Abstract
Purpose
Since the Consensus Statement diffused by the Amsterdam Placental Workshop Group, knowledge of the meaning of placental vascular malperfusion has become essential in the unavoidable analysis of obstetrical history in a patient followed for autoimmune disease or any other maternal comorbidity. We aimed to analyse the prevalence of various placental lesions from a 6-months prospective observational study and to correlate the various placental profiles to obstetrical outcome, maternal diseases and pregnancy treatments. The frequency of foetal vascular malperfusion lesion could be estimated at 8.7%, in our population and to understand its neonatal associations.
Methods
The study groups consisted of 208 consecutive women which ended the pregnancy and have placental analysis during the period of the study.
Results
From December 2015 to October 2017, from overall 4398 delivered pregnancies in university obstetrical department, 208 (4.7%) placental analysis have been done and included in the study. The placental analysis have been done for vascular obstetrical complications during the pregnancy (n = 106; 51%), unexplained abnormal foetal heart rate tracings (n = 59; 28,3%), suspicion of intra-amniotic infection (n = 12; 5,7%%), term new-borns Apgar score <7 or arterial cord blood pH ≤ 7 (n = 7; 3,5%), spontaneous preterm delivery (n = 19; 9,1%), intrahepatic cholestasis of pregnancy (n = 5; 2,4%). An adverse obstetrical event was noted in 87 cases (42%): preeclampsia or HELLP syndrome (n = 15; 7%), FGR (n = 59; 28%), gestational diabetes (n = 33; 16%) and gestational hypertension (n = 19; 9%). Placental histological analysis showed abnormal vascular features in 159 cases (76%), inflammatory features in 16 placentas (8%), vascular and inflammatory features in 10 cases (4%), chorioamnionitis in 38 cases (18%) and absence of any abnormality in 43 cases (21%). A cluster analysis of histological features allowed distinguishing three placental patterns: a normal pattern characterised by the absence of any placental lesions, an inflammatory pattern characterised by the presence of villitis and/or chronic intervillositis; a vascular pattern with the presence of thrombosis, maternal floor infarct with massive perivillous fibrin deposition, infarction and chronic villositis hypoxia. Women with inflammatory placental profile have significantly increased frequencies of tobacco use (50% vs. 9%; P = 0.03), pathological vascular Doppler (50% vs. 5%; P = 0.001), FGR (100% vs. 14%; P = 0.0001) and oligohydramnios (67% vs. 5%; P = 0.0001) than those with normal placentas. A higher rate of vascular or inflammatory lesion were observed in women with Hypertensive disorder of pregnancy, where as those with inflammatory pattern have significantly more frequent FGR (100% vs 34%; P = 0.02) and oligohydramnios (67% vs 5%; P = 0.0002).
Conclusion
The placenta analysis is important to understand the origin of adverse obstetrical outcome and the risk for subsequent pregnancy.
Keywords: Placental lesions, Obstetrical outcome, Chronic intervillositis
AJOG Global Reports at a Glance.
Why was this study conducted?
Data about the placental analysis from various not selected routine issues remain rare, and the value of placental analysis to better guide the clinical evaluation is still debated. This is the first study providing a cluster analysis allowing a correlation of various placental lesions with clinical parameters.
Key findings
This work allowed determining four major placental profiles from women with an indication of placental analysis: normal placenta, vascular, inflammatory and a combined vascular/inflammatory profile pattern. These placental issues have important clinical correlations, such as the high correlation of oligohydramnios with inflammatory lesions, and of FGR and vascular events with vascular placental profile. The prevalence of vascular placental lesions was high and important when drawing the necessary conclusions from the pregnancy that has just ended, to optimise the chances for future pregnancies.
What does this add to what is known?
This study add the correlation of placental and clinical parameters in cohort of woman with adverse obstetrical issues and the prevalence of various placental lesions, showing the interest of placental examination.
