Abstract
Objective
Particular attention is given to the enhancement of melanin-related pigmentation (dark circles, photoaging) and vascular circles, which are commonly located in the tear trough. The objective of the study is to provide an objective evaluation of the impact of carboxytherapy and the treatment regimen combining carboxytherapy with lactobionic acid (20%, pH 2.1) or ferulic acid (14%, pH 4.0–5.0) and ascorbic acid (12%) on skin defects in the eye area.
Materials and Methods
A group of 39 Caucasian people were subjected to a series of five carboxytherapy treatments (right eye area) and five treatments combining carboxytherapy with a selected chemical peel for the skin around the eyes (left eye area). The efficacy of therapy was assessed based on parameters (MI and EI) measured with the Mexameter probe. Measurements were made in the tear trough and the middle of the lower eyelid.
Results
We demonstrated that a series of carboxytherapy (right side) significantly statistically influenced the EI parameter (in different measurement points: P <0.0001, P = 0.015, P = 0.002), which reflects the intensity of vascular circles under the eyes. Improvement of this parameter by 7.2 units was also shown in the tear trough in 82.1% of participants after the application of carboxytherapy combined with acids (left side) on the valley of tears for this parameter (EI). Lactobionic acid and carboxytherapy were associated with a statistically significant improvement (P = 0.011) in the tear trough. In this study, a reduction in the combined pigmentation (MI plus EI) for both the right and left sides (p = 0.001 and p = 0.015, respectively) was observed.
Conclusion
The study provides objective evidence for the effectiveness of sole carboxytherapy and carboxytherapy combined with acids in the reduction of dark circles, in particular vascular circles in the tear trough. Lactobionic acid, ferulic acid, and ascorbic acid can be used as safe supplements to enhance carboxytherapy.
Keywords: carboxytherapy, dark circles, lactobionic acid, ferulic acid, ascorbic acid
Introduction
Dark circles under the eyes can be classified into vascular circles, hyperpigmentation, structural/true circles, and others.1–3 Vascular circles occur in most cases of circles. Vascular circles are a result of genetic factors (the shallow location of blood vessels), the dilation of blood vessels, and the slowing down of the circulation of blood that is inadequately oxygenated (hypoxia). The development of pigmented dark circles is attributed to the accumulation of blood pigment (blood extravasation), specifically hemoglobin, and the resulting products of its enzymatic decomposition in the epidermis and dermis, namely biliverdin, bilirubin, methemoglobin, and hemosiderin (a protein complex that stores iron in cells). Pigmented dark circles are also called hyperpigmentation, and they are most often the result of chronic inflammation and are also associated with the accumulation of melanin in the skin (melanin incontinence, dermal melanophages and perivascular lymphocytic infiltration) and/or in the epidermis.1–12
The treatment of vascular circles should include procedures that stimulate blood flow and improve the flexibility and strength of blood vessels. For such skin problems, carboxytherapy is a recommended option. Carbon dioxide administered during carboxytherapy improves tissue perfusion and is partially responsible for the increase in oxygen concentration due to hypercapnia. In the tissue, CO2 reacts with H2O molecules to form carbonic acid, which lowers the pH of the tissue. In an acidic environment, the affinity of haemoglobin for oxygen decreases. During carboxytherapy, the release of oxygen from haemoglobin to the tissues is increased. Lower blood pH and hyperoxygenation contribute to the release of local growth factors (fibroblast growth factor, endothelial cell growth factor, vascular endothelial growth factor, and angiogenin), which then stimulate angiogenesis. When the pH value drops to 6.8 or lower, the permeability of capillary walls increases. In turn, pH values below 6.5 are associated with enhanced elasticity of collagen fibres in the blood vessel walls and a decrease in their fibrosis and hardness. Moreover, due to the acceleration of local blood flow, the lumen of already existing capillaries increases as a result of the reduction of vascular muscle tension and the opening of valves.13–17 The strong flow of intradermal carbon dioxide can also lead to the remodelling of connective tissue. Carboxytherapy is commonly used to reduce circles around the eyes because there are a few aesthetic therapies that have long-term effects related to the improvement of microcirculation.15,18,19
Lactobionic or ferulic acid with ascorbic acid combined with carboxytherapy was used in this study to treat the skin around the left eye. Based on the indications, the acid type was selected. Lactobionic acid has strong moisturizing (hygroscopic) properties. It acts as an antioxidant and anti-inflammatory substance. It is also an inhibitor of metalloproteinases, and therefore, it exerts an indirect effect on the dermis and vessels, preventing the formation of vascular changes and wrinkles under the eyes.20 In this study, this acid was used in participants with vascular circles under the eyes. The combination of ferulic acid with ascorbic acid exerts antioxidative and anti-inflammatory effect, intensifies angiogenesis, accelerates healing, and inhibits the production of tyrosinase.21–23 Such treatment was used in participants with dark circles under the eyes.
The aim of this study was to assess the effectiveness of a series of carboxytherapy and chemical peels in the reduction of vascular and pigmented circles in the eye area. An objective assessment of the impact of aesthetic treatments is an important source of knowledge regarding the methods used, the effects obtained, and possible side effects. The choice of measure methods allows for an objective assessment of the impact of treatments combining carboxytherapy and chemical peels on the circles around the eyes, which is innovative since there is hardly any literature data on this topic. Moreover, few studies on dark circles include the Caucasian race with Fitzpatrick skin phototype II.
