Abstract
Background
Blood neurofilament light chain (NfL) is increasingly considered as a key trial biomarker in genetic frontotemporal dementia (gFTD). We aimed to facilitate the use of NfL in gFTD multicentre trials by testing its (1) reliability across labs; (2) reliability to stratify gFTD disease stages; (3) comparability between blood matrices and (4) stability across recruiting sites.
Methods
Comparative analysis of blood NfL levels in a large gFTD cohort (GENFI) for (1)–(4), with n=344 samples (n=148 presymptomatic, n=11 converter, n=46 symptomatic subjects, with mutations in C9orf72, GRN or MAPT; and n=139 within-family controls), each measured in three different international labs by Simoa HD-1 analyzer.
Results
NfL revealed an excellent consistency (intraclass correlation coefficient (ICC) 0.964) and high reliability across the three labs (maximal bias (pg/mL) in Bland-Altman analysis: 1.12±1.20). High concordance of NfL across laboratories was moreover reflected by high areas under the curve for discriminating conversion stage against the (non-converting) presymptomatic stage across all three labs. Serum and plasma NfL were largely comparable (ICC 0.967). The robustness of NfL across 13 recruiting sites was demonstrated by a linear mixed effect model.
Conclusions
Our results underline the suitability of blood NfL in gFTD multicentre trials, including cross-lab reliable stratification of the highly trial-relevant conversion stage, matrix comparability and cross-site robustness.
Keywords: COGNITION, FRONTOTEMPORAL DEMENTIA, NEUROPSYCHIATRY
Introduction
Genetic frontotemporal dementias (gFTDs) represent a group of progressive neurodegenerative diseases characterised by a progressive decline of executive, behavioural and language functions, frequently resulting from mutations in the genes chromosome open reading frame 72 (C9orf72), progranulin (GRN) or microtubule-associated protein tau (MAPT).1 Neurofilament light chain (NfL)—an intermediate filament that constitutes part of the neuronal cytoskeleton—is released after neuronal damage into the interstitial fluid, cerebrospinal fluid and blood. Blood-based NfL has an increasing impact as a trial biomarker in gFTD for multiple contexts of use, for example, patient stratification,2–5 trial inclusion,6 toxicity monitoring and treatment-response capture,7 and has now been approved by the U.S. Food and Drug Administration as a surrogate endpoint contributing to approval of novel drugs (tofersen).8 However, its wider use in multicentre trials—as well as in real-world clinical settings—has been questioned due to potential cross-laboratory heterogeneity in analytical approaches and blood sample matrices that might lead to different, non-comparable concentrations of blood NfL.9 10
Leveraging a large gFTD cohort, we here aimed to facilitate the use of blood NfL in gFTD multicentre trials and real-world clinical settings by testing: (1) its reliability across laboratories, measured at different time points, by different end-user devices and kits; (2) cut-off values maximising stratification accuracy of the trial relevant gFTD disease stages (conversion stage, symptomatic stage), with cut-off values validated across labs; (3) comparability between blood matrices and (4) robustness across recruiting sites.
Methods
Cohort and NFL measurements
Subjects were patients with FTD caused by mutations in the genes C9orf72, GRN or MAPT (symptomatic mutation carriers), and their respective first-degree relatives (ie, either presymptomatic mutation carriers or noncarriers serving as within-family controls), recruited by the international Genetic FTD Initiative (GENFI; www.genfi.org.uk)11 at 13 sites. The comparative analysis included n=344 blood samples (n=148 from presymptomatic carriers; n=11 from carriers that converted during the observation period; n=46 from symptomatic carriers; n=139 from within-family-controls; for characteristics of these subcohorts, see online supplemental table 1 that were independently measured for NfL levels by Single molecule array (Simoa; HD-1 analyzer, Quanterix, Billerica, Massachusetts, USA) in three different laboratories (lab 1: Basel, Switzerland5; lab 2: Rotterdam, the Netherlands4; lab 3: London, UK2), using different NfL kits (Basel and Rotterdam: NF-Light Advantage Kit 103186 (V.1); London: Neurology 4-Plex A Kit 102153), according to the manufacturer’s instructions. The blood matrices for NfL analysis were serum (Basel and Rotterdam) and plasma (London). Further methodological details of NfL measurements, details of the GENFI protocol, participant demographics, clinical classification of the disease stages (ie, presymptomatic carriers, converters, symptomatic carriers) as well as NfL quantification were described elsewhere.2 4 5 11
jnnp-2023-332464supp001.pdf (439.9KB, pdf)
Statistical analyses
SPSS for Windows V.29.0 (IBM), Sigmaplot for Windows V.15 (Inpixion, Germany) and RStudio 2022.07.2 were used for statistical analyses. NfL values were not normally distributed and therefore log-transformed. For age-corrected z-scores—taking into consideration the age-related NfL increase observed in controls—log-transformed NfL values were normalised relative to their distribution in controls.5 The consistency of NfL measurements across the three different labs was quantified by intraclass correlation coefficients (ICC; two-way mixed effect model, single measures, absolute agreement12). Bland-Altman analyses13 were used to quantify between-lab bias, defined as the mean of the differences; limits of agreement, that is, the mean of the bias±1.96 times the SD of the differences; and 95% CIs for the bias with lower and upper limits of agreement. The diagnostic performance of NfL was assessed by receiver operating characteristic (ROC) analysis14 and calculating areas under the curve (AUCs), as well as optimal operating points, that is, cut-off values (assuming a cost ratio of 1 and a pretest probability of 0.5), maximising stratification accuracy for different gFTD disease stages. The predictive value for an NfL-based disease stage stratification was addressed by calculating positive and negative likelihood ratios (LR+ and LR−).15 Linear mixed effect models were used to characterise the stability of log-transformed NfL levels across recruiting sites (with categorial factors of disease stage and genetic status, and metric covariate of age as fixed effects).
