Abstract
Background and aim
This study explores healthcare professionals’ perspectives on end-of-life care in pediatric intensive care units (ICUs) in Croatia, aiming to illuminate their experiences with such practices, underlying attitudes, and major decision-making considerations. Amid the high variability, complexity, and emotional intensity of pediatric end-of-life decisions and practices, understanding these perspectives is crucial for improving care and policies.
Methods
The study utilized a cross-sectional survey intended for physicians and nurses across all pediatric ICUs in Croatia. It included healthcare professionals from six neonatal and four pediatric ICUs in total. As the data from neonatal and pediatric ICUs were examined jointly, the term pediatric ICU was used to denominate both types of ICUs. A statistical analysis was performed using Python and JASP, focusing on professional roles, professional experience, and regional differences.
Results
The study included a total of 103 participants (with an overall response rate—in relation to the whole target population—of 48% for physicians and 29% for nurses). The survey revealed diverse attitudes toward and experiences with various aspects of end-of-life care, with a significant portion of healthcare professionals indicating infrequent involvement in life-sustaining treatment (LST) limitation discussions and decisions, as well as somewhat ambiguous attitudes regarding such practices. Notably, discrepancies emerged between different professional roles and, in particular, regions, underscoring the high variability of LST limitation-related procedures.
Conclusions
The findings highlight a pressing need for more straightforward guidelines, legal frameworks, support mechanisms, and communication strategies to navigate the complex terrain of rather burdensome end-of-life pediatric care, which is intrinsically loaded with profound ethical quandaries.
Keywords: pediatrics, intensive care, intensive care units, end-of-life, ethics, withholding, withdrawing, healthcare professionals
1. Introduction
In Western, high-income countries, most child and adolescent (pediatric) deaths take place within hospitals or, more precisely, intensive care units (ICUs) (1, 2). A significant part, if not the majority, of those deaths, occurs after withholding, non-escalation, or withdrawal of life-sustaining treatments (LST) (3–6). LST implies all medical interventions or procedures used to prolong life, that is, delay death regardless of the potential influence on underlying causes, which may or may not be present (7).
Therefore, despite advances in medical technologies and treatments that have improved overall survival rates and quality of life, a considerable subset of cases remain where available interventions are futile, shifting the focus from cure toward comfort and palliation (8, 9). The proper management of end-of-life issues is thus a critical component of (intensive) pediatric care.
In the emotionally charged environment of pediatric ICUs, healthcare professionals face multiple challenges as, while providing cure and care, they must also navigate the complexities of end-of-life decision-making (10, 11). Their attitudes and perspectives, influenced by factors such as demographics, professional roles, and social and cultural context, significantly impact the care provided (12–15). Given the importance, complexity, and substantial variability of end-of-life care in pediatric ICUs, understanding these attitudes and perspectives is essential for developing and adopting support mechanisms, guidelines, and policies aimed at optimizing end-of-life care.
End-of-life decision-making in Croatia may differ due to specific local factors, including those related to social, cultural, and healthcare systems. Croatia is the youngest member of the European Union (EU). However, despite being part of the EU since 2013, Croatia still inherits some features of the former socialist system it was part of, for example, corruption and mistrust in institutions (16). Croatia has a relatively homogenous population. According to the last census in 2021, the share of Croats in Croatia is 91.63% (17). Regarding religion, Christians make up 87.39% of its population 78.97 % of them being Catholics (17). The average age of the population is 44.3 years, which places Croatia among the oldest nations in Europe (while causes of aging are both negative natural increase rates and pronounced emigration (18).
Croatia has a public-private mix healthcare system, but still, most of the care for most of the population is provided within the public system, especially its clearly non-profitable segments, while more profitable ones are under pressure of commodification (19). Nominally, appropriate healthcare within the public system is accessible in Croatia, but there are marked differences in accessibility between rural and urban areas (20).
In Croatia, any kind of medically assisted dying, that is, euthanasia and assisted suicide, is forbidden by Criminal law. However, legal provisions regarding other segments of end-of-life care are rather fragmented. For example, anticipatory decision-making, like advance care directives (ACD), is de iure envisaged in the Family law but is de facto not implementable due to the lack of necessary additional legal provisions (21). In addition, by relevant laws, patients are granted the right to accept or refuse any given medical procedure, but only if it does not threaten their life and health. Put simply, despite their daily presence in a clinical context, the practices of LST limitation are not regulated by law in Croatia. Nonetheless, palliative care is considered an essential part of healthcare.
So far, several studies have dealt with end-of-life issues in Croatia, employing qualitative and quantitative methodologies. Research on public attitudes, without delineation between adult and pediatric applications, showed a rather low level of acceptance of LST limitation as well as euthanasia and assisted suicide (21). On the other hand, most Croatian ICU professionals consider the limitation of LST as ethically acceptable, although such practices are seemingly less often encountered than in most other countries (22). However, almost all previous studies found a high variability of both end-of-life attitudes and practices (22–24).
This study is part of a research project founded by the Croatian Science Foundation entitled “Values and Decisions at the End of Life” (VAL-DE-END), which aims to comprehensively investigate the values, attitudes, and experiences related to end-of-life practices in ICUs across Croatia.
This article reports findings from a cross-sectional survey of healthcare professionals working in pediatric ICUs in Croatia. It complements previous qualitative research and seeks to provide further insights into the particularities of end-of-life care in pediatric ICUs in this context (24). To the best of our knowledge, this is the first study of its kind in Croatia.
In line with the above, the main aim of this study is to explore further the delicate nuances of healthcare professionals’ experiences, challenges faced, and the strategies employed to manage these demanding yet critical aspects of pediatric care.
2. Methods
A cross-sectional study using a questionnaire was conducted. The target population was healthcare professionals (physicians and nurses) working in Croatia's pediatric ICUs (PICUs), encompassing both neonatal (NICUs) and PICUs. Participants were recruited from all such ICUs, excluding those from University Clinical Hospital Osijek as a result of the lack of ethical committee approval.
At the time of the study, Croatia had seven NICUs and five PICUs, all operating at the tertiary level within clinical hospitals (24). This comprised 72 physicians and 325 nurses as the overall target population. With the exclusion of Osijek, the eligible population was 64 physicians and 283 nurses.
This study used equal methodology in terms of questionnaire distribution and collection, as one was conducted among healthcare professionals working in adult ICUs in Croatia [and is reported in more detail in the study by Špoljar et al. (22)]. In short, questionnaires were distributed through ICU directors following thorough instructions from researchers. The directors locally coordinated distribution and collection, ensuring anonymity and voluntary participation. This process occurred between December 2018 and December 2019.
The questionnaire used was similar to one previously employed in a study on adult ICU healthcare professionals within the same research project. The questionnaire was only slightly adjusted, mainly in the introductory part concerning general data, for the pediatric ICU context to allow comparison between pediatric and adult ICU professionals.
The questionnaire, as previously discussed in more detail (22), was consensually coopted from its initial developers (25, 26), who previously used it in a nationwide sample of healthcare professionals working in adult ICU and pediatric ICU in Slovenia. The rationale for using that specific questionnaire relies on the fact that Slovenia and Croatia are neighboring countries that share a significant part of recent historical and current sociocultural context, thus allowing for a more straightforward comparison. Before applying to this research project, the questionnaire was doubly translated and back-translated, further adjusted, pilot-tested, and finally validated (22).
The translated survey questionnaire used in this study is available in the Supplementary Material (Supplementary Data Sheet 1, Survey Questionnaire).
3. Analysis
The statistical analysis was conducted using the Python programming language and JASP software (version 0.18.3). A comprehensive descriptive analysis was performed on the entire dataset. The primary dependent variables analyzed included professional role/status (dichotomized as physicians or nurses), years of professional experience, and geographic location (categorized as Zagreb, Rijeka, or Split). Although other variables were present in the questionnaire, they were excluded from the analysis due to either significant correlation with the primary variables (e.g., age and ICU-specific experience with overall professional tenure) or insufficient representation within certain categories (such as the male gender demographic). This decision was informed by both the research group's prior studies and established literature, indicating these selected variables as critical determinants. Continuous variables were described using statistical measures such as mean, median, standard deviation, and interquartile range where appropriate. Correlation analyses employed Pearson's r and Spearman's rho coefficients. Categorical variables were summarized by frequency counts (n) and percentages. Differences between two groups were assessed using the Mann–Whitney U-test, while the ANOVA and Kruskal–Wallis tests were applied for comparisons across more than two groups, incorporating Tukey's post hoc correction for multiple comparisons. A significance threshold was established at p ≤0.05.
4. Results
4.1. Characteristics of study participants
The study was conducted in six NICUs and four PICUs in five different hospitals (three from Zagreb and one each from Rijeka and Split). The response rate was 48% for physicians (31 out of 64 eligible) and 29% for nurses (82 out of 283 eligible), totaling 103 participants. The majority were female (92%), with 27.4% being physicians. Among the nurses, 32.7% had college degrees, 28.3% were high school graduates, and 11.5% held university degrees. The mean age of participants was 38.9 years (SD ±11.7), with a mean of 16.8 years of working experience (SD ±12.2). Most participants (n = 85, 8%) worked in the ICU regularly, with the largest group from Zagreb (58.4%).
