Abstract
Fusobacterium nucleatum is a commensal pathogen typically found in the oral cavity, digestive tract, and urogenital system which has been associated with Lemierre’s syndrome, periodontal diseases, sinusitis, endocarditis, and intra-abdominal and brain abscesses. Our case is of a 62-year-old male who presented with headaches, nausea, and vision loss. Brain imaging identified a right occipito-parietal brain abscess. Following surgery and abscess drainage, Fusobacterium nucleatum was isolated from intraoperative cultures, and the infectious disease service was consulted for antibiotic recommendations. Additional history uncovered that he had also been experiencing night sweats, generalized weakness and 40-pound weight loss for 2 months, and had a prior history of colon polyps and diverticulitis. Furthermore, the patient disclosed having substandard oral hygiene practices, particularly in relation to the care of his dental appliances. Despite negative blood cultures, suspicion for hematogenous seeding was high. Imaging ruled out periodontal disease, but identified a colovesical fistula and liver abscesses, indicating potential translocation of bacteria via portal circulation to his liver. Echocardiogram workup revealed a 1-cm mobile vegetation on the aortic valve. His course was complicated by breakthrough seizures, renal failure, and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, and he ultimately completed 16 weeks of antibiotics. This case illustrates an uncommon presentation of brain abscess in an immunocompetent adult, with a prior episode of diverticulitis as the probable primary infection source, leading to development of a colovesical fistula and bacterial dissemination to the liver, heart, and brain. It highlights the importance of a comprehensive diagnostic approach, including consideration of atypical pathogens in immunocompetent adults.
Keywords: Fusobacterium nucleatum, F. nucleatum, brain abscess, liver abscess, infective endocarditis, gram-negative bacilli
Introduction
Fusobacteria are commensal pathogens, but in rare circumstances, they can lead to serious human infections including bacteremia, endocarditis, and brain abscesses. The 2 most isolated pathogens in this genus are Fusobacterium nucleatum (F nucleatum) and Fusobacterium necrophorum (F necrophorum). Fusobacterium nucleatum is an anaerobic, gram-negative bacilli that is commonly found in the oral cavity, digestive tract, upper respiratory tract, and urogenital system of humans. Fusobacterium has been associated with Lemierre’s syndrome, periodontal disease, sinusitis, pulmonary and gynecological infections, and intra-abdominal and brain abscesses. In adult patients, bacteremia with Fusobacterium spp. accounts for less than 1% of all bacteremia and less than 10% for all anaerobic bacteremia cases. 1 Most infections caused by F nucleatum occur in older patients with chronic medical conditions, whereas F necrophorum has been seen in younger immunocompetent individuals and classically linked to Lemierre’s syndrome.1,2 Although disseminated Fusobacterium infections advancing to the brain, liver, and other organs have been reported, they are not a common occurrence. 3
In 2007, Hseih et al 4 investigated 122 patients with culture-proven bacterial brain abscess in a retrospective study and discovered that Fusobacterium species accounted for only 6% (7/98) of monomicrobial cases and 17% (4/24) in polymicrobial cases. All 7 cases of brain abscess due to Fusobacterium survived (F nucleatum linked with 6 patients and F necrophorum linked with 1 patient) after receiving combination antimicrobial therapy and neurosurgical intervention with stereotactic aspiration. 4
Fusobacterium brain infections typically result from the hematogenous spread of bacteria from the oral cavity or upper respiratory tract or through direct extension from nearby structures such as teeth or sinuses.5,6 We present an unusual case of F nucleatum cerebral abscess, liver abscesses, and endocarditis in an immunocompetent adult.
