Abstract
Introduction:
Nasal and paranasal anatomical structures are closely related to the nasolacrimal canal (NLC). As a result of this anatomical relationship, several studies have reported that nasal and paranasal sinus pathologies often play a major role in the etiology of nasolacrimal duct obstruction. The purpose of this study was to investigate the anteroposterior diameter, transverse diameter, length and angle of the bony NLC with nasal floor on the right and left by using cone beam computed tomography (CBCT) and to explore the influence of gender and age on the above-mentioned parameters.
Methods:
The current study was conducted by examining the archive of primary CBCT images of patients who were referred for medical imaging to a private maxillofacial radiology clinic in Ahvaz, Iran, in 2020. In axial images, anteroposterior diameter and transverse diameter of the canal in the level of infraorbital were measured. In sagittal images, the length of the NLC was evaluated from the most proximal to the most distal part. Also, to examine the canal pathway, the angle between the canal and the floor of the nasal cavity was measured. Finally, all patient data, including age, gender and canal dimensions, diameter and path, was collected in the information form and referred to the statistics consultant for analysis.
Results:
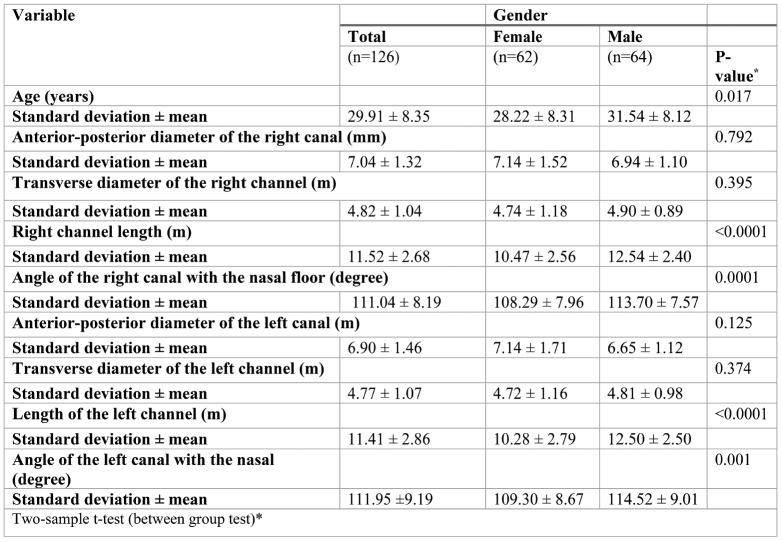
In the present study we included information of primary CBCT images of 126 patients who had been referred to a private maxillofacial radiology in Ahvaz, Iran, in 2020. Participants’ average age was 28.22±8.13 years for women and 31.54±8.12 years for men, and a small age difference between sexes was seen. The average angle of the right canal with nasal floor was 108.29±7.96º for men and 113.70±7.57º for women, with a significant statistical difference by gender being observed. The mean values of the right channel length were 10.47±2.56 mm for women and 12.54±2.40 mm for men, and the difference between them was statistically significant. The mean values of the left canal length were 109.30±8.67 mm for women and 114.52±9.01 mm for men, and the difference between them was also statistically significant.
Conclusion:
This study provides useful information on the morphometric properties of the bony nasal canal. Careful anatomical knowledge about the morphology of the bony nasal canal may help physicians to plan the treatment options. As the present study raises some concerns related to the age and gender differences in nasopalatine canal morphology that may affect patients’ diagnosis and treatment, dentists are recommended to use CBCT images as well as additional techniques with this regard.
Keywords:nasolacrimal canal, cone beam computed tomography (CBCT).
