Abstract
Background
Children with disabilities experience poorer oral health and frequently have complex needs. The accessibility of oral health care services for children with disabilities is crucial for promoting oral health and overall well-being. This study aimed to systematically review the literature to identify the barriers and facilitators to oral health care services for children with disabilities, and to propose priority research areas for the planning and provision of dental services to meet their needs.
Methods
This was a mixed methods systematic review. Multiple databases searched included MEDLINE, Scopus, PsycINFO, EMBASE, and CINAHL. The search strategy included Medical Subject Heading (MeSH) terms related to children, disabilities, and access to oral health. Eligibility criteria focused on studies about children with disabilities, discussing the accessibility of oral health care.
Results
Using Levesque’s framework for access identified barriers such as professional unwillingness, fear of the dentist, cost of treatment, and inadequate dental facilities. Facilitators of access offered insight into strategies for improving access to oral health care for children with disabilities.
Conclusion
There is a positive benefit to using Levesque’s framework of access or other established frameworks to carry out research on oral healthcare access, or implementations of dental public health interventions in order to identify gaps, enhance awareness and promote better oral health practices. The evidence suggests that including people with disabilities in co-developing service provision improves accessibility, alongside using tailored approaches and interventions which promote understanding of the importance of dental care and increases awareness for professionals, caregivers and children with disabilities.
Trial registration
Protocol has been registered online on the PROSPERO database with an ID CRD42023433172 on June 9, 2023.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-024-04767-9.
Keywords: Access, Disability, Children, Dental care, Oral health care
Background
The United Nations Children’s International Emergency Fund (UNICEF) estimates the number of children with disabilities is nearly 240 million [1]. According to the World Health Organisation (WHO), disability is a comprehensive concept that encompasses impairments, limitations in activities, and restrictions in participation. It is not solely a biological or social construct, but rather emerges from the interplay between health conditions and various environmental and personal factors [2]. Children with disabilities are at higher risk of poorer health than the general population and the academic evidence highlights the existence of health disparities between children with and without disabilities [3]. Children with disabilities also experience poorer oral health, with problems ranging from tooth decay and gingivitis to severe periodontal disease [4]. One longitudinal clinical study has identified that oral health inequity tends to begin in childhood, perpetuating and increasing across the lifecourse, with access to oral health care a key factor associated with better oral health [5]. Compared to their non-disabled peers, children with disabilities frequently possess complex oral health care needs [6–10]. For example, underlying health conditions may exert an effect on oral health [6, 7], sensory and motor impairments may affect their ability to attend routine dental care [8, 9] and physical impairments can make oral health care practices, such as toothbrushing, challenging [10].
Children with and without disabilities need support to access healthcare services, but this can be variable and is dependent on the skills and abilities of caregivers to distinguish between the type and extent of support needed [11, 12]. Limited access to oral health care services links to poor oral health outcomes, which may lead to inequalities in oral health for children with disabilities [13, 14]. Access, however, is complex, it does not merely mean physically entering a service, it has numerous constructs and potentially modifiable factors such as negative attitudes of professionals, a lack of service provision, or poor geographical distribution of services, amongst others. Then there are fixed factors such as a lack of socio-economic resources in the family, or factors relating to impairment, all of which create barriers to access.
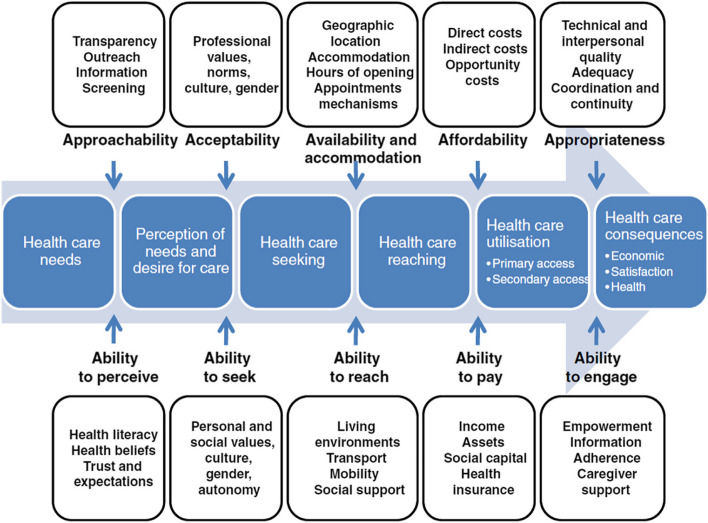
Over the past four decades, various frameworks have been developed to help understand healthcare access dynamics [15–19]. One recent and comprehensive framework is Levesque’s Conceptual Framework for Healthcare Access (Fig. 1), published in 2013 after an extensive review of existing literature on healthcare access [20]. This framework offers a multidimensional perspective on healthcare access within the context of health systems, encompassing approachability, acceptability, availability/accommodation, affordability, and appropriateness. It takes into account socioeconomic determinants and incorporates five corresponding abilities of individuals and populations: to perceive, to seek, to reach, to pay, and to engage, in healthcare access [20]. Unlike approaches that solely focus on health system failures, Levesque’s framework allows researchers to explore barriers to access resulting from individuals’ abilities to perceive, seek, reach, pay, or engage with healthcare. Access, as defined in this framework, encompasses the opportunity to identify, seek, reach, obtain, or use healthcare services while meeting individual needs access [20].
Fig. 1.
Levesque’s conceptual framework for healthcare access
Existing systematic reviews highlights main barriers to dental services for individuals with disabilities, including professional unwillingness to care for their teeth, fear of the dentist, cost of treatment, lack of adaptation of access routes to dental offices or clinics and inadequate health care or dental facilities [21, 22]. The work by da Rosa and colleagues [22] and Krishnan and colleagues [21] only provides a brief overview because one is restricted to including only cross-sectional studies, and the other refers to barriers faced by caregivers alone. Neither represents a comprehensive analysis of the literature using a broader theoretical framework. Moreover, these reviews [21, 22] failed to discuss the facilitators of access to oral health services for people with disabilities. Facilitators of access may resolve barriers to accessing dental services. In contrast, one qualitative study discusses facilitators and barriers, which cross-sectional studies fail to, because the design does not infer cause and effect relationship [23]. However, this small-scale qualitative study is about adults with disabilities in the UK and not generalizable to other populations. Children with disabilities need support to access dental care, therefore, it is important to identify factors that promote or inhibit access and thereby provide a template of how to increase positive oral health outcomes and attempt to reduce inequalities.
Using Levesque’s Conceptual Framework for Healthcare Access as an a priori framework, this study aimed to (1) systematically review the literature to identify the barriers and facilitators to oral health care services for children with disabilities, and (2) to propose priority research areas for the planning and provision of dental services to meet their needs. The identification of barriers and facilitators to dental care services among children with disabilities could provide guidance for the development of targeted interventions to improve access to oral health care and overall health.
Methods
This study is a mixed method systematic review of the evidence on access to oral health care services for children with disabilities, up to 31st May 2024. Using Participant, Intervention, Comparator and Outcome (PICO) to develop the question, the overarching research question guiding this systematic review was ‘What interventions or designs enable the accessibility of oral health care services for children with disabilities and their parents/carers?’ Other questions are ‘What are the barriers to accessibility of oral health care services for children with disabilities and their parents/carers?’ ‘What increases utilization of oral health care services for children with disabilities and their parents/carers?’
The study follows the updated JBI methodological guidance for conducting a mixed methods systematic review [24].
Registration of the protocol and PRISMA guidelines
The review adhered to the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [25]. Prior to conducting the systematic review, the authors developed a review protocol and registered it with the International Prospective Register of Systematic Reviews PROSPERO on June 9, 2023, under the registration number (CRD42023433172).
Data sources and searches
The search strategy for this systematic review involved searching multiple databases, including MEDLINE, Scopus, PsycINFO, EMBASE, CINAHL and Google Scholar to ensure a comprehensive coverage of relevant studies beyond the databases. Backward or chain searching of references, involves identifying and examining the references or works and enables learning around the development of a topic, whilst identifying experts in the area. Forward searching of references within retrieved records cited in an article after its publication enables finding new theoretical developments in the area and consideration of any other methodologies employed. Second generation forward searching enables the researcher to search for inconsistencies. This process of backward and forward searching of references identified any additional relevant literature for inclusion. To ensure accuracy in the research terminology used, librarians from The University of Sheffield and Manchester University were consulted. Additional file 1. illustrates the complete list of MeSH search terms and the full electronic search strategy.
Eligibility criteria
Population
The studies included in the review included children with disabilities aged 18 years or below. In cases where studies included both adults and children or adolescents, they were considered eligible for inclusion if at least 75% of the participants were children or adolescents, or if separate outcome data were available for this subgroup. This study uses People First language and employs the term children with disabilities, rather than disabled children, although it acknowledges that using the term disabled children implies that society creates barriers because it employs language favored by the social model of disability [26].
Interventions
Studies discussing access or mentioning dimensions of access to oral health care for children with disabilities were included. Studies of reasonable adjustments and improved access to oral health care for children with disabilities were also included. Oral health studies that solely focused on a particular condition (e.g., Down’s syndrome) or focused solely on the diagnosed oral health condition (e.g., caries or periodontal disease) without any mention of access were excluded. All oral healthcare settings, including dental clinics, hospitals, community health centers, or specialized dental facilities for children with disabilities, were included.
Comparators
Studies with any comparator or no comparator were included. Comparators included intervention or care as usual, as well as studies utilizing alternative approaches for access to oral health care.
Outcomes
The primary outcome assessed in the study was access to oral health care for children with disabilities. If otherwise eligible, for studies that did not report a relevant outcome, attempts were made to contact the authors to determine the outcome. In cases where it was not possible to determine this, the study was listed but the data not fully extracted or included. There is a difference between access to services and effectiveness [27]. Therefore, papers reporting the ability to physically access, use a service, and/or the standard of service provision were included. Additionally, studies reporting the effectiveness of measures or interventions designed to improve access to the relevant services were reviewed.
Levesque et al.’s model of access [20] was used as an a priori framework to code how each study measured dimensions of accessibility and corresponding abilities.
Study selection
The study included the following research designs: randomized controlled trials, non-randomized controlled studies, cohort studies, cross-sectional studies, and process evaluations. Mixed method studies and qualitative studies were also included. Systematic and scoping reviews were used to identify primary studies but were not directly included. Studies without primary data, case reports, government reports, guidelines, editorials, commentaries, opinion pieces and conference abstracts, were excluded. Publications in English or Arabic languages, including Arabic due to the Arabic-speaking first and second authors, were included. No countries were excluded from the study. No date restrictions were applied in the search strategy, ensuring a comprehensive inclusion of relevant studies regardless of their publication date. The search was completed up to 31st May 2024.
Inclusion screening
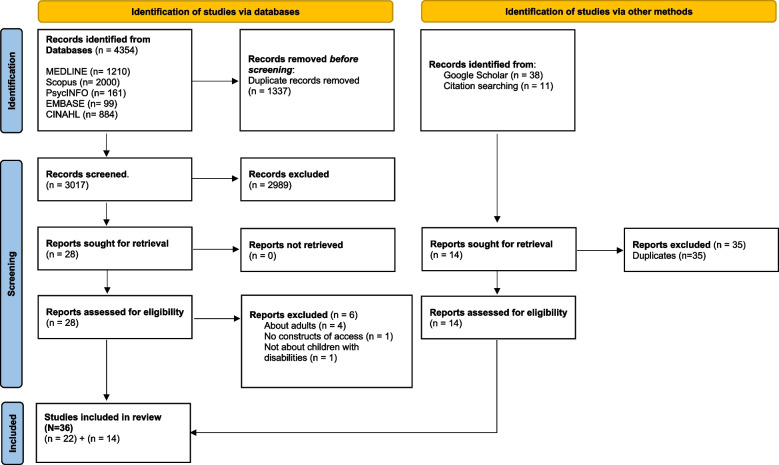
The articles resulting from the search were exported to an Endnote library [28] and duplicates removed. To ensure consistency, three reviewers (MA, AJ and JO) screened an initial 100 references. Any queries or uncertainties were resolved through discussion. Two reviewers (MA, AJ) then independently assessed the evidence for inclusion using the eligibility criteria at both the title/abstract and full-text screening stages. Disagreements were addressed through discussion and consensus. In cases where consensus was difficult to reach, a third independent researcher (JO) was involved. Studies that did not meet the eligibility criteria during the full-text screening stage were excluded, and reasons for exclusion were recorded (See Fig. 2).
Fig 2.
