Abstract
Background:
Arthroscopic treatment of femoroacetabular impingement has increased in popularity since the early 2000s when it was first described, although only a few midterm follow-up studies have been published.
Purpose:
To describe the outcomes of patients undergoing hip arthroscopy for femoroacetabular impingement at a mean 12-year follow-up and to determine the risk factors for failure.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
The Non-Arthritic Hip Score (NAHS) and a radiographic evaluation were completed preoperatively and at midterm follow-up. Participants were divided into 2 groups according to their clinical evolution. The success group consisted of patients whose NAHS at the final follow-up was above the established Patient Acceptable Symptom State (PASS) threshold of 81.9, whereas patients who underwent a second surgical intervention or did not reach the PASS threshold at final follow-up were assigned to the failure group. These groups were compared to identify preoperative differences in demographic, pathological, and surgical factors.
Results:
A total of 95 hips were included, after 23 were lost to follow-up (80.5% follow-up). At a mean follow-up of 12.1 years (range, 9.2-16.0 years), 9 hips required total hip arthroplasty (9.5%), 5 required revision hip arthroscopy (5.3%), 29 did not achieve the NAHS PASS threshold (30.5%), and 52 achieved the NAHS PASS threshold (54.7%). The mean NAHS was 82.4 at final follow-up compared with 66.9 preoperatively (mean difference = 15.5; P < .001). Higher mean body mass index (24.9 vs 23.0; P = .030), older age (30.0 vs 27.2; P = .035), and inferior preoperative lateral joint space width (3.9 vs 4.4; P = .019) were associated with inferior prognosis in the failure group versus success group. Osteoarthritis progression was observed in 69.2% of the failure group and in 34.8% of the success group (P = .082). Labral ossification was observed in 78.3% of all patients, and its lateral projection length was statistically associated with failure (P = .015).
Conclusion:
At a mean 12-year follow-up, hip arthroscopy for femoroacetabular impingement led to significant clinical improvement, with 55% PASS achievement. In total, 31% of patients were below the PASS threshold, 5% had revision arthroscopy, and only 9% had conversion to total hip arthroplasty for a 45% global failure rate. Increased body mass index, older age, and smaller preoperative lateral joint space width were significant negative prognostic factors. Postoperative degenerative changes were highly prevalent and demonstrated association with failure.
Keywords: hip arthroscopy, femoroacetabular impingement, labral repair, osteoarthritis
Femoroacetabular impingement (FAI) was described in 2003 by Ganz et al 25 as bony deformities of the femur and acetabulum that lead to abnormal contact between these structures. In patients who have FAI, repeated hip impingement leads to articular damage, including labral tears and chondral defects, and ultimately predisposes to osteoarthritis.1,5,25 The goals of surgical treatment are to alleviate the patient's symptoms in the short term and slow down degenerative changes in the midterm. Since its inception, arthroscopic treatment of FAI has demonstrated comparable outcomes to the open approach while presenting fewer complications 8 and has proven to be superior to physical therapy and nonoperative care alone. 28 However, data are lacking to assist clinicians in effectively managing patient expectations regarding their midterm prognosis.
In the past few years, several studies have successfully identified predictors of outcomes after hip arthroscopy for FAI. # A decrease in preoperative joint space width (JSW) to <2 mm, has been the most important risk factor reported for inferior patient-reported outcome measures (PROMs) and higher conversion rate to total hip arthroplasty (THA).40,45 Other well-established predictors associated with negative outcomes include advanced age, higher body mass index (BMI), and smoking.19,23 Patients who undergo labral repair have demonstrated superior outcomes compared with those who undergo debridement,31,33,37,43 whereas patients requiring microfracture tend to exhibit a higher risk of THA conversion. 19 Patients undergoing revision hip arthroscopy have presented significantly inferior PROMs compared with propensity-matched patients with primary procedures.12,38
The current evidence emanates from small sample studies with failure based only on conversion to THA. Evaluation of risk factors to illustrate postoperative health status reduction is still lacking. Postoperative labral ossification was identified as potentially related to failure after hip arthroscopy9,10; however, its effect and prevalence in the postoperative setting remain unexplored.
The objective of this study was to better understand the midterm clinical results after arthroscopic surgery for FAI. Additionally, this study aimed to identify risk factors associated with inferior outcomes.
Methods
Patient Selection
Ethics committee approval was obtained before the beginning of the study. Potential participants who underwent surgery between June 2006 and April 2013 were identified from the surgical list of a single surgeon.
This was a retrospective cohort study, where patients were prospectively recruited and followed for the initial 2 years, with an additional follow-up conducted at 9 to 16 years. Included patients had to present symptomatic FAI, treated exclusively through an arthroscopic approach. There was no age-related exclusion criterion, and all patients from the surgical list were between 16 to 40 years of age at the time of surgery, as this was an indication criterion at our institution. The clinical presentation had to meet the Warwick criteria for diagnosing FAI established in 2016 by research experts: (1) evidence of joint irritability in the hip manifested by the patient's symptomatic condition, (2) restriction of hip movement upon physical examination, and (3) anatomic parameters suggesting FAI on imaging studies. 27 Exclusion criteria consisted of preoperative Tönnis grade 2 or 3 osteoarthritis, collagen disorders, or any other hip-related pathology including, but not limited to, inflammatory, rheumatoid, and septic arthritis. Childhood deformities, congenital malformations, and posttraumatic sequelae were also excluded. Finally, patients for whom it was not possible to obtain any postoperative follow-up were excluded. Taking these criteria into consideration, we identified 118 potential participants.
Surgical Procedure
Every patient underwent hip arthroscopy in the supine position using a postdistractor set-up performed by the senior surgeon (E.L.B.). An interportal capsulotomy without closure and either labral debridement or repair, depending on the state of labral tissue at the time of surgery, were performed in all cases. Femoroplasty2,39 and acetabuloplasty were used to correct cam-type and pincer-type impingement, 15 respectively. Acetabular microfracture was performed to treat Outerbridge grade 4 defects. 50
Data Collection
Demographic data, along with participants’ medical and surgical history, were extracted from medical charts. Operative notes were also reviewed to collect the surgical procedure details and intraoperative findings.
