Abstract
Background
The burden of childhood trauma (violence, injury/illness, loss) in low-resource settings is high, although the effect of trauma on children’s mental and cognitive health is under-researched. Child gender may moderate the association between trauma and outcomes; boys are more likely to experience trauma, but girls are more likely to show distress following trauma.
Methods
We draw on data from the Bachpan cohort (n = 888), a sample of mother-child dyads in rural Pakistan, to investigate these associations among 6-year-old children in a South Asian, low-resource setting. Mothers reported on children’s lifetime exposure to 15 possible traumas and their current mental health. In addition, children were assessed for their verbal skills, working memory, and inhibitory control. We estimated trauma prevalence and used generalized estimating equations to test the association between number of traumatic events and child mental health and cognitive skills in the overall sample and by gender.
Results
90.5% of children experienced at least one trauma. The most common traumas were death of a loved one (47%) and hearing about war/terrorism on the TV/radio (48%). On average, boys experienced more traumas (M = 3.00) than girls (M = 2.67). Specifically, boys were more likely than girls to experience an injury or hospitalization (30% vs. 21%, p < .05) and to hear about war/terrorism on the TV/radio (52% vs. 43%, p < .05). Trauma was associated with increased mental health difficulties and increased anxiety scores. There was little evidence that trauma exposure was associated with child cognitive skills. The strength of association between trauma and outcomes was similar for boys and girls.
Conclusions
Findings show that childhood trauma exposure is common in this setting and associated with worse mental health problems among young boys and girls. Results suggest that trauma-informed interventions are important for supporting child mental health in South Asia.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40359-024-01944-x.
Keywords: Child trauma, Mental health, Cognitive skills, South Asia
Exposure to potentially traumatic events, including interpersonal (e.g., abuse, witnessing violence) and non-interpersonal events (e.g., accidents) is common in children’s lives around the globe [1–4]. In low- and middle-income countries (LMICs), such as Pakistan, the burden of childhood trauma exposure is high, with significant morbidity and mortality associated with childhood exposure to violence and injury [4, 5]. Research suggests a gender difference in rates of trauma exposure in this region, with higher exposure to potentially traumatic events among boys compared to girls [6–8]. Given the high prevalence of childhood trauma exposure, an important priority for public health research is understanding the impact of such exposures on child outcomes, including mental health and cognitive function. Furthermore, understanding gender differences in the associations between trauma exposure and child functioning can aid in identifying populations at risk for adverse outcomes following trauma.
Trauma can encompass several domains of adverse events, including interpersonal events (e.g., directly experiencing abuse, witnessing violence in the home or community), and non-interpersonal events (e.g., injuries, road accidents). In addition, trauma may include large scale events such as natural disasters or war. Although many children show resilience following traumatic events such as these, some children go on to develop mental health difficulties [9–11]. A sizable literature links trauma exposure to post-traumatic stress disorder (PTSD) in youth [12]. This is evident in work in the United States and Europe, and among war-affected populations in Afghanistan, Sri Lanka, Bangladesh, and Nepal [13–19]. In addition to PTSD, research has shown that children exposed to traumatic events are also more likely to experience other mental health difficulties, such as anxiety and depression [20–25]. Specifically, in Pakistan, studies have shown that adolescents with histories of exposure to traumatic events show increased anxiety and PTSD symptoms, decreased prosocial behavior, and increased aggressive behavior [23]. Scholarly work in this region also suggests a gender difference in the association between trauma and child mental health [11, 26, 27]. For instance, Nawaz and colleagues (2018) found that adolescent girls exposed to trauma were more likely to show PTSD symptoms and decreased prosocial behavior, whereas boys exposed to trauma were more likely to show delinquency [28]. Literature in other contexts, such as the United States, also affirms that girls are more likely to show PTSD symptoms and depression following trauma exposure compared to boys [29–34]. This may be due to increased vulnerability to internalizing disorders among girls more generally, which may be driven by several social and physiological factors (e.g., coping styles, social support, stress system functioning) [35]. For instance, girls are more likely to engage in a ruminative response style, which involves passively and repetitively analyzing one’s distress. This coping pattern is associated with worse internalizing symptoms [36].
Trauma exposure may also impact children’s cognitive skills. Although this is an emerging area of research, evidence suggests that exposure to trauma, especially at a young age, is associated with poorer performance on cognitive and memory tasks [13, 37]. However, other studies of executive function do not find a link between trauma and child cognitive skills, suggesting a need for further research in this area [38]. Trauma may impact cognitive skills through its impact on brain development. In particular, trauma exposure may increase activity in stress response systems, which then interferes with the functioning of brain regions involved in memory and executive function, such as the hippocampus and prefrontal cortex [39]. In addition, symptoms of trauma exposure, such as poor concentration, may also impact performance on cognitive tasks [40].
Importantly, much of the research on trauma exposure and child outcomes is conducted in either high-income countries or with highly traumatized populations, such as individuals affected by armed conflict or displacement. However, most of the world’s youth lives in LMIC settings and may be exposed to trauma outside of the severe context of war or migration [41]. Understanding the associations between trauma exposure and child outcomes in LMICs is crucial for building the evidence base for trauma’s effects on children globally. Furthermore, much of the work examining trauma and child development focuses on adolescents. Given that trauma exposure is common during early childhood [42], and this stage is a key sensitive period for brain development [43], an important next step in this research is identifying associations with mental health and cognition earlier in the life course. In particular, middle childhood is a period of extensive social, psychological, and physiological development that may be impacted by trauma exposure [44].
In rural Pakistan, children face many additional adversities, such as poverty and low access to healthcare, that may impact their development alongside trauma. In addition, there are documented differences in how young boys and girls are treated that may inform gender differences in trauma exposure, as well as the effects of trauma. For instance, young boys in Pakistan are encouraged to be autonomous and spend time outside the home [45, 46]. This may give more opportunities for boys to witness accidents or experience injuries themselves, leading to higher rates of trauma exposure. In contrast, parents in Pakistan describe a drive to protect young girls and keep them in the home, which may lead to lower, or differential, exposure to potentially traumatic events [47]. For instance, girls in the home may be more likely to experience household accidents (such as burns), or may be more likely to witness interpersonal violence among family members [48].
