Abstract
Context:
Athletes are almost 3 times more at risk of experiencing urinary incontinence (UI) than sedentary women, with prevalence rates varying from 10.9% in low-impact sports such as cycling to 80% when engaging in high-impact sports such as trampoline gymnastics. To treat UI, pelvic floor muscle (PFM) training (PFMT) is recommended as a first line of treatment.
Objective:
The aim of the present study was to perform a meta-analysis of the available literature on the efficacy of PFMT interventions in young, nulliparous female athletes.
Data Sources:
A literature research was conducted using PubMed, Sport Discus, and Web of Science.
Study Selection:
The inclusion criteria were studies with PFMT intervention in female athletes or recreationally active women. Interventions could be carried out for treatment or prevention of pelvic floor dysfunctions.
Study Design:
Systematic review with meta-analysis.
Level of Evidence:
Level 5.
Data Extraction:
A descriptive analysis of the articles included in the systematic review was carried out. Meta-analyses could be performed on 6 of the included articles, evaluating the maximal voluntary contraction (MVC) of the PFMs, the amount of urinary leakage (AUL), and the vaginal resting pressure (VRP). Random-effects model and standardized mean differences (SMD) ± 95% CI were reported.
Results:
The meta-analysis showed that PFMT produced a significant increase in MVC (SMD, 0.60; 95% CI, 0.11 to 1.08; P = 0.02) and a significant reduction of AUL (SMD, -1.13; 95% CI, -1.84 to -0.41; P < 0.01) in female athletes. No effects were shown in VRP (SMD, -0.05; 95% CI, -1.27 to 1.17; P = 0.93).
Conclusion:
PFMT is shown to be effective in increasing PFM strength and reducing urine leakage in female athletes, being a powerful tool to prevent and treat pelvic floor dysfunction in this population.
Keywords: exercise, incontinence, meta-analysis, pelvic floor disorders, sport, women’s health
The pelvic floor is composed of a set of muscles and connective tissue that supports the structures of the abdomen and pelvis. It is responsible for urinary and fecal continence, among other functions. 4
A pelvic floor disorder (PFD) encompasses an alteration of normal pelvic floor muscle (PFM) function. PFDs can be classified as dysfunction due to increased PFM tone, PFM pain, decrease in PFM tone, or disorders of PFM coordination. 12
The most common PFD is urinary incontinence (UI), defined as “any complaint of involuntary leakage of urine”, 16 which affects 1 in 4 women during their lifetime. 31
The practice of high-impact physical exercise is shown to be one of the risk factors for the occurrence of UI. 40 An increase in intra-abdominal pressure (IAP) is associated with the practice of physical activity, leading to changes in the morphology and functionality of the ligaments and connective tissue of the pelvic floor. This may explain the presence of UI in young nulliparous athletes without other risk factors.8,14
Female athletes are almost 3 times more at risk of experiencing UI than their sedentary counterparts. 40 One plausible explanation of this fact is the engagement in high-impact activities, where the reaction force of the feet against the ground and the lack of contraction of the PFM during exercise leads to an increase in IAP that might compromise the closure of the urethra. 27 Consequently, previous studies have found UI prevalence rates varying from 10.9% in low-impact sports such as cycling to 80% in high-impact sports such as trampoline gymnastics. 8
Although UI is not life-threatening, it can cause embarrassment and discomfort in female athletes, creating a barrier to sports practice and affecting their well-being and health-related quality of life (HRQoL). 17 To treat UI, PFM training (PFMT) is recommended as a first line of treatment, showing Level 1 scientific evidence.4,9 PFMT consists of voluntary PFM contractions that increase, strengthen, and improve the support of the structures to counteract increased IAP and ground-reaction forces during exercise, leading to an improvement of the automatic function of the pelvic floor, 4 and improving UI when it occurs or preventing possible future UI.
For the prevention of PFD, some studies conducted in women during pregnancy showed evidence of efficacy of PFMT in reducing the risk of UI.25,34 However, in the athlete population, most studies have been observational in nature, reporting UI prevalence rates,2,11,15,30,40 rather than PFMT interventions, which are scarce.28,29,38
Preventive PFMT should be a priority for female athletes to avoid future dysfunction that could compromise exercise practice or HRQoL. Therefore, coaches and exercise professionals must have knowledge of preventive practical tools and strategies to include during training.
The aim of the present study was to perform a meta-analysis of all available literature on the efficacy of PFMT interventions in young, nulliparous female athletes.
The main outcomes of interest were the mean values and the corresponding standard deviation (SD) of maximal voluntary contraction (MVC) of the PFM, vaginal resting pressure (VRP) and the amount of urinary leakage (AUL) as indicators of the intervention effectiveness. The secondary outcome of interest was HRQoL variations due to the interventions.
Methods
A systematic review of the literature and associated meta-analysis was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the Patient, problem or population, Intervention, Comparison, control or comparator, Outcome(s), Study type (PICOS) criterion. This work was registered with the PROSPERO database (CRD42022284843).
Search Strategy and Study Selection
A literature search was conducted using PubMed, Sport Discus, and Web of Science databases, between November 1, 2021 and February 28, 2022. A search strategy was devised using the words “pelvic floor” OR “pelvic floor muscle training” AND “sports” OR “athletes” AND “trial.” The search was conducted without any publication year restriction, and date or language filters were not used.
