Abstract
LPA (lysophosphatidic acid), a potent bioactive phospholipid, elicits diverse cellular responses through activation of the G-protein-coupled receptors LPA1–LPA4. LPA-mediated signalling is partially regulated by LPPs (lipid phosphate phosphatases; LPP-1, -2 and -3) that belong to the phosphatase superfamily. This study addresses the role of LPPs in regulating LPA-mediated cell signalling and IL-8 (interleukin-8) secretion in HBEpCs (human bronchial epithelial cells). Reverse transcription–PCR and Western blotting revealed the presence and expression of LPP-1–3 in HBEpCs. Exogenous [3H]oleoyl LPA was hydrolysed to [3H]-mono-oleoylglycerol. Infection of HBEpCs with an adenoviral construct of human LPP-1 for 48 h enhanced the dephosphorylation of exogenous LPA by 2–3-fold compared with vector controls. Furthermore, overexpression of LPP-1 partially attenuated LPA-induced increases in the intracellular Ca2+ concentration, phosphorylation of IκB (inhibitory κB) and translocation of NF-κB (nuclear factor-κB) to the nucleus, and almost completely prevented IL-8 secretion. Infection of cells with an adenoviral construct of the mouse LPP-1 (R217K) mutant partially attenuated LPA-induced IL-8 secretion without altering LPA-induced changes in intracellular Ca2+ concentration, phosphorylation of IκB, NF-κB activation or IL-8 gene expression. Our results identify LPP-1 as a key regulator of LPA signalling and IL-8 secretion in HBEpCs. Thus LPPs could represent potential targets in regulating leucocyte infiltration and airway inflammation.
Keywords: bioactive phospholipid, cytokine, inflammation, interleukin-8 secretion, lipid phosphate phosphatase-1 (LPP-1), lysophosphatidic acid (LPA)
Abbreviations: AP-1, activator protein-1; BAPTA/AM, bis-(o-aminophenoxy)ethane-N,N,N′,N′-tetra-acetic acid tetrakis(acetoxymethyl ester); BEBM, bronchial epithelial basal medium; [Ca2+]i, intracellular Ca2+ concentration; COPD, chronic obstructive pulmonary disease; EGF, epidermal growth factor; EGF-R, epidermal growth factor receptor; ERK, extracellular-signal-regulated kinase; HBEpC, human bronchial epithelial cell; IκB, inhibitory κB; IL-8, interleukin 8; LPA, lysophosphatidic acid; LPP, lipid phosphate phosphatase; hLPP, human LPP; mLPP, mouse LPP; MAPK, mitogen-activated protein kinase; MOG, mono-oleoylglycerol; MOI, multiplicity of infection; NF-κB, nuclear factor-κB; OMPT, D-sn-1-oleoyl-2-methylglyceryl-3-phosphothionate; PA, phosphatidic acid; PLD, phospholipase D; PPARγ, peroxisome proliferator-activated receptor γ; RT, reverse transcription; S1P, sphingosine 1-phosphate; SPP, sphingosine-1-phosphate phosphatase; TBST, Tris-buffered saline containing 0.1% Tween 20; TNF-α, tumour necrosis factor-α; wt, wild type
INTRODUCTION
The bioactive phospholipids LPA (lysophosphatidic acid) and S1P (sphingosine 1-phosphate) are present in biological fluids and tissues [1–3]. LPA induces a variety of signalling cascades, including release of intracellular Ca2+, and activation of phospholipases and the small G-protein Rho and MAPK (mitogen-activated protein kinase) family [ERK (extracellular-signal-regulated kinase), p38 and JNK (c-Jun N-terminal kinase)], via heterotrimeric G-protein-coupled LPA1, LPA2, LPA3 and LPA4 receptors [4–9]. More recently, PPARγ (peroxisome proliferator-activated receptor γ) was shown to be an intracellular receptor for LPA [10]. We detected the expression of LPA1, LPA2 and LPA3 receptors in HBEpCs (human bronchial epithelial cells) by RT-PCR (reverse transcription–PCR), Western blotting and immunocytochemistry [11].
Because of its role in airway repair and remodelling [12,13], LPA has been implicated in the pathology of asthma and COPD (chronic obstructive pulmonary disease). Recent studies have demonstrated that S1P or LPA induces IL-8 (interleukin-8) expression and secretion in HBEpCs [14,15], ovarian cancer cells [16,17], endothelial cells [18] and human colon DLD1 cells [19]. The chemoattractant IL-8 is a key component of the innate immune response [20], and plays a critical role in the migration of neutrophils across the alveolar–capillary membrane in lung inflammation and injury [21,22]. Secretion of IL-8 is regulated primarily at the level of gene transcription, and IL-8's promoter region contains binding sites for NF-κB (nuclear factor-κB) and AP-1 (activator protein-1) [23,24].
Although LPA-mediated cellular signalling has been studied extensively, pathways regulating LPA concentrations and LPA-dependent signalling are not sufficiently well understood. The LPPs (lipid phosphate phosphatase) family consists of five members, LPP-1, LPP-2, LPP-3, SPP-1 (S1P phosphatase-1) and SPP-2. The LPPs dephosphorylate several bioactive lipid phosphates, including LPA, PA (phosphatidic acid), S1P and ceramide 1-phosphate [25–28]. The active site of LPPs in three conserved domains lies either on the outside of the cell or on the luminal surface of the endoplasmic reticulum or Golgi [29–31]. The LPPs hydrolyse exogenous lipid phosphates and attenuate cell signalling [32,33]. In ovarian cancer cells, >90% of LPA degradation was mediated by LPP-like enzyme(s), while LPP-1 mRNA levels in ovarian cancer and lung cancer were decreased 2–5-fold as compared with normal epithelium [34,35]. Overexpression of recombinant LPP-1 decreased MAPK activation, DNA synthesis, PLD (phospholipase D) activation and changes in [Ca2+]i (intracellular Ca2+ concentration) induced by exogenous LPA in rat fibroblasts [33]. The functional role of LPPs is not limited to their ecto-enzyme activities, as LPP-3 has been shown to regulate cell–cell interactions in human endothelial cells [36]. Using an LPP-3 knockout mouse, this phosphatase has been shown to regulate extra-embryonic vasculogenesis and axis patterning [37].
In the present study, we have investigated potential signalling pathways for stimulating IL-8 secretion that are activated by LPA in HBEpCs. Our results show that LPA-induced IL-8 expression and secretion are dependent on changes in [Ca2+]i, IκB (inhibitory κB) phosphorylation and translocation of NF-κB to the nucleus. Furthermore, we studied the role of LPPs in regulating LPA-mediated signalling and IL-8 secretion. All three LPP isoforms are expressed in HBEpCs, and overexpression of hLPP-1 (human LPP-1) attenuates the LPA-induced release of intracellular Ca2+, IκB phosphorylation, translocation of NF-κB to nucleus, and IL-8 secretion. These results show for the first time a physiological role for LPP-1 in regulating these signalling pathways and in attenuating the LPA-induced secretion of the inflammatory cytokine IL-8 in HBEpCs.
EXPERIMENTAL
Materials
1-Oleoyl (C18:1)-LPA was purchased from Avanti Polar Lipids (Alabaster, AL, U.S.A.). Mono-oleoyl[9,10-3H]LPA (specific radioactivity 58 Ci/mmol) was obtained from Perkin Elmer Life Sciences (Boston, MA, U.S.A.). Bay11-7082 and BAPTA/AM [bis-(o-aminophenoxy)ethane-N,N,N′,N′-tetra-acetic acid tetrakis(acetoxymethyl ester)] were purchased from A. G. Scientific Inc. (San Diego, CA, U.S.A.). Antibodies for phospho-IκB (phosphorylated on Ser32), β-actin and the NF-κB p65 subunit were from Santa Cruz Biotechnology Inc. (Santa Cruz, CA, U.S.A.). Antibodies against EGF-R (epidermal growth factor receptor) were from Upstate Biotechnology (Lake Placid, NY, U.S.A.), and antibodies against phospho-EGF-R (phosphorylated on Tyr1173) were from Cell Signaling Technology (Beverly, MA, U.S.A.). Human anti-LPP-2 and anti-LPP-3 antibodies were purchased from Exalpha Biologicals, Inc. (Watertown, MA, U.S.A.). Horse-radish peroxidase-conjugated goat anti-rabbit, anti-mouse and Alexa Fluor-488 goat anti-rabbit and anti-mouse were purchased from Molecular Probes (Eugene, OR, U.S.A.). ECL® kit for detection of proteins by Western blotting was obtained from Amersham Pharmacia Inc. (Piscataway, NJ, U.S.A.). The ELISA kit for IL-8 measurement was purchased from Biosource International Inc. (Camarillo, CA, U.S.A.). All other reagents were of analytical grade.
Cell culture
Primary HBEpCs were isolated from normal human lung obtained from lung transplant donors following overnight digestion of the tissue as described previously [38]. The protease was neutralized by the addition of 10% (v/v) fetal calf serum, and the epithelial cells were freed from the tissue by agitation, isolated by centrifugation and then seeded on to Vitrogen-coated P-100 dishes in serum-free basal essential growth medium (supplied by Clonetics, BioWhittaker, Walkersville, MD, U.S.A.) supplemented with growth factors. Cells were incubated at 37 °C in 5% CO2/95% air and subsequently propagated in 35 mm or 100 mm collagen-coated dishes. All experiments were carried out between passages 1 and 4.
Measurement of IL-8 secretion
HBEpCs were pretreated with various concentrations of BAPTA/AM or Bay11-7082 for 1 h. After pretreatment, the media were aspirated and the cells were challenged in basal essential growth medium containing 0.1% (w/v) BSA with or without LPA or other agonists at the indicated concentrations for specified time periods, and IL-8 levels in cell supernatants were analysed by ELISA (Biosource International).