Introduction
Since the Consensus Statement published by the Amsterdam Placental Workshop Group,1 knowledge of the meaning of placental vascular malperfusion has become essential in the unavoidable analysis of obstetrical history for patients with autoimmune diseases or any other maternal comorbidities. The Amsterdam Placental Workshop Group Consensus Statement that was published in 20161 focused on the distinction between foetal vascular malperfusion and maternal vascular malperfusion conditions. Most importantly, possibly in association with the latter, pregnancies with “chronic intervillositis (CIUE), or high-grade (more than 10 contiguous villi affected) villitis of unknown etiology (VUE), were considered important to identify “by virtue of their high recurrence risk and their association with adverse pregnancy outcomes.” The express purpose of the proposed terminology was “to assist in international comparability of clinicopathologic and scientific studies and assist in refining the significance of lesions associated with adverse pregnancy and later health outcomes.” Indeed, the associated adverse obstetrical events and their possible recurrence are an important challenge for the obstetrician, as the diagnosis of the primum movens may be difficult to determine specifically in each case, and the placental analysis available after delivery, appears as the best way to understand and clarify the mechanism having led to the adverse obstetrical outcome.2,3 Catov et al 4 who studied 20,091 births (15,710 term and 4381 preterm) with placental evaluations, found that the combination of placental malperfusion with inflammatory lesions at various degrees was associated with earlier delivery (adjusted difference -2.28 weeks, P < 0.0001) and reduced foetal growth (adjusted birthweight z-score difference, -0.24, P = 0.001) than when no lesion was present. However, it appears essential to distinguish patterns of ascending intrauterine infection from those of chronic placental inflammatory lesions, identified as VUE or CIUE that implies a histiocytic infiltrate in the intervillous space. Indeed these placental lesions have a significantly higher rate of pregnancy loss, foetal growth restriction (FGR) and a notably high likelihood of recurrence,5 of which the pathophysiology is still hotly debated and not fully evaluated.6,7 Now, the precise evaluation of the placental phenotype and the correlation to the clinical and obstetrical features are crucial to determine the risk of recurrence for the subsequent pregnancy, and the chances of success of a potential preventive treatment.
In this study, we aimed to analyse the prevalence of these placental lesions from a 6-months prospective observational study preceding the implementation of the Amsterdam Placental Workshop Group Consensus Statement in our centre and used a cluster analysis to correlate the various placental profiles to obstetrical outcome, maternal diseases and pregnancy treatments.
Patients and methods
Participants
This study was conducted with the collaboration of the Department of Internal Medicine and the Department of Obstetrics and Gynaecology of Jean Verdier Hospital (Bondy) from December 2015 to May 2016.
The study groups consisted of 208 consecutive women (Figure 1), who delivered and who's placental required an analysis during the period of the study. The reasons for the placental analysis were: (i) vascular obstetrical complications during pregnancy (hypertensive disorder, pre-eclampsia and/or foetal growth Restriction (FGR); and/or8 any event during the delivery such as abnormal foetal heart rate tracings (FIGO classification); suspicion of intrauterine infection (IUI); and/or new-born with a 5 minute Apgar score < 7 or arterial cord blood pH ≤ 7; preterm delivery; intrahepatic cholestasis of pregnancy .
Figure 1.
Clinical characteristics of placental analysis
Boujenah. Prevalence and association of placental lesions with obstetrical features and outcome: data from French prospective study. Am J Obstet Gynecol Glob Rep 2024.
All patients gave informed consent before enrolment and the local ethics committee approved the study protocol.
Data were collected as follows: age, number of previous pregnancies, number and type of previous adverse obstetrical outcome, body mass index, tobacco and alcohol use, prior medical and surgical history, foetal and maternal adverse outcomes, medications during the subsequent pregnancy, type of delivery, new-born's weight and Apgar scores.
