Abstract
Aim
This study aimed to elucidate the risk of electric shock when the general public, not wearing Personal Protective Equipment (PPE), is in contact with a patient, and a defibrillation shock is inadvertently delivered.
Methods
A simulation study was conducted simulating the following scenarios. 1) Both the rescuer and the patient were isolated from the ground, with the rescuer making single-point contact with the patient. 2) Both the rescuer and the patient were in contact with the common ground, and the rescuer made single-point contact with the patient. 3) The rescuer made contact at two different points to the patient. A mannequin with a towel saturated with 3% saline solution placed on the chest was used. Defibrillation shocks were delivered using a defibrillator three times at each of three energies: 150 J, 200 J, and 360 J. The voltage across the simulated rescuer was measured with an oscilloscope.
Results
In Scenario 1, all measurements were below the detection limit. In Scenario 2, the voltage and current across the rescuer increased with higher defibrillation shock energy, averaging 156.8 V and 156.8 mA at 360 J. In Scenario 3, voltage peaked at 326.0 V and current at 326.0 mA at 360 J.
Conclusion
In a simulated setting of defibrillation, over 300 mA of current could pass through the rescuer without PPE when having two contact points between the manikin and the rescuer. However, due to the brief duration and low energy, immediate danger to the rescuer is considered low.
Keywords: Automated External Defibrillator, Basic Life Support, Cardiopulmonary Resuscitation, Electric Countershock, Out-of-Hospital Cardiac Arrest
Introduction
One concern arising when the general public uses Automated External Defibrillators (AEDs) is the risk of rescuers being exposed to electric shocks during contact with the patient. In recent years, the prevalence of fully automatic AEDs, which administer defibrillation shocks automatically, has increased alongside conventional AEDs, which require the rescuer to press a button to administer a shock. This trend has heightened awareness of the potential electric shock risks for rescuers employing AEDs.1 The administration of defibrillation shocks using AEDs constitutes a vital intervention at the core of Basic Life Support (BLS).2 Objectively assessing the risk of electric shock when the general public uses AEDs is important in the context of promoting BLS awareness.
Previous experimental studies on the risk of electric shock during defibrillation shock delivery have mainly concerned hands-on defibrillation in healthcare professionals wearing Personal Protective Equipment (PPE). Those studies concluded that uninterrupted manual chest compressions during defibrillation shock delivery are feasible.3, 4 However, there are notable differences between these studies and scenarios where the general public might use an AED in terms of the environmental context. Another study, specifically assessed leakage current during AED usage in a wet environment but solely concentrated on measuring electric potential during defibrillation shock implementation and neglected the consideration of a rescuer's presence.5 For example, when the general public engages in cardiopulmonary resuscitation (CPR), they may not wear PPE, such as gloves, and their exposed knees may come into contact with the ground, potentially acting as a grounding point. In these instances, if a defibrillation shock is inadvertently administered, there is a risk of a substantial electric current passing through the rescuer. However, there is a lack of research examining the risk of electric shock when non-PPE-wearing rescuers use AEDs, and the extent of the risk in such scenarios remains unclear.
To address this knowledge gap, we conducted a simulation study by simulating several scenarios involving the administration of defibrillation shocks. This study aimed to elucidate the risk of electric shock when the general public, not wearing PPE, is in contact with a patient, and a defibrillation shock is inadvertently delivered.
Methods
Study design
This study was a simulation study conducted in the Hiroshima International University research lab. This study did not involve the use of human subjects; therefore, it is not subject to review by the Ethics Committee of Hiroshima International University.
Study model
This study was conducted using the following model to simulate highly hazardous conditions:
-
1)
The impedance between the electrode pads was assumed to be 50 Ω.6
-
2)
To simulate conductive properties between the electrode pads and the patient's ground, each was bypassed with a resistance of 500 Ω.7
-
3)
The conductive properties of the rescuer were simulated with a 1 kΩ resistor.8
-
4)
The resistance of the dermis and stratum corneum was omitted.
-
5)
Current was assumed to flow near the body surface of the patient.
Scenarios
This study conducted experiments simulating the following three scenarios:
-
1)
Patient and rescuer are in contact at one point (rescuer’s hands are on chest), each isolated from the ground.