PRISMA Flowchart
Extraction of data
Data were tabulated in an Excel sheet, which included author and date, study design, country, sample size, type of disability, outcomes, and barriers and facilitators to access (See Table 1).
Table 1.
Characteristics of Included Studies
| Author/Year | Study design | Country | Sample size | Type of disability | Outcomes | Barriers and facilitators to access |
|---|---|---|---|---|---|---|
| Abduludin et al., (2019) [33] | Qualitative | Malaysia | 10 parents/ caregivers | Cerebral Palsy | The study identified five domains of promoting and hindering factors relating to the accessibility of children with CP to oral health care. These were dental experience, family support, mobility, ability to pay and social value. |
Barriers: Lack of family support to access care, poor previous experience of services, proximity of parking at the clinic, lack of reasonable adjustments to access dental surgery, societal discrimination about disability Facilitators: Ability to pay, free treatment, dental outreach program, positive attitudes of dental staff, sharing experiences with other parents of disabled children |
| Al Agili et al., (2004) [35] | Cross-sectional | USA | 714 parents | Different disabilities | Association with lack of insurance and difficulty accessing dental services. Waiting times of 3-6 months barrier to access. Length of time in waiting room added to child’s distress. |
Barriers: Difficulties in finding willing dentists who accept their health insurance, lack of dentists’ knowledge and training in providing care. Lack of transportation, Scheduling challenges such as long wait times for appointments and extended waiting times at the dental office also hindered access to care. Facilitators: Private insurance coverage |
| Al Habashneh et al., (2012) [60] | Cross-sectional | Jordan | 206 comprising 103 with DS and 103 age and gender-matched non-DS ⁄public school children | Downs Syndrome (DS) | The most common reason cited for not taking children to the dentist for DS group was ‘Not aware of the dental problems of their children |
Barriers: Not aware of the dental problems of their children, no awareness of the importance of dental visit, Fear of children as a reason for not taking children to dental care and financial. Facilitators: Not mentioned |
| AlHammad et al., (2020) [45] | Cross-sectional | KSA | 263 parents of autistic children | Autism | A total of 41.4% of the parents visit the dental clinic when the child complains about dental problems and 54% find difficulty in locating appropriate dental clinic to deal with their ASD children. Most parents reported taking their child to a private office (38.8%). Only 3.8% of parents reported that their children had seizures during dental procedures. |
Barriers: Dislike of dental treatment, complications related to the medical condition, trouble in locating a competent dentist. Facilitators: Accessibility of a variety of dental services |
| Allison et al., (2000) [36] | Cross-sectional | France |
204 reports on children with DS 161 reports on siblings without DS |
DS | Parents of children with DS nearly twice as likely to report problems finding dental services. Parents 20x more likely to use specialist medical services than dental services, indicating low priority for oral healthcare. |
Barriers: Time-consuming healthcare, difficulty finding dental services, limited availability of dental services, and a higher reliance on specialist medical services rather than dental services. Insufficient behavior management skills of the general practitioner Facilitators: individuals with DS are more likely to consult a dentist yearly if they also seek speech therapy and ophthalmology services, suggesting an association of health problems and/or of parental health and illness behavior |
| Al-Shehri, (2012) [64] | Cross-sectional | KSA | 119 caregivers | Different disabilities |
84.7% of persons with disabilities saw a dentist only for an emergency, and 46.2% reported having difficulty in obtaining dental care in their community. Fear of the dentist (52.1%), cost (48.7%), being unable to sit in the dental chair (28.2%), transportation difficulties (26.9%), distance to the dental clinic (18.5%), and the dentist’s unwillingness to treat those with disabilities (16.8%) were all barriers to dental care for individuals with disabilities |
Barriers: fear of the dentist, cost, being unable to sit in a dental chair, transportation difficulty, distance to the dental clinic, and the dentist’s unwillingness to treat those with disabilities Facilitators: Caregivers' higher level of education correlates with improved oral hygiene practices and a higher probability of seeking dental care for individuals with disabilities. |
| Alshihri et al., (2021) [46] | Cross-sectional | KSA | 142 mothers | Autism Spectrum Disorders (ASD) | 68.3% of mothers reported difficulty finding a dental care. 75.4% found cost prohibitive. 74.6% reported difficulty finding a dentist willing to treat their child. 72% of dentists visited failed to offer any oral heath advice. Only 45% believed that their child’s behavior would affect their ability to seek dental care. |
Barriers: Perceived behavior of child, cost of dental treatment, insurance shortfall, and difficulty finding a dentist who treats autistic children. Facilitators: Not mentioned |
| Barry et al., (2014) [37] | Cross-sectional | UK |
112 / 56 parents/carers of children with ASD 56 parents/carers of children without ASD |
ASD | Although there was no significant difference in accessing dental care between the study and control groups, the ASD group perceived it as more difficult. They faced greater challenges in traveling to the dental surgery and exhibited more predicted negative behaviors. |
Barriers: Difficulties in transport, cost of treatment, Importance of parking proximity, finding a suitable dentist, long waiting time in the waiting room, difficulties and discomfort experienced by children with ASD during dental procedures, perceived lack of cooperation by the child during dental care, perceived challenging behaviors of children with ASD, difficulty in recognizing dental pain and challenges in communication. Facilitators: Medical insurance and positive experience |
| Bhaskar et al., (2016) [47] | Cross‑sectional | India | 331 differently abled children and their parents | Differently abled children | Financial difficulty was a major barrier to dental care, particularly for intellectually impaired children (39%). |
Barriers: Cost of treatment and transportation difficulties, fear of the dentist, perceived inability to cooperate with dental treatments, geographical distance of clinic. Facilitators: Dentists showing willingness to treat children. |
| Brickhouse et al., (2009) [48] | Cross-sectional | USA | 55 caregivers of at least 1 child with an autism spectrum disorder. | ASD | Household income and child’s history of difficult behavior in the dental office significantly related to the ability to receive care when needed and whether the child had a regular dental provider. An inability to find a dentist with the skills or willingness to work with people with disabilities was the most frequent reason cited for not having a regular dental provider. |
Barriers: Respondents’ education and income, insurance coverage, the child’s perceived history of behavior in the dental office, inability to find a dentist with special skills or a willingness to work with disabled patients. Facilitators: Insurance coverage and household income |
| Chi et al., (2010) [61] | Cross-sectional | USA | IDD children (N = 4,385), non-IDD children (N = 103,220) | Children with intellectual and/or developmental disability | Factors such as older age, not residing in a dental Health Professional Shortage Area, interaction with the medical system, and family characteristics increased one’s likelihood of receiving preventive dental care. |
Barriers to preventive dental care: younger age, not residing in areas with sufficient dental professionals, limited integration between medical and dental systems, and unequal dentist distribution in urban/rural counties. Facilitators of preventive dental care: Interaction with medical system, having another Medicaid-enrolled child, enrolling children from same low-income families in Medicaid. |
| Como et al., (2022) [41] | Qualitative | Black/African American, USA | 11 caregivers of children with Autism | Autism | Three themes emerged from the data concerning the barriers that affect oral health experiences: (a) difficulty in maintaining good oral health practices, (b) challenges with access to care and resources, and (c) poor patient-provider relationships |
Barriers to accessing dental care include financial constraints, dental insurance issues, difficulty finding local dentists, limited community resources, and negative experiences with health care professionals. Facilitators: Not mentioned |
| De Jongh et al., (2008) [49] | Cross-sectional | Netherlands |
61 Children, 126 Caretakers and 40 dentists |
Severe mental disabilities |
- Ethnic minority children with disabilities had lower access to routine dental care (53.1% vs. 23.8%). -Dutch noninstitutionalized children with severe disabilities received limited quality dental care. -Non-cooperation of patients was a significant challenge for caretakers (68%). -Perceived communication problems were the primary barrier to treatment according to dentists (75%). |
Barriers: Children belonging to an ethnic minority not receiving routine oral care. Treatment barriers as indicated by the dentists: Perceived communication problems, lack of financial compensation, lack of experience in treating children with intellectual disabilities, lack of knowledge, and unequipped surgeries. Facilitators: Regular professional oral care and high satisfaction levels reported by dentists and caretakers. |
| de Souza et al., (2023) [42] | Cross-sectional | Brazil | 100 caregivers | ASD | The caregivers reported that 25% of the children had never been to the dentist and 57% had an appointment over the past 12 months. Seeking primary care for dental treatment and frequent toothbrushing were positively associated with both outcomes and participating in oral health preventive activities decreased the chance of never having been to the dentist. Having male caregivers and activity limitations due to autism decreased the chance of having been to the dentist over the past year. |
Barriers: Male caregivers and children with profound autism. Facilitators: Knowledge of oral health and carrying out existing oral health practices, as well as participation in an oral healthcare program. |
| Du et al., (2019) [38] | Case–control | Hong Kong, China | 257 pre-schoolers with ASD, 257 without ASD | ASD | Children with ASD had a lower frequency of tooth-brushing and toothpaste usage, but they required parental assistance more often during tooth-brushing (p < .05). Barriers to dental care were more frequently reported among children with ASD (p < .001). Parents of children with ASD had higher scores in dental knowledge and attitudes compared to those without ASD |
Barriers: The inability to find a dentist willing to treat the child, difficulty finding a dentist near the child’s home, dental staff being anxious or nervous about treating the child, time constraints, and high dental costs. Non-environmental reasons included the child’s perceived dislike of dental procedures, perceived inability to behave cooperatively during dental visits, complex medical conditions complicating dental treatment, and other more urgent healthcare needs. Facilitators: Better oral health knowledge and more positive oral health attitudes among parents of children with ASD. |
| Fenning et al., (2020) [65] | Cross-sectional | USA | 375 families of children ages 4 to 17 | ASD | 92% of families reported accessing dental care, with 64.2% obtaining two preventive dental visits, 33.7% reporting one preventive dental visit, and only 2% reporting no preventive dental visits. Families of children on the register were more likely to report a high level of access to dental visits. However, disparities existed in the type of care received, as younger child age and lower levels of child IQ and adaptive behavior were associated with receiving less comprehensive dental care. Moreover, caregiver education found to be positively associated with receiving a greater number of dental services. Study primarily focused on attributing impairments to the children rather than exploring ways to adapt the dental environment to their needs. |
Access barriers: Perceived child IQ and behavioral issues. Access facilitators: Caregiver education, oral health education in preventive services.es. |
| Gerreth et al., (2016) [50] | Cross-sectional | Poland |
264 parents/ caregivers |
Intellectual Disability | Only 31.8% of parents/caregivers had no access problems to dental care. The primary barrier reported was a protracted waiting time for appointments, affecting 36.7% of respondents. Notably, 90.1% of children were treated in dental surgery conditions. Additionally, only 42.1% of respondents expressed satisfaction with their children’s dental care. |
Barriers: Perceived degree of intellectual disability, long waiting time for appointments, dentist reluctance, high costs of dental services, inconvenient opening hours of dental offices, the location of dental surgeries in relation to the patient’s residence, architectural limitations in the dental surgery, and limited access to transport and communication challenges for individuals with more profound intellectual disabilities. Facilitators: Having a milder degree of intellectual disability |
| Holt & Parry, (2019) [51] | Cross-sectional | UK | Parents/carers of 17 children and young people with autism spectrum conditions | ASD | Time spent in waiting areas can increase anxiety in children and young people with autism spectrum conditions. All parents viewed Real-time Text Messaging as having a positive impact on the dental attendance experience. The majority believed it reduced anxiety and enabled children and young people with autism spectrum conditions to be more accepting of dental treatment |
Barriers: Time spent in waiting areas can increase anxiety. Facilitators: Real-time text messaging reduces anxiety and enables acceptance of dental treatment |
| Hu & Da Silva, (2022) [44] | Cross-sectional | Canada | 189 parents or caregivers | Developmental disabilities |
Common barriers were cost (63%), location (55%), the child’s behavior (78%) and caregiver anxiety (60%). 35% of caregivers believed their dentist lacked adequate knowledge of Fetal Alcohol Spectrum Disorder. Univariate analysis reveals that income, caregiver education, residence location, and insurance status were significantly associated with reporting barriers. |
Barriers: included cost, location of a dentist, and scheduling. Personal barriers involved the child’s anticipated behavior, caregiver anxiety, lack of perceived need, and other health care priorities. Interpersonal barriers included difficulties finding a dentist without a referral, the belief that the dentist lacked adequate knowledge of the child’s condition, feelings of discrimination or disrespect, and the belief that the dentist did not spend enough time with the child. Additionally, income, caregiver education, residence location, and insurance status were significantly associated with reporting barriers. Facilitators: Higher education levels and higher incomes among caregivers aid in accessing oral health care |
