Abstract
Background
Sickle cell disease (SCD) is a common monogenic inheritable condition in sub-Saharan Africa. 30% of Ghanaians are estimated to be carriers creating a condition for stable SCD penetrance. Being inheritable, SCD is scientifically preventable through intentional spousal selection. This study therefore explored young adults’ knowledge, beliefs and prevention strategies regarding SCD.
Methods
This exploratory study employed a mixed-methods approach (semi-structured questionnaires and focus group discussion [FGD]) to explore the SCD knowledge and beliefs of participants (15–49 years). The data collection was intentionally sequential; initial administration of 386 questionnaires and then followed by the FGD (16 participants). FGD was thematically analysed whereas quantitative data was explored using structural equation modeling (SEM); p < 0.05 was considered statistically significant under two-tailed assumptions.
Results
Whereas 98.7% reported having heard about SCD, < 50% got the information through formal education. Overall, 49.7% knew their respective SCD status; the proportion increased with age (48.8% in < 30 years vs 64.4% in ≥ 30 years old), or higher degree status (48.8% in undergraduates vs 67.4% in postgraduates). Moreover, whereas nine-in-ten correctly identified that SCD is hereditable, three-in-ten believed that having a SCD child was a matter of fate. Our FGD revealed that whereas curses, and spiritual attack were misconceived as potential causes of SCD, stigmatization associated with SCD was a major concern. The SEM demonstrated that one’s knowledge about SCD prevention is significantly positively associated with relationship choices (b = 0.757, p < 0.05). Also, a participant’s knowledge about SCD preventive strategies was significantly associated with the individual’s beliefs about SCD (b = 0.335; p < 0.05). However, a participant’s SCD beliefs negatively mediated SCD preventive strategies-relationship choices association.
Conclusions
SCD beliefs likely transform linear quantitative associations into a complex non-linear interaction; public health campaigns ought to unearth and address SCD beliefs to maximize achieving the intended targets.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-024-01379-1.
Keywords: Sickle cell disease, Structural equation modeling, Mixed-methods, Focus group discussion
| Text box 1. Contributions to the literature |
|---|
| 1. Research has found knowledge gap to be a hindrance to public health interventional strategies aimed at addressing sickle cell disease (SCD). |
| 2. In spite of higher education, misconceptions were a major concern regarding SCD; whereas 30% of participants believed fate decides having a SCD child, others consider curses to cause of SCD. |
| 3. Participants’ knowledge about SCD prevention is significantly positively associated with relationship decisions. |
| 4. Beliefs about SCD negatively mediate application of relationship choice as a SCD prevention strategy. |
Background
Sickle cell disease (SCD) is a common monogenic disorder of haemoglobin that primarily affects people of African, Indian, Mediterranean and Middle Eastern ancestry. Since the gene controlling SCD is recessively inherited, only the homozygous state generally leads to clinical sequelae disease called sickle cell anaemia (SCA); the heterozygous state is however, generally clinically silent. At its 63rd session, the UN General Assembly adopted a resolution recognizing sickle-cell anaemia as a public health problem and subsequently urged Member States to employ annual SCD awareness creation to tackle the disease [1]. In Ghana, about 2% of newborns (approximately 15,000) are annually estimated to inherit SCD [2], with 55% of them having the homozygous form [3]; it is further estimated that 30% of Ghanaian adults are carriers [4]. Although the life expectancy of the Ghanaian SCD patient is not known, it is generally suggested that in view of improved medical care, increasingly more SCD children now survive into adulthood.
Being inheritable, SCD is scientifically preventable through an intentional spousal selection that either discourages at-risk individuals from marrying if they intend to give birth or take advantage of assistive reproductive technologies [5, 6]; alternatively, such at-risk couples could be counseled to consider adopting children. Previous studies have however, demonstrated a knowledge gap that hinders adequacy of education for at-risk groups [7, 8]. One of the effective interventional strategies that could be harnessed in SCD prevention is educational efforts targeting young people who are about starting to make reproductive decisions. Interventional strategies that prioritize increased knowledge to address long-held misconceptions and attitudes about SCD, and their attendant reproductive consequences could hypothetically yield greater chances of reducing SCD burden [9–11]. Tertiary students are majority youthful population as well as being mostly at the point of starting to plan their long-term relationships and reproductive decisions. They therefore represent a key group that could be targeted in any educational modalities that seeks to promote genetic literacy in order to interrupt the cycle of misinformation that is perpetuated by and within families [12]. Besides, these young adults if adequately informed about SCD, could eventually serve as ambassadors championing public health advocacy campaigns aimed at reducing SCD penetrance. SCD carrier screening and increased education at the university level are critical to reducing the spread of SCD because this is the level at which most students begin dating and selecting potential life partners [10, 13]. However, previous studies have reported that high-risk groups were ill-informed about SCD [14], inheritance patterns [8], as well as SCD’s reproductive repercussions [10]. This study therefore used mixed-methods approach as well as structural equation modeling to explore tertiary students’ knowledge and beliefs about SCD, SCD prevention strategies as well as how SCD knowledge ought to inform relationship choices.
Materials and methods
Study design
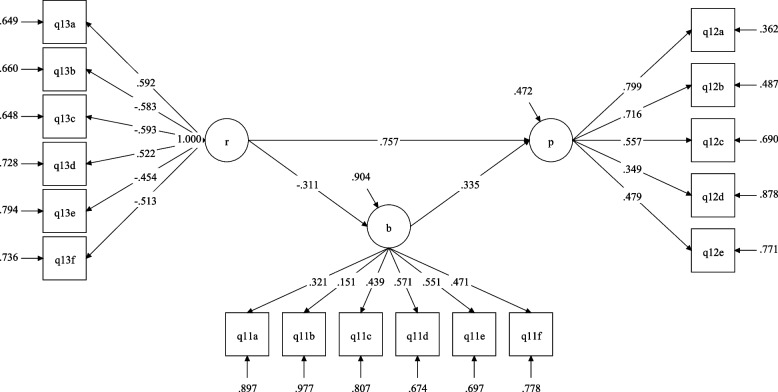
This was a cross-sectional study that employed mixed-methods approach, specifically through the use of a semi-structured questionnaires and focus group discussions to explore participants’ knowledge about sickle cell disease (Fig. 1). The data collection was intentionally sequential; administration of the questionnaires was completed and then followed by the focus group discussions. The investigation was carried out (from 2nd February to 22nd December 2022) at the main campus of the University of Cape Coast in the central region of Ghana. A convenience sampling technique was used to recruit eligible participants.
Fig. 1.
A flowchart illustrating participant recruitment and data collection strategies at University of Cape Coast from 2nd February to 22nd December 2022. SCD: sickle cell disease; SEM: structural equation modeling; FGD: focus group discussion
Study population
The sampling frame was the regular students of the University of Cape Coast. Information from the university’s website revealed that the university at the time of the study had a student population of about 74,710 of which 18,949 were regular undergraduate students, 1445 were sandwich undergraduate students, 1014 regular postgraduate students, 2773 sandwich postgraduate students, 48,989 distance undergraduate students and 1540 postgraduate distance students. Overall, the undergraduate student population constituted 92.9% of the student population.
Inclusion and exclusion criteria
The study included all University of Cape Coast regular students on campus. Students who were offering distance programmes or sandwich programmes were excluded because they were not on campus at the time of sampling and could not partake of the FGD. Also, students who did not provide written informed consent were excluded.
Sample size determination
At the time of the study, the total population of students of the University of Cape Coast (UCC) in the regular mode was determined as 19,963; 18,949 regular undergraduate students and 1014 regular postgraduate students. The desired sample size was estimated to be 377 using a 95% confidence level, a population proportion of 50%, and a 5% margin of error. In total, 300 printed questionnaires were distributed, 250 of them were fully completed and returned to the research team (return rate of 83.0%). Additionally, 136 students completed the online questionnaire. Therefore, 386 students completed the questionnaire in both printed and online forms.