Prospectively collected PROMs from the first 2 years of follow-up were retrospectively retrieved. Patients with bilateral procedures were asked to score each hip individually. The French version of the Non-Arthritic Hip Score (NAHS) was chosen a priori to assess hip pain, symptoms, and function, because this instrument has been shown to be the best quality questionnaire in hip arthroscopy.14,16,49 The NAHS consists of 20 questions scored on a scale of 0 to 4 for a maximum score of 80, which is reported on a scale of 100. In a previous study, the Patient Acceptable Symptom State (PASS) threshold for the NAHS was determined to be 81.9 at 5-year follow-up in patients undergoing hip arthroscopy for FAI. 44 The midterm evaluation was completed with an in-person clinical or remote follow-up, including PROMs and radiographs.
Preoperative and last follow-up radiographs of pelvic anteroposterior and Dunn 45° lateral views were analyzed by a blinded nontreating physician (GC). Patients who underwent THA or revision arthroscopy were included in the preoperative radiographic analysis but were excluded from the postoperative analysis. The alpha angle was measured to evaluate the femoral head-neck junction. An additional evaluation of the immediate postoperative alpha angle was conducted to assess the quality of the femoroplasty correction. Lateral center-edge angle and acetabular index were used to assess acetabular coverage. Acetabular retroversion was evaluated through the posterior wall sign, ischial spine sign, crossover sign, and retroversion index. Osteoarthritis was graded using the Tönnis scale (0 to 3), and JSW was measured at the lateral edge, middle, and medial edge of the sourcil.21,41,42,45 The anteroposterior pelvic radiograph was evaluated for the presence or absence of labral ossification; when present, labral ossification was measured from the lateral edge of the acetabulum to the most lateral point of the ossification.
To provide a global analysis of factors predicting an inferior prognosis, participants were divided into 2 groups according to successful or failed arthroscopy based on the 9- to 16-year follow-up. The success group consisted of patients whose NAHS was above the established PASS threshold of 81.9 at final follow-up. In contrast, patients who underwent a second surgical intervention or did not reach the PASS threshold value at the latest follow-up were assigned to the failure group. These groups were compared to identify preoperative differences in demographic, pathological, and surgical factors.
Statistical Analysis
Bivariate analyses were conducted to compare patient characteristics, radiographic variables, and operative procedural details between groups. Chi-square or Fisher tests were used for dichotomous variables, and Student t tests or Wilcoxon rank-sum tests were used for continuous variables. The alpha level was set at .05. Multivariate analysis was performed using logistic regression. Variables with P < .10 in the bivariate analysis were considered for inclusion in the model. Pearson correlation tests were then used to identify collinearity between eligible variables. The final selection was made based on clinical judgment and previously published data. This selection consisted of age, BMI, preoperative lateral JSW, postoperative alpha angle, and postoperative labral ossification length. A survival analysis based on reoperation (THA or revision hip arthroscopy) was conducted using the Kaplan-Meier method with Hall-Wellner 95% CI. Patients with missing data were excluded from the concerned variable analysis. SAS software Version 3.18 (SAS Institute) was used for all our statistical analysis.
Results
A total of 118 hips met the inclusion criteria. Among them, data for 95 hips (75 individual patients) were retrieved, and the patients agreed to participate in the study (80.5% follow-up, 20 bilateral surgeries). The remaining 23 hips were lost to follow-up due to outdated patient contact information (n = 15) or refusal to participate (n = 8). Recruitment and follow-up details are shown in Figure 1.
Figure 1.
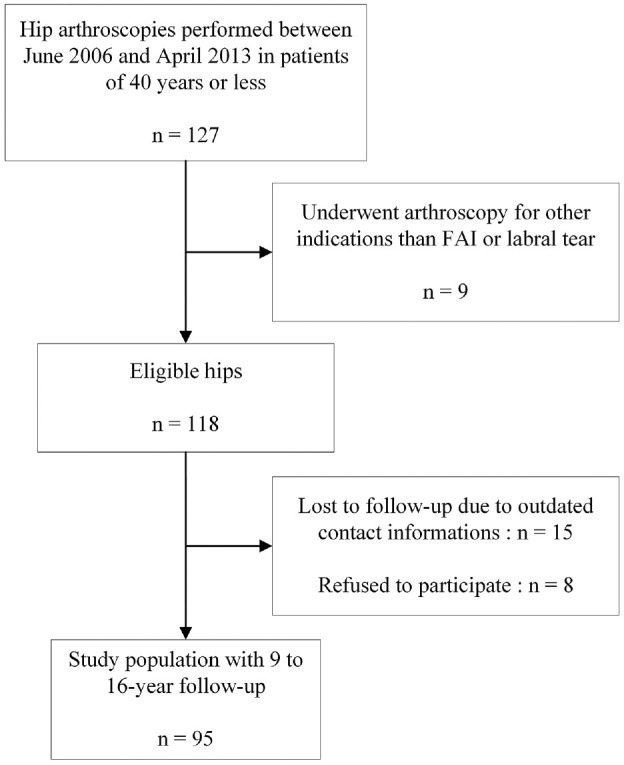
Flow diagram of patient recruitment. FAI, femoroacetabular impingement.
Among the recruited hips, 9 required conversion to THA (9.5%), 5 required revision hip arthroscopy (5.3%), 29 did not achieve NAHS PASS threshold value (30.5%), and 52 achieved the NAHS PASS threshold value (54.7%). Therefore, the success group consisted of 52 hips (54.7%), whereas the failure group consisted of 43 hips (45.3%). Recruited patients’ characteristics are shown in Table 1.
Table 1.