| Junnarkar et al., (2023) [39] | Qualitative | Singapore | 23 parents of autistic children | Autism | Accessing dental services was hindered by a lack of parental knowledge on the importance of an early dental home, parental apprehension about the child’s acceptance of dental care, lack of information on specialized dentists and perceived high cost of dental visits |
Barriers: Parental knowledge issues, parental attitude and anxiety, dentist-related factors (dentists unwilling to treat persons with ASD, long waiting time to see specialist dentists, lack of information on dentists who can treat persons with ASD), and cost concerns. Facilitators: Providing parents with coping strategies and utilizing techniques such as social stories, visual aids, and pretend play to improve the dental experience for autistic children |
| Kachwinya et al., (2022) [62] | Cross-sectional | Uganda | 90 children and their caregivers. | Cerebral palsy | The most common barrier reported by the caregivers was the challenge in modality of transportation availability from the children’s homes to the health facilities (34.4%). |
Barriers: Transportation difficulties, high transportation costs, low income, and a limited perception of the need for regular dental care. Some caregivers believed that dental care was only necessary for specific issues such as swelling, cracked teeth with pain, or mobile teeth, which contributed to a restricted understanding of the importance of regular dental visits. Facilitators: Not mentioned. |
| Krishnan et al., (2018) [52] | Mixed Methods | India | 195 dentists and 100 caregivers, whose children were between 3 and 15 years of age. | Different disabilities | The majority of dentists (83.7%) reported not receiving enough training to handle children with special needs. Caregivers (38%) reported the children’s perceived fear of dentists as a major barrier to utilizing dental services. |
Barriers: Inadequate training of dentists, infrastructural limitations in dental clinics, fear of dentists, financial constraints, and a lack of adequate facilities. Facilitators: Positive behavior and understanding demonstrated by dentists, as well as their assistance with transfers between wheelchairs and dental chairs. |
| Lai et al., (2012) [53] | Cross-sectional | USA |
(555) children with ASD / caregivers |
ASD | The main barriers were perceived child’s behavior, cost, and lack of insurance. The significant predictor variables of unmet needs were perceived child’s behavior (p = 0.01), child’s dental health (p\0.001), and caregiver’s last dental visit greater than 6 months ( p = 0.002). |
Barriers: Perceived child cooperation, cost of dental care, lack of dental insurance, limited availability of dentists, transportation problems, difficulty in getting appointments, lack of knowledge about where to go for dental care, inconvenient office hours, long wait times in clinics/offices, family and caregiver factors (health of another family member, other family priorities), negative perceptions and trust issues towards dentists, child being too young, language barrier. Facilitators: Promoting positive behavior in children can play a beneficial role in the dental setting. |
| Liu et al., (2022) [40] | Cross-sectional | Australia | 169 carers | Developmental Disabilities | Nearly 25% of the participants found it extremely difficult to obtain appropriate oral health care. Amongst the participants 10% had to abandon dental treatment due to difficulties, while 13% have yet to receive any sort of dental care. Amongst school-aged children, 64.5% were unable to receive dental care from the school dental service |
Barriers to accessing dental care: Lack of appropriate dental equipment; difficulties in booking appointments and a poor referral system; limited oral health awareness and knowledge of available services; negative attitude and inadequate knowledge and experience of staff, along with lack of infrastructure; shortages in special needs dentistry specialists. Cost, travel distances, and waiting times; challenges related to wheelchair access; and feelings of discrimination, insecurity, anxiety, and fear reported by patients. Facilitators: Not mentioned |
| Mansoor et al.,(2018) [54] | Case-control | UAE | parents of 84 ASD and 53 healthy children | ASD | A majority of parents of ASD children (83.3%) reported that their children needed assistance in brushing their teeth, while only 15.4% of parents of healthy controls reported the same. During dental visits, perceived uncooperative behavior, and a significantly higher percentage of parents (37%) rated their child’s experience as negative, compared to 9.5% among parents of control children. The dental visits for autistic children mostly involved extraction |
Barriers: Limited availability of dentists who can handle the child’s needs, perceived child uncooperative behavior during dental visits, fear or anxiety experienced by the child towards dental care, and a lack of complaints or perceived dental issues leading to reluctance or avoidance of dental visits. Facilitators: Not mentioned |
| Nelson et al., (2011) [14] | Cross-sectional | USA | 1,128 Parents | CSHCN | Children with craniofacial anomalies had twice as many unmet needs and children with cystic fibrosis had fewer unmet needs. Children with cerebral palsy, autism, developmental delay, and Down syndrome had more perceived aversion to dental treatment, more treatment complications posed by their medical conditions, and more difficulty finding a dentist willing to provide care. Children with cystic fibrosis, metabolic disorders, or hemophilia encountered fewer barriers to care. |
Barriers: Environmental and non-environmental barriers to accessing dental care for children include cost constraints, difficulties in finding a dentist willing to treat the child, complicated medical conditions of the child affecting dental treatment, income limitations, perceived child’s fear and anxiety towards dental care, perceived behavioral challenges, and oral healthcare having a lower priority compared to the child’s other healthcare needs. Facilitators: None mentioned. |
| Parry et al., (2023) [55] | Qualitative | UK | 6 parents of 10 children diagnosed with ASD | Autism | Parental perceptions included the need for understanding and training among dental professionals, awareness of sensory issues, recognition of individual autistic traits, clear communication, and factors affecting parental confidence in advocating for their children. Focus group participants emphasized empathizing with autistic perspectives, the importance of positive oral health messages, and the challenges in altering dietary regimes and establishing dental preventive habits for their children |
Barriers: Lack of understanding and training, awareness of sensory issues, recognition of the individuality of autistic traits, time and clarity for communication, factors affecting parental confidence in advocating in the clinical environment, lack of understanding regarding altering self-imposed, ritualistic dietary regimes, and difficulty in enacting good dental preventive habits for autistic children. Facilitators for children’s dental care include immersive empathy from oral health team members, visual communication, distraction techniques, tailored information, ASD awareness and training, strategic preparation, autonomy support, addressing sensory challenges, recognizing hidden disabilities, minimizing anticipatory distress, valuing parents’ expertise, adjusting power dynamics, and adapting to changing behaviors. |
| Puthiyapurayil et al., (2022) [56] | Cross-sectional | India | 300 children and their parents | Children with intellectual needs | Predominant barriers for access dental care were financial difficulties (35.3%), lack of knowledge about dental care (24%), transportation difficulties (15%). |
Barriers: Financial difficulties, lack of knowledge about dental care, transportation difficulties, lack of trained dentists, perceived uncooperative behavior of children, and dentists not willing to treat. Facilitators: None mentioned. |
| Rajput et al., (2021) [57] | Cross-sectional | India | 600: 300 differently abled children and 300 healthy children | Differently abled children | In the study group, the highest mean scores for barriers observed in the areas of lack of priority care (8.82±2.81), difficulty in communicating with the dentist (7.85±1.92), high treatment cost (6.90±1.98), and fear of dental instruments (6.90±1.98). Conversely, in the control group, the main barriers related to affordability and perceived fear. Additionally, deficiencies found in dental clinic facilities, specifically the absence of wheelchairs (76.3% and 76.7%) and corridor signs (66.3% and 61.7%) |
Barriers: Lack of dental awareness among parents, lack of priority care, communication challenges, high treatment costs, fear-related concerns, inadequate clinic infrastructure, limited access due to scarcity of nearby dentists, insufficient time for visits, high travel costs, and time-consuming appointments. Facilitators for dental care utilization include increased awareness, treatment availability, accessibility, effective communication, priority care, addressing fear, and improving facilities in dental clinics. |
| Sabbarwal et al., (2018) [43] | Cross‑sectional | India | 100 DS children, 100 non‑DS and their parents/ caregivers | DS | DS children had poor oral hygiene and considerable caries experience and faced certain barriers to utilization of oral health care services. |
Barriers: the presence of medical conditions, the cost of dental treatment, and dentist-related factors. Facilitators: Parental awareness of dental problems positively influenced the utilization of oral health services. |
| Schultz et al., (2001) [34] | Cross-sectional | USA | 12,539 children ages 2–17 years for the study population. | Developmentally disabled children | Parental perception of unmet need was significantly associated with developmentally disabled children 2-17 years in lower socioeconomic groups. |
Barriers: Children from lower socioeconomic groups who are eligible for Medicaid coverage face cost barriers to accessing dental care. Additionally, children with developmental disabilities encounter perceived barriers to care that influenced by family income levels. Facilitators: Lack of income-related barriers to dental care access |
| Shyama et al., (2015) [58] | Cross-sectional | Kuwait | 308 parents of children with disabilities + teachers, who had normal children (n = 112) | Physical disability & DS | Perceived barriers to dental care for children with disabilities and typically developing children include difficulty in getting appointments, reported by 37.3% of parents. Parents of disabled children consider difficulty in cooperation as a more important barrier to treatment (34.7%) compared to parents of typically developing children (20.3%). A larger proportion of parents of typically developing children (82%) rate the present dental services as excellent/good, compared to 52% of parents of disabled children (p < 0.001). Toothache and curative treatment needs are the main reasons for dental visits among disabled children. |
Barriers: Difficulty in getting an appointment, perceived challenges with cooperation, distance and transportation challenges, and cost. Facilitators to dental care access for children include higher dental visits, early dental check-ups, and availability of government dental clinics, and positive perceptions of dental services. |
| Stein et al., (2012) [59] | Cross-sectional | California (USA) | 396 parents of ASD children or typically developing | ASD | Significantly more parents of ASD children than parents of typically developing children reported difficulty across almost all oral care variables explored, including oral care in the home, oral care at the dentist, and access to oral care. |
Barriers: Negative experiences, sensory sensitivities, perceived uncooperative behaviors, and difficulties in finding accommodating dental providers. Facilitators: Parental persistence, the availability of dental care, and supportive dental professionals who are trained to work with children with special health care needs. |
| Zahran et al., (2023) [66] | Cross-sectional | KSA | 602 caregivers |
Children with autistic spectrum disorder (ASD), Down syndrome, cerebral palsy, and developmental delay |
The most common reported barrier was fear of the dentist (61.6%) followed by child uncooperativeness (37.8%) and treatment costs (27.8%). |
Barriers: larger family size, low income, low education levels, fear of the dentist, child uncooperativeness, and treatment costs. Facilitators: Caregivers with higher education levels and smaller family sizes |
| Zhou et al., (2021) [63] | Cross-sectional | Hong Kong, China | 383 children | Children with special education needs (SEN)(children were diagnosed with cerebral palsy, intellectual disabilities, autism, developmental delay, Down syndrome, Williams syndrome, or other specific syndromes) | Most parents (72.3%) faced challenges with dental visits for their children, citing barriers such as high cost (33.2%) and perceived children’s aversion to mouth procedures (58.1%). A small percentage of parents (1.4%) also reported sensitivity to sound and light as an additional barrier. |
Barriers: The environmental barriers to accessing dental care included high dental costs, difficulty finding a dentist willing to treat the child due to their medical condition, and the challenge of finding a dentist near their home. Non-environmental barriers included the child’s perceived resistance to dental procedures, perceived inability to behave cooperatively during dental visits, being too young for dental appointments, fear of the dentist, and parental anxiety. Facilitators: Children’s age and parents’ education attainment can act as facilitators to dental care access. |
| Zickafoose et al., (2015) [67] | Cross-sectional | USA | Parents of 2055 children with special health care needs | CSHCN | The Children’s Health Insurance Program (CHIP) demonstrates greater access to dental services for children with special health care needs (CSHCN) and their families compared to uninsured children and their families. |
Barriers: There were large differences in access to and use of dental services. Lack of insurance coverage or inadequate private policies did not sufficiently cover dental services for children with additional needs. Facilitator: The Children’s Health Insurance Program (CHIP) provides access to dental care for children with additional needs |
Key: ASD Autism Spectrum Disorders, DS Down Syndrome, CSHCN Children with special health care needs
Two researchers (MA, AJ) utilized Levesque’s five dimensions of accessibility and abilities of persons to interact with the dimensions of accessibility. The table was piloted for 10% of the studies and any discrepancies were resolved through discussion before continuing. A third member of the review team (JO) resolved conflicts of agreement. Table 2 provides detailed analysis of the dimensions of accessibility and ability to interact with the dimensions.
Table 2.
