Abstract
The occurrence of Central Giant Cell Granuloma (CGCG) represents a rare yet clinically significant entity within the realm of maxillofacial pathology. This article presents a compelling case of CGCG in a 17-year-old female, shedding light on the diagnostic and therapeutic challenges encountered in managing this condition. Given the relative infrequency of CGCG in this demographic, the case not only contributes to the clinical understanding of CGCG but also underscores the importance of tailored, patient-specific management strategies. Through this presentation, we aim to elucidate the intricacies of CGCG manifestation, diagnosis, and treatment while highlighting the nuanced considerations essential in addressing this pathology in adolescent patients.
Key Words: Central Giant Cell Granuloma, Diagnosis, Pathology, Treatmentc
INTRODUCTION
Central giant cell granuloma (CGCG) is a rare, benign lesion of the jaw bones characterized by the presence of multinucleated giant cells within a fibrous stroma. Although it is typically considered a benign entity, CGCG can cause significant morbidity due to its potential for aggressive behavior and destruction of surrounding tissues 1.
CGCG is most commonly found in the mandible, and it typically presents as a painless swelling or bony overgrowth. The lesion may be discovered incidentally on radiologic imaging or may be symptomatic, causing facial asymmetry, pain, or difficulty chewing. The etiology of CGCG remains uncertain, with several theories proposed. It has been suggested that CGCG may arise from an aberrant immune response or be triggered by local trauma. However, the exact mechanism underlying its development and progression is still not fully understood 2.
Diagnosis of CGCG requires a combination of clinical examination, imaging studies, and histopathologic analysis. Differential diagnoses include other benign and malignant lesions, such as odontogenic tumors, giant cell tumors, and metastatic lesions. Treatment options for CGCG range from conservative approaches, such as curettage or intralesional corticosteroid injections, to more radical interventions like surgical resection or embolization 3.
Surgical excision with curettage is the most commonly utilized treatment modality for CGCG. This approach involves removal of the lesion and surrounding bone, followed by thorough curettage to ensure complete removal of all affected tissue. While surgical excision is effective in the majority of cases, it can be associated with significant morbidity, including facial disfigurement, nerve damage, and impaired function 4, 5.
In recent years, alternative approaches for the management of CGCG have been explored, including non-surgical interventions such as intralesional injections of corticosteroids or calcitonin. These treatments are typically reserved for smaller lesions or cases where surgery is not feasible due to patient comorbidities or location of the lesion 6.
Other novel treatments for CGCG include radiation therapy, embolization, and pharmacotherapy. Radiation therapy has been shown to be effective in controlling the growth of aggressive or recurrent lesions, although long-term effects on dental development and function require further study. Embolization, which involves blocking the blood supply to the lesion, may be an effective approach in select cases, although there is limited data on its use in CGCG. Pharmacotherapy, including the use of bisphosphonates and denosumab, has shown promise in the treatment of CGCG, but further studies are needed to determine safety and efficacy 7, 8.
Despite its relative rarity, CGCG is an important lesion for clinicians to be aware of given its potential for aggressive growth and recurrence. Improved understanding of the pathogenesis and clinical behavior of CGCG will facilitate better management of this challenging entity, and ultimately lead to improved patient outcomes.
We aim to provide a comprehensive overview of CGCG, including its clinical presentation, diagnostic workup, and therapeutic options, to increase awareness and promote optimal management strategies for this rare lesion.
