Abstract
Introduction: The management of chronic groin and scrotal content pain (orchialgia) is a complex condition after varicocelectomy that is encountered by most practicing clinicians. The aim of this study was to evaluate the effectiveness of low-level laser therapy (LLLT) in orchialgia after varicocelectomy surgery.
Methods: This study was performed as a double-blind, placebo-controlled randomized clinical trial in which sixty patients with orchialgia after varicocelectomy were randomly divided into three groups of 20 as follows: (1) low-level laser group with red (650 nm, 50 mW), (2) low-level laser group with infrared (IR) (820 nm, 100 mW), and (3) laser placebo group. The treatment protocol consisted of 15 minutes, three times a week, for only 12 sessions. Then, the patients were evaluated for pain and sexual satisfaction during the 12-week follow-up.
Results: The pain score in the two groups of low-level laser with red light and IR spectra showed a significant relief (P<0.05) 6 and 12 weeks after starting the treatment, In addition, a significant increase was observed in the level of sexual satisfaction in the red and infrared spectra LLLT groups (P<0.05).
Conclusion: We concluded that the use of LLLT with red light (650 nm, 50 mW)/IR (820 nm, 100 mW) spectra with power of 6-25 J/cm2/day in 15 minutes, three times a week, for 12 sessions can significantly reduce pain and increase sexual satisfaction in these patients.
Keywords: Low-level laser therapy, Red light spectra, Infrared spectra, Orchialgia, Varicocelectomy
Introduction
Varicocele occurs in approximately 15% of the male population. About 10% of these patients suffer from pain which is the main complaint. Varicocelectomy is still the most preferred treatment option in these patients, and its success rate in reducing pain is almost 80%. Currently, Varicocelectomy is used to control chronic inguinal pain due to varicocele.1
Most studies on varicocelectomy have been performed to only evaluate the treatment of male infertility, and limited works have been done to assess chronic pain management after varicocelectomy. Orchialgia after varicocelectomy is a common reason for many patients to be referred to urologists and other specialists.
Misdiagnosis, idiopathic orchialgia, postoperative complications, and recurrent or refractory varicocele are some of the reasons for treatment failure in these patients. Recurrent varicocele is the most common postoperative complication that is associated with painful varicocele in patients. Still, the main cause and the exact pathophysiology of orchialgia remain unknown. So far, detailed information on the prevalence and incidence of orchialgia has not been available; however, in certain groups, its prevalence rate is 0.4%-4.75% and its incidence rate is estimated to be more than one hundred thousand people annually.2-4 In certain groups of men with vasectomy, the rate of chronic pain after surgery is 1%-15% and the rate of chronic pain after inguinal hernia repair has been reported to be present in more than 3%-6% of patients.3
It is estimated that 2.5% of all urological visits are reserved for these patients. The patients with orchialgia were visited at least by an average of 4.5 physicians, and the averages of 7.2 medical interventions were performed for the final diagnosis of their pain.4 Treatment process may be disappointing for over 50% of these patients because despite the diagnostic procedures performed, no identifiable cause for their pain has been reported.5,6 Orchialgia after varicocelectomy is one of the most important and controversial issues among urologists and pain specialists.
In a cohort study conducted on 48 patients with unilateral / bilateral varicocele with dull scrotal pain after laparoscopic varicocelectomy, VAS scores were assessed and showed a relative pain improvement in 90% of the patients and a significant improvement in 87%, but in 2% of them, no change in pain was reported. Interestingly, after varicocelectomy, 10% of the patients had recurrence and 8% of the patients had de novo hydrocele.7
It has been more than 10 years since low-level laser radiation was used in various medical treatments like physical therapy. The low-level laser with the mechanism of vasodilation increases lymphatic drainage, and better tissue circulation reduces tissue edema, removes pressure from the nerve ending, and reduces its stimulation. The low-level laser is also effective in cellular and subcellular processes. In previous studies, no pathological effects on bone and muscle have been reported in laser therapy.8-10
One of the treatments of choice for chronic pain is the low-level laser as an alternative to medical treatments, which, despite its widespread use, is still a controversial medical issue. Considering the advantages of the low-level laser in reducing chronic pain, limited studies in the treatment of chronic pain of the genitourinary system, and therapeutic interventions in patients with orchialgia, our study is the first clinical study on the effectiveness of low-level laser therapy (LLLT) in orchialgia after varicocelectomy in the sample of Iranian population.