Results
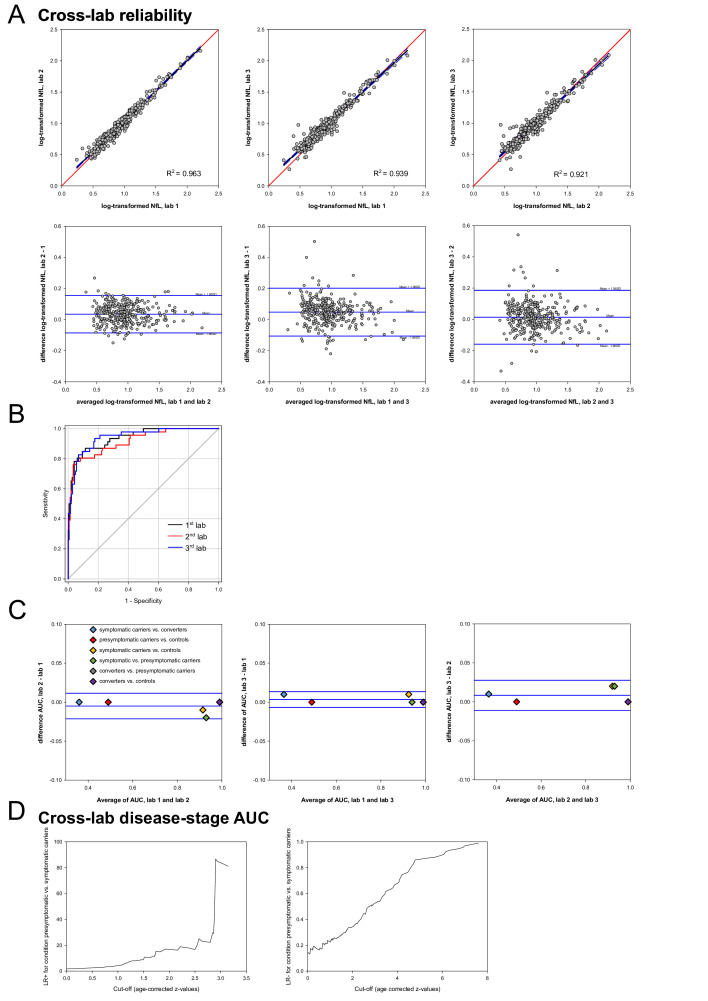
NfL levels showed an excellent consistency across the three labs (ICC 0.964, 95% CI lower to upper limit 0.946 to 0.974), as demonstrated by a two-way mixed effect model. Reliability of NfL levels was high and bias was low across all three labs, as shown by linear regressions and Bland-Altman analyses with a maximal bias±SD of 1.12 pg/mL±1.20 (for summary, see figure 1A). The performance of blood NfL to serve as a disease stage stratification biomarker in gFTD was investigated by ROC curve analyses and calculation of optimal cut-off values maximising stratification accuracy for different gFTD disease stages. Blood NfL allowed discrimination of conditions (1) symptomatic carriers versus controls (AUC: 0.91; cut-off, given as z-value: 2.83), (2) converters versus controls (AUC: 0.89; cut-off z: 3.05), (3) converters versus presymptomatic carriers (AUC: 0.86; cut-off z: 3.19) and (4) symptomatic versus presymptomatic carriers (AUC: 0.88; cut-off z 3.20). NfL did not allow a discrimination of (5) presymptomatic carriers versus controls (AUC: 0.57) or (6) symptomatic carriers versus converters (AUC: 0.59), with AUCs close to the random classifier level (for detailed results, see table 1). Concordance of AUCs across the three labs for all comparisons was high (maximum difference±SE 0.02±0.01), as exemplified in figure 1B for the discrimination of symptomatic vs presymptomatic carriers (lab 1 AUC±SE 0.94±0.02, 95% CI 0.90 to 0.98; lab 2 AUC±SE 0.92±0.02, 95% CI 0.86 to 0.96; lab 3 AUC±SE 0.94±0.02, 95% CI 0.91 to 0.98)). The high reliability of AUC across labs for all disease stage comparisons was further corroborated by Bland-Altman analysis (see figure 1C), with a maximal bias of 0.01±0.01 (AUC±SD). For a genotype-specific analysis (C9orf72, MAPT, GRN) of NfL cross-lab reliability and disease-stage AUC, see online supplemental figures 1,2 and online supplemental tables 3,4.
Figure 1.