Data collection procedures
Semi-structured questionnaire
Semi-structured questionnaires in the form of hard and online copies were used for the initial data collection. The questionnaire (supplementary file S1) consisted of five sections; demographic characteristics (section 1), knowledge about SCD (section 2), beliefs about SCD (section 3), prevention of SCD (section 4), and SCD and relationship choices (section 5). In the sections 3–5 of the questionnaires, students judged their agreement with specific statements on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The questionnaire was initially pre-tested using 19 random students (approximately 5% of the required sample size) to test for construct validity and clarity of items; inputs from this pilot study informed revision of the questionnaire items prior to large-scale data collection. The questionnaire was made accessible to students both online and in printed copy. The link for the online survey was sent to students via WhatsApp. The printed form was distributed in lecture halls, libraries, and students’ residences for individuals who wished to participate in the study. The raw questionnaire data in Excel format is enclosed as Supplementary file S2.
Focus group discussion
In the second phase of data collection, two sets of focus group discussions (FGDs), were undertaken to evaluate participants’ in-depth understanding of sickle cell disease. In all, sixteen (16) participants were involved in the FGD; nine (9) in the first session and seven (7) in the second session. Only individuals who had initially answered the questionnaires could participate in the FGD; participants indicated willingness to partake in the FGD during the questionnaire filling. The conversation was facilitated by a member of the study team and the supervisors with local dialect competencies. The group facilitator used these initial questions as a guide: What general knowledge participants had concerning sickle cell disease; what measures participants considered important to take to prevent sickle cell disease; what effects sickle cell disease have on afflicted people and society as a whole; and the possible implication(s) of inherited sickle cell disease and relationship choices. However, based on the initial responses, the facilitator probed further to explore participants’ SCD knowledge. Each focus group session lasted between 45 and 60 min, each was tape-recorded for the purpose of transcription. Although the FGD was conducted in English language, participants were encouraged to freely switch between local dialect (Twi/Fante) and English if that will aid better expression of their submissions. Even after consenting to be part of the FGD, individuals who were not willing to be recorded were excluded from the discussion. Participants were encouraged to use only their first names throughout the FGD. All FGDs were facilitated by trained research assistants and the supervisors with local dialect competencies, and took place at the School of Allied Health Science conference room II (SAHS-Room II), University of Cape Coast. In conformity with the COREQ guidelines [15], verbatim quotes were included in specific sections of the discussion accompanied by anonymous identifier to highlight participants’ expressed submissions.
Data analysis
The data obtained from the questionnaire and focus group discussion were analyzed using the SPSS version 26.0 (IBM Corp., USA). Prior to data analyses, Cronbach’s alpha (a = 0.5) was calculated to ensure the amended instrument had appropriate levels of validity before conducting data analyses. Descriptive statistics, such as frequency distributions and percentages were used to describe the data. Cross tabulations were used to determine if there were significant differences among groups; statistical significance level was determined at p < 0.05 under the two-tailed assumptions. In the data analyses presented in Tables 3, 4 and 5, the strongly agree and agree categories were merged as agree, whereas strongly disagree and disagree were also merged as “disagree” to ultimately provide three scales i.e., disagree, uncertain, and agree. However, in the structural equation model, the five item Likert scales were maintained. The themes that emerged from the questionnaire data analysis served as the guide for the two (2) focus group discussions. Data obtained from the focus group discussion was thematically analyzed to identify common themes and sub-themes that have been reported in this study.
Table 3.
Participants’ beliefs about sickle cell disease stratified by age and sex for an exploratory study at University of Cape Coast from 2nd February to 22nd December 2022
| Total | Sex | P-value | Age (years) | P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | 15–19 | 20–29 | 30–39 | ≥40 | ||||
| Sickle cell condition is a spiritual disease | 0.360 | 0.802 | |||||||
| Disagree | 356 (92.2) | 175 (93.1) | 181 (91.4) | 26 (83.9) | 280 (94.6) | 43 (82.7) | 7 (100.0) | ||
| Uncertain | 20 (5.2) | 7 (3.7) | 13 (6.6) | 4 (12.9) | 12 (4.1) | 4 (7.7) | 0 (0.00) | ||
| Agree | 10 (2.6) | 6 (3.2) | 4 (2.0) | 1 (3.2) | 4 (1.4) | 5 (9.6) | 0 (0.00) | ||
| Sickle cell condition can be prevented by personal choices | 0.173 | 0.347 | |||||||
| Disagree | 189 (49.0) | 96 (51.1) | 93 (47.0) | 19 (61.3) | 146 (49.3) | 22 (42.3) | 2 (28.6) | ||
| Uncertain | 61 (15.8) | 23 (12.2) | 38 (19.2) | 6 (19.4) | 46 (15.5) | 7 (28.6) | 2 (28.6) | ||
| Agree | 136 (35.2) | 69 (36.7) | 67 (33.8) | 6 (19.4) | 104 (35.1) | 23 (44.2) | 3 (42.9) | ||
| I may be stigmatized if people get to know that I have sickle cell disease | 0.654 | 0.136 | |||||||
| Disagree | 165 (42.7) | 83 (44.1) | 82 (41.4) | 9 (29.0) | 128 (43.2) | 26 (50.0) | 2 (28.6) | ||
| Uncertain | 89 (23.1) | 45 (23.9) | 44 (22.2) | 10 (32.3) | 71 (24.0) | 8 (15.4) | 0 (0.0) | ||
| Agree | 132 (34.2) | 60 (31.9) | 72 (36.4) | 12 (38.7) | 97 (32.8) | 18 (34.6) | 5 (71.4) | ||
| Knowing my sickle cell status will make me less confident about forming a relationship | 0.199 | 0.544 | |||||||
| Disagree | 227 (58.8) | 111 (59.0) | 116 (58.6) | 14 (45.2) | 176 (59.5) | 32 (61.5) | 5 (71.4) | ||
| Uncertain | 53 (13.7) | 31 (16.5) | 22 (11.1) | 7 (22.6) | 41 (13.9) | 5 (9.6) | 0 (0.0) | ||
| Agree | 106 (27.5) | 46 (24.5) | 60 (30.3) | 10 (32.3) | 79 (26.7) | 15 (28.8) | 2 (28.6) | ||
| Testing for sickle cell disease is painful and difficult | 0.501 | 0.011 | |||||||
| Disagree | 265 (68.7) | 124 (66.0) | 141 (71.2) | 17 (54.8) | 207 (69.9) | 34 (65.4) | 7 (100.0) | ||
| Uncertain | 85 (22.0) | 44 (23.4) | 41 (20.7) | 8 (25.8) | 69 (23.3) | 8 (15.4) | 0 (0.0) | ||
| Agree | 36 (9.3) | 20 (10.6) | 16 (8.1) | 6 (19.4) | 20 (6.8) | 10 (19.2) | 0 (0.0) | ||
| Having a child with sickle cell disease is a matter of fate as life is unpredictable | 0.009 | 0.328 | |||||||
| Disagree | 217 (56.2) | 100 (53.2) | 117 (59.1) | 13 (41.9) | 171 (57.8) | 27 (51.9) | 6 (85.7) | ||
| Uncertain | 53 (13.7) | 19 (10.1) | 34 (17.2) | 4 (12.9) | 41 (13.9) | 8 (15.4) | 0 (0.0) | ||
| Agree | 116 (30.1) | 69 (36.7) | 47 (23.7) | 14 (45.2) | 84 (28.4) | 17 (32.7) | 1 (14.3) | ||
The data is presented as frequencies n (%) with statistical significance at p < 0.05 determined using chi-square test
Table 4.
