and patient satisfaction by the Picker Patient Experience Questionnaire. Pain assessments13,15 were completed during the index admission before the procedure at baseline, at 1 hour, then every 8 hours for the first 24 hours after procedure, and on the day of discharge. IS readings were recorded at the same intervals. All recorded pain scores were subjective. After discharge, the study team contacted the patients to assess pain levels, adverse events, and satisfaction with the procedure. Additional assessments16 17 were completed at baseline and on discharge to assess return to functionality and impact of injuries on quality of life. Patient course of admission was not adjusted to meet study time points. The complete assessment schema is presented in table 1. The CARE case report guidelines were used to ensure proper reporting of patient information and discussion (online supplemental file 2).18
Table 1. Prospective case series study design time points and procedures.
| After procedure | |||||||
| Study procedure | Baseline | 1 h | 8 h | 16 h | 24 h | Discharge | 14 and 30-day follow-up |
| Informed consent | X | ||||||
| Incentive spirometry | X | X | X | X | X | X | |
| Pain (NRS) | X | X | X | X | X | X | X |
| Pain (MPQ) | X | X | X | ||||
| Pain interference (BPI) | X | X | X | ||||
| MOS-Sleep Interference | X | X | X | ||||
| Sleep Quality (PSQI) | X | X | X | ||||
| QOLS | X | X | |||||
| Patient satisfaction | X | ||||||
| Additional pain control | X | X | X | X | X | X | X |
Procedure included informed consent of the patient, incentive spirometry, pain (NRS and MPQ) scores, pain interference, MOS-Sleep Interference, Sleep Quality (PSQI), quality of life (QOLS), patient satisfaction, and use of additional pain management for rib fracture-associated pain. 1–24 h post-procedure inpatient time points have been demarcated.
BPIBrief Pain Inventoryhr(s)hour(s)MOSMedical Outcomes StudyMPQMcGill Pain QuestionnaireNRSNumeric Rating ScalePSQIPittsburgh Sleep Quality IndexQOLSQuality of Life Scale
Patient enrollment was based on a rolling assessment of patient safety and provider discretion. Enrollment was limited to patients with non-operative rib fractures to ribs 3–10 in adult trauma patients able to provide consent who reported their rib fracture-associated pain to be their most severe source of pain. Only patients with baseline rib fracture pain of greater than 3 out of 10 were considered for enrollment. Patients with fractures closer than 6 cm to the spine were excluded due to associated risk of sympathetic chain neurolysis and incomplete pain relief. The study was designed to conclude after successful treatment of five patients. Each case was documented individually before compiling aggregate data, aiming to identify patterns within the treated group. Due to the nature of this case series study, no statistical analysis was conducted. Patients were followed up at 14 and 30 days after procedure to assess pain via NRS and MPQ, pain interference via BPI, MOS-Sleep Interference, PSQI, QOLS, patient satisfaction, and the use of additional pain control modalities, specifically for pain related to the rib fracture. Pain scores and IS at pre-procedure, procedure, and post-procedure time points (table 2) were reported as median and IQR. QOLS (table 3) and pain interference survey (table 4) were also reported as median and IQR.
Table 2. Patient-reported pain rating (Numeric Rating Scale; 0–10/10) and incentive spirometry volumes (milliliters) before and after bedside intercostal nerve cryoneurolysis to treat rib fracture pain.
| Patient | Pre-procedure | 1 h | 8 h | 16 h | 24 h | Post-procedure pain rating | ||||||
| Pain rating | IS (mL) | Pain rating | IS (mL) | Pain rating | IS (mL) | Pain rating | IS (mL) | Pain rating | IS (mL) | 14 days | 30 days | |
| Case 1 | 8/10 | 800 | 0/10 | 1000 | 0/10 | 1250 | 0/10 | 1500 | 0/10 | 1250 | ||
| Case 3 | 8/10 | 1500 | 5/10 | 1500 | 5/10 | 2400 | 5/10 | 2400 | 7/10 | 2300 | 2/10 | 1/10 |
| Case 4 | 10/10 | 2000 | 4/10 | 2100 | 1/10 | 1700 | 6/10 | 2000 | 8/10 | 2100 | 3/10 | 4/10 |
| Case 5 | 7/10 | 1000 | 2/10 | 1200 | 2/10 | 1250 | 4/10 | 1250 | 3/10 | 1500 | 6/10 | |
| Case 6 | 7/10 | 1000 | 2/10 | 1500 | 4/10 | 1500 | 1/20 | 2000 | 0/10 | 2250 | 2/10 | |
| Median (IQR) | 8/10(7/10–8/10) | 1000(1000–1500) | 2/10(2/10–4/10) | 1500(1200–1500) | 2/10(1/10–4/10) | 1500(1250–1700) | 4/10(1/10–5/10) | 2000(1500–2000) | 3/10(0/10–7/10) | 2100(1500–2250) | 2.5/10(2/10–3.75/10) | 2.5/10(1.75/10–3.25/10) |
Missing values indicate loss to follow-up.