Case Presentation
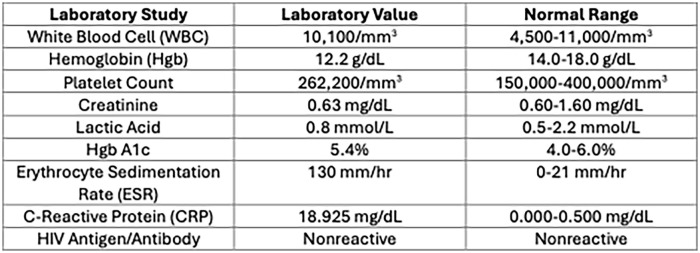
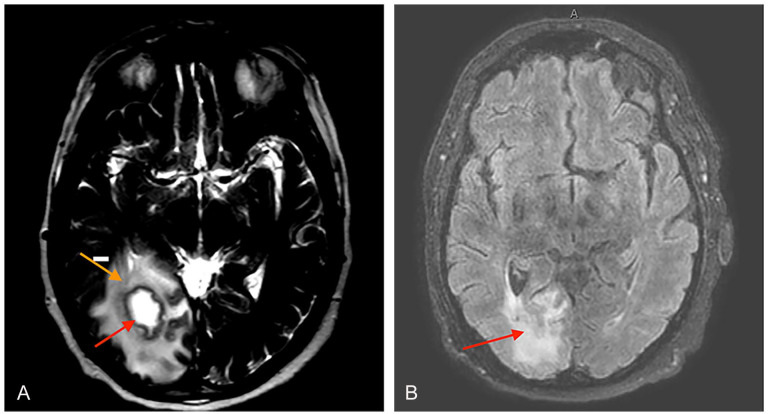
A 62-year-old male with a history of hypertension, paroxysmal atrial fibrillation on rivaroxaban, and obstructive sleep apnea on home continuous positive airway pressure (CPAP) presented to an outside hospital with frontal lobe headaches, left-sided vision loss, and nausea for 1 week. He also endorsed a 2-month history of fevers, night sweats, generalized weakness, and 40-pound weight loss. Computed tomography (CT) head showed a 2.4-cm right occipito-parietal mass which led to transfer to our hospital for urgent neurosurgical evaluation. On admission, initial vital signs were stable with temperature of 37.7°C, heart rate 92 bpm, blood pressure 131/86 mm Hg, and respiratory rate of 22 breaths/minute on room air. Lab tests were significant for a white blood cell (WBC) count of 10 100/mm3, hemoglobin of 12.2 g/dL, platelet count of 262 000/mm3, creatinine of 0.63 mg/dL, lactic acid of 0.8 mmol/L, Hgb A1c of 5.4%, erythrocyte sedimentation rate (ESR) of 130 mm/h, c-reactive protein (CRP) of 18.925 mg/dL, and HIV antigen/antibody nonreactive (Figure 1). Magnetic resonance imaging (MRI) brain confirmed a right parietal-occipital lobe abscess with vasogenic edema (Figure 2A). Levetiracetam was initiated for seizure prophylaxis and broad-spectrum antibiotics (vancomycin, ceftriaxone, and metronidazole) were started. The neurosurgery service performed a right parietal burr hole for stereotactic biopsy and drainage. His cerebral abscess cultures grew F nucleatum (Figure 3) and infectious disease (ID) service was consulted for antibiotic recommendations. The suspicion for hematogenous seeding remained high despite multiple negative blood cultures.
Figure 1.
Initial laboratory tests.
Figure 2.
(A) MRI brain with and without IV contrast showing a right parietal-occipatal lobe brain abscess (red arrow) with vasogenic edema (orange arrow). (B) MRI brain with and without IV contrast showing post-surgical changes and edema (red arrow) at the right parietal burr hole without evidence of residual right parietal-occipital brain abscess.
Figure 3.
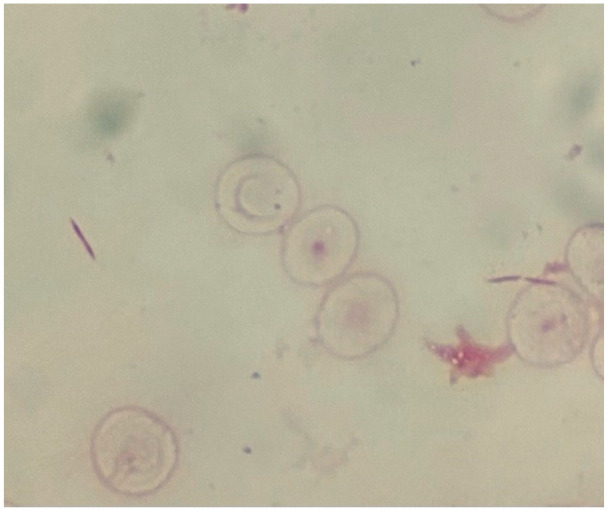
Gram stain from brain abscess showing thin fusiform gram-negative rods.
