Abstract
Background and Hypothesis
Schizophrenia is a mental disorder usually presented in adulthood that affects roughly 0.3 percent of the population. The disease contributes to more than 13 million years lived with disability the global burden of disease. The current study aimed to provide new insights into the quality of care in Schizophrenia via the implementation of the newly introduced quality of care index (QCI) into the existing data.
Study Design
The data from the global burden of disease database was used for schizophrenia. Two secondary indices were calculated from the available indices and used in a principal component analysis to develop a proxy of QCI for each country. The QCI was then compared between different sociodemographic index (SDI) and ages. To assess the disparity in QCI between the sexes, the gender disparity ratio (GDR) was also calculated and analyzed in different ages and SDIs.
Study Results
The global QCI proxy score has improved between 1990 and 2019 by roughly 13.5%. Concerning the gender disparity, along with a rise in overall GDR the number of countries having a GDR score of around one has decreased which indicates an increase in gender disparity regarding quality of care of schizophrenia. Bhutan and Singapore had 2 of the highest QCIs in 2019 while also showing GDR scores close to one.
Conclusions
While the overall conditions in the quality of care have improved, significant disparities and differences still exist between different countries, genders, and ages in the quality of care regarding schizophrenia.
Keywords: global burden, mental disorder, gender disparity
Introduction
Schizophrenia is a severe and often life-long psychiatric disorder that usually presents in adulthood1 and affects roughly 0.3 percent of the population.2 Men have a higher risk of being diagnosed with schizophrenia with a relative risk of about 1.4 compared with women.3 Apart from extensive social and employment problems associated with the disease resulting in rates of unemployment as high as 90%,4 patients also suffer from long-term cognitive disabilities.5
Despite being known for centuries,6 an exact definition and etiology for the disease are still lacking.6,7 Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) provides a set of 6 criteria for the diagnosis of schizophrenia, the criteria include aspects of the disease’s symptoms and signs, as well as the exclusion of other probable causes.8 The disease is usually said to have three categories of symptoms: Positive symptoms (hallucinations, delusions, etc.), negative symptoms (lack of motivation, etc.), and cognitive impairments.9,10 Of the 3, negative and cognitive symptoms are more challenging to manage and are the true cause of impairment following the disease.11
Patients tend to have a shorter life expectancy of about 15 years compared to the general population and have elevated chances of suicide throughout their lives.5 Most of the other early deaths are due to cardiovascular disease, diabetes, cancer, and other diseases.12 Even though it is believed that most of this mortality stems from an unhealthy lifestyle exacerbated by low income and limited access to healthcare,13 new evidence points to physical changes and elevated inflammation that may also play a role in the observed decrease in life expectancy.14
Globally, schizophrenia contributes 13.4 million years lived with disability (YLDs) to the burden of disease,2 and the prevalence and the burden of disease seem to peak at about thirty years of age in both sexes.15 Also, the burden of disease experienced by the lower and middle-income countries is up to 4 times more than higher income regions.2 Furthermore, the patients’ socioeconomic status near the time of admission seems to be inversely correlated with the disease prevalence.15 That is, a deterioration in socioeconomic status is usually seen prior to the first hospitalization.
The annual societal cost of the disease was calculated to range from US $5818 to US $94 587 depending on the country.16 Furthermore, there seems to be a huge difference in the percentage of each country’s gross domestic product per capita spent for each person with schizophrenia, with numbers ranging from 37 to 214 percent in Switzerland and the UK, respectively.16 These data point to the fact that major inequality and differences exist between different regions in the quality and quantity of care.
Bearing in mind these challenges and problems, the present study aimed to assess the quality of care and its possible age and sex disparities regarding schizophrenia. To achieve our goal, the global burden of disease (GBD) database17 was used as the source of data.
Materials and Methods
Overview and Data Source
For the current study, the data from GBD database (1990–2019) was accessed through the IHME (Institute for Health Metrics and Evaluation) and retrieved (see supplementary material 3 for details). GBD is an international collaboration with the aim of creating a worldwide picture of current status of diseases.18
Schizophrenia, recorded in the 10th revision of the International Classification of the Diseases (ICD-10) under the codes F20-F20.9, and F25-F25.919 was reported on by the GBD under the classification code B.6.1 and age-standardized incidence, prevalence, disability-adjusted life years, and YLDs were available for the disease. As well as individual countries, the data is also available for different regions of the world, namely, the seven super-regions (High-income; Sub-Saharan Africa; Southeast Asia, East Asia and Oceania; North Africa and the Middle East; South Asia; Latin America and Caribbean; and Central Europe, Eastern Europe, and Central Asia). The study was created in accordance with the GATHER guidelines20 and was approved by the center’s research ethics committee.
Quality of Care Index
Quality of care index (QCI) was developed to enable us to compare disease-specific quality of care. To calculate QCI, four epidemiologically meaningful secondary indices are introduced by combining the available primary indices (ie, YLD, Prevalence, incidence): (1) The mortality-to-incidence ratio (MIR), (2) DALY-to-prevalence ratio, (3) Prevalence-to-incidence ratio, and (4) years of life lost-to-YLDs ratio. Next, a principal component analysis is performed in which the secondary indices are further summarized into a single index. principal component analysis is a statistical procedure that obtains orthogonal linear combinations of different variables into various components. The first principal component is therefore a linear combination of all the initial variables, that can best explain the variation in the data.21 This component is selected as the QCI by rescaling it into 0 to 100 with higher scores meaning better quality of healthcare. The exact calculations of QCI,22 as well as other implementations of the index, are previously published.23–34 For further details, refer to supplementary material 3.
Of the primary indices used in the calculation of QCI, death and years of life lost were not available in the current dataset and are essentially difficult to estimate for a non-fatal condition such as schizophrenia.35 Also, based on its definition, DALY is calculated as the sum of YLL and YLD, and due to the unavailability of YLL in the data, it had effectively the same value as the YLD. Ultimately, a proxy of QCI was calculated and used instead via inclusion of 2 of the 4 secondary indices, namely the DALY (YLD) to prevalence ratio and the prevalence to incidence, in the principal component analysis.