The placental analysis included (i) the macroscopic analysis: placental weight, presence of hematoma, perivillous fibrin deposition (PFD), maternal floor infarction (MFI), infarctions and (ii) microscopic analysis: presence of placental vascular process (Maternal or foetal stromal-vascular lesions) or Placental inflammatory-immune processes (acute or chronic Infectious inflammatory lesions, Immune/idiopathic inflammatory lesions (such as VUE and related/associated lesion) or massive perivillous fibrinoid deposition (maternal floor infarction)
The following placental patterns were particularly noted: inflammatory lesions in the presence of villitis and chorioamnionitis with or without malperfusion vascular lesions, in the absence of any infectious disease; vascular in the presence of vascular intramural or perivillous fibrin deposition and/or thrombosis and /or maternal vascular malperfusion; placental weight and/or fetoplacental weight ratio as surrogates for placental function, has been suggested as a possible indicator of adequacy of placental reserve capacity in the event of foetal growth restriction, chorioangiosis, chronic hypoxia and increased syncytial knots.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research
Statistical analysis
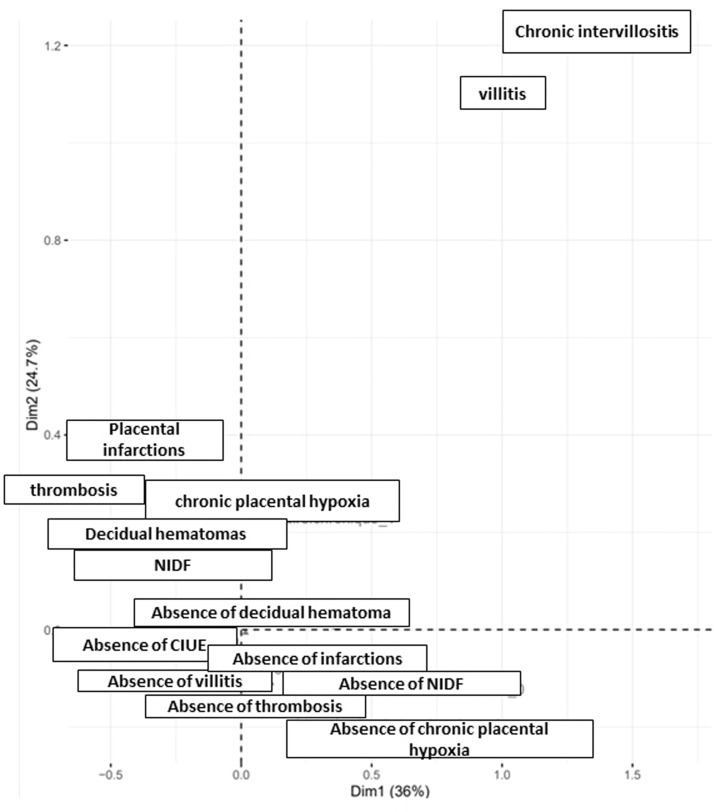
Data are described with numbers and frequencies (%) for categorical variables and medians (ranges) for continuous variables. The categorical and continuous variables were analysed respectively with a Chi-squared or a Fisher's exact test and a Mann-Whitney/Wilcoxon or Kruskal–Wallis test when appropriate. A multiple correspondence analysis (MCA) was used to identify three groups of lesions. This method allows summarising the information contained in large number of categorical variables in order to ease the interpretation. After identifying all dimensions explaining the maximum variance in the data, we used a graphical approach with the first two dimensions, containing more than 60% of the total explained variance. All statistical differences are considered significant at P -value < 0.05. Statistical analyses involved use of GraphPad Prism v7.0 (GraphPad Software, San Diego, CA, USA), Python and R
Results
Patients’ general and placental histological characteristics
From December 2015 to May 2016, from overall 4398 delivered pregnancies in university obstetrical department, 208 (4.7%) placental analysis have been done and thus patients have been included in the study. The placental analysis have been done for vascular obstetrical complications during the pregnancy (n = 106; 51%), unexplained abnormal foetal heart rate tracings (n = 59; 28,3%), suspicion of IUI (n = 12; 5,7%), term new-borns Apgar scores <7 or arterial cord blood pH ≤ 7 (n = 7; 3,5%), spontaneous preterm delivery (n = 19; 9,1%), intrahepatic cholestasis of pregnancy (n = 5; 2,4%). Median age of women was 29 years [ranges, 15–45] (Table 1). 118 women had at least one previous uncomplicated pregnancy, 63 were primigesta and others had at least one previous complicated pregnancy (more than 3 early miscarriages in 2 cases, previous intrauterine deaths in 2 cases, gestational hypertension with intrauterine growth restriction and/or preeclampsia in 23 cases). Ethnic origins were Caucasians (n = 62; 30%), Asian Indians (n = 37; 17%), North Africans (n = 36; 17%), and Sub-Saharan Africans (n = 72; 35%). The subsequent pregnancy was mostly spontaneous (n = 201; 97%). An adverse obstetrical event was noted in 87 cases (42%): preeclampsia or HELLP syndrome (n = 15; 7%), FGR (n = 59; 28%), gestational diabetes (n = 33; 16%) and gestational hypertension (n = 19; 9%) (Table 1). Aspirin was used in 13 cases (6%) and low molecular heparin in 5 cases (2%). Delivery characteristics and newborn features are presented in Table 1.