Measurement of [Ca2+]i
HBEpCs were plated on regular glass coverslips (30 mm×8 mm) that were coated with 0.1% vitronectin solution for 1 h at room temperature. Cells (∼80% confluence) were loaded with the fluorescent calcium indicator fura 2 acetoxymethyl ester (5 μM) for 15 min in 1 ml of total BEBM (bronchial epithelial basal medium). Cells were challenged with LPA (1 μM), and fura 2 fluorescence was measured at excitation wavelengths of 340 and 380 nm and an emission wavelength of 510 nm, as described in [39].
Adenovirus production of wild-type and catalytically inactive LPP-1
The hLPP-1 complete cDNA expression vector, an inactive hLPP-1 (R217K) mutant [40], mLPP-1 (mouse LPP-1) complete cDNA or an inactive mLPP-1 mutant [31] with a cytomegalovirus promoter were transferred into an adenovirus-packing cell line following the manufacturer's instructions. The recombinant plasmids were linearized and propagated in HEK 293 cells, and high-titre purified preparations (∼1010 plaque-forming units/ml) were generated by the University of Iowa Gene Transfer Vector Core.
Adenoviral infection of HBEpCs
Infection of HBEpCs (60– 80% confluence) in 35 or 60 mm dishes was carried out with vector, hLPP-1 wt (wild type), hLPP-1 (R217K) mutant [MOI (multiplicity of infection) 25], Myc-tagged mLPP-1 or Myc-tagged mLPP-1 mutant (MOI 1–10). Viral infection was allowed to proceed in complete BEBM for a further 24– 48 h.
Preparation of cell lysates, immunoprecipitation, and Western blots
HBEpCs infected with control, vector control or adenovirus were grown in 100 mm dishes and stimulated with LPA, rinsed twice with ice-cold PBS and lysed in 1 ml of lysis buffer [11]. Equal amounts of protein (500 μg) were incubated with anti-Myc antibody (1:100 dilution) overnight at 4 °C followed by addition of 50 μl of Protein A/G–agarose and additional incubation for 1–2 h at 4 °C. Cell lysates were centrifuged at 5000 g for 2 min, and washed five times with ice-cold PBS. Equal amounts of protein (20 μg) were subjected to SDS/PAGE on 10% gels and incubated with primary antibodies against c-Myc (9E10), LPPs, IκB or β-actin in 5% (w/v) BSA in TBST (Tris-buffered saline containing 0.1% Tween 20) for 1 h at room temperature. The membranes were washed at least three times with TBST at 15 min intervals and then incubated with either mouse or rabbit horseradish peroxidase-conjugated secondary antibody (1:3000 dilution) for 1–2 h at room temperature, and developed with an enhanced chemiluminescence detection system according to the manufacturer's instructions (Amersham).
RT-PCR
Total cellular RNA was extracted from HBEpCs using an RNEasy kit (Qiagen, Los Angeles, CA, U.S.A.) according to the manufacturer's instructions. cDNA was generated using a cDNA synthesis kit according to the manufacturer's recommendation. The PCR programme for LPPs was as follows: denaturation at 94 °C for 3 min, and then 30 cycles of amplification consisting of denaturation at 94 °C for 1 min, annealing at 55 °C for 2 min, and extension at 72 °C for 3 min. The PCR products were confirmed by sequencing. Specific primers for hLPP-1, hLPP-2, hLPP-3 and human SPP-1 were constructed based on published data in GenBank. LPP-1: forward, 5′-CTTCAAGCCAGGATGAAGGGAG-3′; reverse, 5′-CTGGTGATTGCTCGGATAGTG-3′ (294 bp); LPP2: forward, 5′-CATCTCAGACTTCTTCAAAGCCCG-3′; reverse, 5′-CAGCAACTATCTGATCTCTCGG-3′ (429 bp); LPP-3: forward, 5′-CAGCGCCATCAAAACTACAAG-3′; reverse, 5′-CACAGAGCACAGCGTCATTTATTG-3′ (275 bp); SPP-1: forward, 5′-GGTAAAGCCAGGTCAGAATTAGGC-3′; reverse, 5′-GCCTCCCATGTTCAACATCATGG-3′) (536 bp).
Real-time PCR
Total RNA was extracted and isolated using TRIzol reagent (Life Technologies, Gaithersburg, MD, U.S.A.). One-step RT-PCR was performed in a Light-Cycler using the SYBR Green QuatiTet RT-PCR kit (Qiagen, Valencia, CA, U.S.A.). Primers for 18 S RNA were used as a housekeeping gene to normalize expression. Primers were designed based on the cDNA of human IL-8 (forward, 5′-TTCTGCAGCTCTGTGTGAAGG-3′; reverse, 5′-ATGAATTCTCAGCCCCTCTTC-3′; 295 bp). RT was carried out at 50 °C for 20 min followed by cycling to 95 °C for 15 min. Amplicon expression in each sample was normalized to its 18 S RNA content.
Measurement of LPP ecto-activity in HBEpCs
HBEpCs were grown on 35 mm dishes to ∼90% confluence. LPA (1 μM) (unlabelled plus [3H]LPA at 100000 d.p.m. per dish; specific radioactivity 2.2×103 d.p.m./pmol) complexed to 0.1% (w/v) BSA in 1 ml of BEBM was added to HBEpCs and cells were incubated at 37 °C for various times (0–120 min). The media (1 ml) were transferred to glass tubes and 2 ml of methanol/HCl (100:1, v/v) was added. Lipids were extracted by addition of 2 ml of chloroform and 0.8 ml of water, and centrifuged to separate the chloroform and methanol/aqueous phases. The lower chloroform phase was removed into vials and evaporated under N2, and the hydrolysis of [3H]LPA to [3H]monoacylglycerol and other metabolites such as free oleic acid was determined after separation by TLC on silica gel H plates in the presence of unlabelled monoacylglycerol, oleic acid and triacylglycerol, which were added as carriers to the total lipid extracts. The TLC plates were developed in hexane/diethyl ether/acetic acid (60:40:1, by vol.), exposed to iodine vapours to identify the lipids, and areas corresponding to monoacyl-, diacyl- and triacyl-glycerol and oleic acid were scraped into vials and counted for radioactivity. The hydrolysis of [3H]LPA was expressed as a percentage of the total radioactivity added to the cells.
Measurement of LPP activity in cell-free preparations
Dephosphorylation of [3H]LPA complexed with fatty acid-free BSA was determined as described previously [41]. In brief, LPP activity assays were performed in total cell lysates or immunoprecipitates from cells infected with vector control, Myc-tagged mLPP-1 wt, or Myc-tagged mLPP-1 (R217K) mutant (MOI 10; 24 h). Unlabelled 1-oleoyl LPA was mixed with [3H]LPA (2.2×106 d.p.m.; specific radioactivity 2.2×103 d.p.m./pmol) to give a final concentration of 1 μM LPA, dried under N2 and dispersed in a medium containing 20 mM Tris, pH 7.5, and 1 mM EGTA. The assay volume was 200 μl, which contained 1 μM [3H]LPA plus total cell lysate (20– 40 μg of protein) or an equal volume of immunoprecipitate of cells expressing mLPP-1 wt or mLPP-1 mutant. Incubations were carried out at 37 °C for 30 min in a shaking water bath. Assays were terminated by the addition of 25 μl of 12 M HCl, and lipids were extracted after adding 1 ml of methanol, 1 ml of chloroform and 0.65 ml of water. The samples were centrifuged for 10 min at 5000 g and [3H]MOG (mono-oleoylglycerol), free oleic acid and non-hydrolysed LPA were quantified after separation on TLC using hexane/diethyl ether/acetic acid (40:60:1, by vol.) as the developing solvent system. Non-labelled MOG and oleic acid were added as carriers for visualization under I2 vapours. In this solvent system, LPA stayed at the origin with other polar lipids, while MOG and oleic acid exhibited relative mobilities of 0.15 and 0.45 respectively.
Immunocytochemistry
Control, vector control or Myc-tagged-mLPP-1-overexpressing HBEpCs were grown on coverslips to ∼80% confluence. After treatment, coverslips were rinsed with PBS and treated with 3.7% (v/v) formaldehyde in PBS at room temperature and cells were permeabilized with 0.5% Triton X-100 for 2 min. Cells were subjected to immunostaining with antibody against NF-κB p65 subunit (1:200 dilution) or c-Myc (9E10; 1:200 dilution) for 1 h, washed three times with TBST and stained with Alexa Fluor 488 (1:200 dilution in blocking buffer; 1 h) as secondary antibody. After washing twice with TBST, the coverslips were mounted using commercial mounting medium for fluorescent microscopy (Kirkegaard and Perry Laboratories, Gaithersburg, MD, U.S.A.), and were examined using a Nikon Eclipse TE 2000-S immunofluorescent microscope.
Statistical analyses
All results were subjected to statistical analysis using one-way ANOVA and, where appropriate, analysed by a Student–Newman–Keuls test. Data are expressed as means±S.D. of triplicate samples from at least three independent experiments, and the level of significance was taken to be P<0.05.