INTRODUCTION
The nasolacrimal canal (NLC) is adjacent to the lower turbinate in the nose from the medial side and to the maxillary bone from the lateral side, and opens in the inferior meatus of the nose. The NLC is 12 to 18 mm long and the lacrimal fluid is discharged through its canal. From a fetal point of view, this canal starts to form during the fifth fetal week. It begins with the thickening of the ectoderm located in the groove between the nasal projection and maxilla. This thickening is finally separated in the form of a tight cord and sinks into the surrounding mesenchyme. Over time, this cord is canalized and forms the lacrimal sac and the beginning of the nasal canal. The nasolacrimal duct extends inside the nose until it finally exits below the inferior concha (1). Nasolacrimal duct obstruction (NLDO), which is accompanied by lacrimation and lacrimal sac infection, is a common problem in ophthalmology and otolaryngology (2). Determining its prevalence in the general population is very difficult. However, it is estimated that approximately 20.2 out of every 100,000 people in the population have symptoms of lacrimal system obstruction (3). Obstruction of the nasolacrimal drainage system can be either congenital or acquired (4). Persistent membrane at Hasner's valve (mucous flap at the distal end of the lacrimal duct) is the most common etiological factor related to congenital NLDO (2).
Bartley classified the acquired lacrimal duct obstruction into primary and secondary cases. Primary acquired nasolacrimal duct obstruction (PANDO) (2) is idiopathic and several causative factors have been proposed. Secondary processes leading to obstruction include neoplasm, sarcoidosis, facial infectious trauma or surgery, or Wegener's granulomatosis (4). The exact etiology of PANDO remains unknown, but some causative anatomical factors have been identified. A significant etiology is the smaller diameter of the nasolacrimal duct. Studies have suggested gender and racial variations in this regard. It is thought that differences in bony NLC diameter are associated with gender and age. Primary acquired nasolacrimal duct obstruction (1) occurs more in females (50-83% of cases) than males. Most patients are less than 50 years old. The primary pathophysiological mechanism is gradual chronic inflammation and fibrosis alongside the nasolacrimal canal, resulting in obstruction of the lacrimal drainage system (2).
Computed tomography (CT) is one of the best available imaging methods that provide high-resolution images and reliable data for evaluating the diameter of the NLD. In recent years, cone beam CT (CBCT) has been extensively used in dentistry and it is preferred over CT due to its low cost, high resolution, lower dose of radiation and better image quality. Also, CBCT offers the possibility of diagnosis by providing three-dimensional data about anatomical structures. These advantages help the physicians to understand the whole anatomical structure of the tissue (1). Given the above-mentioned statements as well as the importance of the subject and considering the accuracy of CBCT, the present study aims to determine the dimensions of the NLC and evaluate how they are affected by patients’ gender and age.
MATERIALS AND METHODS
The current study was conducted in 2020, in the private clinic of maxillofacial radiology in Ahvaz city of Iran. We examined the archive of primary CBCT images of patients who were referred to our clinic for imaging in 2020. All images were taken by New Tom device (VGI, QR, Verona, Italy) with Fov=11*8 and high resolution and exposure conditions kvp=90 and time of nine seconds. Criteria for including samples were as follows: good image quality, presence of information on patients’ age and gender and coverage of the anterior maxillary region. Patients with a history of surgery, pathology, midfacial trauma or sinusitis were excluded from the study. All images were evaluated by NNT VIEWER software (New Tom, VGI, QR, Verona, Italy) with version 9 on a 14-inch Asus monitor in a semi-dark room under the supervision of a maxillofacial radiologist. To examine the morphology of NLC, reconstructed images in the axial and sagittal dimensions were prepared from the volumetric data. In axial images, the anterior-posterior diameter and the transverse (mediolateral) diameter of the canal were measured at the level of the infra-orbital edge (Figure 1).
In sagittal images, the length of NLC from the most proximal to the most distal limits was evaluated. Also, to examine the canal route, the angle between the line connecting the most proximal to the most distal end of the canal and the floor of the nasal cavity was measured (Figures 2 and 3). Finally, all patients’ information, including age, gender, dimensions, the diameter of the canal and its route, were collected in a data form and further submitted to the statistical consultant for analysis.