Table 1.
Patients’ general characteristics and obstetrical history.
| Characteristics | N=208 |
|---|---|
| Age (years), medians (ranges) | 29 (15–45) |
| Caucasians (n, %) | 62 (30) |
| Sub-Saharan Africans (n,%) | 72 (35) |
| North Africans (n,%) | 36 (17) |
| Asians (n,%) | 37 (17) |
| Obstetrical history | |
| Gestity, medians (ranges) | 2 (1-9) |
| Parity, medians (ranges) | 2 (1-6) |
| Intrauterine deaths (n,%) | 3 (1) |
| Miscarriages (n,%)/ Number, medians (ranges) | 45 (22) / 0 (0-4) |
| Previous Preeclampsia (n,%) | 23 (11) |
| Cardiovascular factors | |
| BMI, medians (ranges) | 24 (16-41) |
| Autoimmune disease / thrombosis (n,%) | 4 (2) / 2 (1) |
| Diabetes mellitus / arterial hypertension (n,%) | 5 (2) / 6 (3) |
| Tobacco (n,%) | 26 (12.5) |
| Pregnancy outcome | |
| Spontaneous pregnancy (n,%) | 201 (97) |
| Gestational diabetes (n,%) | 33 (16) |
| Preeclampsia (n,%) | 14 (7) |
| Gravida arterial hypertension (n,%) | 19 (9) |
| Pathological Doppler (n,%) | 23 (11) |
| FGR (n,%) | 59 (28) |
| Oligohydramnios (n,%) | 10 (5) |
| Gravida cholestasis (n,%) | 6 (3) |
| Aspirin / LMWH (n,%) | 13 (6) / 5 (2) |
| Delivery | |
| Prematurity<37 wg / 34 wg (n,%) | 36 (17) / 6 (3) |
| Spontaneous labour (n,%) | 118 (57) |
| Term (weeks’ gestation), medians (ranges) | 39 (24-42) |
| MAP (n,%) | 9 (4) |
| Caesarean section (n,%) | 67 (32) |
| Abnormal foetal heart rate tracing (n,%) | 100 (48) |
| Delivery haemorrhage (n,%) | 9 (4) |
| Neonates characteristics | |
| Birth weight (gr), medians (ranges) | 2765 (560–4530) |
| Placenta weight (gr), medians (ranges) | 510 (220–1230) |
| Apgar 5, medians (ranges) | 10 (9–10) |
| Sex male (n,%) | 102 (49) |
Boujenah. Prevalence and association of placental lesions with obstetrical features and outcome: data from French prospective study. Am J Obstet Gynecol Glob Rep 2024.
Placental histological analysis showed abnormal vascular features in 159 cases (76%), inflammatory features in 16 placentas (8%), vascular and inflammatory features in 10 cases (4%), chorioamnionitis in 38 cases (18%) and absence of any abnormality in 43 cases (21%) (Table 2).
Table 2.
Microscopic placental lesions
| Histological features | N = 208 |
|---|---|
| Normal placenta (n,%) | 43 (21) |
| Inflammatory lesions | n = 16 (8) |
| Villitis (n,%) | 8 (4) |
| Chronic intervillositis (n,%) | 1 (0.5) |
| Villitis and intervillositis (n,%) | 7 (3.3) |
| Vascular lesions | N = 144 |
| Perivillous fibrin deposition (n,%) | 86 (42) |
| Infarctions (n,%) | 49 (24) |
| Thrombosis (n,%) | 9 (4) |
| Placental insufficiency | n = 159 (76) |
| Placental hypotrophy (n,%) | 33 (16) |
| Chorangiosis (n,%) | 19 (9) |
| Villositis chronic hypoxia (n,%) | 96 (46) |
| Increased syncytial knots (n,%) | 89 (43) |
| Infectious lesions | N = 38 |
| Chorioamnionitis (n,%) | 38 (18) |
Boujenah. Prevalence and association of placental lesions with obstetrical features and outcome: data from French prospective study. Am J Obstet Gynecol Glob Rep 2024.