RESULTS
Expression of LPPs in primary culture of HBEpCs
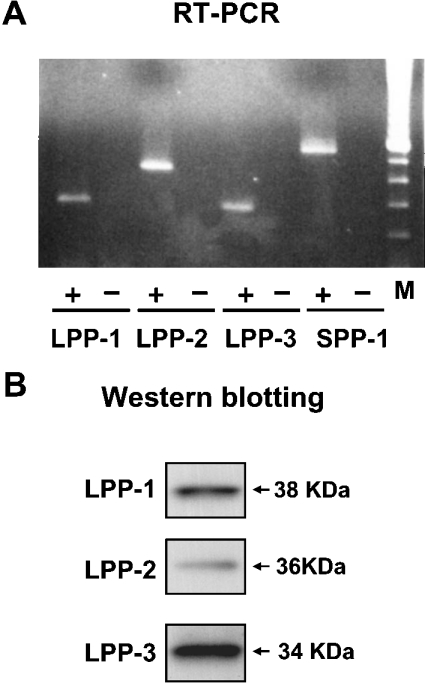
LPPs control lipid phosphate levels in tissues and biological fluids via their ecto-enzyme activity [33–35]. To determine the role of LPPs in LPA-induced IL-8 secretion, we characterized LPP isoforms in HBEpCs by RT-PCR and Western blotting. RNA was extracted from HBEpCs, primers were designed from hLPP-1, hLPP-2, hLPP-3 and human SPP-1 cDNA sequences, and RT reactions were performed using random primers with and without reverse transcriptase enzyme. As shown in Figure 1(A), LPP-1, -2 and -3 as well as SPP-1 were detected by RT-PCR and showed the expected size (bp) on the gel. The PCR products were subcloned into the TOPO vector, and were then confirmed by sequencing (Y. Zhao and V. Natarajan, unpublished work). Additionally, protein expression of the LPP-1 (∼38 kDa), LPP-2 (∼36 kDa) and LPP-3 (∼34 kDa) isoforms was confirmed by Western blotting with LPP-specific antibodies (Figure 1B). These data show that HBEpCs express LPP-1, -2 and -3 as well as SPP-1. We did not detect the presence of SPP-2 by RT-PCR.
Figure 1. Detection of LPPs by RT-PCR and Western blotting in HBEpCs.
(A) Total RNA was extracted from HBEpCs and transcription of the genes encoding LPPs (LPP-1, -2 and -3, and SPP-1) was assessed by RT-PCR (− indicates the absence of reverse transcriptase and + indicates the presence of reverse transcriptase during the RT reaction) with primers to the indicated LPPs. Lane M contains molecular size markers. (B) Cell lysates (20 μg of protein) were subjected to SDS/PAGE and analysed by Western blotting with anti-LPP-1, -LPP-2 and -LPP-3 antibodies. Each Western blot is representative of three independent experiments.
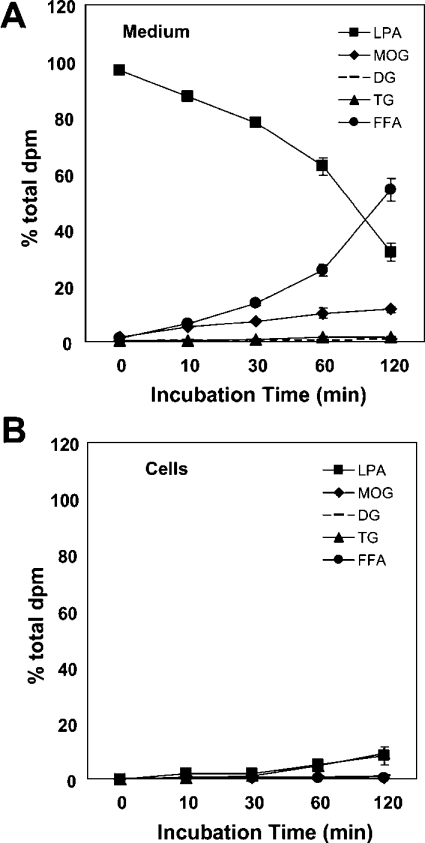
As LPP-1–3, but not SPP-1 and -2, are ecto-enzymes, their catalytic sites are located outside the plasma membrane. When [3H]-LPA (1 μM) complexed to 0.1% BSA in BEBM was added on top of the HBEpCs, time-dependent hydrolysis to MOG and free oleic acid was observed; at the end of 2 h, almost 70% of the added [3H]LPA had been hydrolysed (Figures 2A and 2B). Of the total radioactivity added to cells, ∼80% and ∼20% was recovered from the medium and cells respectively. Analysis by TLC of the lipid extracts from the medium revealed that, up to 30 min of incubation, [3H]MOG and oleic acid accumulated almost equally; however, at 60 and 120 min the major breakdown product was [3H]oleic acid (Figure 2A). Also, approx. 10% of the total radioactivity in the lipid extracts from the medium and from the cells was in diacylglycerol, triacylglycerol and phospholipid fractions. Our data also show the presence of small amounts of [3H]LPA in the lipid extracts from cells. The LPP-mediated hydrolysis of [3H]-LPA was attenuated by vanadate and diperoxovanadate, but not by the serine/threonine phosphatase inhibitors okadaic acid and tautomycin (results not shown).
Figure 2. Time course of hydrolysis of [3H]LPA by LPPs in HBEpCs.
HBEpCs (∼90% confluence) were incubated with [3H]LPA (1 μM; specific radioactivity 2.2×103 d.p.m./pmol) complexed with 0.1% BSA in BEBM for up to 120 min. At each time point, medium was removed and lipids were extracted from the medium (A) and the cells (B) and analysed by TLC as described in the Experimental section. Values are from three independent experiments in triplicate, and are expressed as a percentage of the total radioactivity (d.p.m.) in the lipid extract. DG, diacylglycerol; TG, triacylglycerol; FFA, non-esterified (‘free’) fatty acids.
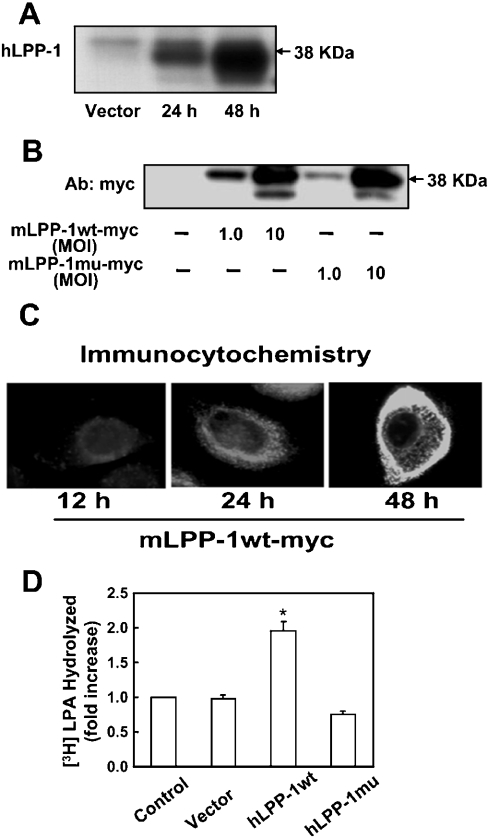
Next we investigated the effects of overexpression of hLPP-1 wt and hLPP-1 mutant on LPA hydrolysis in intact and cell-free preparations. HBEpCs were infected with empty vector or adenoviral constructs containing hLPP-1 cDNA (25 MOI) for 24 h and 48 h, and cell lysates were analysed for increased expression of hLPP-1 wt, Myc-tagged mLPP-1 wt or Myc-tagged mLPP-1 mutant protein by Western blotting and immunocytochemistry. As shown in Figure 3(A), infection of HBEpCs with adenoviral constructs of hLPP-1 wt enhanced the expression of the wt protein in a time-dependent fashion. Also, the expression of Myc-tagged mLPP-1 wt or mutant was increased at a MOI of either 1 or 10, as detected by Western blotting with anti-Myc antibody (Figure 3B). To determine the localization of overexpressed LPP-1, HBEpCs were infected with adenoviral vectors containing C-terminally Myc-tagged mLPP-1 wt (MOI 10) for 12, 24 and 48 h, and cells were immunostained with anti-Myc antibody (9E10) to examine the distribution. In unstimulated HBEpCs, overexpressed mLPP-1 wt was localized at the cell surface and possibly in intracellular organelles, including the perinuclear membrane, but not inside the nucleus (Figure 3C). Furthermore, overexpression of hLPP-1 wt or mLPP-1 mutant had no effect on the expression of LPP-2 or LPP-3, as determined by RT-PCR and Western blotting (results not shown). The functional significance of overexpression of LPP-1 wt or mutant was tested by determining the hydrolysis of [3H]LPA in intact cells as well as in cell-free preparations. Overexpression of hLPP-1 wt enhanced the hydrolysis of exogenously added [3H]LPA by ∼2-fold compared with vector control cells; however, overexpression of hLPP-1 mutant had no effect on [3H]LPA hydrolysis (Figure 3D).
Figure 3. Overexpression of adenoviral constructs of LPP-1 wt and LPP-1 mutant in HBEpCs.
(A) HBEpCs (∼70% confluence in 35 mm dishes) were infected with empty vector or hLPP-1 wt adenoviral construct (MOI 25) in complete BEBM for 24 and 48 h. At the indicated time points, cell lysates were prepared as described in the Experimental section, and subjected to SDS/PAGE and Western blotting with anti-hLPP-1 antibody. (B) HBEpCs (∼70% confluence) were infected with empty vector, Myc-tagged mLPP-1 wt or Myc-tagged mLPP-1 mutant adenoviral constructs (MOI 1 and 10) in complete BEBM for 24 h. Cell lysates were subjected to SDS/PAGE and Western blotting with anti-Myc antibody (Ab). (C) HBEpCs grown on coverslips to ∼70% confluence were infected with Myc-tagged mLPP-1 wt in adenoviral constructs (MOI 10) for 12, 24 h and 48 h. Cells were subjected to immunostaining with anti-Myc antibody (9E10) and examined by fluorescent microscopy. Each immunofluorescence image is representative of three independent experiments. (D) HBEpCs (∼70% confluence) were infected with empty vector, hLPP-1 wt or hLPP-1 mutant adenoviral constructs (MOI 25) for 48 h. [3H]LPA (1 μM; specific radioactivity 2.2×103 d.p.m./pmol) complexed with 0.1% BSA in BEBM was added to each dish and dephosphorylation was examined at the end of a 30 min incubation. Lipids were extracted from the medium under acidic conditions and separated by TLC on silica gel H developed in hexane/diethyl ether/acetic acid (60:40:1, by vol.) as the solvent system. Unlabelled MOG was added as carrier, and radioactivity associated with the dephosphorylated product of LPA was quantified by counting in a scintillation spectrometer and corrected to d.p.m. Values are means±S.D. of three independent experiments, and are expressed as fold increase in LPA hydrolysis; *P<0.05 compared with vector control.
