Abstract
Horse riding is a popular yet dangerous sport, often resulting in facial traumas due to unpredictable horse reactions or falls. This retrospective study examines 20 patients. The aim of the study is to analyze maxillofacial traumas of equine origin and discuss prevention strategies. Conducted from 2004 to 2021 at our university hospital’s emergency department in France, inclusion criteria encompassed patients with maxillofacial trauma admitted to the emergency department and referred to ENT and/or dentistry post-horse-related accidents. Patients were identified from the Health Data warehouse. While 35 medical files were accessed, 15 did not meet inclusion criteria. Analysis of patient parameters, including age, sex, injury date, circumstances, injury type, management, helmet usage, operative interventions, and potential sequelae, revealed a predominantly female population (16 versus 4) under 48 years old. Traumas were most prevalent in summer (80%) and frequently involved riders on foot (60%). Seventy percent of patients sustained at least 1 facial fracture, with helmet use documented in only 1 case. In conclusion, horse riding can lead to various traumas, often necessitating surgical intervention. Preventive measures such as protective helmets, even for nonmounted riders, are crucial as the literature highlights many injuries occurring due to helmet omission.
Key Words: Facial trauma, horse, horse riding
Horse riding is the third most practiced sport in France, with 6 74 176 license holders in 2022, and this number has been increasing since 2017. Eighty-five percent of the members are women, making it the leading female sport in France. It is predominantly practiced by young people, with more than 60% of the riding population under 18 years old.1 About 5.34% of the French members are in Brittany.
Horse riding is risky, surpassing motorcycle and car racing in terms of risk.2 For instance, a study involving 162 patients found 12.4% of maxillofacial injuries related to equine sports, ranking just behind Gaelic football, soccer, and rugby.3 An adult horse weighs on average more than 500 kg and can reach galloping speeds of 65 km/H.4 The force of a hoof strike can reach 10 000 Newton.5
Horses, despite being mostly trained and desensitized to various situations, remain unpredictable animals, occasionally reacting suddenly and leading to accidents in diverse ways.
Accidents can occur while the rider is mounted on horseback: falls resulting in trauma against the ground or objects, being crushed or trampled by the horse after a fall, being dragged by the horse while caught in the harness, receiving a head-butt from the horse, or colliding with objects such as branches. In addition, accidents can happen when the rider is on foot around the horse, while walking the horse, or during horse care, including being kicked by hooves, headbutted, or bitten.
The rider’s face is particularly vulnerable in accidents, often necessitating multidisciplinary hospital management and potentially leading to severe consequences, including the death of the patient.
Patients from across the region seek treatment at our University Hospital, the largest medical center in North Finistere. Due to the ENT Department’s expertise in managing maxillofacial traumas, most patients with such injuries present here. This study focused on the population of Finistere, covering an area of 6000 km2 and home to over 9 00 000 residents.
The aim of this study is to retrospectively and descriptively analyze various maxillofacial traumas of equine origin and their management at our University Hospital between 2004 and 2021. In addition, the study seeks to explore potential preventive measures that could mitigate such incidents. Another objective is to compare the findings of our study with existing data from the literature.
MATERIALS AND METHODS
After contacting the Medical Information Department, the research focused on patients’ files from 2004 to 2021, meeting specific inclusion criteria: individuals who experienced maxillofacial trauma admitted to our University Hospital’s emergency department and subsequently to ENT and/or dentistry following horse-related accidents. Searches were conducted in the Health Data warehouse of our University Hospital using keywords such as “horse,” “hoof,” “riding,” and “pony,” yielding 39 million references, including reports, observations, and nurse transmissions. Access to the Ehop software was granted, enabling direct retrieval of reports and letters about each patient, with files anonymized. The study period spanned from 2004 to 2021 to encompass over 15 years of consultations, providing a more comprehensive representation of craniofacial trauma. Given the rarity of maxillofacial traumas and their random occurrence, this timeframe was deemed suitable.