Materials and Methods
Sampling Method
Sixty patients were selected sequentially by using the simple non-random sampling method and randomly by the random number table method, and they were divided into three groups of 20.
According to the study by Esmaeeli Djavid et al,11 the sample size for each group is estimated to be 20 people, considering α = 0.05, ß = 20%, α-z = 1.96, ß-z = 0.85, p1 = 60%, and p2 = 40%.
N = (z (1- α /2) 2p(1-p) + z(1- β ) √p1(1-p1) + p2(1-p2) / d)2
Methods
The present study was conducted after the approval of the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.REC.1396.110). This study is a double-blind, placebo-controlled randomized clinical trial (identifier: IRCT 201709278146N23) conducted on patients with orchialgia after varicocelectomy who were referred to the pain clinic of Imam Hossein, Shohadaye Tajrish, and Sajjad hospitals during 2015 and 2016.
The inclusion criteria were as follows: patients with the consent to participate in the study, patients aged 18 years and above, patients with at least 12 weeks after the onset of pain, patients with a recurrence of varicocele, patients with no response to conventional treatments, and patients examined by a urologist (medical history, Doppler ultrasound of testis, and urography).
The exclusion criteria were as follows: patients with no consent to participate in the study and patients with malignant disease, epididymitis, epididymal cyst, flank pain, hydrocele, neurological defects, abnormal laboratory findings, or systemic or psychiatric illness.
The patients were randomly divided into three groups of 20: (1) Red low-level laser group with a wavelength of 650 nm and power of 50 mW, (2) Infrared (IR) low-level laser group with a wavelength of 820 nm and power of 100 mW, and (3) Placebo laser group. The patients received laser therapy and a placebo laser three times a week for four weeks (12 sessions), and at each session the patient received the laser for 15 minutes. It should be noted that the treatment was done bilaterally. The therapist and the patient were not aware of laser therapy and placebo. The outcome of treatment was measured by another physician who was unaware of the groups upon entering the study, six weeks after the treatment (after the last intervention session), and 12 weeks after starting the treatment (last six weeks without intervention).
Intervention
In group I, red low level laser radiation at 810 nm (50 mw) was performed, and in group II, the IR low-level laser at 820 nm (100 mw) was performed (L.H.H Medical Science Development CO., Ltd, Beijing, China ). The power output was calibrated with a thermopile power meter. In each session, according to the standard method, low-level laser irradiation was done with a contact laser device at 3 points in the upper part of the scrotum, which is innervated by the ilioinguinal nerve in the T10-L2 segments.
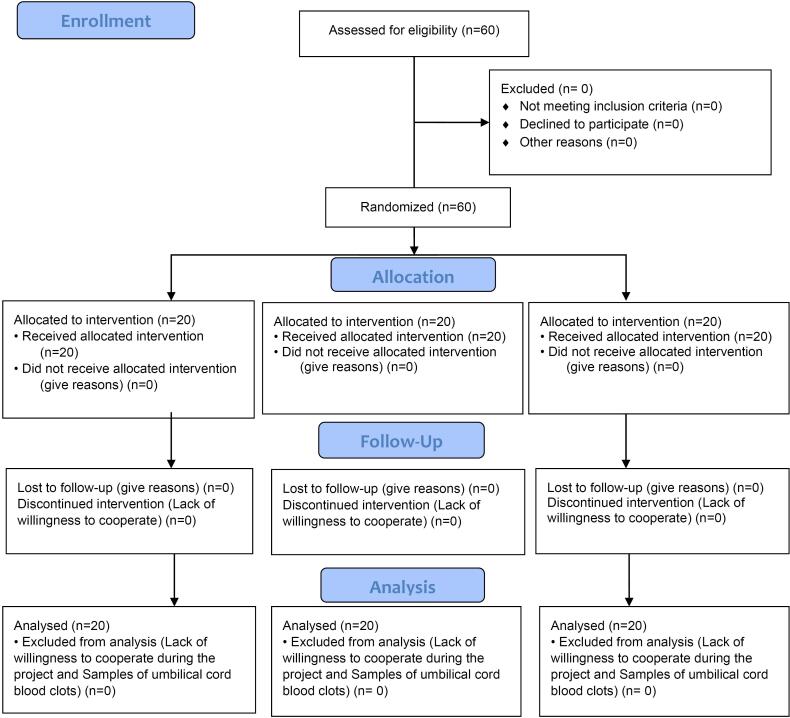
In groups I and II, the laser was irradiated with a dose of 6-25 joules per square centimeter, while in the placebo group (group III), the laser was irradiated with an in-active probe. The duration of each laser treatment session was approximately 15 minutes. The treatment protocol consisted of 12 sessions (15 minutes, three times a week for four weeks) in three groups (Figure 1).