The goal of the current study is to characterize trauma exposure and its associations with mental health and cognitive function in a sample of 6-year-old children in rural Pakistan. This study will address key gaps in the literature by focusing on those in middle childhood who live in the often-understudied context of rural Pakistan. We also will expand the literature by addressing both mental and cognitive health outcomes in this sample. We hypothesize that exposure to potentially traumatic events will be associated with increased mental health difficulties and decreased cognitive skills in this sample. We also hypothesize that boys will experience more traumatic events compared to girls. Finally, we will explore whether the associations between trauma and child outcomes differ based on child gender.
Methods
Sample
Data for this cross-sectional analysis come from the 6-year-old wave of the Bachpan Study, with some covariate data drawn from earlier waves. The Bachpan Study is a combined cluster-randomized control trial and cohort study which enrolled women residing in a rural subdistrict of Rawalpindi, Pakistan in their third trimester of pregnancy [49, 50]. Study recruitment took place from December 2014 through August 2016. All participants who screened positive (≥ 10) for depression at baseline according to the 9-item Patient Health Questionnaire (PHQ-9) were randomly assigned at the village cluster level to either a cognitive behavioral therapy-based intervention or enhanced usual care (EUC). About one third of those who screened negative (< 10) were not randomized to intervention or control but were enrolled in the cohort component of the study. Mother-child dyads were followed-up at 3 months, 6 months, 1 year, 2 years, 3 years, 4 years, and 6 years postpartum, with further data collection ongoing [49, 50]. Children available for follow-up at the 6-year-old wave were included in this analysis (N = 898). Trial results at the 3-year follow-up did not show intervention impacts on children’s mental health or cognitive skills [51, 52]. Data collection was performed by trained assessors in the participant’s homes. Assessors interviewed mothers and electronically recorded their responses. Cognitive testing for children was performed in a quiet space in the home where distractions could be minimized. Family members were asked to leave the room during cognitive testing. If family members chose to stay in the room, they were asked, with the help of a field coordinator, to watch the testing quietly without interrupting.
Measures
Exposure
Childhood trauma was assessed at 6-years using the Traumatic Events Screening Inventory- Parent Report Revised (TESI-PRR) [53]. The TESI-PRR consists of 15 parent-reported items assessing the child’s lifetime exposure to potentially traumatic events. Items included: experiencing a serious accident, witnessing a serious accident, experiencing a natural disaster, severe illness or injury of a close friend or relative, death of a close friend or relative, undergoing a serious illness or hospitalization, separation from a parent or caretaker, experiencing physical violence, being threatened with physical violence, being attacked by an animal, witnessing family physical violence, incarceration of a family member, direct exposure to war or terrorism, witnessing war or terrorism on the television or radio, and experiencing psychological violence. Scores on the TESI-PRR range from 0 to 15, with higher scores indicating exposure to a greater number of traumatic events [53–55]. Items on the TESI-PRR were translated into Urdu and adapted for use in Pakistan by the study team. The adult version of this measure has been used previously in LMIC settings [56, 57]. The item assessing sexual abuse was removed from the scale due to concerns around acceptability to participants.
Outcomes
Multiple domains of child mental and cognitive health were included as outcomes in this analysis. Mental health difficulties were measured using the parent-reported Strengths and Difficulties Questionnaire (SDQ) total difficulties score. The SDQ includes 25 items, evaluating emotional symptoms, conduct problems, hyperactivity and inattention, peer relationship problems, and prosocial behaviors. Each item has a response scale of 0–2, with higher scores representing greater levels of mental health difficulties [58]. The total difficulties score is calculated by summing the items on all problem scales, omitting the prosocial behavior scale and has a range from 0 to 40 (α = 0.66). The SDQ has been validated for use in Urdu-speaking populations [59]. Child anxiety was evaluated using the 6-item generalized anxiety disorder subscale of the parent-reported Spence Children’s Anxiety Scale (α = 0.64). Each item has a response scale of 0–3 and total scores range from 0 to 18, with higher scores representing greater levels of anxiety [60].
Four of the Wechsler Preschool and Primary Scale of Intelligence (WPPSI-IV) subtests were used to assess child cognition – picture memory, information, similarities, and vocabulary. The WPPSI picture memory subscale assesses working memory, the information and similarities subscales evaluate verbal comprehension, and the vocabulary subscale is used to measure vocabulary acquisition. The information and similarities subtests were combined into a single verbal comprehension score. Scaled scores ranging from 1 to 19 are calculated for each test. For all subscales, higher scores represent greater cognitive ability for the respective domain [61]. The WPPSI has been translated and adapted for use in Pakistan [62]. The original WPPSI adaptation was conducted with 4 year-old children, which is slightly younger than the current sample. It is likely that this sample is more likely to have attended school compared to the validation sample, which would support their performance on the WPPSI. The Day/Night Stroop task was also used as a measure of working memory and inhibitory control. In the Day/Night task, children are asked to say the word “day” when presented with a picture of the moon and say “night” when shown a picture of the sun. One point is assigned per correct response on the Day/Night task, resulting in a score ranging from 0 to 16, with higher scores representing better working memory and inhibitory control [63]. All cognitive measures were pilot tested prior to data collection.
Potential modifiers and confounders
Child gender was used in this analysis as a potential predictor of child trauma exposure and a potential modifier of the relationship between child trauma and mental and cognitive health. Child gender is mother-reported and was assessed at the 3-month postpartum interview. Household socioeconomic status (SES), maternal education, maternal adverse childhood experiences, and trial arm were included as potential confounders. Trial arm (non-depressed, intervention, or control) was assigned at baseline. Household SES was measured at 6 years follow-up and modeled as a continuous variable using polychoric principal component analysis following the methodology employed in the Demographic and Health Survey Wealth Index [64]. Maternal education was self-reported at baseline in years, and maternal adverse childhood experiences were evaluated at 3 years follow-up using the Adverse Childhood Experience Questionnaire (ACE) [65]. There were no differences in household SES, maternal education, or maternal ACEs by child gender.
Statistical analysis
In this analysis, we used data collected at the 6-year timepoint (N = 898). We first examined the average number of traumatic events per child and the prevalence of having experienced each event in our sample. We used t-tests to evaluate differences in number of trauma exposures by gender and chi-square tests to determine whether there were gendered differences in exposure to each traumatic event. The level of statistical significance was set at p < .05.
We used generalized estimating equations to test the association between number of traumatic events experienced and child mental and cognitive health outcomes [66]. Child mental health outcomes include total mental health difficulties and anxiety. Child cognitive health outcomes include working memory, inhibitory control, vocabulary, and verbal comprehension. We estimated separate models for each outcome and adjusted for household SES, maternal education, and maternal ACEs.