Data extracted from patient files included age, sex, injury date, circumstances, injury type, management, helmet usage, operative follow-up, and potential sequelae. Specifically, data focused on mucocutaneous and osseous facial trauma involving teeth, mandible, maxilla, nasal, frontal, orbits, and zygomatic bones. Subsequently, collected data were compared with other articles sourced from PubMed and Web of Science.
RESULTS
Selection of Files
Thirty-five medical files were retrieved from the database. Upon initial review of these 35 files, 20 met the inclusion criteria. Among the 15 files that were not included:
Seven documented equine injuries not involving the maxillofacial area: 5 were isolated cranial traumas (without maxillofacial involvement), 1 involved a knee trauma, and 1 pertained to a cervical spine trauma.
Five cases involved patients with a history of equine maxillofacial trauma.
One file did not involve any trauma.
One documented a cow-related injury.
One file contained information about a trauma that occurred outside the study period.
Sociodemographic Data
Of the 20 patients included in our study, 16 were women and 4 were men, accounting for 80% of the total participants (see Table 1 in the supplementary material, Supplemental Digital Content 1, http://links.lww.com/SCS/G16).
The average age of the selected patients was 24.6 years, the median 21 years, with a range of 6 to 48 years.
Trauma-Related Data
When analyzing the dates of the injuries, we observed a higher incidence during the summer period. Specifically, 80% of the injuries occurred during the week, while 20% occurred during the weekend. Of the 20 patients, 8 had accidents while riding, whereas 12 had accidents while walking. Hence, 60% of the maxillofacial injuries involved riders on foot.
Among the riders who were on horseback at the time of their trauma:
Six fell from their horses.
One fell and was subsequently run over.
One fell and was then struck by a hoof.
Among riders who were on foot:
Eleven were kicked.
One was bitten.
Accidents involving contact with the horse at the time of the trauma (such as hoof strikes, crushing, and biting) were predominant, accounting for 70% of maxillofacial traumas.
Of the 20 patients included in the study, 14 exhibited at least 1 facial fracture, constituting 70% of the total. Specifically, this encompasses 9 out of the 11 patients who were kicked while walking (82%), and 5 out of the 8 patients who fell (62.5%). The remaining 6 patients solely sustained soft tissue injuries (refer to Fig. 1).
FIGURE 1.
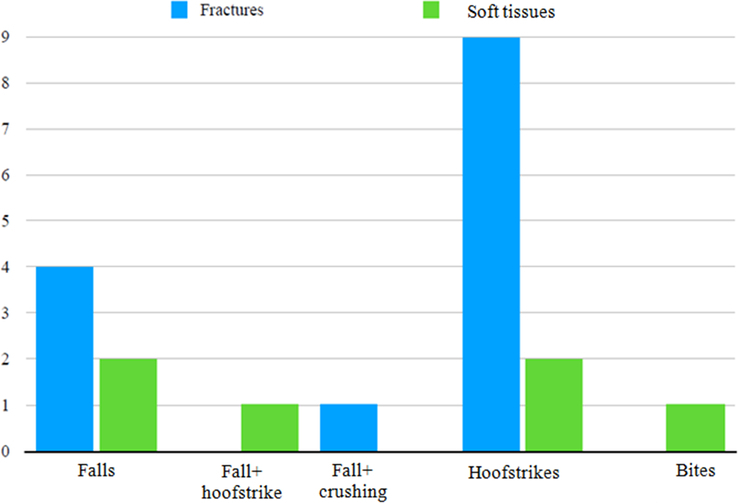
Repartition of lesion types based on trauma type.
In total, 44 injuries were documented across all patients, with fractures representing 63.7% of the lesions (n=28). As depicted in Table 2 of the Supplementary Material, Supplemental Digital Content 1, http://links.lww.com/SCS/G16, the most common injuries were soft tissue injuries (n=12) and mandible fractures (n=11). In all cases, hoof strikes were identified as the primary cause of fractures.
Out of the 14 patients with fractures, 8 required fracture reduction:
Five necessitated surgical reduction and osteosynthesis due to displacement fractures: 3 for isolated mandible fractures and 2 for mandible fractures associated with Lefort fractures.