fx(s)fracture(s)IQRinterquartile rangeISincentive spirometry
Table 3. Quality of Life Scale (QOLS) before and after procedure between baseline and 14-day follow-up of patients with rib fracture(s).
| Patient satisfaction with… | Before procedure | After procedure | Percent change |
| Material comforts of home, food, conveniences, financial security, median (IQR) | 7.0 (5.0–7.0) | 7.0 (7.0–7.0) | 0.0 |
| Health—being physically fit and vigorous, median (IQR) | 5.0 (5.0–6.0) | 5.0 (4.8–5.3) | 0.0 |
| Relationships with parents, siblings, and other relatives, median (IQR) | 6.0 (6.0–7.0) | 6.0 (5.8–6.3) | 0.0 |
| Having and rearing children, median (IQR) | 6.0 (6.0–6.3) | 6.0 (6.0–6.5) | 0.0 |
| Close relationships with spouse or significant other, median (IQR) | 6.5 (6.0–7.0) | 7.0 (6.8–7.0) | 7.7 |
| Close friends, median (IQR) | 7.0 (6.0–7.0) | 7.0 (7.0–7.0) | 0.0 |
| Helping and encouraging others, volunteering, giving advice, median (IQR) | 5.0 (5.0–5.0) | 6.0 (5.0–7.0) | 20.0 |
| Participating in organizations and public affairs, mean±SD | 5.0 (5.0–6.0) | 5.5 (5.0–6.3) | 10.0 |
| Learning—attending school, improving understanding, etc, median (IQR) | 6.0 (6.0–7.0) | 7.0 (6.8–7.0) | 16.7 |
| Understanding yourself—knowing your assets and limitations, mean±SD | 6.0 (6.0–7.0) | 7.0 (6.8–7.0) | 16.7 |
| Work—job or in home, median (IQR) | 5.0 (5.0–6.0) | 4.5 (3.8–5.3) | −10.0 |
| Expressing yourself creatively, median (IQR) | 6.0 (6.0–6.0) | 7.0 (6.8–7.0) | 16.7 |
| Socializing—meeting other people or doing things, median (IQR) | 6.0 (6.0–6.0) | 6.0 (4.8–7.0) | 0.0 |
| Reading, listening to music, or observing entertainment, median (IQR) | 6.0 (5.0–7.0) | 7.0 (7.0–7.0) | 16.7 |
| Participating in active recreation, median (IQR) | 5.0 (3.0–5.0) | 5.0 (5.0–5.3) | 0.0 |
| Independence, doing for yourself, median (IQR) | 7.0 (3.0–7.0) | 5.0 (5.0–5.5) | −28.6 |
The patient lost to follow-up has been excluded. A positive percent change indicates improved patient satisfaction. A negative percent change indicates reduced patient satisfaction. A score of 1 is equal to ‘terrible’ and a score of 7 is equal to ‘very happy’.
Table 4. Pain interference survey before and after procedure between baseline and 14-day follow-up of patients with rib fracture(s).
| Pain interference with… | Before procedure | After procedure | Percent change |
| General activity, median (IQR) | 10.0 (10.0–10.0) | 4.5 (3.0–5.3) | −55.0 |
| Mood, median (IQR) | 7.0 (0.0–8.0) | 2.5 (0.8–5.5) | −64.3 |
| Walking, median (IQR) | 10.0 (10.0–10.0) | 6.5 (4.5–7.0) | −35.0 |
| Normal work (home, work, school), median (IQR) | 10.0 (10.0–10.0) | 6.0 (4.5–6.3) | −40.0 |
| Relation with other people, median (IQR) | 3.5 (0.0–7.3) | 0.5 (0.0–3.0) | −85.7 |
| Sleep, median (IQR) | 5.0 (5.0–7.0) | 4.5 (3.0–6.3) | −10.0 |
| Enjoyment of life, median (IQR) | 10.0 (10.0–10.0) | 5.0 (3.0–6.8) | −50.0 |
The patient lost to follow-up has been excluded. A negative percent change indicates reduced pain interference reported from the patient. A score of 0 is equal to no pain and a score of 10 is equal to high pain. Adapted from: McGill Pain Questionnaire (MPQ) and the Cleeland’s Brief Pain Inventory (BPI).