Placental histological patterns and association with obstetrical outcome
A cluster analysis of histological features is represented in Figure 2. This analysis allowed distinguishing three placental patterns: a normal pattern characterised by the absence of any placental lesions, an inflammatory pattern characterised by the presence of villitis and/or chronic intervillositis; a vascular pattern with the presence of thrombosis, perivillous fibrin deposition (PFD), infarction and chronic villositis hypoxia. Then, we analysed patients’ characteristics, obstetrical history and outcome according to these placental histological patterns (Table 3). Women with inflammatory placental profile have significantly increased frequencies of tobacco use (50% vs. 9%; P = 0.03), FGR (100% vs. 14%; P = 0.0001), oligohydramnios (67% vs. 5%; P = 0.0001) and abnormal uterine artery Doppler (50% vs. 5%; P = 0.001) as compared with those with normal placentas (Table 3). The rate of preeclampsia and gravida hypertension were not significantly different in pregnancies with inflammatory and vascular histological patterns. Moreover, the pattern of the placenta differed according to the occurrence of hypertensive disorder of pregnancy (34 vs. 174 women), with a higher rate of vascular or inflammatory and lower normal placenta (82.4%, 5.9%, 8.9% versus 71.2%, 2.3%, 22.9%, P = 0.16). Also, we observe that inflammatory pattern have significantly more frequent FGR (100% vs. 34%; P = 0.02) and oligohydramnios (67% vs 5%; P =0.0002).
Figure 2.
Cluster analysis of histological features
Boujenah. Prevalence and association of placental lesions with obstetrical features and outcome: data from French prospective study. Am J Obstet Gynecol Glob Rep 2024.
Table 3.
Patients’ characteristics and obstetrical outcome according to placental lesions.
| Characteristics | All N=208 | Normal placenta N= 43 | Inflammatory placenta N = 6 | Vascular placenta N = 149 | Vascular and inflammatory lesions N=10 |
|---|---|---|---|---|---|
| Age (years) | 29 (15–33) | 29 (15–33) | 25 (15–33) | 29 (15–33) | 29 (15–33) |
| Obstetrical history | |||||
| Gestity, medians (ranges) | 0 (0–3) | 0 (0–3) | 0 (0–3) | 0 (0–3) | 0 (0–3) |
| Parity, medians (ranges) | 0 (0–3) | 0 (0–3) | 0 (0–2) | 0 (0–3) | 0 (0–3) |
| Previous Intrauterine deaths (n, %) | 3 (1.4) | 0 | 0 | 3 (2) | 0 |
| Previous Miscarriages (n, %) N medians (ranges) | 45 (22) 0 (0–4) | 9 (21) 0 (0-4) | 2 (33) 0 (0–1) | 36 (24) 0 (0–3) | 2 (20) - |
| Previous FGR (n, %) | 23 (11) | 4 (9) | 1 (17) | 17 (11) | 1 (10)su |
| Cardiovascular factors | |||||
| BMI, medians (ranges) | 24 (16-41) | 23 (17-36) | 21 (18-37) | 23 (16-41) | 21 (18-37) |
| Tobacco (n, %) | 26 (13) | 4 (9) | 3 (50) | 22 (15) | 0 |
| Pregnancy outcome | |||||
| Gestational diabetes (n, %) | 33 (16) | 6 (14) | 1 (17) | 26 (17) | 0 |
| Preeclampsia (n, %) Gravida arterial hypertension (n, %) | 14 (7) 19 (9) | 1 (2)/0 2 (5) | 1 (17) 1 (17) | 1 (8) 16 (11) | 0 0 |
| Abnormal uterine artery Dopplers (n, %) | 25 (12) | 2 (5) | 3 (50) | 21 (14) | 0 |
| FGR (n, %) | 59 (28) | 6 (14) | 6 (100) | 51 (34) | 1 (10) |
| Oligohydramnios (n, %) | 11 (5) | 2 (5) | 4 (67) | 7 (5) | 1 (10) |
| Gravida cholestasis (n, %) | 6 (3) | 1 (2) | 0 | 5 (3) | 0 |
| Aspirin (n, %) Low molecular weight heparin (n, %) | 13 (16) 5 (2) | 1 (2) 1 (2) | 2 (33) 0 | 12 (8) 4 (3) | 2 (20) 0 |
| Delivery | |||||
| Prematurity<37 wg (n, %) Prematurity<34 wg (n, %) | 36 (17) 6 (3) | 10 (23) 3 (7) | 1 (17) 0 | 26 (17) 3 (2) | 0 0 |