The inclusion criteria were studies with PFMT intervention in female athletes or recreationally active women. Interventions could be carried out for treatment or prevention of PFD. The exclusion criteria were studies that included subjects with a previous history of pelvic surgery, menopause, parous, pregnant, or postpartum women. Conference proceedings, doctoral theses, dissertations, case studies, and other reviews and meta-analyses were excluded.
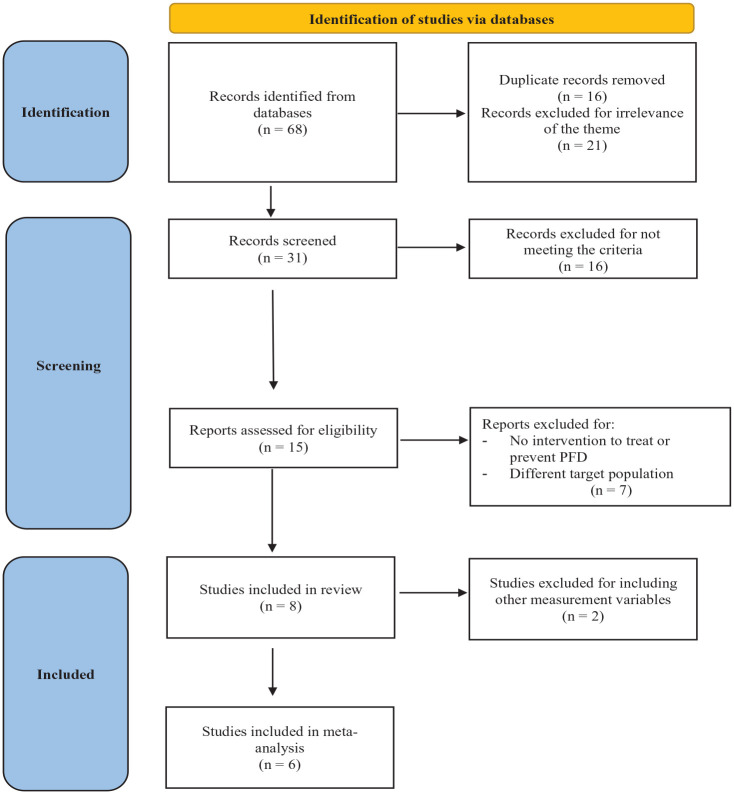
Initially, 68 potential articles were identified. After a thorough examination, 8 articles were elected for qualitative analysis and 6 for meta-analysis. The study selection flow chart is shown in Figure 1.
Figure 1.
PRISMA flowchart for study selection. PFD, pelvic floor disorder; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Methodological Quality
Two independent reviewers selected and analyzed the articles for this study. Any disagreements were resolved by a third author.
Risk of Bias Assessment
Risk of bias assessment using the McMaster instrument for quantitative studies was evaluated independently by 2 reviewers. 20 This tool provides information about the purpose, literature review, design, sample, outcomes, intervention, results, and conclusions of the studies. One point was awarded if the criterion was met and zero points if it was not met. The methodological quality of the studies was considered as follows: poor ≤8 points; acceptable 9 to 10 points; good 11 to 12 points; very good 13 to 14 points; excellent ≥15 points.
Statistical Analysis
A descriptive analysis of the articles included in the systematic review was carried out. The 8 articles selected showed heterogeneity in design. However, 3 meta-analyses could be performed on 6 of the included articles.
The outcome measure for the analysis was the standardized mean difference (SMD). A random-effects model was then matched to the data. The restricted maximum-likelihood (RML) estimator was considered to check the amount of heterogeneity (ie, τ2). 41 In addition to the RML estimator, the Q test for heterogeneity and the I2 statistic were reported. 6 When the amount of heterogeneity was large (ie, τ2 > 0, regardless of the results of the Q test), a prediction interval for the true outcomes was provided. Studentized residuals and Cook’s distances were calculated to check whether studies might be outliers and/or influential in the context of the model. Studies with values>100 × (1 - 0.05/(2 × k))th percentile of a standard normal distribution were considered as potential outliers (ie, using a Bonferroni correction with 2-sided alpha = 0.05 for k studies included in the meta-analysis). Studies with a Cook’s distance larger than the median plus 6 times the interquartile range of the Cook’s distances were considered to be influential. The rank correlation test and the regression test, using the standard error of the observed outcomes as predictor, were used to check for funnel plot asymmetry. All data analyses were run using the free statistical software Jamovi (Version 1.6.15). 18
Results
Study characteristics are presented in Table 1.
Table 1.
