Abstract
Vitiligo is an autoimmune skin depigmenting disorder that can negatively impact quality of life. A new FDA approved treatment for vitiligo offers considerable promise, and to maximize benefits strategies to implementation should consider disease burden, healthcare access, and healthcare utilization of individuals with vitiligo. Using the All of Us Research Program’s large data set, including survey responses, we investigated these outcomes among participants with and without vitiligo. Our analysis used quality of life, delayed care due to an obstacle, and seeing a doctor in the past year as dichotomized proxies for disease burden, healthcare access, and healthcare utilization. The results show that people with vitiligo are more likely to report worse quality of life but ostensibly greater healthcare access and utilization compared to people without vitiligo. However, these relationships are not significant when adjusted for demographics, socioeconomic characteristics, and comorbidities of vitiligo. Prior research has shown non-Caucasian individuals have worse health outcomes in general, and worse quality of life within the vitiligo population. Our data demonstrated consistent findings; moreover, we found that non-Caucasian individuals with vitiligo had inferior healthcare access and lower health care utilization than Caucasian individuals. Implementation of new treatments for vitiligo should prioritize disadvantaged individuals to improve health equity.
Keywords: Vitiligo, Healthcare Access, Healthcare Utilization, Quality of Life
Introduction
Vitiligo is an autoimmune skin disorder caused by the loss of melanocytes and resulting in white patches of skin [4]. It is the most common depigmenting skin disorder and affects 0.5%−2% of people [4]. The condition can develop at any age, but most commonly presents in individuals 10 to 30 years old [4]. The disorder appears in people of all ethnic groups and skin types [4], but it may affect the quality of life of people with darker skin more severely [5]. Ruxolitinib Cream is the only treatment FDA approved for the repigmentation of vitiligo [8].
Patients with vitiligo are more likely to experience negative psychosocial effects such as anxiety, depression, and poorer quality of life [7, 13, 16]. One literature review of health-related quality of life impacts of vitiligo reported that negative effects “are evidenced in measurements of self-esteem, body image, stigma, and anxiety” [5]. The study also found that characteristics, such as having highly contrasting dark skin, were associated with worse health-related quality of life [5], indicating different health outcomes by race and ethnicity. A more recent survey found a similar result among patients with skin disease on the face and hands generally, reporting they are more likely to feel stigmatized and to experience other negative social effects [17].
Individuals with vitiligo may also have limited access to health care. A recent real-world study by Rosmarin et al. found that roughly half of patients with vitiligo did not receive any treatment during the first year following diagnosis [18]. In response to a 2016 survey of 87 individuals with vitiligo, some participants reported barriers to healthcare access, including treatment cost and the scheduling of medical appointments [6]. Notably, this putative finding of limited healthcare access may reflect the tendency for non-Caucasian individuals older than age 65 to be diagnosed with vitiligo, as reported for participants in a large dataset, [2] and the well-established health care access barriers and worse health outcomes prevalent among non-Caucasian individuals in the US [11, 12].
This study takes advantage of a large dataset of demographically, geographically, and medically diverse participants to further explore the disease burden imposed by vitiligo, and healthcare access and utilization among individuals with vitiligo. Further, we aim to investigate whether these outcomes may be mediated by race and ethnicity, socioeconomic status, and related health conditions. An examination of disease burden, healthcare access, and healthcare utilization can inform implementation strategies to maximize treatment uptake and optimize patient outcomes. Analyzing the relationship between patient characteristics and these health measures can help identify subgroups at higher risk of poor outcomes or lower healthcare access, facilitating the development of targeted interventions.
Materials and Methods
Data Source and Study Sample
Our analysis used survey data from “All of Us”, a research program from the National Institute of Health that provides a large, longitudinal dataset on U.S. participants [3]. The All of Us dataset is well-suited for this investigation because it collects a broad range of sociodemographic, clinical, and healthcare utilization information, targeting populations that have been historically underrepresented in biomedical research [3]. The program provides data from surveys, electronic health records (EHR), physical measurements, biospecimens, and digital health data such as wearables [3].
Within the All of Us data portal (“workbench”), we identified individuals with vitiligo using pre-set cohorts based on their clinical characteristics. Vitiligo is identified in All of Us based on the following diagnosis codes available in participants’ EHRs: ICD-10-CM code L80, ICD-9-CM code 709.01, and SNOMED code 56727007.
