Abstract
Context:
The limb symmetry index (LSI) is recommended as a milestone of return to play (RTP), and relying on the LSI value of a single-leg hop for distance (SLHD) test may overestimate rehabilitation status. Identifying a more reliable functional test can help to carefully make decisions for RTP.
Objective:
The aim was to compare the LSI value of the SLHD test with that of a single-leg vertical jump (SLVJ) test after anterior cruciate ligament reconstruction (ACLR) and determine which test provides lower LSI values.
Data Sources:
The PubMed, Web of Science, Embase, and Cochrane Library databases were searched from inception to July 2022.
Study Selection:
Observational studies with participants who had both SLHD and SLVJ tests after ACLR and LSI values of an SLHD and SLVJ were included. Disagreements were resolved after discussion between the 2 researchers.
Study Design:
Systematic review and meta-analysis.
Level of Evidence:
Level 4.
Data Extraction:
Data on the primary outcomes (LSI values of the SLVJ and SLHD tests) were collected. Means and standard deviations (SDs) for each variable of interest were used to calculate standardized mean differences (SMDs).
Results:
A total of 12 studies met the inclusion criteria for the meta-analysis. A total of 587 patients underwent SLHD and SLVJ tests at different time points after ACLR. Compared with the SLHD test, the SLVJ test provided lower LSI values (SMD -0.42; 95% confidence interval (CI) -0.67 to -0.17). Subgroup analysis found that the SLVJ test provided a lower LSI value than the SLHD test in a specific period (approximately 7-18 months after ACLR, SMD -0.53; 95% CI -0.91 to -0.14) and a similar LSI value at other times.
Conclusion:
The SLVJ test provided lower LSI values in a specific period (7-18 months after ACLR).
Keywords: anterior cruciate ligament, hop for distance, limb symmetry index, meta-analysis, vertical jump
Despite the mechanical stability of an injured knee being restored by anterior cruciate ligament (ACL) reconstruction (ACLR), return to play (RTP) is still not guaranteed for many people, and nearly 25% of athletes who undergo ACLR suffer a secondary injury after RTP.17,40
A successful surgical outcome is related to rigorous rehabilitation after ACLR and the moment of RTP.22,39 To achieve the goal of RTP, complications and functional deficits after ACLR, such as decreased muscle size and quadricep and hamstring strength and proprioceptive deficiency, need to be resolved by rehabilitation.4,6,32 The moment of RTP is closely related to the prognosis of patients, and the inappropriate estimation of rehabilitation efficacy and premature RTP will increase the risk of secondary injury.9,39
The clinical criteria of rehabilitation guide patients in returning to play, which usually relies on the hop test and strength test; the single-leg hop for distance (SLHD) test is the most commonly reported functional test.2,20 The hop test, which is easy to implement after ACLR, can reflect the coordination of muscles throughout the body and be used to calculate the limb symmetry index (LSI) value. The LSI value is recommended as a cutoff point to determine the moment of RTP. 7 The LSI is the ratio of data obtained from the same function tests, including the hop test and strength test, of both lower limbs. The SLHD test of the operated leg and nonoperated leg is commonly used to calculate the LSI value, and the equation is as follows: LSI = (SLHD of the operated leg)/(SLHD of the nonoperated leg) × 100%.3,11,15,19 According to the clinical practice guidelines for ACL rehabilitation recommended by the Royal Dutch Society for Physical Therapy, 39 when the LSI value is higher than 90%, RTP is recommended. However, measuring only the hop distance is insufficient to reflect asymmetry between the operated and nonoperated legs.20,21 In contrast, several studies reported that vertical jump performance, assessed by a single-leg vertical jump (SLVJ), provides a lower LSI value. The SLVJ test was a more sensitive functional test than the SLHD test to detect asymmetry between the operated leg and nonoperated leg.21,23,29,36,41 The SLHD and SLVJ tests involve 2 different modes of motion. In an SLVJ test, the subject jumps with 1 leg in the standing place to reach the maximum vertical height. In the SLHD test, the patient jumps with 1 leg in a horizontal direction, which resembles a standing long jump with 1 leg.36,41 The different motions result in different evaluations of limb asymmetry, as reported in the study of Ohji et al. 29 Even though SLHD asymmetry improved in patients at approximately 12 months (range, 8-24 months) after ACLR, SLVJ asymmetry persisted, which indicated that patients needed more time to meet the rehabilitation criteria. More specifically, Kotsifaki et al 21 found that during the concentric phase of a horizontal hop, the knee accounted for only 10% of the total lower limb work. However, during the concentric phase of SLVJ, the knee joint accounted for approximately 30% of the total lower limb work. This finding indicated that only measuring the SLHD was insufficient and could explain why athletes exhibited knee biomechanical deficits during the SLVJ test despite showing SLHD symmetry.
Consequently, in this meta-analysis, we reviewed and analyzed the latest studies to compare the LSI values of the SLHD and SLVJ tests after ACLR and evaluate the importance of the 2 functional tests in the determination of the moment of RTP. We hypothesized that the SLVJ test could better recognize asymmetry of the lower limbs than the SLHD test after ACLR and capture deficits in performance.