Sociodemographic Index
Based on the emphasis of the literature on the correlation between socioeconomic status and diagnosis and outcome of schizophrenia,36–38 the data were also divided based on the sociodemographic index (SDI) into 5 different subgroups. SDI is an index devised by the GBD study in which average educational attainment in the population above 15, lag-dependent income per capita, and total fertility rate are each scaled from 0 to 1 and then weighed equally to construct a geometric mean.17
Age and Gender Disparities
To investigate the inequities between different ages in terms of quality of care, the population was divided into age groups, and the QCI change was plotted in each group. As for gender inequity, gender disparity ratio (GDR) was defined as the ratio of female QCI to male QCI. GDR was calculated for each country and was used in the analysis.
Validation of QCI
The healthcare access and quality index was introduced by the IHME in order to assess personal healthcare access and quality in different regions.39 To check the validity of QCI, first a mixed-effect regression model by random effect of countries was used with the QCI as the dependent variable and the inpatient admissions per capita, outpatient visits per capita, and schizophrenia prevalence as the independent variables.40 Age-standardized values were used to enable comparison. The Pearson’s correlation coefficient was then calculated between the healthcare access and quality index and this predicted value of QCI to be 0.70. This suggests that both indices assess relatively similar constructs in quality of care evaluation analysis (see supplementary material 3 for details).
Results
Epidemiology of Schizophrenia:
Schizophrenia accounted for more than 15 million (95% uncertainty interval: 11 to 19) YLDs in the year 2019, this was an increase of 65.4% (62.4 to 68.9) from the 9 million (7 to 12 million) YLDs in 1990. The same was true for prevalence and incidence which showed increases of 65.9% (62.8 to 69.1) and 37.1% (33.1 to 41.3), respectively. Even though in the years between 1990 and 2019, the all-ages values for all these primary indices (YLD, prevalence, and incidence) were increased, the age-standardized rates were slightly decreased by 0.6% (−1.6 to 0.4), 0.9% (−1.7 to −0.1), and 3.3% (−4.3 to −2.2) for YLDs, prevalence, and incidence, respectively.
A comparison based on the SDI class revealed that while an increase in primary indices was observed in all classes, the lower SDI class witnessed the greatest increase with all the values roughly doubled during this period (an increase of 127.9 percent (125.1 to 130.6) in prevalence, 116.2 percent (113.5 to 118.8) in incidence, and 129.8 percent (125.0 to 134.6) in YLDs). As for the age-standardized values, regardless of the SDI class, the changes were minimal (details in supplementary material 2A). The studies used for the estimation of the prevalence, incidence, YLDs and disability-adjusted life years related to schizophrenia globally, regional, and country-based are provided in supplementary material 1.
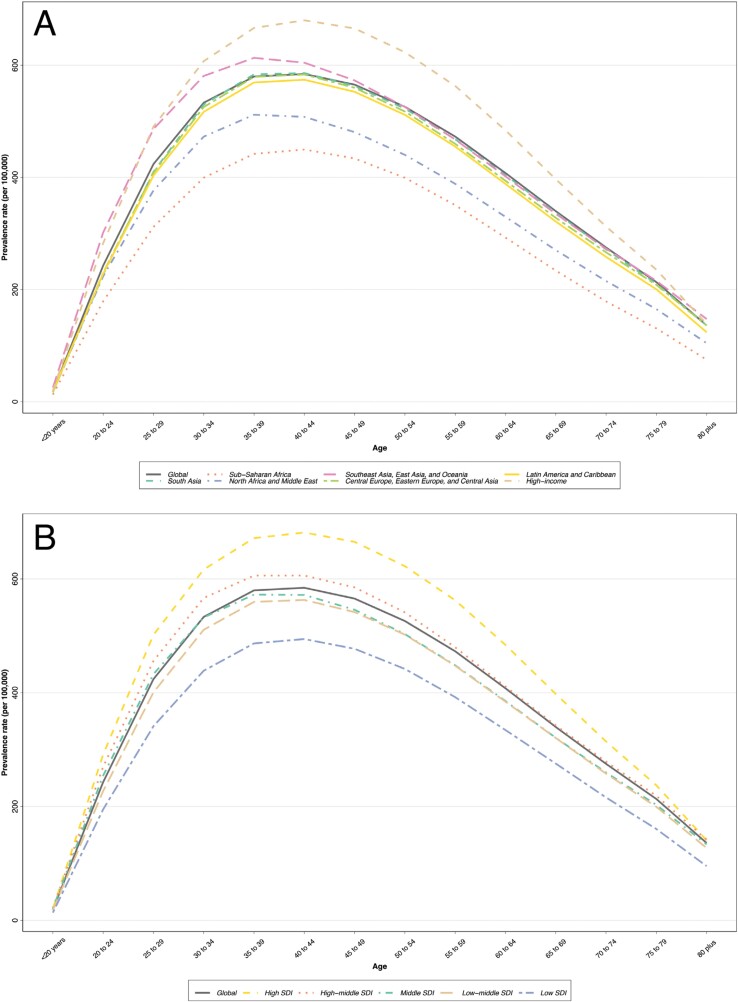
Assessment of schizophrenia’s prevalence in different ages in 2019 revealed that disease prevalence followed an expected pattern of increasing until adulthood and then decreased gradually towards the end of life both globally and in different regions. The same overall prevalence pattern was also observed in different classes of SDI (figure 1).
Fig. 1.
Prevalence of Schizophrenia in different ages based on (A) 7 global burden of disease super-regions and (B) sociodemographic index quintiles.