Two required simple surgical reduction without osteosynthesis for zygomatic fractures.
One underwent reduction through an external maneuver for a nasal bone fracture with displacement.
Mandible fractures with displacements and Lefort fractures were fractures that required osteosynthesis. Mandible fractures concerned a subcondylar fracture with displacement, 2 parasymphysial fractures and 1 angular fracture. Three files mentioned a treatment by intermaxillary blocking with arches. It was for mandible fractures. For 2 condylar fractures, physiotherapy was used to rehabilitate the joint.
Seven out of the 20 patients required sutures only. In all cases, medication (antibiotics and analgesics) and hygiene advice (diet and oral hygiene) were provided.
Four patients suffered dental injuries during their trauma, including:
Luxation of upper teeth, with no information on the treatment carried out.
Luxation of tooth 32, which was urgently avulsed.
Fracture of tooth 21, reconstructed in an emergency.
Complex dental trauma necessitates repositioning and contention of several teeth.
Of the 11 patients who were kicked while walking, 10 (91%) required surgical intervention, either fracture reduction or sutures. Only 1 patient in this group required monitoring, although intervention of the fractured tooth was still necessary.
Conversely, among patients who fell without horse contact, half of the injuries did not necessitate surgery (Fig. 2).
FIGURE 2.
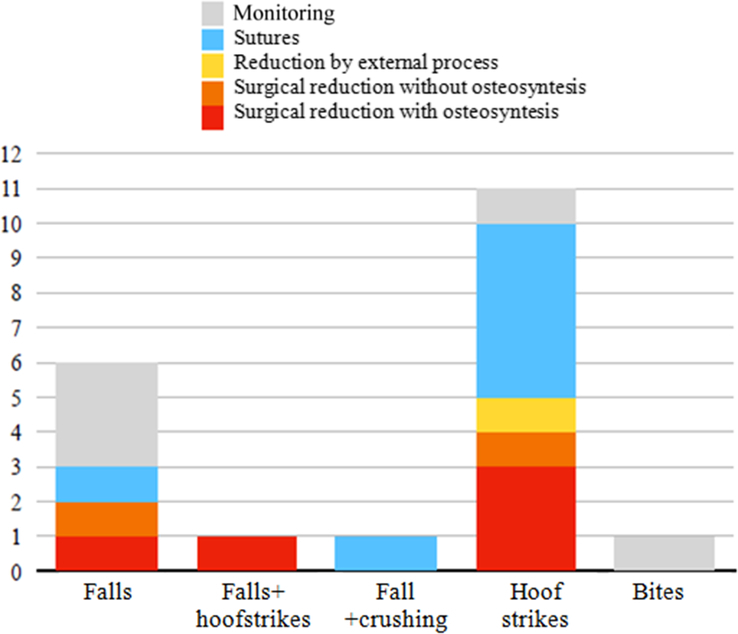
Treatment repartition based on trauma type.
Three out of the 20 patients, 3 (15%) had other associated lesions (2 on the cranium and 1 at the hip).
The available documents in the patient files did not provide sufficient information regarding the long-term effects of these traumas on most patients.
Only 1 case out of the 20 mentioned that the patient was wearing a protective helmet at the time of the injury.
Our study’s results were compared with those of other articles in the literature. Articles were selected from PubMed and Web of Science using keywords such as “Trauma and horse,” “Trauma and riding,” “Trauma and equestrian,” and “Trauma and hoof.” Off-topic or duplicate articles were excluded. After reading the abstracts, the selection of articles was refined. Articles specifically focusing on jockeys, western riding, and veterinarians were excluded, as were those about veterinary medicine and sports other than horse riding. The remaining articles after this selection were read in full (n=99). Studies with data suitable for comparison with our study’s data were included (n=57) (Fig. 3).
FIGURE 3.