Methods
Literature Search
This study was designed and conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. 26 The PubMed, Web of Science, Embase, and Cochrane Library databases were searched from inception to July 2022. Two independent researchers searched each database using the following strategy: ((ACL OR anterior cruciate ligament) AND (reconstruction)) AND (vertical jump OR vertical hop) AND (hop test OR hop distance OR single-leg hop for distance OR horizontal hop). A manual search for references of included articles was also conducted to ensure that no eligible studies were missed.
Study Selection
The same 2 researchers independently included and excluded studies based on titles, abstracts, and full texts. After reading the full texts, the 2 researchers selected the studies that met the inclusion criteria. At the end of selection, disagreements were resolved after discussion between the 2 researchers. The inclusion criteria were as follows:
(1) Observational studies (prospective cohort studies, case-control studies, case series, and cross-sectional studies) comparing operated legs and nonoperated legs.
(2) Participants who underwent ACLR.
(3) Participants who underwent both the SLHD and SLVJ tests.
(4) The LSI values of the SLHD and SLVJ tests were reported.
The exclusion criteria were as follows:
(1) Animal studies, abstracts, reviews, or conference proceedings.
(2) Studies failing to report clearly the data that met our interest.
(3) Participants who underwent revision ACLR.
(4) Participants who underwent SLHD and SLVJ tests with a functional brace or tape.
Assessment of Methodological Quality
The same 2 researchers independently assessed the risk of bias for all included studies using a modified version of the Downs and Black checklist, 13 as described previously.18,20,27,28 Because this systematic review explored descriptive studies, the modified version of the checklist was used, consisting of 14 items from the original 27 items, with a total score of 15, including questions regarding reporting (questions 1, 2, 3, 5, 6, 7, and 10), external validity (questions 11, 12, and 13), internal validity (questions 18, 20, and 25), and power (question 27). Disagreements were resolved by discussion.
Data Extraction
Two researchers independently checked all suitable studies using the data extraction sheet, and all disagreements were resolved by discussion. The extracted data included study design, participant information (age, height, weight, graft type, time since ACLR, the number of participants), and primary outcomes (LSI values of the SLVJ and SLHD tests).
Data Analysis
Data analyses were performed with Review Manager software (version 5.4.1; Nordic Cochrane Centre, the Cochrane Collaboration). The LSI values of the SLHD and SLVJ tests were compared. Means and standard deviations (SDs) for each variable of interest were used to calculate standardized mean differences (SMDs). Heterogeneity was assessed by I2 tests. I2 values of 25%, 50%, and 75% were considered to indicate low, medium, and high heterogeneity, respectively. When the I2 value was higher than 50% and the P value was <0.10, the random-effects model was chosen. When the I2 value was lower than 50% and P was >0.10, the fixed-effects model was chosen.
Results
Search Results
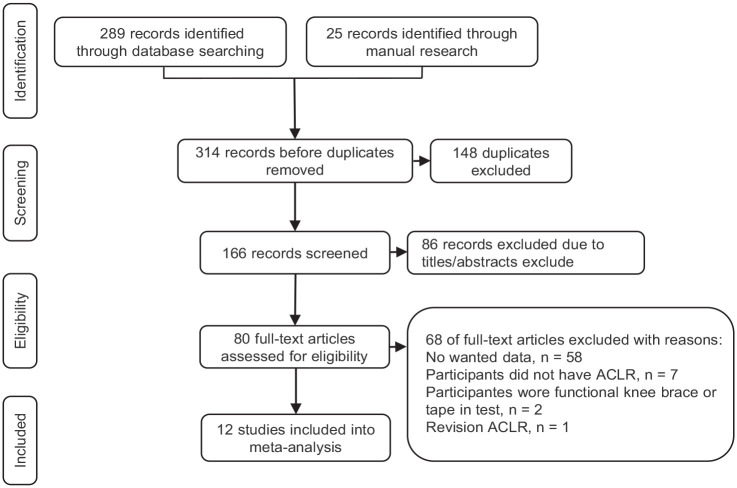
A total of 314 articles were selected after the initial search (PubMed = 73, Embase = 80, Web of Science = 119, Cochrane Library = 17, manual research = 25). Among these articles, 148 were excluded due to being identified as duplicates, and 86 were removed after a review of the titles and abstracts. Sixty-eight studies were excluded after reviewing the full texts. Ultimately, 12 records3,5,11,15,19,23,29-31,36,37,40 were included in our meta-analysis. A summary is presented in Figure 1.
Figure 1.
Flowchart of the article selection process. ACLR, anterior cruciate ligament reconstruction.
Characteristics of the Included Studies
The 12 selected studies included 8 cross-sectional studies, 3 case-control studies, and 1 case series. The baseline data of the participants and outcomes are listed in Tables 1 and 2, respectively. A total of 507 participants who underwent ACLR (347 men, 145 women, 15 not reported) were included in this review. All participants underwent the SLHD and SLVJ tests and engaged in rehabilitation before the test, and the LSI ± SD was collected. In particular, in the studies of Curran et al 11 and Petschnig et al, 31 patients were divided into different groups based on postoperative time. In the study of Kinikli et al, 19 patients were divided into different groups based on different rehabilitation plans. In the study of Gobbi et al, 15 the same group of patients underwent the test at different time points after the operation to form a before-and-after comparison. In total, 12 studies included 18 groups of participants, and 507 patients (347 men, 145 women, 15 not reported) underwent the functional tests mentioned above.