-
2)
Patient and rescuer are in contact at one point (rescuer’s hands are on chest), each connected to a common ground.
-
3)
Patient and rescuer are in contact at two points (rescuer’s hands are on chest and their knee is also touching the patient).
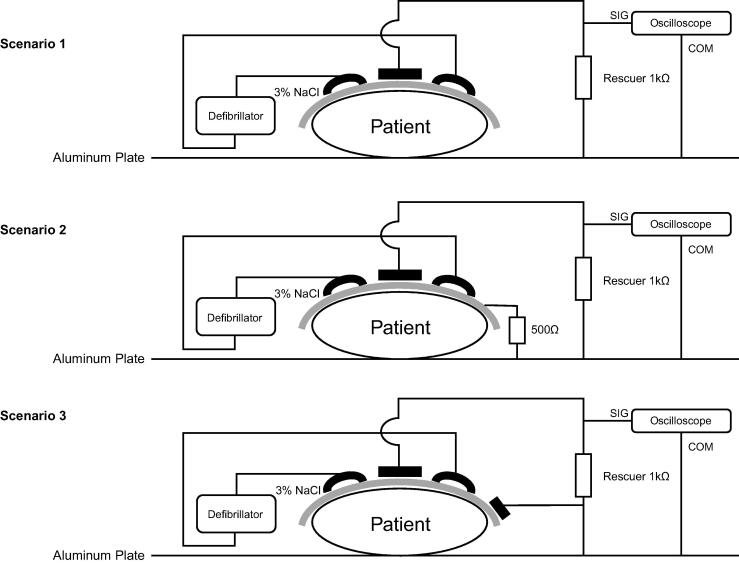
Each simulated scenario is illustrated in Fig. 1.
Fig. 1.
Three simulated scenarios conducted in this study. In scenario 1, an electrical shock was delivered to a patient isolated from the ground, with the rescuer making single-point contact (rescuer’s hands are on chest). In scenario 2, an electrical shock was delivered to a patient while both the rescuer and the patient were in contact with the common ground, and the rescuer made single-point contact with the patient (rescuer’s hands are on chest). In scenario 3, an electrical shock was delivered to a patient with the rescuer making contact at two different points (rescuer’s hands are on chest and their knee is also touching the patient). SIG, signal; COM, common.
Study protocol
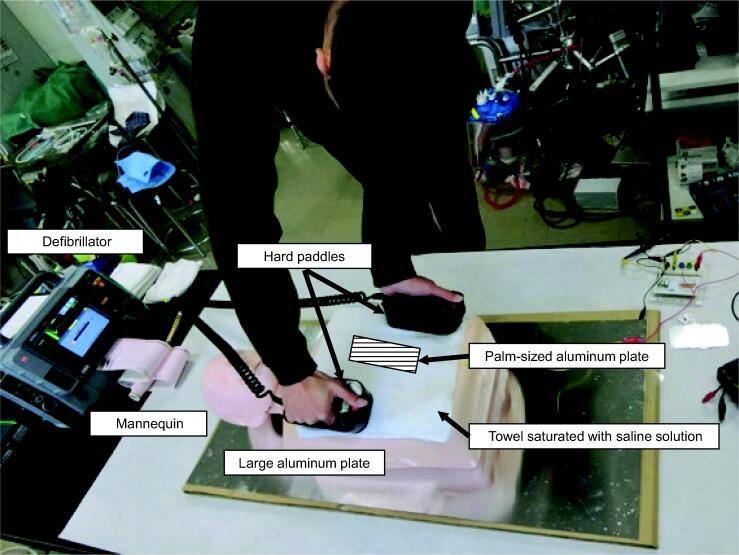
We used a mannequin (JAMY-P, YAGAMI Inc., Nagoya, Japan) as a simulated patient. Placing a towel saturated with saline solution on the mannequin's chest to replicate subcutaneous tissue. The saline concentration was set at 3%, which mimicked the human body's electrical characteristics (50 Ω). To measure alternating current impedance, an LCR meter (DE-5000, DER EE, New Taipei City, Taiwan) was used. A palm-sized aluminum plate (10 cm × 20 cm) was closely affixed to the towel, replicating a scenario where a rescuer is in contact with the patient. The electrode on this aluminum plate was connected to a resistor circuit with a 1 kΩ resistance, simulating the human body's resistance. The patient was positioned on a larger conductive aluminum plate. We reproduced a scenario where the patient was grounded by introducing a 500 Ω resistor between the larger aluminum plate and the towel (Scenario 2). Likewise, we simulated the condition of the patient being insulated from the ground by removing the 500 Ω resistor (Scenario 1). Another aluminum plate was attached to the towel to simulate a situation where the patient and rescuer are in contact at two different points (Scenario 3). We replicated a scenario where the rescuer was grounded by connecting the rescuer resistor circuit to the larger aluminum plate beneath the patient. The rescuer resistance circuit was linked to a storage oscilloscope (PicoScope 2205, Pico Technology Ltd., UK), and the voltage across the resistor was measured. A LIFEPAK 15 defibrillator (Stryker, USA) was used to deliver defibrillation shocks. Defibrillation shocks were delivered using hard paddles in manual mode, on the saline-soaked towel placed on the mannequin. The paddles were placed in the anterolateral position. One paddle was placed above the mannequin’s right nipple, just below the clavicle. The other paddle was placed below the mannequin’s left nipple, more to the side of the chest. We delivered defibrillation shocks avoiding direct contact with the smaller aluminum plate on the mannequin’s chest. Defibrillation shocks were delivered three times each at energies of 150 J, 200 J, and 360 J. The scene during defibrillation shock delivery is shown in Fig. 2.