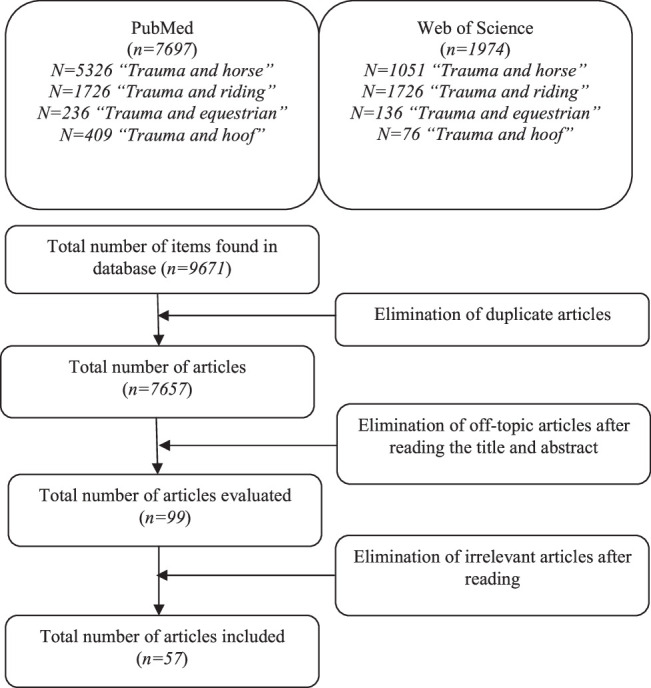
Flow chart for the articles selection.
In our study, there was a higher proportion of women than men (80%). Many studies on equestrian injuries also report a majority of female participants. This predominance of women in equestrian injuries may be attributed to the fact that horse riding is predominantly practiced by females.
The patient sample in our study was comprised predominantly of young individuals (mean age 24 years). Other studies on equestrian injuries generally report a higher average age and a wider age range (Fig. 4).5
FIGURE 4.
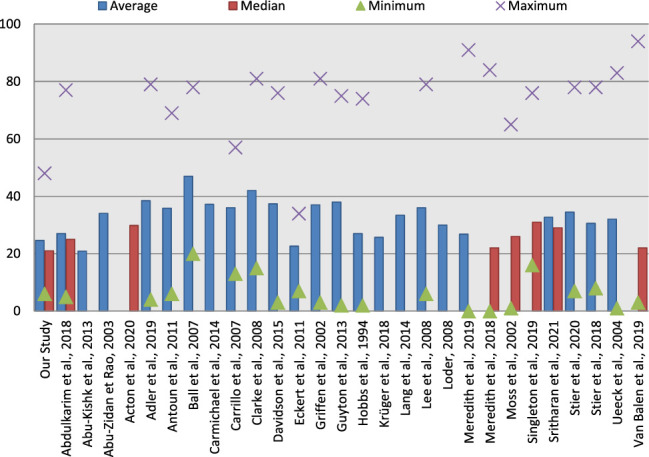
Age repartition in other studies.5
It can be observed that studies on equestrian injuries generally indicate a significant majority of accidents associated with falls ranging between 44.6% and 83% (Figs. 5 6 and 6), with a minority attributed to hoof strikes, ranging between 1.7% and 29% (Figs. 5 and 7). However, studies like ours, which specifically focus on maxillofacial trauma, report a lower proportion of falls, ranging between 17.8% and 46%, and a much higher percentage of hoof strikes, ranging between 35% and 73%. (Fig. 5).
FIGURE 5.