Table 1.
Basic information of participants
| Author | Study Design | Graft (Nnumbers) | Sample Size (Male/Female) | Test Time Post-ACLR ± SD | Age (years) ± SD | Weight (kg) ± SD | Height (cm) ± SD |
|---|---|---|---|---|---|---|---|
| Ageberg and Roos (2016) 3 | Cross-sectional | PT (20); HT (16) | 36 (27/9) | The patients data were from a randomized controlled trial (the KANON study; ISRCTN84752559) that investigated training plus early ACLR and training with the option of later ACL | |||
| Baltaci et al (2012) 5 | Case-control | PT | 15 | 18-24 months | 29.6 ± 5.9 | 77.7 ± 10.3 | 176.4 ± 8.3 |
| Curran et al (2020) 11 | Cross-sectional | ||||||
| Group 1 | PT (14); HT (3); QT (3) | 19 (8/11) | 9 months ± 21 days | 19.5 ± 5.7 | 75.0 ± 20.2 | 168.9 ± 10.2 | |
| Group 2 | PT (15); HT (5); QT (2) | 22 (9/13) | 12 months ± 21 days | 20.2 ± 7.8 | 70.0 ± 10.4 | 169.1 ± 8.2 | |
| Group 3 | PT (15); HT (4); QT (1) | 20 (12/8) | 18 months ± 21 days | 20.5 ± 6.6 | 75.9 ± 15.3 | 174.3 ± 9.5 | |
| Group 4 | PT (13); HT (8) | 21 (8/13) | 24 months ± 21 days | 20.5 ± 6.4 | 74.6 ± 14.5 | 169.1 ± 7.4 | |
| Gobbi et al (2003) 15 | Cross-sectional | HT | 80 (52/28) | 6-month test and final test (36 months, range, 24-52 months) | 28 | NR | NR |
| Kinikli et al (2014) 19 | Cross-sectional | HT | 33 (31/2) | 16 weeks | Study group: 33.87 ± 8.19 Control group: 32.64 ± 8.21 |
BMI: Study group: 24.50 ± 2.36 Control group: 24.52 ± 0.94 |
|
| Lee et al. (2018) 23 | Case series | HT | 75 (75/0) | 9 months | 27.5 ± 9.2 | 72.3 ± 11.0 | 172.2 ± 8.2 |
| Ohji et al (2021) 29 | Cross-sectional | HT | 44 (24/20) | 8-24 months | 21.5 ± 4.1 | 61.2 ± 10.9 | 164 ± 10 |
| Perry et al (2005) 30 | Case-control | NR | 24 (18/6) | 57 days ± 4 | 32 ± 6 | 78 ± 13 | 173 ± 9 |
| Petschnig et al (1998) 31 | Case-control | ||||||
| Group B | PT | 30 (30/0) | 12.9 weeks ± 3.0 | 27.8 ± 9.0 | 78.1 ± 11.6 | 176.0 ± 6.9 | |
| Group C | PT | 25 (25/0) | 53.9 weeks ± 13.2 | 29.9 ± 5.8 | 73.1 ± 8.7 | 176.4 ± 6.9 | |
| Taylor et al (2020) 36 | Cross-sectional | PT (3); HT (6); QT (1); CA (2) | 12 (0/12) | 4.7 years ± 2.6 | 21.1 ± 3.2 | 68.3 ± 8.8 | 165.8 ± 6.0 |
| Tengman et al (2014) 37 | Cross-sectional | PT + LAD (19); LAD (9); HT (5) | 33 (21/12) | Around 20 years | 45.6 ± 4.5 | 83.0 ± 15.6 | 174.0 ± 9.1 |
| Zarro et al (2021) 41 | Cross-sectional | NR | 18 (7/11) | 7.33 months ± 2.05 | 20.39 ± 1.11 | 75.61 ± 15.38 | 175 ± 9.0 |
ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; CA, cadaver allograft; HT, hamstring tendon; LAD, Kennedy ligament augmentation device; NR, not reported; PT, patellar tendon; QT, quadriceps.
Table 2.