Summary of dimensions and abilities explored according to the Levesque framework
| Author/Year | Access focus (Dimensions VS abilities) | Number of Dimensions/ abilities Explored |
Dimensions and abilities explored. (Yes/No) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Approachability | Acceptability | Availability/ accommodation |
Affordability | Appropriateness | To perceive | To seek | To reach | To pay | To engage | |||
| Abduludin et al., (2019) [33] | Both | 10 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Al Agili et al., (2004) [35] | Both | 5 | Yes | No | Yes | Yes | No | No | No | Yes | Yes | No |
| Al Habashneh et al., (2012) [60] | Both | 2 | No | No | No | Yes | No | Yes | No | No | No | No |
| AlHammad et al., (2020) [45] | Both | 2 | No | No | Yes | No | No | No | No | No | No | Yes |
| Allison et al., (2000) [36] | Both | 6 | Yes | No | Yes | No | Yes | Yes | Yes | No | No | Yes |
| Al-shehri., (2012) [64] | Both | 6 | No | No | No | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Alshihri et al., (2021) [46] | Both | 3 | No | No | Yes | Yes | No | No | No | No | No | Yes |
| Barry et al., (2014) [37] | Both | 9 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Bhaskar et al., (2016) [47] | Both | 5 | No | No | Yes | Yes | No | Yes | No | Yes | No | Yes |
| Brickhouse et al., (2009) [48] | Both | 4 | No | No | Yes | No | No | Yes | No | No | Yes | Yes |
| Chi et al., (2010) [61] | Both | 3 | No | No | No | Yes | Yes | No | No | No | Yes | No |
| Como et al., (2022) [41] | Both | 5 | No | Yes | Yes | Yes | No | No | Yes | No | Yes | No |
| De Jongh et al., (2008) [49] | Both | 4 | No | No | Yes | Yes | No | No | Yes | No | No | Yes |
| de Souza et al., (2023) [42] | Both | 4 | No | Yes | No | No | No | Yes | No | Yes | No | Yes |
| Du et al., (2019) [38] | Both | 7 | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes |
| Fenning et al., (2020) [65] | Abilities | 3 | No | No | No | No | No | Yes | Yes | No | No | Yes |
| Gerreth et al., (2016) [50] | Both | 5 | No | No | Yes | Yes | Yes | No | No | Yes | No | Yes |
| Holt & Parry, (2019) [51] | Dimensions | 2 | No | No | Yes | No | Yes | No | No | No | No | No |
| Hu & Da Silva, (2022) [44] | Both | 8 | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Junnarkar et al., (2023) [39] | Both | 7 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | No |
| Kachwinya et al., (2022) [62] | Both | 4 | No | No | No | Yes | No | Yes | No | Yes | Yes | No |
| Krishnan et al., (2018) [52] | Both | 3 | No | No | Yes | No | No | No | No | No | Yes | Yes |
| Lai et al., (2012) [53] | Both | 6 | No | No | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Liu et al., (2022) [40] | Both | 8 | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Mansoor et al., (2018) [54] | Both | 3 | No | No | Yes | No | No | Yes | No | No | No | Yes |
| Nelson et al., (2011) [14] | Both | 5 | No | No | Yes | Yes | No | Yes | Yes | Yes | No | No |
| Parry et al., (2023) [55] | Both | 4 | No | No | Yes | No | Yes | Yes | Yes | No | No | No |
| Puthiyapurayil et al., (2022) [56] | Both | 5 | No | No | Yes | No | No | Yes | No | Yes | Yes | Yes |
| Rajput et al., (2021) [57] | Both | 6 | No | No | Yes | Yes | No | Yes | No | Yes | Yes | Yes |
| Sabbarwal et al., (2018) [43] | Both | 5 | No | Yes | No | Yes | Yes | Yes | No | No | No | Yes |
| Schultz et al., (2001) [34] | Abilities | 1 | No | No | No | No | No | No | No | No | Yes | No |
| Shyama et al., (2015) [58] | Both | 4 | No | No | Yes | Yes | No | No | No | Yes | No | Yes |
| Stein et al., (2012) [59] | Both | 4 | No | No | Yes | No | Yes | Yes | No | No | No | Yes |
| Zahran et al., (2023) [66] | Abilities | 4 | No | No | No | No | No | Yes | Yes | No | Yes | Yes |
| Zhou et al., (2021) [63] | Both | 5 | No | No | Yes | Yes | No | Yes | Yes | Yes | No | No |
| Zickafoose et al., (2015) [67] | Abilities | 1 | No | No | No | No | No | No | No | No | Yes | No |
Data synthesis and analysis
This mixed methods systematic review uses questions focusing on different aspects of the same phenomenon. Therefore, the synthesis took a convergent segregated approach, which consisted of conducting separate and independent quantitative and qualitative syntheses but using thematic analysis for both [24]. Both syntheses employed deductive thematic analysis based on the predefined themes from Levesque et al.’s model of access [20]. This approach synthesized findings from both qualitative and quantitative studies, offering a comprehensive understanding of access to oral health care for children with disabilities.
Quality and risk of bias assessment strategy
Given the variety of research designs included in this review, the quality of the studies was assessed using the Quality Appraisal for Diverse Studies (QuADS) [29], and risk of bias was evaluated using appropriate tools for each study design (AXIS Tool for Cross-Sectional Design, and Joanna Briggs Institute critical appraisal tools for both qualitative and case-control studies) [30–32].
QuADS assesses various important aspects of the studies, such as the underlying theory, defined objectives, appropriateness and rigor of the design, data collection methods, and analytical methods. It consists of 13 evaluative indicators, each rated on a four-point Likert scale ranging from 0 (not at all) to 3 (complete), allowing researchers to determine the extent to which each criterion is met. To ensure consistency, two reviewers (MA, AJ) conducted an initial pilot on 10% of the sample, resolving discrepancies through discussion or with a third reviewer (JO). Table 3 provides detailed scoring of the included studies.
Table 3.
Quality Assessment of the included studies using QuADS
| Author / Year | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Item 12 | Item 13 | Score/39 | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abduludin et al., (2019) [33] | 2 | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 0 | 3 | 3 | 2 | 29 | 74% |
| Al Agili et al., (2004) [35] | 1 | 3 | 3 | 3 | 2 | 0 | 0 | 2 | 2 | 2 | 3 | 1 | 1 | 23 | 59% |
| Al Habashneh et al., (2012) [60] | 1 | 3 | 3 | 3 | 1 | 0 | 2 | 2 | 3 | 2 | 3 | 0 | 3 | 26 | 67% |
| AlHammad et al., (2020) [45] | 1 | 3 | 1 | 2 | 1 | 0 | 1 | 1 | 1 | 0 | 3 | 2 | 0 | 16 | 41% |
| Allison et al., (2000) [36] | 1 | 3 | 3 | 2 | 2 | 3 | 2 | 2 | 3 | 3 | 3 | 0 | 3 | 30 | 77% |
| Al-shehri., (2012) [64] | 0 | 3 | 3 | 2 | 0 | 0 | 2 | 1 | 1 | 1 | 2 | 1 | 1 | 17 | 44% |
| Alshihri et al., (2021) [46] | 1 | 3 | 3 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 3 | 0 | 2 | 24 | 62% |
| Barry et al., (2014) [37] | 1 | 3 | 3 | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | 23 | 59% |
| Bhaskar et al., (2016) [47] | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 3 | 1 | 0 | 25 | 64% |
| Brickhouse et al., (2009) [48] | 1 | 3 | 3 | 2 | 1 | 2 | 1 | 2 | 2 | 1 | 3 | 0 | 3 | 24 | 62% |
| Chi et al., (2010) [61] | 1 | 2 | 3 | 2 | 3 | 2 | 2 | 2 | 3 | 1 | 2 | 0 | 2 | 25 | 64% |
| Como et al., (2022) [41] | 1 | 3 | 2 | 3 | 3 | 2 | 3 | 2 | 2 | 3 | 3 | 2 | 2 | 31 | 79% |
| De Jongh et al., (2008) [49] | 1 | 3 | 3 | 2 | 2 | 1 | 2 | 3 | 2 | 1 | 2 | 0 | 1 | 23 | 59% |
| de Souza et al., (2023) [42] | 1 | 3 | 3 | 2 | 3 | 2 | 1 | 1 | 3 | 3 | 3 | 1 | 3 | 29 | 74% |
| Du et al., (2019) [38] | 1 | 3 | 3 | 2 | 2 | 2 | 3 | 2 | 1 | 0 | 3 | 0 | 0 | 22 | 56% |
| Fenning et al., (2020) [65] | 1 | 3 | 3 | 2 | 2 | 1 | 2 | 1 | 1 | 3 | 3 | 0 | 0 | 22 | 56% |
| Gerreth et al., (2016) [50] | 1 | 3 | 3 | 3 | 2 | 0 | 0 | 1 | 1 | 0 | 3 | 0 | 0 | 17 | 44% |
| Holt & Parry, (2019) [51] | 1 | 3 | 2 | 2 | 1 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 2 | 15 | 39% |
| Hu & Da Silva, (2022) [44] | 2 | 3 | 3 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 3 | 0 | 2 | 24 | 62% |
| Junnarkar et al., (2023) [39] | 2 | 3 | 3 | 3 | 3 | 1 | 3 | 1 | 1 | 3 | 3 | 0 | 3 | 29 | 74% |
| Kachwinya et al., (2022) [62] | 1 | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 3 | 3 | 3 | 2 | 2 | 31 | 79% |
| Krishnan et al., (2018) [52] | 2 | 3 | 2 | 3 | 2 | 2 | 0 | 2 | 1 | 0 | 2 | 3 | 2 | 24 | 62% |
| Lai et al., (2012) [53] | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 3 | 2 | 3 | 3 | 2 | 2 | 31 | 79% |
| Liu et al., (2022) [40] | 2 | 3 | 1 | 2 | 1 | 2 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 14 | 36% |
| Mansoor et al., (2018) [54] | 0 | 3 | 2 | 2 | 2 | 1 | 2 | 2 | 1 | 0 | 2 | 1 | 0 | 18 | 46% |
| Nelson et al., (2011) [14] | 0 | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 3 | 0 | 3 | 3 | 1 | 30 | 77% |
| Parry et al., (2023) [55] | 1 | 3 | 3 | 3 | 2 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 1 | 33 | 85% |
| Puthiyapurayil et al., (2022) [56] | 0 | 3 | 2 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 16 | 41% |
| Rajput et al., (2021) [57] | 0 | 3 | 1 | 2 | 1 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 20 | 51% |
| Sabbarwal et al., (2018) [43] | 1 | 3 | 2 | 2 | 3 | 1 | 2 | 1 | 1 | 3 | 3 | 1 | 2 | 25 | 64% |
| Schultz et al., (2001) [34] | 1 | 3 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 2 | 0 | 0 | 18 | 46% |
| Shyama et al., (2015) [58] | 1 | 3 | 3 | 2 | 2 | 1 | 1 | 2 | 2 | 1 | 2 | 0 | 0 | 20 | 51% |
| Stein et al., (2012) [59] | 1 | 3 | 2 | 2 | 2 | 1 | 0 | 1 | 1 | 2 | 2 | 0 | 3 | 20 | 51% |
| Zahran et al., (2023) [66] | 1 | 3 | 3 | 3 | 0 | 2 | 3 | 3 | 2 | 3 | 3 | 1 | 2 | 29 | 74% |
| Zhou et al., (2021) [63] | 0 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 2 | 3 | 3 | 0 | 3 | 31 | 79% |
| Zickafoose et al., (2015) [67] | 0 | 3 | 3 | 3 | 3 | 2 | 0 | 2 | 2 | 3 | 3 | 0 | 3 | 27 | 69% |
Coding reference
1. Theoretical or conceptual underpinning to the research:
0. No mention at all
1. General reference to broad theories or concepts that frame the study. E.g., key concepts identified in the introduction section.
2. Identification of specific theories or concepts that frame the study and how these informed the work undertaken. E.g., key concepts identified in the introduction section and applied to the study.
3. Explicit discussion of the theories or concepts that inform the study, with application of the theory or concept evident through the design, materials and outcomes explored. E.g., key concepts identified in the introduction section and the application apparent in each element of the study design.
2. Statement of research aim/s
4. No mention at all
5. Reference to what the sought to achieve embedded within the report but no explicit aims statement.
6. Aims statement made but may only appear in the abstract or be lacking detail.
7. Explicit and detailed statement of aim/s in the main body of report.
3. Clear description of research setting and target population
8. No mention at all.
9. General description of research area but not of the specific research environment e.g. ‘in primary care.’
10. Description of research setting is made but is lacking detail e.g. ‘in primary care practices in region [x]’.
11. Specific description of the research setting and target population of study e.g. ‘nurses and doctors from GP practices in [x] part of [x] city in [x] country.