Case 1
A patient in their 70s with a medical history of diabetes mellitus, hypertension, and chronic kidney disease presented after slipping and falling on ice with a left-sided 9th rib fracture and left superior and inferior pubic rami fractures. Despite the continued use of analgesics, the patient continued to endorse posterior rib pain at the site of the mildly displaced fracture. The patient’s initial reported pain level was 9/10 on the subjective pain scale and initial IS reading was about 800 mL. After just 1 hour, the patient reported their pain level as 1/10 on the subjective pain scale and IS measured as 1000 mL. At the 8-hour follow-up, pain was 0/10 at rest and 7–8/10 with movement and IS was 1250 mL. At 16 hours, pain continued to be 0/10 at rest, 5/10 with movement and IS was up to 1500 mL. Finally, at 24 hours, the patient’s pain was 0/10 at rest and with movement and IS remained constant between 1250 and 1500 mL. The patient could not be reached for the 14-day follow-up.
Case 2
A previously healthy patient in their 30s presented after motor vehicle crash (MVC) with multiple injuries including left-sided rib fractures to ribs 2–7, a left hemopneumothorax, left L2–L4 transverse process fractures, bilateral superior and inferior pubic rami fractures, and right comminuted sacral fracture. The patient was in obvious pain due to their rib fractures but was uncomfortable and in much more pain due to the position they had to be placed in to complete the procedure. We asked the patient if they wanted to terminate the procedure; it was our opinion that we could not effectively and safely continue if the patient was so uncomfortable. Ultimately, the patient agreed they were not tolerating the procedure and decided it would be best to terminate the procedure at that time due to concomitant injuries.
Case 3
A previously healthy patient in their 20s presented after MVC with right-sided rib fractures to ribs 3–6. They were admitted to the trauma service for uncontrolled pain. The patient’s initial reported pain level was 8/10 on the subjective pain scale and initial IS reading was 1500 mL. After 1 hour, the patient’s reported pain level was 5/10 on the subjective pain scale and their IS measured was 1500 mL. At the 8-hour follow-up, pain was 5/10 at rest and IS was 2400 mL. At 16 hours, the pain continued to be 5/10 and IS was 2400 mL. Finally, at 24 hours, the patient’s pain was 7/10 at rest and IS remained constant between 2300 and 2400 mL. While ongoing subjective pain scores demonstrated minimal reduction, the patient was not in any visible distress or discomfort and was walking normally without guarded behavior. At the 14-day follow-up, the patient reported a complete reduction in pain interference with general activity, normal work, and sleep.
Case 4
A previously healthy patient in their 60s presented after MVC with left-sided rib fractures to ribs 3–7. They were admitted to the trauma service for uncontrolled pain. The patient’s initial reported pain level was 10/10 on the subjective pain scale and initial IS was about 2000 mL. After 1 hour, the patient’s reported pain level was 2/10 on the subjective pain scale and IS was 2000 mL. At the 8-hour follow-up, pain was 1/10 at rest and IS was 1700 mL. At 16 hours, pain was 5/10 and IS was measured at 1900 mL. Finally, at 24 hours, the patient’s pain level was 8/10 at rest and IS remained constant between 1900 and 2100 mL. At the 14-day follow-up, the patient reported a reduction in pain interference with general activity and normal work, and an increase in pain interference with sleep.
Case 5
A patient in their 30s with a medical history of diabetes mellitus presented after MVC with right-sided posterior rib fractures to ribs 5–8 with moderate right pneumothorax and lung contusion. The patient’s initial reported pain level before the procedure was 7/10 on the subjective pain scale and initial IS was about 1000 mL. At 1-hour after cryoneurolysis, pain was 2/10 and IS was 1200 mL. At the 8-hour follow-up, pain was 2/10 and IS was 1250 mL. At 16 hours, pain was 4/10 and IS was 1250 mL. On discharge at 24-hour follow-up, the patient reported rib-specific pain as 3/10 and IS remained stable between 1200 and 1500 mL. At the 14-day follow-up, the patient reported a reduction in pain interference with general activity and normal work, and an increase in pain interference with sleep.