Fig. 2.
The situation during the defibrillation shock.
Results
The summarised measurements for each scenario are presented in Table 1. In Scenario 1, all measurements were below the detection limit, regardless of the defibrillation shock energy setting. In Scenario 2, with an increase in defibrillation shock energy, both voltage and current measured at the rescuer rose, reaching an average of 156.8 V (current: 156.8 mA) at 360 J. The range of total energies delivered to the rescuer were 0.02 J to 0.07 J. The proportion of energy received by the rescuer in relation to the total energy generated by the defibrillator during shock delivery averaged 0.02%, regardless of the defibrillation shock energy. The duration of the shock to the rescuer was consistently within 10 ms for all instances. Scenario 3 exhibited similar trends, with the average voltage across the rescuer at 360 J reaching 326.0 V (current: 326.0 mA). The range of total energies delivered to the rescuer were 0.16 J to 0.32 J. The proportion of energy received by the rescuer to the total energy generated during defibrillation shock implementation ranged from 0.09% to 0.11%. The duration of the shock to the rescuer remained within 10 ms for all instances.
Table 1.
Summary of measurements.
| 1st | 2nd | 3rd | Mean | |
|---|---|---|---|---|
| Scenario 1 | ||||
| Below the detection limit. | ||||
| Scenario 2 | ||||
| 150 J | ||||
| Maximum voltage across rescuer, V | 97.7 | 60.1 | 61.9 | 73.2 |
| Maximum current through rescuer, mA | ||||
| Total energy, J | 0.04 | 0.01 | 0.02 | 0.02 |
| Proportion of energy*, % | 0.03 | 0.01 | 0.01 | 0.02 |
| 200 J | ||||
| Maximum voltage across rescuer, V | 98.6 | 94.1 | 96.8 | 96.5 |
| Maximum current through rescuer, mA | ||||
| Total energy, J | 0.04 | 0.04 | 0.03 | 0.04 |
| Proportion of energy*, % | 0.02 | 0.02 | 0.02 | 0.02 |
| 360 J | ||||
| Maximum voltage across rescuer, V | 155.9 | 164.0 | 150.5 | 156.8 |
| Maximum current through rescuer, mA | ||||
| Total energy, J | 0.08 | 0.08 | 0.06 | 0.07 |
| Proportion of energy*, % | 0.02 | 0.02 | 0.02 | 0.02 |
| Scenario 3 | ||||
| 150 J | ||||
| Maximum voltage across rescuer, V | 222.2 | 258.0 | 232.0 | 237.4 |
| Maximum current through rescuer, mA | ||||
| Total energy, J | 0.16 | 0.19 | 0.14 | 0.16 |
| Proportion of energy*, % | 0.11 | 0.13 | 0.09 | 0.11 |
| 200 J | ||||
| Maximum voltage across rescuer, V | 318.0 | 232.0 | 265.1 | 271.7 |
| Maximum current through rescuer, mA | ||||
| Total energy, J | 0.32 | 0.19 | 0.24 | 0.25 |
| Proportion of energy*, % | 0.16 | 0.10 | 0.12 | 0.13 |
| 360 J | ||||
| Maximum voltage across rescuer, V | 318.9 | 347.5 | 311.7 | 326.0 |
| Maximum current through rescuer, mA | ||||
| Total energy, J | 0.35 | 0.34 | 0.26 | 0.32 |
| Proportion of energy*, % | 0.10 | 0.09 | 0.07 | 0.09 |
Represents the fractional energy delivered to the rescuer arising from the electric potential difference on the rescuer between the two points of contact with the patient and/or common ground, calculated as the energy experienced by the rescuer/the total energy output of the defibrillator.