Patient Characteristics a
| Global (n = 95) | Success (n = 52) | Failure (n = 43) | P | |
|---|---|---|---|---|
| Age, y | 28.5 ± 6.7 (15.9-40.0) |
27.2 ± 6.6 (15.9-39.6) |
30.0 ± 6.4 (18.0-40.0) |
.035 |
| Body mass index b | 23.9 ± 3.8 (16.9-36.0) |
23.0 ± 3.3 (17.3-31.7) |
24.9 ± 4.2 (16.9-36.0) |
.030 |
| Sex | .304 | |||
| Male | 61 (64.2) | 31 (59.6) | 30 (69.8) | |
| Female | 34 (35.8) | 21 (40.4) | 13 (30.2) | |
| Smoking | 9 (9.5) | 7 (13.5) | 2 (4.7) | .177 |
| Bilateral | 41 (43.2) | 23 (44.2) | 17 (39.5) | .645 |
| Compensation | 10 (10.5) | 7 (13.5) | 3 (7.0) | .504 |
| Follow-up, y | 12.1 ± 1.9 (9.2-16.0) |
12.2 ± 1.9 (9.4-16.0) |
11.9 ± 1.9 (9.2-16.0) |
.539 |
Values are presented as mean ± SD (range) or n (%). Boldface P values indicate statistical significance.
nglobal = 80; nsuccess = 43; nfailure = 37.
The study population had a mean age of 28.5 years (range, 15.9-40.0 years) at the time of surgery with a mean BMI of 23.9 (range, 16.9-36.0), and 61 (64.2%) were male. Labral tears were repaired for 28 (29.5%) patients, and femoroplasty was the most common procedure, performed in 78 (82.1%) cases. Only 8 (8.4%) participants required microfracture. No statistically significant differences were found between groups regarding any surgical procedures (Table 2).
Table 2.
Surgical Procedures a
| Global (n = 95) | Success (n = 52) | Failure (n = 43) | P | |
|---|---|---|---|---|
| Labral treatment | .883 | |||
| Repair | 28 (29.5) | 15 (28.9) | 13 (30.2) | |
| Debridement | 67 (70.5) | 37 (71.2) | 30 (69.8) | |
| Acetabular microfracture | 8 (8.4) | 5 (9.6) | 3 (7.0) | .725 |
| Femoroplasty | 78 (82.1) | 41 (78.9) | 37 (86.1) | .362 |
| Acetabuloplasty | 28 (29.5) | 13 (25.0) | 15 (34.9) | .293 |
| Both osteoplasties | 24 (25.3) | 12 (23.1) | 12 (27.9) | .590 |
| No osteoplasty | 13 (13.7) | 10 (19.2) | 3 (7.0) | .133 |
Values are presented as n (%).
Patient-Reported Outcome Measures
For our entire patient population, NAHS improved from 66.9 ± 14.8 at the preoperative assessment to 82.4 ± 17.4 at the last follow-up (mean difference = 15.6, P < .001). No statistically significant difference was found in either preoperative or 1-year follow-up NAHS of patients in the success group compared with those in the failure group (Table 3).
Table 3.
Patient-Reported Outcome Measures a
| Global (n = 95) | Success (n = 52) | Failure (n = 43) | P | |
|---|---|---|---|---|
| NAHS preoperative b | 66.9 ± 14.8 (31.3 to 91.3) |
68.3 ± 14.5 (31.3 to 91.3) |
65.3 ± 15.1 (33.8 to 90.0) |
.350 |
| NAHS 1-year follow-up c | 85.6 ± 12.3 (33.8 to 100.0) |
87.1 ± 9.2 (63.8 to 100.0) |
83.5 ± 15.5 (33.8 to 100.0) |
.259 |
| NAHS last follow-up d | 82.4 ± 17.4 (33.8 to 100.0) |
93.1 ± 5.3 (82.5 to 100.0) |
63.2 ± 14.7 (33.8 to 81.3) |
<.001 |
| Change in NAHS at last follow-up from | ||||
| Preoperative e | 15.6 ± 21.4 (–47.5 to 68.8) |
25.3 ± 15.3 (–1.3 to 68.8) |
−0.3 ± 20.7 (–47.5 to 27.5) |
<.001 |
| 1-year follow-up f | −1.4 ± 16.8 (–48.8 to 35.0) |
6.2 ± 9.5 (–15.0 to 35.0) |
−16.1 ± 18.3 (–48.8 to 22.5) |
<.001 |
Values are presented as mean ± SD (range). Boldface P values indicate statistical significance. NAHS, Non-Arthritic Hip Score.
nglobal = 81, nsuccess = 43, nfailure = 38.
nglobal = 71, nsuccess = 41, nfailure = 30.
nglobal = 81, nsuccess = 52, nFailure = 29.
nglobal = 69, nsuccess = 43, nfailure = 26.
nglobal = 62, nsuccess = 41, nfailure = 21.
Radiographic Findings
Preoperative and postoperative radiographic analyses included 50 and 69 patients, respectively. Among preoperative radiographic parameters, increased lateral JSW showed the only statistically significant association with successful midterm evolution (mean ± SD, 4.4 ± 0.6 vs 3.9 ± 0.9 mm; P = .019) with a global range of 2.5 to 5.6 mm (Table 4). No statistically significant associations were found with Tönnis grade, labral ossification, alpha angles, acetabular coverage, or retroversion (Table 4).
Table 4.