Characteristics of the selected studies
| Author (Year) | Study Design | Aim | CG | Sample | Inclusion Criteria | Age, years | N (total) | N (EG) | Assessment | Intervention | Duration, weeks | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Piernicka (2021) 28 | Randomized controlled trial | To test the hypothesis that a high-impact aerobics program, combined with PFMT does not impair PFM function in young active women | Yes | Sport students | Nulliparous women without diagnosed urinary tract problems Women who did not have a good QoL based on IIQ Classified as physically active in IPAQ |
22.0 ± 2 | 32 | 13 | Biofeedback EMG QoL IIQ |
PFMT | 6 | Post MVC: increase of 5% EG and 2% CG EG increase mean EMG in contractions and present lower EMG values in relaxations |
| Szumilewicz (2019) 39 | Randomized controlled trial | To assess how well future female exercise professionals contract the PFM, and whether a biofeedback session is necessary to train them to contract PFM | Yes | Future exercise professionals | Nulliparous students Health condition that allowed for physical activity Available to implement a 6-week training program Ready to comply with the requirements of the study |
23.0 ± 3 | 84 | 53 | Biofeedback EMG Self-elaborated questionnaire |
PFMT with or without biofeedback | 6 | Pretest: 17% could not activate the PF and 45% presented correct technique Posttest: both intervention groups presented better technique score by 0.6 (90% confidence limits ± 0.5) relative to the CG, and 65% of the intervention groups presented the correct technique |
| da Roza (2012) 7 | Pre-post test pilot study | To evaluate the effect of a comprehensive PFMT program on UI symptoms in young nulliparous sport students | No | Sport students | Nulliparous Incontinent Performing high levels of physical activity classified according to the IPAQ-SF |
20.0 ± 0.8 | 7 | 7 | Vaginal palpation MVC (perineometry) ICIQ-SF QoL |
PFMT | 8 | VRP: pre 38.4 ± 15.7, post 55.8 ± 9.0 (P = 0.04) MVC: pre 73.4 ± 24.9, post 89.8 ± 19.1 (P = 0.04) FUL: pre 1.6 ± 1.5, post 0.1 ± 0.4 (P = 0.02) AUL pre 2.6 ± 1.5, post 0.3 ± 0.8 (P = 0.02) Impact on QOL: pre 2.9 ± 3.8, post 0.9 ± 2.3 (P = 0.07). ICIQ-SF score: pre 4.08 ± 6.0, post 0.75 ± 2.6 (P = 0.03) |
| Ferreira (2014) 10 | Randomized controlled trial | To verify the effectiveness of the PFMRP in female volleyball athletes, analyzing the amount and frequency of urinary leakage | Yes | Volleyball athletes | Nulliparous female volleyball athletes Symptoms of stress UI Age between 13 and 30 years Amount of urinary leakage >1 g |
19.3 | 32 | 16 | Pad test Questionnaires 7-day diary urinary leaking |
PFMT | 12 | Decrease in AUL: EG 45.5%, CG 4.9% Reduction in FUL: EG 14.3%, CG 0.05% P < 0.01 between groups |
| Pires (2020) 29 | Randomized controlled trial | To investigate the effects of PFMT in elite female volleyball athletes and whether it is an effective therapy for stress UI | Yes | Volleyball athletes | Age ≥18 years Elite female volleyball athletes Nulliparous Able to provide informed consent |
22.3 | 14 | 7 | MVC Pad test King’s Health Questionnaire |
PFMT | 16 | EG improved MVC (P < 0.01) and reduced urine loss (P = 0.03) Urine loss pre-post 71.4-42.9% Significant differences between groups in the variation from the initial to final phases |
| Alvarez Saez (2016) 1 | Quasi-experimental study | To test the effects of an HT program on body composition and PFM function parameters in a group of female rugby players | No | Rugby players | Nulliparous No contraindications to physical activity Not pregnant No hypertension |
23.4 ± 2.7 | 8 | 8 | Isolation TA test with biofeedback MVC during 10 seconds with a perionometer PFM tone with perionometer (2 isometric contraction of 10 seconds each) |
HT | 8 | MVC pre-post: 1165.29 (510.85)-1453.14 (529.69) (P = 0.02) PF tonicity pre-post: 212.57 (114.74) 329.00 (92.82) (P = 0.02) |
| Rivalta (2010) 33 | Case study | To test the use of combined PF rehabilitation treatment techniques in 3 young female athletes affected by UI | No | Volleyball athletes | 30.6 | 3 | 3 | 48-hour voiding diary PC test: PFM function and strength |
Biofeedback Electrical stimulation PFMT PFMT with vaginal cones |
12 | PC-test values pre-post (graded by the modified Oxford Grading Scale from 0 to 5) Patient 1: 2-5 Patient 2: 1-5 Patient 3: 2-5 After intervention, women stopped using UI requiring devices. No urinary leaking was reported during physical activity |
|
| Sousa (2015) 38 | Randomized controlled trial | To evaluate the effect of a comprehensive PFMT protocol on UI symptoms in young nulliparous athletes using a biomechanical model | Yes | Physically active females | Nulliparous Age ≥18 years Regular physical activity Consent to participate in the study Incontinent |
21.8 ± 3.6 | 7 | 7 | CONTILIFE PFM contraction (self-efficacy Scale of Broome) IPAQ-SF Pad Test PFM strength (perionometer) |
PFMT with or without supervision of a physical therapist | 8 | Pad-test pre-post supervised groups (P = 0.05) Supervised group: improvements in QoL, in self-efficacy of the PFM contractions, increase in PFM strength and decrease in leakage of urine by Pad-test |
AUL, amount of urinary leakage; CG, control group; EG, experimental group; EMG, electromyography; FUL, functional urethral length; HT, hypopressive technique; IIQ, Incontinence Impact Questionnaire; IPAQ, International Physical Activity Questionnaire; IPAQ-SF, IPAQ-short form; MVC, maximal voluntary contraction; PC, puborectalis; PF, pelvic floor; PFM, pelvic floor muscle; PFMRP, PFM rehabilitation program; PFMT, PFM training; QoL, quality of life; TA, transversus abdominis; UI, urinary incontinence; VRP, vaginal resting pressure.