All the other characteristics of study participants are presented in Table 1.
Table 1.
Characteristics of study participants.
| Frequency | Percent | ||
|---|---|---|---|
| Hospital | UCH Holy Spirit | 27 | 23.89 |
| UCH Zagreb | 32 | 28.31 | |
| UCH Sisters of Mercy | 7 | 6.19 | |
| UCH Split | 25 | 22.12 | |
| UCH Rijeka | 22 | 19.46 | |
| Region | Zagreb | 66 | 58.40 |
| Split | 25 | 22.12 | |
| Rijeka | 22 | 19.46 | |
| Gender | Female | 104 | 92.03 |
| Male | 9 | 7.96 | |
| Vocation | Nurse | 82 | 72.56 |
| Nurse-college graduate | 37 | 32.74 | |
| Nurse-high school graduate | 32 | 28.31 | |
| Nurse-university graduate | 13 | 11.50 | |
| Physician | 31 | 27.43 | |
| Type of work in ICU | Occasional | 16 | 14.15 |
| Regular | 97 | 85.84 | |
| Years of practice (as nurse of physician) | Median | 15 | |
| Standard deviation | 12.23 | ||
| Mean | 16.81 | ||
| Age | Median | 38 | |
| Standard deviation | 11.70 | ||
| Mean | 38.99 |
4.2. Experiences with LST limitation at designated ICUs
Approximately half of healthcare professionals reported that they do not attempt cardiopulmonary resuscitation (DNACPR) and that withholding LST decisions were made in their ICUs, although such decisions were fairly rare (41.6% and 42.5%, respectively). Over one-third indicated such decisions were never made.
The majority of healthcare professionals stated that decisions to withdraw artificial ventilation (58.4%), antibiotics (57.5%), endotracheal tube (71.7%), and hydration (83.2%) are never made. However, decisions to withdraw inotropes were more commonly encountered, albeit on rare occasions (37.2%).
Physicians reported more often experiences with withholding LST (U = 840.5; p < 0.001), withdrawing of artificial ventilation (U = 840.5; p = 0.066), and withdrawing inotropes (U = 712; p = 0.008).
A significant majority of healthcare professionals, three-quarters of them, reported never being involved in the LST limitation decision-making process, with notable differences between physicians (51.6% involvement) and nurses (9.8% involvement) (U = 629.5; p < 0.001).
Physicians were generally more often seen as the primary initiators of LST discussions (60.2%), and this was also more commonly reported by physicians themselves (U = 864; p = 0.038). LST limitation decision-making process predominantly involved physicians (73.4%), with a much lesser involvement of nurses (29.2%) and ethics committees (15%). Family members and/or legal guardians were frequently included in those decision-making processes (82.3% usually or always included).
In general, a significant minority (82.3%) never consulted ethics committees. Physicians reached out to ethics committees more often than nurses (29% vs. 13.4%), although this was not statistically significant. Knowledge about whom to contact for ethical dilemmas was limited, with only one-third of healthcare professionals knowing the appropriate contacts.
Compliance with DNACPR decisions is relatively high (63.7% always complied), while, expectedly, personal disagreement with LST limitation decisions was relatively low (44.2% never disagreed, 47.8% rarely disagreed).
Lack of consensus was rare among both physicians and family members (69.9%) and even more so among physicians themselves (77.9%). Physicians, however, more frequently reported a lack of consensus between physicians and family members/legal guardians (U = 849; p = 0.004).
Decisions were either not recorded or documented equally for DNACPR (38.1%) and LST limitations (35.4%). Nonetheless, it was implemented quickly once a decision was made (66.3%).
For more details on participants’ answers, refer to Table 2.
Table 2.
Experiences of healthcare professionals with LST limitation at designated ICUs: description and analysis according to vocation (nurses/physicians).
| Question | Answer | All, N (%) | Physician, N (%) | Nurse, N (%) | Mann–Whitney | |
|---|---|---|---|---|---|---|
| U | p | |||||
| I.11. Knowledge on whom to reach when encountering ethical dilemmas | 0a | 1 (0.9%) | 1 (3.2%) | 0 (0.0%) | ||
| No | 73 (64.6%) | 18 (58.1%) | 55 (67.1%) | |||
| Yes | 39 (34.5%) | 12 (38.7%) | 27 (32.9%) | |||
| I.12. Ever contacted ethical committee | No | 93 (82.3%) | 22 (71.0%) | 71 (86.6%) | ||
| Yes | 20 (17.7%) | 9 (29.0%) | 11 (13.4%) | |||
| II.1.1. Experiencing DNACPR decisions | 0a | 10 (8.8%) | 3 (9.7%) | 7 (8.5%) | 923.000 | 0.302 |
| Never | 44 (38.9%) | 9 (29.0%) | 35 (42.7%) | |||
| Rarely | 47 (41.6%) | 16 (51.6%) | 31 (37.8%) | |||
| Frequently | 12 (10.6%) | 3 (9.7%) | 9 (11.0%) | |||
| II.1.2. Experiencing withholding LST | 0a | 14 (12.4%) | 3 (9.7%) | 11 (13.4%) | 606.500 | <.001 |
| Never | 41 (36.3%) | 3 (9.7%) | 38 (46.3%) | |||
| Rarely | 48 (42.5%) | 22 (71.0%) | 26 (31.7%) | |||
| Frequently | 10 (8.8%) | 3 (9.7%) | 7 (8.5%) | |||
| II.1.3. Experiencing withdrawing of artificial ventilation | 0a | 10 (8.8%) | 3 (9.7%) | 7 (8.5%) | 840.500 | 0.066 |
| Never | 66 (58.4%) | 14 (45.2%) | 52 (63.4%) | |||
| Rarely | 30 (26.5%) | 11 (35.5%) | 19 (23.2%) | |||
| Frequently | 7 (6.2%) | 3 (9.7%) | 4 (4.9%) | |||
| II.1.4. Experiencing withdrawing of endotracheal tube | 0a | 10 (8.8%) | 3 (9.7%) | 7 (8.5%) | 985.500 | 0.506 |
| Never | 81 (71.7%) | 21 (67.7%) | 60 (73.2%) | |||
| Rarely | 16 (14.2%) | 4 (12.9%) | 12 (14.6%) | |||
| Frequently | 6 (5.3%) | 3 (9.7%) | 3 (3.7%) | |||
| II.1.5. Experiencing withdrawing of inotropes | 0a | 11 (9.7%) | 3 (9.7%) | 8 (9.8%) | 712.000 | 0.008 |
| Never | 48 (42.5%) | 7 (22.6%) | 41 (50.0%) | |||
| Rarely | 42 (37.2%) | 16 (51.6%) | 26 (31.7%) | |||
| Frequently | 12 (10.6%) | 5 (16.1%) | 7 (8.5%) | |||
| II.1.6. Experiencing withdrawing of antibiotics | 0a | 10 (8.8%) | 3 (9.7%) | 7 (8.5%) | 926.500 | 0.284 |
| Never | 65 (57.5%) | 15 (48.4%) | 50 (61.0%) | |||
| Rarely | 30 (26.5%) | 11 (35.5%) | 19 (23.2%) | |||
| Frequently | 8 (7.1%) | 2 (6.5%) | 6 (7.3%) | |||
| II.1.7. Experiencing withdrawing of hydration | 0a | 10 (8.8%) | 3 (9.7%) | 7 (8.5%) | 1,023.000 | 0.688 |
| Never | 94 (83.2%) | 25 (80.6%) | 69 (84.1%) | |||
| Rarely | 8 (7.1%) | 3 (9.7%) | 5 (6.1%) | |||
| Frequently | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| II.2. Recording of DNACPR decisions | 0a | 1 (0.9%) | 1 (3.2%) | 0 (0.0%) | 1,230.000 | 1.000 |
| No | 43 (38.1%) | 11 (35.5%) | 32 (39.0%) | |||
| In writing | 43 (38.1%) | 11 (35.5%) | 32 (39.0%) | |||
| Orally | 26 (23.0%) | 8 (25.8%) | 18 (22.0%) | |||
| II.3. Compliance with DNACPR decisions | 0a | 4 (3.5%) | 1 (3.2%) | 3 (3.7%) | 1,262.000 | 0.535 |
| Never | 16 (14.2%) | 4 (12.9%) | 12 (14.6%) | |||
| Rarely | 21 (18.6%) | 8 (25.8%) | 13 (15.9%) | |||