| Term (weeks), medians (ranges) | 39 (24–42) | 38 (28–41) | 39 (36–42) | 39 (24–42) | 39 (29–42) |
| Threatened preterm labour (n, %) | 9 (4) | 5 (12) | 1 (17) | 3 (2) | 0 |
| Abnormal foetal heart rate tracing (n, %) | 100 (48) | 19 (44) | 1 (17) | 77 (52) | 1 (10) |
| Neonates characteristics | |||||
| Birth weight (gr), medians (ranges) | 2765 (560–4560) | 2868 (1000–3990) | 2903 (2070–4503) | 2760 (560–4140) | 2760 (560–4140) |
| Placenta weight, medians (ranges) | 477 (100–1230) | 468 (100-1230) | 467 (100–1230) | 481 (100–1000) | 481 (100–1000) |
| Apgar 5 (n, %) | 10 (10) | 10 (10) | 10 (10) | 10 (10) | 10 (10) |
Boujenah. Prevalence and association of placental lesions with obstetrical features and outcome: data from French prospective study. Am J Obstet Gynecol Glob Rep 2024.
A univariate analysis was performed including clinical features associated with the placental histological patterns considering age, ethnical origin, comorbidities, tobacco use, previous obstetrical history, adverse obstetrical events (preeclampsia, diabetes, FGR, oligohydramnios, etc), therapies during the pregnancy, delivery and neonates characteristics (Table 4) to highlight the 3 different patterns. Maternal vascular malperfusion was associated with FGR, and hypertensive disorder of pregnancy, oligohydramnios was the only factor associated with the placental inflammatory pattern, and threatened preterm labour, previous normal pregnancy and Caucasian ethnicity were associated with normal placental pattern (Table 4).
Table 4.
Univariate analysis of obstetrical features associated with different placental profiles.
| Patients features | Univariable odds ratio (95% CI) | P value |
|---|---|---|
| Inflammatory placental pattern | ||
| Oligohydramnios | 10.3 (2.6–41.6) | 0.004 |
| Placental vascular pattern | ||
| FGR | 3.6 (1–12.2) | 0.03 |
| FGR with hypertensive disorders | 2.4 (1– 5.5) | 0.03 |
| Threatened preterm labour | 0.1 (0.03–0.6) | 0.006 |
| Caucasians | 0.3 (0.1–0.7) | 0.04 |
| Normal placenta | ||
| Threatened preterm labour | 5.3 (1.4–20.6) | 0.02 |
| History of normal pregnancy | 2.6 (1.3–5.2) | 0.02 |
| Caucasians | 3.2 (1.4–7.4) | 0.04 |
Boujenah. Prevalence and association of placental lesions with obstetrical features and outcome: data from French prospective study. Am J Obstet Gynecol Glob Rep 2024.
Discussion
Main results
The analysis of our patients allowed determining four major placental profiles from women with an indication of placental analysis: normal placenta, vascular, inflammatory and a combined vascular/inflammatory profile pattern. Indeed, the cluster analysis allows regrouping several placental profiles and showing some important clinical correlations, such as the high correlation of oligohydramnios with inflammatory lesions, and of FGR and vascular events with vascular placental profile. In our study, the prevalence of vascular placental lesions was high and important when drawing the necessary conclusions from the pregnancy that has just ended, to optimise the chances for future pregnancies.
Interpretations
Our results highlighted that most of the obstetrical outcomes could be driven by placental pathology, as the rate of normal placental analysis is low. This study represents a real-life cohort study using the placental analysis done for various adverse obstetrical events during pregnancy and/or delivery, and its usefulness in a prospective view.