4. The study design is appropriate to address the stated research aim/s
12. No research aim/s stated or the design is entirely unsuitable e.g. a Y/N item survey for a study seeking to undertake exploratory work of lived experiences.
13. The study design can only address some aspects of the stated research aim/s e.g. use of focus groups to capture data regarding the frequency and experience of a disease.
14. The study design can address the stated research aim/s but there is a more suitable alternative that could have been used or used in addition e.g. addition of a qualitative or quantitative component could strengthen the design.
15. The study design selected appears to be the most suitable approach to attempt to answer the stated research aim/s.
5. Appropriate sampling to address the research aim/s
16. No mention of the sampling approach.
17. Evidence of consideration of the sample required e.g. the sample characteristics are described and appear appropriate to address the research aim/s.
18. Evidence of consideration of sample required to address the aim. e.g. the sample characteristics are described with reference to the aim/s.
19. Detailed evidence of consideration of the sample required to address the research aim/s. e.g. sample size calculation or discussion of an iterative sampling process with reference to the research aims or the case selected for study.
6. Rationale for choice of data collection tool/s
20. No mention of rationale for data collection tool used.
21. Very limited explanation for choice of data collection tool/s. e.g. based on availability of tool.
22. Basic explanation of rationale for choice of data collection tool/s. e.g. based on use in a prior similar study.
23. Detailed explanation of rationale for choice of data collection tool/s. e.g. relevance to the study aim/s, co-designed with the target population or assessments of tool quality.
7. The format and content of data collection tool is appropriate to address the stated research aim/s
24. No research aim/s stated and/or data collection tool not detailed.
25. Structure and/or content of tool/s suitable to address some aspects of the research aim/s or to address the aim/s superficially e.g. single item response that is very general or an open-response item to capture content which requires probing.
26. Structure and/or content of tool/s allow for data to be gathered broadly addressing the stated aim/s but could benefit from refinement. E.g., the framing of survey or interview questions are too broad or focused to one element of the research aim/s.
27. Structure and content of tool/s allow for detailed data to be gathered around all relevant issues required to address the stated research aim/s.
8. Description of data collection procedure
28. No mention of the data collection procedure.
29. Basic and brief outline of data collection procedure e.g. ‘using a questionnaire distributed to staff’.
30. States each stage of data collection procedure but with limited detail or states some stages in detail but omits others e.g. the recruitment process is mentioned but lacks important details.
31. Detailed description of each stage of the data collection procedure, including when, where and how data was gathered such that the procedure could be replicated.
9. Recruitment data provided
32. No mention of recruitment data.
33. Minimal and basic recruitment data e.g. number of people invited who agreed to take part.
34. Some recruitment data but not a complete account e.g. number of people invited and agreed.
35. Complete data allowing for full picture of recruitment outcomes e.g. number of people approached, recruited, and who completed with attrition data explained where relevant.
10. Justification for analytic method selected
36. No mention of the rationale for the analytic method chosen.
37. Very limited justification for choice of analytic method selected. E.g. previous use by the research team.
38. Basic justification for choice of analytic method selected e.g. method used in prior similar research.
39. Detailed justification for choice of analytic method selected e.g. relevance to the study aim/s or comment around of the strengths of the method selected.
11. The method of analysis was appropriate to answer the research aim/s
40. No mention at all.
41. Method of analysis can only address the research aim/s basically or broadly.
42. Method of analysis can address the research aim/s but there is a more suitable alternative that could have been used or used in addition to offer a stronger analysis, e.g. for qualitative interpretative phenomenological analysis might be considered preferable for experiences vs. content analysis to elicit frequency of occurrence of events.
43. Method of analysis selected is the most suitable approach to attempt answer the research aim/s in detail
12. Evidence that the research stakeholders have been considered in research design or conduct.
44. No mention at all.
45. Consideration of some the research stakeholders e.g. use of pilot study with target sample but no stakeholder involvement in planning stages of study design
46. Evidence of stakeholder input informing the research. E.g., use of pilot study with feedback influencing the study design/conduct or reference to a project reference group established to guide the research.
47. Substantial consultation with stakeholders identifiable in planning of study design and in preliminary work e.g. consultation in the conceptualization of the research, a project advisory group or evidence of stakeholder input informing the work.
13. Strengths and limitations critically discussed
48. No mention at all.
49. Very limited mention of strengths and limitations with omissions of many key issues. E.g., one or two strengths/limitations mentioned with limited detail.
50. Discussion of some of the key strengths and weaknesses of the study but not complete. E.g. several strengths/limitations explored but with notable omissions or lack of depth of explanation.
51. Thorough discussion of strengths and limitations of all aspects of study including design, methods, data collection tools, sample & analytic approach
Included studies were also critically appraised by two independent reviewers (MW and AJ) for risk of bias, using tools appropriate for each research design. Cross-sectional studies were evaluated with the “Appraisal Tool for Cross-Sectional Studies (AXIS)” [30] Table 4. The standardized Joanna Briggs Institute (JBI) critical appraisal checklists were used for qualitative research [32] Table 5, and for case-control studies [31] Table 6. Disagreements between reviewers were resolved through discussion or consultation with a third reviewer.
Table 4.
Risk of bias assessment using AXIS tool for cross-sectional design risk of bias
| Author / Year | Introduction | Methods | Results | Discussion | Other | Total Out of 20 | Quality | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13a | 14 | 15 | 16 | 17 | 18 | 19a | 20 | |||
| Al Agili et al., (2004) [35] | 1 | 1 | 0 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | x | 1 | 14 | M |
| Al Habashneh et al., (2012) [60] | 1 | 1 | 0 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 17 | H |
| AlHammad et al., (2020) [45] | 1 | 1 | 0 | 1 | x | x | x | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 10 | M |
| Allison et al., (2000) [36] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | x | 14 | M |
| Al-shehri., (2012) [64] | 1 | 1 | 0 | 1 | 0 | 0 | x | 1 | 1 | 1 | 1 | 1 | x | 0 | 1 | 1 | 1 | 1 | x | 1 | 13 | M |
| Alshihri et al., (2021) [46] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 16 | H |
| Barry et al., (2014) [37] | 1 | 1 | 1 | 1 | 1 | 0 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | x | 1 | 16 | H |
| Bhaskar et al., (2016) [47] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 15 | H |
| Brickhouse et al., (2009) [48] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | x | 1 | 17 | H |
| Chi et al., (2010) [61] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 18 | H |
| De Jongh et al., (2008) [49] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | x | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | x | 1 | 16 | H |
| de Souza et al., (2023) [42] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | x | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 17 | H |
| Fenning et al., (2020) [65] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 18 | H |
| Gerreth et al., (2016) [50] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | x | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | x | 1 | 12 | M |
| Holt & Parry, (2019) [51] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 13 | M |
| Hu & Da Silva, (2022) [44] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 18 | H |
| Kachwinya et al., (2022) [62] | 1 | 1 | 1 | 1 | 0 | 0 | x | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 15 | H |
| Krishnan et al., (2018) [52] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 14 | M |
| Lai et al., (2012) [53] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 16 | H |
| Liu et al., (2022) [40] | 1 | 1 | 0 | 1 | 0 | 0 | x | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 10 | M |
| Nelson et al., (2011) [14] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | x | 1 | 17 | H |
| Puthiyapurayil et al., (2022) [56] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | x | 1 | 16 | H |
| Rajput et al., (2021) [57] | 1 | 1 | 1 | 1 | 1 | 0 | x | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 14 | M |
| Sabbarwal et al., (2018) [43] | 1 | 1 | 1 | 1 | 0 | 1 | x | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 16 | H |
| Schultz et al., (2001) [34] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | x | 1 | 14 | M |
| Shyama et al., (2015) [58] | 1 | 1 | 0 | 1 | 0 | 0 | x | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | x | 1 | 12 | M |
| Stein et al., (2012) [59] | 1 | 1 | 0 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | x | 1 | 15 | H |
| Zahran et al., (2023) [66] | 1 | 1 | 1 | 1 | 1 | 1 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 18 | H |
| Zhou et al., (2021) [63] | 1 | 1 | 0 | 1 | 1 | 0 | x | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 16 | H |
| Zickafoose et al., (2015) [67] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | x | 1 | 17 | H |
Y Yes = 1, N No = 0, DK Don’t know = x
aItem is reverse scored
low-quality (L) scores range from 1-7 (RED), medium quality (M) from 8-14 (Yellow), and high quality (H) scores range from 15-20 (Green)
Items:
1. Were the aims/objectives of the study clear?
2. Was the study design appropriate for the stated aim(s)?
3. Was the sample size justified?
4. Was the target/reference population clearly defined? (Is it clear who the research was about?)
5. Was the sample frame taken from an appropriate population base so that it closely represented the target/reference population under investigation?
6. Was the selection process likely to select subjects/participants that were representative of the target/reference population under investigation?
7. Were measures undertaken to address and categorise non-responders?
8. Were the risk factor and outcome variables measured appropriate to the aims of the study?
9. Were the risk factor and outcome variables measured correctly using instruments/measurements that had been trialled, piloted or published previously?
10. Is it clear what was used to determined statistical significance and/or precision estimates? (e.g. p-values, confidence intervals).
11. Were the methods (including statistical methods) sufficiently described to enable them to be repeated?
12. Were the basic data adequately described?
13. Does the response rate raise concerns about non-response bias?
14. If appropriate, was information about non-responders described?
15. Were the results internally consistent?
16. Were the results presented for all the analyses described in the methods?
17. Were the authors' discussions and conclusions justified by the results?
18. Were the limitations of the study discussed?
19. Were there any funding sources or conflicts of interest that may affect the authors’ interpretation of the results?
20. Was ethical approval or consent of participants attained?
Table 5.
Critical appraisal of qualitative studies using Joanna Briggs Institute (JBI) tools
| Author / Year | |||||
|---|---|---|---|---|---|
| Abduludin et al., (2019) [33] | Como et al., (2022) [41] | Junnarkar et al., (2023) [39] | Parry et al., (2023) [55] | Krishnan et al., (2018) [52] | |
| Q1: Is there congruity between the stated philosophical perspective and the research methodology? | Y | Y | Y | Y | Y |
| Q2: Is there congruity between the research methodology and the research question or objectives? | Y | Y | Y | Y | Y |
| Q3: Is there congruity between the research methodology and the methods used to collect data? | Y | Y | Y | Y | Y |
| Q4: Is there congruity between the research methodology and the representation and analysis of data? | Y | Y | Y | Y | Y |
| Q5: Is there congruity between the research methodology and the interpretation of results? | Y | Y | Y | Y | Y |
| Q6: Is there a statement locating the researcher culturally or theoretically? | N | N | N | N | N |
| Q7: Is the influence of the researcher on the research, and vice- versa, addressed? | N | N | N | U | N |
| Q8: Are participants, and their voices, adequately represented? | Y | Y | Y | Y | Y |
| Q9: Is the research ethical according to current criteria or, for recent studies, and is there evidence of ethical approval by an appropriate body? | Y | Y | Y | Y | Y |
| Q10: Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data? | Y | Y | Y | Y | Y |
Key: Y yes, N no, U unclear, NA not applicable
Table 6.
Critical appraisal of case control studies using Joanna Briggs Institute (JBI) tools
| Author / Year | ||
|---|---|---|
| Du et al., (2019) [38] | Mansoor et al., (2018) [54] | |
| Q1: Were the groups comparable other than the presence of disease in cases or the absence of disease in controls? | Y | Y |
| Q2: Were cases and controls matched appropriately? | Y | Y |
| Q3: Were the same criteria used for identification of cases and controls? | Y | Y |
| Q4: Was exposure measured in a standard, valid and reliable way? | NA | NA |
| Q5: Was exposure measured in the same way for cases and controls? | NA | NA |
| Q6: Were confounding factors identified? | Y | Y |
| Q7: Were strategies to deal with confounding factors stated? | N | N |
| Q8: Were outcomes assessed in a standard, valid and reliable way for cases and controls? | Y | Y |
| Q9: Was the exposure period of interest long enough to be meaningful? | NA | NA |
| Q10: Was appropriate statistical analysis used? | Y | Y |
Key: Y yes, N no, U unclear, NA not applicable
Results
The PRISMA flowchart (Fig. 2) illustrates the search results. After screening and applying the eligibility criteria, a total of 36 studies were included in the review.