Participants’ knowledge about sickle cell disease prevention stratified by age and sex for an exploratory study at University of Cape Coast from 2nd February to 22nd December 2022
| Total | Sex | P-value | Age (years) | P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | 15–19 | 20–29 | 30–39 | ≥40 | ||||
| Sickle cell condition testing must be mandatory for all couples before marriage | 0.020 | 0.747 | |||||||
| Disagree | 27 (7.0) | 12 (6.4) | 15 (7.6) | 1 (3.2) | 21 (7.1) | 4 (7.7) | 1 (14.3) | ||
| Uncertain | 7 (1.8) | 0 (0.0) | 7 (3.5) | 0 (0.0) | 7 (2.4) | 0 (0.0) | 0 (0.0) | ||
| Agree | 352 (91.2) | 176 (93.6) | 176 (88.9) | 30 (96.8) | 268 (90.5) | 48 (92.3) | 6 (85.7) | ||
| It should be mandatory for all newborns to be tested for sickle cell condition | 0.268 | 0.384 | |||||||
| Disagree | 21 (5.4) | 9 (4.8) | 12 (6.1) | 0 (0.0) | 18 (6.1) | 2 (3.8) | 1 (14.3) | ||
| Uncertain | 26 (6.7) | 9 (4.8) | 17 (8.6) | 3 (9.7) | 22 (7.4) | 1 (1.9) | 0 (0.0) | ||
| Agree | 339 (87.8) | 170 (90.4) | 169 (85.4) | 28 (90.3) | 256 (86.5) | 49 (94.2) | 6 (85.7) | ||
| Two people who have sickle cell condition should be stopped from marrying | 0.071 | 0.890 | |||||||
| Disagree | 51 (13.2) | 19 (10.1) | 32 (16.2) | 3 (9.7) | 40 (13.5) | 8 (15.4) | 0 (0.0) | ||
| Uncertain | 47 (12.2) | 19 (10.1) | 28 (14.1) | 3 (9.7) | 38 (12.8) | 5 (9.6) | 1 (14.3) | ||
| Agree | 288 (74.6) | 150 (79.8) | 138 (69.7) | 25 (80.6) | 218 (73.6) | 39 (75.0) | 6 (85.7) | ||
| If I know that I am at risk of giving birth to a sickle cell child, it will change my pregnancy plans | 0.224 | 0.533 | |||||||
| Disagree | 71 (18.4) | 28 (14.8) | 43 (21.7) | 6 (19.4) | 52 (17.6) | 12 (23.1) | 1 (14.3) | ||
| Uncertain | 112 (29.0) | 57 (30.3) | 55 (27.8) | 8 (25.8) | 91 (30.7) | 13 (25.0) | 0 (0.0) | ||
| Agree | 203 (52.6) | 103 (54.8) | 100 (50.5) | 17 (54.8) | 153 (51.7) | 27 (51.9) | 6 (85.7) | ||
| Pastors/Imams should advise all prospective couples who have sickle cell disease from marrying | 0.165 | 0.110 | |||||||
| Disagree | 97 (25.1) | 41 (21.8) | 56 (28.3) | 8 (25.8) | 71 (24.0) | 18 (34.6) | 0 (0.0) | ||
| Uncertain | 53 (13.7) | 23 (12.2) | 30 (15.2) | 3 (9.7) | 47 (15.9) | 3 (5.8) | 0 (0.0) | ||
| Agree | 236 (61.1) | 124 (66.0) | 112 (56.6) | 20 (64.5) | 178 (60.1) | 31 (59.6) | 7 (100.0) | ||
The data is presented as frequencies n (%) with statistical significance at p < 0.05 determined using chi-square test
Table 5.
Participants’ perception about sickle cell disease and relationship choices stratified per age and sex for an exploratory study at University of Cape Coast from 2nd February to 22nd December 2022
| Total | Sex | P-value | Age (years) | P-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | 15–19 | 20–29 | 30–39 | ≥40 | ||||
| I will insist on screening for sickle cell condition before committing to a long-term relationship | 0.152 | 0.086 | |||||||
| Disagree | 28 (7.3) | 15 (8.0) | 13 (6.6) | 4 (12.9) | 22 (7.4) | 1 (1.9) | 1 (14.3) | ||
| Uncertain | 21 (5.4) | 6 (3.2) | 15 (7.6) | 0 (0.0) | 21 (7.1) | 0 (0.0) | 0 (0.0) | ||
| Agree | 337 (87.3) | 167 (88.8) | 170 (85.9) | 27 (87.1) | 253 (85.5) | 51 (98.1) | 6 (85.7) | ||
| Sickle cell condition testing is not a priority for me when it comes to marriage | 0.304 | 0.164 | |||||||
| Disagree | 294 (76.2) | 143 (76.1) | 151 (76.3) | 23 (74.2) | 228 (77.0) | 37 (71.2) | 6 (85.7) | ||
| Uncertain | 36 (9.3) | 14 (7.4) | 22 (11.1) | 2 (6.5) | 32 (10.8) | 2 (3.8) | 0 (0.0) | ||
| Agree | 56 (14.5) | 31 (16.5) | 25 (12.6) | 6 (19.4) | 36 (12.2) | 13 (25.0) | 1 (14.3) | ||
| I will not be happy if sickle cell screening is mandatory in pre-marital counseling | 0.200 | 0.652 | |||||||
| Disagree | 282 (73.1) | 145 (77.1) | 137 (69.2) | 21 (67.7) | 216 (73.0) | 40 (76.9) | 5 (71.4) | ||
| Uncertain | 36 (9.3) | 14 (7.4) | 22 (11.1) | 2 (6.5) | 28 (9.5) | 6 (11.5) | 0 (0.0) | ||
| Agree | 68 (17.6) | 29 (15.4) | 39 (19.7) | 8 (25.8) | 52 (17.6) | 6 (11.5) | 2 (28.6) | ||
| I would advise would-be couples to screen for sickle cell condition before marriage | 0.420 | 0.551 | |||||||
| Disagree | 27 (7.0) | 15 (8.0) | 12 (6.1) | 2 (6.5) | 22 (3.8) | 2 (3.8) | 1 (14.3) | ||
| Uncertain | 17 (4.4) | 6 (3.2) | 11 (5.6) | 2 (6.5) | 15 (5.1) | 0 (0.0) | 0 (0.0) | ||
| Agree | 342 (88.6) | 167 (88.8) | 175 (88.4) | 27 (87.1) | 259 (87.5) | 50 (96.2) | 6 (85.7) | ||
| Having a sickle cell condition should not deter me from marrying another person with sickle cell condition | 0.143 | 0.190 | |||||||
| Disagree | 232 (60.1) | 120 (63.8) | 112 (56.6) | 18 (58.1) | 170 (57.4) | 37 (71.2) | 7 (100.0) | ||
| Uncertain | 75 (19.4) | 29 (15.4) | 46 (23.2) | 7 (22.6) | 62 (20.9) | 6 (11.5) | 0 (0.0) | ||
| Agree | 79 (20.5) | 39 (20.7) | 40 (20.2) | 6 (19.6) | 64 (21.6) | 9 (17.3) | 0 (0.0) | ||
| Having sickle cell disease is a matter of fate and should not be a consideration in choosing a spouse | 0.081 | 0.433 | |||||||
| Disagree | 263 (68.1) | 132 (70.2) | 131 (66.2) | 21 (67.7) | 203 (68.6) | 33 (63.5) | 6 (85.7) | ||
| Uncertain | 52 (13.5) | 18 (9.6) | 34 (17.2) | 2 (6.5) | 44 (14.9) | 6 (11.5) | 0 (0.0) | ||
| Agree | 71 (18.4) | 38 (20.2) | 33 (16.7) | 8 (25.8) | 49 (16.6) | 13 (25.0) | 1 (14.3) | ||
The data is presented as frequencies n (%) with statistical significance at p < 0.05 determined using chi-square test
The FGDs were transcribed verbatim by trained personnel with prior experience in transcribing qualitative interviews and in agreement with suggested best practices in qualitative research interviews [16]. To assess the quality and accuracy of the interview transcription, two members of the research team independently listened to the recorded interviews and cross-checked these with the interview transcription. Furthermore, two members of the research team independently undertook the thematic analyses of the transcripts, in accordance with an initially generated a priori list for organizing themes/sub-themes based on the research objectives [17]. In the Discussion section, representative quotes that best capture shared ideas are presented for illustration and to further elaborate participants’ views on specific themes.