Preoperative Radiographic Findings a
| Global (n = 50) | Success (n = 28) | Failure (n = 22) | P | |
|---|---|---|---|---|
| Tönnis grade | .063 | |||
| 0 | 30 (60.0) | 20 (71.4) | 10 (45.5) | |
| 1 | 20 (40.0) | 8 (28.6) | 12 (54.6) | |
| JSW, mm | ||||
| Lateral | 4.2 ± 0.8 (2.5 to 5.6) |
4.4 ± 0.6 (3.1 to 5.6) |
3.9 ± 0.9 (2.5 to 5.6) |
.019 |
| Middle | 4.1 ± 0.7 (2.3 to 5.6) |
4.3 ± 0.6 (3.0 to 5.5) |
3.9 ± 0.8 (2.3 to 5.6) |
.053 |
| Medial | 4.1 ± 0.9 (2.5 to 6.1) |
4.1 ± 0.8 (2.8 to 6.1) |
4.1 ± 0.9 (2.5 to 5.9) |
.902 |
| Minimum | 3.7 ± 0.7 (2.3 to 5.5) |
3.8 ± 0.7 (2.8 to 5.5) |
3.5 ± 0.7 (2.3 to 5.0) |
.097 |
| Labral ossification | 34 (68.0) | 16 (57.1) | 18 (81.8) | .076 |
| Ossification length, mm | 2.2 ± 2.1 (0.0 to 7.7) |
2.0 ± 2.3 (0.0 to 7.7) |
2.4 ± 1.7 (0.0 to 5.9) |
.460 |
| Alpha angle, deg | 70.9 ± 15.1 (39.0 to 98.2) |
67.6 ± 14.5 (39.0 to 87.0) |
75.1 ± 15.1 (42.0 to 98.2) |
.083 |
| Corrected alpha angle, deg | 55.5 ± 15.5 (35.8 to 88.0) |
52.0 ± 11.7 (38.6 to 82.1) |
58.9 ± 17.9 (35.8 to 88.0) |
.085 |
| LCEA, deg | 27.7 ± 7.7 (14.0 to 53.0) |
27.6 ± 6.5 (14.0 to 39.0) |
27.9 ± 9.1 (15.2 to 53.0) |
.865 |
| AI, deg | 6.4 ± 5.7 (–9.4 to 19.2) |
6.3 ± 5.5 (–5.2 to 19.2) |
6.5 ± 6.0 (–9.4 to 15.6) |
.914 |
| Retroversion index | 0.1 ± 0.1 (0.0 to 0.7) |
0.1 ± 0.2 (0.0 to 0.7) |
0.1 ± 0.1 (0.0 to 0.3) |
.786 |
| Crossover sign | 17 (34.0) | 8 (28.6) | 9 (40.9) | .361 |
| Posterior wall sign | 26 (52.0) | 14 (50.0) | 12 (54.6) | .750 |
| Ischial spine sign | 9 (18.0) | 5 (17.9) | 4 (18.2) | .976 |
Values are presented as mean ± SD (range) or n (%). Boldface P values indicate statistical significance. AI, acetabular index; JSW, joint space width; LCEA, lateral center-edge angle.
At the last follow-up, statistically significant associations were found between clinical success and Tönnis grade; lateral, middle, and minimum JSW; lateral projection length of labral ossification; and alpha angle. All patients in the success group presented few (Tönnis grade 1, 59.1%) or no signs of osteoarthritis (Tönnis grade 0, 40.9%), whereas only 56.0% of patients in the failure group had Tönnis grade 0 (16.0%) or 1 (40.0%) (P < .001). Osteoarthritis progression was observed in 47.2% of patients. Labral ossification was detected in 70.5% of the success group and 92.0% of the failure group (P = .066), and its mean lateral projection length was significantly higher in the failure group (P = .015). We noted no association with medial JSW, acetabular coverage, or retroversion (Table 5).
Table 5.
Postoperative Radiographic Findings at Last Follow-up a
| Global (n = 69) | Success (n = 44) | Failure (n = 25) | P | |
|---|---|---|---|---|
| Tönnis grade | <.001 | |||
| 0 | 22 (31.9) | 18 (40.9) | 4 (16.0) | |
| 1 | 36 (52.2) | 26 (59.1) | 10 (40.0) | |
| 2 | 10 (14.5) | 00 (0.0) | 10 (40.0) | |
| 3 | 1 (1.5) | 00 (0.0) | 1 (4.0) | |
| JSW, mm | ||||
| Lateral | 3.6 ± 1.0 (0.0 to 5.6) |
3.9 ± 0.7 (2.6 to 5.4) |
3.1 ± 1.2 (0.0 to 5.6) |
.003 |
| Middle | 4.1 ± 1.0 (0.0 to 7.2) |
4.4 ± 0.8 (2.6 to 7.2) |
3.7 ± 1.3 (0.0 to 5.9) |
.023 |
| Medial | 4.1 ± 0.9 (1.5 to 6.0) |
4.1 ± 0.9 (2.6 to 6.0) |
4.2 ± 1.0 (1.5 to 6.0) |
.664 |
| Minimum | 3.3 ± 0.9 (0.0 to 5.6) |
3.6 ± 0.6 (2.6 to 5.1) |
2.8 ± 1.1 (0.0 to 5.6) |
.005 |
| Osteoarthritis progression b | 17 (47.2) | 8 (34.8) | 9 (69.2) | .082 |
| Labral ossification | 54 (78.3) | 31 (70.5) | 23 (92.0) | .066 |
| Ossification length, mm | 4.3 ± 3.6 (0.0 to 14.1) |
3.5 ± 3.4 (0.0 to 14.1) |
5.6 ± 3.6 (0.0 to 13.1) |
.015 |
| Alpha angle, deg | 62.5 ± 16.5 (33.9 to 89.2) |
58.8 ± 15.9 (33.9 to 85.3) |
69.1 ± 15.5 (43.8 to 89.2) |
.011 |
| LCEA, deg | 29.5 ± 8.0 (13.0 to 52.0) |
29.2 ± 7.7 (13.4 to 43.1) |
29.9 ± 8.6 (13.0 to 52.0) |
.720 |
| AI, deg | 7.0 ± 7.7 (–4.2 to 49.9) |
5.9 ± 6.2 (–4.2 to 25.7) |
9.0 ± 9.7 (–2.9 to 49.9) |
.160 |
| Retroversion-index | 0.1 ± 0.1 (0.0 to 0.7) |
0.1 ± 0.1 (0.0 to 0.7) |
0.1 ± 0.1 (0.0 to 0.6) |
.559 |
| Crossover sign | 24 (34.8) | 17 (38.6) | 7 (28.0) | .373 |
| Posterior wall sign | 31 (44.9) | 21 (47.7) | 10 (40.0) | .535 |
| Ischial spine sign | 18 (26.1) | 13 (29.6) | 5 (20.0) | .385 |
Values are presented as mean ± SD (range) or n (%). Boldface P values indicate statistical significance. AI, acetabular index; JSW, joint space width; LCEA, lateral center-edge angle.
nglobal = 36, nsuccess = 23, nfailure = 13.
Multivariate Analysis
Increased preoperative lateral JSW maintained a statistically significant association with successful midterm evolution (odds ratio = 6.7; 95% CI, 1.3-54.5; P = .040) when adjusted for age, BMI, postoperative alpha angle, and postoperative labral ossification length. This means that the odds of not requiring secondary surgery and of exceeding the PASS threshold for the NAHS at a mean 12-year follow-up were 6.7 times higher with every supplemental 1 mm of preoperative lateral JSW. Other variables included were not statistically associated with midterm outcomes after adjustment for covariates (P > .05).