CASE PRESENTATION
A 17-year-old female patient presented with the main complaint of swelling on the left side of her face and the presence of purulent discharge in her mouth to the Department of Maxillofacial Surgery, Mashhad Dental School, Mashhad, Iran in July 2021 (Fig. 1). The swelling, located in the left mandibular angle (having started six months prior), was reported by the patient to have initially been small, gradually increasing in size, causing no functional impairment. The patient denied any associated pain or fever. The swelling was accompanied by purulent mouth discharge (without extraoral fistula). There was no history of trauma, hospitalization, surgical operation, radiotherapy, bisphosphonate use, specific drug use (excluding antidepressants and antihistamines), alcohol or smoking consumption, or tooth extraction. Family history did not indicate any genetic or hereditary diseases. Tenderness was present on palpation, but there were no extraoral fistulas, proptosis, nasal obstruction, or lymphadenopathy. Firm consistency of the lesion was noted, with no signs of inflammation (absence of erythema, warmth, or spontaneous pain). Moderate expansion was visible intraorally in the buccal and lingual aspects, with no buccal or lingual displacement and no associated facial or inferior alveolar nerve anesthesia.
Fig. 1.
Clinical & panoramic view
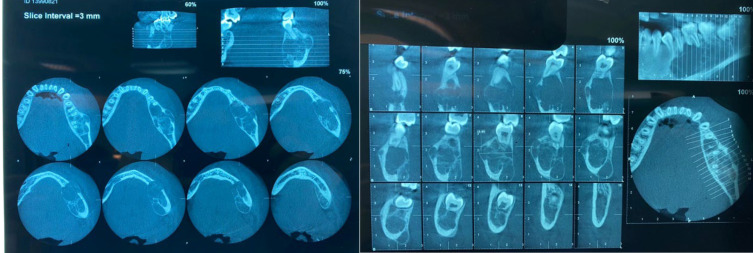
The patient’s oral hygiene was fair, and her lower teeth, despite decay, were vital and non-mobile. Displacement of teeth 5, 6, and 7 was observed, along with an intraoral fistula in the region of tooth 7 with purulent drainage. Salivary duct milking was normal. A panoramic X-ray revealed a defined, multilocular, radiolucent lesion extending from the left mandibular first premolar to the distal of the left mandibular second molar, with septations appearing as intermediate (Fig. 1). Root resorption of the left mandibular first molar and inferior alveolar nerve deviation were evident. Expansion of the lesion was observed in the lower border of the mandible. Additionally, a cone-beam computed tomography (CBCT) scan showed buccal and lingual expansion behind the left mandibular angle, with a multilocular appearance (Fig. 2) 9. Aspiration yielded a yellowish fluid, and laboratory tests indicated a Ca: 8 mg/dl level. Considering the location of the lesion, the radiographic report, and the aspirate appearance, the differential diagnoses of 1. CGCG, 2. Aneurysmal bone cyst (ABC), and 3. Aneurysmal fibrous histiocytoma (AF) were considered. An excisional biopsy was performed (Fig. 3), and the histopathological examination revealed multiple fragments of brownish tissue ranging from soft to bony consistency, measuring 2 × 0.7 × 0.5 cm in total. Microscopic evaluation showed proliferative patterns with the presence of multinucleated giant cells amid a background of mesenchymal cell proliferation and extravasated red blood cells, leading to the diagnosis of mandibular mass compatible with giant cell granuloma 10.
Fig. 2.
CBCT view of pathologic lesion before treatment
Fig. 3.
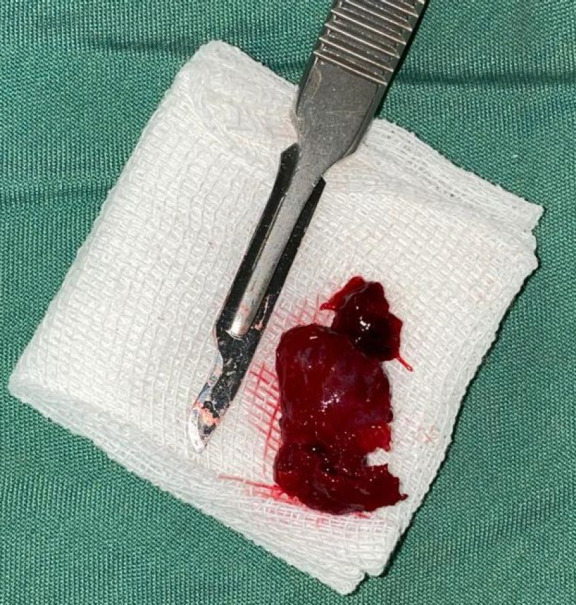
Macroscopic view of excisional biopsy
Treatment options considered for the patient’s CGCG diagnosis included 1. Intralesional steroid injection (triamcinolone; 6 injections weekly for 6 weeks 11) and 2. Resection with clear histological margins. Due to the lack of improvement after 6 weeks of corticosteroid therapy, surgical excision with a clear bone margin was decided upon. The patient was followed up for one year postoperatively, during which significant soft and hard tissue healing was observed in the affected area (Fig. 4).