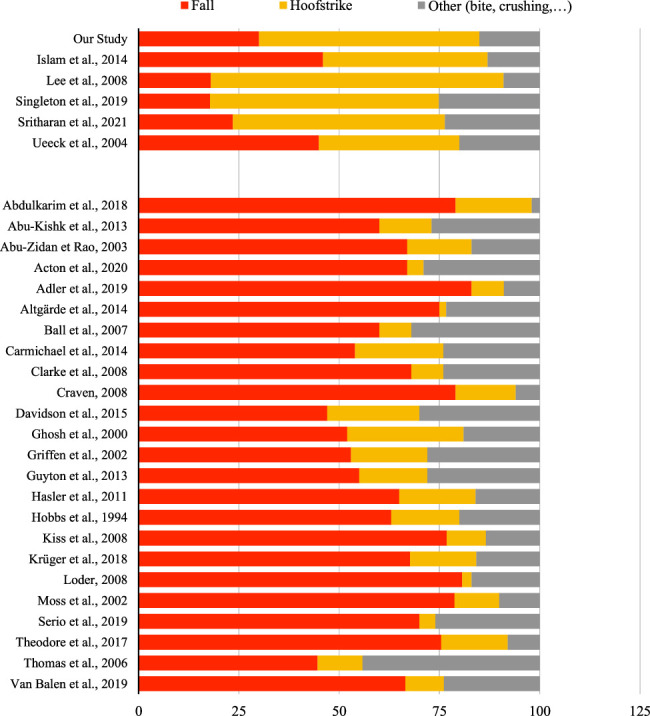
Comparison between trauma causes’ percentages compared with other studies (on the top studies about equestrian maxillo-facial traumas and on the bottom equestrian traumas in general).6
FIGURE 6.
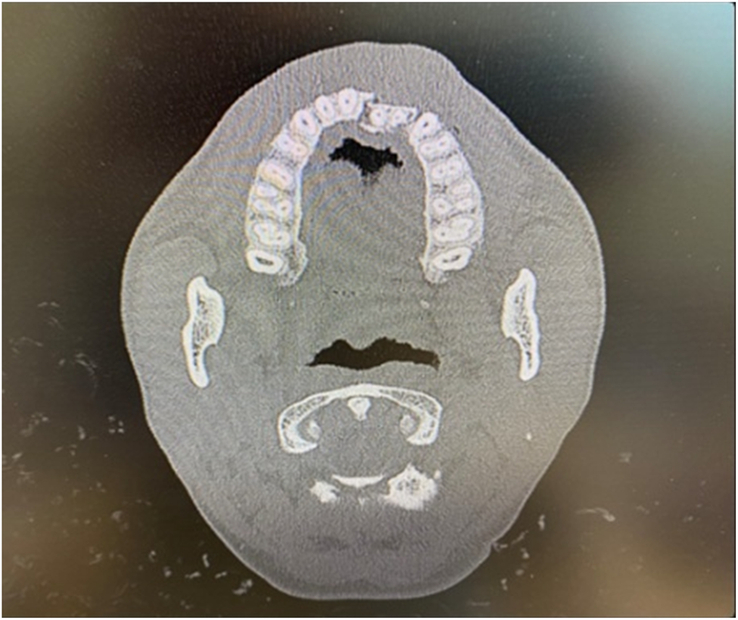
Example of a dentoalveolar trauma caused by a horse.
FIGURE 7.

Median mandible fracture caused by a pony hoof kick.
DISCUSSION
This study does not provide information on the effectiveness of the helmet in this type of trauma because of the lack of data about helmet use.
In France, wearing protective helmets is not obligatory for riders except during official competitions, where it is mandatory for mounted participants. Many riding schools make it mandatory for riders to wear a helmet. While many riding establishments enforce helmet requirements, many riders, whether mounted or near horses, opt not to wear protective gear.7,8
Especially when pedestrians are near horses, helmet usage is not prevalent, and there are no specific regulations mandating helmet use in this context. Nevertheless, numerous studies have demonstrated that injuries resulting from hoof strikes can be as severe, if not more so, than those resulting from falls. In one study, 85% of riders who fell from a horse wore a helmet, while those who were kicked or bitten wore the helmet in 18.7% of cases.9 This underscores the widespread lack of adherence to helmet-wearing practices around horses.
It is essential to note that these studies typically encompass riders who sought emergency medical attention following an injury. One study reported that riders wearing helmets were 50% less likely to sustain injuries.10 Another study highlighted a higher rate of hospital admissions among unhelmeted patients demonstrating that wearing a helmet decreases the severity of head injuries.11 Consequently, individuals without helmets are more prone to hospitalization, potentially explaining the lower percentage of helmet wearers among those presenting to emergency departments. A large proportion of accidents involving helmeted riders may not necessitate hospitalization, as the protective gear effectively fulfills its intended function.