We examined child gender as a modifier between child trauma and mental and cognitive health by creating an interaction term between the number of traumatic events and gender for each aforementioned model. We investigated differences in gender-specific estimates and conducted likelihood ratio tests to determine whether models allowing for modification by gender were a better fit than models simply adjusting for gender [67].
Missing data in analysis was minimal (< 10%), most of which was due to lack of covariate data at 3 years follow-up. The total number of participants included in regression models was 820. We used inverse probability of censoring weighting to account for missingness at 3 years [68].
Results
Descriptive characteristics
Table 1 shows demographic characteristics of children included in the study. Half of the children were female, and their mothers had an average of 7.61 years of education (SD = 4.44) and reported having experienced 1.18 events throughout their lifetime based on the ACE questionnaire (SD = 1.41). At 6-years old, children in the study had experienced, on average, 2.84 traumatic events in the TESI-PRR in their lifetimes. Over 90% of the sample reported at least one traumatic event. The average SDQ total difficulties score among the children (M = 13.04, SD = 4.97) was similar to other community samples in Pakistan [59]. The average WPPSI subtest scores (picture memory: M = 8.54, SD = 3.40; verbal comprehension: M = 16.44, SD = 5.35) were slightly higher compared to other studies of cognitive development of young children in rural Pakistan [62] .
Table 1.
Demographic characteristics of Bachpan Study participants (n = 898)
| Percent or mean (SD) | Range | |
|---|---|---|
| Maternal & household characteristics | ||
| Maternal education (years)b | 7.62 (4.44) | 0–18 |
| Household SES (polychoric PCA score)a | -0.62 (1.13) | |
| Maternal ACE scorec | 1.18 (1.41) | 0–10 |
| Child characteristics | ||
| Number of traumatic eventsa | 2.84 (1.96) | 0–11 |
| Gender (female)a | 49.9% | |
| SDQ total scorea | 13.04 (4.97) | 2–28 |
| SCAS generalized anxietya | 3.41 (2.53) | 0–16 |
| WPPSI picture memorya | 8.54 (3.40) | 1–19 |
| WPPSI verbal comprehensiona | 16.44 (5.35) | 1–38 |
| WPPSI vocabularya | 8.96 (3.01) | 1–19 |
| Day & Night taska | 12.60 (4.64) | 0–16 |
a. Characteristic measured at 6 years follow-up
b. Characteristic measured at baseline
c. Characteristic measured at 3 years follow-up
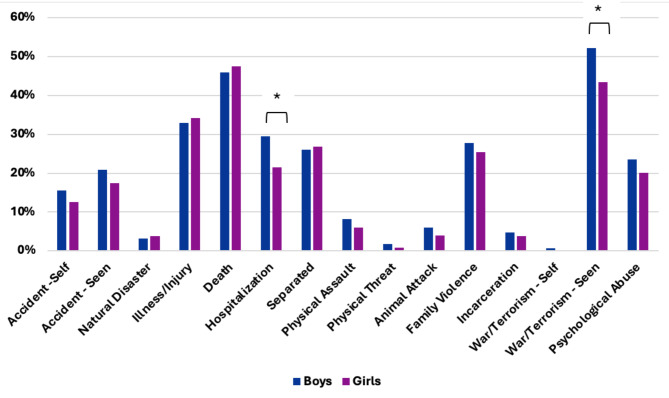
Figure 1 and Supplemental Table 1 show the number of traumatic experiences by gender. Boys experienced, on average, a greater number of traumatic events (M = 3.00) than girls did (M = 2.67, p = .01). The top three most commonly reported items for both genders were witnessing war or terrorism on the television or radio (47.8%), death of a loved one (46.7%), and severe illness or injury of a loved one (33.5%). The least commonly endorsed items were direct exposure to war or terrorism (0.3%) and experiencing threat of physical violence (1.3%). Gender differences were observed in two domains: hospitalization or serious illness and witnessing war or terrorism on the television or radio, with boys being more likely to experience these than girls.
Fig. 1.
Traumatic experiences by child gender. Stars indicate statistically significant (p < .05) difference in prevalence of traumatic event by gender
As shown in Table 2, both mental health scales were positively associated with number of traumatic experiences. For each one-item increase in the TESI-PRR score, the SDQ total score was found, on average, to increase by 0.42 points (95% confidence interval (CI): 0.24, 0.59) and SCAS generalized anxiety score increased by 0.27 points (95% CI: 0.19, 0.36), after adjustment for trial arm, child gender, maternal education, household SES, and maternal ACEs. Standardized estimates are presented in Supplemental Table 2. We did not find evidence for associations between traumatic events and cognitive outcomes, with the exception of vocabulary. There was a positive association between number of traumatic experiences and the WPPSI vocabulary score. We hypothesized that this effect may have been driven by increased exposure to media (i.e., television and radio). So, in a post-hoc sensitivity analysis, we removed the trauma item “witnessed war or terrorism on the television or radio”. When this item was removed, the association between traumatic events and the WPPSI vocabulary score was attenuated towards the null value (Supplemental Table 3).
Table 2.
Association between number of traumatic events and unstandardized mental and cognitive health outcomes among 6-year old children in the Bachpan Cohort, n = 820
| Outcome | Coefficient | 95% Confidence Interval | P-Value |
|---|---|---|---|
| Socioemotional outcomes | |||
| SDQ Total Difficulties Score | 0.42 | (0.24, 0.59) | < 0.0001 |
| SCAS Generalized Anxiety | 0.27 | (0.19, 0.36) | < 0.0001 |
| Cognitive outcomes | |||
| WPPSI Picture Memory | 0.05 | (-0.07, 0.17) | 0.39 |
| WPPSI Verbal Comprehension | 0.15 | (-0.04, 0.34) | 0.11 |
| WPPSI Vocabulary | 0.12 | (0.01, 0.23) | 0.03 |
| Day & Night Task | 0.12 | (-0.05, 0.28) | 0.17 |
Note Estimates are from generalized estimating equations, adjusted for trial arm, child gender, maternal education, household SES, and maternal ACEs. IPCW was used for missingness at 3 years
Table 3 presents gender-specific estimates for interaction models and shows that, for the mental health outcomes, there is a significant, positive association between number of traumatic experiences for girls, but not boys. For instance, for every one point increase on the TESI-PRR, there was a 0.13 point increase in the SDQ total score in boys (95% CI: -0.40, 0.66) and a 0.32 point increase in girls (95% CI: 0.09, 0.56). However, the likelihood ratio tests for models with the interaction term did not provide substantial evidence that they were a better fit with an interaction between trauma and gender included than a model controlling for gender.