Survival Analysis
Our Kaplan-Meier analysis produced the survival plot seen in Figure 2. At 16 years, the rate of survival without reoperation was estimated at 82.1%.
Figure 2.

Kaplan-Meier plot of survival without reoperation after hip arthroscopy for femoroacetabular impingement (FAI).
Discussion
This study aimed to provide a portrait of patients undergoing hip arthroscopy for FAI at up to 16 years of follow-up. In addition, preoperative risk factors and midterm postoperative degenerative changes were investigated. The overall analysis of our study participants showed that 85% did not need secondary surgery after a mean follow-up of 12 years, and 55% had successful outcomes, exceeding the NAHS PASS threshold. None of the concomitant surgical procedures performed during hip arthroscopy showed statistically significant associations with the midterm success of the procedure. BMI, age, and preoperative lateral JSW were identified as significant risk factors for secondary surgery and inferior PASS achievement, but only preoperative lateral JSW maintained its statistical association in the multivariate analysis. Moreover, our postoperative radiographic analysis indicated that degenerative articular changes were significantly associated with failure.
The 9% THA conversion rate observed in our study is consistent with previously reported findings.11,17,51 In 2017, Menge et al 36 demonstrated that patients undergoing arthroscopic correction of FAI achieved satisfactory functional outcomes, with a subsequent conversion rate to THA of 34% at 10 years, regardless of labral treatment. However, those investigators did not exclude patients who had advanced preoperative osteoarthritis, and the mean age of their population was 41 years. Similarly, Zimmerer et al 51 conducted a 10-year follow-up study revealing that patients who had preoperative Tönnis grade 2 changes had a significantly poorer prognosis, with a conversion rate to THA reaching 54%, compared with only 14% for those with preoperative Tönnis grade 1 or 0 changes. In 2022, Carton et al 11 presented a 10-year follow-up case series of patients undergoing arthroscopic correction of FAI excluding preoperative Tönnis grade 2 or 3. Those investigators found an 8.4% THA conversion rate and 5.9% revision hip arthroscopy rate, with 62% of remaining patients achieving the PASS threshold for the modified Harris Hip Score questionnaire. However, the PASS achievement rate could be different when the NAHS is used instead. In the most recent study, conducted by Domb et al, 17 who assessed the midterm outcomes of hip arthroscopy in athletes with FAI, the incidence of THA was 14.3%, whereas the rate of revision hip arthroscopy was 10.6%. Additionally, those investigators showed a longer time to conversion to THA when labral repair was performed instead of debridement. We showed a similarly low THA conversion rate after arthroscopy for FAI in the midterm (8%-15%), despite the fact that many patients underwent labral debridement and no capsular closure given the practice patterns at the time.
The relevance of capsular repair after interportal capsulotomy for hip arthroscopy has long been debated. During our inclusion period, data regarding management of the capsule were scarce, relying mostly on expert opinions insisting more on the importance of visualization than ligament preservation.6,26 Between 2018 and 2023, studies focusing specifically on capsular management emerged. In the short-term (≤2 years), benefits from closure remain unclear, with comparable improvement seen in high-quality studies including randomized controlled trials.4,18,22,24 However, at 5-year follow-up, Domb et al 18 found a significant difference in THA conversion rates favoring repair along with a decrease in PROMs from 2 to 5-year follow-up observed only in the group whose capsule was left unrepaired. Similarly, Bolia et al 7 showed decreased THA conversion rates and superior PROMs with capsular repair at 5-year follow-up of hip arthroscopy. In 2023, Kaplan et al 30 published a systematic review including only follow-ups of ≥5 years in order to compare studies performing closure versus those that did not. Those investigators demonstrated lower revision rates with repair but no significant difference in THA conversion rates or PROMs between these 2 subgroups. That being said, comparative cohort studies might be more reliable to avoid bias relating to interstudy differences. Therefore, it is possible that better results would have been obtained had capsular closure been performed in our cohort, but further mid- to long-term comparative studies are needed to clarify this topic.
In our cohort, preoperative and 1-year follow-up NAHS did not exhibit a statistically significant association with midterm clinical success. At the last follow-up, patients in the success group demonstrated a substantial and sustained improvement from baseline, whereas the failure group tended to revert to their baseline levels after a brief, comparable, initial improvement at 1 year after surgery. This pattern has not previously been described and highlights the importance of appropriate patient counseling that postoperative clinical improvement may not be directly proportional to early clinical evolution or the patient's preoperative state. As our postoperative radiographic analysis pointed out, multiple degenerative changes are associated with poorer prognosis and could be the main cause for deterioration after arthroscopy for FAI. In our study, almost half of the failure group (44%) had postoperative Tönnis grade 2 or 3 changes at the last follow-up compared with none of the patients in the success group. Participants in the failure group also had a higher rate of osteoarthritis progression compared with the success group (69% vs 35%, respectively; P = .082). This result is higher than previously reported by Husen et al, 29 who found a global 27% rate of osteoarthritis progression at a mean 10.6 years of follow-up. This discrepancy could be attributed to a shorter minimum follow-up time in their study (5 years) and the inclusion of younger patients (minimum 12.5 years old). Considering the high prevalence of osteoarthritis progression and its effect on postoperative symptomatic state demonstrated in this study, the benefits of osteoarthritic prevention therapies as adjuvants for arthroscopic correction of FAI could be worth investigating. Furthermore, we showed that preoperative lateral JSW was the most critical risk factor for poorer prognosis and remained statistically significant after adjustment for confounding variables, even though we did not have any patients with values <2 mm. This finding highlights the importance of assessing the JSW as a continuous variable rather than using the 2-mm cutoff only, as Ruzbarsky et al 45 indicated in their recent study. Moreover, these findings could help better inform patients of their risk of longer term hip osteoarthritic changes.