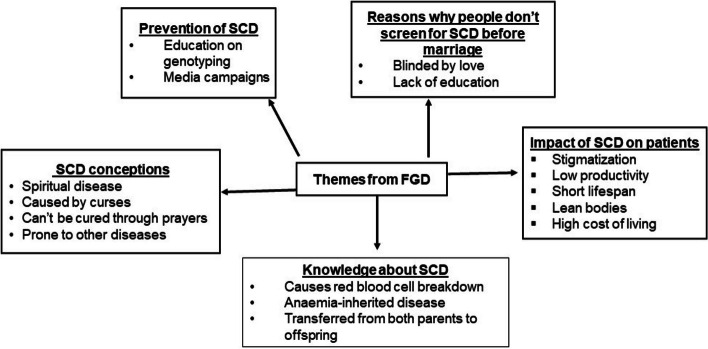
Structural equation modeling (SEM) was undertaken using Mplus software version 7 (Muthen & Muthen, U.S.A.) to explore the relationship between participants SCD beliefs, knowledge about prevention of SCD, and participants views on how these should inform relationship choices. Prior to the structural equation modeling (SEM) of the data, the Little’s MCAR test was undertaken to explore missing data pattern; however, there was no missing data in the constructs used in the SEM. The Kaiser-Meyer-Olkin (KMO) test and Bartlett’s test of Sphericity were respectively used to test the adequacy of the questionnaire items and scale correlations. Only constructs with KMO > 0.7 was included in the SEM; Bartlett’s test of Sphericity was statistically significant (p < 0.001).
In the SEM, the five Likert scale was maintained. In fitting the SEM, the independent variables were beliefs about SCD, and participants’ perception about how SCD should inform relationship choices, whereas the dependent variable was participants’ views on SCD prevention strategies. The latent variable structural model provided a good fit for the data to test the hypothesis that beliefs about sickle cell disease significantly impacted the association between participants’ understanding of relationship choices and SCD prevention strategies. Model fit parameters were: [Estimator: ML (Maximum likelihood); Chi-Square Test of Model Fit (426.901; DF: 116, p-value = 0.0000; RMSEA (Root Mean Square Error of Approximation) = 0.083; 90% C.I.: 0.075 – 0.092; Comparative fit index (CFI): 0.758; and Standardized Root Mean Square Residual (SRMR): 0.073].
Results
Background characteristics of study participants
Table 1 shows the socio-demographics of the participants in this study. An overwhelming majority of the participants were within the 20 – 29 age range with only 1.8% in the ≥ 40 years group. Also, males constituted a slight majority (51.3% vs 48.7% females). Furthermore, 89.4% and 88.9% of the participants were single or undergraduate students respectively. In general, participants from the non-science-biased programmes comprised a slight majority of the study population (58.5% vs 41.5% of sciences-biased participants).
Table 1.
Socio-demographic details of study participants at University of Cape Coast from 2nd February to 22nd December 2022
| Variable | N (%) |
|---|---|
| Age (years) | |
| 15–19 | 31 (8.0) |
| 20–29 | 296 (76.7) |
| 30–39 | 52 (13.5) |
| ≥ 40 | 7 (1.8) |
| Sex | |
| Female | 188 (48.7) |
| Male | 198 (51.3) |
| Marital status | |
| Co-habiting | 2 (0.5) |
| Divorced | 24 (6.2) |
| Married | 15 (3.9) |
| Single | 345 (89.4) |
| Educational level | |
| Undergraduate | 343 (88.9) |
| Masters/MPhil | 37 (9.6) |
| PhD | 6 (1.6) |
| College | |
| Humanities and Legal services | 173 (44.8) |
| Education | 34 (8.8) |
| Health and Allied Sciences | 93 (24.1) |
| Agriculture and Natural Sciences | 67 (17.4) |
| Missinga | 19 (4.9) |
Missinga indicates missing data
Participants’ awareness about sickle cell disease (SCD)
Participants’ knowledge about SCD was explored in Table 2. An overwhelming majority (98.7%) of participants indicated having heard about SCD, with 42.2% indicating school as the means of the knowledge. Also, majority of participants (93.8%) indicated that SCD is an inherited condition. Although 90.9% of participants stated that a blood test was required to diagnose SCD, only 49.7% indicated knowing their SCD status.
Table 2.
General sickle cell disease awareness, and sickle cell status stratified per demographic variables of study participants at University of Cape Coast from 2nd February to 22nd December 2022
| Variable | Total | ||
|---|---|---|---|
| Have you heard about sickle cell disease? | |||
| No | 372 (98.7) | ||
| Yes | 5 (1.3) | ||
| Sources of information about sickle cell disease | |||
| Print media | 14 (3.6) | ||
| School | 163 (42.2) | ||
| Health professionals | 62 (16.1) | ||
| Social media | 31 (8.0) | ||
| Broadcast media | 42 (10.9) | ||
| Church, family and peers | 61 (15.8) | ||
| aMissing | 13 (3.4) | ||
| How does one get sickle cell disease? | |||
| Blood transfusion | 15 (3.9) | ||
| Destiny | 1 (0.3) | ||
| Spiritual attack | 1 (0.3) | ||
| Hereditary | 362 (93.8) | ||
| Blood transfusion and hereditary | 7 (1.8) | ||
| Do you know your sickle cell status? | |||
| aMissing | 9 (2.3) | ||
| No | 185 (47.9) | ||
| Yes | 192 (49.7) | ||
| How does one get diagnosed with sickle cell disease? | |||
| Blood test | 351 (90.9) | ||
| Eye examination | 1 (0.3) | ||
| Physical examination | 23 (6.0) | ||
| X-ray | 10 (2.6) | ||
| Do you know your sickle cell status? | |||
| No | Yes | ||
| Age (years) | |||
| 15–19 | 30 (7.9) | 18 (60.0) | 12 (40.0) |
| 20–29 | 288 (76.4) | 146 (50.7) | 142 (49.3) |
| 30–39 | 52 (13.8) | 20 (38.5) | 32 (61.5) |
| ≥ 40 | 7 (1.9) | 1 (14.3) | 6 (85.7) |
| Sex | |||
| Female | 183 (48.5) | 93 (50.8) | 90 (49.2) |
| Male | 194 (51.5) | 92 (47.4) | 102 (52.6) |
| Marital status | |||
| Married | 15 (4.0) | 2 (13.3) | 13 (86.7) |
| Divorced | 24 (6.4) | 12 (50.0) | 12 (50.0) |
| Single | 336 (89.6) | 170 (50.6) | 166 (49.4) |
| Educational levelb | |||
| Undergraduate | 334 (88.6) | 171 (51.2) | 163 (48.8) |
| Masters/MPhil | 37 (9.8) | 13 (35.1) | 24 (64.9) |
| PhD | 6 (1.6) | 1 (16.7) | 5 (83.3) |
aMissing indicates missing data
bIndicates that the proportions are significantly different at p < 0.05 as determined by Chi-square test
When the knowledge about sickle cell status was explored per demographic details, less than half of the participants < 30 years indicated knowing their sickle cell status compared to 64.4% of participants ≥ 30 years who indicated knowing their sickle cell status. Moreover, a slightly higher proportion of males knew their sickle cell status (52.6% vs 49.2% of females). Furthermore, whereas less than half of the participants pursuing undergraduate degrees knew their sickle cell status, more than two-thirds of graduate students indicated knowing their sickle cell status.