Figure 1.
Consort Diagram of the Study
Assessment of the Outcomes
Sexual satisfaction and orchialgia were measured by using the visual analogue scale (VAS) (0-10). The patients were asked to rate their pain and sexual satisfaction by showing a score. In case of complication, the type of complication was also recorded.
Statistical Analysis
The information needed for the plan was recorded and entered into the statistical SPSS software version 19. After examining the normality of quantitative data by the Kolmogorov–Smirnov test, the mean of quantitative variables between the two groups was compared by the t test and paired t test, and the mean of quantitative variables was compared between the three groups by one-way ANOVA post hoc tests. Also, qualitative variables between the three groups were compared by the chi-square test. The P value < 0.05 was considered statistically significant.
Results
The comparison of patients’ demographic information between the three groups is shown in Table 1.
Table 1. The comparison of the demographic data between the groups .
| IR LLLT | Red LLLT | Placebo LLLT | P Value | |
| Age (y) | 25.8 ± 1.1 | 23.0 ± 8.6 | 27.9 ± 6.2 | 0.113 |
| BMI (kg/m2) | 26.4 ± 1.5 | 26.4 ± 3.9 | 28.2 ± 1.4 | 0.174 |
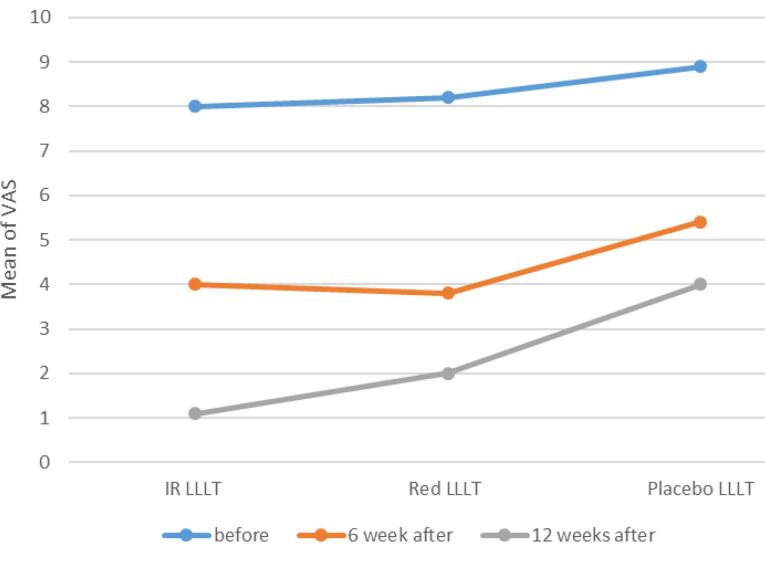
The comparison of the changes in pain level based on the VAS at different times in the three groups is shown in Table 2 and Figure 2. The results showed a statistically significant reduction at different times after LLLT in comparison with the placebo group (P < 0.05). In the post hoc test, the pain score showed a statistically significant difference six weeks after the treatment between the placebo and IR LLLT groups (P = 0.0001), but it did not show a significant difference between the IR LLLT and red LLLT groups (P = 0.553). Also, 12 weeks after treatment, a statistically significant difference was found in the placebo and IR LLLT groups (P = 0.003), but no statistically significant difference was shown in the IR LLLT and red LLLT groups (P = 0.727).