We then examined LPP activity in cell lysates and immunoprecipitates from HBEpCs infected with vector control or Myc-tagged mLPP-1 wt or mLPP-1 mutant. As shown in Table 1, lysates from vector-infected cells hydrolysed ∼2.8% of added [3H]LPA to [3H]MOG, while in lysates from mLPP-1 wt infected cells, hydrolysis of LPA to MOG was increased to ∼16%. However, the mLPP-1 mutant did not block the basal activity (Table 1). The immunoprecipitates obtained from cell lysates of Myc-tagged mLPP-1 wt and mutant were also tested for LPP activity. As shown in Table 1, ∼27% of the added [3H]LPA was hydrolysed to [3H]MOG by immunoprecipitates of cells containing Myc-tagged mLPP-1, while the mutant exhibited negligible activity. Our results are consistent with earlier published work on LPP-1 localization and activity in fibroblasts [42], and in resting and stimulated platelets [41].
Table 1. LPP activity in cell lysates and immunoprecipitate from HBEpCs.
HBEpCs (∼70% confluence in 60 mm dishes) were infected with vector, Myc-tagged mLPP-1 wt, or Myc-tagged mLPP-1 (R217K) mutant adenoviral constructs (MOI 10; 1× 106 cells per dish) for 24 h. Cell lysates were prepared as described in the Experimental section and aliquots of 500 μg of protein were subjected to immunoprecipitation overnight with anti-Myc antibody (1 μl per 500 μg of protein). For dephosphorylation of [3H]LPA, total cell lysates or immunoprecipitates from cells transfected with vector, wt or mutant LPP-1 were incubated with 1 μM [3H]LPA (specific radioactivity 2.2×103 d.p.m./pmol) complexed with 0.1% BSA for 30 min at 37 °C. Lipids were extracted under acidic conditions and dephosphorylation of [3H]LPA to [3H]MOG was quantified by separation of lipids on TLC using hexane/diethyl ether/acetic acid (60:40;1, by vol.) as the developing solvent system. Results are expressed as % [3H]MOG formed from total [3H]LPA added for dephosphorylation.
| [3H]MOG formed (%) | |||
|---|---|---|---|
| Vector | mLPP-1 wt–Myc | mLPP-1 mutant–Myc | |
| Cell lysate | 2.8 | 16.0 | 2.4 |
| Immunoprecipitate | − | 27.3 | 1.4 |
Overexpression of LPP-1 attenuates LPA-induced changes in [Ca2+]i, NF-κB activation and IL-8 secretion
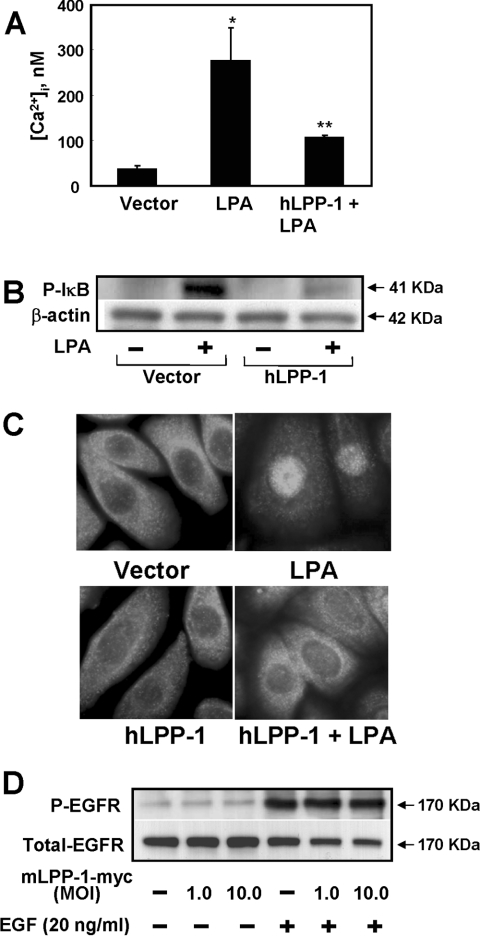
We have recently reported that LPA stimulates IL-8 production via activation of protein kinase Cδ and NF-κB signalling pathways in HBEpCs [43]. Furthermore, it has been shown that overexpression of LPP-1 attenuates LPA-mediated ERK phosphorylation and PLD activation in rat fibroblasts [33] and Rho activation in platelets [41]. This prompted us to determine whether overexpression of LPP-1 modulates LPA-induced changes in [Ca2+]i, NF-κB signalling and IL-8 secretion in HBEpCs. Cells were grown on coverslips and loaded with the fluorescent calcium indicator fura 2 acetoxymethyl ester (5 μM) for 10 min; they were then challenged with 1 μM LPA for 10 min and changes in [Ca2+]i were measured as the ratio of 340/380 nm fluorescence. In LPA-challenged cells (Figure 4A) [Ca2+]i increased approx. 6-fold compared with unstimulated cells (from basal levels of 40±3 nM to 260±20 nM with LPA), and overexpression of hLPP-1 blocked ∼70% of the LPA-induced release in [Ca2+]i. Pretreatment of cells with various concentrations of the cell-permeable calcium chelator BAPTA/AM blocked the LPA-mediated changes in [Ca2+]i (results not shown).
Figure 4. Effects of overexpression of hLPP-1 on LPA-induced changes in [Ca2+]i, IκB phosphorylation, NF-κB translocation and EGF-R phosphorylation.
HBEpCs (∼70% confluence) on coverslips were infected with vector control or hLPP-1 wt adenoviral construct (MOI 25) for 48 h. (A) Cells were loaded with the fluorescent calcium indicator fura 2 acetoxymethyl ester (5 μM) for 15 min and then challenged with 1 μM LPA for 10 min. [Ca2+]i was measured as the ratio of 340/380 nm fluorescence and expressed as nM. *P<0.05 compared with vector control; **P<0.05 compared with LPA treatment. (B) Cells were challenged with 1 μM LPA for 10 min, and total cell lysates were subjected to SDS/PAGE and Western blotting with antibodies against phospho-IκB and IκB. Equal loading was confirmed by blotting for β-actin. Shown is a representative blot of three independent experiments performed in triplicate. (C) Cells were challenged with medium containing or not 1 μM LPA for 15 min and subjected to immunostaining with antibody against NF-κB subunit (p65) and examined by fluorescent microscopy. Each immunofluorescent image is representative of three different experiments. (D) HBEpCs (∼70% confluence in 35 mm dishes) were infected with vector or with Myc-tagged mLPP-1 wt adenoviral construct (MOI 1–10) for 24 h. Cells were challenged with medium alone or medium containing EGF (20 ng/ml) for 15 min. Cell lysates were prepared as described above and subjected to SDS/PAGE and Western blotting with antibodies against phospho-EGF-R (Y1173) and EGF-R. Each Western blot is representative of two independent experiments.
Next we investigated the effects of overexpression of LPP-1 on LPA-mediated NF-κB activation. LPA (1 μM) challenge for 15 min increased IκB phosphorylation in HBEpCs, and overexpression of hLPP-1 for 48 h attenuated LPA-dependent phosphorylation of IκB and translocation of NF-κB to the nucleus, as determined by immunocytochemistry (Figures 4B and 4C). In these experiments, hLPP-1 overexpression increased the hydrolysis of added LPA (vector control ∼1.5% to 3.5% in overexpressing cells), indicating that availability of total exogenous LPA in the medium was unlikely to be a major limiting factor in attenuating the signalling of NF-κB. Also, pretreatment of HBEpCs with BAPTA/AM (10 –25 μM) attenuated LPA-induced IκB phosphorylation and translocation of NF-κB to the nucleus (results not shown), suggesting that activation of NF-κB by LPA is dependent on increases in [Ca2+]i. Next we checked the specificity of LPP-1 by studying its effects on EGF-R activation by EGF. As shown in Figure 4(D), overexpression of mLPP-1 wt did not alter EGF-mediated phosphorylation of EGF-R.
In parallel experiments, we examined the effects of hLPP-1 overexpression on LPA-, PMA- and TNF-α (tumour necrosis factor-α)-induced IL-8 secretion in HBEpCs. Overexpression of hLPP-1 (MOI 10) for 24 h attenuated LPA-mediated IL-8 production by ∼80% compared with control cells (Table 2). Interestingly, overexpression of hLPP-1 also prevented PMA- and TNF-α-mediated IL-8 secretion by ∼20% and ∼40% respectively. These results demonstrate that hLPP-1 overexpression significantly decreased LPA-induced IL-8 production, and it also decreased, to a lesser extent, the effects of PMA and TNF-α in this respect. Similar to Ca2+ signalling, BAPTA/AM also blocked LPA-induced IL-8 secretion [vehicle, 0.3±0.04 pg/μg; LPA, 2.1±0.3 pg/μg; BAPTA/AM (10 μM), 0.15±0.1 pg/μg; BAPTA/AM (10 μM)+LPA, 1.0±0.2 pg/μg; BAPTA/AM (25 μM), 0.15±0.1 pg/μg; BAPTA/AM (25 μM)+LPA, 0.3±0.1 pg/μg]. These results demonstrate that overexpression of LPP-1 modulates LPA-induced Ca2+ release, NF-κB activation and IL-8 secretion in HBEpCs.