The studies included in the review date from 2010 to 2021. All were longitudinal in nature, with interventions lasting between 6 and 16 weeks. A total sample of n = 187 women was included in the qualitative analysis, with a mean age of 22.8 years. Participants were physically active women (62.5%, n = 5), volleyball players (25%, n = 2), and rugby players (12.5%, n = 1).
Health-Related Quality of Life
Of the 8 articles, 4 included questionnaires to measure HRQoL.7,28,29,38 Different scales were used for each item. In the study by Sousa et al, 38 CONTILIFE scores were improved after an 8-week protocol in the group supervised by a physical therapist but not in the unsupervised group. Da Roza et al 7 used the ICIQ-SF questionnaire, with improved scores also after the 8-week PFMT course (P = 0.03). Furthermore, of the 7 sportswomen included in the study, 1 participant reported embarrassment and a desire to give up practicing sports because of UI. No significant differences were found between groups in the study of Piernicka et al 28 after the PFMT protocol according to the Incontinence Impact Questionnaire (IIQ) (P = 0.69). Pires et al 29 used the King’s Health Questionnaire, where the athletes did not feel like they were having urine loss and thus did not report it (P > 0.99).
Quantitative Analysis
Of the 8 articles selected for the review, 2 were excluded from the meta-analysis because they presented measurement variables that were unique among the other interventions.33,39 The remaining 6 articles were included in the meta-analysis, of which 66.7% (n = 4) included a control group.10,28,29,38 Because of this, pre- and postmeasurements were taken for all experimental groups to carry out comparison between them. Hence, a total sample of 58 women was included, with a mean age of 21.4 years. Three variables were analyzed: MVC of the PFM, AUL, and VRP.
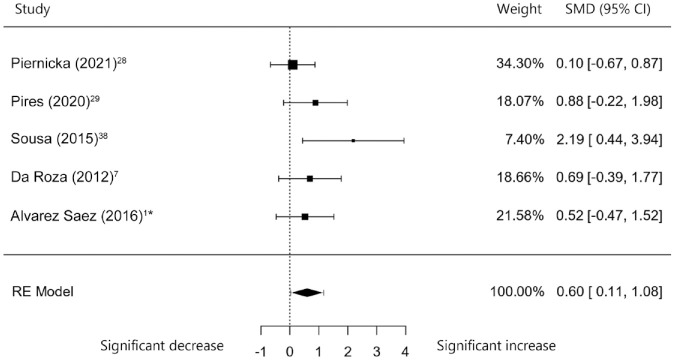
Maximal Voluntary Contraction
This variable was analyzed in k = 5 studies.1,7,28,29,38 The obtained values for the SMD ranged from 0.10 to 2.19, with most estimates being positive (100%). The estimated average SMD according to the random-effects model was 0.60 (95% CI, 0.11-1.08). Therefore, the average outcome differed significantly from zero (z = 2.42; P = 0.02). According to the Q test, there was no significant amount of heterogeneity in the true outcomes (Q (4) = 5.10; P = 0.28; τ2 = 0.02; I2 = 7.43%). The 95% prediction interval for the true outcomes was 0.03 to 1.17. Thus, even if there was some heterogeneity, the true outcomes of the studies analyzed were generally in the same direction as the estimated average outcome. The analysis of the studentized residuals showed that none of the studies had values larger than ±2.58; and then the model did not show outliers. Based on the Cook’s distances, none of the studies could be considered overly influential (Figure 2). Analyses of the rank correlation and the regression test did not indicate potential funnel plot asymmetry (P = 0.02 and P = 0.03, respectively).
Figure 2.
MVC forest plot (asterisk indicates measured for 10 seconds). MVC, maximal voluntary contraction; RE, random effects; SMD, standardized mean differences.
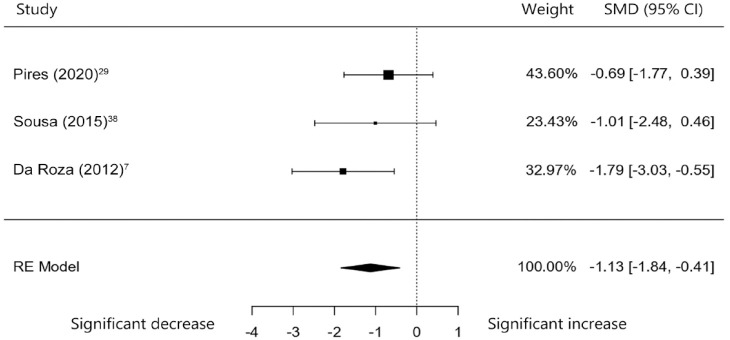
Amount of Urinary Leakage
The variable AUL was analyzed in k = 3 studies.7,29,38 The observed SMD showed values between -1.79 and -0.69, with most estimates being negative (100%). The estimated average SMD controlling for the random-effects model was -1.13 (95% CI, -1.84 to -0.41). Thus, the average outcome was significantly different from zero (z = -3.10; P < 0.01). The Q-test showed that there was no significant amount of heterogeneity in the true outcomes (Q (2) = 1.76; P = 0.41; τ2 = 0.00; I2 = 0.06%). The 95% prediction interval for the true outcomes ranged from -1.84 to -0.41. Thus, despite some heterogeneity, the true outcomes of the studies analyzed were generally in the same direction as the estimated average outcome. The studentized residuals analysis pointed out that none of the studies had values greater than ±2.39 and hence this model was not affected by outliers. None of the studies overly influenced the results according to the Cook’s distances (Figure 3). In addition, no funnel plot asymmetry was found according to the rank correlation and regression test (P > 0.99 and P = 0.77, respectively).