Table 2. The Comparison of the Pain (VAS) Between the Three Groups .
| IR LLLT | Red LLLT | Placebo LLLT | P Value | P Value IR-Red | P Value IR-Placebo | P Value Red -Placebo | |
| Before | 9.0 ± 0.7 | 8.9 ± 1.7 | 8.8 ± 1.4 | 0.531 | 0.533 | 0.529 | 0.530 |
| 6 Weeks after | 3.7 ± 0.3 | 3.6 ± 0.8 | 4.4 ± 0.6 | 0.006 | 0.553 | 0.0001 | 0.0001 |
| 12 Weeks after | 2.1 ± 1.0 | 2.1 ± 0.4 | 3.3 ± 1.4 | 0.023 | 0.727 | 0.003 | 0.001 |
Figure 2.
The comparison of the changes in pain score at different times between the groups (P < 0.05)
The comparison between the IR LLLT and red LLT groups implicated no significant difference in the pain score at 6 and 12 weeks after the treatment (Table 2).
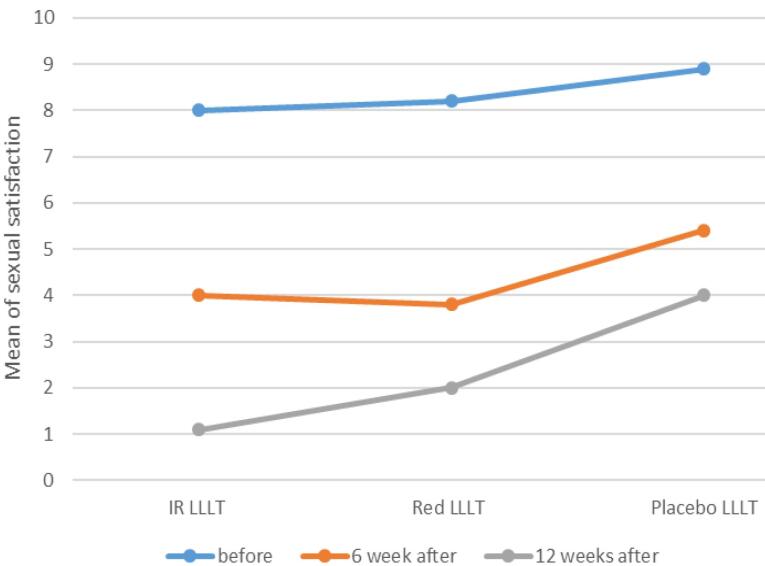
The comparison of the changes in sexual satisfaction at different times in the three groups is shown in Table 3 and Figure 3. It showed a statistically significant increase at different times after LLLT in comparison with the placebo group (P < 0.05). In the Post Hoc test, sexual satisfaction, six weeks after treatment in placebo group and IR LLLT group, it was showed a statistically significant difference (P = 0.001) but in the IR LLLT group and Red LLLT, it did not show statistically significant difference (P = 0.682). Twelve weeks after the treatment, a statistically significant difference was observed between the placebo group and the IR LLLT group (P = 0.001), and there was not a statistically significant difference between the IR LLLT group and the red LLLT group (P = 0.549).
Table 3. The Comparison of the Changes in Sexual Satisfaction Level Between the Groups .
| IR LLLT | Red LLLT | Placebo LLLT | P Value | P Value IR-Red | P Value IR-Placebo | P Value Red -Placebo | |
| Before | 8.0 ± 0.4 | 8.2 ± 0.7 | 8.9 ± 1.4 | 0.538 | 0.439 | 0.520 | 0.533 |
| 6 Weeks after | 4.0 ± 0.3 | 3.8 ± 0.9 | 5.4 ± 0.9 | 0.003 | 0.682 | 0.001 | 0.006 |
| 12 Weeks after | 1.1 ± 0.2 | 2.0 ± 0.1 | 4.0 ± 1.9 | 0.036 | 0.549 | 0.001 | 0.001 |
Figure 3.