Beliefs of participants about sickle cell disease
Table 3 demonstrates the beliefs that participants had concerning SCD stratified per gender and age. An overwhelming majority (92.2%) of participants indicated that SCD is not a spiritual ailment; this belief did not significantly differ per age or gender. A little over one-third (35.2%) of participants indicated that acquiring SCD could be prevented by personal choices. When the potential impact of screening for SCD was explored, whereas 34.2% indicated that knowing their sickle cell status might lead to stigmatization, 27.5% indicated that knowing their sickle cell status could make them less confident in forming relationships. Interestingly, only 9.3% indicated that testing for SCD was associated with pain. Moreover, 30.1% of the participants indicated that having a child with SCD was a matter of fate; a significantly higher proportion of females haboured this knowledge compared to their male counterparts (36.7% females vs 23.7% males; p = 0.009).
Sickle cell disease prevention strategies
Table 4 presents the participants’ understanding of SCD prevention. An overwhelming majority (91.2%) of participants were in favor of mandatory sickle cell testing for all couples prior to marriage; a significantly higher proportion of females agreed to this notion compared to males (93.6% vs 88.9%; p = 0.020). Moreover, the majority of participants (87.8%) indicated that sickle cell testing for all newborns should be mandatory. Also, a higher proportion (74.6%) of participants opined that two would-be couples who have been diagnosed with sickle cell disease should be discouraged from marrying. Moreover, 52.6% of the participants indicated that if they were aware of the risk of having a child with sickle cell condition, it would influence their pregnancy plans. Furthermore, over half of the participants believed that Pastors/Imams should counsel all prospective couples with sickle cell disease not to marry.
Sickle cell disease and relationship choices
Table 5 illustrates the perception of participants concerning SCD and relationship choices. The majority of participants (87.3%) stated that they would demand sickle cell condition testing before entering into a long-term relationship. Notably, 76.2% of participants disagreed with the notion that sickle cell testing is not a priority for them in marriage considerations, with a higher agreement rate (16.5%) among females. The majority of participants disagreed with the idea that they would be unhappy if sickle cell screening became mandatory in pre-marital counseling. Most participants (88.6%) expressed their intention to advise prospective couples to screen for sickle cell conditions before marriage. Additionally, 60.1% of the participants disagreed with the notion that having a sickle cell condition should not deter them from marrying someone else with the same condition. Furthermore, the majority of participants (68.1%) did not agree with the idea that having SCD is a matter of fate and should not be a consideration when choosing a spouse.
Mediation effect of beliefs about SCD on the relationship between preventive strategies and relationship choices
To further understand the underlying themes in the constructs used in the questionnaire, we modeled the data (Fig. 2). Our latent variable structural model demonstrated that one’s knowledge about SCD prevention is significantly and positively associated with relationship choices (b = 0.757, p < 0.05). Also, a participants’ beliefs about SCD were significantly inversely associated with relationship choices (b = -0.311, p < 0.05). Furthermore, a participant’s knowledge about the preventive strategies of SCD is significantly associated with the individual’s beliefs about SCD (b = 0.335; p < 0.05). However, in the overall scheme of the data, a participant’s beliefs about SCD negatively mediateed the association between preventive strategies and relationship choices.
Fig. 2.
Structural equation model of the effect of beliefs about sickle cell disease on the association between preventive strategies and relationship choices for an exploratory study at University of Cape Coast from 2nd February to 22nd December 2022. “r” is the latent variable measuring relationship choices; “b” is the latent variable measuring belief systems held by participants; “p” is latent variable measuring participants’ knowledge about SCD prevention strategies. The arrows shown are only significant associations with respective standardized parameter estimates, STDYX. Constructs in questionnaire items Q11, Q12 and Q13 were used to solicit participants beliefs about SCD, SCD prevention and impact of SCD on relationship choices respectively (Supplementary file S1). Model fit parameters were: [Estimator: ML (Maximum likelihood); Chi-Square Test of Model Fit (426.901; DF: 116, p-value = 0.000; RMSEA (Root Mean Square Error of Approximation) = 0.083; 90% C.I.: 0.075–0.092; Comparative fit index (CFI): 0.758; and Standardized Root Mean Square Residual (SRMR): 0.073]
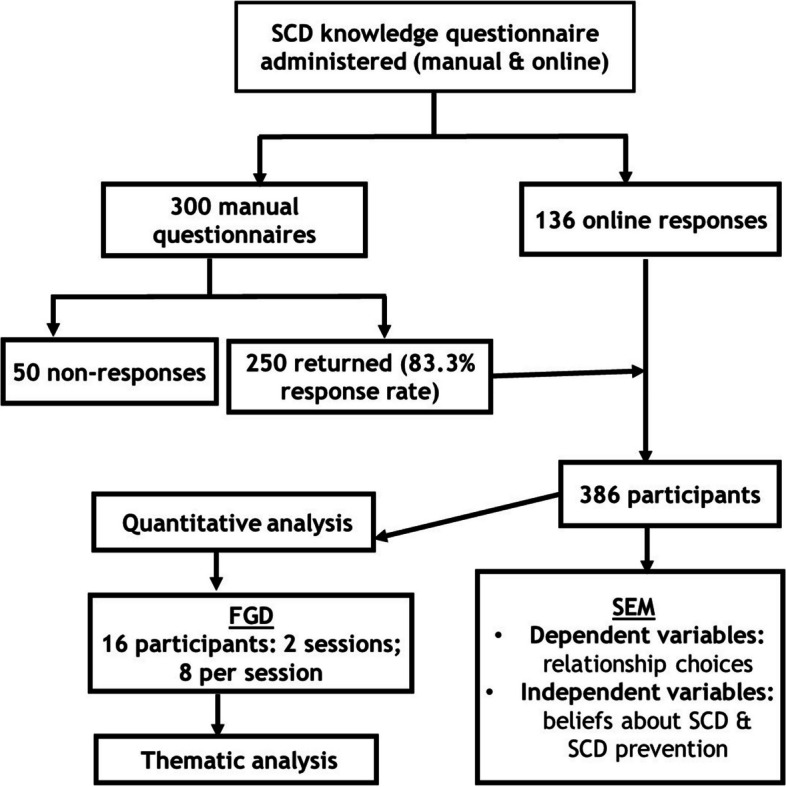
Exploring participants’ SCD understanding through focus group discussion
Focused group discussions explored the potential rationale underlying the responses of participants during the initial questionnaire data collection (Fig. 3). Regarding the causes of SCD, participants indicated that it was a disease inherited from parents and causes frequent red cell breakdown. A significant proportion of participants also indicated SCD was either a spiritual disease or caused by curses although it cannot be cured by prayers. Furthermore, participants unanimously agreed that SCD has negative impacts on the person which invariably included stigmatization, high cost of living because of added medical cost, low productivity as a result of time lost to seeking medical care and perceived shortened lifespan. In spite of the perceived negative effects of SCD, participants stated that lack of education about the condition, as well as would-be couples being blinded by their love for each other were major reasons why individuals do not screen for the disease during pre-marital counseling period. On the issue of how SCD could be prevented, participants overwhelmingly expressed that media campaigns to educate people about SCD inheritance and prevention were potential avenues to reduce the disease burden (Fig. 3).
Fig. 3.
Thematic analyses of the FGD on Sickle Cell Disease for an exploratory study at University of Cape Coast from 2nd February to 22nd December 2022. Major themes are in bold; sub-themes are in light print
Discussion
Sickle cell disease is a prevalent monogenic inherited disease in sub-Saharan Africa. Annually, it is estimated that 2% of newborns (approximately 15,000) in Ghana have SCD, with 55% of them having the homozygous form [3]. It is further estimated that 30% of Ghanaians are carriers [4] of the sickle cell trait; a situation that ensures stable penetrance of the disease. Since SCD is inheritable disease, individual choices particularly during the time of choosing lifetime partners could be leveraged as a proactive public health campaign to actively select against the disease via a mandated premarital SCD screening. University students by virtue of their national representativeness since students are recruited randomly from across the country could provide a gauge of the baseline SCD knowledge of young adults across the country. This is particularly important considering that most of this majority youthful population may be at the crucial stages in the process of making reproductive choices. In this observational, exploratory study that employed a mixed-methods approach, we found that although an overwhelming majority (98.7%) of these youthful participants indicated having heard about SCD, and knew that it was inherited (93.8%), only about a-half of the participants actually knew their respective SCD status. More importantly, our structural equation modeling demonstrated that although a participant’s knowledge about SCD prevention is significantly and positively associated with perceived relationship choices, this SCD prevention-relationship association is significantly negatively mediated by the SCD belief held by these young adults. Taken together, our study argues for a need to pursue deliberate public health campaigns that address the belief systems that these young adults hold regarding SCD to ensure that knowledge about SCD inheritance and risks could be translated into spousal choices to proactively select against the disease to reduce its socio-economic burden.