Quality of Care Index
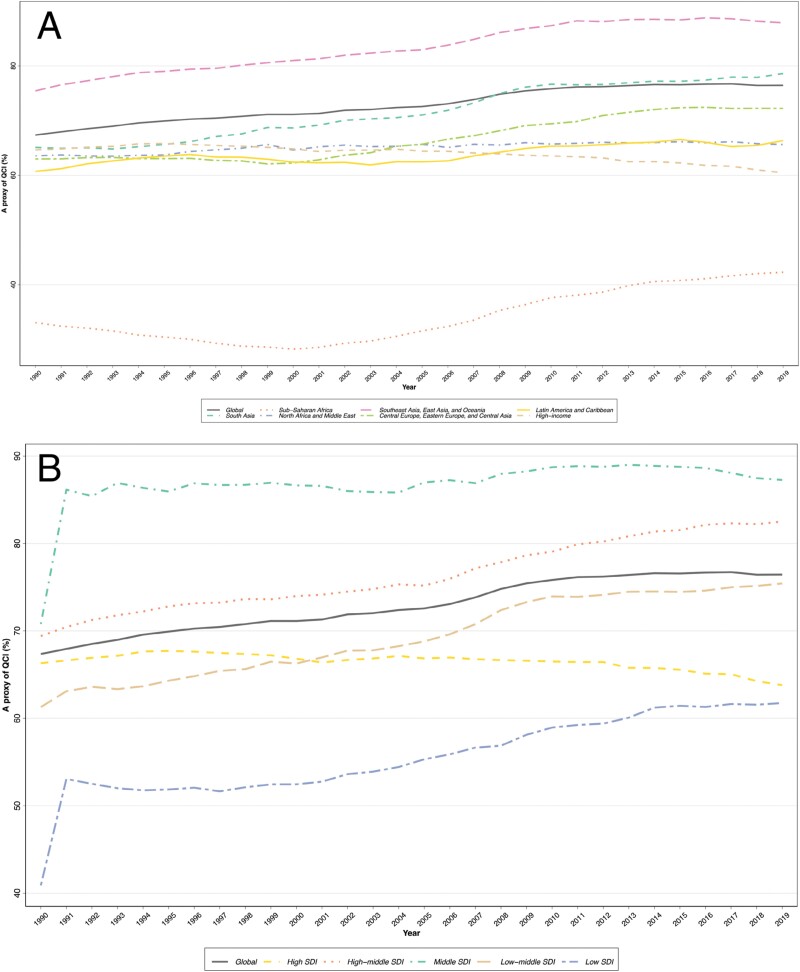
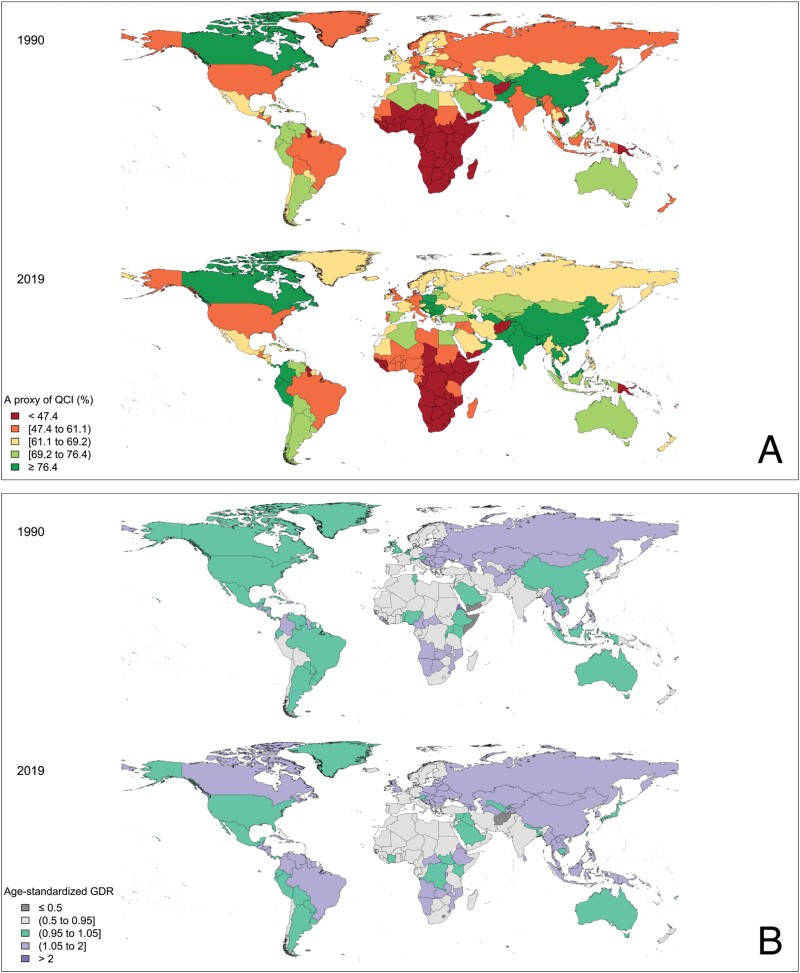
The global age-standardized QCI for schizophrenia increased 13.5%, from 1990 to 2019 with the index being 67.4 and 76.4, respectively. As for the regional situation, both in 1990 and 2019 the highest age-standardized QCI belonged to Southeast Asia, East Asia, and Oceania (75.4 in 1990 and 87.9 in 2019) while the lowest belonged to the Sub-Saharan Africa (33.1 in 1990 and 42.3 in 2019). View table 1 for more details. At the country level in 1990, Bermuda, Canada, and Bhutan had the highest age-standardized QCI of 87.9, 87.1, and 87.1, respectively, while the lowest QCI belonged to Central African Republic, Uganda, and Afghanistan with values of 4.8, 8.0, and 9.8, respectively. In 2019, the countries with the highest QCI were Bhutan, Singapore, and Bangladesh (100, 98.2, and 97.6, respectively) while those with the lowest QCI were Lesotho, Central African Republic, and Afghanistan (5.6, 11.5, and 15.2, respectively). Uganda had the most significant improvement in QCI with an increase of 347.1% from 8.0 to 35.9 and Lesotho showed the most drastic decline with a decrease of 81.9% (from 31.0 to 5.6). A yearly trend showing the change in QCI in each of the 7 super-regions is shown in figure 2A and a world map depicting the QCI in each country for both sexes is shown in figure 3A.