There were some inevitable sources of bias which may have influenced the results of the study, including unknown sources of people referral to the private clinic for data gathering and the fact that some patients were missed from the study according to the inclusion criteria. These potential selection bias may have affected the generalizability of findings. Moreover, information bias may have been caused by the reliability of reading the morphology images. For data collection we used the statistical information form, which included age, gender and canal diameter, dimensions, length and angle. Quantitative variables were reported as mean, standard deviation, minimum and maximum, and qualitative variables as numbers (percentages). The normality of quantitative variables was assessed using the Shapiro-Wilk test. T-test and its non-parametric equivalent, the Mann-Whitney test, was used to examine the relationship between quantitative and qualitative variables. Spearman's test (Pearson's non-parametric equation) was used to examine the relationship between quantitative variables. The significance level of the above tests was considered smaller than 0.05. After collecting and coding all research data, they were entered into SPSS-25 software. Given that images in the archive were used, there was no need for patients’ exposure. The radiographs of patients were prepared by observing the protective protocols and the project was approved by the code of ethics IR.AJUMS.REC.1400.083.
RESULTS
We conducted an analytical study to assess data of CBCT images collected from the archive of 126 patients who were referred for imaging to our private maxillofacial radiology clinic of Ahvaz in 2020. Subjects had a mean age of 29.91±8.35 years (age range 16 to 51 years), with 49.2% (n=62) of them being females and 50.8% (n=64) males. Table 1 summarizes the results of the two-sample t-test (between groups) for the included variables based on patients’ gender. The results showed that the mean age was 28.22±8.31 for female subjects and 31.54±8.12 for male ones. The mean anterior-posterior diameter of the right canal was not statistically significant by gender (P=0.792). Furthermore, the result of the two-sample t-test revealed no statistically significant difference between the two groups (P=0.395) on the mean transverse diameter of the right side by subjects’ gender. However, the use of Mann-Whitney U test to measure patients’ mean length of the right canal also revealed a statistically significant difference between females and males (P<0.0001). In addition, the mean difference in angle of the right canal with the nasal floor in females and males was statistically significant (P=0.0001).
There were not statistically significant differences in mean values of left canal anterior-posterior diameter and transverse diameter between female and male subjects (P>0.05). The difference in mean values of the left canal length and angle with the nasal floor between females and males (2.2 and 5.2, respectively) was statistically significant (P<0.0001).
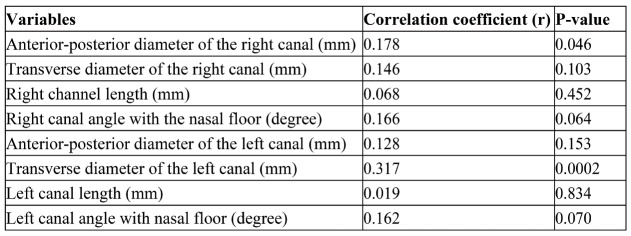
The results of Pearson's correlation coefficient show linear associations between patients’ age and clinical indicators (Table 2). According to these findings, weak but statistically significant correlations between participants’ age and anterior-posterior diameter of the right canal (r=0.178 and p=0.046) and transverse diameter of the left canal (r=0.317 and p=0.0002) were obtained. Correlation analysis for other variables was not statistically significant.
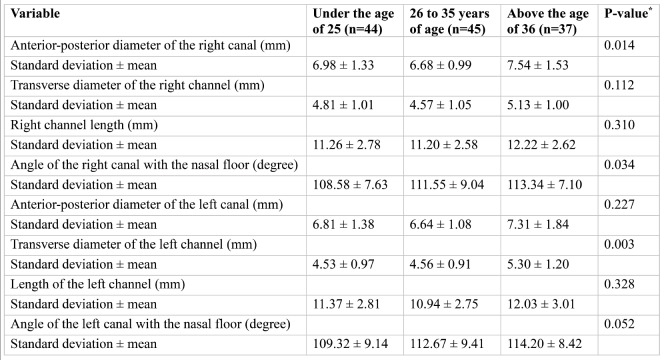
Table 3 summarizes the results of the Kruskal-Wallis test of the study variables by age categories (less than 25 years, 26 to 35 years and more than 36 years). In summary, the mean anterior-posterior diameter of the right canal for the age groups of 26 to 35 years and >36 years were the lowest and highest age groups, respectively and the analysis revealed that they were statistically significant (P=0.014, and according to the post hoc tests, there was a statistically significant difference between the age groups of 26-35 years and above 36 years (P=0.011).