Materials and Methods
Materials
The study included a group of 39 Caucasian subjects, aged 25–55 (35 women and 4 men) with II and III skin phototypes according to Fitzpatrick, who had dark or vascular shadows around the eyes. The study group was divided according to the classification of circles under the eyes and the individual treatment indication. The recruitment criteria also included the age: 25–55 years. There was no control group, since the study focused on the comparison of skin states before and after the series of treatments.
The exclusion criteria for carboxytherapy included: failure of organs (renal, heart, respiratory and circulatory) involved in the metabolism and elimination of CO2 from the body and the disorders such as stroke, pulmonary embolism, active pulmonary tuberculosis, cerebrovascular events, haemorrhagic diathesis and phlebitis also connective tissue diseases, diseases of the blood and coagulation system. Active neoplastic diseases and cancers up to 5 years from the recovery, history of radiotherapy are also contraindicated and active autoimmune diseases. We excluded infectious diseases, including those caused by anaerobic bacteria, herpes, skin inflammation within the treated area. Also considered as relative contraindications were: epilepsy, glaucoma, uncontrolled diabetes and hypertension. Carboxytherapy not be used in individuals treated with anticoagulants, carbonic anhydrase inhibitors, metformin (diabetes), systemic corticosteroids, NSAIDs, retinoids and isotretinoin. The procedure was not performed on pregnant or breastfeeding women. Participants had not previously undergone any other aesthetic medicine treatments around the eyes.
The treatments were performed according to known treatment standards. Study participants were subjected to five treatments at weekly intervals. They were instructed about home care so that they do not perform any procedures that can affect the skin state. The participants were informed about possible transient side effects related to the specificity of the treatments and other possible but unpredictable effects. All individuals from the study group signed an informed consent form to participate in this study. They agreed on the procedures, measurement and photographic documentation. The treatment used has a proven overall beneficial effect on the skin, therefore, all individuals underwent the therapy eagerly.
Patients were informed about the post-procedure procedure and that in connection with the injections, petechiae and swelling may occur at the injection site, which disappears spontaneously after a short time. All these symptoms constitute a normal peri-procedural clinical picture and do not require medical intervention, and their intensity is an individual matter. By following the post-procedure recommendations, the proband is not exposed to long-term complications. However, as with all procedures affecting the skin, there is a risk of unpredictable reactions. Post-procedure recommendations included the use of cold compresses and a light tapping massage of the treatment area. It was recommended that immediately after the procedure, for up to 6 hours, one should not perform intensive physical exercise or use cold (eg swimming pool) or hot baths, sauna or solarium. In order to accelerate the absorption of petechiae that have formed after the procedure, it is recommended to use ointments and creams for bruises and petechiae, eg with arnica, heparin and vitamin K. In the absence of any side effects, patients could use their previous home care.
Methods
Carboxytherapy (Criss Carbo, Poland) involves a controlled intradermal injection of purified, sterile, laparoscopic carbon dioxide (CO2) for therapeutic purposes. Before the procedure, the injection area was disinfected. A disposable, thin 32 G 4 mm needle was inserted at an angle of 15–30°, to a depth of 1 mm. The CO2 flow rate was adjusted in manual mode (from 10 ccs) and its dosage was controlled (from 0.5 ccs). The following flow parameters were used: 10 cc/min and dose (sum of cc): 3 ccs per eye.24 The treatment of the eye area lasted a few minutes.
The risk of infection was reduced to a minimum through the use of sterile medical gas, a particulate filter at the gas outlet, sterile tubes and disposable needles. Additionally, before the carboxytherapy procedure, after thorough cleansing of the skin, a skin disinfectant was applied to the injection area.
Skin temperature was randomly measured with the use of a non-contact infrared thermometer.
Additionally, one out of two superficial chemical peels were applied to the skin area under the left eye, depending on the diagnosis/indication. The classification (clinical assessment) was performed by the clinicians performing the research. The circles were divided into vascular and pigmented categories. Initial measurements were taken using the Mexameter probe (melanin and haemoglobin/erythema index) for validation. Based on clinical observation and pre-procedure interview/consultation and initial mexametric measurements, which facilitated qualification. Unrecorded measurements were taken in the lower eyelid area and on the cheek to compare vascular and melanin pigmentation. Combining these several assessment criteria, we drew conclusions and qualified the circles under the eyes as vascular or pigmented. There were fewer people in the study who showed signs of pigmented circles under the eyes. Therefore, in the case of mixed circles, the subjects were classified as pigmented circles.
We used either 20% lactobionic acid with pH 2.1 (application time 10 min) or 14% ferulic acid with pH 4.0–5.0 combined with 12% L-ascorbic acid applied for 5 hours. After 5 h participants were asked to clean the skin and apply a moisturizing preparation. Ferulic acid with L-ascorbic acid was used for dark/pigment circles and lactobionic acid (20% pH 2.1) for people with vascular dark circles.
Measurement
The assessment of changes in the level of melanin and haemoglobin in the skin around the eye after a series of carboxytherapy treatments was made using the Mexameter MX 18 probe connected to the Multi Probe Adapter Courage + Khazaka electronic GmbH. This device is designed to measure skin properties. The Mexameter MX 18 precisely measures the content of melanin (melanin index; MI) and haemoglobin (erythema index; EI) in the skin. In our study, this device was used to assess the effectiveness of carboxytherapy treatments in the reduction of vascular and dark circles around the eyes. The measurement is based on light absorption. The Mexameter probe emits light of three wavelengths:
green: λ = 568 nm ± 3 nm,
red: λ = 660 nm ± 3 nm,
infrared: λ = 870 nm ± 10 nm.