One main objective of the placenta analysis is to focus the postnatal exploration (for example: cardiovascular maternal status, biological analysis for thrombophilia, infectious process) to minimise the risk of recurrent adverse disease in a subsequent pregnancy. Our cluster analysis of histological features supports the recent framework for placenta classification that define 2 main patterns (placenta vascular versus inflammatory-immune processes).2 As far as we know, this is the first cluster analysis trying to determine a correlation of clinical obstetrical features with these placental features. The description of clinical context with several obstetrical adverse events, such as FGR, preeclampsia, or oligohydramnios could be also helpful to avoid unhelpful placental examinations.
Chronic inflammation with intervillositis was identified in half cases of “inflammatory lesions” a majority of them with FGR (37%) and/or hypertensive disorders (12%). In the event of early 222 onset FGR, Levytska et al showed that women with normal uterine artery Doppler examination delivered later than those with bilaterally abnormal UAD (30.1 ± 3.5 vs. 28.0 ± 3.5 weeks; mean ± standard deviation; P = 0.03), and their placentas exhibited higher rates of chronic intervillositis (15.8 vs. 0.9%; P = 0.01), chorangiosis (15.8 vs. 0.9%; P < 0.0001), massive perivillous fibrin deposition (21.1 vs. 7.4%; P = 0.05), and lower rates of uteroplacental vascular insufficiency (26.3 vs. 79.6%; P < 0.0001).8 The findings of these authors confirm, as stated by the Amsterdam Placental Workshop Group Consensus, and in line with our results, the importance of a specific pattern combining some lesions, such as chronic intervillositis (CIUE) or high-grade VUE, and/or perivillous fibrin deposition and/or thrombosis, in spite of lower rates of uteroplacental vascular insufficiency, due to their high recurrence risk and their association with adverse pregnancy outcomes.
Even if the chronic inflammatory lesions are found in less than 10% of the placental histological analyses, their recognition is particularly important. Indeed, the risk of recurrence during subsequent pregnancy, when intervillositis has been identified, is especially increased, varying from 30-60% in CIUE and VUE. As expected, the vascular profile was correlated with preeclampsia, HELPP syndrome and FGR. The inflammatory profile (VUE and/or CIUE) may rarely be associated with vascular placental lesions, and the prevalence of preeclampsia in these conditions rare, and the oligohydramnios was the only factor from our study. Few large studies analysed the correlation of various placental lesions to overall obstetrical outcome. Another recent prospective study of 350 women, placental abnormalities correlated with neonatal sepsis, preterm birth and small for gestational age babies,9 emphasing the importance of placental analysis to consider the prognosis of subsequent pregnancies.
Limitation
The main limit of our study is the absence of normal pregnancy. Recently, Romero et al performed histologic analysis in placentas delivered by women with a normal pregnancy outcome. They found that 78% of placenta had inflammatory or vascular lesions. These lesions were considered as mild suggesting a transient and acute phenomenon due the course of parturition. As in our study, the rate of normal placenta was close to 20%. Therefore, the mode of delivery could be a confounder or an effect modifier of the underlying maternal pathology in the pathogenesis of placenta lesions. In addition, the generalisability of our findings could be compromised by the rate of placenta analysis over the period study (5%). Some analysis could have been missed, especially in case of atypical pre-eclampsie (i.e., without the classic findings), or abnormal neonatal status (acidosis) that does not meet the inclusion criteria (arterial cord blood pH between 7 and 7,15).
Overall, placental examination is essential when synthesising the course of a high-risk pregnancy or after an obstetrical adverse event, in order to draw the appropriate conclusions and to decide the preventive measures to be taken during the next pregnancy
Conclusion
Placental histological analysis is essential, and the placental findings should be stratified to help to better management of subsequent pregnancy. The two distinct placenta patterns (vascular and inflammatory process) seem to be associated with specific clinical context.
CRediT authorship contribution statement
Jeremy Boujenah: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Data curation, Conceptualization. Jonathan Cohen: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Data curation, Conceptualization. Michael Allouche: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Marianne Ziol: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Amélie Benbara: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Marion Fermaut: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Olivier Fain: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Lionel Carbillon: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Arsène Mekinian: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Data curation, Conceptualization.
