Abstract
Craniopharyngioma (CP) and Rathke's cleft cyst (RCC) are both suprasellar lesions. They are sometimes difficult to distinguish due to their similar findings. We report a case of papillary craniopharyngioma (pCP) with the clinical findings suggesting RCC. A 42-year-old female with intellectual disability presented to our hospital with severe visual dysfunction. Preoperative images revealed a suprasellar cystic lesion without calcification. We performed transsphenoidal surgery. Since the cyst had condensed-milk-like content suggesting RCC, we performed cyst fenestration and wash without removal of the cyst wall. Thereafter, we found fish-egg-like structures on the cyst wall. The histopathological analysis revealed that they had papillary structures surrounded by hyperplastic squamous epithelium with parakeratosis. Immunostaining for BRAF V600E was positive, leading to the diagnosis of pCP. After the surgery, her visual function improved and follow-up Magnetic resonance imaging at 18 months postoperatively showed no apparent recurrence. The presence of condensed-milk-like content suggests a likelihood of RCC indicating that aggressive resection may not be necessary. In contrast, the existence of fish-egg-like structures suggests pCP and requires careful follow-up.
Keywords: rathke's cleft cyst, papillary craniopharyngioma, squamous metaplasia, stratified squamous epithelium
Introduction
Craniopharyngioma (CP) is a suprasellar lesion that forms cyst and is believed to originate from remnant of the craniopharyngeal duct. It can be classified into two types: adamantinomatous and papillary. These subtypes exhibit distinct patterns of genetic mutations, with β-catenin and BRAF V600E mutations in adamantinomatous and papillary subtypes, respectively, which are now considered entirely separate entities. The latter subtype poses challenges in intraoperative pathological diagnosis due to its lesion consisting of stratified squamous epithelium, necessitating the differentiation from RCC with squamous metaplasia. Although there may be some imaging overlap between pCP and RCC, differentiating between the two during surgery is often achievable based on the cyst content; motor-oil-like content typically suggests CP, whereas condensed-milk-like content is more characteristic of RCC. In this study, we present a case of pCP with condensed-milk-like contents within the cyst.
Written informed consent for publication of this case report and accompanying images was obtained from the patient.
Case Report
Patient
A 42-year-old woman with intellectual disability presented to our hospital with severe visual disturbance. Magnetic resonance imaging (MRI) revealed a cystic mass in the suprasellar region. There were no neurological abnormalities other than severe vision loss with bitemporal hemianopsia. MRI showed a single cyst with a maximum diameter of 34 mm, compressing the optic chiasm and no obvious substantial components. T1- and T2-weighted image showed isointensity and low intensity in the cyst, respectively. Gadolinium contrast-enhanced T1-weighted images showed a slight contrast effect on the cyst wall. Computed tomography (CT) showed no calcification (Fig. 1). Baseline hormonal evaluations revealed growth hormone and insulin-like growth factor-1 levels below the reference range, and stimulation testing indicates adult growth hormone deficiency, but other hormonal values were within the normal range. No diabetes insipidus was detected.
Fig. 1.
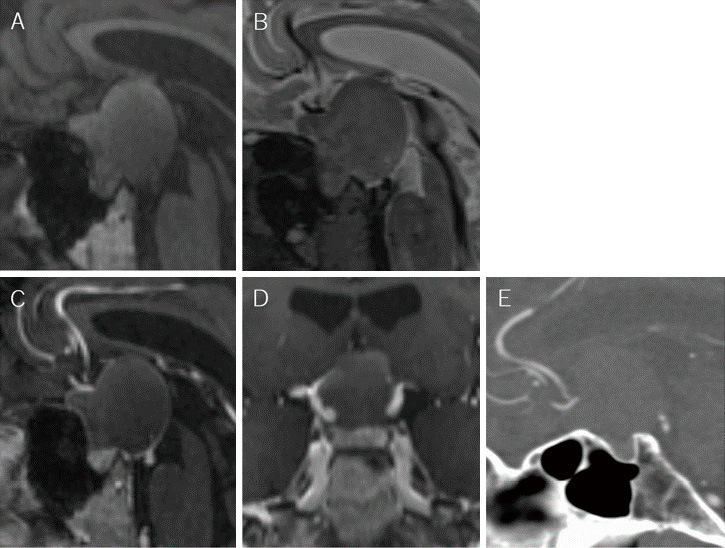
Preoperative images.
A, B: Sagittal view of T1-weighted (A) and T2-weighted (B) MR images. C, D: Coronal (C) and sagittal (D) view of T1-weighted contrast-enhanced MR images. E: Sagittal view of contrast-enhanced CT image.