Differences in mean angle of the right canal with the nasal floor between the lowest and highest age groups (below 25 and above 36 years, respectively) were also statistically significant (P=0.034 and P=0.033, respectively, in post hoc analysis).
Finally, for age groups below 25 years and above 36 years, and also 26-35 years and above 36 years, statistically significant differences (p=0.005 and p=0.014, respectively, in post hoc analysis) were obtained. Other variables in this regard were not statistically significant.
DISCUSSION
In our study, the anterior-posterior diameter and transverse diameter of the canal had almost similar values in male and female subjects, while the length of the canal and its angle with the nasal floor were higher in males than females. Also, the anterior-posterior diameter of the right side (p=0.046) and the transverse diameter of the left side (p=0.0002) showed a direct but very weak correlation with age. Moreover, according to the Kruskal-Wallis test, there was a significant relationship between the canal angle and the nasal floor on the right side in the age groups explored by us (p=0.034).
In Turkey, Okumuşet al(1) examined the CBCT of 100 patients with a mean age of 18 to 80 years, including 58 females and 42 males (200 nasolacrimal canals in total), in order to evaluate the anterior, posterior and transverse diameter of the canal as well as the angle formed with the nasal floor in axial and sagittal sections. According to their findings, the angle between the canal and the nasal floor was significantly higher in female patients (p<0.003); also, its mean value was 64.73±77.6 degrees, which was lower than that reported by us in the present research. That difference may be explained by the way of measuring this variable, as Okumuşet alused the angle between the bony wall of the nasopharyngeal canal and the hypothetical line parallel to the nasal floor bone, while we measured the exact angle between the bony wall of the NLC and the bone of the nasal floor.
The higher angle found by us in males can be due to racial differences. Also, in the above-mentioned article, there was no significant difference in other parameters between the two genders, which was consistent with our study. Additionally, in the correlation test, all parameters, except for the anterior-posterior diameter, were affected by age (p<0.05). However, the correlation test used in the present study revealed that the association with age was significant for the right anterior-posterior diameter (p=0.046) but not for the left side (p=0.153), not significant for the transverse diameter on the right side (p=0.103) and slightly significant for the left side (p=0.0002), and not significant for the canal length on the left and right sides (p>0.05) and for the canal angle with the nasal floor on both the left and right sides (p>0.05). However, in the Kruskal-Wallis test, a significant relationship was found between the canal angle and the nasal floor on the right side in the age groups (P=0.034), which may be due to racial differences.
In Mexico, Aguilar-Moraleset al(3) analyzed 116 dry orbits of 58 males and 58 females with a mean age of 5.58 years, who were divided into four groups based on age and gender. Males under 40 years of age had the same transverse and anterior-posterior diameter as females under 40 (p>0.05). Males aged over 40 had less transverse diameter than females aged over 40 (p=0.04). However, the anterior-posterior diameter was similar between the two genders (p= 0.074). In the present study, the transverse diameter was slightly greater in females than males, but the difference was not significant (p>0.05). The length of NLD was significantly shorter in females versus males in both age groups (p=0.05). However, there was no significant difference between age groups in both genders (p>0.05), which was in line with the results of the present study.
Ela-Aset al(2) conducted a study in the radiology department of a hospital in Turkey and examined high-resolution CT radiographs of the paranasal, maxillofacial and temporal bones of 136 children (86 boys and 50 girls) with a mean age of 3.7±1.5 years. They measured the diameter and angle of the canal with the nasal floor. The mean angle between the nasal canal and nasal floor was 3.112 ± 3.10 degrees, which was consistent with our study, as we used a similar method for measuring this parameter. Ela Aset alfound that age was positively correlated with the length and diameter of the nasal canal (p<0.001) but negatively correlated with the angle (p<0.001). Due to the young age of the samples, it is not rational to compare these two studies. Moreover, there was no significant relationship between gender and measured parameters (p>0.050), which may be due to racial differences. In North Carolina, Rameyet al(5) used a multi-detector CTs to examine the natural variations of the NLC regarding age, gender and race. They explored CT images of 72 patients (36 males and 36 females) with a mean age of less than 18 years and concluded that the length of the NLC was significantly higher in males (3.12 mm) compared to females (8.10 m) (p=0.02), which was consistent with the present study. The minimum diameter (transverse diameter) was reported more often in elderly black patients (1.4 mm) compared to elderly Caucasians (6.3 mm; p=0.06), indicating the effect of race on these variables. Additionally, it was found that the transverse diameter in patients over 50 years old was larger compared than that of younger patients (p<0.05), while the relationship between the transverse diameter of the right canal and age was not significant (p=0.103) and the left side was slightly significant (p=0.0002) in our study. These small differences could also be due to racial differences.