While it may be encouraging to note that a little over half of the participants indicated that the source of their SCD knowledge was not through the school system, it is equally concerning that less than half of the SCD knowledge was attributed to the school system. The fact that social media, broadcast media, social groups (church, and families) and information from health professionals constituted 50% of the source of SCD knowledge for these highly educated individuals is indicative that these mediums of public health campaigns could be leveraged for the entire populace. Given the widespread use of various media platforms to create both audio and visual content that could be readily comprehensible to even those with no formal education, the idea that these mediums are already being used in Ghana to craft SCD educational campaigns should be encouraging to public health practitioners. Contrastingly, given the high prevalence of SCD in Ghana, one would presume that these young adults pursuing tertiary education would have had multiple chances to learn about the disease through the education system. This finding may be suggestive of a need to re-evaluate the curriculum of the educational system to ensure that students irrespective of their disciplines would have some basis on topical issues of public health concern such as SCD and related haemoglobinopathies. In the FGD, it was evident that the majority of those who could correctly identify the hereditable basis of SCD were those from life sciences-biased programs. In a similar observational study among University of Ghana students, Boadu and colleagues [18] reported that the knowledge on SCD diagnosis, inheritance, symptoms and management was poor despite a generally high awareness of the disease. This is in contrast to the findings of this study where more than 90% of participants self-reported about knowing the means of diagnosis as well as inheritance of the disease.
Notably, the proportion of participants who knew their respective status was less than a-half, and seemed to improve from four-in-ten among teenagers to greater than eight-in-ten among those > 40 years old. Similarly, whereas less than half of undergraduate students were aware of their SCD status, this improved to greater than six-in-ten among those pursuing masters’ or doctoral degrees. It is instructive to note that the University of Cape Coast organizes a mandatory SCD screening for all freshly admitted students [19], which would presuppose that by virtue of this unique privilege of mandatory SCD screening, all these students should know of their respective SCD status. The fact that less than a-half of the participants actually recall their respective SCD status raises questions about the extent of disclosure of the medical screening data to individual students. Disturbingly, a little over a-third of these tertiary students (34.2%) feared stigmatization [20] should they have SCD and it came to the knowledge of others in their community. Inevitably, individuals fearful of being stigmatized are more likely to intentionally not screen for the disease; this will only inure to a high sickle cell gene carrier rate and sustain SCD penetrance in the population. In agreement with previous studies [20, 21], various views expressed by the FGD participants were indicative that stigmatization may be real in the communities as suggested by opinions such as:
“Personally, I lived in a community with a gentleman who had sickle cell disease and because of the condition the parents didn’t take him to school. He was just in the house, always falling sick but then I’m sure right now he would be around 40 years and because of the condition a lot of people looked down upon him. But his other siblings were in school. the way they look at children with sickle cell disease is as if nothing good can come out of them…it is so bad.” (Female FGD participant).
“Yes, I have…. like a small girl and she was very active but her parents actually took her to the village because they say that she can’t keep up with city so her grandparents were the ones taking care of her … And they said on a normal day she can do like every single thing but when the crises start then she is really down.” (Female FGD participant).
Although stigma associated with SCD was not the main focus of the present study, our findings highlight a need to explore the actual lived experiences of individuals with sickle cell anaemia and curate the various components of the SCD stigma in future studies. However, it should be evident to public health educators and health professionals that any intervention should first seek to unearth and dispel SCD misconceptions to reduce the stigma attached to the condition. Noteworthily, whereas an overwhelming majority (93.8%) indicated that SCD is inherited from parents, a further 9-in-10 participants intimated that SCD screening ought to be mandatory for all would-be couples. What is not readily reconcilable in the data is why only a little over a third (35.2%) indicated that SCD is preventable, with a further 3-in-10 suggesting that giving birth to a SCD child was a matter of fate. Decidedly, if SCD is inherited from parents as indicated by these young adults, then one would suppose that these participants could further deduce that it could be prevented through informed partner selection and/or through the emerging assistive technologies [5]. It should be obvious thus that the SCD knowledge/understanding of these young adults might not be comprehensive enough to guide their respective relationship choices. As evidence of this, during the focus group discussion, a sizable proportion of the participants held a misconception that SCD could be caused by curses or occurred as a result of a spiritual attack as illustrated in these quotes:
“Growing up, my grandparents thought it was some spiritual disease but because they didn’t have any idea about it…they go here and there for herbal medicine. So, after we discovered … everything came to normal…. They started taking me to the hospital for medications…. everything came to normal.” (Male FGD participant who is a sickle cell anaemia patient).
“Some people think they don’t grow older. They have some specific age or something they get and then it’s final.” (Female FGD participant).
“Others too may think it is a curse, maybe in your childhood you did something bad to someone, and then that person might even say that. So, giving birth to such children in your future, you may think it’s what the person said that is happening.” (Male FGD participant).
Evidently, misconceptions about SCD are real even among these tertiary students; thus, public health educational campaigns ought to itemize these misconceptions, and device context-specific strategies to address these misconceptions to demystify the disease to ensure that would-be couples make informed decisions at the time of spousal selection.
It is important to note that when exploring avenues to reduce SCD burden, nine-in-ten of these young adults intimated that SCD screening ought to be mandatory for all would-be couples, compared to a little over seven-in-ten who indicated that would-be couples who each has SCD should be discouraged from going ahead with their marriage plans. This SCD status-induced marital choice as reported herein is in contrast to a community-based study in Odisha district, India, where participants could not relate that SCD status ought to inform relationship choices [22]. Whereas our study participants were all tertiary students, the Odisha study recruited a significant proportion of participants with non-tertiary education; this differences in educational attainment of participants could account for the differences in implications of SCD knowledge on spousal selection. Moreover, majority of these young adults favoured mandatory pre-marital sickle cell testing [18] in contrast to a previous qualitative study that found 4-in-10 college students in Nigeria [23] who demonstrated a negative attitude towards premarital SCD screening.
In Ghana, faith leaders, particularly pastors, fetish priests/priestesses, or imams, have become the custodians entrusted with the role of solemnizing marriages. Not surprisingly, six-in-ten of the participants intimated that these faith leaders should be empowered to advise would be couples with the potential of giving birth to SCD children to halt their matrimonial plans. We believe such prohibition will be high-handed considering that not all couples go into marriage with intention to procreate. Although arrogating such powers to these faith leaders might be extreme with potential ethical implications as argued elsewhere [24], it is noteworthy that the trust reposed in these faith leaders could be leveraged in public health programs intended to reduce SCD penetrance and/or burden in the population. It will be interesting to explore the SCD knowledge of these faith leaders and their perspectives on assistive reproductive technologies in future studies as their relevant knowledge may be key in the discharge of their gatekeeping functions. It is our expressed opinion that empowering these faith leaders with resources to discharge their gatekeeping function could be used as an alternative public health screening intervention to curb the penetrance of SCD in Ghana. It became clear during the focus group discussion that participants were doubtful as to whether these faith leaders had the requisite knowledge about SCD. For example, some views expressed (and supported by the majority of the focus group discussants) regarding SCD knowledge by faith leaders included:
“Maybe it all cut across the education, they (faith leaders with premarital responsibilities) are not much enlightened about it so they don’t really care…it is not that they don’t care, but like they don’t know so when you go for counseling, they don’t include it.” (Male FGD participant 1).