Primary outcomes
| Author | Single-leg Vertical Jump LSI (%) ± SD | Single-Leg Hop LSI (%) ± SD |
|---|---|---|
| Ageberg and Roos (2016) 3 | 96.3 ± 13.4 | 99.5 ± 8.2 |
| Baltaci et al (2012) 5 | 92.9 ± 10.1 | 88.1 ± 8.4 |
| Curran et al (2020) 11 | ||
| Group 1 | 87.06 ± 17.35 | 90.01 ± 9.46 |
| Group 2 | 89.64 ± 18.43 | 93.48 ± 5.53 |
| Group 3 | 89.67 ± 16.42 | 96.24 ± 6.47 |
| Group 4 | 90.70 ± 15.13 | 96.30 ± 6.46 |
| Gobbi et al (2003) 15 | ||
| 6-Month test | 0.90 ± 0.12 | 0.90 ± 0.09 |
| Final test | 0.93 ± 0.10 | 0.95 ± 0.10 |
| Kinikli et al (2014) 19 | ||
| The study group | 89.18 ± 10.36 | 91.14 ± 8.6 |
| The control group | 77.25 ± 14.98 | 84.58 ± 7.4 |
| Lee et al (2018) 23 | 89.4 ± 14.9 | 90.7 ± 11.7 |
| Ohji et al (2021) 29 | 90.4 ± 10.7 | 98.2 ± 6.1 |
| Perry et al (2005) 30 | 78 ± 14 | 75 ± 17 |
| Petschnig et al (1998) 31 | ||
| Group B | 46.3 ± 12.9 | 73 ± 9.9 |
| Group C | 74.9 ± 13.3 | 88.4 ± 8.4 |
| Taylor et al (2020) 36 | 94.9 ± 7.6 | 97.4 ± 6.6 |
| Tengman et al (2014) 37 | 94 ± 2 | 94 ± 11 |
| Zarro et al (2021) 41 | 84.48 ± 11.41 | 95.48 ± 8.02 |
LSI, limb symmetry index.
Risk of Bias Assessment
A modified version of the Downs and Black quality index was used for the 12 included studies, with a median total score of 11.5 (range, 9-14). Table 3 provides the full details of each included study’s risk of bias. All included studies reported their aim/hypotheses, main outcomes, and participant characteristics, and used valid and reliable assessment and outcome tools. The most frequent sources of potential bias were representative of the population (n = 9), no power analysis (n = 8), and no or limited adjustment for potential confounders (n = 7).
Table 3.
The modified version of the Downs and Black checklist
| Author | The Number of Items | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 5 | 6 | 7 | 10 | 11 | 12 | 13 | 18 | 20 | 25 | 27 | Total (/15) | |
| Ageberg and Roos (2016) 3 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 |
| Baltaci et al (2012) 5 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 12 |
| Curran et al (2020) 11 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 14 |
| Gobbi et al (2003) 15 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 |
| Kinikli et al (2014) 19 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 12 |
| Lee et al (2018) 23 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 10 |
| Ohji et al (2021) 29 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 13 |
| Perry et al (2005) 30 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 |
| Petschnig et al (1998) 31 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 9 |
| Taylor et al (2020) 36 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 11 |
| Tengman et al (2014) 37 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 14 |
| Zarro et al (2021) 41 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 12 |
Quantity Analysis
In the quantity analysis, the LSI was analyzed as the main outcome, and sensitivity analysis and subgroup analysis were performed to explain the heterogeneity. When the heterogeneity was high (I2 value higher than 50% and P < 0.10), the random effects model was used in the meta-analysis, but the conclusion could be relevantly conservative. Therefore, the subgroup analysis and sensitivity analysis aimed to determine the possible sources of heterogeneity to make the conclusion more reliable.
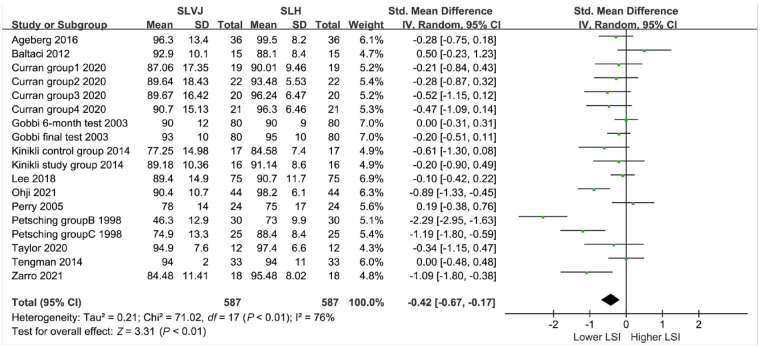
Limb Symmetry Index
Twelve studies involving 587 tests compared the LSI values of the SLVJ and SLHD tests (Figure 2). The results suggested that the LSI value of the SLVJ was significantly lower than that of the SLHD test (SMD -0.42; 95% CI -0.67 to -0.17). The data, analyzed in a random-effects model, exhibited high heterogeneity (I2 = 76%, P < 0.01).
Figure 2.
Forest plot of the LSI values. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
Sensitivity Analysis
The LSI value of the SLVJ test in group B of the study by Petschnig et al 31 (46.3%) was significantly lower than that in the other groups, and sensitivity analysis was performed. After removing this group, the heterogeneity changed (I2 = 56%, P < 0.01), and a random-effects model was used (SMD -0.31; 95% CI -0.50 to -0.12), indicating that the above result was stable.