Cross-lab reliability, cross-lab disease-stage cut-offs and likelihood ratios (LR) and blood matrix comparability in genetic FTD. (A) Reliability of blood NfL measurements in genetic FTD (gFTD) across three labs (lab 1 and 2 serum, lab 3 plasma)—linear regressions and Bland-Altman analyses of log-transformed NfL values. For detailed statistics, see online supplemental table 2. (B) Comparative across-lab analysis of ROC curves and AUC values for the condition ‘presymptomatic versus symptomatic carriers’. Detailed values of AUC±SE and 95% CI are given in the Results section. (C) Reliability of AUC values across three labs—Bland-Altman analyses for all stage comparisons. For detailed statistics, see online supplemental table 2. (D) Prediction of individual risk factors at different cut-offs for the condition ‘presymptomatic versus symptomatic carriers’ (age-corrected z-values, first lab) by positive (LR+) and negative (LR−). AUC, area under the curve; FTD, frontotemporal dementia; NfL, neurofilament light chain; ROC receiver operating characteristic
Table 1.
Receiver operating characteristic (ROC) curve analysis with areas under the curve (AUC) and optimal cut-offs for separating different gFTD stages and conditions
| gFTD conditions | AUC | SE | Optimal cut-off | ||
| z-value | Specificity (%) | Sensitivity (%) | |||
| Symptomatic carriers versus controls | 0.91 | 0.02 | 2.83 | 100 | 49.5 |
| Converters versus controls | 0.89 | 0.07 | 3.05 | 100 | 42.9 |
| Converters versus presymptomatic carriers | 0.86 | 0.08 | 3.19 | 100 | 42.9 |
| Symptomatic versus presymptomatic carriers | 0.88 | 0.02 | 3.20 | 100 | 46.2 |
| Presymptomatic carriers versus controls | 0.57 | 0.03 | |||
| Symptomatic carriers versus converters | 0.59 | 0.10 | |||
Data from lab 1; optimal cut-off values are given as z-values (corrected for age). For the data from lab 2 and 3, see figure 1B and C.
gFTD, genetic frontotemporal dementia.
The disease stage-specific stratification value of NfL levels—beyond dichotomising cut-offs—was demonstrated by LR (see figure 1D). For exemplary illustration of the individual risk prediction of being presymptomatic versus symptomatic carrier at different NfL levels by LR+ and LR− see figure 1C (NfL values from lab 1). An NfL z-value of 3 corresponded to an LR+ of 83 and an LR− of 0.5.
NfL values in serum and plasma (n=344 samples of each matrix) were largely comparable (ICC 0.967, 95% CI lower to upper 0.894 to 0.977), as calculated by a two-way mixed effect model. The median ratio serum/plasma was 0.95.
The high robustness of NfL across 13 recruiting sites was shown by a linear mixed effect model, as the categorial variable ‘recruiting site’ did not explain any variance (estimate 0.001, SE 0.001, Wald-Z 1.403, significance 0.161).
Discussion
Blood NfL has an increasing impact as a trial biomarker in gFTD for multiple contexts of use5 7 and is now being increasingly acknowledged by the FDA as a surrogate endpoints in drug approval processes.8 However, its wider use in multicentre trials and real-world clinical settings is limited by lack of larger data demonstrating cross-lab reliability, cross-lab validated cut-off values and cross-lab validated comparability between blood matrices in gFTD. Leveraging a large genetic FTD, our findings show that blood NfL is a biomarker in gFTD with high reliability across labs—even if assessed at different time points, and by partly different kits (NF-Light Advantage Kit vs Neurology 4-Plex A Kit). This finding confirms and extends earlier findings showing a good cross-lab reliability of blood NfL, which so far, however, has been limited to smaller sample sets and non-gFTD cohorts.16 Given, however, that all three labs in our study still used the same type of platform (Simoa HD-1), future studies need to investigate a potential decrease in cross-lab reliability if different measurement platforms are being used for blood NfL (eg, Ella,17 Uman,18 Atellica19). A pilot study on this showed promising results.20
Reliable cut-off values of blood NfL for accurately stratifying different gFTD disease stages are key for its use as a molecular stratification marker of gFTD subjects into treatment trials.3 5 7 In particular, reliable blood-based stratification of subjects close to conversion to the symptomatic phase of the disease will be of extremely high value to identify and recruit subjects into upcoming mechanistic treatment trials tailored to prevent neurodegeneration by early intervention.5 21 Extending earlier findings on blood NfL cut-offs in gFTD,3 our findings now indicate that these cut-off values can be provided by blood NfL for gFTD even with a high reliability across labs. In addition, they also show that NfL levels in converting carriers are already more similar to symptomatic carriers than (non-converting) presymptomatic carriers. Nevertheless, in the absence of a certified reference material, value assigned by a certified reference method, the reported cut-offs remain preliminary and prospective laboratory-specific validation remains required.
