Abstract
Introduction
The deep inferior epigastric artery perforator (DIEP) free flap is the gold-standard for breast reconstruction but is technically demanding, resource intensive and time-consuming, making it a daunting task for the junior surgeon.
Aim
To report the lessons learnt from the experience of a single surgeon performing their first 150 DIEP reconstructions as a guide for junior surgeons.
Methods
Data regarding patient demographics and surgical outcomes from April 2021 to October 2022 were collected retrospectively from medical records. Surgical outcomes were analysed using Microsoft Excel.
Results
Over 17 months, 150 flaps were completed in 97 patients by the senior author (BS). Operative duration was negatively correlated with case number for unilateral DIEPs (r = -0.73, p < 0.05) and for bilateral DIEPs (r = -0.67, p = 0.14). Raise time and ischaemic time were also negatively correlated with case number (r = -0.82, p < 0.05 and r = -0.79, p < 0.05, respectively). There were 10 complications and no flap losses.
Discussion
The data demonstrate an expected improvement in surgical efficiency with increased experience. We describe the key factors contributing to efficiency in our series, such as preoperative CT angiography, surgical markings prior to the day of surgery, a two-team approach with three diathermy sets, flap raise using monopolar diathermy, preference towards choosing a single dominant perforator and early commitment to perforator choice. This case series acts as a guide for the junior plastic surgeon in achieving safe, aesthetic and efficient results when completing free DIEP flap breast reconstructions.
Keywords: Breast/surg, Plastic surgery procedures, Learning curve, Efficiency, Clinical decision making
Introduction
Breast cancer is the second commonest cancer amongst women worldwide.1 Aesthetic concerns following breast cancer treatment, especially following mastectomy, are an important health issue owing to the psychological distress caused by poor aesthetic outcomes.2 Therefore, reconstructive techniques must be oncologically and surgically safe, and also aesthetically pleasing.
Autologous breast reconstruction has multiple benefits over implant-based reconstruction. In particular, autologous reconstruction avoids the risks associated with long-term implant failure while providing a naturally textured, well-shaped and permanent aesthetic result.3,4 Deep inferior epigastric artery perforator (DIEP) flap reconstructions are associated with greater satisfaction and psychosexual well-being when compared to implants.5 The DIEP flap was first described by Koshima and Soeda in 1989 and its first use in breast reconstruction was documented by Allen and Treece in 1994.6,7 Since then, the DIEP flap has grown in popularity owing to the decreased abdominal and overall morbidity and shorter hospital stay when compared with transverse rectus abdominis muscle flaps.8,9
Aim
This case series documents the experience of a single surgeon performing their first 150 DIEP reconstructions. The DIEP flap is a technically demanding, resource intensive and time-consuming operation, making it a daunting task for the new surgeon. We report the specific lessons learnt and compare the outcomes from before and after these changes were introduced. We intend to provide strategies which the junior plastic surgeons can implement to improve their outcomes and efficiency without compromising safety.
Methods
Data were collected retrospectively from the patient's medical records. Demographics (age and sex), medical background (medical history, smoking status and American Society of Anaesthesiologists score), surgical variables (defect, history of radiotherapy and/or chemotherapy, raise time, ischaemic time and microsurgical details) and outcomes (complications, follow-up and oncological outcome) were recorded.
Data were recorded and analysed using Microsoft Excel V16. Normality was tested using the Shapiro-Wilk test and frequency histograms. Outliers were identified using boxplots and were subsequently removed for data analysis. Correlation was determined using the Pearson correlation coefficient and variables were compared using the Mann-Whitney U test. A p-value of < 0.05 was considered statistically significant.
Ethics approval was granted by Western Sydney Local Health District Research and Education Network (2304-02).
Technique
The method below stipulates a refined technique settled upon after considering the lessons learnt throughout the series.
Preoperatively, all patients underwent computed tomography angiography (CTA) to map the deep inferior epigastric artery (DIEA) and its perforators. Where possible, the patients were marked at an outpatient appointment one day prior to surgery and all patients were admitted on the day of surgery.