| Always | 72 (63.7%) | 18 (58.1%) | 54 (65.9%) | |||
| II.4. Recording of LST limitation decisions | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,059.500 | 0.177 |
| No instructions used | 40 (35.4%) | 9 (29.0%) | 31 (37.8%) | |||
| Oral instructions | 32 (28.3%) | 12 (38.7%) | 20 (24.4%) | |||
| Written instructions | 40 (35.4%) | 10 (32.3%) | 30 (36.6%) | |||
| II.5.1. Involvement in LST limitation decision-making | 0a | 5 (4.4%) | 2 (6.5%) | 3 (3.7%) | 629.500 | <.001 |
| No | 84 (74.3%) | 13 (41.9%) | 71 (86.6%) | |||
| Yes | 24 (21.2%) | 16 (51.6%) | 8 (9.8%) | |||
| II.6. Initiator of LST limitation discussions | 0a | 29 (25.7%) | 7 (22.6%) | 22 (26.8%) | 864.000 | 0.038 |
| Doctor + family/legal guardian | 4 (3.5%) | 1 (3.2%) | 3 (3.7%) | |||
| Doctor + nurse | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | |||
| Doctor's initiative | 68 (60.2%) | 23 (74.2%) | 45 (54.9%) | |||
| Family/legal guardian's initiative | 10 (8.8%) | 0 (0.0%) | 10 (12.2%) | |||
| II.7.2. LST limitation decision-making process includes physicians (ICU and others involved in treatment) | 0a | 8 (7.1%) | 0 (0.0%) | 8 (9.8%) | 1,307.500 | 0.229 |
| Strongly disagree | 13 (11.5%) | 5 (16.1%) | 8 (9.8%) | |||
| Disagree | 5 (4.4%) | 1 (3.2%) | 4 (4.9%) | |||
| Undecided | 4 (3.5%) | 1 (3.2%) | 3 (3.7%) | |||
| Agree | 38 (33.6%) | 14 (45.2%) | 24 (29.3%) | |||
| Strongly agree | 45 (39.8%) | 10 (32.3%) | 35 (42.7%) | |||
| II.7.3. LST limitation decision-making process includes physicians and nurses | 0a | 15 (13.3%) | 3 (9.7%) | 12 (14.6%) | 861.500 | 0.341 |
| Strongly disagree | 27 (23.9%) | 5 (16.1%) | 22 (26.8%) | |||
| Disagree | 18 (15.9%) | 5 (16.1%) | 13 (15.9%) | |||
| Undecided | 20 (17.7%) | 8 (25.8%) | 12 (14.6%) | |||
| Agree | 24 (21.2%) | 8 (25.8%) | 16 (19.5%) | |||
| Strongly agree | 9 (8.0%) | 2 (6.5%) | 7 (8.5%) | |||
| II.7.4. LST limitation decision-making process includes consultation of ethics committee | 0a | 13 (11.5%) | 2 (6.5%) | 11 (13.4%) | 1,129.500 | 0.426 |
| Strongly disagree | 43 (38.1%) | 13 (41.9%) | 30 (36.6%) | |||
| Disagree | 16 (14.2%) | 8 (25.8%) | 8 (9.8%) | |||
| Undecided | 24 (21.2%) | 3 (9.7%) | 21 (25.6%) | |||
| Agree | 7 (6.2%) | 3 (9.7%) | 4 (4.9%) | |||
| Strongly agree | 10 (8.8%) | 2 (6.5%) | 8 (9.8%) | |||
| II.8. Family members/legal guardians involvement in LST limitation decision-making | 0a | 1 (0.9%) | 1 (3.2%) | 1 (1.2%) | 1,114.000 | 0.411 |
| Never | 8 (7.1%) | 3 (9.7%) | 5 (6.1%) | |||
| Rarely | 10 (8.8%) | 1 (3.2%) | 9 (11.0%) | |||
| Usually | 43 (38.1%) | 10 (32.3%) | 33 (40.2%) | |||
| Always | 50 (44.2%) | 16 (51.6%) | 34 (41.5%) | |||
| II.11. Frequency of no consensus among physicians | 0a | 3 (2.7%) | 1 (3.2%) | 2 (2.4%) | 1,348.500 | 0.154 |
| Never | 11 (9.7%) | 5 (16.1%) | 6 (7.3%) | |||
| Rarely | 88 (77.9%) | 23 (74.2%) | 65 (79.3%) | |||
| Frequently | 11 (9.7%) | 2 (6.5%) | 9 (11.0%) | |||
| II.12. Frequency of no consensus among physicians and family members | 0a | 4 (3.5%) | 1 (3.2%) | 3 (3.7%) | 849.000 | 0.004 |
| Never | 17 (15.0%) | 0 (0.0%) | 17 (20.7%) | |||
| Rarely | 79 (69.9%) | 24 (77.4%) | 55 (67.1%) | |||
| Frequently | 13 (11.5%) | 6 (19.4%) | 7 (8.5%) | |||
| II.13. Disagreement with LST limitation decisions | 0a | 2 (1.8%) | 1 (3.2%) | 1 (1.2%) | 1,215.500 | 1.000 |
| Never | 50 (44.2%) | 13 (41.9%) | 37 (45.1%) | |||
| Rarely | 54 (47.8%) | 16 (51.6%) | 38 (46.3%) | |||
| Frequently | 7 (6.2%) | 1 (3.2%) | 6 (7.3%) | |||
| II.15. Time from decision to treatment withdrawal | 0a | 8 (7.1%) | 1 (3.2%) | 7 (8.5%) | ||
| Immediately | 10 (8.8%) | 2 (6.5%) | 8 (9.8%) | 1,211.000 | 0.486 | |
| Immediately after decision and family agreement | 65 (57.5%) | 18 (58.1%) | 47 (57.3%) | |||
| About 6 h | 13 (11.5%) | 5 (16.1%) | 8 (9.8%) | |||
| About 24 h | 12 (10.6%) | 4 (12.9%) | 8 (9.8%) | |||
| More than 24 h | 5 (4.4%) | 1 (3.2%) | 4 (4.9%) | |||
0 = Non-response to a given questionnaire item.
4.3. Attitudes and values regarding LST limitation
There was significant polarization in attitudes toward the ethical acceptability of LST limitation. Nearly half found it acceptable, while the other half had a completely opposite view. Physicians tended to find LST limitation more ethically acceptable than nurses, although this was not statistically significant.
DNACPR was viewed more favorably, although one-third found it unacceptable, especially among nurses (34.1%) compared to physicians (22.6%).
Participants were divided on whether there is an ethical difference between withholding and withdrawing of LST. Physicians were less likely to see a difference (16.1%) compared to nurses (41.5%), but again with a lack of statistical significance. Most professionals (83.9%) were undecided about the ethical acceptability of limiting hydration.
Participants were also divided in their evaluation of ethical differences between different kinds of end-of-life cases [namely, cases of brain-dead patients, terminal patients, and patients in a (irreversible) vegetative state]. At the same time, physicians were less prone than nurses to consider these cases as equal (25.8% vs. 41.5%). Prognostic certainty and finality of being brain-dead (as opposed to being terminal or in a vegetative state) were among the most often highlighted reasons for unequal evaluation of those cases. A thin majority of our participants (64.6%) considered LST limitation decision-making in pediatric and adult contexts as ethically equal, with nurses being more likely to see a difference (29.3% vs. 16.1%).
A significant majority (80.5%) believed competent patient verbal or written decisions should be respected, though a notable portion of physicians (22.6%) remained undecided. However, participants reported not being very often informed about the wishes of patients, family members, or legal guardians regarding LST limitation (43.4% rarely or very rarely informed).
Most participants, approximately three-quarters, found ACDs valuable and useful in the LST limitation context, although an almost equal share of them have yet to encounter one. Physicians valued ACDs more than nurses (83.3% vs. 69.5%).
Views on one's legal responsibility in the context of LST limitation were also somewhat divided. Physicians were split between feeling individually responsible (45.2%) and undecided (41.9%), while nurses were more evenly distributed between agreement, disagreement, and being undecided.
A detailed list of participants’ responses is shown in Table 3.
Table 3.
Attitudes of healthcare professionals regarding LST limitation at designated ICUs: description and analysis according to vocation (nurses/physicians).