As for management of labral tears, repair did not show superiority to debridement in our cohort. Similarly, most studies evaluating midterm outcomes after arthroscopy for FAI have failed to show differences in outcomes between the 2 techniques11,17,36 other than a longer time to conversion to THA after repair. 17 However, this factor is difficult to assess without controlling for other variables due to indication bias related to the state of labral tissue and its close relation with articular degenerative changes. This said, studies that have specifically compared both procedures have observed better results after labral repair compared with debridement.31,33,37,43 Our proportion of labral debridement was 70%, which is considerably higher than previous long-term studies, which reported 30% to 35%.11,17 This is probably due to the inclusion period of our study starting from 2006, when this procedure was more commonly performed as opposed to other studies beginning in 2008.11,17 In their matched-pair study, Chen et al 13 demonstrated that small and stable labral tears with enough remaining tissue to preserve the suction-seal were good candidates to undergo debridement and showed comparable results to a labral repair control group. Therefore, variability in patient selection and indications for repair in different studies might explain the discrepancies in clinical results observed. In our study, although labral repair was considered the gold standard in most cases, selective debridement showed good and sustained clinical results in the midterm and did not appear to be a negative prognostic factor.
In most previously published studies, requirement for microfracture has been identified as a risk factor for inferior results after arthroscopy for FAI.3,19,36 When analyzing a cohort of 1038 participants, Domb et al 19 found that patients undergoing this procedure had significantly inferior postoperative NAHS. However, their population had a mean age of 36 years with a range of 13.2 to 76.4 years. In our study, patients with Outerbridge grade 4 chondral defects treated with microfracture were not more likely to be in the failure group. In their recent study, Westermann et al 50 demonstrated that microfracture in patients younger than 35 years obtained good clinical results without significant risk of THA conversion. The relatively young population of our study combined with the low number of microfractures might explain this result, which aligns with the findings of Westermann et al.
Postoperative labral ossification has not been reported in previous studies. However, Byrd et al 9 assessed its effect in the preoperative setting. They found that patients with pincer FAI caused by labral ossification had worse symptoms, which increased with the age of presentation, suggesting a more progressive disease compared with controls who had pincer-type FAI of other causes. Their labral ossification cohort was also older and had proportionately more female patients than the control group, with similar improvement after arthroscopic treatment. 9 In our study, we found that 78.26% of patients presented at least a partially ossified labrum after surgery, which is more prevalent than expected. Patients in the failure group were more prone to develop ossified labrum (92%) than those in the success group (70.5%; P = .066) and had significantly more extensive ossifications (mean, 5.64 vs 3.50 mm; P = .015). This condition may contribute to ongoing painful impingement and worse clinical outcomes after hip arthroscopy. More research is needed to better define the different types of postoperative labral ossifications and determine which are more likely to be symptomatic.
Limitations
This study had some limitations. First, all surgeries were performed by a single surgeon at a tertiary referral center, which could limit the generalizability of our findings considering that the outcomes are inextricably related to the quality of the surgical procedure. However, this removes the risk of intersurgeon variability that may bias the results of a study relying on multiple surgeons. Second, this was a retrospective study, making it challenging to retrieve all intended data from >9 years ago and to achieve sufficient follow-up rate. Radiographs from 2008 and before were not registered in our picture archiving and communication system, limiting the sample size for our radiographic analysis. Third, the NAHS PASS threshold we used was obtained from a cohort with shorter follow-up and may not correspond to the same level of clinical success in our patient population. As such, we may have possibly underestimated the true rate of patients who obtained a satisfactory functional outcome given their ages and levels of activity.
Conclusion
After 9 to 16 years of follow-up, patients undergoing arthroscopy for FAI maintained a significant clinical improvement with a 55% successful PASS achievement. We found that 31% of patients were below the PASS threshold, 5% had revision arthroscopy, and 9% had conversion to THA, for a 45% global failure rate. Increased BMI, older age, and inferior preoperative lateral JSW were significant negative prognostic factors. Postoperative degenerative changes were highly prevalent and demonstrated association with failure.
Acknowledgments
We thank Sylvie Turmel for her invaluable help with patient recruitment and follow-up evaluations.
Footnotes
Submitted February 2, 2024; accepted June 3, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.D. has received research support from SOFCOT. B.A.M. has received speaking fees from Arthrex and Pendopharm. E.L.B. is on the advisory board of Pendopharm and Bodycad; has received speaking fees from Pendopharm, Sanofi, Stryker, Smith + Nephew, and ConMed; and has received royalties from Bodycad. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
ORCID iD: Gabriel Champagne  https://orcid.org/0000-0003-4197-6467
https://orcid.org/0000-0003-4197-6467
References
- 1. Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918-923. doi: 10.1136/annrheumdis-2012-201643 [DOI] [PubMed] [Google Scholar]