A two-team approach was used. The ‘bottom team’ completed the DIEP flap raise and closed the abdominal donor site. The ‘top team’ prepared the breast pocket and recipient vessels and completed microsurgery and flap inset.
Flaps were raised using solely monopolar diathermy set to coagulation and blend. Three monopolar instruments were required: a ‘hot’ instrument set to 60/60 (coagulation/cut) with smoke suction and a ‘cold’ instrument set to 20/20 without suction for the ‘bottom team’ and an additional instrument for the ‘top team’.
The safe and efficient use of monopolar cautery around vessels was achieved using the ‘tension-tap-sweep’ technique. Throughout dissection, it was essential that the assistant provided gentle tension on the tissue by folding and lightly tractioning the flap medially to avoid inadvertent damage from tissue folding onto the perforator. The ‘hot’ instrument was first used to dissect from lateral to medial until the lateral border of the rectus. At this point, the ‘cold’ instrument was used for perforator dissection. The use of one dominant perforator was preferred, with a decision to commit to the preoperatively selected perforator. While the assistant retracted the flap, the surgeon used forceps in their non-dominant hand to tension the tissue surrounding the perforator. The ‘cold’ monopolar was then used to ‘tap’ this taught tissue between the forceps and perforator. This ‘tap’ should be light and very short in duration. It should also be far enough away from the vessel to avoid thermal damage but close enough to allow clean dissection. Following this, the blunt blade of the monopolar was used to ‘sweep’ the cauterised tissue away from the vessel.
Once the perforator was isolated, a fascial incision was made with a small cuff surrounding the vessels. The same ‘tension-tap-sweep’ technique was used to trace the pedicle until a suitable calibre (not necessarily extending to the DIEA/V origin). Tension during intramuscular dissection was aided through careful placement of Gelpi retractors on either side of the vessel. The provision of muscle relaxant by the anaesthetist is fundamental to avoid jumping of the muscle with monopolar diathermy.
Langenbecks retractors were then used as the vessel descends towards its origin. Care was taken to preserve crossing nerves, especially at the arcuate line, and not to split the anterior sheath and muscle past the arcuate line, rather relying on good lighting and firm retraction to allow the completion of vessel dissection. Thereby, mitigating the risk of rectus denervation.10
Once pedicle dissection was completed, the flap was islanded and de-epithelialised on the abdomen.
Whilst the raise was completed, the ‘top team’ prepared the chest wall. Haemostasis was prioritised and drains were inserted. The breast pocket was plicated inferolaterally to allow medialisation of the DIEP flap when inset to achieve a better aesthetic result. Completing these steps prior to vessel preparation limits flap manipulation post-microsurgery.
Arterial anastomosis was end-to-end to the internal mammary artery with interrupted 8/0 nylon sutures. Venous anastomosis was completed using a venous coupler. Two venous anastomoses (antegrade/retrograde with the addition of superficial inferior epigastric vein) were completed if the deep inferior epigastric vein appeared engorged when the flap was islanded or if the flap appeared congested. The pedicle was wrapped with Surgicel mesh and Spongostan sponge was used to prevent kinking.
The flap was coned and prior to formal inset, stapled in place and the patient sat up for full appreciation of the aesthetic outcome. The flap shape was adjusted and this process was repeated until an excellent aesthetic result was achieved.
As the ‘top team’ completed microsurgery and inset, the ‘bottom team’ completed subscarpal fat excision, mons pubis liposuction, rectus abdominis plication and closed the abdominal donor site after progressive tension sutures. Abdominal tap blocks were completed for regional anaesthesia and negative pressure wound therapy with 3M Prevena was applied to the abdominoplasty suture line.
Post-operatively, patient-controlled analgesia was started immediately. Intravenous heparin, 5000U, was administered once on table with regular chemical venous thromboembolism prophylaxis commencing on the night of operation until discharge. Patients were administered 48-hours of intravenous antibiotics and oral antibiotics were continued for five days. In accordance with our unit's enhanced recovery after surgery (ERAS) guidelines, normal diet and oral aperients were started on day one post-operative and patients sat out of bed and progressed to mobilisation with physiotherapists.