Health Outcomes
All of Us collects various health outcomes in surveys conducted when participants enter the program. In this analysis, we assessed three outcome measures.
Our first health outcome was quality of life. We used responses to a question from the “Overall Health” survey asking participants to rate their overall quality of life on a five-point scale: excellent, very good, good, fair, or poor. We transformed responses to a binary outcome indicating either worse quality of life (fair or poor) or better quality of life (good, very good, or excellent).
Our second health outcome was healthcare access. We used responses to a question from the “Healthcare Access & Utilization” survey asking participants if they have experienced delayed care during the past calendar year due to the following obstacles: didn’t have transportation, lived in a rural area where distance to the health care provider is too far, nervous about seeing a health care provider, couldn’t get time off work, couldn’t get child care, provide care to an adult and could not leave him/her, couldn’t afford the copay, deductible was too high or could not afford the deductible, or had to pay out of pocket for some or all of the procedure. We represented access with a binary outcome that indicated the imposition of delay if the participant reported care to be delayed for any reason.
Our third health outcome was healthcare utilization. We used another response from the “Overall Health” survey and designated healthcare utilization as “yes” if the respondent indicated they had visited a doctor within the past year.
Sample Characteristics
Participant characteristics data came from the All of Us “The Basics” survey for demographic and socioeconomic characteristics, including race/ethnicity, gender, age, education level, household income, whether the participant was born in the U.S., whether the participant has health insurance, and the number of difficulties in daily activities. Possible responses for race/ethnicity come from the U.S. Census 2015 National Content Test [1], which we transformed to a categorical variable with levels Caucasian, Black, Hispanic, and Other (including American Indian or Alaska Native, Asian, Middle Eastern or North African, Native Hawaiian or other Pacific Islander, multiple race/ethnicities, and does not identify with any listed race/ethnicity). Number of difficulties in daily activities came from a multi-choice survey question that asks participants if they experience: serious difficulty hearing or deafness, serious difficulty seeing or blindness, difficulty concentrating, remembering, or making decisions, difficulty walking or climbing stairs, difficulty dressing or bathing, or difficulty doing errands.
We used All of Us’ EHR data to identify comorbidities prevalent among individuals with vitiligo using ICD-9, ICD-10, and SNOMED codes. Comorbidities were selected based on previous literature and included psoriasis, atopic dermatitis, localized scleroderma, alopecia areata, cutaneous lupus erythematosus, rheumatoid arthritis, type I diabetes mellitus, disorder of thyroid gland, inflammatory bowel disease, Sjogren syndrome, systemic lupus erythematosus, Addison’s disease, celiac disease, pernicious anemia, and dermatomyositis [2, 14].
Statistical Analysis
We used descriptive and regression analyses to assess the association between vitiligo and health outcomes of interest. We completed all analyses within the All of Us workbench using R from April to September 2023. We compared sample characteristics between participants with and without vitiligo using chi-squared tests for categorical variables and t-tests for continuous variables. We conducted descriptive analysis using chi-squared tests to evaluate differences in the three health outcomes between the populations with and without vitiligo, and between Caucasian and non-Caucasian individuals within the vitiligo population.
We performed three sets of logistic regression analysis to assess relationships between vitiligo and the three dichotomized health outcomes (quality of life, delayed care due to obstacles, and seeing a doctor within the past year), adjusting for demographics, socioeconomic characteristics, and comorbidities of vitiligo.
Results
Population Characteristics
As of September 2023, there were 409,218 participants with available data in the All of Us program. Of these participants, 1,094 have vitiligo (0.3%). Ahmed and colleagues [2] found that compared with the non-vitiligo population, All of Us participants with vitiligo were older, more likely to have health insurance, more likely to identify as Hispanic, and more likely to have a comorbidity associated with vitiligo. Our results suggested similar trends (Table 1).