Table 3.
Association between traumatic events and mental and cognitive health outcomes, interaction by gender
| Gender Girls: (n = 410) Boys: (n = 410) |
Coefficient | 95% Confidence Interval | LRT P-Value | |
|---|---|---|---|---|
| SDQ Total Difficulties Score | Boys | 0.13 | (-0.40, 0.66) | 0.26 |
| Girls | 0.32 | (0.09, 0.56) | ||
| SCAS Generalized Anxiety | Boys | 0.09 | (-0.18, 0.35) | 0.15 |
| Girls | 0.21 | (0.10, 0.33) | ||
| WPPSI Picture Memory | Boys | -0.09 | (-0.47, 0.28) | 0.42 |
| Girls | 0.01 | (-0.16, 0.17) | ||
| WPPSI Verbal comprehension | Boys | 0.16 | (-0.41, 0.74) | 0.96 |
| Girls | 0.15 | (-0.10, 0.41) | ||
| WPPSI Vocabulary | Boys | -0.06 | (-0.38, 0.27) | 0.26 |
| Girls | 0.06 | (-0.08, 0.21) | ||
| Day & Night Task | Boys | -0.05 | (-0.55, 0.46) | 0.51 |
| Girls | 0.06 | (-0.16, 0.29) |
Note Estimates are from generalized estimating equations, adjusted for trial arm, maternal education, household SES, and maternal ACEs. IPCW was used for missingness at 3 years
Discussion
In this study, we examined exposure to potentially traumatic events and child mental health and cognitive outcomes in a sample of 6-year-olds in rural Pakistan. We found that exposure to trauma was highly prevalent in this sample, with 90.5% of mothers reporting their child experienced at least one potentially traumatic event in their lifetime. We also found that boys were exposed to more traumatic events overall than girls, a difference driven by higher prevalence of hospitalization/illness and seeing or hearing about war/terrorism on TV/Radio. Finally, exposure to potentially traumatic events was associated with increased total mental health difficulties and increased anxiety, but much less so with cognitive function, among both boys and girls.
The high prevalence of exposure to at least one potentially traumatic event aligns with previous work showing the ubiquity of trauma exposure globally [3]. The most common exposures in this sample were death of a loved one, serious illness or injury of a loved one, and exposure to war or terrorism on the TV/radio. Previous work in Pakistan has shown that exposure to violence through the media is common and can be harmful for youth mental health [69, 70]. While the high prevalence applied to all children, we found that boys were exposed to more events than girls. Specifically, boys were more likely to experience a hospitalization or illness and were more likely to see or hear about war/terrorism through the media. Previous work has also shown that boys are more likely to experience trauma, especially accidents or injuries [8]. This gender difference may be due to differences in how boys and girls are encouraged to spend their time. Previous qualitative work in Pakistan has shown that boys are encouraged to play independently outside the home, whereas girls are encouraged to stay in the home [45, 47, 71]. For boys, this increased freedom may also lead to increased risk for injuries requiring hospitalization. In terms of media exposure, some work shows that caregivers in Pakistan are protective of their young girls, and thus may be more likely to shield them from distressing media exposure (such as the news) [72]. In addition, girls in this setting may be less likely to watch TV or listen to the radio in general because they are expected to spend more time on household chores [47]. This may result in higher rates of exposure to war/terrorism in the media for boys compared to girls.
Our findings that exposure to potentially traumatic effects was associated with worse mental health aligns with the broader literature showing that trauma exposure is deleterious to mental health [12]. The effects in this study are somewhat smaller than other studies examining mental health and trauma in children, although estimates across studies vary. For instance, in a sample of Afghani adolescents, Panter-Brick and colleagues (2011) found that SDQ scores increased by 0.16 points following the death of a family member in the previous year and 3.19 points after witnessing family violence in the previous year [73]. In a sample of children from a post-conflict setting in Uganda, Catani and colleagues (2016) found a 0.21–0.24 standard deviation (about 1 point) increase in SDQ scores for each reported traumatic event, which included war-related trauma and family violence [74]. In our study, each increase in traumatic events was associated with an increase of 0.42 points on the SDQ. Our work differs from these studies in important ways, such as the timing and type of trauma exposure, but further supports the conclusion that trauma exposure is associated with worse child mental health.
While much of the existing research examines adolescents, our study extends these findings to middle childhood. They are also consistent with several proposed mechanisms of how trauma may impact brain development. For example, children who experience trauma early in life may have differences in stress responsivity that predispose them to mental health challenges, such as altered physiological stress reactivity [75] and increased amygdala reactivity [76, 77]. These physiological changes can underlie heightened emotional reactivity to stress and problems with emotion regulation [78]. Psychologically, children exposed to trauma may have biases in how they perceive the world that increase their susceptibility to mental health concerns, including hypervigilance to threat, or a view that the world is scary or unsafe [78].
There was little evidence that trauma exposure was associated with cognitive skills in this study. There are few other studies investigating trauma exposure and cognitive functioning among children in LMIC contexts. In a sample in Colombia, Duque (2017) found that exposure to violence in early childhood was associated with reduced language and math skills [79]. Other studies in LMICs show that children who experience trauma and go on to develop PTSD perform worse on cognitive tasks [13, 80, 81]. Our results may differ from other studies in LMICs because we focus on traumatic events exposure, rather than PTSD symptoms. In general, more research is needed on these associations in LMIC contexts.
We found a positive association between trauma and vocabulary. However, in sensitivity analyses, we found that this effect was driven by the radio/tv item. When this item was removed from analyses, there was no longer a statistically significant association between trauma and vocabulary (see Supplemental Table 3). It is possible that exposure to media was a confounder in the association between trauma and verbal skills. Children who have high media exposure may be more likely to be exposed to distressing content (i.e., war or terrorism), but also may be more exposed to varied information and language that then leads to improved verbal skills. Future research may explore the potential trade-off between exposure to distressing information and exposure to language when allowing children to engage with media.
We did not find a statistically significant gender difference in the relationship between traumatic events and child mental and cognitive health in this sample. It is possible that a gender difference may emerge as children age into adolescence when many psychological disorders first onset. Indeed, there is evidence that gender differences in trauma-related mental health difficulties don’t emerge until adolescence [82] and much of the evidence for gender differences is among adolescents and adults [32, 83]. This also may reflect the relative lack of gender differences in trauma exposure in this sample. There were no events that were more prevalent in girls compared to boys that may have contributed to variation in mental health symptoms between genders.