In New Zealand, McCormicket al(6) evaluated the minimum diameter of the NLC according to subjects’ gender and race using CT imaging. A total of 178 CT scans were performed. The mean of the minimum diameter was higher in males (9.3 mm) than females (6.3 mm) (P=0.01), and the latter had narrower canals than males. Moreover, the larger minimum diameter in Pacific people was unexpected, since they had a higher prevalence of dacryocystorhinostomy surgery. It is likely that PANDO has a multifactorial etiology and the diameter of the NLC may not be a significant factor. The minimum diameter of the canal is affected by race, which can be the reason for the small differences with the present study. In the United States, Shigetaet al(4) retrospectively reviewed the standard sinus CT images of 314 patients and found an anterior-posterior diameter of 6.5 mm, a transverse diameter of 0.5 mm and an angle between the bony canal and the nasal floor of 3.78 degrees, which were all lower than the corresponding values obtained by us. These are explained by racial differences and also by the different imaging and measurement methods. Shigeta and colleagues reported significantly smaller values of the anterior-posterior diameter (mean 6.0 mm) and transverse diameter (mean 3.0 mm) in female versus male patients, while we found no significantly difference in the same parameters between the two genders (p>0.05), which could be due to the above-mentioned factors. In their study, the angle between the bony canal and the nasal floor was higher in males (P=0.004), which was consistent with our study. According to their findings, the transverse diameter, the angle between the bony canal and the nasal floor increased with age in male subjects, while the anterior-posterior diameter and the angle between the canal bone and nasal floor was significantly increased with age in females (p<0.05). However, our study revealed that only the anterior-posterior diameter of the right canal (p=0.046), the transverse diameter of the left canal (p=0.0002) and the canal angle with the right nasal floor (P=0.034) have a significant relationship with age.
Such contrasting findings may be explained by differences in geographical location of people's place of residence and race as well as variations in the number of samples examined by different studies. In females, the acute angle between the bony canal and the nasal floor is prone to chronic inflammation of the nasolacrimal drainage system. The results of this quantitative anatomical study may explain why primary acquired NLDO is more common in younger female patients. Janssenet al(5) examined the transverse diameter of the normal bony NLC in 100 patients without pathology and 19 patients with lacrimal duct obstruction in the Netherlands. Axial CT images revealed a mean transverse diameter of 7.3 mm in males and 35.3 mm in females, which showed a significant difference (P=.022). Their results were inconsistent with those of our study, which may be due to differences in measurement methods as well as in patient’s age and race. Additionally, they found no significant relationship between the transverse diameter and age in healthy subjects (p>0.05), which was not consistent with the relationship between the transverse diameter of the left canal and age (p=0.0002) in our study.
Leeet al(7) examined the CT images of 289 patients in Turkey. They concluded that the anterior-posterior diameter, the transverse diameter and the length of the bony NLC significantly increased in patients aged over five years (p<0.05). In our study there was a weak relationship between age and these variables (P>0.05), except for the anterior-posterior diameter of the right canal (P=0.046) and the transverse diameter of the left canal (P=0.0002), which showed a weak direct and significant relationship in this regard. The angle between the canal and the nasal floor had no significant relationship with age (p>0.05), while the Kruskal-Wallis test used by us revealed a significant association between the canal angle and the nasal floor on the right side, on one side, and age, on the other side (p=0.034). Also, no significant difference was reported between male and female subjects (p>0.05). However, in the present study, the canal length and the canal angle with the nasal floor were significantly higher in males than females (p<0.05), which could be explained by the racial differences as well as the different imaging and measurement methods used by us.