Multicentre use of blood NfL—whether in trials or real-world clinical settings—is inherently characterised by cross-centre variability in preanalytical sample handling. Our data from a large set of different sites (n=13) suggest that this variability might not exert a substantial effect on multicentre blood NfL values—even despite the fact that no strictly enforced cross-centre harmonised standard operating procedure or centralised biosampling monitoring had been employed across centres. These data corroborate blood NfL as a very stable biomarker that is resistant to most types of clinically relevant variation in preanalytical sample handling.22 Future studies with larger sample batches per centre and testing more extreme variabilities in preanalytical sample handling are warranted to further investigate and specify the limits of this cross-centre comparability.
Real-world clinical multicentre use of blood NfL moreover often faces the challenge that samples come from different blood matrices (eg, serum vs plasma).9 While our findings confirm differences in the absolute blood NfL concentrations between serum and plasma, they at the same time show a high consistency between both blood matrices, allowing comparability of both matrices. The calculated median ratio serum/plasma might be a first coarse help when comparing results derived from these different matrices. However, its use might be limited to Simoa-based blood NfL measurements, and further larger in-depth studies in independent cohorts are required to confirm this factor.
Our study has several limitations. First, although leveraging the largest gFTD cohort existing so far, the sample size is partly limited by the requirement to measure each sample in three labs, leading to limited sample sizes in particular for some gFTD subcohorts (eg, converters). Second, the construct and wording of ‘cut-offs’ suggest a separating dichotomy where in fact a biological continuum of NfL levels and disease progression exists.
Despite these limitations, our results underline the suitability of blood NfL as a fit-for-purpose biomarker in gFTD multicentre trials.
Acknowledgments
The authors thank the participants in the GENFI study.
Footnotes
@HarroSeelaar, @sducharme66
Collaborators: Annabel Nelson Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UKMartina Bocchetta Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UKDavid Cash Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UKDavid L Thomas Neuroimaging Analysis Centre, Department of Brain Repair and Rehabilitation, UCL Institute of Neurology, Queen Square, London, UKEmily Todd Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UKHanya Benotmane UK Dementia Research Institute at University College London, UCL Queen Square Institute of Neurology, London, UKJennifer Nicholas Department of Medical Statistics, London School of Hygiene and Tropical Medicine, London, UKKiran Samra Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UKRachelle Shafei Department of Neurodegenerative Disease, Dementia Research Centre, UCL Queen Square Institute of Neurology, London, UKCarolyn Timberlake Department of Clinical Neurosciences, University of Cambridge, Cambridge, UKThomas Cope Department of Clinical Neuroscience, University of Cambridge, Cambridge, UKTimothy Rittman Department of Clinical Neurosciences, University of Cambridge, Cambridge, UKAntonella Alberici Centre for Neurodegenerative Disorders, University of Brescia, Brescia, ItalyEnrico Premi Stroke Unit, ASST Brescia Hospital, Brescia, ItalyRoberto Gasparotti Neuroradiology Unit, University of Brescia, Brescia, ItalyValentina Cantoni Centre for Neurodegenerative Disorders, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, ItalyEmanuele Buratti ICGEB, Trieste, ItalyAndrea Arighi Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, ItalyChiara Fenoglio Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, ItalyElio Scarpini Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, ItalyGiorgio Fumagalli Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, ItalyVittoria Borracci Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Neurodegenerative Diseases Unit, Milan, Italy; University of Milan, Centro Dino Ferrari, Milan, ItalyGiacomina Rossi Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalyGiorgio Giaccone Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalyGiuseppe Di Fede Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalyPaola Caroppo Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalyPietro Tiraboschi Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalySara Prioni Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalyVeronica Redaelli Fondazione IRCCS Istituto Neurologico Carlo Besta, Milano, ItalyDavid Tang-Wai The University Health Network, Krembil Research Institute, Toronto, CanadaEkaterina Rogaeva Tanz Centre for Research in Neurodegenerative Diseases, University of Toronto, Toronto, CanadaMiguel Castelo-Branco Faculty of Medicine, University of Coimbra, Coimbra, PortugalMorris Freedman Baycrest Health Sciences, Rotman Research Institute, University of Toronto, Toronto, CanadaRon Keren The University Health Network, Toronto Rehabilitation Institute, Toronto, CanadaSandra Black Sunnybrook Health Sciences Centre, Sunnybrook Research Institute, University of Toronto, Toronto, CanadaSara Mitchell Sunnybrook Health Sciences Centre, Sunnybrook Research Institute, University of Toronto, Toronto, CanadaChristen Shoesmith Department of Clinical Neurological Sciences, University of Western Ontario, London, Ontario, CanadaRobart Bartha Department of Medical Biophysics, The University of Western Ontario, London, Ontario, Canada; Centre for Functional and Metabolic Mapping, Robarts Research Institute, The University of Western Ontario, London, Ontario, CanadaRosa Rademakers Center for Molecular Neurology, University of AntwerpJackie