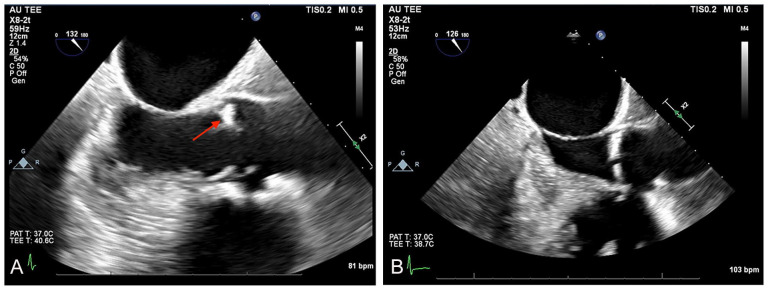
Given his night sweats and weight loss, additional imaging was obtained to rule out malignancy or other sites of infection. The CT scans of the chest, abdomen, and pelvis identified a colovesical fistula extending from the sigmoid colon into the bladder dome, an intramural bladder wall abscess (2 × 2.5 cm), and 2 focal liver lesions. General surgery and urology deferred surgical intervention in the absence of active gastrointestinal issues or voiding dysfunction and recommended outpatient follow-up with cystoscopy and colonoscopy. The MRI liver imaging confirmed 2 sizable intrahepatic abscesses, each 5 cm in size (Figure 4). An infective endocarditis workup was initiated, and a transthoracic echocardiogram (TTE) showed thickening of the noncoronary cusp on the aortic valve. Follow-up transesophageal echocardiogram (TEE) detected a 1-cm mobile vegetation on the aortic valve (Figure 5A). Interventional radiology (IR) performed CT-guided percutaneous drainage with multiple hepatic drain placements; however, all his liver abscess cultures remained negative. He was discharged home to complete a 6-week course of oral metronidazole 500 mg thrice daily and intravenous ceftriaxone 2 g twice daily to address his brain abscess, liver abscess, and aortic valve endocarditis.
Figure 4.
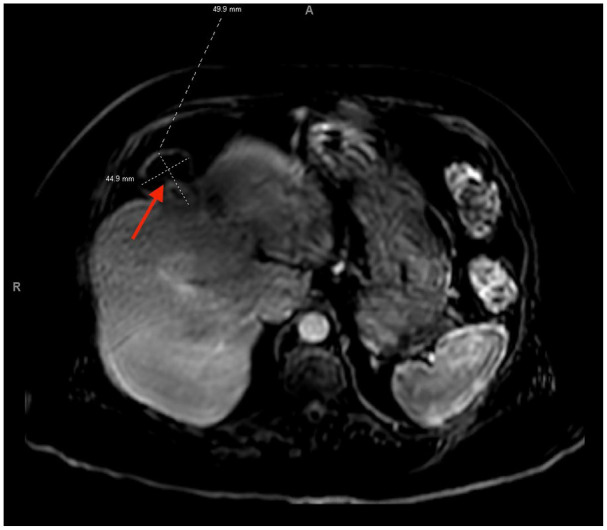
MRI liver shows a 5 × 5.5-cm subcapsular lesion in the anterosuperior subsegment of the right lobe (red arrow) and a 4.5 × 5-cm lesion in medial superior subsegment of the left lobe with an exophytic component and mild surrounding inflammation.
Figure 5.
(A) Transesophageal echocardiogram showing a 1 cm vegetation on the aortic valve (red arrow). (B) Repeat transesophageal echocardiogram showing resolution of aortic valve vegetation after antibiotic treatment.
One week later, the patient underwent an outpatient cystoscopy which confirmed a trabeculated bladder with 2 diverticula but showed no evidence of a communicating colovesical fistula. The IR performed a hepatic drainage catheter check and subsequent removal given his liver abscesses had substantially decreased in size on repeat CT imaging. He developed elevated hepatic transaminases of unknown etiology on his outpatient surveillance labs, and his antibiotics were briefly held for possible concern of drug-induced liver injury (DILI). Our patient’s liver enzymes improved, but he then developed acute renal failure with eosinophilia and a widespread maculopapular rash affecting his neck, trunk, and upper and lower extremities. He was readmitted 3 weeks later for further workup, and both Dermatology and Nephrology were contacted for further assistance. The Dermatology service suspected the patient had experienced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, so his antibiotics were stopped, and corticosteroids were initiated for treatment. His renal function and eosinophilia improved; repeat TEE and MRI of the brain performed 7 weeks after the beginning of antibiotic treatment showed completed radiographic resolution of his cerebral abscess and aortic valve vegetation (Figures 2B and 5B). Repeat CT abdomen and pelvis revealed a persistent fistulous tract extending from the sigmoid colon into the bladder dome with near resolution of his bladder wall abscess and decreased size of his hepatic abscesses. The patient restarted oral metronidazole while inpatient and continued on discharge given his persistent hepatic abscesses. He continued metronidazole for approximately 13 weeks until he ran out of refills and did not show up to his outpatient ID clinic appointment.