Table 2. Effects of overexpression of Myc-tagged mLPP-1 on LPA-, PMA- and TNF-α-induced IL-8 secretion in HBEpCs.
HBEpCs (∼70% confluence in 35 mm dishes) were infected with vector control or Myc-tagged mLPP-1 wt adenoviral constructs (MOI 10; 2×105 cells per dish) for 24 h. Cells were challenged with 1 ml of medium alone or containing LPA (1 μM), PMA (25 nM) or TNF-α (20 ng/ml) for 3 h. The supernatants were collected and centrifuged, and aliquots stored at −80 °C for analysis of IL-8 by ELISA as described in the Experimental section. Values are means±S.D. of three independent experiments in triplicate, and are expressed either as pg/μg of protein in cell lysates or % of control.
| IL-8 | ||
|---|---|---|
| Treatment | (pg/μg of protein) | (% of control) |
| Vehicle | 1.2±0.01 | 100 |
| LPA (1 μM) | 16.3±2.6 | 1358 |
| PMA (25 nM) | 29.4±3.9 | 2450 |
| TNF-α (20 ng/ml) | 11.6±2.4 | 967 |
| mLPP-1 wt+vehicle | 1.1±0.2 | 92 |
| mLPP-1 wt+LPA (1 μM) | 4.2±0.6 | 350 |
| mLPP-1 wt+PMA (25 nM) | 24.2±2.3 | 2017 |
| mLPP-1 wt+TNF-α (20 ng/ml) | 6.8±0.4 | 567 |
As LPA added exogenously to HBEpCs is metabolized to MOG and free oleic acid, we tested if these metabolites also stimulated IL-8 secretion. Treatment of HBEpCs with LPA (1 μM), but not with MOG (1 μM) or oleic acid (1 μM), for 3 h resulted in significant secretion of IL-8 (results not shown). This indicates that LPA, but not its major breakdown products MOG and oleic acid, stimulates IL-8 production in HBEpCs.
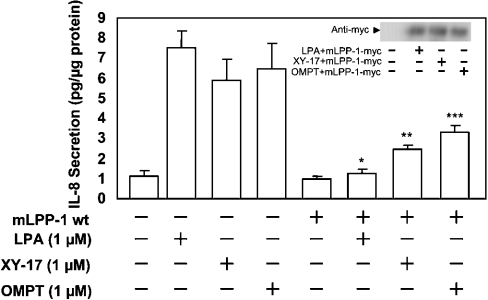
Effects of LPA3 receptor agonists on IL-8 secretion
To test the possible role of LPP-1 in regulating intracellular signal transduction and IL-8 generation, we tested the effects of the LPA3 receptor agonists XY-17 [(3S)-1-fluoro-3-hydroxy-4-(oleoyloxy)butyl-1-phosphonate] and OMPT (D-sn-1-oleoyl-2-methylglyceryl-3-phosphothionate). XY-17 is a phosphonate analogue of LPA that is resistant to LPP action, while OMPT is hydrolysed by LPPs, but a much lower rate compared with LPA [44,45]. HBEpCs were infected with vector control or mLPP-1 wt adenoviral constructs (MOI 10) for 24 h prior to exposure to LPA (1 μM), XY-17 (1 μM) or OMPT (1 μM) for 3 h. As shown in Figure 5, these two receptor agonists stimulated IL-8 secretion similarly to LPA in vector-infected cells (vehicle, 1.12±0.1; LPA, 7.5±0.3; XY-17, 5.9±0.4; OMPT, 6.5±0.4 pg of IL-8/μg of protein). Overexpression of hLPP-1 prevented ∼84% of LPA-induced IL-8 secretion; however, it only blocked ∼60% and ∼49% of XY-17- and OMPT-mediated IL-8 production. These results further suggest that overexpressed LPP-1 may regulate IL-8 production by LPA and LPA receptor agonists by modulating intracellular signals in addition to any effect on the extracellular breakdown of LPA.
Figure 5. Effects of overexpression of mLPP-1 wt on LPA-, XY-17- and OMPT-mediated IL-8 secretion.
HBEpCs (∼70% confluence) were infected with vector control or Myc-tagged mLPP-1 wt adenoviral constructs (MOI 10) for 48 h. Cells were challenged with 1 μM LPA, XY-17 or OMPT for 3 h, and IL-8 secreted into the medium was quantified by ELISA. Values are means±S.D. of three independent experiments in triplicate, and are expressed as pg/μg of protein. *P<0.05 compared with LPA treatment; **P<0.05 compared with XY-17 treatment; ***P<0.05 compared with OMPT treatment.
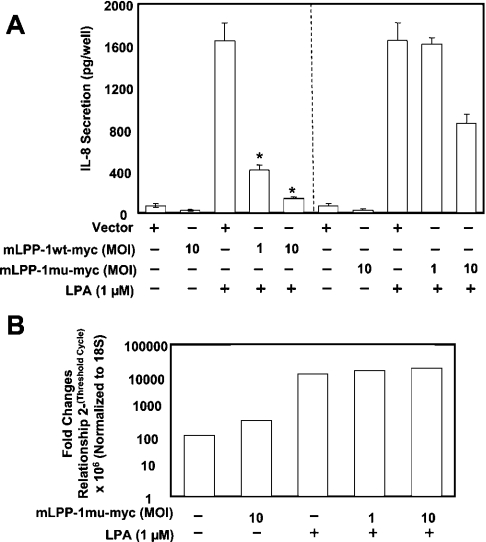
Overexpression of the mLPP-1 (R217K) mutant has no effect on LPA-induced changes in [Ca2+]i, NF-κB activation and IL-8 secretion
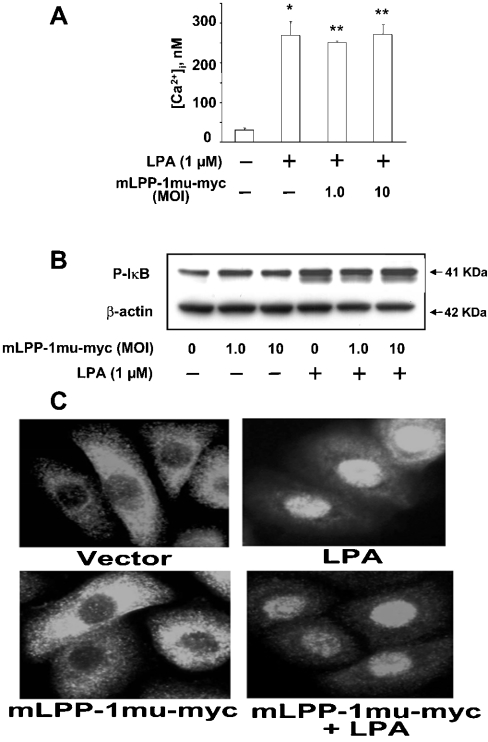
To establish whether the catalytic activity of LPP-1 is involved in modulating LPA signalling, we investigated the effects of the overexpression of the catalytically inactive mLPP-1 (R217K) mutant on LPA-induced Ca2+ release, NF-κB activation and IL-8 gene expression and secretion. As shown in Figure 6(A), overexpression of mLPP-1 wt (MOI 1 and 10) for 24 h attenuated LPA-induced IL-8 secretion. Overexpression of mLPP-1 (R217K) mutant at MOI 1 had no effect on LPA-induced IL-8 secretion; however, infection of cells with mLPP-1 (R217K) at MOI 10 blocked ∼40% of LPA-induced IL-8 secretion (Figure 6A). To further understand the effect of infection with a higher dose of the mLPP-1 mutant on LPA-induced IL-8 secretion, we determined the expression of IL-8 mRNA by real-time PCR. As shown in Figure 6(B), LPA increased IL-8 gene expression, and overexpression of the mLPP-1 mutant (MOI 1 and 10) did not modulate IL-8 gene expression by LPA. Since our results show that LPA-induced IL-8 gene expression and secretion are dependent on [Ca2+]i and NF-κB signalling, we also checked the effects of overexpression of the mLPP-1 (R217K) mutant on LPA-mediated [Ca2+]i and NF-κB signalling. Unlike the effect of LPP-1 wt, overexpression of mLPP-1 (R217K) mutant had no effect on LPA-induced changes in [Ca2+]i, IκB phosphorylation or NF-κB nuclear translocation (Figures 7A–7C). These results show that the partial attenuation of LPA-mediated IL-8 secretion by the mLPP-1 (R217K) mutant does not occur at the transcriptional level and is not due to altered Ca2+ responses, IκB phosphorylation or NF-κB activation.
Figure 6. Effects of overexpression of mLPP-1 mutant on LPA-induced IL-8 secretion and gene expression.
(A) HBEpCs (∼70% confluence in 35 mm dishes) were infected with vector or with Myc-tagged wt or mutant (mu) mLPP-1 adenoviral constructs (MOI 10) for 24 h. Cells were then challenged with medium alone or containing 1 μM LPA for 3 h, then the medium was collected and IL-8 secreted into the medium was measured by ELISA. *P<0.05 compared with LPA treatment in vector. (B) HBEpCs were infected with adenoviral Myc-tagged mLPP-1 mutant adenoviral construct (MOI 1 or 10) for 24 h, and then challenged with 1 μM LPA for 90 min. IL-8 mRNA levels were measured by real time RT-PCR using IL-8 specific primers.
Figure 7. Effects of overexpression of mLPP-1 mutant on LPA-induced changes in [Ca2+]i, IκB phosphorylation and NF-κB activation.