Footnotes
Tweetable statement: This work allowed determining four major placental profiles from women with an indication of placental analysis: normal placenta, vascular, inflammatory and a combined vascular/inflammatory profile pattern. Indeed, the cluster analysis allows regrouping several placental profiles and showing some important clinical correlations, such as the high correlation of oligohydramnios with inflammatory lesions, and of FGR and vascular events with vascular placental profile. In our study, the prevalence of vascular placental lesions was high and important when drawing the necessary conclusions from the pregnancy that has just ended, to optimise the chances for future pregnancies.
Conflicts of interest: AM is investigator of CELGENE, ROCHE, CHUGAI founded trials with APHP and Hospital 15-20 promotion; AM received several fees for congress travels and experts’ fees from LFB, SANOFI, SHIRE, and CELGENE.
Funding: None.
Ethics statement: All pregnant women booked to deliver in our university hospital are informed that data is routinely entered at birth into an electronic record-keeping system, then checked during the maternity stay of each woman by a midwife qualified in data management and storage for contributions to the national “Programme de médicalisation des systems d'information” (PMSI) database. They are also informed that indicators of perinatal health are regularly analysed to assess the overall quality of obstetric care and to update medical management protocols and publication of research results. The database has been declared to the French data protection authority (Commission Nationale de l'Informatique et des Libertés [CNIL]).
Data availability statement: The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1.Khong TY, Mooney EE, Ariel I, Balmus NC, Boyd TK, Brundler MA. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch Pathology Lab Med. 2016;140(7):698–713. doi: 10.5858/arpa.2015-0225-CC. [DOI] [PubMed] [Google Scholar]
- 2.Redline RW. Classification of placental lesions. Am J Obstetr Gynecol. 2015;213(4 Suppl):S21–S28. doi: 10.1016/j.ajog.2015.05.056. [DOI] [PubMed] [Google Scholar]
- 3.Katzman PJ. Chronic inflammatory lesions of the placenta. Semin Perinatol. 2014;39(1):20–26. doi: 10.1053/j.semperi.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Catov JM, Scifres CM, Caritis SN, Bertolet M, Larkin J, Parks WT. Neonatal outcomes following preterm birth classified according to placental features. Am J Obstetr Gynecol. 2017;216(4) doi: 10.1016/j.ajog.2016.12.022. 411.e1-e14. [DOI] [PubMed] [Google Scholar]
- 5.Simula NK, Terry J, Kent NE, Robertson J, Purkiss S, Bloomenthal D, Williams C, Bedaiwy MA. Chronic intervillositis of unknown etiology (CIUE): prevalence, patterns and reproductive outcomes at a tertiary referral institution. Placenta. 2020;100:60–65. doi: 10.1016/j.placenta.2020.07.032. [DOI] [PubMed] [Google Scholar]
- 6.Mekinian A, Costedoat-Chalumeau N, Carbillon L, Coulomb-L'Hermine A, Le Guern V, Masseau A. [Chronic histiocytic intervillositis: diagnosis and management] Rev Med Interne. 2017 doi: 10.1016/j.revmed.2017.10.422. [DOI] [PubMed] [Google Scholar]
- 7.Redline RW. Villitis of unknown etiology: noninfectious chronic villitis in the placenta. Human Pathol. 2007;38(10):1439–1446. doi: 10.1016/j.humpath.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 8.Levytska K, Higgins M, Keating S, Melamed N, Walker M, Sebire NJ, Kingdom JC. Placental pathology in relation to uterine artery doppler findings in pregnancies with severe intrauterine growth restriction and abnormal umbilical artery doppler changes. Am J Perinatol. 2017;34(5):451–457. doi: 10.1055/s-0036-1592347. [DOI] [PubMed] [Google Scholar]
- 9.Loverro MT, Damiani GR, Di Naro E, Schonauer LM, Laforgia N, Loverro M. Analysis of relation between placental lesions and perinatal outcome according to Amsterdam criteria: a comparative study. Acta bio-medica: Atenei Parmensis. 2020;91(3):e2020061. doi: 10.23750/abm.v91i3.8274. [DOI] [PMC free article] [PubMed] [Google Scholar]