Discussion
In our experimental study, we examined the risk of electric shock for the general public without PPE when in contact with a patient, and an unintended defibrillation shock with an AED is delivered. Our findings revealed that as the defibrillation shock energy increased, both voltage and current measured at the rescuer also increased. Specifically, when a 360 J defibrillation shock was delivered to a patient, and the rescuer made contact at two different points on the patient, the maximum measured voltage reached 347.5 V. Furthermore, when the patient was isolated from the ground, all recorded measurements remained below the detection limit. This study models the rescuer as being in the “worst-case scenario”, given their lack of PPE and the assumption that the current primarily flows through the skin of the patient.
There are limited experimental studies on the risk of rescuers experiencing electric shock during the delivery of defibrillation shocks. Lyster et al. conducted a study where they attached an AED to a raw turkey using adhesive electrodes and placed it on a cement floor covered with either pool water or salt water.5 They measured the voltage that a rescuer might be exposed to at various points around the surrogate during the delivery of a defibrillation shock. The calculated current for a bystander reached a maximum of 14 mA in the pool water scenario and 30 mA in the saltwater scenario, both significantly lower than our obtained results. However, their study did not assess the effects of direct rescuer contact with a patient, limiting direct comparisons with our study, which assumes the rescuer is in contact with the patient. In another study by Lloyd et al., the leakage current through simulated rescuers was measured while they performed chest compressions on patients receiving external countershocks.3 The study found that currents ranging from 18.9 to 907 µA were observed in rescuers. While there are significant differences between the findings of our study and theirs, it is important to note that in their research, rescuers used polyethylene gloves, and specific conditions, such as the connection between the rescuer and the patient through ground resistance (120 Ω), might have created an environment less conducive to the flow of current through the rescuer. Although our study differs from these previous studies in the simulated environment, it builds on them, and extends the existing evidence by assessing risk through the simulation of a more hazardous situation for the rescuer.
The hazard of electrical shocks to rescuers during defibrillation can be understood by conceptualising the patient and rescuer as an electrical circuit. When delivering a defibrillation shock to a patient using defibrillation pads, the voltage applied across the chest generates an electric current within the patient's chest. Typically, the current moves between the pads, ensuring no risk to the rescuer as long as there is no direct contact with the patient. Yet, if a collateral circuit forms unintentionally through a rescuer, the total current between the pads splits into one part passing through the patient's chest and another through the rescuer. This division poses a potential risk of current flow to the rescuer. To establish a collateral rescuer circuit, the rescuer needs to make electrical contact with two points at different potentials. Hence, the values in Scenario 1 of the present experiment were below the detection limit likely because the patient was insulated, and the rescuer had only a single point of contact with the patient. As a result, no collateral circuit was formed, leading to almost no current flow to the rescuer.
In a typical cardiac arrest situation faced by the general public, numerous potential conductive pathways exist within the rescue environment.9 These pathways involve the patient, the rescuer, non-earthed conductive materials, and earth conductive materials. Any combination of these categories in contact with each other may form a circuit.10 In Scenarios 2 and 3, the establishment of collateral circuits caused current to flow through the rescuer. The magnitude of the current is contingent upon the voltage across the two points where the rescuer is in contact and the impedance at those specific points.10 In Scenario 3, where the rescuer had direct contact with the patient at two distinct points, the recorded value would have been higher due to the collateral circuit having the lowest total impedance. Furthermore, given the consistent impedance throughout this experiment, an increase in defibrillation energy corresponded to higher voltage and consequently, greater current flow to the rescuer.