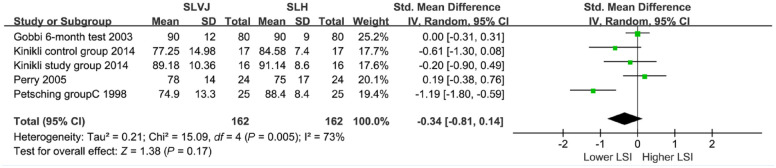
Subgroup Analysis
After ACLR, physical rehabilitation, vascular reconstruction, graft maturation, and other processes require some time, so subgroup analysis was performed according to the time since surgery. The time points were set at 6, 12, 18, and 24 months after surgery based on the recovery time after ACLR.
In 6 months. Four studies,15,19,30,31 including 5 groups of participants whose time post-ACLR was 57 days to 6 months, formed subgroup 1 (Figure 3). High heterogeneity was found among the 5 groups (I2 = 73%, P < 0.01). The results suggested that the LSI value of the SLVJ test was not significantly lower than that of the SLHD test from 57 days to 6 months after surgery (SMD -0.34; 95% CI -0.81 to 0.14). The heterogeneity was from group B in the study of Petschnig et al. 31 After removing this group, low heterogeneity was found among the other 4 groups (I2 = 13%, P = 0.33), so the fixed-effects model was used (SMD -0.06; 95% CI -0.30 to 0.18).
Figure 3.
Forest plot of subgroup 1. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
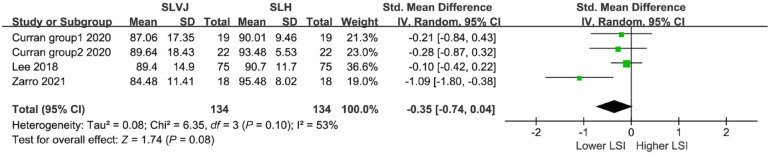
6 to 12 months. Three studies,11,23,41 including 4 groups of participants whose time post-ACLR was 7 to 12 months, formed subgroup 2 (Figure 4). Medium heterogeneity was found among the 4 groups (I2 = 53%, P = 0.10). The results suggested that the LSI value of the SLVJ test was not significantly lower than that of the SLHD test from 6 to 12 months after surgery (SMD -0.35; 95% CI -0.74 to 0.04).
Figure 4.
Forest plot of subgroup 2. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
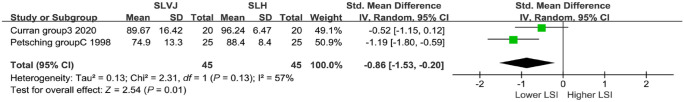
12 to 18 months. Two studies,11,31 including 2 groups of participants whose time post-ACLR was 12 to 18 months, formed subgroup 3 (Figure 5). Medium heterogeneity was found between the 2 groups (I2 = 57%, P = 0.13), so the random-effects model was used. The results suggested that the LSI value of the SLVJ test was significantly lower than that of the SLHD test from 12 to 18 months after surgery (SMD-0.86; 95% CI -1.53 to -0.20).
Figure 5.
Forest plot of subgroup 3. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
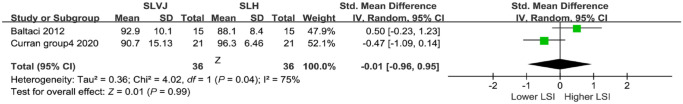
18 to 24 months. Two studies,5,11 including 2 groups of participants whose time post-ACLR was 18 to 24 months, formed subgroup 4 (Figure 6). High heterogeneity was found between the 2 groups (I2 = 75%, P = 0.04), so the random-effects model was used. The results suggested that the LSI value of the SLVJ test was not significantly lower than that of the SLHD test from 18 to 24 months after surgery (SMD -0.01; 95% CI -0.96 to 0.95).
Figure 6.
Forest plot of subgroup 4. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
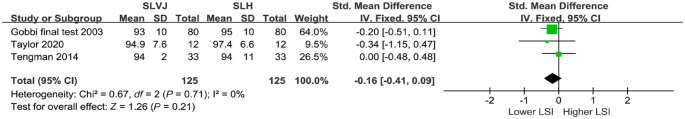
More than 24 months. Three studies,15,37,41 including 3 groups of participants whose time post-ACLR was more than 24 months, formed subgroup 5 (Figure 7). Low heterogeneity was found between the 2 groups (I2 = 0%, P = 0.71), so the fixed-effects model was used. The results suggested that the LSI value of the SLVJ test was not significantly lower than that of the SLHD test more than 24 months after surgery (SMD -0.16; 95% CI -0.41 to 0.09).
Figure 7.
Forest plot of subgroup 5. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
Subgroup 2, subgroup 3, and subgroup 4 showed medium or high heterogeneity, and subgroup 2 and subgroup 3 only included 2 groups of participants, which indicated that the source of heterogeneity was unclear. The time point was adjusted and set at 6 and 18 months.