The results of this study should be interpreted in the context of several limitations. First, our measure of trauma was mother reported and assessed for lifetime exposure to potentially traumatic events for the child. Given the age of the children, parent report was appropriate. However, this measure does not assess the child’s reaction to each traumatic event, just whether the child experienced it. Therefore, we do not have information on whether the child was distressed by the reported events. In addition, all events in our measure are weighted equally, but each event may vary in terms of severity (e.g., experiencing violence may have a stronger impact on children compared to witnessing violence). There is emerging research to suggest that type of traumatic event may be an important predictor of child outcomes, with events characterized by threat showing different associations than events characterized by deprivation [84, 85]. While this distinction was outside the scope of our study, it could be considered in future research.
Furthermore, our measure of trauma assessed for lifetime exposure, so we do not have information on when these events occurred in relation to our measures of mental health and cognitive development. It is possible that more recent events would be more impactful on child mental health compared to more distal events, especially if children do not remember more distal events. There also may be recall bias, with mothers being more likely to remember severe events compared to less severe events. We are also not able to differentiate events that occurred once or multiple times. In addition, our measure of trauma does not include questions about childhood sexual abuse. This was based on concerns around stigma and under-reporting. However, by missing information on childhood sexual abuse, we may also be missing an important source of gender differences in trauma exposure, as sexual abuse is more common in girls compared to boys [86].
In addition, our measures of child mental health were mother reported, which may introduce bias. Specifically, mothers who reported more traumatic events for their children may think they are more distressed and thus report more mental health symptoms. Future studies may use multiple reporting methods to assess child mental health, including self-report, teacher report, and observational measures, to better understand the association between trauma and mental health. It should be noted that the reliability estimates for our mental health measures were low, suggesting that the items on these measures may not be capturing unified constructs. The limitations of the SDQ in particular have been noted in the literature [87], further underscoring the need for multiple measures of mental health in future research. Finally, our analysis was cross-sectional. Future research would benefit from examining the longitudinal impact of childhood trauma on mental health and cognitive development.
Our study also has several strengths, including a rich dataset with information on multiple aspects of child mental health and cognitive development. In addition, our sample size was large enough to investigate gender differences in trauma exposure and child outcomes. Finally, this study focuses on an under-researched population in rural Pakistan, furthering our understanding of trauma exposure and child development across diverse contexts.
Overall, our study suggests that trauma is associated with mental health difficulties in young children in rural Pakistan, and points to the importance of addressing the mental health sequalae of trauma exposure in this population. Future research could expand on this work with fine-grained measures of trauma exposure to investigate how to the frequency, severity, and type of trauma may impact child development. Furthermore, next steps in this research could involve examining the child-, family-, and neighborhood-level factors that may buffer children from the harmful effects of trauma. Such work could inform interventions aimed at improving child mental health globally.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank the team at the Human Development Research Foundation (HDRF) including Rakshanda Liaqat, Tayyiba Abbasi, Maria Sharif, Samina Bilal, Anum Nisar, Amina Bibi, Shaffaq Zufiqar, Ahmed Zaidi, Ikhlaq Ahmad, and Najia Atif. Finally, we are very grateful to the families who participated in the study.
Author contributions
AF and AC conceptualized the analysis and drafted the manuscript. AC analyzed the data. JM further contributed to data interpretation. AF, AC, EC, MEC, AH, SG, AB, SS, and JM contributed substantively to revisions and final edits. JM and SS designed the larger study. AB and SS led data collection for this study. AF, AC, EC, MEC, AH, SG, AB, SS, and JM approved the final version to be submitted for publication, and AF was responsible for final submission.
Funding
The Bachpan cohort was established by funding through the Human Development Research Foundation and leveraging the research study funded by the National Institute of Mental Health (U19MH95687) and National Institute of Child Health and Development (R01 HD075875; PI: Maselko).
Data availability
The datasets used during the current study are available from the Principal Investigator, Joanna Maselko, on reasonable request.
Declarations
Ethical approval
This study was approved by the institutional review boards at the Human Development Research Foundation (IRB/1017/2021), Duke University, and the University of North Carolina at Chapel Hill (#20–1433) in accordance with the “Common Rule” set out in the Belmont Report and the Declaration of Helsinki. Written informed consent was obtained from a parent/guardian, or if the parent was illiterate, witnessed verbal informed consent was obtained. Verbal informed assent was also obtained from children.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Catani C, Schauer E, Neuner F. Beyond individual war trauma: domestic violence against children in Afghanistan and Sri Lanka. J Marital Fam Ther. 2008;34(2):165–76. 10.1111/j.1752-0606.2008.00062.x [DOI] [PubMed] [Google Scholar]