Surgery
The patient underwent extended transsphenoidal surgery (eTSS). Under general anesthesia, she was placed in a supine position with the upper body elevated at 15, and the head was fixed in a Sugita four-point head holder (Mizuho Medical Innovation, Tokyo, Japan). We accessed the lesion via the right transseptal approach by a 4 mm, 0° rigid neuroendoscope (Olympus, Tokyo, Japan) with an Endo Arm (Olympus, Tokyo, Japan). Septal bone was resected and preserved as autologous graft material for rigid sellar reconstruction. The anterior wall of sphenoid sinus was widely opened, and an adequate amount of sellar and parasellar bones was removed based on the size and shape of the lesion. The dura mater was then incised in an inverted “T” shape. There was a cystic lesion with condensed-milk-like contents (Fig. 2A, B). Since this finding was suggestive of RCC, we opted for the partial resection of the cyst (specimen 1), followed by aspiration of the contents and washing of the cyst. In addition, we found a very small, fish-egg-like structures on the posterior wall of the cyst (Fig. 2C, Supplementary Movie 1), which was also collected as a pathological specimen (specimen 2). The dura was closed by shoelace suture with inlay collagen matrix same as reported by Nagata et al.1) and covered by onlay collagen matrix. Rigid reconstruction was performed using the septal bone and a resorbable fixation mesh.
Fig. 2.
Intraoperative findings.
A: Intraoperative neuroendoscopic photograph showing a cyst after dura incision. B: Condensed-milk-like contents (asterisk) in the cyst. C: Fish-egg-like structures in the cyst (arrowhead).
Pathology
Microscopic examination revealed two components: One had flat squamous epithelium partly with superficial ciliated columnar cells in specimen 1, and the other had papillary proliferation of squamous epithelium with a fibrous core in specimen 2 (Fig. 3A-D). Immunohistochemical analysis in both components was positive for BRAF V600E, and there was no nuclear staining of β-catenin, leading to the diagnosis of pCP (Fig. 3E-H).
Fig. 3.
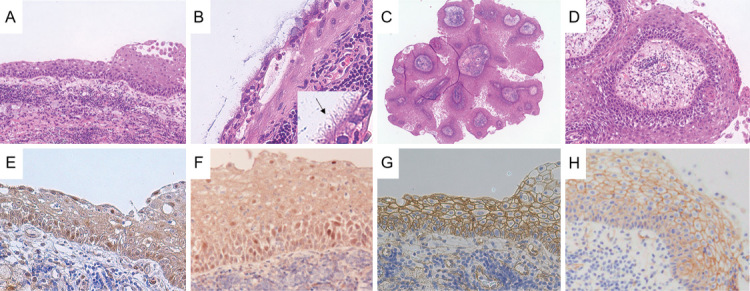
Histopathological findings.
A: Squamous epithelium of specimen 1 (HE stain ×200). B: Ciliated (arrows) columnar epithelium of specimen 1 (HE stain ×400). C, D: Stratified squamous epithelium of specimen 2 (C: HE stain ×40, D: HE stain ×200). E, F: BRAF V600E is positive in both of specimens 1 (E) and 2 (F) (BRAF V600E immunostain ×400). G, H: Nuclear β-catenin accumulation is not found in both of specimens 1 (G) and 2 (H) (β-catenin immunostain ×400).
Postoperative course
The postoperative MRI showed successful cyst fenestration (Fig. 4), and the patient's recovery was uneventful, with an improvement in visual function. There were no indications of anterior pituitary hypofunction or diabetes insipidus. Follow-up MRI at 18 months postoperatively showed no apparent recurrence.
Fig. 4.

Postoperative image.
Postoperative sagittal view of T1-weighted contrast-enhanced MR image.
Discussion
Both pCP and RCC are believed to originate from remnants of the craniopharyngeal duct, and when they present as a single cystic lesion without calcification,2) there may be overlap in imaging and intraoperative findings, making it difficult to differentiate between the two pre- and intraoperatively. Pathologically, pCP and RCC with squamous metaplasia resemble each other.3) Liu et al. reported that the triggering receptor expressed on myeloid cells-1 is positive in RCC and pCP but negative in aCP, suggesting that the pathogenesis of RCC and pCP is similar.4) In addition, there is a hypothesis that some pCP may originate from RCC. Okada et al. reported a case where the diagnosis changed from RCC at the first surgery to pCP at recurrence.5) Moreover, Ahmed et al. reported a case where both components were found within the same lesion.6) The name “ciliated” CP is sometimes used as an intermediate entity.7) While the cyst contents of craniopharyngiomas are typically motor-oil-like fluid, there have been reports of cases with condensed-milk-like content; these cases were considered as ciliated CP.5,8)
In this case, pathological examination revealed that the cyst was covered by squamous epithelia partly with the ciliated columnar cells and partly with papillary structure with fibrous cores, resembling a fish-egg-like appearance. These findings suggest that this case may represent the early stages of the development of a pCP. Therefore, the existence of fish-egg-like structures is an important finding suggesting pCP that can be observed during the surgery.