Fig. 4.
1 year after of treatment, the patient shows remission of the periapical image
Ethics
All procedures conducted in this study involving human participants adhered to the ethical standards established by the Research Committee of Zahedan Faculty of Dentistry, as well as the principles outlined in the 1964 Helsinki Declaration and its subsequent amendments or comparable ethical guidelines. Informed consent was obtained from the patient’s family prior to participation in the study.
DISCUSSION
In this case presentation, we have described the clinical features, diagnostic challenges, and treatment strategies for a CGCG in a 17-year-old female patient. CGCG is a rare benign lesion that primarily affects the jaws, and it typically presents as a slow-growing mass. This case highlights the importance of early recognition, proper diagnosis, and appropriate management of CGCG in young individuals 12.
The clinical presentation of our patient aligns with the typical characteristics of CGCG. She presented with a painless swelling in the mandible, which gradually increased in size over several months. Radiographic examination revealed a well-defined radiolucent lesion with internal septations and cortical thinning. These findings were consistent with the imaging features commonly associated with CGCG. However, it is important to note that the radiographic appearance of CGCG can vary, and other lesions such as odontogenic tumors and giant cell tumors should be considered in the differential diagnosis 2, 12.
Histopathological analysis confirmed the diagnosis of CGCG in our patient. The presence of multinucleated giant cells within a fibrous stroma was consistent with the characteristic histologic findings of CGCG. Immunohistochemical staining may also be performed to rule out other differential diagnoses, particularly giant cell tumor, which shares some morphological similarities with CGCG 3, 13.
The management of CGCG in our patient involved a multidisciplinary approach. Considering the size and aggressiveness of the lesion, as well as the patient’s age and overall health status, surgical excision with curettage was chosen as the treatment modality. The surgery was performed successfully, and the patient experienced satisfactory healing without any significant complications. Regular follow-up is essential to monitor for recurrence or any potential complications 3, 4, 14.
Recurrence is one of the most challenging aspects of managing CGCG. The reported recurrence rates vary widely in the literature, ranging from 10% to 45%. Factors associated with an increased risk of recurrence include younger age, aggressive behavior of the lesion, incomplete removal, and inadequate curettage. Therefore, meticulous surgical technique, thorough curettage, and close long-term follow-up are crucial to minimize the risk of recurrence 14, 15.
Alternative treatment options for CGCG, such as intralesional corticosteroid injections or calcitonin therapy, have been reported in the literature. These non-surgical interventions are typically reserved for smaller lesions or cases where surgery is contraindicated. However, their efficacy and long-term outcomes need further investigation 6, 14, 16.
CONCLUSION
This case presentation highlights the importance of recognizing and properly managing CGCG in young individuals. Timely diagnosis, careful surgical planning, and close long-term follow-up are essential for achieving favorable outcomes and minimizing the risk of recurrence. Further research is needed to optimize treatment strategies and explore alternative therapeutic approaches for CGCG, with the goal of improving patient care and outcomes.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interests.