Poos Department of Neurology, Erasmus Medical Center, Rotterdam, NetherlandsJanne M. Papma Department of Neurology, Erasmus Medical Center, Rotterdam, NetherlandsLucia Giannini Department of Neurology, Erasmus Medical Center, Rotterdam, NetherlandsRick van Minkelen Department of Clinical Genetics, Erasmus Medical Center, Rotterdam, NetherlandsYolande Pijnenburg Amsterdam University Medical Centre, Amsterdam VUmc, Amsterdam, NetherlandsBenedetta Nacmias Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, ItalyCamilla Ferrari Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, ItalyCristina Polito Department of Biomedical, Experimental and Clinical Sciences “Mario Serio”, Nuclear Medicine Unit, University of Florence, Florence, ItalyGemma Lombardi Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, ItalyValentina Bessi Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, ItalyMichele Veldsman Nuffield Department of Clinical Neurosciences, Medical Sciences Division, University of Oxford, Oxford, UKChristin Andersson Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, SwedenHakan Thonberg Center for Alzheimer Research, Division of Neurogeriatrics, Karolinska Institutet, Stockholm, SwedenLinn Öijerstedt Center for Alzheimer Research, Division of Neurogeriatrics, Department of Neurobiology, Care Sciences and Society, Bioclinicum, Karolinska Institutet, Solna, Sweden; Unit for Hereditary Dementias, Theme Aging, Karolinska University Hospital, Solna, SwedenVesna Jelic Division of Clinical Geriatrics, Karolinska Institutet, Stockholm, SwedenPaul Thompson Division of Neuroscience and Experimental Psychology, Wolfson Molecular Imaging Centre, University of Manchester, Manchester, UKTobias Langheinrich Division of Neuroscience and Experimental Psychology, Wolfson Molecular Imaging Centre, University of Manchester, Manchester, UK; Manchester Centre for Clinical Neurosciences, Department of Neurology, Salford Royal NHS Foundation Trust, Manchester, UKAlbert Lladó Alzheimer’s disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, SpainAnna Antonell Alzheimer’s disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, SpainJaume Olives Alzheimer’s disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, SpainMircea Balasa Alzheimer’s disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, SpainNuria Bargalló Imaging Diagnostic Center, Hospital Clínic, Barcelona, SpainSergi Borrego-Ecija Alzheimer’s disease and Other Cognitive Disorders Unit, Neurology Service, Hospital Clínic, Barcelona, SpainAna Verdelho Department of Neurosciences and Mental Health, Centro Hospitalar Lisboa Norte - Hospital de Santa Maria Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, SpainAna Gorostidi Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, SpainJorge Villanua OSATEK, University of Donostia, San Sebastian, Gipuzkoa, SpainMarta Cañada CITA Alzheimer, San Sebastian, Gipuzkoa, SpainMikel Tainta Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, SpainMiren Zulaica Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, SpainMyriam Barandiaran Cognitive Disorders Unit, Department of Neurology, Donostia University Hospital, San Sebastian, Gipuzkoa, Spain; Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, SpainPatricia Alves Neuroscience Area, Biodonostia Health Research Insitute, San Sebastian, Gipuzkoa, Spain; Department of Educational Psychology and Psychobiology, Faculty of Education, International University of La Rioja, Logroño, SpainBenjamin Bender Department of Diagnostic and Interventional Neuroradiology, University of Tübingen, Tübingen, GermanyLisa Graf Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research and Center of Neurology, University of Tübingen, Tübingen, GermanyAnnick Vogels Department of Human Genetics, KU Leuven, Leuven, BelgiumMathieu Vandenbulcke Geriatric Psychiatry Service, University Hospitals Leuven, Belgium; Neuropsychiatry, Department of Neurosciences, KU Leuven, Leuven, BelgiumPhilip Van Damme Neurology Service, University Hospitals Leuven, Belgium; Laboratory for Neurobiology, VIB-KU Leuven Centre for Brain Research, Leuven, BelgiumRose Bruffaerts Department of Biomedical Sciences, University of Antwerp, Antwerp, Belgium; Biomedical Research Institute, Hasselt University, 3500 Hasselt, BelgiumKoen Poesen Laboratory for Molecular Neurobiomarker Research, KU Leuven, Leuven, BelgiumPedro Rosa-Neto Translational Neuroimaging Laboratory, McGill Centre for Studies in Aging, McGill University, Montreal, Québec, CanadaSerge Gauthier Alzheimer Disease Research Unit, McGill Centre for Studies in Aging, Department of Neurology Reference Network for Rare Neurological Diseases (ERN-RND)Anne Bertrand Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP - Hôpital Pitié-Salpêtrière, Paris, France; Inria, Aramis project-team, F-75013, Paris, France; Centre pour l’Acquisition et le Traitement des Images, Institut du Cerveau et la Moelle, Paris, FranceAurélie Funkiewiez Centre de référence des démences rares ou précoces, IM2A, Département de Neurologie, AP-HP - Hôpital Pitié-Salpêtrière, Paris, France; Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP - Hôpital Pitié-Salpêtrière, Paris, FranceDaisy Rinaldi Centre de référence des démences rares ou précoces, IM2A, Département de Neurologie, AP-HP - Hôpital Pitié-Salpêtrière, Paris, France; Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP - Hôpital Pitié-Salpêtrière, Paris, France; Département de Neurologie, AP-HP - Hôpital Pitié-Salpêtrière, Paris, FranceDario Saracino Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP - Hôpital Pitié-Salpêtrière, Paris, France; Inria, Aramis project-team, F-75013, Paris, France; Centre de référence des démences rares ou précoces, IM2A, Département de Neurologie, AP-HP - Hôpital Pitié-Salpêtrière, Paris, FranceOlivier Colliot Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP - Hôpital