- 2.Haque MA, Moniruzzaman S, Janson S, Rahman AF, Mashreky SR, Eriksson UB. Children’s exposure to psychological abuse and neglect: a population-based study in rural Bangladesh. Acta Paediatr. 2021;110(1):257–64. 10.1111/apa.15340 [DOI] [PubMed] [Google Scholar]
- 3.Hillis S, Mercy J, Amobi A, Kress H. Global prevalence of past-year violence against children: a systematic review and minimum estimates. Pediatrics. 2016;137(3). [DOI] [PMC free article] [PubMed]
- 4.Hyder AA, Razzak JA. The challenges of injuries and trauma in Pakistan: an opportunity for concerted action. Public Health. 2013;127(8):699–703. 10.1016/j.puhe.2012.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiragu AW, Dunlop SJ, Mwarumba N, Gidado S, Adesina A, Mwachiro M, et al. Pediatric Trauma Care in Low Resource settings: challenges, opportunities, and solutions. Front Pediatr. 2018;6:155. 10.3389/fped.2018.00155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbas SS, Jabeen T. Prevalence of child abuse among the University students: a retrospective cross-sectional study in University of the Punjab, Pakistan. Int Q Community Health Educ. 2020;40(2):125–34. 10.1177/0272684X19861578 [DOI] [PubMed] [Google Scholar]
- 7.Gray C, Pence B, Ostermann J, Whetten R, O’Donnell K, Thielman N, et al. Gender (in) differences in prevalence and incidence of traumatic experiences among orphaned and separated children living in five low-and middle-income countries. Global Mental Health. 2015;2:e3. 10.1017/gmh.2015.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lasi S, Rafique G, Peermohamed H. Childhood injuries in Pakistan: results from two communities. J Health Popul Nutr. 2010;28(4):392–8. 10.3329/jhpn.v28i4.6046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Masoom Ali S, Yildirim M, Abdul Hussain S, Vostanis P. Self-reported mental health problems and post-traumatic growth among children in Pakistan care homes. Asia Pac J Social Work Dev. 2020;30(1):62–76. 10.1080/02185385.2019.1710726 [DOI] [Google Scholar]
- 10.Ungar M. Resilience, trauma, context, and culture. Trauma Violence Abuse. 2013;14(3):255–66. 10.1177/1524838013487805 [DOI] [PubMed] [Google Scholar]
- 11.Escobar Carías MS, Johnston DW, Knott R, Sweeney R. Flood disasters and health among the urban poor. Health Econ. 2022;31(9):2072–89. 10.1002/hec.4566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alisic E, Zalta AK, Van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, et al. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. Br J Psychiatry. 2014;204(5):335–40. 10.1192/bjp.bp.113.131227 [DOI] [PubMed] [Google Scholar]
- 13.Elbert T, Schauer M, Schauer E, Huschka B, Hirth M, Neuner F. Trauma-related impairment in children—A survey in Sri Lankan provinces affected by armed conflict. Child Abuse Negl. 2009;33(4):238–46. 10.1016/j.chiabu.2008.02.008 [DOI] [PubMed] [Google Scholar]
- 14.Kumar M, Fonagy P. Differential effects of exposure to social violence and natural disaster on children’s mental health. J Trauma Stress. 2013;26(6):695–702. 10.1002/jts.21874 [DOI] [PubMed] [Google Scholar]
- 15.Neuner F, Schauer E, Catani C, Ruf M, Elbert T. Post-tsunami stress: a study of posttraumatic stress disorder in children living in three severely affected regions in Sri Lanka. J Trauma Stress: Official Publication Int Soc Trauma Stress Stud. 2006;19(3):339–47. 10.1002/jts.20121 [DOI] [PubMed] [Google Scholar]
- 16.O’Connor K, Seager J. Displacement, violence, and mental health: evidence from Rohingya adolescents in Cox’s bazar. Bangladesh Int J Environ Res Public Health. 2021;18(10):5318. 10.3390/ijerph18105318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Panter-Brick C, Eggerman M, Gonzalez V, Safdar S. Violence, suffering, and mental health in Afghanistan: a school-based survey. Lancet. 2009;374(9692):807–16. 10.1016/S0140-6736(09)61080-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajan V, Neuner F, Catani C. Explaining the accumulation of victimization in vulnerable children: interpersonal violence among children traumatized by war and disaster in a children’s home in Sri Lanka. Dev Psychopathol. 2022;34(1):147–56. 10.1017/S0954579420001078 [DOI] [PubMed] [Google Scholar]
- 19.Silwal S, Chudal R, Dybdahl R, Sillanmäki L, Lien L, Sourander A. Post-traumatic stress and depressive symptoms among adolescents after the 2015 earthquake in Nepal: a longitudinal study. Child Psychiatry Hum Dev. 2021;1:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Catani C, Gewirtz AH, Wieling E, Schauer E, Elbert T, Neuner F. Tsunami, war, and cumulative risk in the lives of Sri Lankan schoolchildren. Child Dev. 2010;81(4):1176–91. 10.1111/j.1467-8624.2010.01461.x [DOI] [PubMed] [Google Scholar]
- 21.Dhakal S, Niraula S, Sharma NP, Sthapit S, Bennett E, Vaswani A, et al. History of abuse and neglect and their associations with mental health in rescued child labourers in Nepal. Australian New Z J Psychiatry. 2019;53(12):1199–207. 10.1177/0004867419853882 [DOI] [PubMed] [Google Scholar]
- 22.Fernando GA, Miller KE, Berger DE. Growing pains: the impact of disaster-related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child Dev. 2010;81(4):1192–210. 10.1111/j.1467-8624.2010.01462.x [DOI] [PubMed] [Google Scholar]
- 23.Khan NZ, Shilpi AB, Sultana R, Sarker S, Razia S, Roy B, et al. Displaced rohingya children at high risk for mental health problems: findings from refugee camps within Bangladesh. Child Care Health Dev. 2019;45(1):28–35. 10.1111/cch.12623 [DOI] [PubMed] [Google Scholar]
- 24.Kohrt BA, Jordans MJ, Tol WA, Speckman RA, Maharjan SM, Worthman CM, et al. Comparison of mental health between former child soldiers and children never conscripted by armed groups in Nepal. JAMA. 2008;300(6):691–702. 10.1001/jama.300.6.691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sriskandarajah V, Neuner F, Catani C. Parental care protects traumatized Sri Lankan children from internalizing behavior problems. BMC Psychiatry. 2015;15(1):1–11. 10.1186/s12888-015-0583-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Datar A, Liu J, Linnemayr S, Stecher C. The impact of natural disasters on child health and investments in rural India. Soc Sci Med. 2013;76:83–91. 10.1016/j.socscimed.2012.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Axinn WG, Ghimire DJ, Williams NE, Scott KM, Gender. Traumatic events, and Mental Health Disorders in a rural Asian setting. J Health Soc Behav. 2013;54(4):444–61. 10.1177/0022146513501518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nawaz N, Khalily MT, Gul S. Outcomes of trauma exposure among adolescents of Pakistan: role of PTSD and social support. Pakistan Armed Forces Med J. 2018;68(6):1737–43. [Google Scholar]