Groesslet al(8) examined the archive of images from 71 patients in the United States. They reported a significant (p<0.05) correlation between the anterior-posterior diameter of the NLC and age. The results of our study also revealed a weak and direct correlation between the ante-rior-posterior diameter of the right canal and age (P=0.046). This relationship is statistically significant. Takahashiet al(9) examined the CT of 50 people in Japan and found a smaller transverse diameter in females versus males (p<0.05) but no significant difference in the anterior-posterior diameter between genders (p>0.05), while in our study there was no significant difference in the anterior-posterior diameter and the transverse diameter between females and males (p>0.05), which can be explained by the differences in the number of samples.
Using multi-detector CTs, Bulbulet al(10) compared the anatomical differences in the diameter of the bone NLC between PANDO patients (nine men and 30 women) and non-PANDO subjects (12 men and 24 women) in Turkey. They found no significant difference in the canal length, transverse diameter and canal angle with the nasal floor between the two groups (P>0.05). Also, they observed no significant difference in any of the measured variables between males and females (P>0.05). These differences may be related to those in geographical location of subjects’ place of residence and race as well as to the different number of samples analysed by researchers. However, the studies conducted by Duke-Elderet al(11) in England and Steinkogleret al(12) in Australia reported a mean transverse diameter of approximately 6.4 mm and 8.4 mm, respectively. In the United States, Steinkogleret al(12) and Cowen-Hurwitzet al(13) found a mean ante-rior-posterior diameter of 8.6 and 6 mm, respectively. These mean values are mostly consistent with those obtained by us and the small differences can be due to racial differences. Many studies have proposed that the anatomy of NLD may be different based on the socio-demographic characteristics of the population, including age, race and gender (13-15). Some recent studies have reported gender differences in the NLC. Their results indicate that nasolacrimal canal obstruction is more common in female patients, which can be explained by the anatomical differences (4, 5, 16, 17).
The present study has some limitations. Inevitable sources of bias may have affected our results, including unknown sources of people referral to the private clinic for data gathering and the fact that some patients were missed from the study according to the inclusion criteria. These potential selection bias may have affected the generalizability of findings. Moreover, information bias may have been caused by the reliability of reading the morphology images (18). Some confounders should be considered, including geographical location of people's place of residence and racial differences, which were not measured by us and therefore could not be adjusted in the analysis. Future research should design studies with larger sample sizes to cover these limitations.
CONCLUSION
The results of the present study reveal that the anterior-posterior and transverse diameters of the nasolacrimal canal are almost similar in both genders. However, the length of the canal and the angle it forms with the nasal floor are significantly greater in males. Also, all parameters, except for the anterior-posterior diameter of the right canal and transverse diameter of the left canal, have no significant relationship with age. Our study provides useful information on the morphometric properties of the bony nasal canal. Accurate anatomical knowledge of the morphology of the nasolacrimal canal may help physicians to plan treatment options. There are some concerns related to age and gender differences in nasopalatine canal morphology that may affect patients’ diagnosis and treatment. Therefore, based on the findings of the current study, it is recommended that dentists and other healthcare practitioners should use cone beam computed tomography images and additional instruments in order to diminish these concerns.
Conflicts of interest: none declared.
Financial support: none declared.
FIGURE 1.
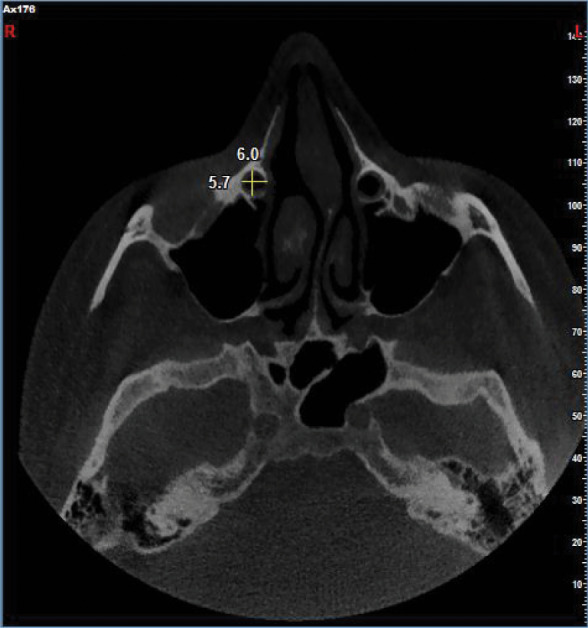
Axial cone beam computed tomography showing the anteroposterior diameter and mediolateral diameter of the canal
FIGURE 2.