Results
Patient Demographics
Between April 2021 and October 2022, the senior author (BS) completed his first 150 free DIEP flap reconstructions in Sydney, Australia. Patient demographics are presented in Table 1. Fifty-three of the 97 patients had bilateral DIEP reconstructions and 44 patients had unilateral reconstructions. Treatment options for all patients regarding mastectomy type, radiotherapy, chemotherapy and timing of reconstruction were discussed in a multi-disciplinary meeting. Mean age was 53.6 years (38-73 years) and mean BMI was 27.6 kg/m2 (20.2-36.5 kg/m2). Sixty-nine (71%) patients were non-smokers, 25 (26%) were ex-smokers and three (3.1%) were smokers who had quit within 6 weeks of operation. Sixty-nine (71%) patients had immediate resection and reconstruction, whilst 28 (29%) underwent delayed reconstruction. There were 113 (75%) skin-sparing mastectomies, 18 (12%) nipple-sparing mastectomies, 17 (11%) simple mastectomies and 2 (1.3%) radical mastectomies. Twenty-seven flaps (18%) were completed post mastectomy and adjuvant radiotherapy with delayed reconstruction, 24 flaps (16%) were completed post neo-adjuvant radiotherapy followed by mastectomy and immediate reconstruction with the average time between completion of neo-adjuvant radiotherapy and mastectomy and reconstruction being 6.8 weeks, and five patients underwent radiotherapy to a neo-breast post-reconstruction.
Table 1.
Patient Demographics.
| Total Patients (n) | 97 | |
| Mean age (years) | 53.6 (38-73) | |
| Mean weight (kg) | 73 (53-109) | |
| BMI (kg/m2) | 27.6 (20.2-36.5) | |
| Smoking status | Non-smoker | 69 (71%) |
| Smoker (quit within 6 weeks) | 3 (3.1%) | |
| Ex-smoker | 25 (26%) | |
| Reconstruction timing | Immediate | 69 (71%) |
| Delayed | 28 (29%) | |
| Bilateral/Unilateral | Bilateral | 53 (55%) |
| Unilateral | 44 (45%) | |
| Total flaps | 150 | |
| Defects | Skin sparing mastectomy | 113 (75%) |
| Nipple sparing mastectomy | 18 (12%) | |
| Simple mastectomy | 17 (11%) | |
| Radical mastectomy | 2 (1.3%) | |
| Radiotherapy | Pre-reconstruction | 51 (34%) |
| Neo-adjuvant | 24 (13%) | |
| Delayed reconstruction | 27 (21%) | |
| Post-reconstruction | 5 (3.3%) | |
| None | 94 (63%) | |
| Chemotherapy | Pre-reconstruction | 42 (43%) |
| Post-reconstruction | 34 (35%) | |
| None | 21 (22%) |
Outcomes
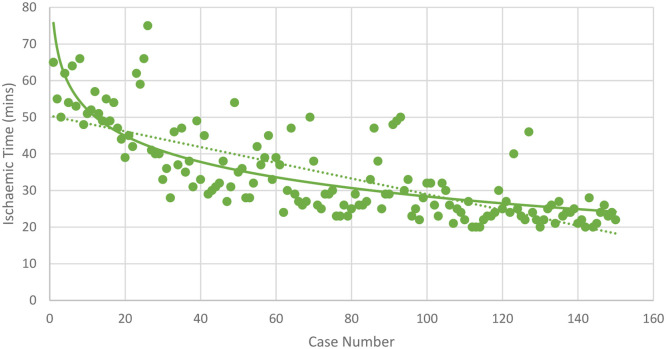
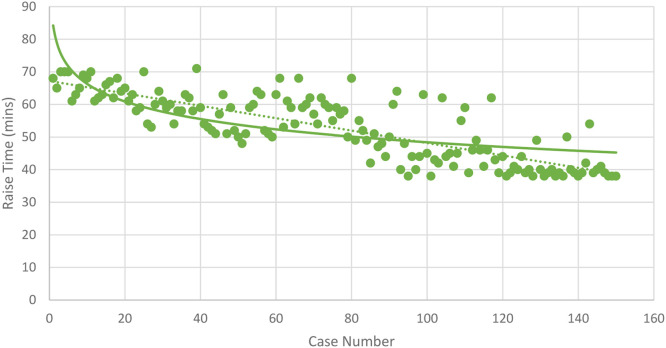
Mean length of hospital stay was 5 days (4-8 days) with mean length of follow-up being 10.4 months (9-14 months). Mean operative duration for unilateral DIEP reconstructions was 4 h 32 min (3 h 29 min to 7 h 39 min) and 6 h 11 min (4 h 20 min to 8 h 55 min), for bilateral DIEP reconstructions. The mean raise time for each flap was 53 min (38-71 min) and mean ischaemic time was 34 min (20-75 min). A single perforator was used in 137 flaps and two perforators were used in 13 flaps. A single venous anastomosis was completed in 32 flaps and two venous anastomoses were completed for 118 flaps. Operative and hospital outcomes are displayed in Table 2.