Table 1.
Values of Age-Standardized Quality of Care Index (QCI) and Gender Disparity Ratio (GDR) in 7 Global Burden of Disease Super-Regions and 5 Sociodemographic Index Quintiles
| Location Type | Location Name | Age-Standardized QCI | Age-Standardized GDR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Both | Female | Male | 1990 | 2019 | |||||
| 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | ||||
| global | 67.4 | 76.4 | 68.6 | 80 | 68 | 75.1 | 1.01 | 1.06 | |
| 7 GBD Super-regions | Central Europe, Eastern Europe, and Central Asia | 63 | 72.2 | 73.6 | 81.2 | 56.6 | 66.5 | 1.3 | 1.22 |
| High-income | 64.6 | 60.5 | 64.2 | 59.8 | 67.7 | 64.5 | 0.95 | 0.93 | |
| Latin America and Caribbean | 60.7 | 66.3 | 63.1 | 70.3 | 62.2 | 66.1 | 1.01 | 1.06 | |
| North Africa and Middle East | 63.5 | 65.6 | 58 | 60.6 | 69 | 69.9 | 0.84 | 0.87 | |
| South Asia | 65.1 | 78.6 | 58.1 | 76 | 69.6 | 80.9 | 0.83 | 0.94 | |
| Southeast Asia, East Asia, and Oceania | 75.4 | 87.9 | 77.6 | 94 | 73.8 | 82.4 | 1.05 | 1.14 | |
| Sub-Saharan Africa | 33.1 | 42.3 | 33.2 | 42.7 | 36.6 | 45.4 | 0.91 | 0.94 | |
| SDI | High SDI | 66.3 | 63.8 | 66.5 | 64.2 | 68.6 | 66.2 | 0.97 | 0.97 |
| High-middle SDl | 69.4 | 82.5 | 73.2 | 86.1 | 67.9 | 79.8 | 1.08 | 1.08 | |
| Middle SDl | 70.8 | 87.3 | 71.7 | 84.7 | 70.6 | 89.1 | 1.02 | 0.95 | |
| Low-middle SDI | 61.3 | 75.4 | 57.3 | 72.2 | 65 | 78.6 | 0.88 | 0.92 | |
| Low SDI | 40.9 | 61.7 | 36.6 | 49 | 46.9 | 72.9 | 0.78 | 0.67 | |
Fig. 2.
Time trend of age-standardized quality of care index proxy from 1990 to 2019 in (A) the global and 7 global burden of disease super-region, both sexes, and (B) the global and 5 sociodemographic index quintile, both sexes.
Fig. 3.
Geographical distribution of (A) age-standardized quality of care index proxy in 1990 and 2019 for both sexes and (B) age-standardized gender disparity ratio in 1990 and 2019.
Sociodemographic Indices
A comparison of QCI based on SDI revealed that the middle-SDI countries had the highest QCI both in 1990 and 2019 (70.8 and 87.3, respectively). Even though a considerable improvement was observed in the QCI in low-SDI countries (40.9 in 1990 to 61.7 in 2019; 51.0% increase), they remained low both in 1990 and 2019. Yearly trends of change in the QCI based on the SDI classification were illustrated in figure 2B.
Gender Disparity Ratio
The global age-standardized GDR rose from 1.01 to 1.06 from 1990 to 2019. Overall, Eastern Europe and East Asian countries had the highest GDRs both in 1990 and 2019 (1.30 and 1.22), while the countries in North Africa and Middle East had the lowest (0.84 in 1990 and 0.87 in 2019). More details are available in table 1.
In addition to the slight rise in global age-standardized GDR from 1990 to 2019, there has also been a decrease in the number of countries that show a ratio of near one (between 0.95 and 1.05) from 57 in 1990 to 41 in 2019. Interestingly, the top three countries with the highest QCI in 2019 (Bhutan, Singapore, and Bangladesh) also showed some of the closest GDR scores to one with ratios of 1.02, 1.09, and 0.99, respectively.
Also at the country level, Eritrea had the highest GDR in 1990 (2.70) while Liberia had the lowest (0.31). In 2019, the country with the highest GDR was Burundi (1.91) while the lowest was Lesotho (0.35). Also, Burundi demonstrated the highest increase in the study period with a 94.9% change (from 0.98 to 1.91) while Afghanistan showed the most significant decline with 70.5% (from 1.33 to 0.39). The GDR for individual countries is shown in figure 3B. More details in supplementary material 2C.