- 2. Ayeni OR, Karlsson J, Heels-Ansdell D, et al. Osteochondroplasty and labral repair for the treatment of young adults with femoroacetabular impingement: a randomized controlled trial. Am J Sports Med. 2021;49(1):25-34. doi: 10.1177/0363546520952804 [DOI] [PubMed] [Google Scholar]
- 3. Beals TR, Soares RW, Briggs KK, Day HK, Philippon MJ. Ten-year outcomes after hip arthroscopy in patients with femoroacetabular impingement and borderline dysplasia. Am J Sports Med. 2022;50(3):739-745. doi: 10.1177/03635465211068109 [DOI] [PubMed] [Google Scholar]
- 4. Bech NH, Sierevelt IN, de Waard S, Joling BSH, Kerkhoffs G, Haverkamp D. Capsular closure versus unrepaired interportal capsulotomy after hip arthroscopy in patients with femoroacetabular impingement: results of a patient-blinded randomised controlled trial. Hip Int. 2023;33(1):94-101. doi: 10.1177/11207000211005762 [DOI] [PubMed] [Google Scholar]
- 5. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012-1018. doi: 10.1302/0301-620x.87b7.15203 [DOI] [PubMed] [Google Scholar]
- 6. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011;27(12):1720-1731. doi: 10.1016/j.arthro.2011.08.288 [DOI] [PubMed] [Google Scholar]
- 7. Bolia IK, Fagotti L, Briggs KK, Philippon MJ. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthroscopy. 2019;35(6):1828-1834. doi: 10.1016/j.arthro.2019.01.033 [DOI] [PubMed] [Google Scholar]
- 8. Botser IB, Smith TW, Jr, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27(2):270-278. doi: 10.1016/j.arthro.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 9. Byrd JW, Jones KS, Freeman CR. Surgical outcome of pincer femoroacetabular impingement with and without labral ossification. Arthroscopy. 2016;32(6):1022-1029. doi: 10.1016/j.arthro.2015.12.042 [DOI] [PubMed] [Google Scholar]
- 10. Carreira DS, Shaw DB, Wolff AB, et al. Labral degeneration predicts inferior mid-term outcomes in hip labral repair: a multicenter comparative analysis. Arthroscopy. 2022;38(9):2661-2668. doi: 10.1016/j.arthro.2022.02.019 [DOI] [PubMed] [Google Scholar]
- 11. Carton P, Filan D, Mullins K. Survivorship rate and clinical outcomes 10 years after arthroscopic correction of symptomatic femoroacetabular impingement. Am J Sports Med. 2022;50(1):19-29. doi: 10.1177/03635465211055485 [DOI] [PubMed] [Google Scholar]
- 12. Chapman R, Horner N, Ziauddin L, Hevesi M, Nho SJ. Patients undergoing revision hip arthroscopy demonstrate comparable survivability and improvement but worse postoperative outcomes compared to patients undergoing primary hip arthroscopy: a propensity matched study at five-year follow-up. Arthroscopy. 2024;40(3):802-809. doi: 10.1016/j.arthro.2023.07.047 [DOI] [PubMed] [Google Scholar]
- 13. Chen AW, Yuen LC, Ortiz-Declet V, Litrenta J, Maldonado DR, Domb BG. Selective debridement with labral preservation using narrow indications in the hip: minimum 5-year outcomes with a matched-pair labral repair control group. Am J Sports Med. 2018;46(2):297-304. doi: 10.1177/0363546517739566 [DOI] [PubMed] [Google Scholar]
- 14. Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75-83. doi: 10.1097/01.blo.0000043047.84315.4b [DOI] [PubMed] [Google Scholar]
- 15. Cohen D, Khan A, Kay J, et al. There is no definite consensus on the adequate radiographic correction in arthroscopic osteochondroplasty for femoroacetabular impingement: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):2799-2818. doi: 10.1007/s00167-021-06645-1 [DOI] [PubMed] [Google Scholar]
- 16. Dartus J, Putman S, Champagne G, Matache BA, Pelet S, Belzile EL. Validation of the French version of the Non-Arthritic Hip Score (NAHS) in 113 hip arthroscopy procedures. Orthop Traumatol Surg Res. 2023;109(7):103683. doi: 10.1016/j.otsr.2023.103683 [DOI] [PubMed] [Google Scholar]
- 17. Domb BG, Annin S, Monahan PF, Lee MS, Jimenez AE, Maldonado DR. Ten-year survivorship, outcomes, and sports participation in athletes after primary hip arthroscopy for femoroacetabular impingement syndrome. Am J Sports Med. 2023;51(9):2383-2395. doi: 10.1177/03635465231180305 [DOI] [PubMed] [Google Scholar]
- 18. Domb BG, Chaharbakhshi EO, Perets I, Walsh JP, Yuen LC, Ashberg LJ. Patient-reported outcomes of capsular repair versus capsulotomy in patients undergoing hip arthroscopy: minimum 5-year follow-up-a matched comparison study. Arthroscopy. 2018;34(3):853-863.e1. doi: 10.1016/j.arthro.2017.10.019 [DOI] [PubMed] [Google Scholar]
- 19. Domb BG, Chen SL, Go CC, et al. Predictors of clinical outcomes after hip arthroscopy: 5-year follow-up analysis of 1038 patients. Am J Sports Med. 2021;49(1):112-120. doi: 10.1177/0363546520968896 [DOI] [PubMed] [Google Scholar]
- 20. Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Revision hip preservation surgery with hip arthroscopy: clinical outcomes. Arthroscopy. 2014;30(5):581-587. doi: 10.1016/j.arthro.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 21. Dougados M. Monitoring osteoarthritis progression and therapy. Osteoarthritis Cartilage. 2004;12(suppl A):S55-S60. doi: 10.1016/j.joca.2003.09.009 [DOI] [PubMed] [Google Scholar]
- 22. Economopoulos KJ, Chhabra A, Kweon C. Prospective randomized comparison of capsular management techniques during hip arthroscopy. Am J Sports Med. 2020;48(2):395-402. doi: 10.1177/0363546519894301 [DOI] [PubMed] [Google Scholar]
- 23. Emara AK, Grits D, Samuel LT, Acuña AJ, Rosneck JT, Kamath AF. Hip arthroscopy in smokers: a systematic review of patient-reported outcomes and complications in 18,585 cases. Am J Sports Med. 2021;49(4):1101-1108. doi: 10.1177/0363546520922854 [DOI] [PubMed] [Google Scholar]
- 24. Filan D, Carton P. Routine interportal capsular repair does not lead to superior clinical outcome following arthroscopic femoroacetabular impingement correction with labral repair. Arthroscopy. 2020;36(5):1323-1334. doi: 10.1016/j.arthro.2019.12.002 [DOI] [PubMed] [Google Scholar]
- 25. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. doi: 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 26. Gédouin JE. Arthroscopic treatment of femoroacetabular impingement: technical review. Orthop Traumatol Surg Res. 2012;98(5):583-596. doi: 10.1016/j.otsr.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 27. Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169-1176. doi: 10.1136/bjsports-2016-096743 [DOI] [PubMed] [Google Scholar]