Pitié-Salpêtrière, Paris, France; Inria, Aramis project-team, F-75013, Paris, France; Centre pour l’Acquisition et le Traitement des Images, Institut du Cerveau et la Moelle, Paris, FranceSabrina Sayah Sorbonne Université, Paris Brain Institute – Institut du Cerveau – ICM, Inserm U1127, CNRS UMR 7225, AP-HP - Hôpital Pitié-Salpêtrière, Paris, FranceCatharina Prix Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, GermanyElisabeth Wlasich Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, GermanyOlivia Wagemann Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, GermanySandra Loosli Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, GermanySonja Schönecker Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, GermanyTobias Hoegen Neurologische Klinik, Ludwig-Maximilians-Universität München, Munich, GermanyJolina Lombardi Department of Neurology, University of Ulm, UlmSarah Anderl-Straub Department of Neurology, University of Ulm, Ulm, GermanyAdeline Rollin CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, FranceGregory Kuchcinski Univ Lille, France; Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, FranceMaxime Bertoux Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, FranceThibaud Lebouvier Univ Lille, France; Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, FranceVincent Deramecourt Univ Lille, France; Inserm 1172, Lille, France; CHU, CNR-MAJ, Labex Distalz, LiCEND Lille, FranceBeatriz Santiago Neurology Department, Centro Hospitalar e Universitario de Coimbra, Coimbra, PortugalDiana Duro Faculty of Medicine, University of Coimbra, Coimbra, PortugalMaria João Leitão Centre of Neurosciences and Cell Biology, Universidade de Coimbra, Coimbra, PortugalMaria Rosario Almeida Faculty of Medicine, University of Coimbra, Coimbra, PortugalMiguel Tábuas-Pereira Neurology Department, Centro Hospitalar e Universitario de Coimbra, Coimbra, PortugalSónia Afonso Instituto Ciencias Nucleares Aplicadas a Saude, Universidade de Coimbra, Coimbra, Portugal.
Contributors: CL, CW, DM and MS contributed to the conception and design of the study. All authors contributed to the acquisition and analysis of data. CL and MS contributed to drafting the manuscript.
Funding: JCVS was supported by the Dioraphte Foundation grant 09-02-03-00, Association for Frontotemporal Dementias Research Grant 2009, Netherlands Organization for Scientific Research grant HCMI 056-13-018, ZonMw Memorabel (Deltaplan Dementie, project number 733051042), Alzheimer Nederland and the Bluefield Project. FM received funding from the Tau Consortium and the Center for Networked Biomedical Research on Neurodegenerative Disease. RS-V is supported by Alzheimer’s Research UK Clinical Research Training Fellowship (ARUK-CRF2017B-2) and has received funding from Fundació Marató de TV3, Spain (grant no. 20143810). DG received support from the EU Joint Programme—Neurodegenerative Disease Research and the Italian Ministry of Health (PreFrontALS) grant 733051042. CG received funding from EU Joint Programme—Neurodegenerative Disease Research-refrontals VR Dnr 529-2014-7504, VR 2015-02926 and 2018-02754, the Swedish FTD Inititative-Schörling Foundation, Alzheimer Foundation, Brain Foundation and Stockholm County Council ALF. MM has received funding from a Canadian Institute of Health Research operating grant and the Weston Brain Institute and Ontario Brain Institute. JBR has received funding from the Wellcome Trust (103838) and is supported by the Cambridge University Centre for Frontotemporal Dementia, the Medical Research Council (SUAG/051 G101400) and the National Institute for Health Research Cambridge Biomedical Research Centre (BRC-1215-20014). EF has received funding from a Canadian Institute of Health Research grant #327387. RV has received funding from the Mady Browaeys Fund for Research into Frontotemporal Dementia. JL received funding for this work by the Deutsche Forschungsgemeinschaft German Research Foundation under Germany’s Excellence Strategy within the framework of the Munich Cluster for Systems Neurology (EXC 2145 SyNergy—ID 390857198). MO has received funding from Germany’s Federal Ministry of Education and Research (BMBF). JDR is supported by the Bluefield Project and the National Institute for Health and Care Research University College London Hospitals Biomedical Research Centre and has received funding from an MRC Clinician Scientist Fellowship (MR/M008525/1) and a Miriam Marks Brain Research UK Senior Fellowship. Several authors of this publication (JCVS, MS, RV, AdM, MO, RV and JDR) are members of the European Reference Network for Rare Neurological Diseases (ERN-RND)—Project ID No 739510. This work was also supported by the EU Joint Programme—Neurodegenerative Disease Research GENFI-PROX grant (2019-02248; to JDR, MO, BB, CG, JCVS and MS, and by the Clinician Scientist programme 'PRECISE.net' funded by the Else Kröner-Fresenius-Stiftung (to CW, DM and MS). HZ is a Wallenberg Scholar supported by grants from the Swedish Research Council (#2022-01018 and #2019-02397), the European Union’s Horizon Europe research and innovation programme under grant agreement No 101053962, Swedish State Support for Clinical Research (#ALFGBG-71320), the Alzheimer Drug Discovery Foundation (ADDF), USA (#201809-2016862), the AD Strategic Fund and the Alzheimer's Association (#ADSF-21-831376-C, #ADSF-21-831381-C, and #ADSF-21-831377-C), the Bluefield Project, the Olav Thon Foundation, the Erling-Persson Family Foundation, Stiftelsen för Gamla Tjänarinnor, Hjärnfonden, Sweden (#FO2022-0270), the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 860197 (MIRIADE), the European Union Joint Programme—Neurodegenerative Disease Research (JPND2021-00694), the National Institute for Health and Care Research University College London Hospitals Biomedical Research Centre and the UK Dementia Research Institute at UCL (UKDRI-1003).