| Question | Answer | All, N (%) | Physician, N (%) | Nurse, N (%) | Mann–Whitney | |
|---|---|---|---|---|---|---|
| U | p | |||||
| III.4. Ethical acceptability of LST limitation | Undecided | 7 (6.2%) | 1 (3.2%) | 6 (7.3%) | 1,113.000 | 0.255 |
| No | 53 (46.9%) | 13 (41.9%) | 40 (48.8%) | |||
| Yes | 53 (46.9%) | 17 (54.8%) | 36 (43.9%) | |||
| III.5. Ethical difference between withholding and withdrawing | Undecided | 32 (28.3%) | 12 (38.7%) | 20 (24.4%) | 1,285.000 | 0.926 |
| No | 39 (34.5%) | 5 (16.1%) | 34 (41.5%) | |||
| Yes | 42 (37.2%) | 14 (45.2%) | 28 (34.1%) | |||
| III.6. Ethical acceptability of DNACPR | Undecided | 11 (9.7%) | 4 (12.9%) | 7 (8.5%) | 1,211.000 | 0.661 |
| No | 35 (31.0%) | 7 (22.6%) | 28 (34.1%) | |||
| Yes | 67 (59.3%) | 20 (64.5%) | 47 (57.3%) | |||
| III.7. Ethical acceptability of limitation of hydration alongside limitation of LST | Undecided | 94 (83.2%) | 23 (74.2%) | 71 (86.6%) | 1,114.500 | 0.122 |
| No | 14 (12.4%) | 6 (19.4%) | 8 (9.8%) | |||
| Yes | 5 (4.4%) | 2 (6.5%) | 3 (3.7%) | |||
| III.8. Ethical equality of different end-of-life cases [brain dead, terminal, and patients in (irreversible) vegetative state] | Undecided | 26 (23.0%) | 11 (35.5%) | 15 (18.3%) | 1,417.500 | 0.315 |
| No | 42 (37.2%) | 8 (25.8%) | 34 (41.5%) | |||
| Yes | 45 (39.8%) | 12 (38.7%) | 33 (40.2%) | |||
| III.10. Ethical equality of LST limitation decision-making involving adult and pediatric patients | Undecided | 11 (9.7%) | 3 (9.7%) | 8 (9.8%) | 1,119.000 | 0.248 |
| No | 29 (25.7%) | 5 (16.1%) | 24 (29.3%) | |||
| Yes | 73 (64.6%) | 23 (74.2%) | 50 (61.0%) | |||
| III.13. Competent patient's expressed (verbally or written) decisions should be respected | Don't know | 20 (17.7%) | 7 (22.6%) | 13 (15.9%) | 1,451.500 | 0.092 |
| No | 2 (1.8%) | 2 (6.5%) | 0 (0.0%) | |||
| Yes | 91 (80.5%) | 22 (71.0%) | 69 (84.1%) | |||
| III.16. Frequency of being informed about patient or family wishes regarding LST limitation | 0a | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | 1,280.000 | 0.784 |
| Undecided | 10 (8.8%) | 2 (6.5%) | 8 (9.8%) | |||
| Very rarely | 7 (6.2%) | 2 (6.5%) | 5 (6.1%) | |||
| Rarely | 42 (37.2%) | 12 (38.7%) | 30 (36.6%) | |||
| Often | 39 (34.5%) | 13 (41.9%) | 26 (31.7%) | |||
| Very often | 13 (11.5%) | 2 (6.5%) | 11 (13.4%) | |||
| III.17. Usefulness of ACD in LST limitation decision-making | 0a | 3 (2.7%) | 0 (0.0%) | 3 (3.7%) | 1,199.000 | 0.853 |
| Undecided | 21 (18.6%) | 2 (6.5%) | 19 (23.2%) | |||
| Not useful at all | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| Not useful | 5 (4.4%) | 3 (9.7%) | 2 (2.4%) | |||
| Useful | 63 (55.8%) | 22 (71.0%) | 41 (50.0%) | |||
| Very useful | 20 (17.7%) | 4 (12.9%) | 16 (19.5%) | |||
| III.18. Frequency of encountering ACD | 0a | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | 1.787 | 0.077 |
| Never | 84 (74.3%) | 27 (87.1%) | 57 (69.5%) | |||
| Rarely | 26 (23.0%) | 4 (12.9%) | 22 (26.8%) | |||
| Often | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| III.19. Existence of (your) individual legal responsibility regarding LST limitation decisions and their implementation | 0a | 3 (2.7%) | 0 (0.0%) | 3 (3.7%) | 996.500 | 0.107 |
| Don't know | 34 (30.1%) | 13 (41.9%) | 21 (25.6%) | |||
| No | 32 (28.3%) | 4 (12.9%) | 28 (34.1%) | |||
| Yes | 44 (38.9%) | 14 (45.2%) | 30 (36.6%) | |||
0 = Non-response to a given questionnaire item.
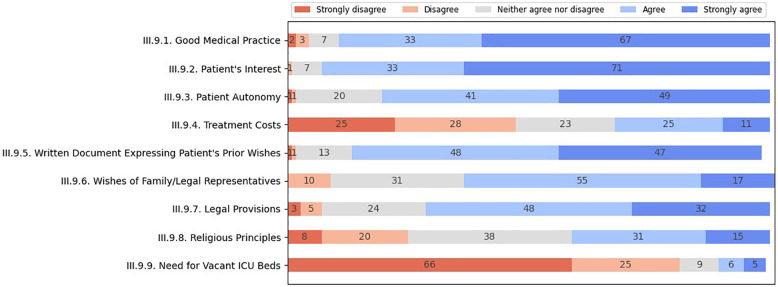
When determining the most critical considerations in LST limitation decision-making, healthcare professionals assigned the highest weight (agreeing and strongly agreeing) to the patient's best interest (94%), good medical practice (90%), respect for the patient's autonomy (90%), ACD (95%), legal regulations (80%), and respect for proxy or surrogate wishes (72%) (presented in Figure 1). Somewhat lesser weight was placed on respecting religious principles (46%). However, the religious and cultural beliefs of patients, family members, or legal representatives were considered more important (approximately 60% agreeing and strongly agreeing) than those of physicians (17% agreeing to a greater or lesser extent). Most participants disagreed with the need to consider treatment costs (53%), resource allocation matters (54%), and the need for vacant ICU beds (91%) in this context.
Figure 1.
Major considerations of healthcare professionals regarding LST limitation.
Nurses considered treatment costs (U = 1,508.5; p = 0.092), resource allocation, and need for free ICU beds (U = 1,623; p = 0.004) more relevant than did physicians, while physicians emphasized more the legal regulations (U = 988.5; p = 0.066) and the importance of the patient's interests (U = 1,004; p = 0.054). In addition, physicians were generally more prone than nurses to consider religious and cultural determinants as important (for everyone involved), although this finding did not reach statistical differences.
A more detailed list of participants’ responses is shown in Table 4.
Table 4.
Major considerations of healthcare professionals regarding LST limitation at designated ICUs: description and analysis according to vocation (nurses/physicians).
| Question | Answer | All, N (%) | Physician, N (%) | Nurse, N (%) | Mann–Whitney | |
|---|---|---|---|---|---|---|
| U | p | |||||
| III.9.1. Good medical practice | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,153.000 | 0.447 |
| Strongly disagree | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | |||
| Disagree | 3 (2.7%) | 1 (3.2%) | 2 (2.4%) | |||
| Undecided | 7 (6.2%) | 1 (3.2%) | 6 (7.3%) | |||
| Agree | 33 (29.2%) | 9 (29.0%) | 24 (29.3%) | |||
| Strongly agree | 67 (59.3%) | 20 (64.5%) | 47 (57.3%) | |||
| III.9.2. Patient's interest | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,004.000 | 0.054 |
| Disagree | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| Undecided | 7 (6.2%) | 1 (3.2%) | 6 (7.3%) | |||
| Agree | 33 (29.2%) | 6 (19.4%) | 27 (32.9%) | |||
| Strongly agree | 71 (62.8%) | 24 (77.4%) | 47 (57.3%) | |||
| III.9.3. Patient's autonomy | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,121.000 | 0.348 |
| Strongly disagree | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| Disagree | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| Undecided | 20 (17.7%) | 4 (12.9%) | 16 (19.5%) | |||
| Agree | 41 (36.3%) | 12 (38.7%) | 29 (35.4%) | |||
| Strongly agree | 49 (43.4%) | 15 (48.4%) | 34 (41.5%) | |||
| III.9.4. Treatment costs | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,508.500 | 0.092 |
| Strongly disagree | 25 (22.1%) | 8 (25.8%) | 17 (20.7%) | |||
| Disagree | 28 (24.8%) | 11 (35.5%) | 17 (20.7%) | |||
| Undecided | 23 (20.4%) | 6 (19.4%) | 17 (20.7%) | |||
| Agree | 25 (22.1%) | 4 (12.9%) | 21 (25.6%) | |||
| Strongly agree | 11 (9.7%) | 2 (6.5%) | 9 (11.0%) | |||
| III.9.5. ACDs | 0a | 3 (2.7%) | 1 (3.2%) | 2 (2.4%) | 1,232.000 | 0.817 |
| Strongly disagree | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| Disagree | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | |||
| Undecided | 13 (11.5%) | 4 (12.9%) | 9 (11.0%) | |||
| Agree | 48 (42.5%) | 14 (45.2%) | 34 (41.5%) | |||
| Strongly agree | 47 (41.6%) | 12 (38.7%) | 35 (42.7%) | |||
| III.9.6. Wishes of family/legal representatives | Disagree | 10 (8.8%) | 4 (12.9%) | 6 (7.3%) | 1,310.000 | 0.789 |
| Undecided | 31 (27.4%) | 7 (22.6%) | 24 (29.3%) | |||
| Agree | 55 (48.7%) | 16 (51.6%) | 39 (47.6%) | |||
| Strongly agree | 17 (15.0%) | 4 (12.9%) | 13 (15.9%) | |||
| III.9.7. Legal regulations | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 988.500 | 0.066 |
| Strongly disagree | 3 (2.7%) | 0 (0.0%) | 3 (3.7%) | |||
| Disagree | 5 (4.4%) | 2 (6.5%) | 3 (3.7%) | |||
| Undecided | 24 (21.2%) | 2 (6.5%) | 22 (26.8%) | |||
| Agree | 48 (42.5%) | 16 (51.6%) | 32 (39.0%) | |||
| Strongly agree | 32 (28.3%) | 11 (35.5%) | 21 (25.6%) | |||
| III.9.8. Religious principles | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,162.500 | 0.533 |
| Strongly disagree | 8 (7.1%) | 0 (0.0%) | 8 (9.8%) | |||
| Disagree | 20 (17.7%) | 7 (22.6%) | 13 (15.9%) | |||
| Undecided | 38 (33.6%) | 10 (32.3%) | 28 (34.1%) | |||
| Agree | 31 (27.4%) | 10 (32.3%) | 21 (25.6%) | |||
| Strongly agree | 15 (13.3%) | 4 (12.9%) | 11 (13.4%) | |||