Unfortunately, the patient developed a seizure episode at home 4 days later after stopping his antiepileptic therapy for 2 weeks and was re-evaluated in the emergency department (ED). Initial CT brain in the ED showed no evidence of recurrent brain abscess, and he was restarted on levetiracetam for secondary seizure prophylaxis. However, he presented again to the ED 1 week later as a code stroke when he was found to be nonverbal with new left-sided weakness. The CT brain on admission revealed a ring-enhancing lesion in the subcortical occipital lobe, concerning early abscess reaccumulation (1.9 × 1.1 cm). The ID service restarted the patient on intravenous metronidazole pending further workup. Subsequent MRI of the brain confirmed his ring-enhancing right occipital lobe lesion with surrounding vasogenic edema. The neurosurgery service attempted another stereotactic biopsy and drainage but was unsuccessful in return of abscess fluid. The catheter was removed, and a small sample of brain tissue was sent for gram stain and culture. Both aerobic and anaerobic cultures remained negative from his intraoperative brain tissue and catheter. Brain tissue cytology ruled out malignancy, and broad-range 16S rRNA bacterial polymerase chain reaction (PCR) testing returned negative for any bacterial infection. His recurrent brain lesion was determined to be due to fibrinous scar tissue from his prior cerebral abscess, and his metronidazole was discontinued after receiving another 3-week course, completing a 16-week total duration of antibiotics.
Discussion
The incidence of brain abscesses is 0.3 to 0.9 per 100 000 population and usually occur in patients with predisposing risk factors such as severe immunocompromised conditions (malignancy, connective tissue disease, organ transplantation, use of immunomodulating therapies, and HIV/AIDS), dental infection and surgery, severe head trauma or neurosurgery, diabetes mellitus, alcohol abuse, and ear, nose, and throat infections.7,8 Fusobacterium nucleatum is a rare pathogen that can lead to intracerebral infections in humans; Fusobacterium species account for 6% of all reported brain abscesses. 4 Fusobacterium nucleatum cannot be isolated using aerobic conventional culture techniques and DNA sequencing assay along with broad-range 16S rRNA bacterial PCR testing can be necessary to diagnose this pathogen.3,9,10 In addition, the specimen collection method in anaerobic condition and the use of prior empirical antibiotics can affect the yield of identification of Fusobacterium by cultures.3,9,10
In 2003, Han et al 11 analyzed 5 patients with Fusobacterium brain abscesses and determined all individuals experienced an insidious onset along with hematogenous seeding. The 5 patients were all men between 45 and 74 years of age; 1 patient had a monomicrobial F necrophorum abscess, whereas the others had polymicrobial F nucleatum abscesses. 11 Fusobacterium nucleatum has been documented to be synergistic with other bacteria, mainly anaerobes, leading to an increased virulence and biofilm production in humans. 12 It is typically susceptible to penicillin, clindamycin, and metronidazole. 13 Most experts recommend a minimum 6-week duration for bacterial brain abscess in immunocompetent patients; however, no clinical studies exist to specifically address treatment duration for brain abscesses. 14
This case illustrates an uncommon presentation of brain and liver abscesses in an immunocompetent adult with colovesical fistula as the probable primary source of disseminated infection. After further interview, the patient admitted to heavy alcohol consumption in the distant past, but denied engaging in high-risk sexual behavior, smoking, or intravenous drug use. The patient had no recent travel history or sick contacts, and his age-appropriate cancer screenings were up to date. He disclosed his last colonoscopy was performed 5 years ago and a personal history of colon polyps and diverticulitis in the past. He initially denied any recent dental surgery or infection, but later disclosed poor oral hygiene with his dental appliances. Periodontal disease was ruled out with negative CT maxillofacial imaging. Fusobacterium nucleatum was diagnosed through stereotactic biopsy and cerebral abscess drainage by neurosurgery. Blood cultures and liver abscess cultures were negative, likely due to prolonged antibiotic exposure. We believe the patient’s prior episode of colonic diverticulitis led to development of a colovesical fistula and dissemination of bacteria to his liver, brain, and heart. His liver abscess likely occurred due to translocation of bacteria via the mesenteric veins to the portal circulation. His aortic valve vegetation and cerebral abscess were more likely secondary foci of infection related to bacteremia.