References
- 1.Nilesh K, Vande A, Tewary S. Giant cell lesion and central giant cell granuloma of jaw: a brief review. AABS. 2017;4:R22–9. [Google Scholar]
- 2.Hoarau E, Quilhot P, Baaroun V, et al. Oral giant cell tumor or giant cell granuloma: How to know? Heliyon. 2023 Mar;9(3):e14087. doi: 10.1016/j.heliyon.2023.e14087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeyaraj P. Management of Central Giant Cell Granulomas of the Jaws: An Unusual Case Report with Critical Appraisal of Existing Literature. Ann Maxillofac Surg. 2019 Jan-Jun;9(1):37–47. doi: 10.4103/ams.ams_232_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malaquias P, Igreja F, França R, et al. Central giant cell granuloma-surgical treatment and reconstruction: case report. Int J Oral Maxillofac Surg. 2019;48:98. [Google Scholar]
- 5.Piotrowska-Seweryn A, Oleś K, Grajek M, Chekan M, Maciejewski A, Lange D. Surgical treatment and reconstruction of central giant cell granuloma (CGCG) of the mandible of the aggressive type–case report and literature review. Pol Prz Otolaryngol. 2019;8(4):30–7. [Google Scholar]
- 6.Mukdad M, Barut O, Sjöström M. Intralesional corticosteroid injections as first option for management of giant cell lesion of the lower jaw in a 56-year-old patient: A case report and brief literature review. Oral Maxillofac Surg Cases. 2022;8(4):100283. [Google Scholar]
- 7.Camarini C, de Souza Tolentino E. Non-surgical treatment as an alternative for the management of central giant cell granuloma: a systematic review. Clin Oral Investig. 2022 Feb;26(2):2111–32. doi: 10.1007/s00784-021-04193-z. [DOI] [PubMed] [Google Scholar]
- 8.Yanik S, Aras MH. Management of central giant cell granuloma of mandible using intralesional corticosteroids: case report and review of literature. J Oral Maxillofac Surg. 2013;71(4):721–2. doi: 10.1016/j.joms.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Tahmasbi-Arashlow M, Patel PB, Nair MK, Liang H, Cheng YL. Cone-beam computed tomographic imaging of central giant cell granuloma: A comprehensive review. Imaging Sci Dent. 2022 Jun;52(2):123–31. doi: 10.5624/isd.20220130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramesh V. “Central giant cell granuloma” - An update. J Oral Maxillofac Pathol. 2020;24(3):413–5. doi: 10.4103/jomfp.jomfp_487_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdo EN, Alves LCF, Rodrigues AS, Mesquita RA, Gomez RS. Treatment of a central giant cell granuloma with intralesional corticosteroid. Br J Oral Maxillofac Surg. 2005;43(1):74–6. doi: 10.1016/j.bjoms.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 12.Kudva A, Cariappa KM, Dhara V, Solomon M. Central giant cell granuloma: An uncommon presentation. Oral Maxillofac Surg Cases. 2018;4(4):135–40. [Google Scholar]
- 13.Alsufyani NA, Aldosary RM, Alrasheed RS, Alsaif RF. A systematic review of the clinical and radiographic features of hybrid central giant cell granuloma lesions of the jaws. Acta Odontol Scand. 2021;79(2):124–31. doi: 10.1080/00016357.2020.1797160. [DOI] [PubMed] [Google Scholar]
- 14.Kumar N, Dadhich A, Patil R. Management of recurrent central giant cell granuloma of mandible using intralesional corticosteroid with long-term follow-up. BMJ Case Rep. 2020;13:9. doi: 10.1136/bcr-2020-237200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yadav S, Singh A, Kumar P, Tyagi S. Recurrent case of central giant cell granuloma with multiple soft tissue involvement. Natl J Maxillofac Surg. 2014 Jan;5(1):60–6. doi: 10.4103/0975-5950.140181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rachmiel A, Emodi O, Sabo E, Aizenbud D, Peled M. Combined treatment of aggressive central giant cell granuloma in the lower jaw. J Craniomaxillofac Surg. 2012 Apr;40(3):292–7. doi: 10.1016/j.jcms.2011.04.002. [DOI] [PubMed] [Google Scholar]