(A) HBEpCs (∼70% confluence) grown on coverslips were infected with vector or Myc-tagged LPP-1 mutant (mu) adenoviral constructs (MOI 1 or 10) for 24 h. Cells were loaded with the fluorescent calcium indicator dye fura 2 (5 μM) for 15 min, and cells were challenged with 1 μM LPA for 10 min. [Ca2+]i was measured as the ratio of 340/380 nm fluorescence, and data are expressed as nM. Values are means±S.D. of three independent experiments in triplicate; *P<0.05 compared with vehicle control; **P<0.05 compared with LPA treatment. (B) HBEpCs (∼70% confluence in 35 mm dishes) were infected with vector or Myc-tagged mLPP-1 adenoviral constructs (MOI 1 or 10) for 24 h. Cells were challenged with 1 μM LPA for 10 min, and cell lysates were subjected to SDS/PAGE and Western blotting with antibody against phospho-IκB. Equal loading was confirmed by blotting for β-actin. Each Western blot is representative of three independent experiments. (C) HBEpCs (∼70% confluence) grown on coverslips were infected with vector or Myc-tagged mLPP-1 mutant adenoviral construct (MOI 10) for 24 h. Cells were challenged with medium alone or medium containing 1 μM LPA for 15 min, and cells were subjected to immunostaining with antibody against NF-κB subunit (p65) and examined by fluorescent microscopy. Each immunofluorescent image is a representative of the monolayers visualized in three different experiments.
DISCUSSION
The present study provides for the first time compelling evidence that LPP-1 regulates LPA-induced IL-8 secretion in HBEpCs. Our results show that overexpression of LPP-1 attenuates LPA-dependent increases in [Ca2+]i, NF-κB activation and IL-8 production. These results are consistent with the hypothesis that LPPs are negative regulators of LPA signalling and have a definite role in the metabolism of intra- and extra-cellular LPA and cellular functions [29–32,41,46]. The LPP superfamily includes bacterial phosphatases, yeast diacylglycerol pyrophosphatase, mammalian glucose-6-phosphatase and Wunen proteins in Drosophila [26,31]. Expression of LPP-1 and LPP-3 has been shown in human lung tissue [26]. We detected expression of all the three isoforms of LPP by RT-PCR and Western blotting (Figure 1), and exogenous LPA was hydrolysed to MOG by LPP-like activity in HBEpCs (Figure 2). In addition to [3H]MOG, there was a substantial accumulation of [3H]oleic acid, that could be attributed to catabolism of MOG or LPA by a lipase or lysophospholipase type of activity.
The localization of native and overexpressed LPP-1, -2 and -3 has been reported in several mammalian cells [29–32,34]. In our present study, infection of cells with adenoviral constructs containing Myc-tagged mLPP-1 wt resulted in localization of the overexpressed protein in both the plasma membrane and the cytoplasm, as shown by immunofluorescence microscopy. The overexpressed LPP-1 was functionally active, as demonstrated by enhanced total LPP activity and hydrolysis of exogenous [3H]LPA as compared with vector control cells. Our present results are compatible with earlier published work on the cell surface localization of LPP-1 that was associated with increased LPP activity and decreased LPA- and S1P-mediated signal transduction. LPP-1 overexpression attenuated the activation of p42/44 MAPK, stimulation of DNA synthesis by exogenous LPA and LPA-induced increases in Ca2+ mobilization and activation of PLD in fibroblast [33]. In platelets, LPP-1 regulates LPA production and signalling, and inhibiting LPP activity by sn-3-substituted difluoromethylenephosphonate potentiated platelet aggregation and shape change responses to LPA [41]. Transfection of LPP-1 or LPP-2, but not LPP-3, substantially decreased S1P-, LPA- or PA-dependent stimulation of the p42/p44 MAPK pathway in HEK 293 cells [33]. Furthermore, in that study the reduced p42/p44 MAPK activation was correlated with decreased formation of intracellular PA, but not with the ecto-LPP activity [33]. Here, we found that overexpression of LPP-1 attenuated LPA-induced increases in [Ca2+]i (Figure 4A), phosphorylation of IκB, translocation of NF-κB to the nucleus (Figures 4B and 4C) and IL-8 secretion (Table 2). We also found that overexpression of the catalytically inactive mLPP-1 (R217K) mutant partially attenuated LPA-mediated IL-8 secretion, which was independent of its lack of enzyme activity. Overexpression of the mLPP-1 (R217K) mutant had no significant effect on [3H]LPA hydrolysis or on LPA-induced Ca2+ release, IκB phosphorylation, NF-κB translocation to the nucleus or IL-8 gene expression in HBEpCs (Figures 6 and 7). Interestingly, infection of cells with the mLPP-1 (R217K) mutant at MOI 10, but not at MOI 1, partially attenuated LPA-induced IL-8 secretion without altering IL-8 mRNA levels, as quantified by real time RT-PCR. At this time, the mechanism responsible for the LPP-1 (R217K) mutant partly blocking IL-8 production by LPA is unclear.
Attenuation of LPA-induced signalling and IL-8 secretion by overexpression of LPP-1 cannot be attributed to significant hydrolysis of exogenous LPA alone. As shown in Figure 3(C), overexpression of LPP-1 enhanced the hydrolysis of [3H]LPA by approx. 2-fold compared with vector control cells. In the present study, all experiments related to LPA signalling, such as Ca2+ release, IκB phosphorylation and NF-κB activation, were performed for 15 or 30 min, suggesting that availability of LPA was not a limiting factor in attenuation of the signals by LPP-1. We also observed that overexpression of LPP-1 wt attenuated PMA- or TNF-α-mediated IL-8 generation to a lower extent compared with its effects on a LPA challenge (Table 2). This suggests that LPP-1 may have additional action(s) on intracellular signalling pathways involved in the regulation of IL-8 formation that may be independent of its activity in the dephosphorylation of exogenous LPA. Experiments conducted with the LPA3 receptor agonists XY-17 and OMPT also indicated possible alternative mechanism(s) for LPP-1 action. XY-17, a non-hydrolysable analogue of LPA, increased IL-8 production in HBEpCs, and overexpression of LPP-1 partially attenuated the XY-17-mediated effect (Figure 5). Similar results were obtained with OMPT in vector control cells and in those overexpressing LPP-1, indicating other possible intracellular effect(s) of LPP-1 on signal transduction and agonist-induced IL-8 generation. Agonists such as XY-17 or PMA/TNF-α may generate intracellular lipid phosphates that could initiate intracellular signalling cascades [5]. Although XY-17 and OMPT are supposed to be specific agonists for LPA3 receptors, our results do not exclude signalling via LPA1 or LPA2 receptors. We have shown previously that butan-1-ol, but not butan-3-ol, and catalytically inactive mutants of PLD1 and PLD2 attenuated S1P-induced IL-8 production in Beas-2B cells, suggesting the involvement of PA generated by PLD signal transduction in enhanced cytokine secretion [11]. Similar to previous studies with S1P [11], overexpression of catalytically inactive mutants of PLD1 and PLD2 or hLPP-1 wt, but not mLPP-1 mutant, attenuated LPA-mediated IL-8 secretion in HBEpCs (results not shown). As LPA stimulates PLD1 and PLD2 in HBEpCs, it is possible that at least some of the observed effects of LPP-1 overexpression may be due to its intracellular action either on PA or on LPA that could be derived from PA.
Alteration of the expression of LPP by genetic manipulation in organisms or cells in culture has been a useful tool in understanding the physiological role of these ecto-enzymes. Overexpression of LPP-3 decreases the growth, survival and tumorigenesis of ovarian cancer cells by increasing the degradation of exogenous LPA [35]. In that study, the decrease in growth caused by LPP-3 was rescued by the addition of a non-hydrolysable LPA analogue, suggesting a role for extracellular LPA in modulating tumour growth [35]. Our finding that LPP-1 modulates LPA-induced signal transduction and IL-8 secretion is intriguing, since this may provide a novel therapeutic approach to regulating airway inflammation resulting from elevated LPA levels in the lung. In Drosophila, inactivation or misexpression of LPP alters germ cell migration in early development, suggesting changes in signal transduction mediated by the LPP-dependent degradation of lipid mediators [47]. Mice that overexpress LPP-1 exhibited decreases in birth weight and abnormalities in fur growth, hair structure and numbers of hair follicles [48]. Furthermore, immortalized fibroblasts isolated from the LPP-1-overexpressing mice showed increased accumulation of diacylglycerol in response to phorbol ester, without significant differences in ERK phosphorylation by LPA, S1P, thrombin, EGF and platelet-derived growth factor [48]. In contrast, LPP-2 knockout mice showed normal viability and phenotype [49], whereas LPP-3 knockout mice displayed severe phenotypic changes, including shortening of the anterior–posterior axis [37]. Additionally, LPP-3 deficiency resulted in decreased β-catenin-mediated transcription of T cell factor, while overexpression of LPP-3 exhibited an opposite effect [37]. Further investigations with LPP knockouts should provide useful information on the role of these phosphatases in regulating cytokine secretion and neutrophil diapedisis in airway inflammatory diseases.
Agonist-induced IL-8 secretion in epithelial cells and ovarian cancer cells is regulated at the transcriptional level by AP-1 and NF-κB [16,43]. Earlier studies suggested possible roles for protein kinase C, MAPKs, Rho and PLD in LPA- and S1P-induced IL-8 production in HBEpCs and Beas-2B cells [14,15,43]. The −162 to +44 nt region of the IL-8 gene promoter contains consensus binding sequences for AP-1 (between −127 and −119) and NF-κB (between −80 and −70) [23,24], suggesting that LPA activates one or both of these transcription factors to regulate IL-8 gene transcription. Consistent with this, inhibition of transcription by actinomycin D abolished LPA-induced IL-8 secretion in HBEpCs (results not shown). LPA-induced IL-8 secretion involving LPPs is of physiological relevance in inflammatory diseases of the airway, such as asthma and COPD. IL-8 is a powerful chemoattractant for neutrophils at sites of acute inflammation, and elevated levels of IL-8 have been reported in the bronchoalveolar lavage of patients with chronic lung disorders, including asthma, pulmonary sarcoidosis and acute respiratory distress syndrome [20–23]. Bronchoalveolar lavage from segmental allergen-challenged asthmatics had higher levels of S1P, that was associated with smooth muscle cell proliferation and IL-6 secretion [50]. Our own studies with bronchoalveolar lavage from allergen-challenged asthmatics indicate higher levels of LPA and eosinophils compared with non-allergen-challenged controls [51]. At present, the source of LPA and the mechanism(s) of LPA production in the bronchoalveolar lavage are unclear.