Table 1:
Demographic, Socioeconomic, and Clinical Characteristics in Populations With and Without Vitiligo
| With Vitiligo (n = 1,094) |
Without Vitiligo (n = 408,124) |
P-value | |
|---|---|---|---|
| Race/Ethnicity | <0.001 | ||
| Caucasian | 532 (49%) | 222,114 (55%) | |
| Black | 210 (19%) | 76,859 (19%) | |
| Hispanic | 241 (22%) | 64,431 (16%) | |
| Other | 94 (9%) | 47,187 (9%) | |
| Female | 694 (64%) | 246,954 (62%) | 0.103 |
| Age | <0.001 | ||
| 18–39 | 104 (10%) | 97,148 (24%) | |
| 40–59 | 295 (27%) | 131,536 (32%) | |
| 60–79 | 581 (53%) | 153,884 (38%) | |
| 80+ | 114 (10%) | 25,556 (6%) | |
| Education Level | 0.008 | ||
| Non-high school graduate | 110 (10%) | 36,322 (9%) | |
| High school graduate | 440 (41%) | 180,710 (45%) | |
| College graduate | 254 (23%) | 92,984 (23%) | |
| Advanced degree | 277 (26%) | 88,830 (22%) | |
| Household Income | 0.179 | ||
| <$25k | 251 (29%) | 102,468 (31%) | |
| $25k-$50k | 159 (18%) | 61,660 (19%) | |
| $50k-$100k | 206 (24%) | 77,290 (23%) | |
| $100k-$200k | 172 (20%) | 61,271 (19%) | |
| >$200k | 88 (10%) | 26,784 (8%) | |
| Born in US | 822 (75%) | 342,748 (84%) | <0.001 |
| Has health insurance | 1047 (96%) | 370,586 (91%) | <0.001 |
| Number of difficulties in daily activities, mean (s.d.) | 0.18 (0.64) | 0.19 (0.64) | 0.629 |
| Number of comorbidities, mean (s.d.) | 0.46 (0.73) | 0.10 (0.35) | <0.001 |
Health Outcomes
To evaluate health outcomes, we included participants who had completed the “Overall Health” and “Healthcare Access & Utilization” surveys, or 190,209 participants (46% of all participants), of whom 573 have vitiligo (52% of the vitiligo population).
Among All of Us participants, the proportion reporting fair or poor quality of life was higher among individuals with vitiligo than among those without the condition (14% vs. 11%, p=0.037) (Figure 1). However, the proportion reporting delayed care during the past year due to obstacles (31% vs. 36%, p=0.020) or not seeing a doctor during the past year (6% vs. 11%, p<0.001) was lower among participants with vitiligo.