Table 2.
Operative and hospital outcomes.
| Mean surgical duration (hh:mm) | Unilateral | 4:32 (3:29-7:39) |
| Bilateral | 6:11 (4:20-8:55) | |
| Mean raise time (min) | All flaps | 53 (38-71) |
| Mean ischaemic time (min) | All flaps | 34 (20-75) |
| Mean flap weight (g) | All flaps | 554.8 (330-1041) |
| Number of perforators (n) | 1 | 137 |
| 2 | 13 | |
| Number of veins (n) | 1 | 32 |
| 2 | 118 | |
| Mean length of stay (days) | All patients | 5 (4-8) |
| Mean length of follow-up (months) | All patients | 10.4 (9-14) |
Progression and Improvement
Statistical analysis of our results demonstrated that the operative duration decreased with more experience. Unilateral DIEP operative durations were negatively correlated with case number, r = -0.73 (p < 0.05), according to Pearson's correlation coefficient. Similarly, bilateral DIEP operative durations decreased as case number increased, r = -0.67 (p = 0.14). Additionally, raise time and ischaemic time were negatively correlated with case number, r = -0.82 (p < 0.05) and r = -0.79 (p < 0.05), respectively. All four of the correlation trends described above were best represented using a logarithmic function (Figure 1, Figure 2, Figure 3).
Figure 1.
Surgical Duration.
Figure 2.
Ischaemic Time.
Figure 3.
Raise Time.
Moreover, as shown in Table 3, our results demonstrate a statistically significant improvement in operative efficiency when comparing the mean total operative duration of the first 10 unilateral DIEP flaps (5 h 48 min) to the last 10 unilateral DIEP flaps (3 h 45 min) and the first 10 bilateral DIEP flaps (8 h 26 min) to the last 10 bilateral DIEP flaps (4 h 35 min). This represents a comparison from before and after several key operative processes, described as lessons learnt below, were implemented.
Table 3.
Improvement.
| Group A | Group B | p-value | ||
|---|---|---|---|---|
| Unilateral DIEP | Count | 10 | 10 | |
| Mean operative duration (hh:mm) | 5:48 | 3:45 | < 0.05 | |
| Bilateral DIEP | Count | 10 | 10 | |
| Mean operative duration (hh:mm) | 8:26 | 4:35 | < 0.05 |
Complications
Complications (listed in Table 4) amongst the 150 flaps in 97 patients totalled 10. Two complications were medical (hospital acquired pneumonia requiring intravenous antibiotics and pulmonary embolus despite venous thromboembolism prophylaxis requiring therapeutic anticoagulation). Seven patients had minor surgical complications, with one patient developing a breast seroma requiring ultrasound-guided drainage and six patients developing superficial wound infections requiring antibiotics and dressings (four abdominal and two neo-breast). Finally, one patient had necrosis of her mastectomy flaps, requiring re-operation for skin grafting. No flap failure or microsurgical complications were recorded across the series. Clinically significant fat necrosis developed in eight flaps in eight different patients. There was no significant difference in the complication rates or fat necrosis amongst flaps with single perforators compared to those with two perforators, and single veins compared to those with two veins.