“They (faith leaders with premarital responsibilities) don’t add those part to it, the education on… because I for instance this is my first time discussing about Sickle cell and genotype. So, the education on that part is low…all they know is those HIV and hepatitis B and those things. But the education on sickle cell anaemia is less.” (Male FGD participant who is married).
“I think pastors/Imams…. they ask the couples to go and do check up at the hospitals, I think when they go to the hospital, they have to do all the other screening.” (Female FGD participant 1).
It also became apparent during the focus group discussions that even those who were married could not remember any specific SCD education they received during their pre-marital counseling sessions. Thus, as public health campaigns are being formulated for implementation, concrete efforts ought to be made to not only educate these faith leaders about preventable inheritable diseases like SCD, but there should also be strategies to standardize the protocols used by these faith leaders during their premarital counseling to ensure that irrespective of one’s faith affiliation, the same protocols are applied across. In this way, these faith leaders will be empowered to discharge their gatekeeping roles to society and consequently raise societal awareness about SCD and related inheritable diseases to the point that informed spousal choices could be made with the expressed intention of selecting against these conditions. Through the FGD, it became abundantly clear that educating the populace about SCD holds much promise to reduce the disease burden and other related issues:
“Through education, I think because SCD deals with genotype, so we have to educate parents about the genotype they are carrying so that they can get married to the right genotype person, so they would prevent giving birth to a sickle cell child” (Male FGD participant).
“I am supporting what my brother said that educating the young ones about the genotype so that in case they are getting married or they are getting into sexual activities, they would know the right person to go with”. (Female FGD participant).
“I think they should advertise about the disease on our various televisions. I think they should advertise it on our various televisions especially for our rural areas, most of them don’t have any idea about SCD. So, I think advertising would help.” (Male FGD participant).
There have been arguments supporting the survival advantages offered by sickle cell trait inheritance in environments with high P. falciparum infection [25, 26]. Whilst this may be a scientific reality that cannot be discounted, it should not be taken to mean that no one would survive in a high P. falciparum infection area in the absence of SCD and related haemoglobinopathies. The sickle cell anaemia-related high economic and psychological burden on both patients and family members alone should be enough incentive for public health educational interventions to select against the disease.
It is equally important to note that nearly nine-in-ten participants indicated that SCD testing ought to be mandatory for all newborns, with a little over a-half indicating that the knowledge that they were at risk of giving birth to a SCD baby would change their pregnancy plans [27]. This may be indicative that these young adults are open to premarital SCD screening given the potential life-altering propensity of a child with the disease which could be leveraged for public health sensitization campaigns. Nearly 9-in-10 indicated that they will insist on sickle cell screening before committing to a long-term relationship, with a further 88.6% indicating that they will advise all would-be couples to screen for SCD before marriage. Considering that 89.4% of our study participants were single, this could be taken as a good indicator and a fertile ground for a targeted public health campaign through the strengthening of premarital SCD screening. This willingness was further substantiated by the fact that almost eight-in-ten indicated that they would not be bothered if SCD screening was made mandatory during the premarital counseling period for all would-be couples. Evidently, these young adults consider SCD as important consideration in relationship choices which is in agreement with previous studies [28, 29]. Ironically, participants in the focus group discussion indicated that the emotional highs associated with relationship matters blind one to these stated realities. For example, FGD participants invariably supported statements like:
“I think even though they are asked to do (screen for SCD), when they get their love, it blinds them so they can tell the doctor not to check for sickle cell. If you check and the person does not have the genotype that matches your own because of that they ignore. I know some people who got married without testing but I think it is not advisable to do that.” (Male FGD participant).
Evidently, the conflict between rational choice and emotional feelings could potentially cloud the judgement of these young adults if left on their own to navigate this spousal selection stage. Societal intervention through family support as well as inputs from faith leaders could be leveraged during this pivotal stage to ensure that informed choices are made.
Although the foregoing discussions shed light on the quantitative data, our structural equation modeling that explored the underlying relationships between the latent variables in the constructs used in the quantitative data demonstrated that the knowledge that the participants have regarding SCD was strongly positively associated with their relationship choices. Perhaps, what is instructive is the fact that the belief system that these young adults have concerning SCD inheritance and/or impact, negatively mediated the association between the SCD knowledge and relationship choices. Our latent variable modeling is evidently suggestive that in a highly religious setting like Ghana, the beliefs systems of individuals might be unspoken undertones that may dictate how even the educated utilize their acquired knowledge even in disease conditions that could have socio-economic implications on the family. Noteworthily, SCD beliefs likely transform apparent quantitatively linear association into a complex non-linear interaction that ought to be considered in public health interventional campaigns. Taken together, SCD public health campaigns that merely target improving the knowledge of these young adults about the inheritance of SCD, the economic burden of the disease, and/or how SCD ought to inform spousal selection, without equally addressing the belief systems held by these young adults might not optimally achieve the intended targets.
Limitations and strengths
Even though our mixed-methods approach to data collection in the study reported herein increased the scientific rigor of the study outcomes, we recognize that this was a one-center study that might not necessarily represent the perspectives and experiences of university students from other tertiary institutions across the nation. Moreover, the fact that the participants were tertiary students also hints of a potential selection bias in that it might not represent the SCD knowledge and belief systems of those without formal education or even those with only primary or secondary education. Notwithstanding these acknowledged limitations, the fact that the University of Cape Coast is an equal-access institution accepting students from all across the country is suggestive that the study outcome reported herein could be taken to favourably approximate the experiences of young adults in Ghana.
Conclusions
We found that SCD public health campaigns merely targeting improving the knowledge about SCD, the economic burden of SCD, and/or SCD-spousal selection dynamics, without equally addressing the belief systems held by young adults might not optimally achieve the intended targets. Future large cohort studies should sample participants across all age stages, as well as the formally educated and non-formal educated groups and model that data to give a comprehensive nationally representative outcome to inform SCD public health planning and policy formulation. Additionally, future studies should consider adopting established frameworks [30, 31] to highlight the various aspects of stigma faced by both SCD patients and their caregivers within the Ghanaian context to provide empirical data on whether it is necessary to implement SCD stigma reduction program.
Supplementary Information
Acknowledgements
We are grateful to all the students who volunteered for this study.
Abbreviations
- SCD
Sickle cell disease
- SEM
Structural equation model
- FGD
Focus group discussion
Authors’ contributions
PA conceptualised the study and methodology, supervision, independently assessed quality of FGD transcript, quantitative data analyses, SEM, prepared figures 1 and 2, and wrote the original draft. JB conceptualized the study, supervision, independently assessed quality of FGD transcript, and critically reviewed the manuscript. BB and EA undertook transcription of FGD, thematic analyses of the FGD, participant recruitment, prepared figure 3, and critically reviewed the manuscript. GKL, JM, EAP, EO, and DBM were involved in participant recruitment, questionnaire administration, FGD and critical review of the manuscript. All authors reviewed and approved the final manuscript.
Funding
This study did not receive any public funding; it was self-financed by the co-authors.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board of the University of Cape Coast (ethical clearance ID: UCCIRB/CHAS/2022/60). Our study protocol conformed to the provisions of the Declaration of Helsinki in 1995 (as revised in Brazil 2013) including confidentiality, risks and benefits assessments, consent to participate, and ensuring respect to participants. Written informed consent was taken from all participants during the questionnaire distribution before a participant was allowed to answer the questionnaire. Participants were fully informed of the study’s objectives, and only those who provided written informed consent were enrolled for the study. However, since the age of consent is 18 years in Ghana, participants who were < 18 years old could only participate via the manual printed questionnaire after they have provided an accent from their legal guardians or parents. The study’s participants were made aware that their information would be kept anonymized and that they had the option at any moment to revoke their consent and request for their data to be excluded from the study at any time point prior to publication of the data. The information gathered from the research was exclusively used for its intended purpose.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Assembly UNG. Recognition of sickle-cell anaemia as a public health problem: draft resolution / Angola, Austria, Belgium, Benin, Brazil, Cameroon, Cape Verde, Central African Republic, Comoros, Congo, Côte d’Ivoire, Democratic Republic of the Congo, Djibouti, France, Gabon, Ghana, Monaco, Senegal, Togo and Zambia. In: Assembly G, editor. 2008. A/RES/63/237. Available at: https://digitallibrary.un.org/record/644129?v=pdf.