The Mexameter probe is very sensitive and measures a wide range of melanin and erythema content (0–999), which enables the recording of even the smallest changes in skin colour. The measurement of erythema is carried out using light of two wavelengths - one corresponding to the absorption spectrum of haemoglobin, and the other one is selected in such a way to avoid the influence of other colours, including bilirubin case, which could hinder the differentiation of vascular and dark/pigment circles under the eyes.
The measurements were made in two places (Figure 1): in the inner area of the eye (so-called tear trough) and the middle area (in the middle of the distance between the outer and inner corners of the eye) of the lower eyelid of the left and right eyes.
Figure 1.
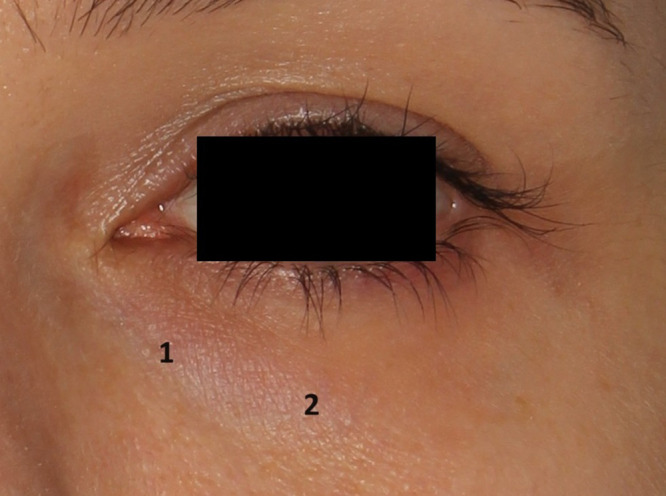
Measurement points.
Subjects have given their written informed consent and that the study protocol was approved by the institute’s committee on human research. This research project and procedures were approved by the Bioethics Committee of the Medical University of Lodz (Protocol No RNN/105/22/ KE) and this study complies with the Declaration of Helsinki.
Statistical Analysis
The mean and standard deviation (mean ± SD) as well as the median and interquartile range (median (25%; 75%) were used for the description of the studied parameters. For data showing no temes from normality (according to Shapiro–Wilk’s test) with equal variances, the standard t-test was utilized to express the differences between groups. In other cases, the Mann–Whitney U-test was performed. In case of repeated measurements, a paired t-test was performed and Wilcoxon signed-rank test was applied, respectively. P values of less than 0.05 were considered statistically significant.
Results
Various evaluation criteria were used in this study, thus a complex statistical analysis was made. Carboxytherapy alone performed in the area of the right eye (Tables 1 and 2) significantly decreased the EI parameter, which reflected the severity of erythema. A reduction by a mean of −3.3 units (improvement in 69.2% of study participants) in the tear trough of the right eye and by −7.8 units (improvement in 82.1% of the individuals) in the middle area of the eye was observed. The improvement was also demonstrated on the left side where combined treatment was applied. A decrease of 7.2 in the EI parameter (improvement in 82.1% of individuals, ie, 32 out of 39 participants) in the tear trough area was reported. However, the effect of the treatment on the MI parameter (melanin level) was statistically insignificant.
Table 1.
The Change in MI/EI After a Series of Treatments in the Tear Trough
| Parameter (n=39) | Time point | p | |
|---|---|---|---|
| Baseline | After treatment | ||
| MI – tear trough (right) | 130.5±57.7 | 122.8±50.9 | NS (P=0.061) |
| Improvement [n] | --- | 25 [64.1%] | --- |
| Change [% vs baseline] | --- | −2.9 (−13.3; 5.2) | --- |
| EI – tear trough (right) | 394.4±77.0 | 378.7±77.0 | 0.015 |
| Improvement [n] | --- | 27 [69.2%] | --- |
| Change [% vs baseline] | --- | −3.3 (−7.8; 0.2) | --- |
| MI – tear trough (left) | 122.5±51.0 | 114.7±45.9 | NS (P=0.066) |
| Improvement [n] | --- | 24 [61.5%] | --- |
| Change [% vs baseline] | --- | −2.4 (−11.0; 4.7) | --- |
| EI – tear trough (left) | 397.6±91.0 | 365.8±81.3 | 0.002 |
| Improvement [n] | --- | 32 [82.1%] | --- |
| Change [% vs baseline] | --- | −7.2 (−14.5; −0.8) | --- |
Note: Bold font indicates statistical significance.
Table 2.
The Change in MI/EI After a Series of Treatments in the Centre of the Lower Eyelid
| Parameter (n=39) | Time point | p | |
|---|---|---|---|
| Baseline | After treatment | ||
| MI – the centre of the lower eyelid (right) | 117.8±49.2 | 111.5±42.2 | NS (P=0.181) |
| Improvement [n] | --- | 27 [69.2%] | --- |
| Change [% vs baseline] | --- | −2.8 (−7.0; 1.8) | --- |
| EI – the centre of the lower eyelid (right) | 347.7±71.7 | 317.5±76.7 | <0.0001 |
| Improvement [n] | --- | 32 [82.1%] | --- |
| Change [% vs baseline] | --- | −7.8 (−17.4; −2.5) | --- |
| MI – the centre of the lower eyelid (left) | 115.8±41.8 | 111.3±39.3 | NS (P=0.321) |
| Improvement [n] | --- | 25 [64.1%] | --- |
| Change [% vs baseline] | --- | −5.8 (−14.2; 10.8) | --- |
| EI – the centre of the lower eyelid (left) | 344.9±82.1 | 337.2±80.9 | NS (P=0.387) |
| Improvement [n] | --- | 21 [53.8%] | --- |
| Change [% vs baseline] | --- | −0.8 (−13.6; 8.0) | --- |
Note: Bold font indicates statistical significance.