Table 4.
Complications.
| Minor surgical complications | 7 patients |
| Major surgical complications | 1 patient |
| Flap loss | 0 patients |
| Microsurgical complications | 0 patients |
| Medical complications | 2 patients |
| Total complications | 10 patients |
| Fat necrosis | 8 flaps |
Discussion
Training and Experience
During his Reconstructive Microsurgical fellowship at the Health Sciences and Maples Surgical Centres in Winnipeg, Canada, the senior author (BS) completed 123 free flaps, including 96 free DIEP flaps, under the guidance of Professor Edward Buchel. It is here that he learnt the major time-saving technique of raising the DIEP flap solely using monopolar diathermy.
Learning Curve and Key Lessons
Over the 150 flaps, surgical technique was refined into a formulaic method to improve operative efficiency. Time was saved in straightforward parts of the operation, allowing sufficient time for perforator dissection, microsurgery, abdominal contouring and breast shaping.
Laporta et al. and Varnava et al. showed that increased experience leads to decreased operative time.11,12 In our study, the decrease in operative duration was logarithmic. In keeping with Grinsell et al. but contrary to Busic et al., Hofer et al. and Cubitt et al., we did not find a change in complication rates through the series, potentially implying that pre-consultancy training is adequate in preparing the plastic surgeon to achieve safe results.13, 14, 15, 16
Our analysis in Table 3 demonstrates significantly shorter operative durations in the last 10 unilateral and bilateral DIEP operations compared to the first 10 unilateral and bilateral DIEP operations. The first 10 and last 10 unilateral and bilateral flaps were chosen for comparison as they represent a time before and after specific new processes were introduced. These processes were introduced throughout this intervening period. Table 5 stipulates which processes were already present at the beginning of the series and those that were present by the end. Whilst experience alone may have contributed to shorter operative duration, we believe that the specific processes implemented between these two time points allowed for improved efficiency without compromising patient safety or outcomes.
Table 5.
Lessons Learnt.
| Techniques employed throughout series | Techniques introduced through the series and present at the end of the series | |
|---|---|---|
| Preoperative |
|
|
| Intraoperative |
|
|
| Post-Operative |
|
Preoperatively, patients must have CTA. di Pompeo et al. contend that a ‘free-style’ technique to perforator choice without preoperative CTA did not increase operative time or complications.17 However, our experience is that preoperative CTA allows for accurate preoperative markings, reduces uncertainty during the raise and permits early commitment to one large perforator. This is supported by O'Connor et al. who showed that preoperative CTA saved 13 min in flap harvest time and reduced complications by 4.3%.18 Secondly, preoperative markings are ideally completed prior to the day of operation. The DIEA perforators are identified according to CTA, dopplered out and marked. This practise was adopted to avoid delays in theatre start-time and rushed preoperative markings when the patients were marked in the anaesthetic bay. Furthermore, this provides a valuable opportunity for patients to ask questions and adjust expectations in line with the planned incisions.
Intraoperatively, raising the flap with monopolar diathermy significantly reduces raise time. Whilst this technique remains foreign to many, we believe that plastic surgeons possess the skills to safely transition from traditional bipolar perforator dissection to exclusively monopolar. To begin, surgeons unfamiliar with the technique may start with dissection around the pedicle and progress to perforator dissection when more confident. At first, a single diathermy machine was used and settings were changed as required. This slowed the operation as the scout nurse had to constantly change the diathermy settings. Therefore, multiple diathermy stacks were employed by using one ‘hot’ and one ‘cold’ instrument for the raise, which immediately reduced the operating time as the surgeon did not have to wait for the diathermy settings to change.
Additionally, the flap was disconnected from its donor blood supply as soon as it was raised, regardless of whether the chest wall vessels were ready, so that the ‘bottom team’ could immediately start closing the abdominal donor site or raising the second flap in bilateral cases. As the DIEP flap is adipocutaneous and does not include muscle, it can withstand a long ischaemic time when problems in identifying appropriate recipient vessels are encountered, although this did not occur in this series.