Figure 1:
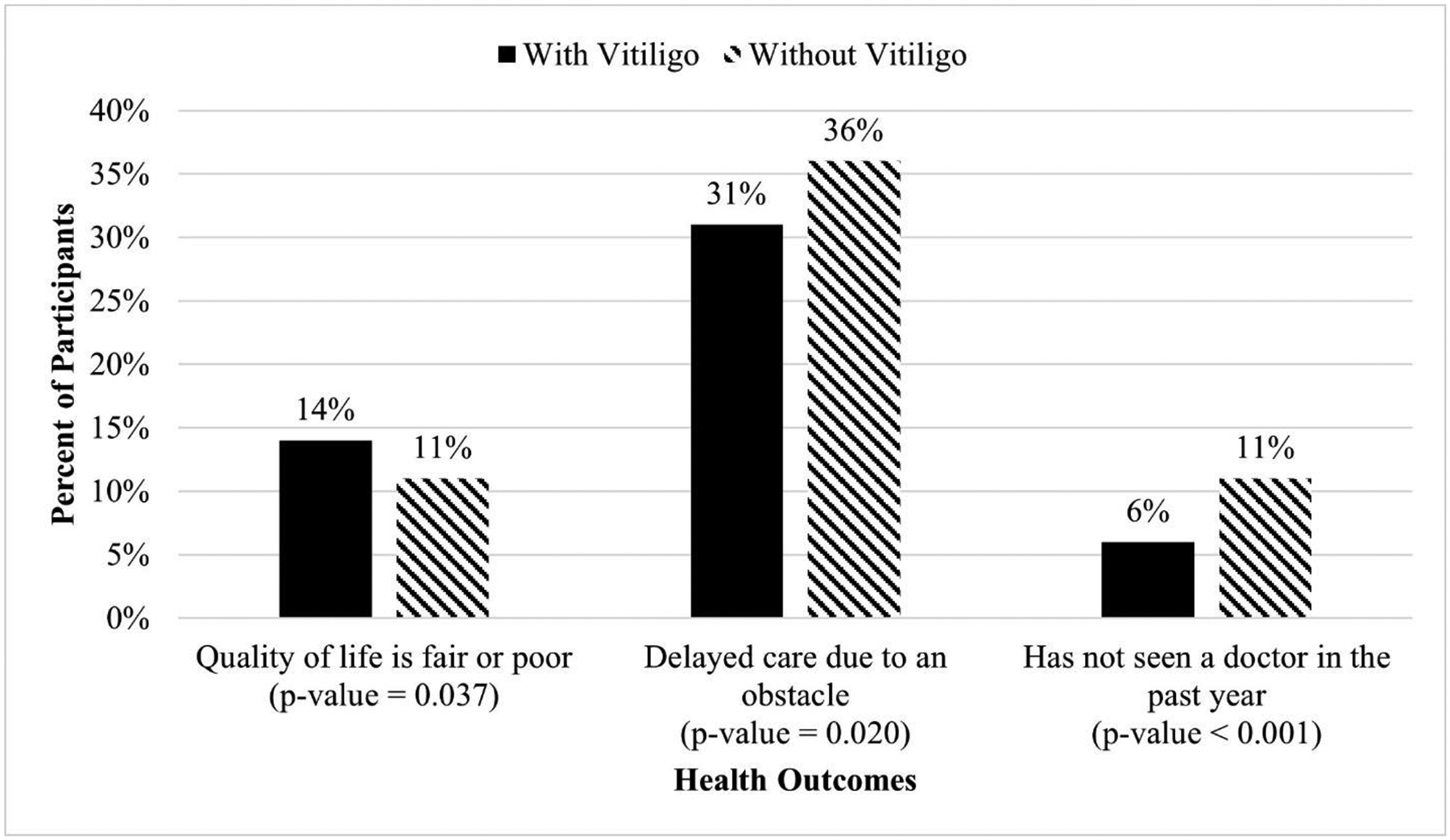
Health Outcomes Among All of Us Participants With and Without Vitiligo (N=190,199)
We repeated this analysis within the vitiligo population and found that compared to participants with vitiligo who identify as Caucasian, participants with vitiligo who identify as non-Caucasian were more likely to report quality of life as fair or poor (24% vs. 7%, p<0.001) and more likely to report delaying care due to an obstacle (42% vs. 26%, p<0.001) (Figure 2).
Figure 2: Health Outcomes Among All of Us Participants With Vitiligo, Stratified by Race/Ethnicity (N=573).
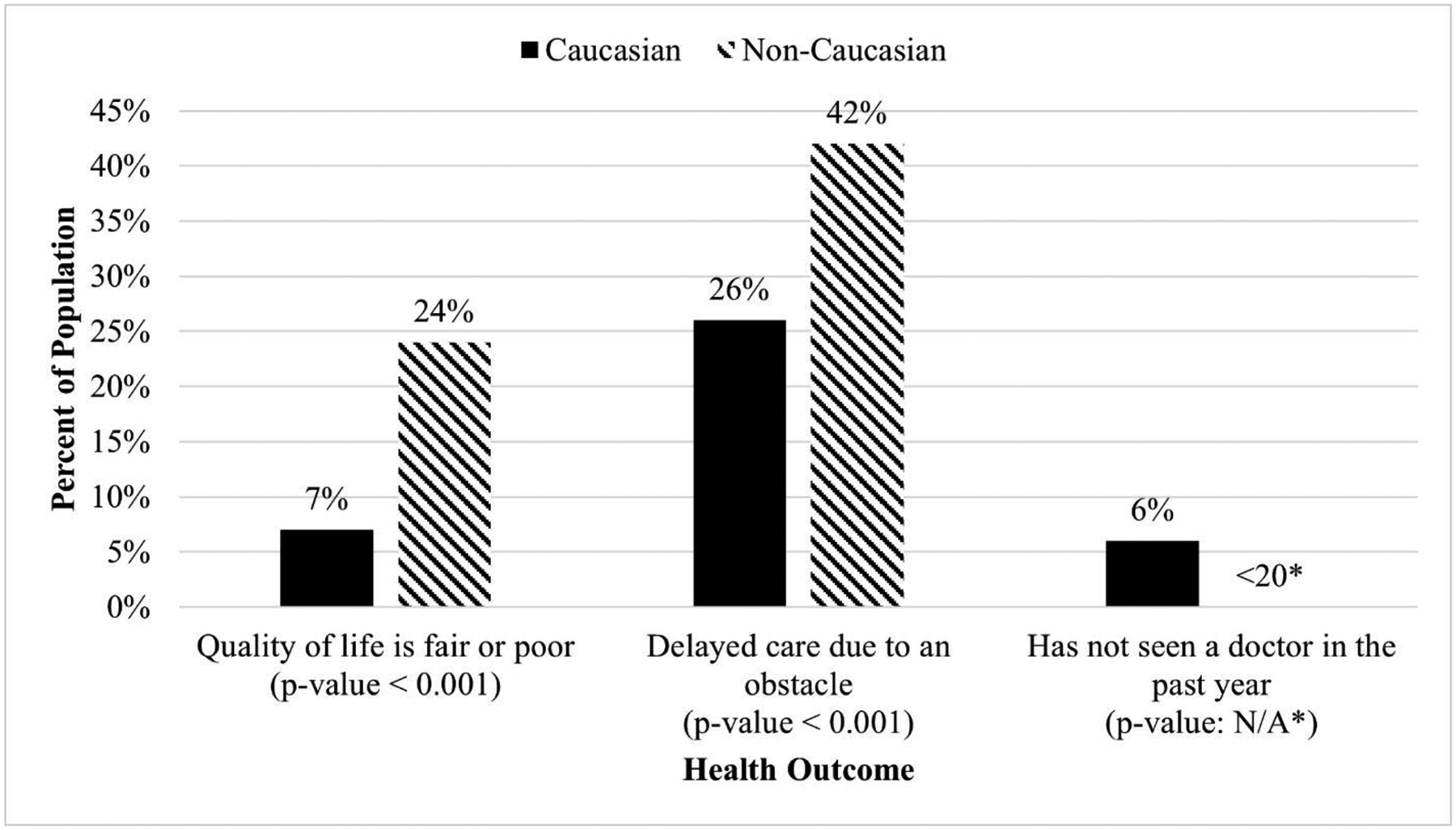
*The All of Us data use agreement prohibits reporting statistics representing fewer than 20 individuals
Regression Analysis
When adjusted for participant characteristics, the relationship between vitiligo and health outcomes was not statistically significant for any of the three health outcomes we examined: quality of life is fair or poor (OR=1.28, 95% CI: 0.98–1.66), delayed care due to an obstacle (OR=1.04, 95% CI: 0.86–1.26), and not seen a doctor in the past year (OR=0.71, 95% CI: 0.50–1.01) (Table 2).
Table 2:
Odds Ratios of Health Outcomes
| Quality of life is fair or poor (n = 188,595) |
Delayed care due to an obstacle (n = 190,199) |
Has not seen a doctor in the past year (n = 190,199) |
|
|---|---|---|---|
| Vitiligo | 1.28 (0.98–1.66) | 1.04 (0.86–1.26) | 0.71 (0.50–1.01) |
| Race/Ethnicity | |||
| Caucasian | Ref | Ref | Ref |
| Black | 1.08 (1.03–1.13)* | 0.95 (0.92–0.98)* | 1.27 (1.21–1.33)* |
| Hispanic | 1.09 (1.04–1.15)* | 0.98 (0.95–1.01) | 1.44 (1.38–1.51)* |
| Other | 1.31 (1.22–1.40)* | 1.07 (1.03–1.12)* | 1.32 (1.25–1.39)* |
| Female vs. Male | 0.94 (0.91–0.97)* | 1.43 (1.40–1.46)* | 0.93 (0.91–0.96)* |
| Age | |||
| 18–39 | Ref | Ref | Ref |
| 40–59 | 1.61 (1.55–1.68)* | 0.67 (0.65–0.69)* | 0.60 (0.58–0.62)* |