Study characteristics
The studies incorporated a range of research designs. The majority of these studies (29 out of 36) adopted a cross-sectional study design, representing 80 % of the total papers. The next most common types of studies were qualitative studies, accounting for 11 % of the included papers, followed by case-control comparative studies (2 studies, 6%), and finally, one Mixed Method study (3%). (See Table 1).
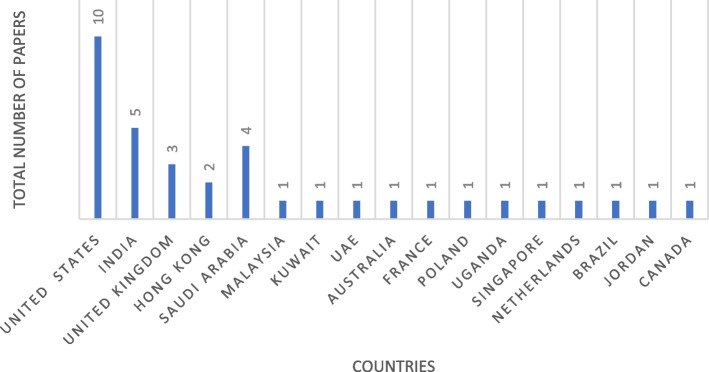
The studies included 17 different countries (See Fig. 3). Among the countries represented in the included studies, the United States (USA) emerged as the most prominent location, contributing 10 studies. These studies encompassed a wide range of sample sizes, varying from 10 participants [33] to a significantly larger cohort of 12,539 participants [34].
Fig. 3.
Total number of papers by country
The studies mentioned a diverse array of disabilities, such as Cerebral Palsy (CP), Autism Spectrum Disorder (ASD), Down Syndrome (DS), Intellectual and/or Developmental Disabilities (IDD), and Physical Disabilities. This broad scope allowed for a comprehensive exploration of the challenges and experiences faced by individuals living with different abilities.
Facilitators and barriers of access to oral health care for children with disabilities
The review identified factors that either facilitated or hindered access to oral healthcare for children with disabilities. These findings were categorized according to Levesque’s healthcare access framework, which organizes them based on dimensions and abilities. Table 1 presents a concise overview of the barriers and facilitators investigated in the included studies, and Table 2 provides a summary of the dimensions and abilities assessed within Levesque’s proposed framework. Included studies addressed barriers, but eight of them did not mention facilitators.
Dimensions of access
Approachability
The term “approachability” describes a provider’s characteristics that make it possible for people to know they exist and are reachable. This systematic review includes findings from seven studies that highlight both facilitators and barriers related to approachability. Dental outreach programs are identified as effective facilitators for enhancing approachability [33]. Conversely, the barriers to approachability include a lack of information about dentists competent to treat individuals with disabilities, as well as limited oral health awareness and knowledge of available services [35–40]. These barriers significantly hindered individuals’ access to and utilization of dental care services, thereby impacting approachability.
Acceptability
Nine of the included studies [33, 37–44] align with the “acceptability” dimension as defined by Levesque et al.’s conceptual framework [20]. These studies considered the influence of cultural and societal factors on individuals’ acceptance of specific aspects of dental care access.
The findings from these studies suggest that societal discrimination against individuals with disabilities, characterized by negative attitudes and discriminatory practices, significantly hindered their ability to access dental care [33, 40]. Some studies cited the presence of male caregivers and the existence of activity limitations associated with profound autism, as factors involved in barriers for individuals seeking dental care [42]. Moreover, individuals with complex medical conditions or more urgent healthcare needs may face difficulties in accessing dental care, leading to reduced acceptability of services [43]. The Acceptability domain failed to identify any facilitators.
Availability/ accommodation
Within the scope of this systematic review, 26 out of the 36 studies included in the analysis contributed insights related to the “availability/accommodation” dimension, specifically addressing barriers and facilitators associated with dental care access [14, 33, 35–41, 44–59]. Barriers linked to availability included the proximity of parking at dental clinics, challenges related to transportation and geographical distance from dental clinics. Other barriers included the absence of reasonable adjustments for accessing dental surgeries, difficulties in locating dentists willing to treat children with specific medical conditions, a shortage of dentists experienced in treating children with intellectual disabilities and prolonged waiting times for appointments or in waiting rooms.
Facilitators enhancing availability included the presence of diverse dental services providing needed care for individuals with disabilities [45, 58, 59], dentists demonstrating willingness to treat children [57], treatment availability, accessibility, and improved facilities in dental clinics.
Affordability
The issue of affordability appeared in twenty-two of the included studies [14, 33, 35, 37–41, 43, 44, 46, 47, 49, 50, 53, 57, 58, 60–64]. One of the most prevalent barriers hindering children with disabilities from accessing dental care is the prohibitively high cost of dental treatment, compounded by financial constraints and ineligibility for healthcare insurance [64]. However, reducing the cost of dental treatment can significantly enhance affordability and accessibility for children [33]. Consequentially, improving access to free dental care services has the potential to increase utilization rates among children with disabilities [33]. Another valuable facilitator is insurance coverage, for those who can afford it, which further enables access to dental care [35, 37].
Appropriateness
Barriers to dental care access for children with disabilities encompass multiple factors. These include the lack of family support [33]. Negative past experiences with dental services can create anxiety and reluctance [33, 59]. A shortage of behavior management skills among general practitioners [36], discomfort experienced by children during dental procedures [37, 64], and the reluctance of some dentists to treat children with disabilities can all affect the appropriateness of care [38, 39, 50, 59]. Furthermore, communication challenges [50] and the limited training and awareness of dental professionals about sensory issues in conjunction with the unique traits of children with disabilities can all hinder appropriate care [55].
Alternatively, facilitators contributing to the appropriateness of dental care access for children with disabilities include the presence of dental staff with positive attitudes [33] and interaction between the medical and dental systems through integrated care [61]. Parental positive attitudes and increased awareness of oral health encourages regular dental care, which enhances appropriateness [38, 43]. Real-time communication tools [51], coping strategies, and immersive empathy from the oral health team alleviates anxiety and ensures the acceptance of dental treatment [55]. Moreover, tailored communication, preparation, and support [55], along with the expertise of dental professionals who are trained to work with children with special health care needs [59], all play significant roles in improving the appropriateness of dental care for children with disabilities.
Abilities related to access
Several specific abilities relate to accessing oral healthcare. These include perceive, seek, reach, pay, and engage. Ability to perceive focuses on individuals’ awareness and understanding of available healthcare services. Ability to seek focuses on individuals’ initiative to look for oral healthcare services. Ability to reach refers to the geographical accessibility of oral healthcare facilities. Ability to pay refers to the financial ability to afford oral healthcare services. Ability to engage refers to individuals’ involvement and participation in their own oral healthcare.
Ability to perceive
Twenty-three studies discuss the ability to perceive the importance of dental care [14, 33, 36–40, 42–44, 47, 48, 53–57, 59, 60, 62–66]. Barriers include a lack of dental awareness among parents regarding oral health and availability of services [40, 56, 57, 60]. Often, there is little to no awareness of the importance of regular dental visits, contributing to limited perceptions of the necessity of ongoing dental care [60]. Some caregivers hold the belief that dental care is only essential for specific issues, such as swelling, cracked teeth with pain, or mobile teeth, providing evidence of a restricted understanding of the importance of regular dental visits [62]. Caregivers frequently perceive their child’s inability to cooperate with dental treatments [37, 47, 56]. They often express concerns about perceived behavioral challenges [14, 33, 37, 65]. The perception that children are too young for dental appointments [53] alongside the fear and anxiety children experience regarding dental care [14, 63], also present substantial barriers. Parental anxiety [63] and oral healthcare may have a lower priority compared to other healthcare needs for their child [14] and contribute to the challenges. Barriers related to children themselves including a lack of complaints expressed by children [54], children may face difficulties in recognizing dental pain and staff encounter challenges in facilitating communication [37]. These barriers collectively emphasize the need for the provision of tailored approaches and interventions to improve the perception of the importance of dental care among both caregivers and children with disabilities. Facilitators for enhancing the perception of the need for oral health care encompass various factors. Research suggests that the association between general health issues and parental health behaviors contributes to the recognition of dental care needs [37, 40, 43, 58, 65]. For example, children with Down Syndrome (DS) are more likely to seek dental care if they are also receiving speech therapy and ophthalmology services, illustrating a connection between overall health concerns and dental care [36]. Knowledge of oral health, active participation in oral healthcare programs [42] and caregiver education [44, 57, 63–66] also serve as facilitators. Providing parents with coping strategies and techniques tailored to autistic children [39] improves access to dental care, contributing to the ability to perceive the need for dental care.
Ability to seek
The ability to seek healthcare is influenced by various factors that impact individuals’ autonomy and choice to seek care. Barriers identified in the studies include difficulties and discomfort experienced by children with Autism Spectrum Disorder (ASD) during dental procedures [37], negative experiences with healthcare professionals [41], limited access to routine oral care among children belonging to ethnic minorities [49], perceived child IQ and behavioral issues [65]. These barriers hinder the ability to seek healthcare, resulting in disparities in accessing appropriate care.
On the other hand, facilitators identified include children’s age and parents’ educational attainment [63]. Older children may possess a better understanding and ability to express their healthcare needs, which facilitates their ability to seek care. Higher levels of education appear to facilitate parent acquisition of knowledge about healthcare options, enabling them to make informed decisions and actively seek necessary care for their children [63, 64].
Ability to reach
“Ability to Reach,” in 17 included studies, identify barriers primarily focusing on personal mobility and transportation availability, affecting individuals’ ability to physically reach healthcare providers [14, 33, 35, 37, 39, 40, 42, 44, 47, 50, 53, 56–58, 62–64]. These barriers encompass issues such as proximity of parking at clinics [33], lack of transportation [35, 50], difficulties in transportation [37, 47, 53, 62, 64], long travel distances, waiting times, challenges related to wheelchair access [40], limited access due to the scarcity of nearby dentists, insufficient time for visits, high travel costs, and time-consuming appointments. No studies mentioned facilitators of access.
Ability to pay
Fifteen studies explore barriers and facilitators related to the dimension of “ability to pay”, for dental care access for children with disabilities [33–35, 40, 41, 44, 48, 52, 53, 56, 57, 61, 62, 66, 67]. Barriers related to financial constraints, low income [34, 40, 56, 62], and a lack of insurance coverage [41, 48, 53, 67]. Facilitators within this domain were private insurance coverage, free treatment options [33], and insurance programs designed to provide dental care for vulnerable populations [35, 48, 67].
Ability to engage
Twenty-five studies discuss the ability to engage [33, 36–38, 40, 42–54, 56–59, 64–66], identifying numerous barriers to engaging children with disabilities in dental care. These obstacles range from children’s hesitance towards dental treatment [45] to difficulties experienced by children with ASD during dental procedures [37] and their perceived lack of cooperation during dental care [47]. Challenging behaviors, emerged from the fear of the dentist [52], which further compounds barriers. The anxiety of dental staff and concerns about uncooperative behavior or fear-related issues also hinder engagement [38]. Effective communication has been identified as a pivotal facilitator for dental care utilization [57]. Some studies suggest that having a milder degree of intellectual disability as a facilitator of access [50], suggesting that children with less severe intellectual disabilities may find it easier to engage with dental care compared to those with more significant communication impairments. Alternatively, dental staff may find it easier to communicate. It also suggests that dental professionals lack effective communication skills. These multifaceted barriers underscore the need for tailored strategies to enhance engagement among children with disabilities in accessing dental care.
Quality and risk of bias assessment
All included papers in this systematic review were rated for quality using the QuADS criteria [29]. (See Table 3). These revealed a mixed picture regarding the methodological rigor of the studies. Scores ranged from 36 to 85%, indicating varying levels of quality. While some studies demonstrated explicit theoretical or conceptual frameworks, clear descriptions of the research setting, and appropriate sampling methods, others lacked these crucial elements. The choice and justification of data collection tools and analytic methods varied, with some studies offering detailed justification and explanation, whilst others offered rudimentary accounts. Furthermore, few studies actively engaged stakeholders in the research design [14, 33, 52], for example, in one study stakeholders were actively involved [33], they formed an expert review committee and conducted pilot interviews with five caregivers to gather feedback on the clarity and language of the interview guide. The collaborative efforts resulted in a refined and validated Malay version of the guide, evidencing the active role of stakeholders in shaping the research design and ensuring methodological quality. Whereas only a limited number of studies provided comprehensive discussions of their strengths and limitations [36, 42, 44, 48, 59, 60, 63, 67].