The aim of the study was also to evaluate the impact of selected acids on specific skin parameters. Table 3 presents the changes in skin parameters in subgroups treated with one chemical peel. Lactobionic acid was used in 25 patients. Its application was associated with a statistically significant improvement in the EI parameter (p= 0.011) in the area of the tear trough. We also observed the improvement in the MI and the EI following the application of carboxytherapy combined with ferulic acid and ascorbic in the middle eyelid area and tear trough, respectively, however, these changes were not statistically significant (p=0.091 and p=0.069, respectively).
Table 3.
The Effects of Chemical Peels with Carboxytherapy on Assessed Skin Parameters Related to Pigmentary and Vascular Components of the Dark Circles
| Time | p | ||
|---|---|---|---|
| Baseline | After treatment | ||
| MI (carboxytherapy + ferulic acid+ ascorbic acid) – tear trough | 160.9±49.4 (n=14) |
142.5±46.5 (n=14) |
NS (P=0.093) |
| MI (carboxytherapy + ferulic acid+ ascorbic acid) – the centre of the eyelid | 147.5±43.1 (n=14) |
131.5±43.6 (n=14) |
NS (P=0.091) |
| EI (carboxytherapy + ferulic acid+ ascorbic acid) – tear trough | 462.2±86.9 (n=14) |
423.3±63.8 (n=14) |
NS (P=0.069) |
| EI (carboxytherapy + ferulic acid+ ascorbic acid) – the centre of the eyelid | 405.2±67.2 (n=14) |
396.0±72.5 (n=14) |
NS (P=0.593) |
| MI (carboxytherapy + lactobionic acid) – tear trough | 101.0±38.3 (n=25) |
99.1±38.1 (n=25) |
NS (P=0.473) |
| MI (carboxytherapy + lactobionic acid) – the centre of the eyelid | 98.0±29.1 (n=25) |
99.9±32.2 (n=25) |
NS (P=0.666) |
| EI (carboxytherapy + lactobionic acid) – tear trough | 361.4±72.3 (n=25) |
333.7±72.5 (n=25) |
P=0.011 |
| EI (carboxytherapy + lactobionic acid) – the centre of the eyelid | 311.1±70.2 (n=25) |
304.3±66.1 (n=25) |
NS (P=0.511) |
Note: Bold font indicates statistical significance.
When both indexes (MI + EI) were analysed together, a statistically significant reduction in pigmentation was observed in the tear trough and the middle of the eyelid together (both measurements point) both after carboxytherapy treatments and carboxytherapy - right side with chemical peelings - left side (Table 4).
Table 4.
Comparative Evaluation of Both Indices Together (MI+ EI) from Both Measurement Points Related to the Summed Pigmentation of the Skin Around the Eyes on the Right and Left Side (Comparing the Right Side with the Left Side Before Treatment and After Treatments: Carboxytherapy - Right Side, Carboxytherapy Plus Chemical Peels - Left Side)
| N=39 | Time | p | |
|---|---|---|---|
| Baseline | After treatment | ||
| MI+EI [Unit] – right side | 990.4±221.3 | 930.4±212.7 | P=0.001 |
| Change [% vs baseline] – right side | −5.6 (−10.2; −0.8) | --- | |
| MI+EI [Unit] – left side | 980.8±235.0 | 929.1±217.2 | P=0.015 |
| Change [% vs baseline] – left side | −3.8 (−10.8; 3.0) | --- | |
Note: Bold font indicates statistical significance.
Side Effects
Since CO2 is a physiological gas in the body, its intradermal administration was not associated with any significant adverse effects, including the occurrence of allergic reactions. Compared to other methods used in aesthetic dermatology and cosmetology, this technique is associated with a low risk of complications and does not disturb everyday functioning. Moreover, in this study, the performed procedure involved a minimal area of the lower eyelids, therefore the symptoms, sensations and side reactions were limited.
During carboxytherapy, participants experienced a spreading gas sensation beneath the skin, a slight sensation of pain, pressure, stinging, burning, itching, and tingling at the site of gas injection. The sensations usually lasted about 3 minutes. As a result of the stimulation of circulation, the temperature in the treated area increased locally by 1° - 1.5 °C for about 10 minutes. Skin temperature was randomly measured with the use of a non-contact infrared thermometer. In two participants, a small ecchymosis appeared at the injection site; however, it disappeared about 2–3 days after the procedure. Four individuals experienced slight swelling in the morning of the day following the treatment. The swelling resolved spontaneously within two hours from waking up. All these effects are normal clinical peri procedural symptoms which do not require medical intervention, and their intensity depends on individual predispositions. However, as with all skin procedures, there is always a risk of unpredictable reactions.
Discussion/Conclusion
Many researchers have assessed the reduction of hyperpigmentation and dark circles under the eyes. There are few scientific reports concerning the use of carboxytherapy to decrease the visibility of dark circles under the eyes.7,17,24–31 Moreover, the results obtained by other researchers differ from each other and sometimes presented changes are not statistically significant. These discrepancies may be associated with differences in the number of therapies in a series, the depth of gas injection, periprocedural care or the intensity of circles around the eyes. The effectiveness of treatments may also be influenced by other factors, such as age, gender, phases of the menstrual cycle in women, medications taken, and lifestyle (smoking and exposure to UV). To obtain objective results, we used the Mexameter probe, which measures the melanin and hemoglobin index separately. The selection of the measuring device enabled the evaluation of the impact of the studied procedure on both parameters.