| 60–79 | 0.88 (0.85–0.92)* | 0.25 (0.24–0.25)* | 0.34 (0.33–0.36)* |
| 80+ | 0.35 (0.31–0.38)* | 0.10 (0.10–0.11)* | 0.22 (0.20–0.24)* |
| Education Level | |||
| Non-high school graduate | Ref | Ref | Ref |
| High school graduate | 0.93 (0.88–0.99)* | 1.11 (1.06–1.17)* | 1.01 (0.95–1.08) |
| College graduate | 0.61 (0.57–0.65)* | 1.00 (0.95–1.05) | 0.92 (0.86–0.98)* |
| Advanced degree | 0.49 (0.46–0.53)* | 0.95 (0.90–1.00)* | 0.90 (0.84–0.96)* |
| Household Income | |||
| <$25k | Ref | Ref | Ref |
| $25k-$50k | 0.68 (0.65–0.71)* | 1.12 (1.09–1.16)* | 0.99 (0.94–1.03) |
| $50k-$100k | 0.38 (0.37–0.40)* | 0.81 (0.78–0.83)* | 0.95 (0.91–1.00)* |
| $100k-$200k | 0.23 (0.21–0.24)* | 0.61 (0.59–0.63)* | 0.88 (0.84–0.93)* |
| >$200k | 0.13 (0.12–0.15)* | 0.47 (0.45–0.49)* | 0.88 (0.82–0.93)* |
| Born in the US | 1.26 (1.20–1.33)* | 1.11 (1.08–1.15)* | 1.07 (1.02–1.12)* |
| Has health insurance | 1.03 (0.97–1.09) | 0.67 (0.64–0.70)* | 0.37 (0.35–0.39)* |
| Number of difficulties in daily activities | 1.90 (1.86–1.93)* | 1.25 (1.23–1.27)* | 0.80 (0.78–0.82)* |
| Number of comorbidities | 1.39 (1.34–1.44)* | 1.00 (0.97–1.03) | 0.52 (0.49–0.55)* |
| Intercept | 0.18 (0.16–0.19)* | 1.50 (1.42–1.59)* | 0.63 (0.59–0.68)* |
Significant at the 0.05 level Ref = reference
With few exceptions, almost all demographic and socioeconomic characteristics in our analysis were significantly associated with quality of life, delayed care due to obstacles, and not seeing a doctor. Compared to Caucasian individuals, other groups were more likely to report quality of life as fair or poor (Black: OR=1.08, 95% CI: 1.03–1.13; Hispanic: OR=1.09, 95% CI=1.04–1.15; other racial/ethnic groups: OR=1.31, 95% CI: 1.22–1.40). These groups were also more likely to report not seeing a doctor in the past year (Black: OR=1.27, 95% CI: 1.21–1.33; Hispanic: OR=1.44, 95% CI: 1.38–1.51; other racial/ethnic groups: OR=1.32, 95% CI: 1.25–1.39). Individuals of other race/ethnicity were significantly more likely to report delayed care due to obstacles (OR=1.07, 95% CI: 1.03–1.12), while this likelihood was lower among Black individuals (OR=0.95, 95% CI: 0.92–0.98).