Finally, having a collaborative two-team approach with like-minded surgeons and a consistent nursing team leads to greater familiarity, reduced uncertainty, more confidence and therefore, improved efficiency. Acosta et al. stipulated the importance of having an experienced theatre team in reducing operative time as they demonstrated the feasibility of completing 2 DIEP flaps in a working day.19 Additionally, Sharma et al. showed that having a 100-step process map reduces operative duration. This result, which is similar to our team's approach, showed that a formulaic plan and consistent team leads to shorter operations.20
After achieving these improvements in efficiency, aesthetic outcomes can be prioritised. To provide better abdominal contour, the following steps were employed: subscarpal fat resection on the abdominal flap, liposuction of the mons pubis, plication of the rectus abdominis regardless of whether diastasis is present and using progressive tension sutures as in abdominoplasty techniques. To improve the breast shape, time was taken for preparing pocket with plication inferolaterally, flap coning and finally sitting the patient up or down to allow readjustment.
Post-operatively, patients are managed according to the ERAS principles. Post-operative pain, return to normal gut function and return to safe mobility are the three major factors which determine patient discharge post-DIEP reconstruction. Therefore, intraoperative regional anaesthesia and immediate implementation of the acute pain service is essential. Adequate analgesia also allows early mobilisation. Lastly, allowing the patient to suck ice overnight and upgrading to full diet on day one post-operatively along with aperients mitigates the risk of post-operative ileus and subsequent delayed discharge.21,22
Importance of Operative Efficiency
Operative efficiency is essential in achieving success in DIEP reconstructions and it is well documented that shorter surgeries are safer for patients.23 Moreover, prolonged DIEP operating times are associated with increased rates of flap failure and extended length of hospital stay.24, 25, 26, 27 Haddock et al. examined 1000 DIEP free flaps while controlling for intraoperative complexity and surgeon experience and found that surgical duration is an independent predictor of operative outcomes and length of stay. In fact, with each hour of increased operating time, patient morbidity (unplanned re-operation, donor site complications, fat necrosis, flap compromise/loss and medical complications) increases by 19%.28 Finally, shorter operations, fewer complications, and reduced length of hospital stay decrease healthcare costs.29
A more efficient theatre environment, flap raise and microvascular anastomosis allows for more time to be spent on the aesthetic outcome, in particular, shaping the abdomen and insetting the flap. When achieved, a good aesthetic outcome following DIEP surgery has been shown to significantly improve a patient's psychological well-being.2
Limitations to this study include: firstly, it is a retrospective case series based on a single surgeon's experience; hence, generalisability to surgeons in different contexts may be difficult. Secondly, only univariate analysis was conducted on the relatively small sample size. In addition, we could not assess the individual contribution of each of the introduced processes to the overall improvement in efficiency. Despite this, we believe that this study serves as a tool for junior surgeons to implement and develop strategies to improve efficiency and patient outcomes in what can be a daunting, complex and potentially inefficient procedure. Finally, patient-rated outcomes were outside the scope of this study but demonstrate a future direction for research in examining operative duration.
Conclusion
Through documenting this case series and the specific lessons learnt as a surgeon beginning their career in free DIEP flap breast reconstructions, we provide a guide for junior surgeons to achieve safe and efficient results. With improved operative experience and implementation of a few key steps, operative efficiency will improve, and surgeries will be shorter. A shorter surgery means reduced complications, lower patient morbidity, shorter hospital stay and lesser healthcare costs. Finally, shorter operative times allow the surgical team to place greater emphasis on the final aesthetic outcome, thereby, ensuring that the woman's psychosocial well-being is kept at the forefront of the surgical team's goals.
Disclosure Statements
The authors have no conflicts of interest to declare and did not receive funding for preparation of this manuscript.
Acknowledgments
Acknowledgement
We thank Mr Satyaki Kar for his assistance with the statistical analysis required for this manuscript.