The comparison of changes in sexual satisfaction level at different times between the groups (P < 0.05)
The comparison between the IR LLLT and red LLT groups implicated no significant difference in sexual satisfaction level during 12 weeks after the treatment (Table 3)
No complication related to LLLT was reported in any of the patients during the follow-up.
Discussion
Our study is the first clinical study that examined the therapeutic effect of red LLLT and IR LLLT on the treatment of orchialgia after varicocelectomy. In our study, the changes of pain intensity in three low-level laser groups with red (650 nm, 50 mW), Infrared (820 nm, 100 mW), and laser placebo were compared. Pain improvement was reported after 12 sessions over four weeks within three months of follow-up.
In the present study, six and twelve weeks after the start of the treatment, the amount of pain in the two groups of red LLLT and IR LLLT showed a significant improvement. Also, the sexual satisfaction showed a significant improvement in the two groups of red LLLT and IR LLLT.
In patients with orchialgia after varicocelectomy, it appears that red LLLT and IR LLLT reduced the pain and increased sexual satisfaction and that laser therapy with one of the types of red LLLT/IR LLLT improved the quality of marital relations of these patients.
Considering the fact that so far no clinical study has been performed with this method in the treatment of patients with orchialgia after varicocelectomy, the findings are not comparable with other studies.
Despite the widespread nature of the LLLT mechanism, the physiological mechanism of LLLT is still not well understood.12-14
Chronic inflammatory epididymitis due to a post-operative infection, a history of viral or bacterial infections, and interstitial cystitis with an unknown cause are among the causes of scrotum pain after surgery.15 One of the most important clinical goals of low-power laser treatment is the treatment of inflammation and tissue degeneration. Probably, low-power laser performance increases the modulation of inflammatory mediators and increases tissue oxygenation.16
One hypothesis is that the pain threshold may increase after LLLT, leading to nerve obstruction, particularly the inhibition of nerve fibers A and C.17,18 Nerve fiber inhibition may be accomplished by altering the nerve axon flow or by inhibiting neuronal enzymes.17-18 In addition, the available data show an increase in endorphin production and binding of opioid receptors through leukocytes containing opioid substances to LLLT.14,17
LLLT probably reduces the effect of anti-inflammatory drugs by reducing prostaglandin-2 (PGE2) levels and mimicking cyclooxygenase 2 (COX-2) inhibition.19,20 In addition, available information has shown that LLLT may increase nitric oxide levels that are a powerful vasodilator that increases blood flow and helps recovery.13,14,21
While the mechanisms of action of LLLT have not been fully explained thus far, it is clear that LLLT is associated with an analgesic effect.
Due to the fact that no standard protocol for LLLT has been provided so far, the use of LLLT as a treatment method is limited.
To date, studies have been performed on the type and protocol of laser therapy with different overall doses and wavelengths, which limits the possibility of drawing an accurate conclusion. Currently, no study has evaluated the long-term effect of LLLT. Pain is a complex condition that manifests itself in different forms. There may not be a specific LLLT standard that addresses the needs of each patient depending on the underlying complaint and diagnosis.
It is clear that LLLT may be effective and helpful for any patient suffering from pain, regardless of the condition causing it.
According to the findings, the use of red low-level laser irradiation with a wavelength of 650 nm (50 mw) and IR low-level laser irradiation with a wavelength of 820 nm (100 mw) is a useful, safe and minimally invasive way in the treatment of orchialgia after varicocelectomy and increases patients’ sexual satisfaction. The therapeutic interventions mentioned in this study were well tolerated by patients.
Orchialgia is a debilitating and difficult disease to treat, and the treatment of these patients is the main concern of urologists and other specialists. Therefore, the use of multidisciplinary approaches to decide on the treatment of these patients is required. Red LLLT (wavelength of 650 nm; 50 mw) and IR LLLT (wavelength of 820 nm; 100 mw) according to the protocol of the present study can reduce chronic pain after varicocelectomy and improve sexual satisfaction and quality of marital relations in these patients. Therefore, specialists in chronic pain, internists, general surgeons and urologists are suggested to consider the use of red/IR LLLT protocol laser according to the treatment protocol of our study in the treatment of patients with orchialgia after varicocelectomy.