Discussion
While in our unadjusted analysis, vitiligo was associated with quality of life, delaying care due to an obstacle, and seeing a doctor in the past year, none of these associations remained following adjustment for demographics, socioeconomic characteristics, and the comorbidities of vitiligo. These findings suggest that other characteristics, rather than vitiligo, mediate and explain the observed differences in health outcomes and access between the vitiligo and non-vitiligo populations. In the vitiligo population, our results suggest that non-Caucasian individuals tend to have worse health outcomes than Caucasian individuals. However, this association is not unique to the vitiligo population, as our analysis and many other investigations have shown.
Our results are consistent with prior findings based on the All of Us data [2] and with analyses showing that vitiligo is more prevalent in Hispanic patients in the US [2, 15]. The previous literature has also shown that diagnosed vitiligo is more prevalent in Asian American patients [15], although this analysis did not explore that association. Other research has shown individuals with vitiligo are more likely to experience psychosocial effects, anxiety, and a generally diminished quality of life [5, 7, 13, 16]. We also found that non-Caucasian individuals have worse health outcomes overall, a finding that is consistent with what surveys of the general population have reported [11, 12]. Our results suggest an association between race/ethnicity and vitiligo that is consistent with prior analyses [5]. Our results suggest that special attention to non-Caucasian individuals may improve equity because of documented systemic disadvantages they face [11, 12] that also may manifest in the vitiligo community.