The most pronounced statistically significant effects were observed in case of the EI parameter. Hemoglobin values were found to decrease in three out of four treatment areas. We were found that hemoglobin values decrease in three out of four treatment areas. Carboxytherapy improves skin microcirculation and, subsequently, promotes the narrowing of the vessel walls. Carboxytherapy has been demonstrated to stimulate the production of the extracellular matrix. It happens degradation of old collagen, as well as increase the production of new collagen. Therefore, carboxytherapy also is used in the treatment of wrinkles and skin laxity around the eyes.25,32 Using 3D, morphometric and histological skin analysis, El-Domyati M. et al showed very good and good improvement in skin texture and pigmentation in the majority of individuals who underwent 8 sessions of carboxytherapy (left side of the face). However, greater improvement was observed in the same patients on the right side of the face after 6 sessions of carboxytherapy combined with two CO2 fractional laser treatments. Carboxytherapy alone was associated with the stimulation of collagen production and improved reorganization of elastic fibres. 3D skin analysis, as well as morphometric and histological analysis, were performed.31 M. A. Nilforoushzadeh et al found that both carboxytherapy and Nd: YAG laser therapy were effective in the treatment of dark circles around the eyes, however, carboxytherapy produced more pronounced effects. Skin lightening and a decrease in the melanin content in the skin around the eyes were observed in the carboxytherapy group (p <0.0001). In this group, also a significant increase in skin elasticity (p <0.05) was shown. Higher skin elasticity translates into reduced visibility of skin capillaries and therefore, decreased erythema.28
Based on the above evidence and our own analysis, we concluded that the thickening of the epidermis and dermis can reduce the visibility of the circles. A statistically significant decrease in the intensity of the erythema was demonstrated around the tears trough area of the left (p = 0.002) and right (p = 0.015) eye. Therefore, it can be assumed that carboxytherapy has a significant effect on the reduction of vascular circles, and the increase in effectiveness (as evidenced by the higher statistical significance) is influenced by lactobionic acid applied to the skin of the left eye. After therapy with lactobionic acid, skin examination with the use of confocal microscopy has shown a significant reduction in the number of telangiectasias as well as a decrease in the lumen of capillaries. The results of the pilot studies indicate the beneficial effect of lactobionic acid on vascular disorders, including telangiectasia and the regulation of microcirculation in the skin.20
In our study, ferulic acid combined with ascorbic acid were used in participants with dark circles (n = 14), while lactobionic acid in individuals with vascular circles (n = 25). The greatest statistically significant change from the baseline values was observed after carboxytherapy combined with the application of lactobionic acid in the tear trough. In turn, Dayal S. et al demonstrated that the use of 20% glycolic acid or 15% lactic acid or 20% vitamin C reduced the pigmentation of periorbital melanosis. In their study, four sessions of treatments with glycolic acid or lactic acid were performed at three-week intervals, while vitamin C was applied topically at night for 12 weeks. The highest efficacy was demonstrated after the application of glycolic acid, and the lowest in the case of vitamin C.33 Zdunska K. et al assessed the effect of ferulic acid in combination with vitamin C on selected skin parameters, including the intensity of erythema and skin discoloration using the Mexameter probe. Statistically, significant reduction in pigmentation and erythema (skin lightening) was observed in case of both acids (p <0.0001).34 In another study, Zduńska K et al demonstrated the erythema-reducing effect of ferulic acid applied to photoaging skins. The changes in the results obtained with the Mexameter probe were highly statistically significant. The greatest improvement in erythema was observed one month after the last treatment (p <0.0001).35
We also combined the effects of carboxytherapy on the MI and the EI parameters in the area of tear trough and the middle of the eyelid for the right and left eyes separately. Statistically, significant differences in skin colour were found in the case of right and left eye. Therefore, it can be concluded that both a series of carboxytherapy alone and carboxytherapy combined with acids prove beneficial and effective in the reduction of periocular hyperpigmentation of various origins - both vascular and dark circles. The decrease in the EI appears to be more pronounced. The treatment used in this study improves skin microcirculation and, subsequently, promotes the narrowing of the vessel walls. Moreover, the thickening of the epidermis and dermis can reduce the visibility of the circles. The acids used in our study, have slightly exfoliating properties and stimulate the renewal of the epidermis, which could additionally intensify the effect of skin lightening and reduce the visibility of dark circles.
We decided on an optimal series of 5 carboxytherapy treatments. In other studies, the authors decided on number of 3–7 treatments in a series. Roshdy et al compared the effects of two different types of carbon dioxide flows (30 mL/min i 60 mL/min) in 40 individuals with dark circles subjected to 6 carboxytherapy treatments. A significant reduction of the circles under the eyes was observed in both groups.26 Also, P. Fioramonti et al demonstrated a 50–60% reduction in the intensity of circles under the eyes in a study carried out on a group of 90 patients who underwent 7 sessions of carboxytherapy at 1-week intervals.25 E. Nofal et al showed the reduction in periorbital hyperpigmentation (POH) in a group of 30 patients who underwent 7 carboxytherapy treatments.27 Eyraud et al conducted a study of the effect of a series of 3 carboxytherapy performed at weekly intervals on 35 subjects. The effects, based on photo analysis, were assessed by 3 independent evaluators and the study participants themselves. A statistical (p <0.00001) improvement of dark circles under the eyes was demonstrated. Moreover, They observed a reduction of superficial and deep wrinkles.17 In our study, we did not conduct a full analysis of the photographic documentation, focusing only on objectively measurable effects obtained from research probes. Nevertheless, the effects of the therapy can be seen in the photographs presented (Figures 2 and 3).