- 2.Asare EV, Wilson I, Benneh-Akwasi Kuma AA, Dei-Adomakoh Y, Sey F, Olayemi E. Burden of sickle cell disease in Ghana: the Korle-Bu experience. Adv Hematol. 2018;2018:6161270. 10.1155/2018/6161270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ohene-Frempong K, Oduro J, Tetteh H, Nkrumah FJP. Screening newborns for sickle cell disease in Ghana. Pediatrics. 2008;121(Supplement_2):S120–1. 10.1542/peds.2007-2022UUU [DOI] [Google Scholar]
- 4.Kyerewaa Edwin A, Edwin F, Etwire V. Controlling sickle cell disease in Ghana–ethics and options. Pan Afr Med J. 2011;10:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oyewo A, Salubi-Udu J, Khalaf Y, Braude P, Renwick P, Lashwood A, El-Toukhy T, Oteng-Ntim E. Preimplantation genetic diagnosis for the prevention of sickle cell disease: current trends and barriers to uptake in a London teaching hospital. Hum Fertil. 2009;12(3):153–9. 10.1080/14647270903037751 [DOI] [PubMed] [Google Scholar]
- 6.Collins SC, Xu X, Mak W. Cost-effectiveness of preimplantation genetic screening for women older than 37 undergoing in vitro fertilization. J Assist Reprod Genet. 2017;34(11):1515–22. 10.1007/s10815-017-1001-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith M, Brownell G. Knowledge, beliefs, attitudes, and behaviors regarding sickle cell disease: implications for prevention. Soc Work Public Health. 2018;33(5):299–316. 10.1080/19371918.2018.1469064 [DOI] [PubMed] [Google Scholar]
- 8.Boyd JH, Watkins AR, Price CL, Fleming F, DeBaun MR. Inadequate community knowledge about sickle cell disease among African-American women. J Natl Med Assoc. 2005;97(1):62–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Smith MN, Praetorius RT. The challenges and opportunities associated with sickle cell disease prevention, education, and management. Soc Work Public Health. 2015;30:592–612. 10.1080/19371918.2015.1087905 [DOI] [PubMed] [Google Scholar]
- 10.Smith M, Praetorius RT. College students’ knowledge about sickle cell disease. J Hum Behav Soc Environ. 2019;29(3):308–20. 10.1080/10911359.2018.1528918 [DOI] [Google Scholar]
- 11.Anie KA, Egunjobi FE, Akinyanju OO. Psychosocial impact of sickle cell disorder: perspectives from a Nigerian setting. Glob Health. 2010;6:2. 10.1186/1744-8603-6-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Acharya K, Lang CW, Ross LF. A pilot study to explore knowledge, attitudes, and beliefs about sickle cell trait and disease. J Natl Med Assoc. 2009;101(11):1163–72. [DOI] [PubMed] [Google Scholar]
- 13.Smith M, Brownell G. College student’s attitudes about SCD carrier screening. J Hum Behav Soc Environ. 2022;32(2):201–13. 10.1080/10911359.2021.1879703 [DOI] [Google Scholar]
- 14.Treadwell MJ, McClough L, Vichinsky E. Using qualitative and quantitative strategies to evaluate knowledge and perceptions about sickle cell disease and sickle cell trait. J Natl Med Assoc. 2006;98(5):704. [PMC free article] [PubMed] [Google Scholar]
- 15.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 16.Helmich E, Cristancho S, Diachun L, Lingard L. ‘How would you call this in English?’: being reflective about translations in international, cross-cultural qualitative research. Perspect Med Educ. 2017;6(2):127–32. 10.1007/S40037-017-0329-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1(3):385–405. 10.1177/146879410100100307 [DOI] [Google Scholar]
- 18.Boadu I, Addoah T. Knowledge, beliefs and attitude towards sickle cell disease among university students. J Community Med Health Educ. 2018;8(593):2161-0711.1000593. [Google Scholar]
- 19.Amoah S, Yartey AN, FosuAdjei P, Owusu-Akyaw M, Boachie J, Simpong DL, Adu P. HBV infection is an intermediate-risk disease, whereas anaemia is a mild-to-moderate public health problem in young Ghanaian adults: a four-year retrospective analysis of students’ medical records. Biomed Res Int. 2023;2023:9318984. 10.1155/2023/9318984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. J Natl Med Assoc. 2010;102(11):1050–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buser JM, Bakari A, Seidu AA, Paintsil V, Osei-Akoto A, Amoah R, Otoo B, Moyer CA. Stigma associated with sickle cell disease in Kumasi, Ghana. J Transcult Nurs. 2021;32(6):757–64. 10.1177/10436596211008216 [DOI] [PubMed] [Google Scholar]
- 22.Bindhani BK, Devi NK, Nayak JK. Knowledge, awareness, and attitude of premarital screening with special focus on sickle cell disease: a study from Odisha. J Community Genet. 2020;11(4):445–9. 10.1007/s12687-020-00471-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hussaini M, Durbunde A, Jobbi Y, Muhammad I, Mansur A, Umar M, Isaac OT, Ummulkulthum K, Bolanle AA, Kambai J. Assessment of experience, perception and attitude towards premarital sickle cell disease screening among students attending federal college of education, Kano, Nigeria. Niger Int J Res Rep Hematol. 2019;2(1):1–12. [Google Scholar]
- 24.Ezugwu EC, Osamor PE, Wendler D. Ethical issues in denial of church wedding based on couple’s hemoglobin genotype in Enugu, south eastern Nigeria. BMC Med Ethics. 2019;20(1):37. 10.1186/s12910-019-0376-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luzzatto L. Sickle cell anaemia and malaria. Mediterr J Hematol Infect Dis. 2012;4(1):e2012065. 10.4084/mjhid.2012.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bunn HF. The triumph of good over evil: protection by the sickle gene against malaria. Blood. 2013;121(1):20–5. 10.1182/blood-2012-08-449397 [DOI] [PubMed] [Google Scholar]
- 27.Alsalman M, Alhamoud H, Alabdullah Z, Alsleem R, Almarzooq Z, Alsalem F, Alsulaiman A, Albeladi A, Alsalman Z. Sickle cell disease knowledge and reproductive decisions: a Saudi cross-sectional study. Patient Prefer Adherence. 2023;17:761–7. 10.2147/PPA.S404811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gbeneol PK, Brisibe SF, Ordinioha B. Knowledge, attitude and uptake of premarital screening for the Sickle trait among married couples in a semi-urban community in south-South Nigeria. Eur J Prev Med. 2015;3(3):49. 10.11648/j.ejpm.20150303.13 [DOI] [Google Scholar]
- 29.Farkındalığı E. Awareness of premarital genetic counselling among youth Corpers in south-West Nigeria. TAF Prev Med Bull. 2010;9(6):575–8. 10.5455/pmb.20100427030409 [DOI] [Google Scholar]
- 30.Bediako SM, Lanzkron S, Diener-West M, Onojobi G, Beach MC, Haywood C. The measure of sickle cell stigma: initial findings from the improving patient outcomes through respect and trust study. J Health Psychol. 2016;21(5):808–20. 10.1177/1359105314539530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leger RR, Wagner LD, Odesina V. Stigma in adults with sickle cell disease and family members: scale development and pilot study in the USA and Nigeria. Int J Afr Nurs Sci. 2018;9:23–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].
No datasets were generated or analysed during the current study.