The All of Us survey data strengthens this research, but we note some limitations. Since participation in All of Us is voluntary, there is potential for self-selection. The fact that some recruitment occurs in health care provider settings [3] could favor participation by individuals with the greatest healthcare access [9]. All of Us mitigates these issues by also using personal interest groups and targeted advertising to recruit subjects, and by targeting groups historically underrepresented in clinical research. Finally, research suggests that up to 40% of U.S. vitiligo cases may be undiagnosed [10] and thus not reflected in the EHR data that identifies the All of Us cohort. All of Us surveys ask about skin disease but not specifically about vitiligo, so we cannot estimate the potential for underdiagnosis. Furthermore, we cannot determine the influence that vitiligo has on survey responses. Future data collection and research should address this gap.
Vitiligo can adversely affect quality of life, and individuals with vitiligo may have greater healthcare access and utilization, but these associations are not statistically significant when adjusted for demographics, socioeconomic characteristics, and comorbidities of vitiligo. However, these results indicate that while all individuals with vitiligo are affected by their disease, individuals who identify as non-Caucasian may experience an increased impact on quality of life and challenges in healthcare access and utilization. Incorporating special considerations for these subpopulations in healthcare practice may lead to improved quality of life outcomes.
Acknowledgements
We would like to thank Swapna Ambati and Dilan Paranagama from Incyte Corporation for their comments on this work. The All of Us Research Program is supported by the National Institutes of Health, Office of the Director: Regional Medical Centers: 1 OT2 OD026549; 1 OT2 OD026554; 1 OT2 OD026557; 1 OT2 OD026556; 1 OT2 OD026550; 1 OT2 OD 026552; 1 OT2 OD026553; 1 OT2 OD026548; 1 OT2 OD026551; 1 OT2 OD026555; IAA #: AOD 16037; Federally Qualified Health Centers: HHSN 263201600085U; Data and Research Center: 5 U2C OD023196; Biobank: 1 U24 OD023121; The Participant Center: U24 OD023176; Participant Technology Systems Center: 1 U24 OD023163; Communications and Engagement: 3 OT2 OD023205; 3 OT2 OD023206; and Community Partners: 1 OT2 OD025277; 3 OT2 OD025315; 1 OT2 OD025337; 1 OT2 OD025276. In addition, the All of Us Research Program would not be possible without the partnership of its participants.
Funding
This study was supported by a grant from Incyte Corporation (Wilmington, DE, USA)
Competing Interests
David Rosmarin has consulted, spoken for, or conducted trials for the following companies: AbbVie, Abcuro, Almirall, AltruBio, Amgen, Arena, Astria, Boehringer-Ingelheim, Bristol Meyers Squibb, Celgene, Concert, CSL Behring, Dermavant, Dermira, Galderma, Incyte, Janssen, Kyowa Kirin, Lilly, Merck, Nektar, Novartis, Pfizer, RAPT, Regeneron, Recludix, Revolo Biotherapeutics, Sanofi, Sun Pharmaceuticals, UCB, VielaBio, Zura Bio; Joshua T. Cohen has consulted or received grant support from the following life sciences companies and groups: Abbvie, Amgen, Analysis Group, Astra Zeneca, Biogen, Brystol Myers Squibb, Eli Lily, Giliead, IQvia, Johnson and Johnson, Lundbeck, Merck, Moderna, National Pharmaceutical Council, No Patient Left Behind, Novartis, Partnership for Health Analytic Research, Patient Square Capital, Pfizer, Pharmerit, PhRMA Foundation, Precision Health Economics, RA Capital, Regeneron, Sage, Sanofi, Sarepta, Vir Bio; Elliott Crummer and Pei-Jung Lin have no relevant competing interests to declare.
This study (STUDY00003692) has been deemed not to be human subjects research by the Tufts Health Sciences Institutional Review Board.
Data Availability
Data are available through the All of Us Research Program.