It is suggested that in order to make a definite clinical recommendation in future studies, this study should be performed with a larger sample size with long-term follow-up and taking into account other LLLT parameters with red and infrared laser irradiation.
Conclusion
We suggested that the use of LLLT with red light (650 nm, 50 mW) / infrared (820 nm, 100 mW) spectra and power of 6-25 joules/cm2/day in 15 minutes, three times a week, for 12 sessions can significantly reduce pain and increase sexual satisfaction in these patients.
Acknowledgments
This double-blind randomized clinical trial study is funded by the Vice chancellor for research of Shahid Beheshti University of Medical Sciences.
Authors’ Contribution
Conceptualization: Cyrus Momenzadeh, Mohammadreza Razzaghi.
Data curation: Cyrus Momenzadeh, Mohammadreza Razzaghi.
Formal analysis: Cyrus Momenzadeh, Mohammadreza Razzaghi.
Investigation: Cyrus Momenzadeh, Mohammadreza Razzaghi.
Methodology: Cyrus Momenzadeh.
Project administration: Cyrus Momenzadeh.
Supervision: Cyrus Momenzadeh.
Visualization: Cyrus Momenzadeh, Davod Ommi, Jafar Birami.
Writing–original draft: Cyrus Momenzadeh, Mohammadreza Razzaghi.
Writing–review & editing: Cyrus Momenzadeh, Mohammadreza Razzaghi.
Competing Interests
The authors claim no conflict of interest.
Ethical Approval
This study was approved under the ethical approval code of “IR.SBMU.REC.1396.110”.
Funding
None.
Please cite this article as follows: Momenzadeh C, Razzaghi M, Ommi D, Birami J. Effectiveness of low-level laser therapy in orchialgia after varicocelectomy surgery. J Lasers Med Sci. 2024;15:e35. doi:10.34172/jlms.2024.35.
References
- 1.Yaman O, Ozdiler E, Anafarta K, Göğüş O. Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology. 2000;55(1):107–8. doi: 10.1016/s0090-4295(99)00374-x. [DOI] [PubMed] [Google Scholar]
- 2.Blendon RJ, Benson JM. The public and the opioid-abuse epidemic. N Engl J Med. 2018;378(5):407–11. doi: 10.1056/NEJMp1714529. [DOI] [PubMed] [Google Scholar]
- 3.Davis BE, Noble MJ, Weigel JW, Foret JD, Mebust WK. Analysis and management of chronic testicular pain. J Urol. 1990;143(5):936–9. doi: 10.1016/s0022-5347(17)40143-1. [DOI] [PubMed] [Google Scholar]
- 4.Ciftci H, Savas M, Yeni E, Verit A, Topal U. Chronic orchialgia and associated diseases. Curr Urol. 2010;4(2):67–70. doi: 10.1159/000253415. [DOI] [Google Scholar]
- 5.Calixte N, Brahmbhatt J, Parekattil S. Chronic testicular and groin pain: pathway to relief. Curr Urol Rep. 2017;18(10):83. doi: 10.1007/s11934-017-0722-7. [DOI] [PubMed] [Google Scholar]
- 6.Levine LA, Hoeh MP. Evaluation and management of chronic scrotal content pain. Curr Urol Rep. 2015;16(6):36. doi: 10.1007/s11934-015-0510-1. [DOI] [PubMed] [Google Scholar]
- 7. Kachrilas S, Popov E, Bourdoumis A, Akhter W, El Howairis M, Aghaways I, et al. Laparoscopic varicocelectomy in the management of chronic scrotal pain. JSLS 2014;18(3):e2014.00302. 10.4293/jsls.2014.00302. [DOI] [PMC free article] [PubMed]
- 8.Haher TR, Gorup JM, Shin TM, Homel P, Merola AA, Grogan DP, et al. Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis: a multicenter study of 244 patients. Spine. 1999;24(14):1435–40. doi: 10.1097/00007632-199907150-00008. [DOI] [PubMed] [Google Scholar]
- 9.Tullberg M, Alstergren PJ, Ernberg MM. Effects of low-power laser exposure on masseter muscle pain and microcirculation. Pain. 2003;105(1):89–96. doi: 10.1016/s0304-3959(03)00166-0. [DOI] [PubMed] [Google Scholar]