- 29.Ascienzo S, Sprang G, Royse D. Gender differences in the PTSD symptoms of polytraumatized youth during isolated phases of trauma-focused cognitive behavioral therapy. Psychological trauma: theory, research, practice, and policy. 2022;14(3):488. [DOI] [PubMed]
- 30.Craig CD, Sprang G. Gender differences in trauma treatment: do boys and girls respond to evidence-based interventions in the same way? Violence Vict. 2014;29(6):927–39. 10.1891/0886-6708.VV-D-13-00016 [DOI] [PubMed] [Google Scholar]
- 31.Schwartz B, Kaminer D, Hardy A, Nöthling J, Seedat S. Gender differences in the violence exposure types that predict PTSD and depression in adolescents. J Interpers Violence. 2021;36(17–18):8358–81. 10.1177/0886260519849691 [DOI] [PubMed] [Google Scholar]
- 32.Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Trauma: Theory Res Pract Policy. 2008;S(1):37–85. 10.1037/1942-9681.S.1.37 [DOI] [PubMed] [Google Scholar]
- 33.Wamser-Nanney R, Cherry KE. Children’s trauma-related symptoms following complex trauma exposure: evidence of gender differences. Child Abuse Negl. 2018;77:188–97. 10.1016/j.chiabu.2018.01.009 [DOI] [PubMed] [Google Scholar]
- 34.Zona K, Milan S. Gender differences in the longitudinal impact of exposure to violence on mental health in urban youth. J Youth Adolesc. 2011;40:1674–90. 10.1007/s10964-011-9649-3 [DOI] [PubMed] [Google Scholar]
- 35.Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocr. 2014;35(3):320–30. 10.1016/j.yfrne.2014.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4(2):146–58. 10.1016/S2215-0366(16)30263-2 [DOI] [PubMed] [Google Scholar]
- 37.Enlow MB, Egeland B, Blood EA, Wright RO, Wright RJ. Interpersonal trauma exposure and cognitive development in children to age 8 years: a longitudinal study. J Epidemiol Community Health. 2012;66(11):1005–10. 10.1136/jech-2011-200727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohodes EM, Chen SH, Lieberman AF, Bush NR. Examination of the associations between young children’s trauma exposure, trauma-symptomatology, and executive function. Child Abuse Negl. 2020;108:104635. 10.1016/j.chiabu.2020.104635 [DOI] [PubMed] [Google Scholar]
- 39.Cross D, Fani N, Powers A, Bradley B. Neurobiological development in the context of childhood trauma. Clin Psychol Sci Pract. 2017;24(2):111. 10.1111/cpsp.12198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Streeck-Fischer A, van der Kolk BA. Down will come baby, cradle and all: diagnostic and therapeutic implications of chronic trauma on child development. Australian New Z J Psychiatry. 2000;34(6):903–18. 10.1080/000486700265 [DOI] [PubMed] [Google Scholar]
- 41.Nations U. World population prospects: the 2017 revision, key findings and advance tables. Volume 46. editor New York: United Nations.: Department of Economics and Social Affairs PD; 2017. [Google Scholar]
- 42.Koenen KC, Roberts AL, Stone DM, Dunn EC. The epidemiology of early childhood trauma. The impact of early life trauma on health and disease: The hidden epidemic. 2010;1.
- 43.Luby JL, Baram TZ, Rogers CE, Barch DM. Neurodevelopmental optimization after early-life Adversity: Cross-species studies to elucidate sensitive periods and brain mechanisms to inform early intervention. Trends Neurosci. 2020;43(10):744–51. 10.1016/j.tins.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DelGiudice M. Middle childhood: An evolutionary-developmental synthesis. Handbook of life course health development. 2018:95–107.
- 45.Ahmed M, Zaman M. Children’s self-concept of their well-being in Rawalpindi and Islamabad: actor’s perspectives of identity and existence. Child Indic Res. 2019;12:501–23. 10.1007/s12187-018-9552-5 [DOI] [Google Scholar]
- 46.Stewart SM, Zaman RM, Dar R. Autonomy as a psychological need: perceptions of Pakistani mothers. Psychol Developing Soc. 2006;18(2):227–39. 10.1177/097133360601800205 [DOI] [Google Scholar]
- 47.Zaman RM. Parenting in Pakistan: an overview. In: Selin H, editor. Parenting across cultures: Childrearing, Motherhood and Fatherhood in non-western cultures. Dordrecht: Springer Netherlands; 2014. pp. 91–104. [Google Scholar]
- 48.Iqbal M, Fatmi Z. Prevalence of emotional and physical intimate partner violence among married women in Pakistan. J Interpers Violence. 2021;36(9–10):NP4998–5013. 10.1177/0886260518796523 [DOI] [PubMed] [Google Scholar]
- 49.Sikander S, Ahmad I, Bates LM, Gallis J, Hagaman A, O’Donnell K, et al. Cohort Profile: perinatal depression and child socioemotional development; the Bachpan cohort study from rural Pakistan. BMJ open. 2019;9(5):e025644. 10.1136/bmjopen-2018-025644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Turner EL, Sikander S, Bangash O, Zaidi A, Bates L, Gallis J, et al. The effectiveness of the peer delivered thinking healthy plus (THPP+) Programme for maternal depression and child socio-emotional development in Pakistan: study protocol for a three-year cluster randomized controlled trial. Trials. 2016;17(1):1–11. 10.1186/s13063-016-1530-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sevim D, Baranov V, Bhalotra S, Maselko J, Biroli P. Trajectories of Early Childhood Skill Development and Maternal Mental Health. J Hum Resour. 2024;59(S):S365–401. 10.3368/jhr.1222-12693R3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maselko J, Sikander S, Turner EL, Bates LM, Ahmad I, Atif N, et al. Effectiveness of a peer-delivered, psychosocial intervention on maternal depression and child development at 3 years postnatal: a cluster randomised trial in Pakistan. Lancet Psychiatry. 2020;7(9):775–87. 10.1016/S2215-0366(20)30258-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ippen CG, Ford J, Racusin R, Acker M, Bosquet K, Ellis C, et al. Traumatic events screening inventory- parent report revised. White River Junction. UT.: National Center for PTSD and Dartmouth Child Psychiatry Research Group; 2002.