Figure 3.
AUL forest plot. AUL, amount of urinary leakage; RE, random effects; SMD, standardized mean differences.
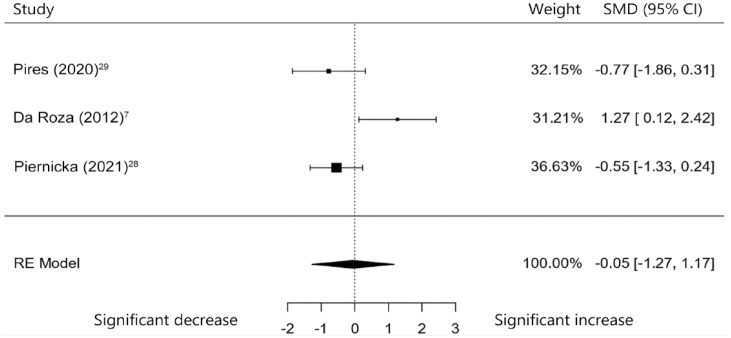
Vaginal Resting Pressure
The variable VRP was analyzed in k = 3 studies.7,28,29 The observed SMD ranged from -0.77 to 1.27, with most estimates being negative (67%). The estimated average SMD based on the random-effects model was -0.05 (95% CI, -1.27 to 1.17). Therefore, the average outcome did not differ significantly from zero (z = -0.08; P = 0.93). The true outcomes of analyses appeared to be heterogeneous according to the Q test: Q (2) = 8.14, P = 0.02, τ2 = 0.90, I2 = 77.68%. The 95% prediction interval for the true outcomes was established at ranging from -2.28 to 2.17. Thus, although the average outcome is estimated to be positive, in some studies the true outcome may in fact be negative. The studentized residuals analyses showed that only 1 study, that of da Roza et al, 7 had a large value (±2.39) and could be a potential outlier in the context of this model. Using Cook’s distances, none of the studies analyzed could be considered overly influential (Figure 4). Lastly, no funnel plot asymmetry was identified using the rank correlation and regression test (P = 0.33 and P = 0.51, respectively).
Figure 4.
VRP forest plot. RE, random effects; SMD, standardized mean differences; VRP, vaginal resting pressure.
Risk of Bias Assessment
Table 2 lists the scores awarded to each study. Of the 6 articles included in the meta-analysis, 5 showed acceptable-to-very-good values. The exception was the study carried out by Sousa et al, 38 which showed a poor methodological design, implying a high risk of bias. Breaking down the different sections, 5 items (purpose, literature review, validity of outcomes, reliability of outcomes, and clinical importance) revealed a score for all articles. The blinding and sample size items were not met for any article. According to ethics and consent, Ferreira et al 10 did not state the ethics committee used, and neither Sousa et al 38 nor da Roza et al 7 specified that participants signed a consent form. In addition, the only articles that specified the training protocol in detail, so that it could be reproduced, were Piernicka et al 28 and Alvarez Saez et al. 1 According to statistical analysis section, the only article that provided effect size was Piernicka et al. 28 Finally, for the conclusions item, there was a lack of information on some outcomes of the study in 4 of the 6 articles.1,7,28,38
Table 2.
McMaster scale for the risk of bias assessment
| Study | Pires (2020) 29 |
Piernicka (2021) 28 | Ferreira (2014) 10 | Sousa (2015) 38 |
da Roza (2012) 7 | Alvarez Saez (2016) 1 | Total | |
|---|---|---|---|---|---|---|---|---|
| Item a | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 6 |
| 2 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | |
| 3 | 1 | 1 | 1 | 1 | 0 | 0 | 4 | |
| 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 5 | 0 | 1 | 1 | 0 | 1 | 1 | 4 | |
| 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 7 | 1 | 1 | 0 | 0 | 0 | 1 | 3 | |
| 8 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | |
| 9 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | |
| 10 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | |
| 11 | 1 | 1 | 1 | 0 | 1 | 1 | 5 | |
| 12 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | |
| 13 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | |
| 14 | 1 | 0 | 1 | 0 | 0 | 0 | 2 | |
| 15 | 1 | 1 | 0 | 1 | 1 | 1 | 5 | |
| 16 | 1 | 1 | 0 | 1 | 1 | 1 | 5 | |
| Total | 11 | 13 | 9 | 8 | 9 | 11 | ||
Items: 1, purpose; 2, literature review; 3, study design; 4, blinding; 5, sample description; 6, sample size; 7, ethics and consent; 8, validity of outcomes; 9, reliability of outcomes; 10, intervention description; 11, statistical significance; 12, statistical analysis; 13, clinical importance; 14, conclusions; 15, clinical implications; 16, study limitations.