Normally, if there is residual tumor after surgery for craniopharyngiomas, a high rate of regrowth is expected (37.9%-75.0%).9-14) Shi et al. reported that the period of regrowth after subtotal or partial resection is an average of 6 months.13) In our case, although only fenestration of the cyst was performed, the tumor did not enlarge for 18 months without any additional treatment. The presence of condensed-milk-like content inside the cyst may suggest a lower tendency to grow, as seen in RCC. Moreover, the total resection of the lesion has a very high risk of diabetes insipidus (55.6%-60.1%) and anterior pituitary dysfunction (72.7%-96.9%).15,16) Therefore, it seemed appropriate not to perform resection to preserve the function of hypothalamus and pituitary in this case.
Although the intraoperative findings and the postoperative course until now are similar to RCC, the pathological diagnosis is pCP, which requires careful follow-up.
Conclusion
We encountered a case that suggests an early stage of pCP. The presence of fish-egg-like structures is an important intraoperative finding suggesting pCP, requiring pathological confirmation with immunohistochemistry for BRAF V600E and careful follow-up.
Conflicts of Interest Disclosure
The authors declare no conflicts of interest.
Supplementary Material
Intraoperative view after the removal of cyst contents. Fish-egg-like structures were found on the cyst wall
References
- 1). Nagata Y, Takeuchi K, Sasaki H, et al. : Modified shoelace dural closure with collagen matrix in extended transsphenoidal surgery. Neurol Med Chir (Tokyo) 62: 203-208, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Lee IH, Zan E, Bell WR, Burger PC, Sung H, Yousem DM: Craniopharyngiomas: radiological differentiation of two types. J Korean Neurosurg Soc 59: 466-470, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Zada G, Lin N, Ojerholm E, Ramkissoon S, Laws ER: Craniopharyngioma and other cystic epithelial lesions of the sellar region: a review of clinical, imaging, and histopathological relationships. Neurosurg Focus 28: E4, 2010 [DOI] [PubMed] [Google Scholar]
- 4). Liu Y, Wang CH, Li DL, et al. : TREM-1 expression in craniopharyngioma and Rathke's cleft cyst: its possible implication for controversial pathology. Oncotarget 7: 50564-50574, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Okada T, Fujitsu K, Miyahara K, et al. : Ciliated craniopharyngioma--case report and pathological study. Acta Neurochir (Wein) 152: 303-306; discussion 307, 2010 [DOI] [PubMed] [Google Scholar]
- 6). Alomari AK, Kelley BJ, Damisah E, et al. : Craniopharyngioma arising in a Rathke's cleft cyst: case report. J Neurosurg Pediatr 15: 250-254, 2015 [DOI] [PubMed] [Google Scholar]
- 7). Oka H, Kawano N, Yagishita S, Kobayashi I, Saegusa H, Fujii K: Ciliated craniopharyngioma indicates histogenetic relationship to Rathke cleft epithelium. Clin Neuropathol 16: 103-106, 1997 [PubMed] [Google Scholar]
- 8). Sato K, Oka H, Utsuki S, Kondo K, Kurata A, Fujii K: Ciliated craniopharyngioma may arise from Rathke cleft cyst. Clin Neuropathol 25: 25-28, 2006 [PubMed] [Google Scholar]
- 9). Yamada S, Fukuhara N, Oyama K, et al. : Surgical outcome in 90 patients with craniopharyngioma: an evaluation of transsphenoidal surgery. World Neurosurg 74: 320-330, 2010 [DOI] [PubMed] [Google Scholar]
- 10). Morisako H, Goto T, Goto H, Bohoun CA, Tamrakar S, Ohata K: Aggressive surgery based on an anatomical subclassification of craniopharyngiomas. Neurosurg Focus 41: E10, 2016 [DOI] [PubMed] [Google Scholar]
- 11). Duff J, Meyer FB, Ilstrup DM, Laws ER Jr, Schleck CD, Scheithauer BW: Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery 46: 291-305; discussion 302, 2000 [DOI] [PubMed] [Google Scholar]
- 12). Lee MH, Kim SH, Seoul HJ, et al. : Impact of maximal safe resection on the clinical outcome of adults with craniopharyngiomas. J Clin Neurosci 19: 1005-1008, 2012 [DOI] [PubMed] [Google Scholar]
- 13). Van Effenterre R, Boch AL: Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97: 3-11, 2002 [DOI] [PubMed] [Google Scholar]
- 14). Shi XE, Wu B, Fan T, Zhou ZQ, Zhang YL: Craniopharyngioma: surgical experience of 309 cases in China. Clin Neurol Neurosurg 110: 151-159, 2008 [DOI] [PubMed] [Google Scholar]
- 15). Guo Y, Pei L, Li Y, et al. : Characteristics and factors influencing hypothalamic pituitary dysfunction in patients with craniopharyngioma. Front Endocrinol (Lausanne) 14: 1180591, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). Karavitaki N, Brufani C, Warner JT, et al. : Craniopharyngiomas in children and adults: systematic analysis of 121 cases with long-term follow-up. Clin Endocrinol (Oxf) 62: 397-409, 2005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative view after the removal of cyst contents. Fish-egg-like structures were found on the cyst wall