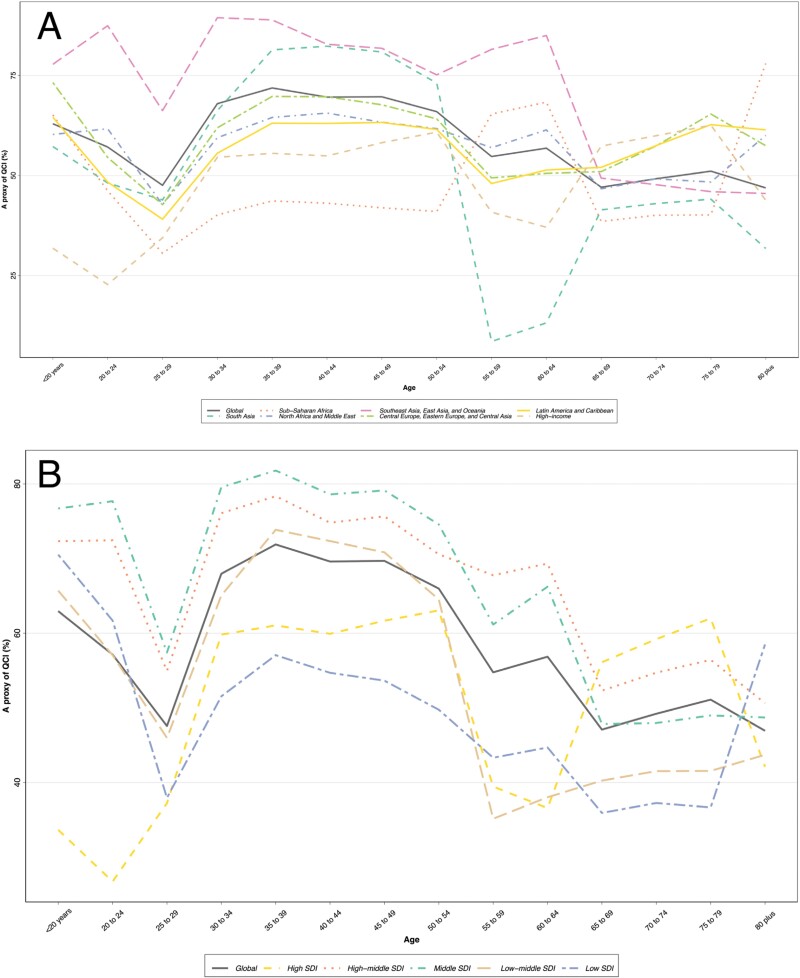
Age Disparity in QCI
Globally, after a sharp decrease in QCI in early adulthood and a subsequent increase in years 30 to 40, the trend showed a gradual decline towards the end of life. The same overall pattern was seen in the world’s seven super-regions except Central Europe, Eastern Europe, and Central Asia in which QCI shows a sudden decrease in the sixth decade of life (figure 4A). As for different SDIs, the same pattern was observed except for a significant increase in QCI in high SDI countries in the elderly (65 to 80). See figure 4B for more detail.
Fig. 4.
Age trend of quality of care index proxy in (A) the global and 7 global burden of disease super-regions, both sexes, and (B) the global and 5 sociodemographic index quintiles, both sexes.
Discussion
While schizophrenia reportedly inflicts less than one percent of the population,41 Its chronic nature coupled with debilitating symptoms account for the disease’s high impact on burden. Furthermore, GBD data show a steady increase in the incidence and prevalence of schizophrenia in the years between 1990 and 2019. Considering the results, the overall quality of care regarding schizophrenia seems to be improving globally as well as in many regions of the world. Such a trend may be explained by recent advances in the treatment approaches and improved outcomes regarding schizophrenia,42–44 as well as, general improvements in healthcare including the rise in health expenditure observed in the same period globally.45,46
Prior studies suggest that a low socioeconomic level especially near the diagnosis period is correlated with a higher prevalence of schizophrenia.15,47,48 Immigrants and especially refugees were also found to have significantly higher chances of being diagnosed with schizophrenia, further emphasizing the role of socioeconomic status in the disease.49 Furthermore, unemployment has been shown to be associated with schizophrenia, especially in older populations.50 This is important because the countries with low SDI are also those with worse QCI scores which can hypothetically exacerbate this situation. Lower access to healthcare combined with lower socioeconomic status in these countries can potentially delay proper diagnosis and care which can impact the prognosis.
Another interesting finding is the fact that the highest QCI scores belong to the middle-SDI countries and not those with the highest SDI score. While higher socioeconomic status is generally thought to be correlated with lower prevalence of schizophrenia, in a study by Lima, a link was found between higher income and greater use of psychoactive drugs,51 which are considered a widely recognized predisposing factor for the disease.49 However, such an observation can also be due to under-reporting of the disease in other classes.
Gender disparity is defined as “the difference in the management of men and women having the same clinical diagnosis, which may eventually have positive, negative or neutral health consequences.”52 The GDR has risen through the study period and while regions such as the southern Asia or many of the European countries have GDRs of roughly equal or greater than one, in other regions such as African or central Asian countries, GDR values are significantly less than one which points to a lower quality of care received by women in these regions compared to men. Furthermore, assuming a lower access of women to healthcare services regarding schizophrenia in these regions, a diagnosis disparity is also likely to occur with women being less likely to be properly diagnosed in the first place and therefore being underrepresented in the available data. In such an instance, the actual gender disparity between the sexes may in fact be even more significant. Similar results were also observed in another QCI study regarding ischemic heart disease.23 This is in contrast with other studies regarding different areas of medicine53 that have reported decreasing trends in GDR. A possible explanation might be that treatment approaches and their efficacies for schizophrenia have significantly advanced in recent years. Better treatment will lead to better outcomes which when coupled with an already existing inherent disparity in healthcare access between the sexes, can potentially magnify such a difference and cause the observed upward trend in GDR.
Gender disparity is not unique to schizophrenia, as in a study in Spain, men and women were found to receive different qualities and types of care while having the same clinical diagnosis and conditions.54 While men tend to have higher overall mortality, women live longer with disease-related morbidities, this, coupled with women’s general lower access to financial resources, imposes a significantly heavier burden on them.55 Another study in Bangladesh found women and children to be underrepresented in the health data largely due to limited access to healthcare services.56 This disparity becomes more evident as age advances, as a study found more than fifty percent of the total gender gap in hospitalization expenses to be due to the disparities between elderly women compared to men.57 Interestingly, in a study in United States concerning psychiatric disorders and in particular late-life depression, men were found to be significantly less likely to receive proper medical care compared with women and this finding was proposed to be due to mental disease social stigma and masculine traits in the society.58 Overall, GDR seems to be highly affected by the geographical, and social norms and differences.