Case 6
A patient in their 80s with a medical history of hypertension, chronic obstructive pulmonary disease, chronic kidney disease, and an L5 vertebra fracture presented with right-sided pneumothorax and fractures to ribs 6–8 on the right side after falling out of bed. Ribs 7 and 8 underwent a second freeze cycle posterior to the fracture and ribs 6 and 7 underwent an additional freeze cycle anterior to the fracture after patient feedback. Follow-up checks were completed after procedure at 1, 8, 16 and 24 hours. The patient’s initial reported pain level was 7/10 on the subjective pain scale and initial IS was about 1000 mL. After 1 hour, the patient’s reported pain level was 2/10 and IS measured was 1500 mL. At the 8-hour follow-up, pain was 4/10 and IS was 1500 mL. At 16 hours, pain was 1/10 without the need for additional pain medication and IS was up to 2000 mL. Finally, at 24 hours, the patient’s pain level was 0/10 and IS was 2000–2500 mL. At the 14-day follow-up, the patient reported a reduction in pain interference with general activity, normal work, and sleep.
Results
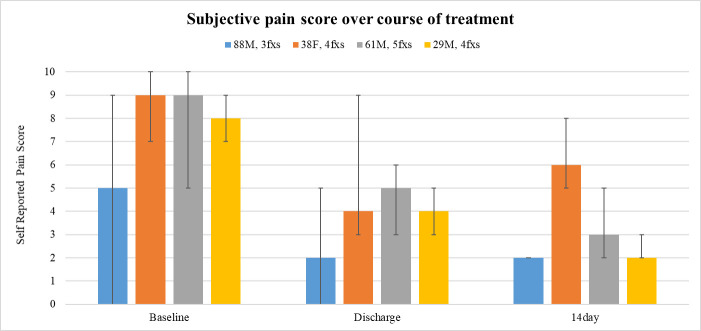
Five out of six enrolled patients completed the iovera° acute rib fracture pain management procedure. One patient was unable to tolerate the procedure due to positioning challenges from concomitant injuries, therefore, their procedure was terminated. The median age of patients was 61 years with an IQR of 38–76 years. Follow-up included phone call to patient by study team at 14 and 30 days after discharge. One patient was lost to follow-up at 14 days and three patients were lost to follow-up at 30 days. All patients who successfully completed treatment for their rib fractures exhibited improved pain management and IS (table 2). While subjective pain was not eliminated completely, control was universally achieved. The median (IQR) for pre-procedure pain rating was 8/10 (7/10–8/10); at 1 hour 2/10 (2/10–4/10); at 8 hours 2/10 (1/10–4/10); at 16 hours 4/10 (1/10–5/10); at 24 hours 3/10 (0/10–7/10); at 14 days after procedure 2.5/10 (2/10–3.75/10); and at 30 days after procedure 2.5/10 (1.75/10–3.25/10) (table 2). The median (IQR) for pre-procedure IS was 1000 (1000–1500); at 1 hour 1500 (1200–1500); at 8 hours 1500 (1250–1700); at 16 hours 2000 (1500–2000); and at 24 hours 2100 (1500–2250) (table 2). Pain management was also maintained through 30 days after discharge for patients who were not lost to follow-up (figure 2). At the 14-day follow-up (n=4) and 30-day follow-up (n=2), the median (IQR) pain scores were reported as 2.5/10 (2/10–3.75/10) and 2.5/10 (1.75/10–3.25/10), respectively, with no complications or need for pain medication due to their rib fracture(s). Quality of life scoring showed minor improvements as well (table 3), but the greatest impact was seen in reduction of pain interference scores (table 4). Patient satisfaction with their admission and the use of IC for pain control was universally positive. Patients did not experience any complications related to the procedure.
Figure 2. Self-reported subjective pain score by study milestone. The mean pain scores with minimum and maximum pain scores are shown for each time point. Patient lost to follow-up was excluded. F, female; fxs, fractures; M, male.
Discussion
In this prospective case series study of six patients, we explored the utility of US-guided percutaneous IC technique for managing acute rib fracture pain using the iovera° handheld cryotherapy device in adult trauma patients. Despite the common occurrence of rib fractures in traumatic injuries leading to substantial pain and respiratory insufficiency, effective pain management remains a challenge.19 Traditional approaches to pain management in this patient population like systemic opioids, regional anesthesia, and surgical fixation have notable limitations.2 19 The nature of this study allowed for real-time data collection minimizing the potential biases associated with retrospective studies and provided resolution on patient experience.