- 28. Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225-2235. doi: 10.1016/s0140-6736(18)31202-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Husen M, Leland DP, Melugin HP, et al. Progression of osteoarthritis at long-term follow-up in patients treated for symptomatic femoroacetabular impingement with hip arthroscopy compared with nonsurgically treated patients. Am J Sports Med. 2023;51(11):2986-2995. doi: 10.1177/03635465231188114 [DOI] [PubMed] [Google Scholar]
- 30. Kaplan DJ, Fenn TW, Jan K, Nho SJ. Capsular repair is associated with lower revision rates yet similar clinical outcomes and arthroplasty conversion 5 years after hip arthroscopy: a systematic review. Arthroscopy. 2023;39(8):1882-1891.e1. doi: 10.1016/j.arthro.2023.04.016 [DOI] [PubMed] [Google Scholar]
- 31. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46-53. doi: 10.1016/j.arthro.2012.07.011 [DOI] [PubMed] [Google Scholar]
- 32. Kyin C, Maldonado DR, Go CC, Shapira J, Lall AC, Domb BG. Mid- to long-term outcomes of hip arthroscopy: a systematic review. Arthroscopy. 2021;37(3):1011-1025. doi: 10.1016/j.arthro.2020.10.001 [DOI] [PubMed] [Google Scholar]
- 33. Larson CM, Dean RS, McGaver RS, Seiffert KJ, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: updated mean 7-year follow-up. Am J Sports Med. 2022;50(3):731-738. doi: 10.1177/03635465211067818 [DOI] [PubMed] [Google Scholar]
- 34. Maerz T, Nepple JJ, Bedi A, et al. Sex differences in clinical outcomes following surgical treatment of femoroacetabular impingement. J Bone Joint Surg Am. 2021;103(5):415-423. doi: 10.2106/jbjs.20.00394 [DOI] [PubMed] [Google Scholar]
- 35. Mas Martinez J, Verdu-Roman C, Bustamante Suarez de Puga D, Morales Santias M, Martinez Gimenez E, Sanz-Reig J. Arthroscopic surgery for femoroacetabular impingement has limited effect in patients with Tönnis grade-2 at 4-year follow-up. Arch Orthop Trauma Surg. 2022;142(10):2801-2809. doi: 10.1007/s00402-021-04249-5 [DOI] [PubMed] [Google Scholar]
- 36. Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am. 2017;99(12):997-1004. doi: 10.2106/jbjs.16.01060 [DOI] [PubMed] [Google Scholar]
- 37. Migliorini F, Maffulli N, Baroncini A, Eschweiler J, Tingart M, Betsch M. Revision surgery and progression to total hip arthroplasty after surgical correction of femoroacetabular impingement: a systematic review. Am J Sports Med. 2022;50(4):1146-1156. doi: 10.1177/03635465211011744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Monahan PF, Jimenez AE, Owens JS, et al. Revision hip arthroscopy in high-level athletes: minimum 2-year outcomes comparison to a propensity-matched primary hip arthroscopy control group. Am J Sports Med. 2021;49(13):3582-3591. doi: 10.1177/03635465211041760 [DOI] [PubMed] [Google Scholar]
- 39. Nepple JJ, Parilla FW, Ince DC, Freiman S, Clohisy JC. Does femoral osteoplasty improve long-term clinical outcomes and survivorship of hip arthroscopy? A 15-year minimum follow-up study. Am J Sports Med. 2022;50(13):3586-3592. doi: 10.1177/03635465221123048 [DOI] [PubMed] [Google Scholar]
- 40. Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013;471(8):2492-2496. doi: 10.1007/s11999-012-2779-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91(1):16-23. doi: 10.1302/0301-620x.91b1.21329 [DOI] [PubMed] [Google Scholar]
- 42. Ratzlaff C, Van Wyngaarden C, Duryea J. Location-specific hip joint space width for progression of hip osteoarthritis—data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2014;22(10):1481-1487. doi: 10.1016/j.joca.2014.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Riff AJ, Kunze KN, Movassaghi K, et al. Systematic review of hip arthroscopy for femoroacetabular impingement: the importance of labral repair and capsular closure. Arthroscopy. 2019;35(2):646-656.e3. doi: 10.1016/j.arthro.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 44. Rosinsky PJ, Kyin C, Maldonado DR, et al. Determining clinically meaningful thresholds for the nonarthritic hip score in patients undergoing arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37(10):3113-3121. doi: 10.1016/j.arthro.2021.03.059 [DOI] [PubMed] [Google Scholar]
- 45. Ruzbarsky JJ, Comfort SM, Lee S, Pierpoint LA, Philippon MJ. The relationship between the joint space and outcomes after hip arthroscopic surgery for femoroacetabular impingement: reevaluating the 2-mm rule. Am J Sports Med. 2023;51(6):1538-1547. doi: 10.1177/03635465231161372 [DOI] [PubMed] [Google Scholar]
- 46. Saadat E, Martin SD, Thornhill TS, Brownlee SA, Losina E, Katz JN. Factors associated with the failure of surgical treatment for femoroacetabular impingement: review of the literature. Am J Sports Med. 2014;42(6):1487-1495. doi: 10.1177/0363546513500766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sivasundaram L, Rice MW, Horner NS, Alter TD, Ephron CG, Nho SJ. Hip arthroscopy for the treatment of femoroacetabular impingement syndrome in hips with mild osteoarthritis (Tönnis grade 1): a matched comparative cohort analysis at minimum 5-year follow-up. Am J Sports Med. 2022;50(10):2598-2605. doi: 10.1177/03635465221107354 [DOI] [PubMed] [Google Scholar]
- 48. Sogbein OA, Shah A, Kay J, et al. Predictors of outcomes after hip arthroscopic surgery for femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2019;7(6):2325967119848982. doi: 10.1177/2325967119848982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tijssen M, van Cingel R, van Melick N, de Visser E. Patient-reported outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskelet Disord. 2011;12:117. doi: 10.1186/1471-2474-12-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Westermann RW, Nepple JJ, Pascual-Garrido C, et al. The impact of age on clinical outcomes of acetabular microfracture during FAI surgery. Am J Sports Med. 2023;51(10):2559-2566. doi: 10.1177/03635465231184398 [DOI] [PubMed] [Google Scholar]
- 51. Zimmerer A, Ramoser A, Streit M, et al. Osteoarthrosis, advanced age, and female sex are risk factors for inferior outcomes after hip arthroscopy and labral debridement for femoroacetabular impingement syndrome: case series with minimum 10-year follow-up. Arthroscopy. 2021;37(6):1822-1828.e1. doi: 10.1016/j.arthro.2021.01.024 [DOI] [PubMed] [Google Scholar]