| III.9.9. Need for vacant ICU beds | 0a | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | 1,623.000 | 0.004 |
| Strongly disagree | 66 (58.4%) | 25 (80.6%) | 41 (50.0%) | |||
| Disagree | 25 (22.1%) | 4 (12.9%) | 21 (25.6%) | |||
| Undecided | 9 (8.0%) | 1 (3.2%) | 8 (9.8%) | |||
| Agree | 6 (5.3%) | 1 (3.2%) | 5 (6.1%) | |||
| Strongly agree | 5 (4.4%) | 0 (0.0%) | 5 (6.1%) | |||
| III.11. Resource allocation considerations | 0a | 4 (3.5%) | 1 (3.2%) | 3 (3.7%) | 1,319.500 | 0.347 |
| Not important at all | 32 (28.3%) | 9 (29.0%) | 23 (28.0%) | |||
| Not important | 29 (25.7%) | 11 (35.5%) | 18 (22.0%) | |||
| Undecided | 29 (25.7%) | 6 (19.4%) | 23 (28.0%) | |||
| Important | 16 (14.2%) | 4 (12.9%) | 12 (14.6%) | |||
| Very important | 3 (2.7%) | 0 (0.0%) | 3 (3.7%) | |||
| III.14. Different religious/cultural beliefs of patient or legal representative | 0a | 1 (0.9%) | 0 (0.0%) | 1 (1.2%) | 1,379.000 | 0.378 |
| Strongly disagree | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | |||
| Disagree | 8 (7.1%) | 4 (12.9%) | 4 (4.9%) | |||
| Undecided | 35 (31.0%) | 9 (29.0%) | 26 (31.7%) | |||
| Agree | 59 (52.2%) | 18 (58.1%) | 41 (50.0%) | |||
| Strongly agree | 8 (7.1%) | 0 (0.0%) | 8 (9.8%) | |||
| III.15. Different religious/cultural beliefs of physician | 0a | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | 1,398.500 | 0.281 |
| Strongly disagree | 34 (30.1%) | 14 (45.2%) | 20 (24.4%) | |||
| Disagree | 34 (30.1%) | 6 (19.4%) | 28 (34.1%) | |||
| Undecided | 23 (20.4%) | 4 (12.9%) | 19 (23.2%) | |||
| Agree | 18 (15.9%) | 7 (22.6%) | 11 (13.4%) | |||
| Strongly agree | 2 (1.8%) | 0 (0.0%) | 2 (2.4%) | |||
0 = Non-response to a given questionnaire item.
4.4. Analysis by regional and professional experience differences
4.4.1. Regional differences
Healthcare professionals from Rijeka reported significantly greater experience with DNACPR decisions than those from Zagreb (p = 0.002) and more experience with LST withholding than those from Split (p = 0.034). There was no difference in participants’ experience with the withdrawal of various procedures (namely, mechanical ventilation, inotropes, and hydration) apart from antibiotics withdrawal, which was more often encountered in Split than in Zagreb (p = 0.034).
Recording of DNACPR orders is more often in Rijeka than both in Zagreb (p = 0.019) and Split (p = 0.010), while compliance with these orders is greater in Rijeka than in Split (p = 0.045). Participants from Split were less likely to report a lack of consensus among physicians (p < 0.001 compared to Zagreb; p = 0.019 compared to Rijeka). Professionals from Rijeka were more aware of whom to contact for ethical dilemmas (p < 0.001 than Zagreb; p = 0.021 than Split) and more often consulted ethics committees (p = 0.009 than Zagreb; p = 0.008 than Split).
Participants from both Rijeka (p = 0.007; p = 0.021) and Split (p = 0.026, p = 0.003) were more likely to consider the limitation of LST and DNACPR as ethically acceptable than those from Zagreb. Participants from Split viewed the limitation of hydration as acceptable and highlighted their individual responsibility more often than participants from Rijeka (in both cases, p = 0.020).
Healthcare providers from Rijeka were more likely than providers from both Zagreb (p < 0.001; p = 0.001) and Split (p = 0.013; p = 0.029) to highlight treatment costs and the need for free ICU beds as important considerations. In relation to participants from Zagreb, participants from Rijeka were also more likely to highlight the importance of wishes from family members (and legal representatives) (p = 0.008), religious principles (p = 0.011), physicians’ religious and cultural beliefs (p = 0.003), and resource allocation considerations (p = 0.013). However, professionals from Zagreb placed a greater emphasis on legal regulations than Rijeka (p = 0.006) and less on patients’ or legal representatives’ religious and cultural beliefs than professionals from both Rijeka (p = 0.006) and Split (p = 0.002).
A more detailed list of responses by regional differences is available in the Supplementary Material (Supplementary Table 1).
4.4.2. Professional experience differences
More experienced healthcare professionals were more aware of whom to contact when encountering ethical dilemmas (p = 0.012), were less likely to comply with DNACPR orders (p = 0.003), highlighted the importance of legal regulations (p = 0.048), highlighted the need to respect different religious/cultural beliefs of patients or representatives (p = 0.014), perceive adult and pediatric LST limitation context as equal (p = 0.048), and consider ACD as a useful tool (p = 0.004).
A more detailed list of responses by professional experience differences is available in the Supplementary Material (Supplementary Table 2).
5. Discussion
This study represents the investigation into the experiences, attitudes, and significant considerations of professionals in Croatian pediatric ICUs regarding end-of-life care. Several main findings can be drawn from this study, and they will be discussed further.
5.1. Commonness and views on ethics of LST limitation in Croatian pediatric ICUs
The findings indicate that limitations of LST, including both withdrawing and withholding, are considerably less common than in other countries. For example, in “Western” high-income countries, 40%–70% of deaths within pediatric ICUs occur after withholding or withdrawing LSTs (3, 5, 6, 27). These findings align with previous findings from a survey of healthcare professionals from adult ICUs in Croatia (22).
However, it seems that this trend is even more prominent in Croatian pediatric ICUs as DNACPR, withholding, and, to a lesser extent, LST withdrawing are even less common than in Croatian adult ICUs for example, 40% vs. 19.2% for DNACPR and 36.3% vs. 24.2% for withholding (22). This is a rather interesting finding, as such a difference between adult and pediatric ICUs was not to be expected based on findings from previous studies from (3, 6, 13, 14) for pediatric and (27–29) for adult settings.
There is an unusual contrast between Croatian adult and pediatric ICU professionals also regarding their views on the ethical acceptability of DNACPR and LST limitations. Only approximately half of pediatric ICU professionals view these practices as acceptable compared to two-thirds in adult ICUs (22). When compared to findings from other countries, these findings are pretty surprising. For example, a vast majority of Slovene pediatricians consider the limitation of LST as ethically acceptable (26), and similar findings can be found elsewhere (12, 30, 31).
Nonetheless, Croatian adult and pediatric ICU professionals share their ambivalence when evaluating ethical differences between withholding and withdrawing LST (22). The nearly equal split of opinions, contrary to the most common ethical standpoints (7, 32), mirrors the findings from other similar studies (26, 31).
5.2. Possible reasons for differences found between Croatian adult and pediatric ICU settings
Previously outlined findings, putting aside possible broader influences, might reflect the fact that there are indeed some significant differences between adult and pediatric end-of-life contexts. Pediatric patients are generally more diverse and complex while also less able to exercise autonomy. This makes healthcare providers more reliant on proxy decision-makers but also highlights the imperative of the primacy of patients’ best interests (33, 34). However, determining the patient's best interest might be quite ambiguous, especially in complex cases burdened with prognostic uncertainty when possible treatments often fall between being clearly beneficial and clearly futile (24, 34). Recent studies also indicate essential differences in end-of-life care considerations between different types of pediatric ICUs—between NICUs and PICUs, as decisions in NICUs are more often based on quality-of-life while in PICUs on survival likelihood considerations (33, 35, 36). Interestingly enough, and quite contrary to what was just mentioned, participants from this study were not likely to characterize differences between adult and pediatric end-of-life contexts as decisive.