In this study, currents exceeding 300 mA passed through the rescuer. However, the risk of harm to the rescuer from leakage current is likely minimal, even in the “worst-case scenario” where the current pathway involves the rescuer's heart. To induce fibrillation, a short duration electrical shock must coincide with the vulnerable period of the cardiac cycle.11 For healthy adults, it is estimated that up to 500 mA of current flow is needed to induce ventricular fibrillation (VF), even with well-timed shocks.12 Moreover, high voltage alone is not enough to cause harmful physiological effects. The voltage experienced with static electricity, often in the thousands of volts, is harmless due to the short duration of current flow, resulting in low associated current. In our study, the duration of the shock to the rescuer remained under 10 ms in all cases. For example, for a 10 ms pulse, current of up to 1000 mA delivered in the vulnerable cardiac period has less than 5% chance of causing fibrillation.13 Even if a current exceeding 300 mA were to pass through the rescuer, the extremely brief duration means that, as demonstrated by our findings, the total energy would be minimal, and the likelihood of the rescuer sustaining lethal damage is extremely low.
This study assumes ideal conditions for current flow through the rescuer. Therefore, the values obtained represent an approximation of the maximum current that could flow through the rescuer. The actual current is likely even lower. However, while the damage may be minimal, the risk of injury from electric shock cannot be completely dismissed. Electric shock could also potentially disrupt resuscitation efforts, such as interrupting chest compressions. Direct comparison with our results is not straightforward, it has been reported that at 10 kHz, people start to feel pain at 6–10 mA.14 While the risk of lethal damage from electric shock is low, rescuers may experience enough discomfort to interrupt chest compressions. To further reduce the risk of electric shock to rescuers, using insulating materials can be beneficial. For example, nitrile gloves, with a resistance of over 100kΩ,15 can increase the rescuer's impedance simply by wearing them, thus decreasing the current flowing through the rescuer.4 Additionally, insulating sheets can prevent the formation of collateral circuits, offering further protection against electric shock.
Even if an electrical shock were delivered while the general public, not wearing PPE, was in contact with a patient, it is highly unlikely to immediately endanger the rescuer's life. This assertion is supported by the absence of any reported cases where a rescuer or bystander suffered a life-threatening condition from an accidental electrical shock during a resuscitation procedure.9 However, adopting a more cautious approach, manufacturers should consider including insulating sheets and gloves in AED kits, and providing prompts through audio guidance to encourage glove usage. When using AEDs, the general public needs to follow the basic rule of not touching the patient during defibrillation shock delivery. Additionally, it is recommended to maintain insulation, such as by wearing gloves, to reduce the risk of electric shock.
The present study has several limitations. First, in this study, we used a mannequin to simulate the human body, but it did not replicate the unique low-frequency characteristics specific to humans. Consequently, if the experiment were conducted on real humans, the results might differ. Nevertheless, as this study intentionally assumes and simulates high-risk situations, the actual risks are expected to be lower than we report. Secondly, in this study, as intentional defibrillation shocks could not be delivered using adhesive pads, only a manual defibrillator with paddles was used to deliver defibrillation shocks. The reason for using paddles instead of pads is that the pads have an impedance measurement function. In this experiment, due to resistance issues, the defibrillator could not deliver the shock when using the pads because it did not recognize that the pads were properly attached. Therefore, there is a possibility that the conditions for delivering defibrillation shocks using pads might be different. Particularly, the use of paddles may have resulted in different contact resistance with the patient. Finally, in this study, we simulated the electrical characteristics of the human body (50 Ω) by using a towel soaked in a 3% saline solution. While we made consistent efforts to keep the impedance constant throughout the experiment, it is possible that variations in impedance could have impacted the results.