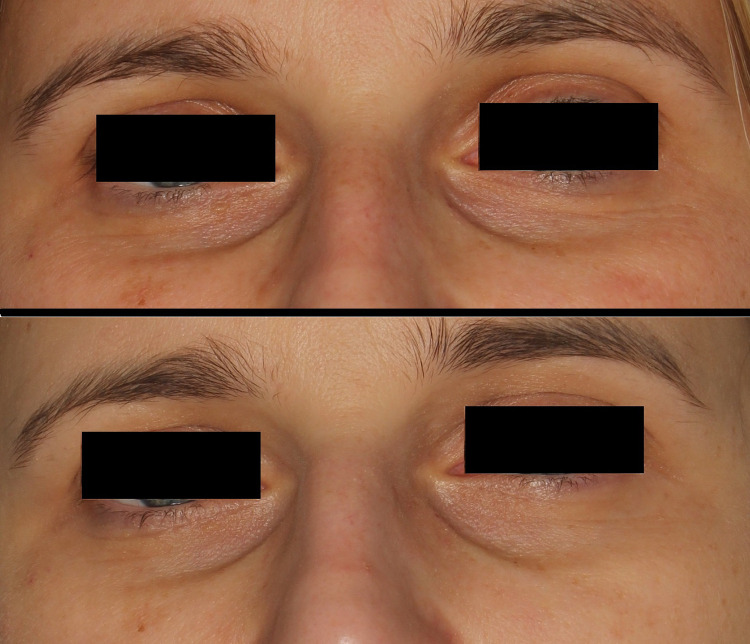
Figure 2.
Patient 38 years old; the effects of a series of carboxytherapy treatment: on the top - before the treatments; on the bottom - after a series of carboxytherapy (right eye area) and carboxytherapy combined with ferulic acid and L-ascorbic acid (left eye area). The effect of brightening the intensity of both the tear trough and minor pigmentation changes around the eyes was observed. It is also indicated to smooth the skin surface, reduce wrinkles that are a symptom of early photoaging of the skin.
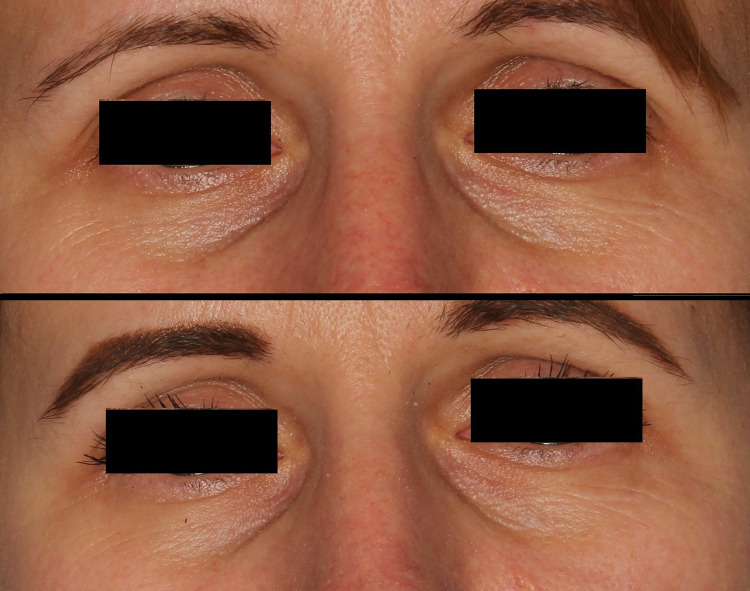
Figure 3.
Patient 30 years old; the effects of a series of carboxytherapy treatment: on the top - before the treatments; on the bottom - after a series of carboxytherapy (right eye area) and carboxytherapy combined with lactobionic acid (left eye area). The effect of reducing the visibility of vascular circles was observed. There is a significant improvement in smoothing (probably due to hydration) of the surface and wrinkles. A general improvement in skin color can be observed.
Limitations
The study was conducted on individuals aged between 25 and 55, thus it appears that a more restricted age range would be more appropriate. The validation process focused on only clinical evaluation and mexametric measurements. It would be beneficial to use multispectral camera analysis or videocapillaroscopy in order to distinguish vascular circles from pigmented circles. (not available to researchers). There was no control group. Despite the assumed difference in effectiveness, the acids turned out to have similar directions and effectiveness in the case of dark circles. We could choose other acids, eg tranexamic. The study group could be larger.
Conclusions
Both the series of carboxytherapy alone and its combination with acids proved to be effective in reducing the pigmentation of the skin around the eyes, the intensity of erythema, especially in case of vascular circles within tear trough. The objective results of this study confirmed the effectiveness of carboxytherapy in patients with ocular circles. Lactobionic acid, ferulic acid and ascorbic acid can be used as a safe supplementary therapy which enhances the effects of carboxytherapy.
Acknowledgments
This study was supported by statutory research at the activity Department of Cosmetology and Aesthetic Dermatology, Faculty of Pharmacy, Medical University of Lódź no. 503/3-066-01/503-31-001-19-00.