However, it is worth noting that the current design of helmets utilized in classic riding lacks facial protection. It would be interesting to design helmets for classic riding that offer facial protection, as in other sports.12,13
Polo players have protective glasses in addition to helmets or face grids to mitigate facial traumas, particularly those resulting from high-velocity impacts with the ball. While face grids offer protection, they can compromise visibility, leading many polo players to opt for protective glasses instead.
Another solution to prevent dental traumas is using mouthguards. In the literature, it appears that riders are familiar with mouthguards, but they do not systematically wear them.14 Moreover, Caglar and Sandalli15 concluded in their study that the prevalence of dental and orofacial trauma in pony and horseback riding children was found to be rather low, and more studies should be carried out to detect the prevalence for comment usage of a mouthguard. Hence, it may be beneficial to implement preventive measures to encourage riders to use mouthguards, akin to practices observed in sports such as rugby or boxing.
We did not have information on the riding level of the riders who suffered trauma. Studies have shown that more than 70% of injuries occur among more experienced riders, including those at advanced or professional levels.7–16 The experience of the rider does not appear to be a protective factor against trauma. For instance, 1 study revealed that over 83% of patients who sustained hoof blows had less than 6 months of riding experience.17 Conversely, another study found that 37% of trauma patients had more than 5 years of riding experience.18.
The study by Stier et al7 showed that among trauma patients, helmets were worn by 67% of beginner riders but only by 44% of riders with a more advanced level and 33% of professional riders. Riders with a higher level therefore appear to protect themselves less than beginners. This suggests that prevention campaigns should not solely focus on beginners but should also target riders with intermediate and advanced proficiency levels.
In this study, concerning fractures, the incidence of mandible fractures is notably prominent, consistent with findings from previous research.19 As noted earlier, the proportion of women is higher in our study than in the general population, reflecting the predominantly female demographic involved in riding activities.20
The limitations of this study are inherent to its retrospective design, including the absence of long-term patient follow-up and a relatively small sample size. The strength of this study is that it covers 18 years.
The sample size of our study could explain why the results are slightly different than results in the literature.
CONCLUSIONS AND PERSPECTIVES
The findings of this study, in line with those of previous research on the same topic, unequivocally demonstrate the gravity of maxillofacial trauma resulting from equestrian activities. The severity of the clinical pictures involving facial fractures and associated complications, particularly among younger individuals, underscores the imperative for the implementation of effective protective measures. In particular, measures to safeguard facial bone structures and alveolar-dental regions are warranted. Mere helmet use may not suffice, as it primarily addresses cranial protection.
Prevention campaigns should be instituted to advocate for helmet usage in all equine-related contexts, whether riders are on horseback or foot. Such campaigns should target not only beginners but also more experienced riders.
Supplementary Material
ACKNOWLEDGMENTS
The authors wish to thank the team of the medical information department for their invaluable statistical assistance.
Footnotes
The local ethical committee of Brest (the EREB) has approved this study (the corresponding document is joined).
This study respects our institutional consent form.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.jcraniofacialsurgery.com.
Contributor Information
Adeline Boiron, Email: a2.boiron@free.fr.
Camille Barazer, Email: camille.barazer@gmail.com.
Camille Clement, Email: camille.clement@chu-brest.fr.
Sonia Sahli Vivicorsi, Email: sonia.sahli-vivicorsi@chu-brest.fr.
Lorenn Bellamy, Email: lorenn.bellamy@chu-brest.fr.
Guy Le Toux, Email: guy.letoux@wanadoo.fr.
Sylvie Boisramé, Email: sylvie.boisrame@chu-brest.fr.