Conclusion
In a simulated setting of defibrillation, over 300 mA of current could pass through the rescuer without PPE when having two contact points between the manikin and the rescuer. However, due to the brief duration and low energy, immediate danger to the rescuer is considered low. It is recommended to avoid contact with the patient during defibrillation shock delivery. Furthermore, to address concerns about the risk of electric shock through contact, the use of insulating materials, such as gloves, might mitigate risk of electrical shock during defibrillation shock delivery.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Credit authorship contribution statement
Hisanori Kurosaki: Writing – review & editing, Writing – original draft. Shinji Ninomiya: Writing – review & editing, Methodology. Koichi Sasaki: Investigation. Yasuharu Yasuda: Supervision, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Hosmans T.P., Maquoi I., Vogels C., et al. Safety of fully automatic external defibrillation by untrained lay rescuers in the presence of a bystander. Resuscitation. 2008;77:216–219. doi: 10.1016/j.resuscitation.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 2.Theresa M.O., Federico S., Giuseppe R., et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation. 2021;161:98–114. doi: 10.1016/j.resuscitation.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd M.S., Heeke B., Walter P.F., Langberg J.J. Hands-on defibrillation: an analysis of electrical current flow through rescuers in direct contact with patients during biphasic external defibrillation. Circulation. 2008;117:2510–2514. doi: 10.1161/CIRCULATIONAHA.107.763011. [DOI] [PubMed] [Google Scholar]
- 4.Neumann T., Gruenewald M., Lauenstein C., Drews T., Iden T., Meybohm P. Hands-on defibrillation has the potential to improve the quality of cardiopulmonary resuscitation and is safe for rescuers-A preclinical study. J Am Heart Assoc. 2012;1 doi: 10.1161/JAHA.112.001313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyster T., Jorgenson D., Morgan C. The safe use of automated external defibrillators in a wet environment. Prehosp Emerg Care. 2003;7:307–311. doi: 10.1080/10903120390936473. [DOI] [PubMed] [Google Scholar]
- 6.Yasmine H., Daniela B., Christian B. A systematic review of the transthoracic impedance during cardiac defibrillation. Sensors (Basel) 2022;22:2808. doi: 10.3390/s22072808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Electrotechnical Commission. IEC 60601-2-2 Medical electrical equipment – Part 2-2: Particular requirements for the basic safety and essential performance of high frequency surgical equipment and high frequency surgical accessories (IDT). Geneva, Switzerland: International Electrotechnical Commission; 2017.
- 8.International Electrotechnical Commission. IEC 60601-1 Medical electrical equipment. General requirements for basic safety and essential performance. Geneva, Switzerland: International Electrotechnical Commission; 2005.
- 9.Hoke R.S., Heinroth K., Trappe H.J., Werdan K. Is external defibrillation an electric threat for bystanders? Resuscitation. 2009;80:395–401. doi: 10.1016/j.resuscitation.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Petley G.W., Cotton A.M., Deakin C.D. Hands-on defibrillation: theoretical and practical aspects of patient and rescuer safety. Resuscitation. 2012;83:551–556. doi: 10.1016/j.resuscitation.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan J.L., Chapman F.W. Will medical examination gloves protect rescuers from defibrillation voltages during hands-on defibrillation? Resuscitation. 2012;83:1467–1472. doi: 10.1016/j.resuscitation.2012.07.031. [DOI] [PubMed] [Google Scholar]
- 12.International Electrotechnical Commission. IEC 479-1 Effects of current on human beings and livestock – Part 1: General aspects. Geneva, Switzerland: International Electrotechnical Commission; 1994.
- 13.International Electrotechnical Commission. IEC 60479-2 Effects of current on human beings and livestock – Part 2: Special aspects. Geneva, Switzerland: International Electrotechnical Commission; 2019.
- 14.Chatterjee I., Wu D., Gandhi O.P. Human body impedance and threshold currents for perception and pain for contact hazard analysis in the VLF-MF band. IEEE Trans Biomed Eng. 1986;33:486–494. doi: 10.1109/TBME.1986.325735. [DOI] [PubMed] [Google Scholar]
- 15.Deakin C.D., Lee-Shrewsbury V., Hogg K., Petley G.W. Do clinical examination gloves provide adequate electrical insulation for safe hands-on defibrillation? I: resistive properties of nitrile gloves. Resuscitation. 2013;84:895–899. doi: 10.1016/j.resuscitation.2013.03.011. [DOI] [PubMed] [Google Scholar]