Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s11695-024-07422-y.
Keywords: Bariatic surgery, Obesity in the elderly, Cardiovascular disease, Heart failure, Echocardiography
Obesity is one of the most important causes of cardiovascular (CV) disease, mainly heart failure (HF) with a preserved ejection fraction (HFpEF). In particular, patients aged ≥ 50 years with severe obesity are at increased risk for the development of HFpEF. [1] In individuals with severe obesity, bariatric surgery was associated with a reduced risk for the development of CV disease, in particular HF. [2] However, especially individuals aged ≥ 50 years with severe obesity may already have profound subclinical myocardial abnormalities. N-terminal probrain natriuretic peptide (NT-proBNP) is a sensitive marker to detect CV disease. [3] It has been suggested that NT-proBNP also can have clinical relevance as a preoperative screening tool in patients aged ≥ 50 years referred for bariatric surgery. [4] While the number of individuals that is referred for bariatric surgery is increasing, [5] the prevalence of echocardiographic abnormalities in these obese patients remain under represented in the literature. Therefore, the present study investigates the echocardiographic characteristics of individuals aged ≥ 50 years with severe obesity and elevated NT-proBNP levels who were referred for bariatric surgery. In particular, we assess the presence of echocardiographic abnormalities related to HFpEF.
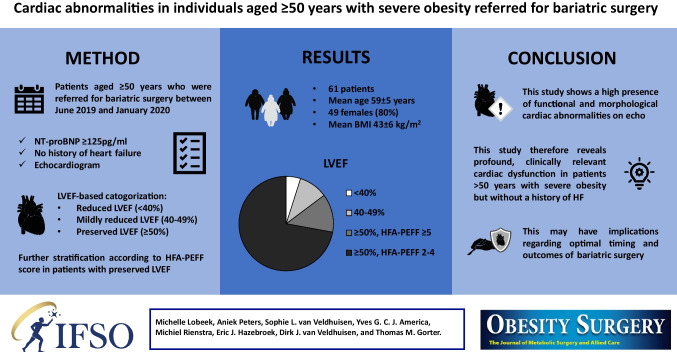
This study is an echocardiographic substudy of an earlier prospective study. [4] Consecutive patients who were referred to the Department of Bariatric Surgery of the Rijnstate Hospital (Arnhem, The Netherlands) between June 2019 and January 2020 were included. Patients aged ≥ 50 years, with NT-proBNP ≥ 125 pg/ml, without a history of HF, meeting the International Federation for the Surgery of Obesity and Metabolic Disorders criteria (i.e. body mass index (BMI) ≥ 35 kg/m2 with an obesity-related co-morbidity or BMI ≥ 40 kg/m2), and who underwent an echocardiogram due to elevated NT-proBNP levels were included. The study was approved by the Local Ethics Committee. Informed consent was obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
All echocardiographic analyses were performed according to recommendations of the American Society of Echocardiography and are described in detail in the Supplementary Material. [6] Recommended cutoff values for abnormality of each individual echocardiographic measure were used. [6] Patients were categorized based on their left ventricular (LV) ejection fraction (LVEF) into: i) reduced (< 40%), ii) mildly reduced (40–49%), and iii) preserved (≥ 50%) LVEF. Patients with a preserved LVEF were further stratified according to the HFA-PEFF (Heart Failure Association – Pretest Assessment, Echocardiographic and Natriuretic Peptide Score, Functional Testing, Final Etiology) diagnostic algorithm and HFA-PEFF scores for each individual were subsequently calculated. [7].
In total, 61 patients were included. Mean age was 59 ± 5 years, 49 (80%) were female, mean BMI was 43 ± 6 kg/m2 and median NT-proBNP was 222 [144–343] pg/ml. Forty-one patients (67%) had hypertension, 5 (8%) had coronary artery disease, 15 (21%) had a history of atrial fibrillation and 15 patients (25%) had type 2 diabetes. Table 1 depicts the echocardiography characteristics of the study population. 26% of the patients had concentric LV remodelling with an increased relative wall thickness. Respectively 39% and 52% of patients had LV diastolic dysfunction, evidenced by a reduced septal and lateral e’. In total, 29% had an increased left atrial volume index, 52% had a reduced LV global longitudinal strain, 52% had an elevated E/e’ and one patient (2%) had increased LV filling pressure with E/e’ > 15. Three patients (5%) had a reduced LVEF, six patients (10%) had a mildly-reduced LVEF and 52 patients (85%) had a preserved LVEF. In the 52 patients with a preserved LVEF, eight patients (15%) had a HFA-PEFF score ≥ 5 points, thus meeting the definite criteria for HFpEF diagnosis. Additionally, 44 patients (85%) had a HFA-PEFF score of 2 to 4 points, suggesting a potential HFpEF diagnosis. Of the 52 patients with a preserved LVEF, 17 (33%) did not have complete data to sum all echocardiographic items of the HFA-PEFF score. Despite this limitation, nine of these patients already had a HFA-PEFF score of 3 or 4 points based on incomplete echocardiographic data.