REFERENCES
- 1.https://www.ffe.com Fédération Française d’Équitation - FFE, 2023. Fédération Fr. D’équitation - FFE. Aaccessed February 18, 2023. Available at:
- 2. Baldini N, Kahn A, Willinger R, et al. Cranio-maxillo-facial injuries in professional jockeys: a systematic review. Sci sports 2022;37:255–266 [Google Scholar]
- 3. Murphy C, O'Connell JE, Kearns G, et al. Sports-related maxillofacial injuries. J Craniofac Surg 2015;26:2120–2123 [DOI] [PubMed] [Google Scholar]
- 4. Sorli JM. Equestrian injuries: a five year review of hospital admissions in British Columbia, Canada. Inj Prev 2000;6:59–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Exadaktylos AK, Eggli S, Inden P, et al. Hoof kick injuries in unmounted equestrians. Improving accident analysis and prevention by introducing an accident and emergency based relational database. Emerg Med J EMJ 2002;19:573–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barazer C. (2022). Les traumatismes maxillo-faciaux d’origine équestre [Mémoire de thèse d’exercice]. Université de Bretagne Occidentale.
- 7. Stier R, Ruter M, Zimmerer R, et al. Patterns of mandibular fractures related to interaction with horses. Arch Trauma Res 2018;7:64–67 [Google Scholar]
- 8. Ueeck BA, Dierks EJ, Homer LD, et al. Patterns of maxillofacial injuries related to interaction with horses. J Oral Maxillofac Surg 2004;62:693–696 [DOI] [PubMed] [Google Scholar]
- 9. Meredith L, Ekman R, Thomson R. Horse-related incidents and factors for predicting injuries to the head. BMJ Open Sport Exerc Med 2018;4:e000398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hasler RM, Gyssler L, Benneker L, et al. Protective and risk factors in amateur equestrians and description of injury patterns: a retrospective data analysis and a case - control survey. J Trauma Manag Outcomes 2011;5:4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bond GR, Christoph RA, Rodgers BM. Pediatric equestrian injuries: assessing the impact of helmet use. Pediatrics 1995;95:487–489 [PubMed] [Google Scholar]
- 12. Goiato MC, dos Santos DM, Moreno A, et al. , Use of facial protection to prevent reinjury during sports practice. J Craniofac Surg 2012;23:1201–1202 [DOI] [PubMed] [Google Scholar]
- 13. Procacci P, Ferrari F, Bettini G, et al. Soccer-related facial fractures: postoperative management with facial protective shields. J Craniofac Surg 2009;20:15–20 [DOI] [PubMed] [Google Scholar]
- 14. Gass M, Kühl S, Connert T, et al. Dental trauma in showjumping - a trinational study between Switzerland, France and Germany. Dent Traumatol 2016;32:174–179 [DOI] [PubMed] [Google Scholar]
- 15. Caglar E, Sandalli N. Dental and orofacial trauma in pony and horseback riding children. Dent Traumatol 2006;22:287–290 [DOI] [PubMed] [Google Scholar]
- 16. Stier R, Tavassol F, Dupke C, et al. Retrospective analysis of 15 years of horse-related maxillofacial fracture data at a major German trauma center. Eur J Trauma Emerg Surg 2020;48:2539–2546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eckert V, Lockemann U, Püschel K, et al. Equestrian injuries caused by horse kicks: first results of a prospective multicenter study. Clin J Sport Med 2011;21:353–355 [DOI] [PubMed] [Google Scholar]
- 18. Bixby-Hammett DM. Youth accidents with horses. Phys Sportsmed 1985;13:105–117 [DOI] [PubMed] [Google Scholar]
- 19. Boffano P, Roccia F, Zavattero E, et al. European maxillofacial trauma (EURMAT) project: a multicentre and prospective study. J Craniomaxillofac Surg 2015;43:62–70 [DOI] [PubMed] [Google Scholar]
- 20. Boffano P, Kommers SC, Karagozoglu KH, et al. Aetiology of maxillofacial fractures: a review of published studies during the last 30 years. Br J Oral Maxillofac Surg 2014;52:901–906 [DOI] [PubMed] [Google Scholar]