- 10.Mulcahy D, McCormack D, McElwain J, Wagstaff S, Conroy C. Low level laser therapy: a prospective double-blind trial of its use in an orthopaedic population. Injury. 1995;26(5):315–7. doi: 10.1016/0020-1383(95)00048-e. [DOI] [PubMed] [Google Scholar]
- 11.Esmaeeli Djavid G, Mehrdad R, Ghasemi M, Hasan-Zadeh H, Sotoodeh-Manesh A, Pouryaghoub G. In chronic low back pain, low level laser therapy combined with exercise is more beneficial than exercise alone in the long term: a randomised trial. Aust J Physiother. 2007;53(3):155–60. doi: 10.1016/s0004-9514(07)70022-3. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto H, Ozaki A, Iguchi N, Kinoshita S. Antinociceptive effects of laser irradiation of Hoku point in rats. Pain Clin. 1988;8:43–8. [Google Scholar]
- 13.Cidral-Filho FJ, Mazzardo-Martins L, Martins DF, Santos AR. Light-emitting diode therapy induces analgesia in a mouse model of postoperative pain through activation of peripheral opioid receptors and the L-arginine/nitric oxide pathway. Lasers Med Sci. 2014;29(2):695–702. doi: 10.1007/s10103-013-1385-3. [DOI] [PubMed] [Google Scholar]
- 14.Moriyama Y, Nguyen J, Akens M, Moriyama EH, Lilge L. In vivo effects of low-level laser therapy on inducible nitric oxide synthase. Lasers Surg Med. 2009;41(3):227–31. doi: 10.1002/lsm.20745. [DOI] [PubMed] [Google Scholar]
- 15.Akiyama Y, Luo Y, Hanno PM, Maeda D, Homma Y. Interstitial cystitis/bladder pain syndrome: the evolving landscape, animal models and future perspectives. Int J Urol. 2020;27(6):491–503. doi: 10.1111/iju.14229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Z, Wu Y, Zhang H, Jin P, Wang W, Hou J, et al. Low-level laser irradiation alters cardiac cytokine expression following acute myocardial infarction: a potential mechanism for laser therapy. Photomed Laser Surg. 2011;29(6):391–8. doi: 10.1089/pho.2010.2866. [DOI] [PubMed] [Google Scholar]
- 17.Kudoh C, Inomata K, Okajima K, Motegi M, Ohshiro T. Effects of 830 nm gallium aluminum arsenide diode laser radition on rat saphenous nerve sodium-potassium-adenosine triphosphate activity: a possible pain attenuation mechanism explained. Laser Surg. 1989;1:63–7. [Google Scholar]
- 18.Chow RT, David MA, Armati PJ. 830 nm laser irradiation induces varicosity formation, reduces mitochondrial membrane potential and blocks fast axonal flow in small and medium diameter rat dorsal root ganglion neurons: implications for the analgesic effects of 830 nm laser. J Peripher Nerv Syst. 2007;12(1):28–39. doi: 10.1111/j.1529-8027.2007.00114.x. [DOI] [PubMed] [Google Scholar]
- 19.Campana VR, Castel A, Vidal AE, Juri H, Palma JA. Prostaglandin E2 in experimental arthritis of rats irradiated with He-Ne laser. J Clin Laser Med Surg. 1993;11(2):79–81. doi: 10.1089/clm.1993.11.79. [DOI] [Google Scholar]
- 20.Sakurai Y, Yamaguchi M, Abiko Y. Inhibitory effect of low-level laser irradiation on LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur J Oral Sci. 2000;108(1):29–34. doi: 10.1034/j.1600-0722.2000.00783.x. [DOI] [PubMed] [Google Scholar]
- 21.Mitchell UH, Mack GL. Low-level laser treatment with near-infrared light increases venous nitric oxide levels acutely: a single-blind, randomized clinical trial of efficacy. Am J Phys Med Rehabil. 2013;92(2):151–6. doi: 10.1097/PHM.0b013e318269d70a. [DOI] [PubMed] [Google Scholar]