Also visible from the results is the fact that healthcare quality is not consistent in different age groups. This is of special importance due to the chronicity of the disease as it can impact the well-being of individuals as their age changes. Considering the correlation between the QCI and age, the global trend tends to follow a gradual decrease through the ages following an increase in the 25–29 years of age which overall matches that of the disease prevalence. Interestingly, however, while south Asian countries have provided the best quality of care based on the QCI and especially in the early adulthood (25 to 50 years of age), there exists a sharp decline in the index in this region in the 55 to 59 years of age which never fully recovers afterwards. Such a result may in part be due to a decline in the number of total population from these age groups forth. Contrary to that, in the sub-Saharan region, the reverse is witnessed in which the QCI has a sudden increase in the same age group while being relatively low for the rest of the age spectrum. Considering the overall quality of care in these two regions and the fact that schizophrenia is usually first diagnosed in the early adulthood,2 allocating more resources in order to ensure better quality of care in this period of life seems to be important in achieving overall better results.
Among the countries in the world, Singapore and Bhutan stand out as both having two of the highest QCI scores in 2019 and also GDRs of close to one. A brief review of their health policies regarding Schizophrenia (and mental health in general) is both informative and interesting especially as these countries have managed to have such favorable results despite having very different economic conditions: In 2019, the world bank reported Bhutan to have a gross domestic product per capita of nearly 3250 US dollars while in the same year Singapore had a gross domestic product per capita of more than 65 500 US dollars.59
Until recently, most of the services provided for mental health in Singapore were only accessible at the Institute of Mental Health, a state hospital specializing in the field. This had led to high workloads in the institute and there was a substantial a shortage of trained workforce. In the last 2 decades, new laws and policies were enacted to decentralize the provision of mental health services and increase the number of specialists. Currently, while Institute of Mental Health remains the sole institute capable of involuntary admission, a considerable portion of the counseling and supportive services are provided in outpatient centers. This helps by both reducing the strain on the inpatient sector and also by improving the availability of the service.60,61 In 2005, the government tasked a committee with formulation of a new policy and roadmap for the improvement of healthcare in the country. The new policy encompasses a wider range of topics from better education and reduction of stigma to encouraging research and an evaluation system. Furthermore, several financial steps have been taken to ensure better accessibility of healthcare for all citizens.62
A small country with limited financial resources, Bhutan implemented its first mental health policy in 1997 in the name of National Mental Health Program. It was created with the goal of ensuring accessible mental healthcare to all the citizens. Considering the limited resources and lack of proper infrastructure, an integration of mental and general healthcare services was proposed in which upon a visit to any of the country’s primary healthcare facilities, people could receive the required mental healthcare. These facilities, though mostly operating without a psychiatrist and relying on the primary physician for the provided care, not only offered outpatient care but were also capable of voluntary and involuntary patient admission.63
Overall, ensuring proper availability and accessibility of the healthcare, along with population education and destigmatization of seeking professional help for mental health issues seems to be the key factor in achieving the present results in both countries.
Strengths and Limitations
The GBD 2019 data and estimates have been used in the present work, and although the GBD data are considered the best available option in global comparison studies, they are the result of complex mathematical modeling and are themselves restricted by the data collection inaccuracies, under-reporting, and lack of published data in different countries. Also, since mortality rates were not available in the GBD data, the original QCI had to be modified to be used here. To overcome possible errors introduced in the result of this issue, the QCI was validated using the healthcare access and quality index.
Another limitation present in all studies implementing QCI is that calculating the confidence intervals for the QCI and GDR is not feasible due to nature of statistics and limited computational resources.24,25,27,30–34,64 However, the study achieves its primary goal of providing a global bird’s eye view of the current status of quality of healthcare regarding schizophrenia.
Conclusion
Considering the overall results, conditions regarding the quality of care in schizophrenia seem to be improving globally. However, the same cannot be said for gender disparity as both a drift in global ratio away from one and a decline in the number of countries with a ratio close to one is observed in the studied period. Furthermore, major differences remain between world regions with different income levels and SDIs. Hence, not all age groups receive healthcare of the same quality when it comes to schizophrenia. With the disease having a chronic and life-long nature and being able to cause significant morbidity, a long way is still ahead to further improve the conditions of those affected worldwide. There are also other potential factors such as race and ethnicity which may have significant effects both on the disease course and outcome, and on the quality of healthcare services received by the individuals.
Supplementary Material
Supplementary material is available at https://academic.oup.com/schizophreniabulletin/.
Acknowledgments
We would like to thank all the staff of Non-Communicable Diseases Research Center (NCDRC) and Endocrinology and Metabolism Research Institute (EMRI) of Tehran University of Medical Sciences for their invaluable cooperation. Sahar Saeedi Moghaddam’s contribution was financially supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany`s Excellence Strategy – EXC 2167-390884018.
Contributor Information
Kaveh Same, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Parnian Shobeiri, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Mohammad-Mahdi Rashidi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Erfan Ghasemi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Sahar Saeedi Moghaddam, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran; Kiel Institute for the World Economy, Kiel, Germany.
Esmaeil Mohammadi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran; Department of Neurological Surgery, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
Masoud Masinaei, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Niloufar Salehi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Sahar Mohammadi Fateh, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Seyed Farzad Maroufi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Elham Abdolhamidi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Mana Moghimi, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Zeinab Abbasi-Kangevari, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Negar Rezaei, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran; Digestive Disease Research Center (DDRC), Digestive Disease Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
Bagher Larijani, Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran; Endocrinology and Metabolism Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran.
Conflicts of interest:
The Authors have declared no conflicts of interest in relation to the subject of this study.