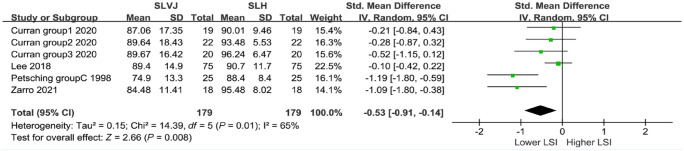
6 to 18 months. Four studies,11,23,31,41 including 6 groups of participants whose time post-ACLR was 7 to 18 months, formed subgroup 6 (Figure 8). High heterogeneity was found among the 6 groups (I2 = 65%, P = 0.01), so the random-effects model was used. The results suggested that the LSI value of the SLVJ test was significantly lower than that of the SLHD test from 6 to 18 months after surgery (SMD -0.53; 95% CI -0.91 to -0.14). The heterogeneity was from group C in the study of Petschnig et al. 31 After removing this group, low to medium heterogeneity was found among the other 5 groups (I2 = 42%, P = 0.14), so the fixed-effects model was used (SMD -0.29; 95% CI -0.52 to -0.07).
Figure 8.
Forest plot of subgroup 6. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
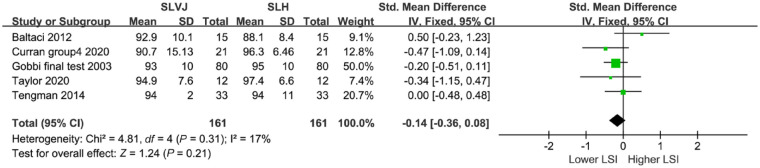
More than 18 months. Five studies,5,11,15,36,37 including 5 groups of participants whose time post-ACLR was more than 18 months, formed subgroup 7 and the longest time post-ACLR was around 20 years 37 (Figure 9). Low heterogeneity was found among the 5 groups (I2 = 17%, P = 0.31), so the fixed-effects model was used. The results suggested that the LSI value of the SLVJ test was not significantly lower than that of the SLHD test more than 18 months after surgery (SMD -0.14; 95% CI -0.36 to 0.08).
Figure 9.
Forest plot of subgroup 7. LSI, limb symmetry index; SLH, single-leg hop; SLVJ, single-leg vertical jump.
The study of Ageberg and Roos 3 only reported the time after injury, and the study of Ohji et al 29 reported a time between 8 and 24 months, which was a long interval, and was not included in the subgroup analysis.
Quality Analysis
According to the aforementioned guidelines, 39 RTP is recommended when the LSI value is higher than 90%. Therefore, quality synthesis was performed based on the criterion of an LSI value >90% and the time post-ACLR. Among the 17 groups of participants, for the LSI value of the SLHD test, the average LSI value of the 12 groups was higher than 90%, the earliest time point was 4 months, and the latest time point was 20.3 years. For the LSI value of the SLVJ test, the average LSI value of the 6 groups was higher than 90%, and the time points of 5 groups were ≥18 months (the left group was from the study of Ohji et al, 29 which had a long interval from 8 to 24 months). Both the LSI values of the SLHD and SLVJ tests from the study of Ageberg and Roos, 3 only reporting the time after injury, were more than 90%.
Discussion
This review was performed to compare the LSI values of the SLVJ and SLHD tests, and a key finding was that individuals had lower LSI values of the SLVJ test than the SLHD test from 7 to 18 months after ACLR, while patients who had tests from 57 days to 6 months or after 18 months had similar LSI values in both tests.
In the early stage after ACLR, there are functional deficits in quadricep and hamstring strength,8,12 and graft healing is essential in rehabilitation and RTP. 8 A similar LSI value was found from 57 days to 6 months after ACLR. The theory of ligamentization and insufficient rehabilitation for muscle atrophy may potentially explain the result. First, after ACLR, a free tendon graft replaces the ruptured ACL through a series of biological processes termed ligamentization. Ligamentization is a necessary process of graft remodeling with characteristic histological and biomechanical changes in different stages. 10 Three different stages of the ligamentization of the free tendon graft are mainly described by other authors, including the early stage, remodeling stage, and mature stage.1,14,33,34 There is lower mechanical strength of the healing graft in the early stage, and the mechanical strength increases step by step in the following 2 stages.34,35 Although the time point of the early stage varies (from 3 to 12 months) in different studies, 10 the theory indicates that graft healing may still be in the early stage in the first 6 months after ACLR. Second, muscle atrophy of the injured leg commonly occurs after ACL injury due to disuse or traumatic factors,24,38 and rehabilitation before surgery can be used to reduce limb asymmetry and accelerate rehabilitation.17,39 Only 1 included study 19 described that some of the participants underwent rehabilitation before surgery, which indicated that more time might be spent in rehabilitation after ACLR. In total, in the early stage, the lower mechanical strength of the healing graft and less time for rehabilitation may make both the SLVJ and SLHD tests able to sensitively recognize limb asymmetry.
Along with rehabilitation and ligamentization, the differences between legs decrease, and different sensitivities of the SLVJ and SLHD tests are exhibited. A lower LSI value of the SLVJ test than that of the SLHD test was found 7 to 18 months after ACLR. A possible explanation is that limb symmetry is performed in specific movements, and limb asymmetry may exist in the vertical and not horizontal directions. 25 Several studies have reported that the SLVJ test was more correlated with quadriceps strength and provided a greater strength-load stimulus than the horizontal jump test.25,36,41 Moreover, a weak-to-moderate correlation between the SLVH and SLHD tests was reported, suggesting that the SLVH test may capture deficits that the SLHD test cannot.36,41
A similar LSI value was found more than 18 months after ACLR. In this period, ligamentization was in the maturation stage and approached the endpoint. Combined with the results of the quality analysis, the LSI values of both the SLHD and SLVJ tests were commonly more than 90% in this period, which indicated that the LSI was not particularly sensitive in the clinical setting. Although the LSI value was more than 90%, as Tengman et al 37 reported, other biomechanical outcomes of the SLVJ test, such as sagittal plane knee impulse and sagittal plane hip impulse of the SLVH test, could also reflect asymmetry in the lower limbs. This result indicated that similar athletic performance could result in different instability between the legs.