Ethics
Ethics approval for this study was granted by the Western Sydney Local Health District Research and Education Network (2304-02).
Footnotes
This project was presented, in part, as a poster presentation at the Royal Australasian College of Surgeons 91st Annual Scientific Congress from 1-5 May 2023 in Adelaide, Australia.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Dominici L, Hu J, Zheng Y, et al. Association of local therapy with quality-of-life outcomes in young women with breast cancer. JAMA Surg. 2021 Oct 1;156(10) doi: 10.1001/jamasurg.2021.3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grotting JC, Beckenstein MS, Arkoulakis NS. The art and science of autologous breast reconstruction. Breast J. 2003 Sep-Oct;9(5):350–360. doi: 10.1046/j.1524-4741.2003.09527.x. [DOI] [PubMed] [Google Scholar]
- 4.Nahabedian MY. Symmetrical breast reconstruction: Analysis of secondary procedures after reconstruction with implants and autologous tissue. Plast Reconstr Surg. 2005 Jan;115(1):257–260. [PubMed] [Google Scholar]
- 5.Toyserkani NM, Jørgensen MG, Tabatabaeifar S, et al. Autologous versus implant-based breast reconstruction: A systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg. 2020 Feb;73(2):278–285. doi: 10.1016/j.bjps.2019.09.040. [DOI] [PubMed] [Google Scholar]
- 6.Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989 Nov;42(6):645–648. doi: 10.1016/0007-1226(89)90075-1. [DOI] [PubMed] [Google Scholar]
- 7.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994 Jan;32(1):32–38. doi: 10.1097/00000637-199401000-00007. [DOI] [PubMed] [Google Scholar]
- 8.He WY, El Eter L, Yesantharao P, et al. Complications and patient-reported outcomes after TRAM and DIEP flaps: A systematic review and meta-analysis. Plast Reconstr Surg Glob Open. 2020 Oct 29;8(10):e3120. doi: 10.1097/GOX.0000000000003120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg. 2006 May;117(6):1711–1719. doi: 10.1097/01.prs.0000210679.77449.7d. [DOI] [PubMed] [Google Scholar]
- 10.Rozen WM, Ashton MW, Kiil BJ, et al. Avoiding denervation of rectus abdominis in DIEP flap harvest II: an intraoperative assessment of the nerves to rectus. Plast Reconstr Surg. 2008 Nov;122(5):1321–1325. doi: 10.1097/PRS.0b013e3181881e18. [DOI] [PubMed] [Google Scholar]
- 11.Laporta R, Longo B, Sorotos M, et al. Time-dependent factors in DIEP flap breast reconstruction. Microsurgery. 2017 Oct;37(7):793–799. doi: 10.1002/micr.30203. [DOI] [PubMed] [Google Scholar]
- 12.Varnava C, Wiebringhaus P, Hirsch T, et al. Breast reconstruction with DIEP flap: The learning curve at a breast reconstruction center and a single-surgeon study. J Clin Med. 2023 Apr 16;12(8):2894. doi: 10.3390/jcm12082894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grinsell DG, McCoubrey GW, Finkemeyer JP. The deep inferior epigastric perforator learning curve in the current era. Ann Plast Surg. 2016 Jan;76(1):72–77. doi: 10.1097/SAP.0000000000000528. [DOI] [PubMed] [Google Scholar]
- 14.Busic V, Das-Gupta R, Mesic H, Begic A. The deep inferior epigastric perforator flap for breast reconstruction, the learning curve explored. J Plast Reconstr Aesthet Surg. 2006;59(6):580–584. doi: 10.1016/j.bjps.2005.04.061. [DOI] [PubMed] [Google Scholar]
- 15.Hofer SO, Damen TH, Mureau MA, Rakhorst HA, Roche NA. A critical review of perioperative complications in 175 free deep inferior epigastric perforator flap breast reconstructions. Ann Plast Surg. 2007 Aug;59(2):137–142. doi: 10.1097/01.sap.0000253326.85829.45. [DOI] [PubMed] [Google Scholar]