Our findings determine this procedure to be feasible for the treatment of non-operative rib fracture pain and contribute preliminary evidence supporting the utility of US-guided percutaneous IC in the context of existing literature. We observed significant pain reduction after procedure, evident from 1 hour and sustained over 24 hours. While immediate lung function improvement was limited, significant enhancement in IS volume was noted after 16 hours. No complications resulted from the utility of this procedure in our patient population. Patient satisfaction was measured at 14 and 30 days after discharge; patients reported satisfaction with their pain management underscoring the potentially positive impact on quality of life.
These data suggest that US-guided percutaneous IC may be a valuable addition to pain management options for traumatic patients with rib fracture. It offers the advantage of providing non-opioid pain relief, particularly at a time when opioid misuse leads to the risk of addiction and respiratory depression.20 21 Moreover, the procedure appears to be beneficial for trauma patients who require rapid pain control to facilitate proper pulmonary functionality and prevent respiratory complications. The significant reduction in pain reported by patients after undergoing this procedure confirms its effectiveness and highlights its role in facilitating faster patient recovery. Patients may have a more rapid return to daily activities leading to a lower incidence of complications associated with immobility. Therefore, our findings support the inclusion of the US-guided percutaneous IC in pain management plans, aiming to improve patient outcomes while reducing the adverse effects associated with traditional opioid-based treatments. Subsequent investigations should focus on hypothesis testing the efficacy and generalizability of this intervention in mitigating the pain resulting from a non-operative rib fracture in the trauma patient population.
Despite the promising results, our study has certain limitations. The small sample size, lack of a control group, and loss to follow-up restrict determining safety, efficacy, and the extent to which these results can be generalized to a larger population. Ideally, only patients with isolated rib fractures would have been enrolled in the study. The variation in patient age and mechanisms of injury may influence the response to treatment, affecting the external validity of the study. Opioid usage was not collected in this study which will be a useful adjunct in further assessments of this technique. Additionally, a single proceduralist was used for all interventions within our trial which could impact reproducibility. Future research should further assess the efficacy, reproducibility, and potential adverse events by conducting larger prospective trials with a more diverse patient population.
Our findings suggest that US-guided percutaneous IC is a feasible option with potentially favorable attributes in the management of trauma patients with acute rib fracture pain. Possible benefits of this procedure include rapid pain relief, improved pulmonary functionality, and high patient satisfaction. To evaluate additional applicability in clinical practice, future investigations should study its utility in specific patient populations, such as those with altered mental status or on mechanical ventilation.
supplementary material
Acknowledgements
The authors thank Dr Michael Truitt for his assistance in obtaining funding and providing education to the research team prior to study start-up; Dr Anne Murray for her contributions in editing materials for this project; and the General Surgery Residency Program at Methodist Dallas Medical Center for their support throughout the study.
Footnotes
Funding: This study and the associated training were funded by PACIRA IIT (grants 2020-0604 and 2021-031).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: The WCG Institutional Review Board approval was obtained for the short case series study (Rib Fracture Cryoanalgesia, Study ID 1338374). Participants gave informed consent to participate in the study before taking part.
Presented at: This work was presented as a poster presentation at the 2024 Chest Wall Injury Summit on April 11–13, 2024 in Salt Lake City, Utah.
Contributor Information
Cynthia I Villalta, Email: CynthiaVillalta@mhd.com.
Rabiya K Mian, Email: RabiyaMian@mhd.com.
Heather M Grossman Verner, Email: HeatherGrossmanVerner@mhd.com.
Dana Farsakh, Email: DanaFarsakh@mhd.com.
Timothy C Browne, Email: TimothyBrowne@mhd.com.
Zachary S Goldstein, Email: Zachary.Goldstein632553@tufts.edu.
Conner McDaniel, Email: ConnerMcDaniel@mhd.com.
Data availability statement
Data sharing not applicable as no datasets generated and/or analyzed for this study.