References
- 1. Addington J, Heinssen R.. Prediction and prevention of psychosis in youth at clinical high risk. Annu Rev Clin Psychol. 2012;8:269–289. [DOI] [PubMed] [Google Scholar]
- 2. Charlson FJ, Ferrari AJ, Santomauro DF, et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. 2018;44(6):1195–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Janoutová J, Janackova P, Sery O, et al. Epidemiology and risk factors of schizophrenia. Neuro Endocrinol Lett. 2016;37(1):1–8. [PubMed] [Google Scholar]
- 4. Owen MJ, Sawa A, Mortensen PB.. Schizophrenia. Lancet. 2016;388(10039):86–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McCutcheon RA, Reis Marques T, Howes OD.. Schizophrenia-an overview. JAMA Psychiatry. 2020;77(2):201–210. [DOI] [PubMed] [Google Scholar]
- 6. Tandon R, Gaebel W, Barch DM, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013;150(1):3–10. [DOI] [PubMed] [Google Scholar]
- 7. Harris LW, Guest PC, Wayland MT, et al. Schizophrenia: metabolic aspects of aetiology, diagnosis and future treatment strategies. Psychoneuroendocrinology. 2013;38(6):752–766. [DOI] [PubMed] [Google Scholar]
- 8. Biedermann F, Fleischhacker WW.. Psychotic disorders in DSM-5 and ICD-11. CNS Spectr. 2016;21(4):349–354. [DOI] [PubMed] [Google Scholar]
- 9. van Os J, Kapur S.. Schizophrenia. Lancet. 2009;374(9690):635–645. [DOI] [PubMed] [Google Scholar]
- 10. Joyce EM, Roiser JP.. Cognitive heterogeneity in schizophrenia. Curr Opin Psychiatry. 2007;20(3):268–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884–897. [DOI] [PubMed] [Google Scholar]
- 12. Laursen TM, Nordentoft M, Mortensen PB.. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425–448. [DOI] [PubMed] [Google Scholar]
- 13. Liu NH, Daumit GL, Dua T, et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. 2017;16(1):30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Filipčić IS, Filipčić I.. Schizophrenia and Physical Comorbidity. Psychiatr Danub. 2018;30(5):299–909. [PubMed] [Google Scholar]
- 15. Häfner H, an der Heiden W.. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42(2):139–151. [DOI] [PubMed] [Google Scholar]
- 16. Jin H, Mosweu I.. The societal cost of schizophrenia: a systematic review. PharmacoEcon. 2017;35(1):25–42. [DOI] [PubMed] [Google Scholar]
- 17. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Murray CJ, Abbafati C, Abbas KM, et al. Five insights from the global burden of disease study 2019. Lancet. 2020;396(10258):1135–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. In. 2nd ed. Geneva: World Health Organization; 2004. [Google Scholar]
- 20. Stevens GA, Alkema L, Black RE, et al. ; GATHER Working Group. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. PLoS Med. 2016;13(6):e1002056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rechner AC. Methods of Multivariate Analysis. New York, United States: Wiley; 2003. [Google Scholar]
- 22. Mohammadi E, Ghasemi E, Saeedi Moghaddam S, et al.. Quality of care index (QCI). Protocolsio. 2020. https://www.protocols.io/view/quality-of-care-index-qci-bprjmm4n.html [Google Scholar]
- 23. Aminorroaya A, Yoosefi M, Rezaei N, et al. Global, regional, and national quality of care of ischaemic heart disease from 1990 to 2017: a systematic analysis for the Global Burden of Disease Study 2017. Eur J Prev Cardiol. 2021;29:371–379. [DOI] [PubMed] [Google Scholar]
- 24. Keykhaei M, Masinaei M, Mohammadi E, et al. A global, regional, and national survey on burden and Quality of Care Index (QCI) of hematologic malignancies; global burden of disease systematic analysis 1990–2017. Exp Hematol Oncol. 2021;10(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mohammadi E, Ghasemi E, Azadnajafabad S, et al. A global, regional, and national survey on burden and Quality of Care Index (QCI) of brain and other central nervous system cancers; global burden of disease systematic analysis 1990-2017. PLoS One. 2021;16(2):e0247120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aryannejad A, Tabary M, Ebrahimi N, et al. Global, regional, and national survey on the burden and quality of care of pancreatic cancer: a systematic analysis for the global burden of disease study 1990–2017. Pancreatology. 2021;21(8):1443–1450. [DOI] [PubMed] [Google Scholar]
- 27. Azadnajafabad S, Saeedi Moghaddam S, Mohammadi E, et al. Global, regional, and national burden and quality of care index (QCI) of thyroid cancer: a systematic analysis of the Global Burden of Disease Study 1990–2017. Cancer Med. 2021;10(7):2496–2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Khanali J, Malekpour M-R, Azangou-Khyavy M, et al. Global, regional, and national quality of care of gallbladder and biliary tract cancer: a systematic analysis for the global burden of disease study 1990–2017. Int J Equity Health. 2021;20(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Momtazmanesh S, Saeedi Moghaddam S, Malakan Rad E, et al. Global, regional, and national burden and quality of care index of endocarditis: the global burden of disease study 1990–2019. Eur J Prev Cardiol. 2021;29:1287–1297. [DOI] [PubMed] [Google Scholar]
- 30. Azadnajafabad S, Saeedi Moghaddam S, Keykhaei M, et al. Expansion of the quality of care index on breast cancer and its risk factors using the Global Burden of Disease Study 2019. Cancer Med. 2022;12:1729–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hanifiha M, Ghanbari A, Keykhaei M, et al. Global, regional, and national burden and quality of care index in children and adolescents: a systematic analysis for the global burden of disease study 1990-2017. PLoS One. 2022;17(4):e0267596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nejadghaderi SA, Roshani S, Mohammadi E, et al. The global, regional, and national burden and quality of care index (QCI) of colorectal cancer; a global burden of disease systematic analysis 1990-2019. PLoS One. 2022;17(4):e0263403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Karimi A, Shobeiri P, Azadnajafabad S, et al. A global, regional, and national survey on burden and Quality of Care Index (QCI) of bladder cancer: the global burden of disease study 1990-2019. PLoS One. 2022;17(10):e0275574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mousavi SF, Peimani M, Moghaddam SS, et al. National and subnational survey on diabetes burden and quality of care index in Iran: a systematic analysis of the global burden of disease study 1990-2019. J Diabetes Metab Disord. 2022;21(2):1599–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Aghababaie-Babaki P, Malekpour M-R, Mohammadi E, et al. Global, regional, and national burden and quality of care index (QCI) of bipolar disorder: a systematic analysis of the Global Burden of Disease Study 1990 to 2019. Int J Soc Psychiatry. 2023:207640231182358. [DOI] [PubMed] [Google Scholar]