Competing interests: HZ has served at scientific advisory boards and/or as a consultant for Abbvie, Acumen, Alector, Alzinova, ALZPath, Annexon, Apellis, Artery Therapeutics, AZTherapies, Cognito Therapeutics, CogRx, Denali, Eisai, Nervgen, Novo Nordisk, Optoceutics, Passage Bio, Pinteon Therapeutics, Prothena, Red Abbey Labs, reMYND, Roche, Samumed, Siemens Healthineers, Triplet Therapeutics, and Wave, has given lectures in symposia sponsored by Cellectricon, Fujirebio, Alzecure, Biogen, and Roche, and is a co-founder of Brain Biomarker Solutions in Gothenburg AB (BBS), which is a part of the GU Ventures Incubator Program (outside submitted work). JK received speaker fees, research support, travel support, and/or served on advisory boards by Swiss MS Society, Swiss National Research Foundation (320030_189140/1), University of Basel, Progressive MS Alliance, Alnylam, Bayer, Biogen, Bristol Myers Squibb, Celgene, Immunic, Merck, Neurogenesis, Novartis, Octave Bioscience, Quanterix, Roche, Sanofi, Stata DX. MS has received consultancy honoraria from Ionis, UCB, Prevail, Orphazyme, Servier, Reata, GenOrph, AviadoBio, Biohaven, Zevra,and Lilly, all unrelated to the present manuscript. The other authors declare no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: GENFI, Annabel Nelson, Martina Bocchetta, David Cash, David L Thomas, Emily Todd, Hanya Benotmane, Jennifer Nicholas, Kiran Samra, Rachelle Shafei, Carolyn Timberlake, Thomas Cope, Timothy Rittman, Antonella Alberici, Enrico Premi, Roberto Gasparotti, Valentina Cantoni, Emanuele Buratti, Andrea Arighi, Chiara Fenoglio, Elio Scarpini, Giorgio Fumagalli, Vittoria Borracci, Giacomina Rossi, Giorgio Giaccone, Giuseppe Di Fede, Paola Caroppo, Pietro Tiraboschi, Sara Prioni, Veronica Redaelli, David Tang-Wai, Ekaterina Rogaeva, Miguel Castelo-Branco, Morris Freedman, Ron Keren, Sandra Black, Sara Mitchell, Christen Shoesmith, Robart Bartha, Rosa Rademakers, Jackie Poos, Janne M. Papma, Lucia Giannini, Rick van Minkelen, Yolande Pijnenburg, Benedetta Nacmias, Camilla Ferrari, Cristina Polito, Gemma Lombardi, Valentina Bessi, Michele Veldsman, Christin Andersson, Hakan Thonberg, Linn Öijerstedt, Vesna Jelic, Paul Thompson, Tobias Langheinrich, Albert Lladó, Anna Antonell, Jaume Olives, Mircea Balasa, Nuria Bargalló, Sergi Borrego-Ecija, Ana Verdelho, Carolina Maruta, Catarina B. Ferreira, Gabriel Miltenberger, Tiago Coelho, Frederico Simões do Couto, Alazne Gabilondo, Ana Gorostidi, Jorge Villanua, Marta Cañada, Mikel Tainta, Miren Zulaica, Myriam Barandiaran, Patricia Alves, Benjamin Bender, Lisa Graf, Annick Vogels, Mathieu Vandenbulcke, Van Damme Philip, Rose Bruffaerts, Koen Poesen, Pedro Rosa-Neto, Serge Gauthier, Agnès Camuzat, Alexis Brice, Anne Bertrand, Aurélie Funkiewiez, Daisy Rinaldi, Dario Saracino, Olivier Colliot, Sabrina Sayah, Catharina Prix, Elisabeth Wlasich, Olivia Wagemann, Sandra Loosli, Sonja Schönecker, Tobias Hoegen, Jolina Lombardi, Sarah Anderl-Straub, Adeline Rollin, Gregory Kuchcinski, Maxime Bertoux, Thibaud Lebouvier, Vincent Deramecourt, Beatriz Santiago, Diana Duro, Maria João Leitão, Maria Rosario Almeida, Miguel Tábuas-Pereira, and Sónia Afonso
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Ethik-Kommission an der Medizinischen Fakultät der Eberhard-Karls-Universität und am Universitätsklinikum Tübingen, Germany, ethics approval: 273/2015BO1. Participants gave informed consent to participate in the study before taking part.