In conclusion, the test battery (including the hop test and strength test) is recommended after ACLR, and the specific test items are suggested to be determined according to patient RTP goals. A complete test battery should include hop tests and strength tests (isokinetic muscle strength tests), which are usually tested by the Biodex system (Biodex Medical Systems), which could keep the muscles working in the same motion to observe muscle function and joint status, and provide valuable information for rehabilitation.11,15,16,23 The Biodex system and the hop test could provide valuable information in different directions, and this study focused on the sensitivity of hop tests. It should be emphasized that the results of this study supported that the SLVJ test was more sensitive than the SLHD test, and could possibly provide more information for enhancing a safe return to high-intensity sports. This review also suggested that in future studies, the test battery could be graded according to different RTP goals to guide patients to RTP at a more appropriate time. We think that both the SLHD and SLVJ tests are meaningful during 7 to 18 months after ACLR, and the key is to choose the appropriate test according to the needs of patients.
Limitations
Several limitations of the review should be considered. First, the rehabilitation method was not limited in this review, which could confound the comparison. Second, only 1 included study 11 reported biomechanical outcomes, such as peak knee flexion, of both the SLVJ and SLHD tests, which limited the comparison of the review to only LSI values.
Conclusion
This review recommended that the SLVJ test can be used to calculate LSI values and capture deficits in performance that the SLHD test is unable to perform in the intermediate phase after ACLR. It is insufficient to measure only the distance of the horizontal jump. The test battery for RTP after ACLR needs to be completed and adjusted to meet different patient rehabilitation goals.
Footnotes
The author(s) report no potential conflicts of interest in the development and publication of this article.
References
- 1. Abe S, Kurosaka M, Iguchi T, Yoshiya S, Hirohata K. Light and electron microscopic study of remodeling and maturation process in autogenous graft for anterior cruciate ligament reconstruction. Arthroscopy. 1993;9(4):394-405. [DOI] [PubMed] [Google Scholar]
- 2. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2(1):2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ageberg E, Roos EM. The association between knee confidence and muscle power, hop performance, and postural orientation in people with anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2016;46(6):477-482. [DOI] [PubMed] [Google Scholar]
- 4. Ashigbi EYK, Banzer W, Niederer D. Return to sport tests' prognostic value for reinjury risk after anterior cruciate ligament reconstruction: a systematic review. Med Sci Sports Exerc. 2020;52(6):1263-1271. [DOI] [PubMed] [Google Scholar]
- 5. Baltaci G, Yilmaz G, Atay AO. The outcomes of anterior cruciate ligament reconstructed and rehabilitated knees versus healthy knees: a functional comparison. Acta Orthop Traumatol Turc. 2012;46(3):186-195. [DOI] [PubMed] [Google Scholar]
- 6. Birchmeier T, Lisee C, Kane K, Brazier B, Triplett A, Kuenze C. Quadriceps muscle size following ACL injury and reconstruction: a systematic review. J Orthop Res. 2020;38(3):598-608. [DOI] [PubMed] [Google Scholar]
- 7. Bisciotti GN, Quaglia A, Belli A, Carimati G, Volpi P. Return to sports after ACL reconstruction: a new functional test protocol. Muscles Ligaments Tendons J. 2016;6(4):499-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brinlee AW, Dickenson SB, Hunter-Giordano A, Snyder-Mackler L. ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Sports Health. 2022;14(5):770-779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buckthorpe M. Optimising the late-stage rehabilitation and return-to-sport training and testing process after ACL reconstruction. Sports Med. 2019;49(7):1043-1058. [DOI] [PubMed] [Google Scholar]
- 10. Claes S, Verdonk P, Forsyth R, Bellemans J. The "ligamentization" process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med. 2011;39(11):2476-2483. [DOI] [PubMed] [Google Scholar]
- 11. Curran MT, Bedi A, Kujawa M, Palmieri-Smith R. A cross-sectional examination of quadriceps strength, biomechanical function, and functional performance from 9 to 24 months after anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48(10):2438-2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. de Jong SN, van Caspel DR, van Haeff MJ, Saris DB. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(1):21-28, 28 e21-23. [DOI] [PubMed] [Google Scholar]
- 13. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Falconiero RP, DiStefano VJ, Cook TM. Revascularization and ligamentization of autogenous anterior cruciate ligament grafts in humans. Arthroscopy. 1998;14(2):197-205. [DOI] [PubMed] [Google Scholar]