Discussion
The current systematic review and meta-analysis provides an in depth analysis of the efficacy of PFMT interventions in young, nulliparous female athletes. In particular, the scientific literature shows evidence of the efficacy of PFMT to prevent and treat PFD in women,4,9 and the need for athletes to maintain good PFM tone and strength to counteract ground-reaction forces. 4 However, few studies have conducted PFMT in athletes.1,7,10,28,29,33,38,39
Despite the low number of articles included, the efficacy of PFMT could be analyzed according to 3 variables: MVC, VRP, and AUL. It could be seen that pelvic floor interventions were effective in improving MVC in sportswomen. This parameter is effective in measuring PFM strength and contractile function, as it is important for building structural support during increases in IAP caused by exercise and day-to-day activities such as coughing or sneezing. 5
AUL was also reduced significantly after the interventions, as measured by the pad test in 2 of the 3 studies.29,38 In the study conducted by da Roza, 7 AUL was measured by ICIQ-SF scores. This, together with the small number of articles included in the meta-analysis of this variable, and the small sample size used by the studies, implies that these results should be viewed with caution. The analysis of the VRP variable in the selected studies did not yield significant results. In the study of Naess and Bø, 26 a reduction in the VRP was shown after several maximal PFM contractions. According to exercise interventions, Middlekauff et al 22 analyzed VRP in healthy nulliparous women after doing strenuous or nonstrenuous physical exercise; in both groups, VRP decreased significantly. This may be due to fatigue of the PFM after any type of exercise. However, in the study of Ree et al, 32 after intense physical exercise, there were no statistically significant variations in VRP, which is consistent with the results of this meta-analysis. Although in the aforementioned study the MVC was reduced by 20% after exercise and the VRP was maintained, the pelvic floor interventions analyzed in this meta-analysis showed that MVC was improved and VPR was maintained constant, which could be due to the good tone of pelvic floor structures that do not vary with performance of the sport but have also improved their contractile strength due to the intervention.
Our outcomes are analogous to those measured by another recent review with meta-analysis. 35 In this latter review, some articles were included in the meta-analysis that did not meet the inclusion criteria of the present study,3,19 whereas some others included in this article were not incorporated in the previous meta-analysis. 28
Young, nulliparous female athletes from different sports or physically active women were included in this study. There are not enough studies in the literature to compare by sporting discipline, leaving a gap in science that should be considered for future studies. Furthermore, despite not initially filtering by sex, no PFMT intervention studies were found in male athletes, even though the scientific literature shows a correlation between lower urinary tract symptoms and years of cycling in male athletes, independent of the age of the subjects. 24 In addition, the prevalence of genital numbness and erectile dysfunction in this male population has also been observed.13,37 Although it is assumed that PFD in men is related to an increase in abdominal and inguinal hernias, to date there are no scientific studies on this subject. Although this study did not investigate this population, it is possible that male athletes may also benefit from performing PFMT as part of their regular training.
Qualitative analysis of HRQoL shows heterogeneity in the results. The lack of significance in the IIQ score may be due to the exclusion of participants who did not have good HRQoL at baseline. 28 Thus, it might be more difficult to improve the HRQoL of those athletes who already had a high score. A different case is the study by Pires et al, 29 where participants were not aware of their urine leakage and therefore showed no impairment of their HRQoL. However, the pad test did show signs of UI, which demonstrates the need to carry out objective measures as, due to their subjective nature, the exclusive use of questionnaires may not be sufficient to detect problems and improvements in the athletes.
PFD is a widely studied problem that affects female athletes in their sports practice and reduces their quality of life. 17 An illustration of this is the study carried out by Sousa et al, 38 in which an athlete reported the desire to stop practising sport. The importance of performing PFMT lies in the fact that it could improve the HRQoL and general well-being of the athletes and, hence, improve their sports performance.
Regarding PFMT protocols, the studies included interventions lasting between 6 and 16 weeks. Half of them divided the protocol into different stages: (1) identification and awareness of contractions; (2) stabilization and strengthening of the PFM with progressive overload; and (3) power and contractions during sports practice.7,29,38 This last stage is aimed at improving closure of the urethra during the sporting actions that generate urine leakage. In 3 of the 6 articles,10,28,29 the knack technique was used, consisting of a voluntary and strong contraction before performing these sporting exercises. 23 Specifically, in these studies, shorter contractions (2-3 seconds) were combined with others of longer duration (6-10 seconds), as the progressive overload was produced, by increasing the intensity and length of the contractions, reducing resting times, and/or evolving performance postures toward standing positions and sports movements. A different case was the study carried out by Alvarez Saez et al. 1 These authors used a training protocol based on the hypopressive technique (HT), which has generated controversy in recent years regarding its benefits to improve the tone of the PFM.21,36
The study carried out by Sousa et al, 38 despite having the least weight in the result of the meta-analysis, is the one that provides the greatest CI in terms of the increase in MVC and decrease in AUL. The opposite occurs with the study of Piernicka et al, 28 who found a greater weight in terms of the result in the improvement of MVC but the smallest CI. However, the study by Sousa et al 38 showed poor methodological design and a high risk of bias, with some information missing. Due to this fact, no firm conclusions can be drawn from this study.