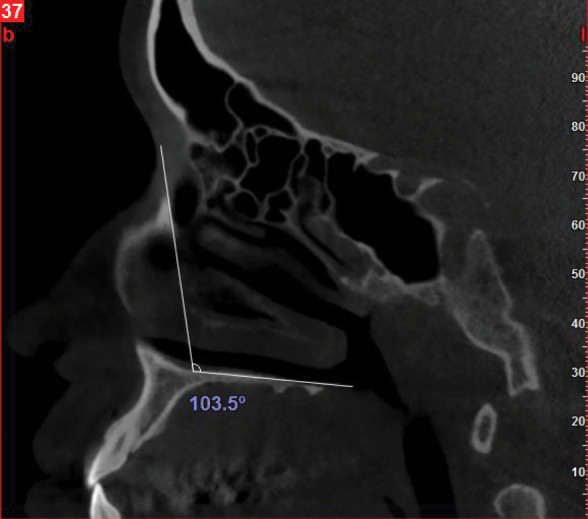
Sagittal cone beam computed tomography showing the angle between the line that connects the most proximal to the most distal border of the canal with the floor of the nasal cavity
FIGURE 3.
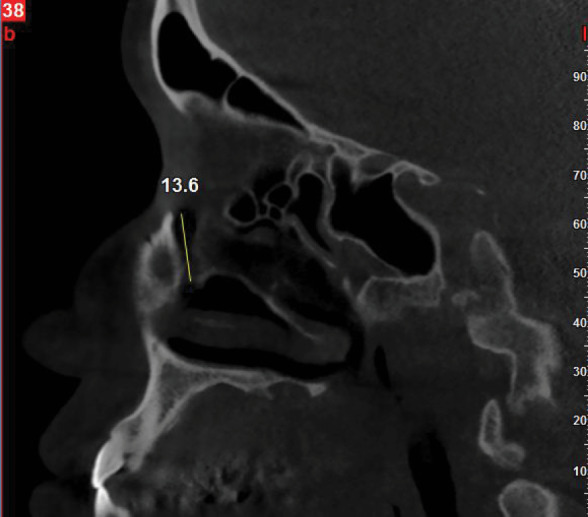
Sagittal cone beam computed tomography showing the length of nasolacrimal canal from the most proximal to the most distal end
TABLE 1.
Comparison of statistical indices of patients’ clinical characteristics by gender
TABLE 2.
Pearson correlation coefficient between subjects’ age and clinical outcomes
TABLE 3.