Statement of Ethics
Study approval statement: This study protocol was reviewed and approved by the Bioethics Committee of the Medical University of Łódź (Protocol No. RNN/105/22/ KE).
Subjects have given their written informed consent, and the study protocol was approved by the institute’s committee on human research.
Disclosure
The authors report no conflicts of interest in this work. The authors themselves are responsible for the content and writing of the paper.
References
- 1.Park KJ, Kwon HJ, Youn Ch S, Seo SJ, Kim MN. Treatments of Infra-Orbital Dark Circles by Various Etiologies. Ann Dermatol. 2018;30:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vrcek I, Ozgur O, Nakra T. Infraorbital dark circles: a review of the pathogenesis, evaluation and treatment. J Cutan Aesthet Surg. 2016;9:65–72. doi: 10.4103/0974-2077.184046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarkar R, Das A. Periorbital hyperpigmentation: what lies beneath? Ind Dermatol Online J. 2018;9(4):229–230. doi: 10.4103/idoj.IDOJ_303_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roh M, Chung KY. Infraorbital dark circles: definition, causes, and treatment options. Dermatol Surg. 2009;35(8):1163–1171. doi: 10.1111/j.1524-4725.2009.01213.x [DOI] [PubMed] [Google Scholar]
- 5.Mac-Mary S, Zornoza Solinis I, Predine O, et al. Identification Of Three Key Factors Contributing To The Aetiology Of Dark Circles By Clinical And Instrumental Assessments Of The Infraorbital Region. Clin Cosmet Invest Dermatol. 2019;12:919–929. doi: 10.2147/CCID.S217956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsui MS, Schalka S, Vanderover G, et al. Physiological and lifestyle factors contributing to risk and severity of peri-orbital dark circles in the Brazilian population. An Bras Dermatol. 2015;90(4):494–503. doi: 10.1590/abd1806-4841.20153520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed NA, Mohammed SS, Fatani MI. Treatment of periorbital dark circles: comparative study of carboxy therapy vs chemical peeling vs mesotherapy. J Cosmet Dermatol. 2019;18(1):169–175. doi: 10.1111/jocd.12536 [DOI] [PubMed] [Google Scholar]
- 8.Park SR, Kim HJ, Park HK, et al. Classification by causes of dark circles and appropriate evaluation method of dark circles. Skin Res Technol. 2016;22(3):276–283. doi: 10.1111/srt.12258 [DOI] [PubMed] [Google Scholar]
- 9.Verschoore M, Gupta S, Sharma VK, Ortonne JP. Determination of Melanin and Haemoglobin in the Skin of Idiopathic Cutaneous Hyperchromia of the Orbital region (ICHOR): a Study of Indian Patients. J Cutan Aesthet Surg. 2012;5(3):176–182. doi: 10.4103/0974-2077.101371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kikuchi K, Masuda Y, Hirao T. Imaging of hemoglobin oxygen saturation ratio in the face by spectral camera and its application to evaluate dark circles. Skin Res Technol. 2013;19(4):499–507. doi: 10.1111/srt.12074 [DOI] [PubMed] [Google Scholar]
- 11.Huang YL, Chang SL, Ma L, Lee MC, Hu S. Clinical analysis and classification of dark eye circle. Int J Dermatol. 2014;53(2):164–170. doi: 10.1111/j.1365-4632.2012.05701.x [DOI] [PubMed] [Google Scholar]
- 12.Colvan L, Fleck T, Vega VL. Global periorbital skin rejuvenation by a topical eye cream containing low molecular weight heparan sulfate (LMW-HS) and a blend of naturally derived extracts. J Cosmet Dermatol. 2019;18(2):530–538. doi: 10.1111/jocd.12857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kołodziejczak A, Podgórna K, Rotsztejn H. Is carboxytherapy a good alternative method in the removal of various skin defects? Dermatol Therap. 2018;31. [DOI] [PubMed] [Google Scholar]
- 14.Barańska-Rybak W, Mehrholz DM. Carboxytherapy in the light of the latest reports. Erythema multiforme-like eruption as a side effect of carboxytherapy. Dermatol Rev/Przegl Dermatol. 2019;106:46–51. [Google Scholar]
- 15.Varlaro V, Manzo G, Mugnaini F, et al. Carboxytherapy: effects on microcirculation and its use in the treatment of severe lymphedema. Acta Phlebol. 2007;8. [Google Scholar]
- 16.Doghaim NN, El-Tatawy RA, Neinaa YME-H, El-samd M.M A. Study of the efficacy of carboxytherapy in alopecia. J Cosmet Dermatol. 2018;17:1275–1285. doi: 10.1111/jocd.12501 [DOI] [PubMed] [Google Scholar]
- 17.Eyraud Q, La Padula S, Pizza C, Hersant B, Meningaud JP. Carboxytherapy, subcutaneous injections of carbon dioxide in the management of infraorbital dark circles: a reliable and effective procedure. J Craniomaxillofac Surg. 2021;49(8):670–674. doi: 10.1016/j.jcms.2021.01.028 [DOI] [PubMed] [Google Scholar]