References
- 1.Saillant NN, Sein V. Management of severe chest wall trauma. J Emerg Crit Care Med. 2018;2:41. doi: 10.21037/jeccm.2018.04.03. [DOI] [Google Scholar]
- 2.Fernandez CA, Narveson JR, Niu F, Norton E, Brown EC, Punja V, Veatch JM, Capasso T, Patel ND, Ewing K, et al. In-hospital outcomes of intercostal nerve cryoablation and surgical stabilization of rib fractures. J Trauma Acute Care Surg. 2022;93:695–701. doi: 10.1097/TA.0000000000003623. [DOI] [PubMed] [Google Scholar]
- 3.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975–9. doi: 10.1097/00005373-199412000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Fabricant L, Ham B, Mullins R, Mayberry J. Prolonged pain and disability are common after rib fractures. Am J Surg. 2013;205:511–5. doi: 10.1016/j.amjsurg.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Vossler JD, Zhao FZ. Intercostal nerve cryoablation for control of traumatic rib fracture pain: A case report. Trauma Case Rep . 2019;23:100229. doi: 10.1016/j.tcr.2019.100229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marturano MN, Thakkar V, Wang H, Cunningham KW, Lauer C, Sachdev G, Ross SW, Jordan MM, Dieffenbaugher ST, Sing RF, et al. Intercostal nerve cryoablation during surgical stabilization of rib fractures decreases post-operative opioid use, ventilation days, and intensive care days. Injury. 2023;54 doi: 10.1016/j.injury.2023.05.034. [DOI] [PubMed] [Google Scholar]
- 7.Kim M, Moore JE. Chest Trauma: Current Recommendations for Rib Fractures, Pneumothorax, and Other Injuries. Curr Anesthesiol Rep. 2020;10:61–8. doi: 10.1007/s40140-020-00374-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finneran Iv JJ, Gabriel RA, Swisher MW, Berndtson AE, Godat LN, Costantini TW, Ilfeld BM. Ultrasound-guided percutaneous intercostal nerve cryoneurolysis for analgesia following traumatic rib fracture -a case series. Korean J Anesthesiol. 2020;73:455–9. doi: 10.4097/kja.19395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ilfeld BM. Continuous Peripheral Nerve Blocks: An Update of the Published Evidence and Comparison With Novel, Alternative Analgesic Modalities. Anesth Analg. 2017;124:308–35. doi: 10.1213/ANE.0000000000001581. [DOI] [PubMed] [Google Scholar]
- 10.Bauman ZM, Loftus J, Raposo-Hadley A, Samuel S, Ernst W, Evans CH, Cemaj S, Kaye AJ. Surgical stabilization of rib fractures combined with intercostal nerve cryoablation proves to be more cost effective by reducing hospital length of stay and narcotics. Injury. 2021;52:1128–32. doi: 10.1016/j.injury.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Cha PI, Min JG, Patil A, Choi J, Kothary NN, Forrester JD. Efficacy of intercostal cryoneurolysis as an analgesic adjunct for chest wall pain after surgery or trauma: systematic review. Trauma Surg Acute Care Open . 2021;6:e000690. doi: 10.1136/tsaco-2021-000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biel E, Aroke EN, Maye J, Zhang SJ. The applications of cryoneurolysis for acute and chronic pain management. Pain Pract. 2023;23:204–15. doi: 10.1111/papr.13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23:129–38. [PubMed] [Google Scholar]
- 14.Farley P, Griffin RL, Jansen JO, Bosarge PL. Quantifying Pain Associated With Rib Fractures. J Surg Res. 2020;246:476–81. doi: 10.1016/j.jss.2019.09.032. [DOI] [PubMed] [Google Scholar]
- 15.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 16.Zitser J, Allen IE, Falgàs N, Le MM, Neylan TC, Kramer JH, Walsh CM. Pittsburgh Sleep Quality Index (PSQI) responses are modulated by total sleep time and wake after sleep onset in healthy older adults. PLoS One. 2022;17:e0270095. doi: 10.1371/journal.pone.0270095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14:353–8. doi: 10.1093/intqhc/14.5.353. [DOI] [PubMed] [Google Scholar]
- 18.The careguidelines: consensus-based clinical case reporting guideline development. 2023. [11-Mar-2024]. https://www.equator-network.org/reporting-guidelines/care/ Available. Accessed.
- 19.Koushik SS, Bui A, Slinchenkova K, Badwal A, Lee C, Noss BO, Raghavan J, Viswanath O, Shaparin N. Analgesic Techniques for Rib Fractures-A Comprehensive Review Article. Curr Pain Headache Rep. 2023;27:747–55. doi: 10.1007/s11916-023-01172-9. [DOI] [PubMed] [Google Scholar]
- 20.Bateman JT, Saunders SE, Levitt ES. Understanding and countering opioid-induced respiratory depression. Br J Pharmacol. 2023;180:813–28. doi: 10.1111/bph.15580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garland EL, Froeliger B, Zeidan F, Partin K, Howard MO. The downward spiral of chronic pain, prescription opioid misuse, and addiction: cognitive, affective, and neuropsychopharmacologic pathways. Neurosci Biobehav Rev. 2013;37:2597–607. doi: 10.1016/j.neubiorev.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analyzed for this study.