In summary, our findings demonstrate that LPA is a potent stimulator of IL-8 secretion, regulated in part by changes in [Ca2+]i, IκB phosphorylation and NF-κB activation, and transcriptional activation of IL-8 gene expression in HBEpCs. Our results also show that HBEpCs express LPPs, and that overexpression of LPP-1 attenuated LPA-dependent intracellular signalling upstream of IL-8 secretion. Our work therefore provides novel information that controlling the metabolism of LPA, or signalling downstream of LPA receptor activation, is able to control the release of the cytokine IL-8, and thus regulate the propagation of an inflammatory signal cascade in the lung. Hopefully this new knowledge will provide a new therapeutic target for treating inflammatory lung disease.
Acknowledgments
This work was supported in part by National Institutes of Health grant HL71152 (to V. N.) and Canadian Institute of Health Research grant MOP 10504 (to D. N. B.).
References
- 1.Tokumura A. Physiological and pathophysiological roles of lysophosphatidic acids produced by secretory lysophospholipase D in body fluids. Biochim. Biophys. Acta. 2002;1582:18–25. doi: 10.1016/s1388-1981(02)00133-6. [DOI] [PubMed] [Google Scholar]
- 2.Goetzl E. J., Dolezalova H., Kong Y., Zeng L. Dual mechanisms for lysophospholipid induction of proliferation of human breast carcinoma cells. Cancer Res. 1999;59:4732–4737. [PubMed] [Google Scholar]
- 3.Huang M. C., Graeler M., Shankar G., Spencer J., Goetzl E. J. Lysophospholipid mediators of immunity and neoplasia. Biochim. Biophys. Acta. 2002;1582:161–167. doi: 10.1016/s1388-1981(02)00151-8. [DOI] [PubMed] [Google Scholar]
- 4.Gennero I., Xuereb J., Simon M. Effects of lysophosphatidic acid on proliferation and cytosol Ca++ of human adult vascular smooth muscle cells in culture. Thromb. Res. 1999;94:317–326. doi: 10.1016/s0049-3848(99)00004-3. [DOI] [PubMed] [Google Scholar]
- 5.Jalink K., Hengeveld T., Mulder S., Postma F. R., Simon M. F., Chap H., van der Marel G. A., van Boom J. H., van Blitterswijk W. J., Moolenaar W. H. Lysophosphatidic acid-induced Ca2+ mobilization in human A431 cells: structure-activity analysis. Biochem. J. 1995;307:609–616. doi: 10.1042/bj3070609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moolenaar W. H. Lysophosphatidic acid, a multifunctional phospholipid messenger. J. Biol. Chem. 1995;270:12949–12952. doi: 10.1074/jbc.270.22.12949. [DOI] [PubMed] [Google Scholar]
- 7.Noguchi K., Ishii S., Shimizu T. Identification of p2y9/GPR23 as a novel G protein-coupled receptor for lysophosphatidic acid, structurally distant from the Edg family. J. Biol. Chem. 2003;278:25600–25606. doi: 10.1074/jbc.M302648200. [DOI] [PubMed] [Google Scholar]
- 8.Retzer M., Essler M. Lysophosphatidic acid-induced platelet shape change proceeds via Rho/Rho kinase-mediated myosin light-chain and moesin phosphorylation. Cell Signaling. 2000;12:645–648. doi: 10.1016/s0898-6568(00)00108-x. [DOI] [PubMed] [Google Scholar]
- 9.Young K. W., Bootman M. D., Channing D. R., Lipp P., Maycox P. R., Meakin J., Challiss R. A. J., Nahorski S. R. Lysophosphatidic acid-induced Ca2+ mobilization requires intracellular sphingosine 1-phosphate production. Potential involvement of endogenous EDG-4 receptors. J. Biol. Chem. 2000;275:38532–38539. doi: 10.1074/jbc.M006631200. [DOI] [PubMed] [Google Scholar]
- 10.McIntyre T. M., Pontsler A. V., Silva A. R., Hilaire A. S., Xu Y., Hinshaw J. C., Zimmerman G. A., Hama K., Aoki H., Prestwich G. D. Identification of an intracellular receptor for lysophosphatidic acid (LPA): LPA is a transcellular PPARγ agonist. Proc. Natl. Acad. Sci. U.S.A. 2003;100:131–136. doi: 10.1073/pnas.0135855100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang L., Cummings R., Zhao Y., Kazlauskas A., Sham J., Morris A., Georas S., Brindley D. N., Natarajan V. Involvement of phospholipase D2 in lysophosphatidate-induced transactivation of platelet-derived growth factor receptor-β in human bronchial epithelial cell. J. Biol. Chem. 2003;278:39931–39940. doi: 10.1074/jbc.M302896200. [DOI] [PubMed] [Google Scholar]
- 12.Bousquet J., Jeffery P. K., Busse W. W., Johnson M., Vignola A. M. Asthma from bronchoconstriction to airways inflammation and remodeling. Am. J. Respir. Crit. Care Med. 2000;161:1720–1745. doi: 10.1164/ajrccm.161.5.9903102. [DOI] [PubMed] [Google Scholar]
- 13.Toews M. L., Ediger T. L., Romberger D. J., Rennard S. I. Lysophosphatidic acid in airway function and disease. Biochim. Biophys. Acta. 2002;1582:240–250. doi: 10.1016/s1388-1981(02)00177-4. [DOI] [PubMed] [Google Scholar]
- 14.Cummings R. J., Parinandi N. L., Zaiman A., Wang L., Usatyuk P. V., Garcia J. G. N., Natarajan V. Phospholipase D activation by sphingosine-1-phosphate regulates interleukin-8 secretion in human bronchial epithelial cells. J. Biol. Chem. 2002;277:30227–30235. doi: 10.1074/jbc.M111078200. [DOI] [PubMed] [Google Scholar]
- 15.Wang L., Cummings R., Usatyuk P., Morris A., Irani K., Natarajan V. Involvement of phospholipases D1 and D2 in sphingosine 1-phosphate-induced ERK (extracellular-signal-regulated kinase) activation and interleukin-8 secretion in human bronchial epithelial cells. Biochem. J. 2002;367:751–760. doi: 10.1042/BJ20020586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang X., Yu S., Bast R. C., Liu S., Xu H., Hu S., LaPushin R., Claret F. X., Aggarwal B. B., Lu Y., Mills G. B. Mechanisms for lysophosphatidic acid-induced cytokine production in ovarian cancer cells. J. Biol. Chem. 2004;279:9653–9661. doi: 10.1074/jbc.M306662200. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz B. M., Hong G., Morrison B. H., Wu W., Baudhuin L. M., Xiao Y., Mok S. C., Xu Y. Lysophospholipids increase interleukin-8 expression in ovarian cancer cells. Gynecol. Oncol. 2001;81:291–300. doi: 10.1006/gyno.2001.6124. [DOI] [PubMed] [Google Scholar]
- 18.Palmetshofer A., Robson S. C., Nehls V. Lysophosphatidic acid activates nuclear factor kappa B and induces proinflammatory gene expression in endothelial cells. Thromb. Haemostasis. 1999;82:1532–1537. [PubMed] [Google Scholar]
- 19.Shida D., Kitayama J., Yamaguchi H., Okaji Y., Tsuno N. H., Watanabe T., Takuwa Y., Nagawa H. Lysophosphatidic acid (LPA) enhances the metastatic potential of human colon carcinoma DLD1 cells through LPA1. Cancer Res. 2003;63:1706–1711. [PubMed] [Google Scholar]
- 20.Baggiolini M., Walz A., Kunkel S. L. Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J. Clin. Invest. 1989;84:1045–1049. doi: 10.1172/JCI114265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huber A. R., Kunkel S. L., Todd R. F. D., Weiss S. J. Regulation of transendothelial neutrophil migration by endogenous interleukin-8. Science. 1991;254:99–102. doi: 10.1126/science.1718038. [DOI] [PubMed] [Google Scholar]
- 22.Strieter R. M. Interleukin-8: a very important chemokine of the human airway epithelium. Am. J. Physiol. Lung Cell Mol. Physiol. 2002;283:L688–L689. doi: 10.1152/ajplung.00146.2002. [DOI] [PubMed] [Google Scholar]
- 23.Albelda S. M., Smith C. W., Ward P. A. Adhesion molecules and inflammatory injury. FASEB J. 1994;8:504–512. [PubMed] [Google Scholar]
- 24.Brasier A. R., Jamaluddin M., Casola A., Wang D., Shen Q., Garofalo R. P. A promoter recruitment mechanism for tumor necrosis factor-α-induced interleukin-8 transcripiton in type II pulmonary epithelial cells. J. Biol. Chem. 1998;273:3551–3561. doi: 10.1074/jbc.273.6.3551. [DOI] [PubMed] [Google Scholar]
- 25.Hooks S. B., Ragan S. P., Lynch K. R. Identification of a novel human phosphatidic acid phosphatase type 2 isoform. FEBS Lett. 1998;427:188–192. doi: 10.1016/s0014-5793(98)00421-9. [DOI] [PubMed] [Google Scholar]