Regarding the intervention times followed in the included studies, interventions lasting ~8 weeks focusing on the abovementioned 3 stages and combining contractions of different length (from 2-3 to 10 seconds) can be proposed.
Also, it may be of interest to reach a final stage in which these contractions are included in the moments during which an increase in IAP is produced, both in sporting actions and outside of sport practice (sneezing, coughing).
There are significant limitations to this study. The results extracted from this study should be viewed with caution due to the existence of very few studies that carried out PFMT interventions with athletes, the small sample size, and the risk of bias present in some items of the analysis.
Conclusion
Female athletes are more at risk of experiencing pelvic floor dysfunctions compared with sedentary women, 40 which affects their quality of life and creates a barrier to sports practice. 17
The present systematic review and meta-analysis shows the efficacy of PFM interventions on increasing PFM strength and reducing urine leakage in female athletes, with PFMT being a powerful tool to prevent and treat pelvic floor dysfunctions in this population.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Alvarez Saez M, Rial Rebullido T, Chulvi Medrano I, García Soidán JL, Cortell Tormo JM. Can an eight-week program based on the hypopressive technique produce changes in pelvic floor function and body composition in female rugby players? Retos Nuevas Tendencias en Educacion Fisica Deporte y Recreacion. 2016;30(5):26-29. [Google Scholar]
- 2. Alves JO, Luz ST da, Brandão S, da Luz CM, Jorge RN, da Roza T. Urinary incontinence in physically active young women: prevalence and related factors. Int J Sports Med. 2017;38(12):937-941. [DOI] [PubMed] [Google Scholar]
- 3. Azevedo RMF. Eficácia do Treino dos Músculos do Pavimento Pélvico no Tratamento da Incontinência Urinária de Esforço em Jovens Atletas: Um Estudo Clínico Randomizado Controlado. Universidade Fernando Pessoa; (Portugal: ); 2013. [Google Scholar]
- 4. Bø K. Physiotherapy management of urinary incontinence in females. J Physiother. 2020;66(3):147-154. [DOI] [PubMed] [Google Scholar]
- 5. Cho ST, Kim KH. Pelvic floor muscle exercise and training for coping with urinary incontinence. J Exerc Rehabil. 2021;17(6):379-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101-129. [Google Scholar]
- 7. da Roza T, de Araujo MP, Viana R, et al. Pelvic floor muscle training to improve urinary incontinence in young, nulliparous sport students: a pilot study. Int Urogynecol J. 2012;23(8):1069-1073. [DOI] [PubMed] [Google Scholar]
- 8. de Mattos Lourenco TR, Matsuoka PK, Baracat EC, Haddad JM. Urinary incontinence in female athletes: a systematic review. Int Urogynecol J. 2018;29(12):1757-1763. [DOI] [PubMed] [Google Scholar]
- 9. Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ferreira S, Ferreira M, Carvalhais A, Santos PC, Rocha P, Brochado G. Reeducation of pelvic floor muscles in volleyball athletes. Rev Assoc Med Bras. 2014;60(5):428-433. [Google Scholar]
- 11. Fozzatti C, Riccetto C, Herrmann V, et al. Prevalence study of stress urinary incontinence in women who perform high-impact exercises. Int Urogynecol J Pelvic Floor Dysfunct. 2012;23(12):1687-1691. [DOI] [PubMed] [Google Scholar]
- 12. Frawley H, Shelly B, Morin M, et al. An International Continence Society (ICS) report on the terminology for pelvic floor muscle assessment. Neurourol Urodyn. 2021;40(5):1217-1260. [DOI] [PubMed] [Google Scholar]
- 13. Gemery JM, Nangia AK, Mamourian AC, Reid SK. Digital three-dimensional modelling of the male pelvis and bicycle seats: impact of rider position and seat design on potential penile hypoxia and erectile dysfunction. BJU Int. 2007;99(1):135-140. [DOI] [PubMed] [Google Scholar]
- 14. Goldstick O, Constantini N. Urinary incontinence in physically active women and female athletes. Br J Sports Med. 2014;48(4):296-298. [DOI] [PubMed] [Google Scholar]
- 15. Hagovska M, Švihra J, Buková A, et al. Prevalence of urinary incontinence in females performing high-impact exercises. Int J Sports Med. 2017;38(3):210-216. [DOI] [PubMed] [Google Scholar]
- 16. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5-26. [DOI] [PubMed] [Google Scholar]
- 17. Jácome C, Oliveira D, Marques A, Sá-Couto P. Prevalence and impact of urinary incontinence among female athletes. Int J Gynecol Obstet. 2011;114(1):60-63. [DOI] [PubMed] [Google Scholar]
- 18. jamovi. The jamovi project. https://www.jamovi.org.Accessed May 25, 2022.