References
- [1].2015 National Content Test: Race and Ethnicity Analysis Report, United States Census Bureau https://www2.census.gov/programs-surveys/decennial/2020/program-management/final-analysis-reports/2015nct-race-ethnicity-analysis.pdf. Accessed 1 February 2024
- [2].Ahmed F, Moseley I, Ragi SD, Ouellette S and Rao B (2023) Vitiligo in underrepresented communities: An All of Us database analysis. Journal of the American Academy of Dermatology 88(4):945–948. 10.1016/j.jaad.2022.11.027 [DOI] [PubMed] [Google Scholar]
- [3].All of Us Research Program Operational Protocol, All of Us (2021) https://allofus.nih.gov/sites/default/files/All%20of%20Us%20Research%20Program%20Operational%20Protocol%202022.pdf. Accessed 1 Feburary 2024
- [4].Bergqvist C and Ezzedine K (2020) Vitiligo: A Review. Dermatology 236(6):571–592. 10.1159/000506103 [DOI] [PubMed] [Google Scholar]
- [5].Bhandarkar SS and Kundu RV (2012) Quality-of-Life Issues in Vitiligo. Dermatologic Clinics 30(2):255–268. 10.1016/j.det.2011.11.013 [DOI] [PubMed] [Google Scholar]
- [6].Chen T, Grau C, Suprun M, Silverberg NB (2016) Vitiligo patients experience barriers in accessing care. Cutis 98(6):385–388. [PubMed] [Google Scholar]
- [7].Ezzedine K, Eleftheriadou V, Jones H, Bibeau K, Kuo FI, Sturm D and Pandya AG (2021) Psychosocial Effects of Vitiligo: A Systematic Literature Review. Am J Clin Dermatol 22(6):757–774. 10.1007/s40257-021-00631-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].FDA approves topical treatment addressing repigmentation in vitiligo in patients aged 12 and older, U.S. Food & Drug Administration (2022) https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-topical-treatment-addressing-repigmentation-vitiligo-patients-aged-12-and-older. Accessed 1 February 2024
- [9].Finneran P, Toribio MP, Natarajan P and Honigberg MC (2023) Delays in Accessing Healthcare Across the Gender Spectrum in the All of Us Research Program. Journal of General Internal Medicine 10.1007/s11606-023-08548-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Gandhi K, Ezzedine K, Anastassopoulos KP, Patel R, Sikirica V, Daniel SR, Napatalung L, Yamaguchi Y, Baik R and Pandya AG (2022) Prevalence of Vitiligo Among Adults in the United States. JAMA Dermatology 158(1):43–50. 10.1001/jamadermatol.2021.4724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Interactive Summary Health Statistics for Adults, Centers for Disease Control and Prevention (2022) https://wwwn.cdc.gov/NHISDataQueryTool/SHS_adult/index.html. Accessed 1 February 2024
- [12].Key Data on Health and Health Care by Race and Ethnicity, KFF (2023) https://www.kff.org/racial-equity-and-health-policy/report/key-data-on-health-and-health-care-by-race-and-ethnicity/. Accessed 1 February 2024
- [13].Kussainova A, Kassym L, Akhmetova A, Glushkova N, Sabirov U, Adilgozhina S, Tuleutayeva R and Semenova Y (2020) Vitiligo and anxiety: A systematic review and meta-analysis. PLoS One 15(11):e0241445. 10.1371/journal.pone.0241445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lee JH, Ju HJ, Seo JM, Almurayshid A, Kim GM, Ezzedine K and Bae JM (2023) Comorbidities in Patients with Vitiligo: A Systematic Review and Meta-Analysis. J Invest Dermatol 143(5):777–789.e6. 10.1016/j.jid.2022.10.021 [DOI] [PubMed] [Google Scholar]
- [15].Mastacouris N, Strunk A, Garg A. Incidence and Prevalence of Diagnosed Vitiligo According to Race and Ethinicity, Age, and Sex in the US. JAMA Dermatol. 2023;159(9):986–990. 10.1001/jamadermatol.2023.2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Picardo M, Huggins RH, Jones H, Marino R, Ogunsola M and Seneschal J (2022) The humanistic burden of vitiligo: a systematic literature review of quality-of-life outcomes. J Eur Acad Dermatol Venereol 36(9):1507–1523. 10.1111/jdv.18129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Richard MA, Saint Aroman M, Baissac C, Merhand S, Aubert R, Audouze A, Legrand C, Beausillon C, Carre M, Raynal H, Bergqvist C, Taieb C and Cribier B (2023) Burden of visible [face and hands] skin diseases: Results from a large international survey. Ann Dermatol Venereol 150(2):95–100. 10.1016/j.annder.2022.11.008 [DOI] [PubMed] [Google Scholar]
- [18].Rosmarin D, Soliman AM and Li C (2023) Real-World Treatment Patterns in Patients with Vitiligo in the United States. Dermatol Ther (Heidelb) 13(9):2079–2091. 10.1007/s13555-023-00983-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available through the All of Us Research Program.