5.3. Possible reasons for lower acceptance rates and lesser experience with LST limitation practices in Croatia
Empirical evidence stresses the importance of many influences on end-of-life perspectives and practices. Besides those case or patient, patient representative, and healthcare provider related, they also include organizational, cultural, and, more broadly speaking, social (21, 31, 37, 38). As mentioned, several recent studies on end-of-life issues in Croatia outlined somewhat more “traditional” views compared to other countries. It's important to emphasize that the term “traditional” is not intended to be pejorative but rather to highlight the connection to more classical and even Hippocratic perspectives on the discussed issues. Studies on the public revealed a rising but still quite low level of acceptance (21). These views are significantly influenced by factors such as age, education, place of residence, and political orientation. In short, younger, more educated, more liberal in their political orientation, and those from urban settings showed a greater level of acceptance of LST limitation as well as euthanasia and assisted suicide (21). Croatian ICU healthcare professionals showed a greater level of acceptance, but both levels of acceptance and actual experience with the limitation of LST are still lower than in other countries (22). Possible reasons already stated from previous Croatian studies are more paternalistic and conservative predilections, ambiguity and vagueness of legal context, and lack of clinical and professional guidelines (21–24, 39). Similarly, Devictor et al. (40), based on findings from landmark pediatric end-of-life studies, also highlighted possible influences of broader ex-communist Eastern European sociocultural factors. This study strongly reaffirms all previous findings while, as previously discussed, adding an additional layer of complexity due to observed marked differences between adult and pediatric contexts.
5.4. Decision-makers and decision-making values and processes
Family members or other patient representatives are frequently involved in LST limitation decision-making processes, similar to findings from many other studies (31, 41, 42). However, healthcare professionals are rarely informed about proxy decision-makers’ wishes, and ACDs, although valued, are seldom encountered. These findings combined point to the possible challenges of the true involvement of both patients and their representatives in decision-making. This might be reminiscent of a more general ambiguity of legal context, as surveyed professionals generally emphasized the importance of the principle of respecting autonomy. On the other hand, specific paternalistic stances of healthcare professionals can also be here at play, as already illustrated by previous studies within the Croatian healthcare context (43, 44). Indeed, when evaluating most important end-of-life considerations, surveyed professionals placed a somewhat higher value on patients’ best interest and good medical practice than on the respect for autonomy. In addition, although generally rare, a lack of consensus was more often perceived between patient representatives and physicians as primary discussion initiators and decision-makers. All the above may be further complicated by expected limited health literacy in the Croatian population, disproportionally affecting those already “worse off” (45). This was also evident from a previous qualitative study in the same settings, where Croatian healthcare professionals highlighted barriers to patient representatives' true awareness, informedness, and disagreements, especially regarding the futility of certain procedures (24). Of note, the Family Act, the primary regulation concerning professional-child-parent/representative interactions in the context of Croatian healthcare, allows special non-litigious court procedures aimed at protecting a child's welfare when discrepancies in opinion between critical decision-makers (child aged over 16 years, representative, or physician) are present.
Nonetheless, nurses in Croatian pediatric ICUs are strikingly less involved in LST limitation decision-making, including initiation and contribution to discussions. This finding aligns with similar ones elsewhere but raises concerns given the crucial role of nurses in end-of-life care (12, 31, 46–48). Previous qualitative research in the same setting indicated that nurses emphasized interprofessional relationships, while physicians were focused more on intra-professional dynamics (24). The same study also found nurses’ contributions to be “highly valued, facilitated, and appreciated” (24). However, other studies in a Croatian healthcare context, as well as elsewhere, also pointed out a rather strict internal (between different medical specializations) and external (between different healthcare professionals) hierarchical structure, contributing to numerous challenges on the many different levels of the healthcare system (49). This is of great importance as discrepancies between perceptions of nurses and physicians are, despite not being uncommon, identified as one of the greatest barriers in delivering appropriate end-of-life care (14, 50).
When decisions in Croatian pediatric ICUs are finally reached, they are enacted almost immediately but without the presence of any written instructions, as they are either absent or only verbal. These particular findings, while reaffirming previous ones, might be a reflection of the lack of not only clear national guidelines but also policies, that is, legal regulations (22, 24, 51).
5.5. Differences by region within Croatia: possible explanations
A significant finding of this study is great variability among different regions, represented by major cities: Zagreb, Rijeka, and Split, both in terms of experiences with, attitudes towards, and primary considerations underpinning LST limitation. If the most relevant regional differences are summed up, professionals from Rijeka have greater acceptance and more experience with LST limitation practices than those from Split and Zagreb.
This is in line with previous local and global findings. Previous research in Croatia on end-of-life issues signaled significant variability in decision-making determinants, processes, and related practices (22–24), and similar findings can also be found elsewhere. High variability is quite certainly a reflection of the complexity of the issue at hand, being influenced by numerous, more or less proximal, factors, but is also a quite straightforward argument for actions aimed at optimization (31, 37, 38). Findings on high variability from this study as Croatia is a relatively small country, with a population, according to the last Census in 2021, of 4,047,680 residents with a relatively ethnically homogenous structure (16, 21), might point toward the importance of organizational/institutional factors. This may also be supported by findings from survey on Croatian adult ICU professionals, which showed significant influences of types of ICUs and their broader hospital context on end-of-life practices (22). Another possible explanation might be the more nuanced social and cultural differences between these regions. However, even in cultural terms, Croatia seems to be rather homogenous—differences are not sufficient to form distinct regional profiles, while regions themselves are not well defined only by geographical characteristics (52). Nonetheless, more experience with and higher acceptance of LST limitation by professionals from Rijeka might potentially be explained by relative proximity, in an actual and metaphoric sense, to Italy and Slovenia, as their perspectives on end-of-life issues seem to be more inclined to those of their fellow neighbors and “Western” countries in general.
5.6. “Meta-finding” of high ambiguity
Another important “meta-finding” from this study, also present in similar studies performed in Croatia including both professionals and the public (21, 22), is a notable share of responses that reflect profound ambivalences regarding end-of-life issues. This ambivalence, seen in high rates of “undecided” answers, may stem from the broader sociocultural context (15, 53). After all, it is certainly not a matter of mere coincidence that in Croatia, the established legal frame for withholding and withdrawing is still non-existent. It is as if all are turning a blind eye, failing to recognize that sometimes one can do more harm than good simply by doing everything one can do. By its advances, medicine allows many great things, many of which have recently been unprecedented. However, that does not automatically mean that these “things” are always good nor beneficial. They can also be futile, utterly disproportionate in terms of expected outcomes. However, and here lies the great trouble; such interventions can also lie somewhere in between. The only way to determine their value in some instances and contexts is through truly shared decision-making (34, 42, 54–56). This is then the only proper way to make not only the right, but also the good decision, one with which each of the persons involved can be, at best, satisfied while at least at peace (49, 55, 57).
5.7. A possible way forward
Some of the previously emphasized Croatia specific influences are more or less modifiable. What seems to be the easiest solution, while clearly within professional responsibilities, is the creation of comprehensive end-of-life guidelines.
The recent publication of “Guidelines for improving quality of palliative care in intensive medicine” by the Ministry of Healthcare in Croatia is undoubtedly a positive step (available at: https://zdravstvo.gov.hr/UserDocsImages/dokumenti/Tekstovi%20razni/Smjernice%20za%20unaprje%C4%91enje%20kvalitete%20palijativne%20skrbi%20u%20intenzivnoj%20medicini_online%20verzija.pdf). However, even here, one can sense a great caution in this (“top-down”) approach by examining the guidelines’ very title. It may come as no surprise that most physicians (intensivists) still do not apply these guidelines, mainly due to the fears stemming from the lack of legal protection and misperceptions from colleagues and family members (51).
This again stresses the importance of the broader legal framework, also a factor that is, at least in principle, modifiable, while also, one could argue, falling within professional responsibilities (49). However, the legal system is largely reflective of a broader sociocultural context. Then again, a lot still needs to be done, primarily in terms of raising the overall health literacy. These are all reinforcing issues, as physicians are less likely to give patients more authority in a setting without clear legal regulations (31).
Due to widespread possibilities of misperceptions, support mechanisms should be implemented, especially as a previous study emphasized the high burden associated with pediatric end-of-life care in this setting, having a great influence both on the personal and professional lives of professionals (24).
Nevertheless, given many “unknowns” are still present, further exploration of fine nuances influencing this critical aspect of pediatric care is needed, as their exploration is crucial for tailoring intervention and policies to this rather specific local context.
5.8. Limitations
This study used a quantitative method—a questionnaire—adopted from previous Slovenian studies, slightly adjusted, and pilot-tested. In that sense, limitations are all those related using such methodology, just to name a few: lack of in-depth insights, recency bias, and social desirability bias. The latter might be of great importance here as the topic is, as many of the findings also suggest, still rather controversial. That is why we used a specific method of approaching potential participants (through immediate colleagues) and emphasized anonymity. In addition, as mentioned earlier, this study is part of the larger research project and, as such, complements findings from other sources and those collected through other research means and methodologies.
Another limitation is the nature of sampling, which could introduce selection bias. In addition, the generalizability of findings from this study might be limited because one potential site (University Clinical Hospital Osijek) did not participate. Further, the response rate, especially in the nurses’ section, is rather low. There are, however, good reasons for that. First, we calculated the response rate in relation to the total eligible population of healthcare professionals—all those working in Croatian pediatric ICUs except Osijek. In other words, not all eligible population members were actually reached (for example, because of absence from work during the study period). Nurses also work in shifts more often, covering the whole day, which could have made them less reachable. Therefore, there is a significant gap between those eligible healthcare professionals and those who were included. All the above makes the yielded low response rate more tolerable (as it is, in essence, underestimated) with a more likely non-systematic (than systemic) influence on measured outcomes.