- 36. Brown AS. The environment and susceptibility to schizophrenia. Prog Neurobiol. 2011;93(1):23–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Allardyce J, Boydell J.. Environment and schizophrenia: review: the wider social environment and schizophrenia. Schizophr Bull. 2006;32(4):592–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Byrne M, Agerbo E, Eaton WW, Mortensen PB.. Parental socio-economic status and risk of first admission with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2004;39(2):87–96. [DOI] [PubMed] [Google Scholar]
- 39. Fullman N, Yearwood J, Abay SM, et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391(10136):2236–2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Institute for Health Metrics and Evaluation. Global Inpatient and Outpatient Health Care Utilization, Unit Costs, and Costs and Services Needed to Achieve Universal Health Coverage 1990-2016. 10.6069/RW6Y-K168. 2018. Accessed September 1, 2022.. [DOI]
- 41. McGrath J, Saha S, Chant D, Welham J.. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30(1):67–76. [DOI] [PubMed] [Google Scholar]
- 42. Yang AC, Tsai SJ.. New targets for schizophrenia treatment beyond the dopamine hypothesis. Int J Mol Sci . 2017;18(8):1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Stępnicki P, Kondej M, Kaczor AA.. Current concepts and treatments of schizophrenia. Molecules. 2018;23(8):2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Silva MA, Restrepo D.. Functional recovery in schizophrenia. Rev Colomb Psiquiatr (Engl Ed). 2019;48(4):252–260. [DOI] [PubMed] [Google Scholar]
- 45. Schäferhoff M, Martinez S, Ogbuoji O, Sabin ML, Yamey G.. Trends in global health financing. BMJ. 2019;365:l2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Global Burden of Disease Health Financing Collaborator Network. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995-2050. Lancet. 2019;393(10187):2233–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ding R, Zhang L, He P, Song X, Zheng X.. Income, income inequality and schizophrenia in China: a population-based multilevel analysis. J Epidemiol Community Health. 2020;74(9):719–725. [DOI] [PubMed] [Google Scholar]
- 48. Hakulinen C, Webb RT, Pedersen CB, Agerbo E, Mok PL.. Association between parental income during childhood and risk of schizophrenia later in life. JAMA Psychiatry. 2020;77(1):17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Stilo SA, Murray RM.. Non-genetic factors in schizophrenia. Curr Psychiatry Rep. 2019;21(10):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chen L, Selvendra A, Stewart A, Castle D.. Risk factors in early and late onset schizophrenia. Compr Psychiatry. 2018;80:155–162. [DOI] [PubMed] [Google Scholar]
- 51. Lima MC, Menezes PR, Carandina L, Cesar CL, Barros MB, Goldbaum M.. [Common mental disorders and the use of psychoactive drugs: the impact of socioeconomic conditions]. Rev Saude Publica. 2008;42(4):717–723. [DOI] [PubMed] [Google Scholar]
- 52. Lenhart S. Gender discrimination: a health and career development problem for women physicians. J Am Med Womens Assoc (1972). 1993;48(5):155–159. [PubMed] [Google Scholar]
- 53. Dougherty D, Chen X, Gray DT, Simon AE.. Child and adolescent health care quality and disparities: are we making progress? Acad Pediatr. 2014;14(2):137–148. [DOI] [PubMed] [Google Scholar]
- 54. Ruiz-Cantero M-T, Blasco-Blasco M, Chilet-Rosell E, Peiró A-M.. Gender bias in therapeutic effort: from research to health care. Farm Hosp. 2020;44(3):109–113. [DOI] [PubMed] [Google Scholar]
- 55. Jiao K, Liu M, Xu M.. Age and cohort trajectories of gender inequality in health among elderly people in China. J Women Aging. 2021;33(3):247–267. [DOI] [PubMed] [Google Scholar]
- 56. Nuri NN, Sarker M, Ahmed HU, et al. Overall care-seeking pattern and gender disparity at a specialized mental hospital in Bangladesh. Mater Sociomed. 2019;31(1):35–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mondal B, Dubey JD.. Gender discrimination in health-care expenditure: an analysis across the age-groups with special focus on the elderly. Soc Sci Med. 2020;258:113089. [DOI] [PubMed] [Google Scholar]
- 58. Hinton L, Zweifach M, Tang L, Unützer J, Oishi S.. Gender disparities in the treatment of late-life depression: qualitative and quantitative findings from the IMPACT trial. Am J Geriatr Psychiatry. 2006;14(10):884–892. [DOI] [PubMed] [Google Scholar]
- 59. TheWorld Bank. GDP per capita (current US$) - Bhutan, Singapore. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?end=2019&locations=BT-SG&start=1960. Published 2022 Accessed April, 2022.
- 60. Chong SA. Mental healthcare in Singapore. Int Psychiatry. 2007;4(4):88–90. [PMC free article] [PubMed] [Google Scholar]
- 61. Ho RC, Ho CS, Khan N, Kua EH.. An overview of mental health legislation in Singapore. BJPsych Int. 2015;12(2):42–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chong S-A. Mental health in Singapore: a quiet revolution? Ann Acad Med Singap. 2007;36(10):795–796. [PubMed] [Google Scholar]
- 63. Pelzang R. Mental health care in Bhutan: policy and issues. WHO South East Asia J Public Health. 2012;1(3):339–346. [DOI] [PubMed] [Google Scholar]
- 64. Gorgani F, Esfahani Z, Ghamari SH, et al. Global, regional, and national burden and quality of care index of liver cirrhosis by cause from global burden of disease 1990-2019. J Gastroenterol Hepatol. 2022;38:119–128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.