Table 1.
Echocardiographic characteristics of the study population
| Mean value | N with abnormal value in all patients (n = 61) | N with abnormal value in patients with LVEF ≥ 50% (n = 52) | |
|---|---|---|---|
| LV ejection fraction, % (n = 61) | 58 ± 11 | 9 (15%) | - |
| LV mass index, g/m2 (n = 58) | 73.8 ± 16.5 | 5 (9%) | 5 (9%) |
| Relative wall thickness (n = 53) | 0.41 ± 0.17 | 14 (26%) | 11 (21%) |
| Septal e’, cm/s (n = 61) | 7.5 [6.5–8.9] | 24 (39%) | 21 (34%) |
| Lateral e’, cm/s (n = 60) | 9.9 [8.3–11.2] | 31 (52%) | 27 (45%) |
| E/e’ (n = 60) | 9.1 ± 2.4 |
30 (50%)a 1 (2%)b |
25 (42%)a 1 (2%)b |
| LA volume index, ml/m2 (n = 54) | 26.7 [22.0–31.0] |
11 (20%)c 5 (9%)d |
8 (15%)c 5 (9%)d |
| LV GLS, % (n = 48) | -16.0 [-18.4–4.0] | 25 (52%) | 19 (40%) |
| TR regurgitation velocity, m/s (n = 12) | 2.4 ± 0.1 | 1 (8%) | 1 (8%) |
Data are presented as mean ± standard deviation, median [interquartile range] or numbers (percentages). GLS global longitudinal strain
LA left atrial, LV left ventricular, TR tricuspid regurgitation
aE/e’ 9–14
bE/e’ ≥ 15
cLA volume 29–34 ml/m2
dLA volume ≥ 34 ml/m2
In summary, this study showed that a significant number of patients aged ≥ 50 years with severe obesity, who were free of HF, already had profound, cardiac dysfunction mostly related to concentric LV remodelling, LV diastolic dysfunction and reduced LV longitudinal strain. Moreover, this study demonstrated that 15% of the patients already met the HFA-PEFF score criteria, fulfilling the diagnosis of HFpEF. Since HFA-PEFF scores could not be calculated completely in all individuals, the number of patients with echocardiographic abnormalities complying with the diagnosis of HFpEF may even be underestimated in this study. Of note, this was a cross-sectional study without a control group and it was only performed in individuals who were referred for bariatric surgery, which limits generalizability. Nevertheless, this study reveals clinically relevant functional and morphological echocardiographic abnormalities in a substantial number of patients aged ≥ 50 years with severe obesity who were referred for bariatric surgery, but without a history of clinical HF. Further study is needed to investigate whether these findings will have clinical implications regarding the optimal timing of bariatric surgery or in predicting early and late postoperative outcomes.
Supplementary Information
Below is the link to the electronic supplementary material.
Data Availability
The data that support the findings of this study are available from the corresponding author, T.M.G., upon reasonable request.
Declarations
Conflict of Interest
No conflict of interest.
Footnotes
Key points
• Bariatric surgery is increasingly performed in individuals with severe obesity.
• Obese patients of ≥ 50 years without heart failure had profound cardiac dysfunction.
• These abnormalities often meet with a diagnosis of heart failure.
• These insights may help the optimal timing of bariatric surgery.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Michelle Lobeek and Aniek Peters contributed equally to this work.
References
- 1.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and Cardiovascular Disease A Scientific Statement From the American Heart Association. Circulation. 2021;143:E984-1010. 10.1161/CIR.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Veldhuisen SL, Gorter TM, Woerden G, et al. Bariatric surgery and cardiovascular disease: a systematic review and meta-analysis. Eur Heart J. 2022;43:1955–69. 10.1093/eurheartj/ehac071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linssen GCM, Bakker SJL, Voors AA, et al. N-terminal pro-B-type natriuretic peptide is an independent predictor of cardiovascular morbidity and mortality in the general population. Eur Heart J. 2010;31:120–7. 10.1093/eurheartj/ehp420 [DOI] [PubMed] [Google Scholar]
- 4.Van Veldhuisen SL, van Woerden G, Hemels MEW, et al. Preoperative cardiac screening using NT-proBNP in obese patients 50 years and older undergoing bariatric surgery: a study of 310 consecutive patients. Surg Obes Relat Dis. 2021;17:64–71. 10.1016/j.soard.2020.08.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mentias A, Aminian A, Youssef D, et al. Long-Term Cardiovascular Outcomes After Bariatric Surgery in the Medicare Population. J Am Coll Cardiol. 2022;79:1429–37. 10.1016/j.jacc.2022.01.047 [DOI] [PubMed] [Google Scholar]
- 6.Lang RM, Badano LP, Victor MA, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1-39.e14. 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 7.Pieske B, Tschöpe C, Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: The HFA-PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019;40:3297–317. 10.1093/eurheartj/ehz641 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, T.M.G., upon reasonable request.