6. Conclusion
This study has illuminated the complexities of end-of-life care practices in pediatric intensive care units in Croatia. Through a comprehensive survey of healthcare professionals, valuable insights into the experiences, challenges, and primary ethical considerations faced by those at the very frontline of pediatric intensive care are provided. The picture it sketched could be better. It reaffirms significant variability in end-of-life decision-making processes and practices from previous studies. It also signals profound ambiguity of healthcare professionals’ related attitudes and beliefs and a need for mote experience with and involvement in such discussions and practices, especially on the part of nurses. The findings underscore the need for clearer guidelines, legal frameworks, improved support mechanisms, and enhanced communication strategies to navigate the complex ethical challenges of pediatric end-of-life care and decision-making. As Croatia moves toward establishing more defined policies, this research contributes to a deeper understanding of the nuanced nature of pediatric end-of-life, advocating for practices that prioritize compassionate, patient- and family-centered care, the wellbeing of everyone included, while above all, the professionals’ integrity and patients’ dignity.
Funding Statement
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This research was undertaken within the research project founded by the Croatian Science Foundation entitled “Values and Decisions at the End of Life” (VAL-DE-END) and by the Alliance4Life project (European Union's Horizon 2020 Research and Innovation Program: “Alliance for Life Sciences: From Strategies to Actions in Central and Eastern Europe”).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by School of Medicine University of Zagreb Ethical Committee and also by all other relevant ethical committees where the study was conducted. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MC: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. FR: Conceptualization, Data curation, Investigation, Resources, Writing – original draft, Writing – review & editing. AJ: Data curation, Formal Analysis, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing. MN: Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. BF-G: Conceptualization, Data curation, Formal Analysis, Investigation, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. JM: Conceptualization, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. KLT: Investigation, Methodology, Writing – original draft, Writing – review & editing. BP: Investigation, Methodology, Writing – original draft, Writing – review & editing. DS: Conceptualization, Data curation, Investigation, Project administration, Resources, Writing – original draft, Writing – review & editing. ŠG: Conceptualization, Data curation, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. SJ: Investigation, Methodology, Writing – original draft, Writing – review & editing. JV: Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. MKT: Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. AŠ: Data curation, Formal Analysis, Methodology, Resources, Writing – original draft, Writing – review & editing. AB: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1394071/full#supplementary-material
References
- 1.Pousset G, Bilsen J, Cohen J, Addington-Hall J, Miccinesi G, Onwuteaka-Philipsen B, et al. Deaths of children occurring at home in six European countries. Child Care Health Dev. (2010) 36(3):375–84. 10.1111/j.1365-2214.2009.01028.x [DOI] [PubMed] [Google Scholar]
- 2.Chang E, MacLeod R, Drake R. Characteristics influencing location of death for children with life-limiting illness. Arch Dis Child. (2013) 98(6):419–24. 10.1136/archdischild-2012-301893 [DOI] [PubMed] [Google Scholar]
- 3.Burns JP, Sellers DE, Meyer EC, Lewis-Newby M, Truog RD. Epidemiology of death in the PICU at five U.S. teaching hospitals. Crit Care Med. (2014) 42(9):2101–8. 10.1097/CCM.0000000000000498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meert KL, Keele L, Morrison W, Berg RA, Dalton H, Newth CJL, et al. End-of-life practices among tertiary care PICUs in the United States: a multicenter study. Pediatr Crit Care Med. (2015) 16:7. 10.1097/PCC.0000000000000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roth A, Rapoport A, Widger K, Friedman JN. General paediatric inpatient deaths over a 15-year period. Paediatr Child Health. (2017) 22:2. 10.1093/pch/pxx005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trowbridge A, Walter JK, McConathey E, Morrison W, Feudtner C. Modes of death within a children’s hospital. Pediatrics. (2018) 142(4):e20174182. 10.1542/peds.2017-4182 [DOI] [PubMed] [Google Scholar]
- 7.Sprung CL, Truog RD, Curtis JR, Joynt GM, Baras M, Michalsen A, et al. Seeking worldwide professional consensus on the principles of end-of-life care for the critically ill: the consensus for worldwide end-of-life practice for patients in intensive care units (WELPICUS) study. Am J Respir Crit Care Med. (2014) 190(8):855–66. 10.1164/rccm.201403-0593CC [DOI] [PubMed] [Google Scholar]
- 8.Orioles A, Morrison WE. Medical ethics in pediatric critical care. Crit Care Clin. (2013) 29(2):359–75. 10.1016/j.ccc.2012.12.002 [DOI] [PubMed] [Google Scholar]
- 9.Buang SNH, Loh SW, Mok YH, Lee JH, Chan YH. Palliative and critical care: their convergence in the pediatric intensive care unit. Front Pediatr. (2022) 10:907268. 10.3389/fped.2022.907268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sieg SE, Bradshaw WT, Blake S. The best interests of infants and families during palliative care at the end of life: a review of the literature. Adv Neonatal Care. (2019) 19(2):E9–14. 10.1097/ANC.0000000000000567 [DOI] [PubMed] [Google Scholar]
- 11.Zhong Y, Cavolo A, Labarque V, Gastmans C. Physician decision-making process about withholding/withdrawing life-sustaining treatments in paediatric patients: a systematic review of qualitative evidence. BMC Palliat Care. (2022) 21(1):113. 10.1186/s12904-022-01003-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burns JP, Mitchell C, Griffith JL, Truog RD. End-of-life care in the pediatric intensive care unit: attitudes and practices of pediatric critical care physicians and nurses. Crit Care Med. (2001) 29(3):658–64. 10.1097/00003246-200103000-00036 [DOI] [PubMed] [Google Scholar]
- 13.Devictor DJ, Nguyen DT. Forgoing life-sustaining treatments in children: a comparison between northern and Southern European pediatric intensive care units. Pediatr Crit Care Med. (2004) 5(3):211–5. 10.1097/01.PCC.0000123553.22405.E3 [DOI] [PubMed] [Google Scholar]
- 14.Devictor DJ, Latour JM, EURYDICE II Study Group. Forgoing life support: how the decision is made in European pediatric intensive care units. Intensive Care Med. (2011) 37(11):1881–7. 10.1007/s00134-011-2357-3 [DOI] [PubMed] [Google Scholar]
- 15.Kirsch RE, Balit CR, Carnevale FA, Latour JM, Larcher V. Ethical, cultural, social, and individual considerations prior to transition to limitation or withdrawal of life-sustaining therapies. Pediatr Crit Care Med. (2018) 19(8S Suppl 2):S10–8. 10.1097/PCC.0000000000001488 [DOI] [PubMed] [Google Scholar]
- 16.Nikodem K, Ćurković M, Borovečki A. Trust in the healthcare system and physicians in Croatia: a survey of the general population. Int J Environ Res Public Health. (2022) 19(2):993. 10.3390/ijerph19020993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Croatian Bureau of Statistics. Population by Ethnicity and Religion, 2021 Census. Statistics in Line (2023). Available online at: https://podaci.dzs.hr/en/statistics/population/ (accessed June 20, 2024).
- 18.Croatian Bureau of Statistics. Average age of population, 1953–2021 Censuses. Statistics in Line (2023). Available online at: https://podaci.dzs.hr/en/statistics/population/ (accessed June 20, 2024).