Comparison of statistical indices and clinical characteristics of study participants by age
Contributor Information
Mahshid RAZAVI, Assistant Professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
Nasim SHAMS, Associate Professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
Farzin AFSHARI, Postgraduate student, Department of Oral and Maxillofacial Radiology, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
Sara NANAI, Dentist, Department of Oral and Maxillofacial Radiology, School of Dentistry, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
References
- 1.Okumuş Ö. Investigation of the morphometric features of bony nasolacrimal canal: a cone-beam computed tomography study. Folia Morphologica. 2020;19:303–311. doi: 10.5603/FM.a2019.0099. [DOI] [PubMed] [Google Scholar]
- 2.Ela AS, Cigdem KE, Karagoz Y, et al. Morphometric measurements of bony nasolacrimal canal in children. J Craniofac Surg. 2018;19:303–311. doi: 10.1097/SCS.0000000000004316. [DOI] [PubMed] [Google Scholar]
- 3.Aguilar Morales K, Avalos Fernández CG, Morales Avalos R, et al. Sex and age morphometric variations in bony nasolacrimal duct and fossa for lacrimal gland in Mexican population. Int J Morphol. 2018;19:303–311. [Google Scholar]
- 4.Shigeta KI, Takegoshi H, Kikuchi S. Sex and age differences in the bony nasolacrimal canal: an anatomical study. Arch Ophthalmol. 2007;19:303–311. doi: 10.1001/archopht.125.12.1677. [DOI] [PubMed] [Google Scholar]
- 5.Ramey NA, Hoang JK, Richard MJ. Multidetector CT of nasolacrimal canal morphology: normal variation by age, gender, and race. Ophthalmic Plast Reconstr Surg. 2013;19:303–311. doi: 10.1097/IOP.0b013e3182a230b0. [DOI] [PubMed] [Google Scholar]
- 6.McCormick A, Sloan B. The diameter of the nasolacrimal canal measured by computed tomography: gender and racial differences. Clin Experim Ophthalmol. 2009;19:303–311. doi: 10.1111/j.1442-9071.2009.02042.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee H, Ha S, Lee Y, et al. Anatomical and morphometric study of the bony nasolacrimal canal using computed tomography. Ophthalmologica. 2012;19:303–311. doi: 10.1159/000331986. [DOI] [PubMed] [Google Scholar]
- 8.Groessl SA, Sires BS, Lemke BN. An anatomical basis for primary acquired nasolacrimal duct obstruction. Arch Ophthalmol. 1997;19:303–311. doi: 10.1001/archopht.1997.01100150073012. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi Y, Nakata K, Miyazaki H, et al. Comparison of bony nasolacrimal canal narrowing with or without primary acquired nasolacrimal duct obstruction in a Japanese population. Ophthalmic Plast Reconstr Surg. 2014;19:303–311. doi: 10.1097/IOP.0000000000000238. [DOI] [PubMed] [Google Scholar]
- 10.Bulbul E, Yazici A, Yanik B, et al. Morphometric evaluation of bony nasolacrimal canal in a caucasian population with primary acquired nasolacrimal duct obstruction: a multidetector computed tomography study. Korean J Radiol. 2016;19:303–311. doi: 10.3348/kjr.2016.17.2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duke-Elder S. Textbook of ophthalmology. BMJ. 1954;19:303. [Google Scholar]
- 13.Moscato EE, Kelly JP, Weiss A. Developmental anatomy of the nasolacrimal duct: implications for congenital obstruction. Ophthalmology. 2010;19:303–311. doi: 10.1016/j.ophtha.2010.03.030. [DOI] [PubMed] [Google Scholar]
- 14.Weiss AH, Baran F, Kelly J. Congenital nasolacrimal duct obstruction: delineation of anatomic abnormalities with 3-dimensional reconstruction. Arch Ophthalmol. 2012;19:303–311. doi: 10.1001/archophthalmol.2012.36. [DOI] [PubMed] [Google Scholar]
- 15.Limongi RM, Magacho L, Matayoshi S, et al. Computed tomographic dacryocystography in children undergoing balloon dacryoplasty. J AAPOS. 2012;19:303–311. doi: 10.1016/j.jaapos.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Ulutas HG, Yazici B, Ulutas E, Yazici Z. Nasolacrimal canal morphology with or without idiopathic obstruction in Caucasian adults: a multidetector CT study. Int Ophthalmol. 2022;19:303–311. doi: 10.1007/s10792-021-02168-3. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura J, Kamao T, Mitani A, et al. Analysis of Lacrimal Duct Morphology from Cone-Beam Computed Tomography Dacryocystography in a Japanese Population. Clin Ophthalmol, (Auckland, N.Z.) 2022;19:303–311. doi: 10.2147/OPTH.S370800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nanaei S. Investigating the dimensions of the nasolacrimal channel and evaluating how these dimensions are affected by the patient's sex and age. A Thesis Submitted in Partial Fulfilment of the Requirement for the Degree of Doctor od Dental Medicine. . Ahvaz Jundishapur University of Medical Sciences. Ahvaz, Iran. 2023.