References
- 1. Woollacott IOC, Rohrer JD. The clinical spectrum of sporadic and familial forms of frontotemporal dementia. J Neurochem 2016;138 Suppl 1:6–31. 10.1111/jnc.13654 [DOI] [PubMed] [Google Scholar]
- 2. Heller C, Foiani MS, Moore K, et al. Plasma glial fibrillary acidic protein is raised in progranulin-associated frontotemporal dementia. J Neurol Neurosurg Psychiatry 2020;91:263–70. 10.1136/jnnp-2019-321954 [DOI] [PubMed] [Google Scholar]
- 3. Saracino D, Dorgham K, Camuzat A, et al. Plasma Nfl levels and longitudinal change rates in C9Orf72 and GRN-associated diseases: from tailored references to clinical applications. J Neurol Neurosurg Psychiatry 2021;92:1278–88. 10.1136/jnnp-2021-326914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van der Ende EL, Meeter LH, Poos JM, et al. Serum neurofilament light chain in genetic frontotemporal dementia: a longitudinal, multicentre cohort study. Lancet Neurol 2019;18:1103–11. 10.1016/S1474-4422(19)30354-0 [DOI] [PubMed] [Google Scholar]
- 5. Wilke C, Reich S, van Swieten JC, et al. Stratifying the presymptomatic phase of genetic frontotemporal dementia by serum Nfl and pNfH: a longitudinal multicentre study. Ann Neurol 2022;91:33–47. 10.1002/ana.26265 [DOI] [PubMed] [Google Scholar]
- 6. Gendron TF, Heckman MG, White LJ, et al. Comprehensive cross-sectional and longitudinal analyses of plasma Neurofilament light across FTD spectrum disorders. Cell Rep Med 2022;3:100607. 10.1016/j.xcrm.2022.100607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zetterberg H, Teunissen C, van Swieten J, et al. The role of neurofilament light in genetic frontotemporal lobar degeneration. Brain Commun 2023;5:fcac310. 10.1093/braincomms/fcac310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mullard A. Hotly anticipated ALS drug could pave way for more brain treatments. Nature April 17, 2023. 10.1038/d41586-023-01039-4 [DOI] [PubMed] [Google Scholar]
- 9. Abdelhak A, Kuhle J, Green AJ. Challenges and opportunities for the promising biomarker blood neurofilament light chain. JAMA Neurol 2023;80:542–3. 10.1001/jamaneurol.2023.0394 [DOI] [PubMed] [Google Scholar]
- 10. Abu-Rumeileh S, Abdelhak A, Foschi M, et al. The multifaceted role of neurofilament light chain protein in non-primary neurological diseases. Brain 2023;146:421–37. 10.1093/brain/awac328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rohrer JD, Nicholas JM, Cash DM, et al. Presymptomatic cognitive and Neuroanatomical changes in genetic Frontotemporal dementia in the genetic Frontotemporal dementia initiative (GENFI) study: a cross-sectional analysis. Lancet Neurol 2015;14:253–62. 10.1016/S1474-4422(14)70324-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Koo TK, Li MY. A guideline of selecting and reporting Intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155–63. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- 14. Fawcett T. An introduction to ROC analysis. Pattern Recognition Letters 2006;27:861–74. 10.1016/j.patrec.2005.10.010 [DOI] [Google Scholar]
- 15. Fierz W, Bossuyt X. Likelihood ratio approach and clinical interpretation of laboratory tests. Front Immunol 2021;12:655262. 10.3389/fimmu.2021.655262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gray E, Oeckl P, Amador MDM, et al. A multi-center study of neurofilament assay reliability and inter-laboratory variability. Amyotroph Lateral Scler Frontotemporal Degener 2020;21:452–8. 10.1080/21678421.2020.1779300 [DOI] [PubMed] [Google Scholar]
- 17. Truffi M, Garofalo M, Ricciardi A, et al. Neurofilament-light chain quantification by Simoa and Ella in plasma from patients with dementia: a comparative study. Sci Rep 2023;13:4041. 10.1038/s41598-023-29704-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shaw G, Madorsky I, Li Y, et al. Uman-type neurofilament light antibodies are effective reagents for the imaging of neurodegeneration. Brain Commun 2023;5:fcad067. 10.1093/braincomms/fcad067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee S, Plavina T, Singh CM, et al. Development of a highly sensitive neurofilament light chain assay on an automated immunoassay platform. Front Neurol 2022;13:935382. 10.3389/fneur.2022.935382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Andreasson U, Gobom J, Delatour V, et al. Assessing the commutability of candidate reference materials for the harmonization of neurofilament light measurements in blood. Clin Chem Lab Med 2023;61:1245–54. 10.1515/cclm-2022-1181 [DOI] [PubMed] [Google Scholar]
- 21. Benatar M, Wuu J, Turner MR. Neurofilament light chain in drug development for amyotrophic lateral sclerosis: a critical appraisal. Brain 2023;146:2711–6. 10.1093/brain/awac394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. van Lierop ZYGJ, Verberk IMW, van Uffelen KWJ, et al. Pre-Analytical stability of serum biomarkers for neurological disease: neurofilament-light, glial fibrillary acidic protein and Contactin-1. Clin Chem Lab Med 2022;60:842–50. 10.1515/cclm-2022-0007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jnnp-2023-332464supp001.pdf (439.9KB, pdf)