- 19. Korelo RIG, Kosiba CR, Grecco L, Matos RA. Influência do fortalecimento abdominal na função perineal, associado ou não à orientação de contração do assoalho pélvico, em nulíparas. Fisioterapia em Movimento. 2011;24(1):75-85. [Google Scholar]
- 20. Law M, MacDermid J. Modified Guidelines for use of the McMasters Critical Appraisal Form for Quantitative Studies. In: Evidence-Based Rehabilitation. 2nd ed. Slack; 1998. [Google Scholar]
- 21. Martín-Rodríguez S, Bø K. Is abdominal hypopressive technique effective in the prevention and treatment of pelvic floor dysfunction? Marketing or evidence from high-quality clinical trials? Br J Sports Med. 2019;53(2):135-136. [DOI] [PubMed] [Google Scholar]
- 22. Middlekauff ML, Egger MJ, Nygaard IE, Shaw JM. The impact of acute and chronic strenuous exercise on pelvic floor muscle strength and support in nulliparous healthy women. Am J Obstet Gynecol. 2016;215(3):316.e1-316.e7. [DOI] [PubMed] [Google Scholar]
- 23. Miller JM, Sampselle C, Ashton-Miller J, Hong GRS, DeLancey JOL. Clarification and confirmation of the Knack maneuver: the effect of volitional pelvic floor muscle contraction to preempt expected stress incontinence. Int Urogynecol J. 2008;19(6):773-782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Molina-Torres G, Ochandorena-Acha M, Echazarreta-Aparicio Y, et al. Is cycling practice related to men’s pelvic floor dysfunctions? A hypothesis-generating observational study. Int J Environ Res Public Health. 2021;18(4):1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mørkved S, Bø K. Effect of pelvic floor muscle training during pregnancy and after childbirth on prevention and treatment of urinary incontinence: a systematic review. Br J Sports Med. 2014;48(4):299-310. [DOI] [PubMed] [Google Scholar]
- 26. Naess I, Bø K. Can maximal voluntary pelvic floor muscle contraction reduce vaginal resting pressure and resting EMG activity? Int Urogynecol J. 2018;29(11):1623-1627. [DOI] [PubMed] [Google Scholar]
- 27. Nygaard IE, Glo Wacki C, Saltzman CL. Relationship between foot flexibility and urinary incontinence in nulliparous varsity athletes. Obstet Gynecol. 1996;87(6):1049-1051. [DOI] [PubMed] [Google Scholar]
- 28. Piernicka M, Błudnicka M, Kortas J, Duda-Biernacka B, Szumilewicz A. High-impact aerobics programme supplemented by pelvic floor muscle training does not impair the function of pelvic floor muscles in active nulliparous women. Medicine. 2021;100(33):e26989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pires TF, Pires PM, Moreira MH, et al. Pelvic floor muscle training in female athletes: a randomized controlled pilot study. Int J Sports Med. 2020;41(4):264-270. [DOI] [PubMed] [Google Scholar]
- 30. Pires T, Pires P, Moreira H, Viana R. Prevalence of urinary incontinence in high-impact sport athletes: a systematic review and meta-analysis. J Hum Kinet. 2020;73:279-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pizzol D, Demurtas J, Celotto S, et al. Urinary incontinence and quality of life: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33(1):25-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ree ML, Nygaard I, Bø K. Muscular fatigue in the pelvic floor muscles after strenuous physical activity. Acta Obstet Gynecol Scand. 2007;86(7):870-876. [DOI] [PubMed] [Google Scholar]
- 33. Rivalta M, Sighinolfi MC, Micali S, de Stefani S, Torcasio F, Bianchi G. Urinary incontinence and sport: first and preliminary experience with a combined pelvic floor rehabilitation program in three female athletes. Health Care Women Int. 2010;31(5):435-443. [DOI] [PubMed] [Google Scholar]
- 34. Romeikienė KE, Bartkevičienė D. Pelvic-floor dysfunction prevention in prepartum and postpartum periods. Medicina (Kaunas). 2021;57(4):387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Romero-Franco N, Molina-Mula J, Bosch-Donate E, Casado A. Therapeutic exercise to improve pelvic floor muscle function in a female sporting population: a systematic review and meta-analysis. Physiotherapy. 2021;113:44-52. [DOI] [PubMed] [Google Scholar]
- 36. Ruiz de Viñaspre Hernández R. Efficacy of hypopressive abdominal gymnastics in rehabilitating the pelvic floor of women: a systematic review. Actas Urol Esp (Engl Ed). 2018;42(9):557-566. [DOI] [PubMed] [Google Scholar]
- 37. Sommer F, König D, Graf C, et al. Impotence and genital numbness in cyclists. Int J Sports Med. 2001;22(6):410-413. [DOI] [PubMed] [Google Scholar]
- 38. Sousa M, Viana R, Viana S, et al. Effects of a pelvic floor muscle training in nulliparous athletes with urinary incontinence: biomechanical models protocol. In: Manuel J, Tavares RS, Natal Jorge RM. (eds) Computational and Experimental Biomedical Sciences: Methods and Applications. Basel: Springer International Publishing; 2015:83-90. [Google Scholar]
- 39. Szumilewicz A, Hopkins WG, Dornowski M, Piernicka M. Exercise professionals improve their poor skills in contracting pelvic-floor muscles: a randomized controlled trial. Res Q Exerc Sport. 2019;90(4):641-650. [DOI] [PubMed] [Google Scholar]
- 40. Teixeira RV, Colla C, Sbruzzi G, Mallmann A, Paiva LL. Prevalence of urinary incontinence in female athletes: a systematic review with meta-analysis. Int Urogynecol J. 2018;29(12):1717-1725. [DOI] [PubMed] [Google Scholar]
- 41. Viechtbauer W. Conducting meta-analyses in R with the Metafor package. J Stat Softw. 2010;36(3):1-48. [Google Scholar]