- 18.King S, King M. Using carboxytherapy as an adjuvant aesthetic treatment for patients with alopecia. J Aesthetic Nurs. 2013;2:434–435. doi: 10.12968/joan.2013.2.9.434 [DOI] [Google Scholar]
- 19.Koutna N. Carboxytherapy: A New Noninvasive Method in Aesthetic Medicine. Vol. 145. Cas Lek Cesk; 2006:841–843. [PubMed] [Google Scholar]
- 20.Alonso S, Rendueles M, Díaz M. Bio-production of lactobionic acid: current status, applications and future prospects. Biotechnol Adv. 2013;31(8):1275–1291. doi: 10.1016/j.biotechadv.2013.04.010 [DOI] [PubMed] [Google Scholar]
- 21.Oresajo C, Stephens T, Hino PD. Protective Effects of a Topical Antioxidant Mixture Containing Vitamin C, Ferulic Acid, and Phloretin against Ultraviolet-Induced Photodamage in Human Skin. J Cosmet Dermatol. 2008;7:290–297. doi: 10.1111/j.1473-2165.2008.00408.x [DOI] [PubMed] [Google Scholar]
- 22.Murray JC, Burch JA, Streilein RD, Iannacchione MA, Hall RP, Pinnell SR. A Topical Antioxidant Solution Containing Vitamins C and E Stabilized by Ferulic Acid Provides Protection for Human Skin against Damage Caused by Ultraviolet Irradiation. J Am Acad Dermatol. 2008;59:418–425. doi: 10.1016/j.jaad.2008.05.004 [DOI] [PubMed] [Google Scholar]
- 23.Zduńska K, Dana A, Kolodziejczak A, Rotsztejn H. Antioxidant Properties of Ferulic Acid and Its Possible Application. Skin Pharmacol Physiol. 2018;31(6):332–336. doi: 10.1159/000491755 [DOI] [PubMed] [Google Scholar]
- 24.Seirafianpour F, Atefi N, Amin NG, et al. Effectiveness, safety, and patient satisfaction of carboxytherapy as an adjunctive treatment for periorbital hyperpigmentation. Skin Res Technol. 2024;30(3):e13651. doi: 10.1111/srt.13651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fioramonti P, Fallico N, Parisi P, Scuderi N. Periorbital area rejuvenation using carbon dioxide therapy. J Cosmet Dermatol. 11:223–228. doi: 10.1111/j.1473-2165.2012.00633.x [DOI] [PubMed] [Google Scholar]
- 26.Roshdy OH, Abd Elall HM, Eid AA. Randomized comparative study of the effect of two different flow rates of carboxytherapy in the treatment of infraorbital dark circles. J Cosmet Dermatol. 2021;1–8. [DOI] [PubMed] [Google Scholar]
- 27.Nofal E, Elkot R, Nofal A, Eldesoky F, Shehata S, Sami M. Evaluation of carboxytherapy and platelet-rich plasma in treatment of periorbital hyperpigmentation: a comparative clinical trial. J Cosmet Dermatol. 2018;17(6):1000–1007. doi: 10.1111/jocd.12478 [DOI] [PubMed] [Google Scholar]
- 28.Nilforoushzadeh MA, Heidari-Kharaji M, Alavi S, Zolghadr S, Mahmoudbeyk M, Nikkhah N. Nikkhah Comparison of carboxy therapy and fractional Q-switched ND: YAG laser on periorbital dark circles treatment: a clinical trial. Lasers Med Sci. 2021;36:1927–1934. doi: 10.1007/s10103-021-03274-5 [DOI] [PubMed] [Google Scholar]
- 29.Tahlawi E, Fawzy MM, Madawy ZE, Nesreen SM. Aboraia Platelet rich plasma versus Carboxytherapy in the treatment of Periorbital dark circles: a split-face study. J Cosmet Dermatol. 2022. [DOI] [PubMed] [Google Scholar]
- 30.Asilian A, Amiri A, Mokhtari F, Faghihi G, Iraji F, Mozafarpoor S. Platelet-rich plasma versus carboxytherapy for the treatment of periocular hyperpigmentation; which approach is superior? Dermatol Ther. 2021;34(4):14980. doi: 10.1111/dth.14980 [DOI] [PubMed] [Google Scholar]
- 31.El-Domyati M, Hosam El-Din W, Medhat W, Ibrahim MR, Khaled Y. The use of Carboxytherapy alone or in combination with fractional CO2 laser for facial rejuvenation: a split-face comparative study. J Cosmet Dermatol. 2020;19:1648–1655. doi: 10.1111/jocd.13470 [DOI] [PubMed] [Google Scholar]
- 32.Oliveira SMD, Rocha LB, da Cunha MTR, Cintra MMM, Pinheiro NM, Mendonça AC. Effects of carboxytherapy on skin laxity. J Cosmet Dermatol. 2020;19(11):3007–3013. doi: 10.1111/jocd.13337 [DOI] [PubMed] [Google Scholar]
- 33.Dayal S, Sahu P, VK J, Khetri S. Clinical efficacy and safety of 20% glycolic peel, 15% lactic peel, and topical 20% vitamin C in constitutional type of periorbital melanosis: a comparative study. J Cosmet Dermatol. 2016;15(4):367–373. doi: 10.1111/jocd.12255 [DOI] [PubMed] [Google Scholar]
- 34.Zduńska-Pęciak K, Kołodziejczak A, Rotsztejn H. Two superior antioxidants: ferulic acid and ascorbic acid in reducing signs of photoaging-A split-face comparative study. Dermatol Ther. 2022;35(2):15254. doi: 10.1111/dth.15254 [DOI] [PubMed] [Google Scholar]
- 35.Zduńska-Pęciak K, Dębowska R, Kołodziejczak A, Rotsztejn H. Ferulic acid - A novel topical agent in reducing signs of photoaging. Dermatol Ther. 2022;35(7):15543. doi: 10.1111/dth.15543 [DOI] [PubMed] [Google Scholar]