- 19.Hodžić S, Vuković D, Muharemović A. The efficiency of healthcare system expenditures: evidence from Croatia. Ekon Vjesn. (2019) 32:361–71. [Google Scholar]
- 20.OECD/European Observatory on Health Systems and Policies. Croatia: Country Health Profile 2017. Brussels: State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies; (2017). 10.1787/9789264283312-en [DOI] [Google Scholar]
- 21.Borovecki A, Curkovic M, Nikodem K, Oreskovic S, Novak M, Rubic F, et al. Attitudes about withholding or withdrawing life-prolonging treatment, euthanasia, assisted suicide, and physician assisted suicide: a cross-sectional survey among the general public in Croatia. BMC Med Ethics. (2022) 23(1):13. 10.1186/s12910-022-00751-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Špoljar D, Vučić M, Peršec J, Merc V, Kereš T, Radonić R, et al. Experiences and attitudes of medical professionals on treatment of end-of-life patients in intensive care units in the republic of Croatia: a cross-sectional study. BMC Med Ethics. (2022) 23(1):12. 10.1186/s12910-022-00752-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ćurković M, Brajković L, Jozepović A, Tonković D, Župan Ž, Karanović N, et al. End-of-life decisions in intensive care units in Croatia—pre COVID-19 perspectives and experiences from nurses and physicians. J Bioeth Inq. (2021) 18(4):629–43. 10.1007/s11673-021-10128-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rubic F, Curkovic M, Brajkovic L, Nevajdic B, Novak M, Filipovic-Grcic B, et al. End-of-life decision-making in pediatric and neonatal intensive care units in Croatia—a focus group study among nurses and physicians. Medicina (Kaunas). (2022) 58(2):250. 10.3390/medicina58020250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Groselj U, Orazem M, Kanic M, Vidmar G, Grosek S. Experiences of Slovene ICU physicians with end-of-life decision making: a nation-wide survey. Med Sci Monit. (2014) 20:2007–12. 10.12659/MSM.891029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grosek S, Orazem M, Kanic M, Vidmar G, Groselj U. Attitudes of Slovene paediatricians to end-of-life care. J Paediatr Child Health. (2016) 52(3):278–83. 10.1111/jpc.13006 [DOI] [PubMed] [Google Scholar]
- 27.Wanders A, Ghinescu C, Levy-Jamet Y, Martin A-L, Barcos-Munoz F, Rimensberger P, et al. Circumstances surrounding end of life in a Swiss pediatric intensive care unit. Intensive Care Med. (2023) 112(5):e371. 10.1007/s44253-023-00005-2 [DOI] [Google Scholar]
- 28.Sprung CL, Cohen SL, Sjokvist P, Baras M, Bulow HH, Hovilehto S, et al. End-of-life practices in European intensive care units: the Ethicus Study. JAMA. (2003) 290(6):790–7. 10.1001/jama.290.6.790 [DOI] [PubMed] [Google Scholar]
- 29.Sprung CL, Ricou B, Hartog CS, Maia P, Mentzelopoulos SD, Weiss M, et al. Changes in end-of-life practices in European intensive care units from 1999 to 2016. JAMA. (2019) 322(17):1692–704. 10.1001/jama.2019.14608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanchez Varela AM, Johnson LM, Kane JR, Kasow KA, Quintana Y, Coan A, et al. Ethical decision making about end-of-life care issues by pediatric oncologists in economically diverse settings. J Pediatr Hematol Oncol. (2015) 37(4):257–63. 10.1097/MPH.0000000000000271 [DOI] [PubMed] [Google Scholar]
- 31.Zhong Y, Cavolo A, Labarque V, Gastmans C. Physicians’ attitudes and experiences about withholding/withdrawing life-sustaining treatments in pediatrics: a systematic review of quantitative evidence. BMC Palliat Care. (2023) 22(1):145. 10.1186/s12904-023-01260-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spoljar D, Curkovic M, Gastmans C, Gordijn B, Vrkic D, Jozepovic A, et al. Ethical content of expert recommendations for end-of-life decision-making in intensive care units: a systematic review. J Crit Care. (2020) 58:10–9. 10.1016/j.jcrc.2020.03.010 [DOI] [PubMed] [Google Scholar]
- 33.Fontana MS, Farrell C, Gauvin F, Lacroix J, Janvier A. Modes of death in pediatrics: differences in the ethical approach in neonatal and pediatric patients. J Pediatr. (2013) 162(6):1107–11. 10.1016/j.jpeds.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 34.Lantos JD. Ethical problems in decision making in the neonatal ICU. N Engl J Med. (2018) 379(19):1851–60. 10.1056/NEJMra1801063 [DOI] [PubMed] [Google Scholar]
- 35.Larcher V, Craig F, Bhogal K, Wilkinson D, Brierley J, Royal College of Paediatrics and Child Health. Making decisions to limit treatment in life-limiting and life-threatening conditions in children: a framework for practice. Arch Dis Child. (2015) 100(Suppl 2):s3–23. 10.1136/archdischild-2014-306666 [DOI] [PubMed] [Google Scholar]
- 36.Snoep MC, Jansen NJG, Groenendaal F. Deaths and end-of-life decisions differed between neonatal and paediatric intensive care units at the same children’s hospital. Acta Paediatr. (2018) 107(2):270–5. 10.1111/apa.14061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meñaca A, Evans N, Andrew EV, Toscani F, Finetti S, Gómez-Batiste X, et al. End-of-life care across Southern Europe: a critical review of cultural similarities and differences between Italy, Spain and Portugal. Crit Rev Oncol Hematol. (2012) 82(3):387–401. 10.1016/j.critrevonc.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 38.Mark NM, Rayner SG, Lee NJ, Curtis JR. Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Intensive Care Med. (2015) 41(9):1572–85. 10.1007/s00134-015-3810-5 [DOI] [PubMed] [Google Scholar]
- 39.Borovečki A, Nikodem K, Ćurković M, Braš M, Palić-Kramarić R, Špoljar D, et al. What constitutes a “good death”?—a representative cross-sectional survey among the general public in Croatia. Omega (Westport). (2023) 86(4):1415–31. 10.1177/00302228211010597 [DOI] [PubMed] [Google Scholar]
- 40.Devictor DJ, Tissieres P, Gillis J, Truog R. Intercontinental differences in end-of-life attitudes in the pediatric intensive care unit: results of a worldwide survey. Pediatr Crit Care Med. (2008) 9(6):560–6. 10.1097/PCC.0b013e31818d358 [DOI] [PubMed] [Google Scholar]
- 41.Akkermans AA, Lamerichs JMWJJ, Schultz MJM, Cherpanath TGVT, van Woensel JBMJ, van Heerde MM, et al. How doctors actually (do not) involve families in decisions to continue or discontinue life-sustaining treatment in neonatal, pediatric, and adult intensive care: a qualitative study. Palliat Med. (2021) 35(10):1865–77. 10.1177/02692163211028079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gillam L, Sullivan J. Ethics at the end of life: who should make decisions about treatment limitation for young children with life-threatening or life-limiting conditions? J Paediatr Child Health. (2011) 47(9):594–8. 10.1111/j.1440-1754.2011.02177.x [DOI] [PubMed] [Google Scholar]
- 43.Vučemilo L, Ćurković M, Milošević M, Mustajbegović J, Borovečki A. Are physician-patient communication practices slowly changing in Croatia?—a cross-sectional questionnaire study. Croat Med J. (2013) 54(2):185–91. 10.3325/cmj.2013.54.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vučemilo L, Borovečki A. Readability and content assessment of informed consent forms for medical procedures in Croatia. PLoS One. (2015) 10(9):e0138017. 10.1371/journal.pone.0138017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bobinac A. Access to healthcare and health literacy in Croatia: empirical investigation. Healthcare (Basel). (2023) 11(13):1955. 10.3390/healthcare11131955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Keenan HT, Diekema DS, O'Rourke PP, Cummings P, Woodrum DE. Attitudes toward limitation of support in a pediatric intensive care unit. Crit Care Med. (2000) 28(5):1590–4. 10.1097/00003246-200005000-00055 [DOI] [PubMed] [Google Scholar]
- 47.Beckstrand RL, Willmore EE, Macintosh JLB, Luthy KEB. Critical care nurses’ qualitative reports of experiences with physician behaviors, nursing issues, and other obstacles in end-of-life care. Dimens Crit Care Nurs. (2021) 40(4):237–47. 10.1097/DCC.0000000000000479 [DOI] [PubMed] [Google Scholar]
- 48.Zanin A, Brierley J, Latour JM, Gawronski O. End-of-life decisions and practices as viewed by health professionals in pediatric critical care: a European survey study. Front Pediatr. (2023) 10:1067860. 10.3389/fped.2022.1067860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ćurković M, Borovecki A. The Bridge Between Bioethics and Medical Practice: Medical Professionalism. Cham: Springer; (2022). [Google Scholar]
- 50.Keele L, Meert KL, Berg RA, Dalton H, Newth CJL, Harrison R, et al. Limiting and withdrawing life support in the PICU: for whom are these options discussed? Pediatr Crit Care Med. (2016) 17:2. 10.1097/PCC.0000000000000614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leventić V, Nešković N, Kvolik S, Kristek G, Škiljić S, Haršanji-Drenjančević I. Are we ready for end of life decisions in intensive medicine? Liječnički Vjesnik. (2023) 145(Suppl 4):60–6. (in Croatian). 10.26800/lv-145-supl4-14 [DOI] [Google Scholar]
- 52.Rajh E, Budak J, Anić ID. Hofstede’s culture value survey in Croatia: examining regional differences. Društvena Istraživanja. (2016) 25:309–27. 10.5559/di.25.3.02 [DOI] [Google Scholar]
- 53.Gómez-Vírseda C, de Maeseneer Y, Gastmans C. Relational autonomy in end-of-life care ethics: a contextualized approach to real-life complexities. BMC Med Ethics. (2020) 21(1):50. 10.1186/s12910-020-00495-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. (2017) 45(1):103–28. 10.1097/CCM.0000000000002169 [DOI] [PubMed] [Google Scholar]
- 55.Gómez-Vírseda C, de Maeseneer Y, Gastmans C. Relational autonomy: what does it mean and how is it used in end-of-life care? A systematic review of argument-based ethics literature. BMC Med Ethics. (2019) 20(1):76. 10.1186/s12910-019-0417-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Linebarger JS, Johnson V, Boss RD, Linebarger JS, Collura CA, Humphrey LM, et al. Guidance for pediatric end-of-life care. Pediatrics. (2022) 149(5):e2022057011. 10.1542/peds.2022-057011 [DOI] [PubMed] [Google Scholar]
- 57.Curkovic M, Kosec A. The ethics (mis)used for filling the voids or harm of harm reduction ethics. J Geriatr Oncol. (2020) 11(7):1168–9. 10.1016/j.jgo.2020.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.