Our patient received combination therapy with metronidazole and ceftriaxone for 6 weeks to target his cerebral abscess due to F nucleatum given its high clinical association with polymicrobial infections. He had complete radiographic resolution of his aortic valve vegetation and cerebral abscess on repeat TEE and MRI brain imaging after completing his initial antibiotic course. Despite our patient developing probable drug-related complications with suspected DRESS syndrome and acute renal failure, metronidazole was continued as the drug of choice to treat his persistent F nucleatum hepatic abscess. His clinical workup was negative for urine eosinophils; however, both the nephrology and dermatology services believed ceftriaxone was the likely culprit for his renal and skin complications. His kidney function improved with intravenous (IV) fluids, cessation of ceftriaxone, and initiation of corticosteroids. During his last hospitalization, his abnormal brain imaging and concern for cerebral abscess reaccumulation was effectively excluded with negative broad-range 16S rRNA PCR testing from his brain tissue. He received more than adequate antimicrobial therapy with 6 weeks of IV ceftriaxone and 16 weeks of PO/IV metronidazole.
In conclusion, Fusobacterium is an emerging infectious pathogen causing invasive disease, which can be multifocal. Earlier recognition of brain abscesses caused by F nucleatum with prompt antibiotics and surgical drainage improves morbidity and mortality in all patients.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases.
Informed Consent: Verbal informed consent was obtained from the patient for their anonymized information to be published.
Prior Presentation of Abstract: This work was presented as a poster at the ACP Internal Medicine Meeting in Boston, MA, on April 19, 2024.
ORCID iDs: Zoheb Irshad Sulaiman  https://orcid.org/0009-0005-8366-0235
https://orcid.org/0009-0005-8366-0235
Divisha Sharma  https://orcid.org/0009-0003-3549-0548
https://orcid.org/0009-0003-3549-0548
References
- 1. Chaovarin C, Polpong P, Sungkhachat O. Fusobacterium nucleatum and brain abscess: case report and literature review. Interdiscip Neurosurg. 2021;24:101062. [Google Scholar]
- 2. Afra K, Laupland K, Leal J, et al. Incidence, risk factors, and outcomes of fusobacterium species bacteremia. BMC Infect Dis. 2013;13:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nohrström E, Mattila T, Pettilä V, et al. Clinical spectrum of bacteraemic fusobacterium infections: from septic shock to nosocomial bacteraemia. Scand J Infect Dis. 2011;43(6-7):463-470. [DOI] [PubMed] [Google Scholar]
- 4. Hsieh MJ, Chang WN, Lui CC, et al. Clinical characteristics of fusobacterial brain abscess. Jpn J Infect Dis. 2007;60(1):40-44. [PubMed] [Google Scholar]
- 5. Akashi M, Tanaka K, Kusumoto J, Furudoi S, Hosoda K, Komori T. Brain abscess potentially resulting from odontogenic focus: report of three cases and a literature review. J Maxillofac Oral Surg. 2017;16(1):58-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pereira AJDSPR, Tavares AT, Prates M, et al. Brain abscess: a rare clinical case with oral etiology. Case Rep Infect Dis. 2022;2022:5140259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess. Neurology. 2014;82:806-813. [DOI] [PubMed] [Google Scholar]
- 8. Bodilsen J, Dalager-Pedersen M, van de Beek D, et al. Risk factors for brain abscess: a nationwide, population-based, nested case-control study. Clin Infect Dis. 2020;71:1040-1046. [DOI] [PubMed] [Google Scholar]
- 9. Chen KP, Lee YP, Hwang MJ, Chiang CP. Fusobacterium nucleatum—caused brain abscess—case report. J Dent Sci. 2021;16(2):776-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chakvetadze C, Purcarea A, Pitsch A, Chelly J, Diamantis S. Detection of fusobacterium nucleatum in culture-negative brain abscess by broad-spectrum bacterial 16S rRNA gene PCR. Idcases. 2017;8:94-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Han XY, Weinberg JS, Prabhu SS, et al. Fusobacterial Brain Abscess: a review of five cases and an analysis of possible pathogenesis. J Neurosurg. 2003;99(4):693-700. [DOI] [PubMed] [Google Scholar]
- 12. Brook I, Walker RI. The relationship between fusobacterium species and other flora in mixed infection. J Med Microbiol. 1986;21(2):93-100. [DOI] [PubMed] [Google Scholar]
- 13. Denes E, Barraud O. Fusobacterium nucleatum infections: clinical spectrum and bacteriological features of 78 cases. Infection. 2016;44(4):475-481. [DOI] [PubMed] [Google Scholar]
- 14. Sonneville R, Ruimy R, Benzonana N, et al. An update on bacterial brain abscess in immunocompetent patients. Clin Microbiol Infect. 2017;23(9):614-620. [DOI] [PubMed] [Google Scholar]