- 16.Cubitt J, Barber Z, Khan AA, et al. Breast reconstruction with deep inferior epigastric perforator flaps. Ann R Coll Surg Engl. 2012 Nov;94(8):552–558. doi: 10.1308/003588412X13373405386457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.di Pompeo FS, Paolini G, D'Orsi G, et al. Free-style technique versus computed tomographic angiography-guided perforator selection in deep inferior epigastric perforator flap harvest: A prospective clinical study. Microsurgery. 2023 Feb 27 doi: 10.1002/micr.31031. [DOI] [PubMed] [Google Scholar]
- 18.O'Connor EF, Rozen WM, Chowdhry M, et al. Preoperative computed tomography angiography for planning DIEP flap breast reconstruction reduces operative time and overall complications. Gland Surg. 2016 Apr;5(2):93–98. doi: 10.3978/j.issn.2227-684X.2015.05.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acosta R, Enajat M, Rozen WM, et al. Performing two DIEP flaps in a working day: an achievable and reproducible practice. J Plast Reconstr Aesthet Surg. 2010 Apr;63(4):648–654. doi: 10.1016/j.bjps.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 20.Sharma HR, Rozen WM, Mathur B, et al. 100 steps of a DIEP flap-A prospective comparative cohort series demonstrating the successful implementation of process mapping in microsurgery. Plast Reconstr Surg Glob Open. 2019 Jan 15;7(1):e2016. doi: 10.1097/GOX.0000000000002016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone JP, Siotos C, Sarmiento S, et al. Implementing our microsurgical breast reconstruction enhanced recovery after surgery pathway: Consensus obstacles and recommendations. Plast Reconstr Surg Glob Open. 2019 Jan 4;7(1):e1855. doi: 10.1097/GOX.0000000000001855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Astanehe A, Temple-Oberle C, Nielsen M, et al. An enhanced recovery after surgery pathway for microvascular breast reconstruction is safe and effective. Plast Reconstr Surg Glob Open. 2018 Jan 18;6(1):e1634. doi: 10.1097/GOX.0000000000001634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howland WS, Schweizer O. Complications associated with prolonged operation and anesthesia. Clin Anesth. 1972;9(1):1–7. [PubMed] [Google Scholar]
- 24.Kotha VS, Abadeer AI, Amdur RL, et al. A critical examination of length of stay in autologous breast reconstruction: A national surgical quality improvement program analysis. Plast Reconstr Surg. 2021 Jan 1;147(1):24–33. doi: 10.1097/PRS.0000000000007420. [DOI] [PubMed] [Google Scholar]
- 25.Frey JD, Salibian AA, Karp NS, et al. Examining length of hospital stay after microsurgical breast reconstruction: Evaluation in a case-control study. Plast Reconstr Surg Glob Open. 2017 Dec 28;5(12):e1588. doi: 10.1097/GOX.0000000000001588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kwok AC, Edwards K, Donato DP, et al. Operative time and flap failure in unilateral and bilateral free flap breast reconstruction. J Reconstr Microsurg. 2018 Jul;34(6):428–435. doi: 10.1055/s-0038-1627445. [DOI] [PubMed] [Google Scholar]
- 27.Marre D, Hontanilla B. Increments in ischaemia time induces microvascular complications in the DIEP flap for breast reconstruction. J Plast Reconstr Aesthet Surg. 2013 Jan;66(1):80–86. doi: 10.1016/j.bjps.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 28.Haddock NT, Wen YE, Steppe C, et al. Operative time predicts postoperative outcomes in bilateral DIEP flap reconstruction: Multivariate 1000 flap analysis. Plast Reconstr Surg Glob Open. 2022 Dec 23;10(12):e4713. doi: 10.1097/GOX.0000000000004713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krishnan NM, Purnell C, Nahabedian MY, et al. The cost effectiveness of the DIEP flap relative to the muscle-sparing TRAM flap in postmastectomy breast reconstruction. Plast Reconstr Surg. 2015 Apr;135(4):948–958. doi: 10.1097/PRS.0000000000001125. [DOI] [PubMed] [Google Scholar]