The study used the appraisal tool for cross-sectional studies (AXIS), detailed in Table 4, revealed several key findings across different study designs. Out of the 29 cross-sectional studies, 11 were medium and 18 high quality, demonstrating a low risk of bias. Studies commonly demonstrated clarity in aims and appropriate study design for the study question. Many of them used sampling frame that makes the results fairly generalizable (such as registries), however, many lacked justifications for sample size as well as detailed statistical methods, as seen in AlHammad et al. [45]. And almost all of them were unclear in terms of dealing with non-responders, raising concern about potential difference between responders and non-responders which might affect how representative the sample is. It worth mentioning that each study used different measures/ questions of access to oral health care services, but all used relevant ways to assess the research aim. Qualitative studies, like those by Abduludin et al. [33] and Parry et al. [55], they were generally well-aligned between methodologies and research questions but often failed to address the influence of researchers and their theoretical positioning on their study findings. Case-control studies, exemplified by Du et al. [38] and Mansoor et al. [54], demonstrated good comparability and valid outcome measurements but frequently did not explicitly state strategies to address confounding factors. Across all designs, ethical standards were typically well-maintained, though improvements in sample justification, detailed data analysis, and addressing researcher influence were needed.
Discussion
This study systematically reviewed barriers and facilitators of oral healthcare access for children with disabilities, adopting Levesque et al.’s healthcare model of access as an a priori framework [20]. Among the 36 studies included, the majority (31 out of 36) explored specific dimensions and abilities of access to healthcare, though not all aspects were equally covered.
The main findings of the review were that only 7 out of 36 studies mentioned or indicated approachability, which ignores the contribution of healthcare professionals in the oral healthcare encounter, 9 out of 36 studies mentioned acceptability, whilst 12 out of 36 mentioned appropriateness, therefore failing to consider issues such as reasonable adjustments. In contrast, 24 out of 36 studies focused on the patient’s ability to engage. This discrepancy suggests that there may be a prevailing attitude that children with disabilities are the “problem” rather than recognizing that the barriers lie within the oral healthcare system itself. This observation aligns with the medical model of care, which views individuals as the issue, as opposed to the social model of disability [26], which focuses on the barriers imposed by the healthcare system. Moreover, children with profound autism and complex medical conditions face additional obstacles in accessing dental care, highlighting the need for a social model of disability to address systemic challenges.
Accessing dental care for carers of children with disabilities presents a range of barriers. Limited oral health awareness and knowledge of available services [35–40], coupled with a lack of information and awareness about dentists willing to treat children with disabilities [40], all contribute to difficulties in finding suitable dental providers. There is a shortage of dentists experienced in treating children with intellectual disabilities, plus a lack of dentists’ knowledge and training in providing care further restricts access to appropriate dental care [48, 49]. The difficulties faced by dentists while treating children with disabilities may stem from inadequate education and training in this area. Research argues that special care dentistry is often omitted from dental curricula [68, 69], leaving future dentists ill-prepared to interact with and treat individuals with disabilities. This highlights the need for comprehensive dental education programs that prepare undergraduate dental students to effectively interact with and treat children with disabilities [70]. Increasing the exposure of dental students to patients with disabilities has proven to enhance their skills, foster positive attitudes, and boost their competence and confidence [71, 72]. Therefore, targeted training for future dental professionals can play a crucial role in supporting the inclusion of children with disabilities in oral health initiatives and reducing oral health disparities.
While the included studies shed light on barriers to dental care access, the discussion around facilitators lacks consistency. Dental outreach programs [33], parental education [57, 63, 65], and collaboration between medical and dental systems [61] have significant potential to improve oral health outcomes and accessibility for children with disabilities. Ensuring parents and caregivers have appropriate and accessible information and health education appears vital to overcoming barriers [73]. Collaborative and multidisciplinary care emphasizes the benefits of continuity of care when patients interact with multiple services [36].
The systematic review has demonstrated that there is a broad international interest in the area, with evidence from a number of countries. This diversity enhances the generalizability of the findings, offering a comprehensive view that spans multiple research environments and contexts. The prominent contributions from countries like the United States and India highlight regions with strong research infrastructure and focus. Meanwhile, the involvement of other nations underscores the universal relevance and collaborative nature of the research field, reflecting a global commitment to advancing knowledge.
Strengths and limitations
The strength of this systematic review lies in its use of a conceptual framework to synthesize findings on oral healthcare access, mapping barriers and facilitators to provider and user characteristics, dimensions and abilities. Employing a systematic and comprehensive approach in collecting and identifying papers minimized the likelihood of missing relevant studies. The methodology used establishes a transparent link between the primary research and the conclusions drawn in this review. The inclusion of multiple reviewers in all study stages also served to reduce selection bias. However, using an existing framework poses a potential limitation, risking oversight of other relevant themes. To address this concern, all authors independently conducted searches for additional themes that could enhance the framework but failed to identify any. Only five papers included in this review adopted a theoretical model of access as a framework to guide the research. Two studies [33, 44] used Levesque’s framework, another [52] employed the Institution of Medicine model of healthcare utilization, one [53] applied the Behavioral Model of Health Services Use, finally, one [40] utilized the Modified Penchansky’s 5A classification. While the remaining 31 included papers did not incorporate a theoretical model of access. Nevertheless, the adoption of Levesque’s framework allowed consolidation of the barriers and facilitators to dental care access from multiple studies, enabling categorization into the five dimensions and five abilities, resulting in a more comprehensive overview.
Implications and future recommendations
This mixed methods systematic review contributes to understanding the complex landscape of oral healthcare access for children with disabilities. Applying Levesque et al.’s [20] theoretical framework provides a comprehensive understanding of barriers and facilitators affecting access. Identified barriers have implications for policymakers, healthcare providers, and educational institutions. This includes collaboration between dental and other medical systems, which appears vital to ensure coordinated and comprehensive care and assists in ensuring the provision of multidisciplinary care. Reducing the cost of dental treatment, insurance coverage, and/or providing access to free or subsidized dental care services for individuals with disabilities are crucial facilitators. Exposing dental professionals to individuals with disabilities during learning years and improving their communications skills with different patients’ group can enhance their skills, confidence, and willingness to provide care to individuals with disabilities. Adopting the social model of disability shifts the focus from individuals as the “problem” to systemic barriers, demanding attention.
Future recommendations include studies employing rigorous methodologies and involving various stakeholders such as children, parents/guardians, dental professionals, and policymakers. Utilizing comprehensive and up-to-date frameworks like Levesque’s conceptual framework enables a deeper exploration of the barriers and facilitators associated with oral health care services for children with disabilities. Addressing barriers and leveraging facilitators, provides the foundations for equitable access to oral healthcare for children with disabilities. This aims to improve their oral health outcomes and contribute to their overall well-being and quality of life.
Conclusions
This review highlights the diverse and global interest in addressing oral healthcare access for children with disabilities, reflecting a collaborative and universal commitment to improving health outcomes. The findings underscore the need for systemic changes, including better training for dental professionals, increased collaboration across healthcare systems, and policy adjustments to reduce financial barriers. By focusing on both barriers and facilitators, this review provides a pathway towards more equitable and effective oral healthcare services for children with disabilities.
Supplementary Information
Additional file 1: Search terms and strategies
Acknowledgements
The authors extend their appreciation to the King Salman Center For Disability Research for funding this work through Research Group no KSRG-2023-171.
Abbreviations
- UNICEF
The United Nations Children’s International Emergency Fund
- QuADS
Quality Appraisal for Diverse Studies
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- AXIS
Appraisal Tool for Cross-Sectional Studies
- JBI
The standardized Joanna Briggs Institute
Authors’ contributions
M.A. and J.O: Conceived the ideas, M.A. conducted data collection and analysis, and led the writing process. A.J. and J.O. Contributed to data collection and analysis, and actively participated in the writing. S.B. Provided insights on methods, supported data analysis, and offered feedback on the draft. All authors contributed to manuscript revisions.
Funding
The research was funded by the King Salman Center For Disability Research through Research Group no KSRG-2023-171.
Availability of data and materials
All data analyzed during this study are included in this manuscript.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable in this section.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNICEF. Seen, Counted, Included: Using data to shed light on the well-being of children with disabilities. 2021. https://data.unicef.org/resources/children-with-disabilities-report-2021/. Accessed 5 Nov 2023.
- 2.World Health Organization. International Classification of Functioning, Disability and Health (ICF). 2023. https://www.who.int/classifications/international-classification-of-functioning-disability-and-health Accessed 5 Nov 2023.
- 3.Allerton LA, Welch V, Emerson E. Health inequalities experienced by children and young people with intellectual disabilities: a review of literature from the United Kingdom. J Intellect Disabil. 2011;15:269–78. 10.1177/1744629511430772 [DOI] [PubMed] [Google Scholar]
- 4.Zhou N, Wong HM, Wen YF, McGrath C. Oral health status of children and adolescents with intellectual disabilities: a systematic review and meta-analysis. Dev Med Child Neurol. 2017;59:1019–26. 10.1111/dmcn.13486 [DOI] [PubMed] [Google Scholar]
- 5.Hong CL, Broadbent JM, Thomson WM, Poulton R. The Dunedin Multidisciplinary Health and Development Study: oral health findings and their implications. J Royal Soc N Z. 2020;50:35–46. 10.1080/03036758.2020.1716816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norwood KW Jr, Slayton RL,Council on Children With D, Section on Oral H, Liptak GS, Murphy NA, et al. Oral health care for children with developmental disabilities. Pediatrics. 2013;131:614–9. 10.1542/peds.2012-3650 [DOI] [PubMed] [Google Scholar]
- 7.Zhou N, Wong HM, McGrath C. Oral health and associated factors among preschool children with special healthcare needs. Oral Dis. 2019;25:1221–8. 10.1111/odi.13057 [DOI] [PubMed] [Google Scholar]
- 8.Cermak SA, Stein Duker LI, Williams ME, Dawson ME, Lane CJ, Polido JC. Sensory adapted dental environments to enhance oral care for children with autism spectrum disorders: a randomized controlled pilot study. J Autism Dev Disord. 2015;45:2876–88. 10.1007/s10803-015-2450-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein LI, Polido JC, Cermak SA. Oral care and sensory over-responsivity in children with autism spectrum disorders. Pediatr Dent. 2013;35:230–5. [PubMed] [Google Scholar]
- 10.Zhou N, Wong HM, McGrath CPJ. A multifactorial analysis of tooth-brushing barriers among mentally challenged children. J Dent Res. 2019;23:1587–94. [Google Scholar]
- 11.National Research Council. Informal caregivers in the United States: prevalence, caregiver characteristics, and ability to provide care. In: Olson S, editor. The role of human factors in home health care: Workshop summary. US: National Academies Press; 2010. [Google Scholar]
- 12.Porterfield SL, McBride TD. The effect of poverty and caregiver education on perceived need and access to health services among children with special health care needs. Am J Public Health. 2007;97:323–9. 10.2105/AJPH.2004.055921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adyanthaya A, Sreelakshmi N, Ismail S, Raheema M. Barriers to dental care for children with special needs: general dentists’ perception in Kerala, India. J Indian Soc Pedod Prev Dent. 2017;35:216–22. 10.4103/JISPPD.JISPPD_152_16 [DOI] [PubMed] [Google Scholar]
- 14.Nelson LP, Getzin A, Graham D, Zhou J, Wagle EM, McQuiston J, et al. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent. 2011;33:29–36. [PubMed] [Google Scholar]
- 15.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208. [PMC free article] [PubMed] [Google Scholar]
- 16.Aday LA, Andersen RM. Equity of access to medical care: a conceptual and empirical overview. Med Care. 1981;19(12):4–27. 10.1097/00005650-198112001-00004 [DOI] [PubMed] [Google Scholar]
- 17.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- 18.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273. [PMC free article] [PubMed] [Google Scholar]
- 19.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–40. 10.1097/00005650-198102000-00001 [DOI] [PubMed] [Google Scholar]
- 20.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:1–9. 10.1186/1475-9276-12-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krishnan L, Iyer K, Madan Kumar PD. Barriers to utilisation of dental care services among children with special needs: a systematic review. Indian J Dent Res. 2020;31:486–93. 10.4103/ijdr.IJDR_542_18 [DOI] [PubMed] [Google Scholar]
- 22.da Rosa SV, Moysés SJ, Theis LC, Soares RC, Moysés ST, Werneck RI, et al. Barriers in access to dental services hindering the treatment of people with disabilities: a systematic review. Int J Dent. 2020;2020:1–17. 10.1155/2020/9074618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Owens J, Mistry K, Thomas AD. Access to dental services for people with learning disabilities: quality care? Br J Disabil Oral Health. 2011;12:17–27. [Google Scholar]
- 24.Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Implement. 2021;19:120–9. 10.1097/XEB.0000000000000282 [DOI] [PubMed] [Google Scholar]
- 25.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 26.Oliver M. Understanding disability: From theory to practice. UK: Bloomsbury Publishing; 2018. [Google Scholar]
- 27.Alborz A, McNally R, Glendinning C. Access to health care for people with learning disabilities in the UK: mapping the issues and reviewing the evidence. J Health Serv Res Policy. 2005;10:173–82. 10.1258/1355819054338997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.ResearchSoft. T. Endnote 9. Stamford, CT: The Thomson Corporation; 2005. http://endnote.com/. Accessed 5 Nov 2023
- 29.Harrison R, Jones B, Gardner P, Lawton R. Quality assessment with diverse studies (QuADS): an appraisal tool for methodological and reporting quality in systematic reviews of mixed-or multi-method studies. BMC Health Serv Res. 2021;21:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016;6:e011458. 10.1136/bmjopen-2016-011458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joanna Briggs I. The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews. Critical Appraisal Checklist for Cohort Studies. 2017. https://jbi.global/critical-appraisal-tools. Accessed 5 May 2024.