- 15. Gobbi A, Tuy B, Mahajan S, Panuncialman I. Quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a clinical investigation in a group of athletes. Arthroscopy. 2003;19(7):691-699. [DOI] [PubMed] [Google Scholar]
- 16. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg, Sports Traumato, Arthrosc: official journal of the ESSKA. 2017;25(1):192-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johnston PT, McClelland JA, Webster KE. Lower limb biomechanics during single-leg landings following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Med. 2018;48(9):2103-2126. [DOI] [PubMed] [Google Scholar]
- 19. Kinikli GI, Yuksel I, Baltaci G, Atay OA. The effect of progressive eccentric and concentric training on functional performance after autogenous hamstring anterior cruciate ligament reconstruction: a randomized controlled study. Acta Orthop Traumatol Turc. 2014;48(3):283-289. [DOI] [PubMed] [Google Scholar]
- 20. Kotsifaki A, Korakakis V, Whiteley R, Van Rossom S, Jonkers I. Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2020;54(3):139-153. [DOI] [PubMed] [Google Scholar]
- 21. Kotsifaki A, Van Rossom S, Whiteley R, et al. Single leg vertical jump performance identifies knee function deficits at return to sport after ACL reconstruction in male athletes. Br J Sports Med. 2022;56(9):490-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg: American volume. 2012;94(19):1737-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee DW, Yang SJ, Cho SI, Lee JH, Kim JG. Single-leg vertical jump test as a functional test after anterior cruciate ligament reconstruction. Knee. 2018;25(6):1016-1026. [DOI] [PubMed] [Google Scholar]
- 24. Lepley LK, Davi SM, Burland JP, Lepley AS. Muscle atrophy after ACL injury: implications for clinical practice. Sports Health. 2020;12(6):579-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Maulder P, Cronin J. Horizontal and vertical jump assessment: reliability, symmetry, discriminative and predictive ability. Phys Ther Sport. 2005;6(2):74-82. [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG; for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mosler AB, Agricola R, Weir A, Holmich P, Crossley KM. Which factors differentiate athletes with hip/groin pain from those without? A systematic review with meta-analysis. Br J Sports Med. 2015;49(12):810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13(1):2-12. [DOI] [PubMed] [Google Scholar]
- 29. Ohji S, Aizawa J, Hirohata K, et al. Single-leg hop can result in higher limb symmetry index than isokinetic strength and single-leg vertical jump following anterior cruciate ligament reconstruction. Knee. 2021;29:160-166. [DOI] [PubMed] [Google Scholar]
- 30. Perry MC, Morrissey MC, Jones JS, et al. Number of repetitions to maximum in hop tests in patients with anterior cruciate ligament injury. Int J Sports Med. 2005;26(8):688-692. [DOI] [PubMed] [Google Scholar]
- 31. Petschnig R, Baron R, Albrecht M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;28(1):23-31. [DOI] [PubMed] [Google Scholar]
- 32. Relph N, Herrington L, Tyson S. The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy. 2014;100(3):187-195. [DOI] [PubMed] [Google Scholar]
- 33. Rougraff B, Shelbourne KD, Gerth PK, Warner J. Arthroscopic and histologic analysis of human patellar tendon autografts used for anterior cruciate ligament reconstruction. Am J Sports Med. 1993;21(2):277-284. [DOI] [PubMed] [Google Scholar]
- 34. Sanchez M, Anitua E, Azofra J, Prado R, Muruzabal F, Andia I. Ligamentization of tendon grafts treated with an endogenous preparation rich in growth factors: gross morphology and histology. Arthroscopy. 2010;26(4):470-480. [DOI] [PubMed] [Google Scholar]
- 35. Scheffler SU, Unterhauser FN, Weiler A. Graft remodeling and ligamentization after cruciate ligament reconstruction. Knee Surg, Sports Traumatol, Arthrosc: official journal of the ESSKA. 2008;16(9):834-842. [DOI] [PubMed] [Google Scholar]
- 36. Taylor JB, Westbrook AE, Head PL, Glover KM, Paquette MR, Ford KR. The single-leg vertical hop provides unique asymmetry information in individuals after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2020;80:105107. [DOI] [PubMed] [Google Scholar]
- 37. Tengman E, Brax Olofsson L, et al. Anterior cruciate ligament injury after more than 20 years: I. Physical activity level and knee function. Scand J Med Sci Sports. 2014;24(6):e491-500. [DOI] [PubMed] [Google Scholar]
- 38. Toth MJ, Tourville TW, Voigt TB, et al. Utility of neuromuscular electrical stimulation to preserve quadriceps muscle fiber size and contractility after anterior cruciate ligament injuries and reconstruction: a randomized, sham-controlled, blinded trial. Am J Sports Med. 2020;48(10):2429-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506-1515. [DOI] [PubMed] [Google Scholar]
- 40. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zarro MJ, Stitzlein MG, Lee JS, et al. Single-leg vertical hop test detects greater limb asymmetries than horizontal hop tests after anterior cruciate ligament reconstruction in NCAA division 1 collegiate athletes. Int J Sports Phys Ther. 2021;16(6):1405-1414. [DOI] [PMC free article] [PubMed] [Google Scholar]