- 26.Kai M., Wada I., Imai S., Sakane F., Kanoh H. Cloning and characterization of two human isoenzymes of Mg2+-independent phosphatidic acid phosphatase. J. Biol. Chem. 1997;272:24572–24578. doi: 10.1074/jbc.272.39.24572. [DOI] [PubMed] [Google Scholar]
- 27.Roberts R., Sciorra V. A., Morris A. J. Human type 2 phosphatidic acid phosphohydrolases. Substrate specificity of the type 2a, 2b, and 2c enzymes and cell surface activity of the 2a isoform. J. Biol. Chem. 1998;273:22059–22067. doi: 10.1074/jbc.273.34.22059. [DOI] [PubMed] [Google Scholar]
- 28.Stunff H. L., Peterson C., Thornton R., Milstien S., Mandala S. M., Spiegel S. Characterization of murine sphingosine-1-phosphate phosphohydrolase. J. Biol. Chem. 2002;277:8920–8927. doi: 10.1074/jbc.M109968200. [DOI] [PubMed] [Google Scholar]
- 29.Brindley D. N., English D., Pilquil C., Buri K., Ling Z. Lipid phosphate phosphatases regulate signal transduction through glycerolipids and sphingolipids. Biochim. Biophys. Acta. 2002;1582:33–44. doi: 10.1016/s1388-1981(02)00135-x. [DOI] [PubMed] [Google Scholar]
- 30.Ishikawa T., Kai M., Wada I., Kanoh H. Cell surface activities of human type 2 phosphatidic acid phosphatase. J. Biochem. (Tokyo) 2000;127:645–651. doi: 10.1093/oxfordjournals.jbchem.a022652. [DOI] [PubMed] [Google Scholar]
- 31.Sciorra V. A., Morris A. J. Roles of lipid phosphate phosphatases in regulation of cellular signaling. Biochim. Biophys. Acta. 2002;1582:45–51. doi: 10.1016/s1388-1981(02)00136-1. [DOI] [PubMed] [Google Scholar]
- 32.Alderton F., Darroch P., Sambi B., McKie A., Ahmed I. S., Pyne N., Pyne S. G-protein coupled receptor stimulation of p42/p44 mitogen activated protein kinase pathway is attenuated by lipid phosphatase 1, 1a, and 2 in HEK 293 cells. J. Biol. Chem. 2001;276:13452–13460. doi: 10.1074/jbc.M006582200. [DOI] [PubMed] [Google Scholar]
- 33.Pilquil C., Singh I., Zhang Q., Ling Z., Buri K., Stromberg L. M., Dewald J., Brindley D. N. Lipid phosphate phosphatase-1 dephosphorylates exogenous lysophosphatidate and thereby attenuates its effects on cell signaling. Prostagladins Other Lipid Mediators. 2001;64:83–92. doi: 10.1016/s0090-6980(01)00101-0. [DOI] [PubMed] [Google Scholar]
- 34.Tanyi J. L., Hasegawa Y., Lapushin R., Morris A. J., Wolf J. K., Berchuck A., Lu K., Smith D. I., Kalli K., Hartmann L. C., et al. Role of decreased levels of lipid phosphate phosphatase-1 in accumulation of lysophosphatidic acid in ovarian cancer. Clin. Cancer Res. 2003;9:3534–3545. [PubMed] [Google Scholar]
- 35.Tanyi J. L., Morris A. J., Wolf J. K., Fang X., Hasegawa Y., Lapushin R., Auersperg N., Sigal Y. J., Newman R. A., Felix E. A., et al. The human lipid phosphate phosphatase-3 decreases the growth, survival, and tumorigenesis of ovarian cancer cells: validation of the lysophosphatidic acid signaling cascade as a target for therapy in ovarian cancer. Cancer Res. 2003;63:1073–1082. [PubMed] [Google Scholar]
- 36.Humtsoe J. O., Feng S., Thakker G. D., Yang J., Hong J., Wary K. K. Regulation of cell-cell interactions by phosphatidic acid phosphatase 2b/VCIP. EMBO J. 2003;22:1539–1554. doi: 10.1093/emboj/cdg165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Escalante-Alcalde D., Hernandez L., Stunff H. L., Maeda R., Lee H., Cheng J. G., Sciorra V. A., Daar I., Spiegel S., Morris A. J., Stewart C. L. The lipid phosphatase LPP3 regulates extra-embryonic vasculogenesis and axis patterning. Development. 2003;130:4623–4637. doi: 10.1242/dev.00635. [DOI] [PubMed] [Google Scholar]
- 38.Bernacki S. H., Nelson A. L., Abdullah L., Sheehan J. K., Harris A., Davis C. W., Randell S. H. Mucin gene expression during differentiation of human airway epithelia in vitro. Muc4 and muc5b are strongly induced. Am. J. Respir. Cell Mol. Biol. 1999;20:595–604. doi: 10.1165/ajrcmb.20.4.3442. [DOI] [PubMed] [Google Scholar]
- 39.Usatyuk P. V., Fomin V. P., Shi S., Garcia J. G., Schaphorst K., Natarajan V. Role of Ca2+ in diperoxovanadate-induced cytoskeletal remodeling and endothelial cell barrier function. Am. J. Physiol. Lung Cell. Mol. Physiol. 2003;285:L1006–L1017. doi: 10.1152/ajplung.00408.2002. [DOI] [PubMed] [Google Scholar]
- 40.Luquain C., Singh A., Wang L., Natarajan V., Morris A. J. Role of phospholipase D in agonist-stimulated lysophosphatidic acid synthesis by ovarian cancer cells. J. Lipid Res. 2003;44:1963–1975. doi: 10.1194/jlr.M300188-JLR200. [DOI] [PubMed] [Google Scholar]
- 41.Smyth S. S., Sciorra V. A., Sigal Y. J., Pamulkar Z., Wang Z., Xu Y., Prestwich G. D., Morris A. J. Lipid phosphate phosphatases regulate lysophosphatidic acid production and signaling in platelets: studies using chemical inhibitors of lipid phosphate phosphatase activity. J. Biol. Chem. 2003;278:43214–43223. doi: 10.1074/jbc.M306709200. [DOI] [PubMed] [Google Scholar]
- 42.Jasinska R., Zhang Q. X., Pilquil C. S., Singh I., Xu J., Dewald J., Dillon D. A., Berthiaume L. G., Carman G. M., Waggoner D. W., Brindley D. N. Lipid phosphate phosphohydrolase-1 degrades exogenous glycerolipid and sphingolipid phosphate esters. Biochem. J. 1999;340:677–686. [PMC free article] [PubMed] [Google Scholar]
- 43.Cummings R., Zhao Y., Jacoby D., Spannhake E. W., Ohba M., Garcia J. G. N., Watkins T., He D., Saatian B., Natarajan V. Protein kinase Cδ mediates lysophosphatidic acid-induced NF-κB activation and interleukin-8 secretion in human bronchial epithelial cells. J. Biol. Chem. 2004;279:41085–41094. doi: 10.1074/jbc.M404045200. [DOI] [PubMed] [Google Scholar]
- 44.Hasegawa Y., Erickson J. R., Goddard G. J., Yu S., Liu S., Cheng K. W., Eder A., Bandoh K., Aoki J., Jarosz R., et al. Identification of a phosphothionate analogue of lysophosphatidic acid (LPA) as a selective agonist of the LPA3 receptor. J. Biol. Chem. 2003;278:11962–11969. doi: 10.1074/jbc.M209168200. [DOI] [PubMed] [Google Scholar]
- 45.Qian L., Xu Y., Hasegawa Y., Aoki J., Mills G. B., Prestwich G. D. Enantioselective responses to a phosphorothioate analogue of lysophosphatidic acid with LPA3 receptor-selective agonist activity. J. Med. Chem. 2003;46:5575–5578. doi: 10.1021/jm034207p. [DOI] [PubMed] [Google Scholar]
- 46.Ogawa C., Kihara A., Gokoh M., Igarashi Y. Identification and characterization of a novel human sphingosine-1-phosphate phosphohydrolase, hSPP2. J. Biol. Chem. 2003;278:1268–1272. doi: 10.1074/jbc.M209514200. [DOI] [PubMed] [Google Scholar]
- 47.Burnett C., Howard K. Fly and mammalian lipid phosphate phosphatase isoforms differ in activity both in vitro and in vivo. EMBO Rep. 2003;4:793–799. doi: 10.1038/sj.embor.embor900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yue J., Yokoyama K., Balazs L., Baker D. L., Smalley D., Pilquil C., Brindley D. N., Tigyi G. Mice with transgenic overexpression of lipid phosphate phosphatase-1 display multiple organotypic deficits without alteration in circulating lysophosphatidate level. Cell Sigalling. 2004;16:385–399. doi: 10.1016/j.cellsig.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 49.Zhang N., Sundberg J. P., Gridley T. Mice mutant for Ppap2c, a homolog of the germ cell migration regulator Wunen, are viable and fertile. Genesis. 2000;27:137–140. doi: 10.1002/1526-968x(200008)27:4<137::aid-gene10>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 50.Ammit A. J., Hastie A. T., Edsall L. C., Hoffman R. K., Amrani Y., Krymskaya V. P., Kane S. A., Peters S. P., Penn R. B., Spiegel S., Panettieri R. A. Sphingosine 1-phosphate modulates human airway smooth muscle cell functions that promote inflammation and airway remodeling in asthma. FASEB J. 2001;15:1212–1214. doi: 10.1096/fj.00-0742fje. [DOI] [PubMed] [Google Scholar]
- 51.Georas S., Liu M., Cummings R., Chen R., Morris A., Berdyshev E., Natarajan V. Lysophosphatidic acid (LPA) levels and LPA-receptor signaling in airway inflammation and asthma. Am. J. Respir. Crit. Care Med. 2004;169:A569. [Google Scholar]