- 32.Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. JBI Evid Implement. 2015;13:179–87. [DOI] [PubMed] [Google Scholar]
- 33.Abduludin DMA, Rahman NA, Adnan MM, Yusuf A. Experience of caregivers caring for children with cerebral palsy in accessing oral health care services: a qualitative study. Arch Orofac Sci. 2019;14(2):133–46. 10.21315/aos2019.14.2.381 [DOI] [Google Scholar]
- 34.Schultz ST, Shenkin JD, Horowitz AM. Parental perceptions of unmet dental need and cost barriers to care for developmentally disabled children. Pediatr Dent. 2001;23:321–5. [PubMed] [Google Scholar]
- 35.Al Agili DE, Roseman J, Pass MA, Thornton JB, Chavers LS. Access to dental care in Alabama for children with special needs: parents’ perspectives. J Am Dent Assoc. 1939;2004(135):490–5. [DOI] [PubMed] [Google Scholar]
- 36.Allison PJ, Hennequin M, Faulks D. Dental care access among individuals with Down syndrome in France. Spec Care Dentist. 2000;20:28–34. 10.1111/j.1754-4505.2000.tb00007.x [DOI] [PubMed] [Google Scholar]
- 37.Barry S, O’Sullivan EA, Toumba KJ. Barriers to dental care for children with autism spectrum disorder. Eur Arch Paediatr Dent. 2014;15:127–34. 10.1007/s40368-013-0075-y [DOI] [PubMed] [Google Scholar]
- 38.Du RY, Yiu CKY, King NM. Oral health behaviors of preschool children with autism spectrum disorders and their barriers to dental care. J Autism Dev Disord. 2019;49:453–9. 10.1007/s10803-018-3708-5 [DOI] [PubMed] [Google Scholar]
- 39.Junnarkar VS, Tong HJ, Hanna KMB, Aishworiya R, Duggal M. Qualitative study on barriers and coping strategies for dental care in autistic children: parents’ perspective. Int J Paediatr Dent. 2023;33:203–15. 10.1111/ipd.13035 [DOI] [PubMed] [Google Scholar]
- 40.Liu N, Drake M, Kruger E, Tennant M. Determining the barriers to access dental services for people with a disability: a qualitative study. Asia Pac J Health Manag. 2022;17(1):72–83. [Google Scholar]
- 41.Como DH, Florindez-Cox LI, Stein Duker LI, Cermak SA. Oral health barriers for African American caregivers of autistic children. Int J Environ Res Public Health. 2022;19(24):17067. 10.3390/ijerph192417067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Souza MLP, de Lima PDL, Herkrath FJ. Utilization of dental services by children with autism spectrum conditions: the role of primary health care. Spec Care Dent. 2023;44(1):175–83. 10.1111/scd.12837 [DOI] [PubMed] [Google Scholar]
- 43.Sabbarwal B, Puranik MP, Uma SR. Oral health status and barriers to utilization of services among down syndrome children in Bengaluru City: a cross-sectional, comparative study. J Indian Assoc Public Health Dent. 2018;16:4–10. 10.4103/jiaphd.jiaphd_138_17 [DOI] [Google Scholar]
- 44.Hu K, Da Silva K. Access to oral health care for children with fetal alcohol spectrum disorder: a cross-sectional study. BMC Oral Health. 2022;22:497. 10.1186/s12903-022-02561-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.AlHammad KAS, Hesham AM, Zakria M, Alghazi M, Jobeir A, AlDhalaan RM, et al. Challenges of autism spectrum disorders families towards oral health care in Kingdom of Saudi Arabia. Pesqui Bras Odontopediatria Clin Integr. 2020;20:e5178. 10.1590/pboci.2020.046 [DOI] [Google Scholar]
- 46.Alshihri AA, Al-Askar MH, Aldossary MS. Barriers to professional dental care among children with autism spectrum disorder. J Autism Dev Disord. 2021;51:2988–94. 10.1007/s10803-020-04759-y [DOI] [PubMed] [Google Scholar]
- 47.Bhaskar BV, Janakiram C, Joseph J. Access to dental care among differently-abled children in Kochi. J Indian Assoc Public Health Dent. 2016;14:29–34. 10.4103/2319-5932.178723 [DOI] [Google Scholar]
- 48.Brickhouse TH, Farrington FH, Best AM, Ellsworth CW. Barriers to dental care for children in Virginia with autism spectrum disorders. J Dent Child. 2009;76:188–93. [PubMed] [Google Scholar]
- 49.De Jongh AD, Van Houtem C, Van Der Schoof M, Resida G, Broers D. Oral health status, treatment needs, and obstacles to dental care among noninstitutionalized children with severe mental disabilities in The Netherlands. Spec Care Dentist. 2008;28:111–5. 10.1111/j.1754-4505.2008.00022.x [DOI] [PubMed] [Google Scholar]
- 50.Gerreth K, Borysewicz-Lewicka M. Access barriers to dental health care in children with disability. A questionnaire study of parents. J Appl Res Intellect Disabil. 2016;29:139–45. 10.1111/jar.12164 [DOI] [PubMed] [Google Scholar]
- 51.Holt S, Parry JA. Parent-reported experience of using a real-time text messaging service for dental appointments for children and young people with autism spectrum conditions: a pilot study. Spec Care Dentist. 2019;39:84–8. 10.1111/scd.12347 [DOI] [PubMed] [Google Scholar]
- 52.Krishnan L, Iyer K, Kumar PDM. Barriers in dental care delivery for children with special needs in Chennai, India: A mixed method research. Disabil CBR Incl Dev. 2018;29:68–82. 10.5463/dcid.v29i4.739 [DOI] [Google Scholar]
- 53.Lai B, Milano M, Roberts MW, Hooper SR. Unmet dental needs and barriers to dental care among children with autism spectrum disorders. J Autism Dev Disord. 2012;42:1294–303. 10.1007/s10803-011-1362-2 [DOI] [PubMed] [Google Scholar]
- 54.Mansoor D, Al Halabi M, Khamis AH, Kowash M. Oral health challenges facing Dubai children with Autism Spectrum Disorder at home and in accessing oral health care. Eur J Paediatr Dent. 2018;19:127–33. [DOI] [PubMed] [Google Scholar]
- 55.Parry JA, Newton T, Linehan C, Ryan C. Dental visits for autistic children: a qualitative focus group study of parental perceptions. JDR Clin Transl Res. 2023;8:36–47. 10.1177/23800844211049404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Puthiyapurayil J, Anupam Kumar TV, Syriac G, R M, Kt R, Najmunnisa. Parental perception of oral health related quality of life and barriers to access dental care among children with intellectual needs in Kottayam, Central Kerala‐A cross sectional study. Spec Care Dentist. 2022;42:177–86. 10.1111/scd.12658 [DOI] [PubMed] [Google Scholar]
- 57.Rajput S, Kumar A, Puranik MP, Sowmya KR, Chinam N. Oral health perceptions, behaviors, and barriers among differently abled and healthy children. Spec Care Dentist. 2021;41:358–66. 10.1111/scd.12573 [DOI] [PubMed] [Google Scholar]
- 58.Shyama M, Al-Mutawa SA, Honkala E, Honkala S. Parental perceptions of dental visits and access to dental care among disabled schoolchildren in Kuwait. Odontostomatol Trop Trop Dent J. 2015;38:34–42. [PubMed] [Google Scholar]
- 59.Stein LI, Polido JC, Najera SOL, Cermak SA. Oral care experiences and challenges in children with autism spectrum disorders. Pediatr Dent. 2012;34:387–91. [PubMed] [Google Scholar]
- 60.Al Habashneh R, Al-Jundi S, Khader Y, Nofel N. Oral health status and reasons for not attending dental care among 12-to 16-year-old children with Down syndrome in special needs centres in Jordan. Int J Dent Hyg. 2012;10:259–64. 10.1111/j.1601-5037.2012.00545.x [DOI] [PubMed] [Google Scholar]
- 61.Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. J Public Health Dent. 2010;70:35–44. 10.1111/j.1752-7325.2009.00141.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kachwinya SM, Kemoli AM, Owino R, Okullo I, Bermudez J, Seminario AL. Oral health status and barriers to oral healthcare among children with cerebral palsy attending a health care center in Kampala, Uganda. BMC Oral Health. 2022;22(1):656. 10.1186/s12903-022-02677-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou N, Wong HM, McGrath C. Dental visit experience and dental care barriers among Hong Kong preschool children with special education needs. Int J Paediatr Dent. 2021;31:699–707. 10.1111/ipd.12770 [DOI] [PubMed] [Google Scholar]
- 64.Al-Shehri SAM. Access to dental care for persons with disabilities in Saudi Arabia (Caregivers’ perspective). J Disabil Oral Health. 2012;13:51. [Google Scholar]
- 65.Fenning RM, Steinberg-Epstein R, Butter EM, Chan J, McKinnon-Bermingham K, Hammersmith KJ, et al. Access to dental visits and correlates of preventive dental care in children with autism spectrum disorder. J Autism Dev Disord. 2020;50:3739–47. 10.1007/s10803-020-04420-8 [DOI] [PubMed] [Google Scholar]
- 66.Zahran SS, Bhadila GY, Alasiri SA, Alkhashrami AA, Alaki SM. Access to dental care for children with special health care needs: a cross-sectional community survey within Jeddah. Saudi Arabia J Clin Pediatr Dentistry. 2023;47(1):50–7. [DOI] [PubMed] [Google Scholar]
- 67.Zickafoose JS, Smith KV, Dye C. Children with special health care needs in CHIP: access, use, and child and family outcomes. Acad Pediatr. 2015;15:S85–92. 10.1016/j.acap.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 68.Dao LP, Zwetchkenbaum S, Inglehart MR. General dentists and special needs patients: does dental education matter? J Dent Educ. 2005;69:1107–15. 10.1002/j.0022-0337.2005.69.10.tb04011.x [DOI] [PubMed] [Google Scholar]
- 69.DeLucia LM, Davis EL. Dental students’ attitudes toward the care of individuals with intellectual disabilities: relationship between instruction and experience. J Dent Educ. 2009;73:445–53. 10.1002/j.0022-0337.2009.73.4.tb04715.x [DOI] [PubMed] [Google Scholar]
- 70.Chávez EM, Subar PE, Miles J, Wong A, LaBarre EE, Glassman P. Perceptions of predoctoral dental education and practice patterns in special care dentistry. J Dent Educ. 2011;75:726–32. 10.1002/j.0022-0337.2011.75.6.tb05099.x [DOI] [PubMed] [Google Scholar]
- 71.Alumran A, Almulhim L, Almolhim B, Bakodah S, Aldossary H, Alrayes SA. Are dental care providers in Saudi Arabia prepared to treat patients with special needs? J Multidiscip Healthc. 2019;12:281–90. 10.2147/JMDH.S201155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Casamassimo PS, Seale NS, Ruehs K. General dentists’ perceptions of educational and treatment issues affecting access to care for children with special health care needs. J Dent Educ. 2004;68:23–8. 10.1002/j.0022-0337.2004.68.1.tb03730.x [DOI] [PubMed] [Google Scholar]
- 73.Liu H-Y, Chen J-R, Hsiao S-Y, Huang S-T. Caregivers’ oral health knowledge, attitude and behavior toward their children with disabilities. J Dent Sci. 2017;12:388–95. 10.1016/j.jds.2017.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Search terms and strategies
Data Availability Statement
All data analyzed during this study are included in this manuscript.