- 54.Choi KR, McCreary M, Ford JD, Rahmanian Koushkaki S, Kenan KN, Zima BT. Validation of the traumatic events screening inventory for ACEs. Pediatrics. 2019;143(4). [DOI] [PubMed]
- 55.Strand VC, Sarmiento TL, Pasquale LE. Assessment and screening tools for trauma in children and adolescents: a review. Trauma Violence Abuse. 2005;6(1):55–78. 10.1177/1524838004272559 [DOI] [PubMed] [Google Scholar]
- 56.Boşgelmez Ş, Aker T, Köklük ÖA, Ford JD. Assessment of lifetime history of exposure to traumatic stressors by incarcerated adults with the Turkish version of the traumatic events screening instrument for adults (TESI-A): a pilot study. J Trauma Dissociation. 2010;11(4):407–23. 10.1080/15299731003783212 [DOI] [PubMed] [Google Scholar]
- 57.Closson K, Dietrich JJ, Nkala B, Musuku A, Cui Z, Chia J, et al. Prevalence, type, and correlates of trauma exposure among adolescent men and women in Soweto, South Africa: implications for HIV prevention. BMC Public Health. 2016;16(1):1–15. 10.1186/s12889-016-3832-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1337–45. 10.1097/00004583-200111000-00015 [DOI] [PubMed] [Google Scholar]
- 59.Samad L, Hollis C, Prince M, Goodman R. Child and adolescent psychopathology in a developing country: testing the validity of the strengths and difficulties questionnaire (Urdu version). Int J Methods Psychiatr Res. 2005;14(3):158–66. 10.1002/mpr.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav Res Ther. 2004;42(7):813–39. 10.1016/S0005-7967(03)00200-6 [DOI] [PubMed] [Google Scholar]
- 61.Wechsler D. Wechsler preschool and primary scale of intelligence—fourth edition. TX: The Psychological Corporation San Antonio; 2012. [Google Scholar]
- 62.Rasheed MA, Pham S, Memon U, Siyal S, Obradović J, Yousafzai AK. Adaptation of the Wechsler Preschool and primary scale of Intelligence-III and lessons learned for evaluating intelligence in low-income settings. Int J School Educational Psychol. 2018;6(3):197–207. 10.1080/21683603.2017.1302851 [DOI] [Google Scholar]
- 63.Gerstadt CL, Hong YJ, Diamond A. The relationship between cognition and action: performance of children 312–7 years old on a stroop-like day-night test. Cognition. 1994;53(2):129–53. 10.1016/0010-0277(94)90068-X [DOI] [PubMed] [Google Scholar]
- 64.Maselko J, Bates L, Bhalotra S, Gallis JA, O’Donnell K, Sikander S, et al. Socioeconomic status indicators and common mental disorders: evidence from a study of prenatal depression in Pakistan. SSM-population Health. 2018;4:1–9. 10.1016/j.ssmph.2017.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–58. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 66.Hanley JA, Negassa A, Edwardes MDd, Forrester JE. Statistical analysis of Correlated Data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–75. 10.1093/aje/kwf215 [DOI] [PubMed] [Google Scholar]
- 67.Lewis F, Butler A, Gilbert L. A unified approach to model selection using the likelihood ratio test. Methods Ecol Evol. 2011;2(2):155–62. 10.1111/j.2041-210X.2010.00063.x [DOI] [Google Scholar]
- 68.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–95. 10.1177/0962280210395740 [DOI] [PubMed] [Google Scholar]
- 69.Khalily N. The unrelenting media exposure in Pakistan and its link with vicarious trauma. Bahria J Prof Psychol. 2017;16(1):67–79. [Google Scholar]
- 70.Khan MA, Rawan B, Ullah A. Growing up with media violence and psychological trauma among youth in Pakistan. Pakistan J Criminol. 2020;12(1):79–88. [Google Scholar]
- 71.Stewart SM, Bond MH, Chan W, Zaman RM, Dar R, Anwar M. Autonomy from parents and psychological adjustment in an interdependent culture. Psychol Developing Soc. 2003;15(1):31–49. 10.1177/097133360301500103 [DOI] [Google Scholar]
- 72.Kausar R, Shafique N. Gender differences in perceived parenting styles and socioemotional adjustment of adolescents. Pakistan J Psychol Res. 2008:93–105.
- 73.Panter-Brick C, Goodman A, Tol W, Eggerman M. Mental Health and Childhood adversities: a longitudinal study in Kabul, Afghanistan. J Am Acad Child Adolesc Psychiatry. 2011;50(4):349–63. 10.1016/j.jaac.2010.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Catani C, Ertl V, Neuner F, Saile R. Children of the postwar years: a two-generational multilevel risk assessment of child psychopathology in northern Uganda. Dev Psychopathol. 2016;28(2):607–20. 10.1017/S0954579415001066 [DOI] [PubMed] [Google Scholar]
- 75.Siciliano RE, Anderson AS, Compas BE. Autonomic nervous system correlates of posttraumatic stress symptoms in youth: meta-analysis and qualitative review. Clin Psychol Rev. 2022;92:102125. 10.1016/j.cpr.2022.102125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, et al. Heightened neural reactivity to threat in child victims of family violence. Curr Biol. 2011;21(23):R947–8. 10.1016/j.cub.2011.10.015 [DOI] [PubMed] [Google Scholar]
- 77.Suzuki H, Luby JL, Botteron KN, Dietrich R, McAvoy MP, Barch DM. Early life stress and trauma and enhanced limbic activation to emotionally valenced faces in depressed and healthy children. J Am Acad Child Adolesc Psychiatry. 2014;53(7):800–13. e10. 10.1016/j.jaac.2014.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McLaughlin KA, Lambert HK. Child trauma exposure and psychopathology: mechanisms of risk and resilience. Curr Opin Psychol. 2017;14:29–34. 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Duque V. Early-life conditions and child development: evidence from a violent conflict. SSM - Popul Health. 2017;3:121–31. 10.1016/j.ssmph.2016.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Scharpf F, Mueller SC, Masath FB, Nkuba M, Hecker T. Psychopathology mediates between maltreatment and memory functioning in Burundian refugee youth. Child Abuse Negl. 2021;118:105165. 10.1016/j.chiabu.2021.105165 [DOI] [PubMed] [Google Scholar]
- 81.Schoeman R, Carey P, Seedat S. Trauma and posttraumatic stress disorder in South African adolescents: a case-control study of cognitive deficits. J Nerv Ment Dis. 2009;197(4):244–50. 10.1097/NMD.0b013e31819d9533 [DOI] [PubMed] [Google Scholar]
- 82.Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psychol Rev. 2012;32(2):122–38. 10.1016/j.cpr.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 83.Hanson RF, Self-Brown S, Borntrager C, Kilpatrick DG, Saunders BE, Resnick HS, et al. Relations among gender, violence exposure, and mental health: the national survey of adolescents. Am J Orthopsychiatry. 2008;78(3):313–21. 10.1037/a0014056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–91. 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Johnson D, Policelli J, Li M, Dharamsi A, Hu Q, Sheridan MA, et al. Associations of early-life threat and deprivation with executive functioning in Childhood and Adolescence: a systematic review and Meta-analysis. JAMA Pediatr. 2021;175(11):e212511. 10.1001/jamapediatrics.2021.2511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta-analysis. Int J Public Health. 2013;58:469–83. 10.1007/s00038-012-0426-1 [DOI] [PubMed] [Google Scholar]
- 87.Kankaanpää R, Töttö P, Punamäki R-L, Peltonen K. Is it time to revise the SDQ? The psychometric evaluation of the strengths and difficulties Questionnaire. Psychol Assess. 2023. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used during the current study are available from the Principal Investigator, Joanna Maselko, on reasonable request.