Abstract
We examined patterns of longitudinal trajectories of loneliness during the COVID-19 pandemic using six time points (January 2020 [pre-pandemic] to March/April 2021) and whether trajectories were associated with psychological distress (depression/anxiety) and substance use (alcohol/cannabis) outcomes in Spring 2021. Participants were 644 young adults who completed online assessments. Outcomes were regressed on most-likely loneliness trajectory adjusting for pre-pandemic measures. Three loneliness trajectories varied from consistently lower to consistently higher. Pre-pandemic social support was associated with lower odds of a higher loneliness trajectory. Higher loneliness trajectories were associated with greater odds of past-month cannabis use compared to Low trajectories, but not significantly associated with depression, anxiety, or alcohol use in Spring 2021. Interventions addressing co-occurring loneliness and cannabis use are needed.
Loneliness, or perceived social isolation, is characterized as “the social equivalent of physical pain, hunger, and thirst” and is conceptualized as a distressing feeling that arises when an individual perceives their social needs, or the quality of their relationships, are not met (Hawkley & Cacioppo, 2010). Loneliness is a public health concern and is associated with significant negative physical and mental health outcomes, including physical health impairment and risk of mortality (Holt-Lunstad et al., 2015), and major depressive episodes (Cacioppo et al., 2006; Killgore et al., 2020). Although theory would also suggest relationships between loneliness and substance use, there is little research, particularly longitudinal, on the topic.
As young adults (ages 18–25) are at increased risk for mental health symptoms, increased levels of loneliness, and the highest rates of alcohol and cannabis misuse (Substance Abuse and Mental Health Services Administration (SAMHSA, 2021), understanding patterns of loneliness during the COVID-19 pandemic in relation to later mental health and substance use could clarify how loneliness may impact well-being and inform future prevention and intervention efforts during public health crises and other high risk historical periods of stress marked by limited social interaction. The current study aimed to examine trajectories of loneliness during the COVID-19 pandemic (assessed from January 2020 through March/April 2021) and associations with mental health and alcohol and cannabis use in spring 2021.
Loneliness and psychological distress during the COVID-19 pandemic
There have been increasing concerns about the psychological and emotional well-being among young adults as prevalence of mental health conditions, including major depressive disorder and generalized anxiety disorder, have risen sharply over the past decade (SAMHSA, 2021). Concerns have been heightened more recently as studies suggest mental health symptoms have risen more sharply from 2019–2021 as the pandemic has unfolded. One national study found in fall 2019 (pre-pandemic) that 10.8% of adults ages 18 and older in the sample reported symptoms of depression or anxiety; however in February 2021, the prevalence increased to 41.5% (Vahratian, Blumberg, Terlizzi, & Schiller, 2021). Further, other national data show that throughout the pandemic (i.e., April 2020 through January 2022), young adults have consistently reported the highest levels of depression and anxiety symptoms compared to any other age group (Centers for Disease Control and Prevention, 2022) with nearly half of young adults reporting symptoms of depression or anxiety in a given week, ranging from 43.9% (June 2021) to 58.7% (November 2020). Other studies also elevated symptoms of depression and anxiety among young adults in Spring/Summer 2020 (Hawes, Szenczy, Olino, Nelson, & Klein, 2021). A recent Advisory from the U.S. Surgeon General (2021) reported rapidly increasing rates of psychological distress among young adults, with a 40% increase in persistent feelings of sadness or hopeless from 2009 to 2019. The Advisory called for an urgent public health need to support the mental health of young adults, especially during the pandemic.
Loneliness has been examined during the pandemic, with most findings showing increases in loneliness. A systematic review examined 13 longitudinal studies where the prevalence of loneliness was assessed pre-pandemic and during the pandemic (Buecker & Horstmann, 2021). Nearly all studies, including work from our team (Lee, Cadigan, & Rhew, 2020) reported increases in the trajectory of loneliness from pre-pandemic to during the pandemic, although two studies with adult populations reported stable trends. Daily level assessment of loneliness during the initial phase of the pandemic (March/April 2020) found a temporary increase in loneliness among German residents, followed by a decrease to pre-pandemic levels (Buecker et al., 2020), suggesting daily level feelings of loneliness may be temporary. One study with adults from the UK examined trajectories of loneliness during the early phase of the pandemic (from March 2020 to May 2020), finding classes ranging from low to high levels of loneliness (Bu, Steptoe, & Fancourt, 2020).
Young adults may be at an especially increased risk of loneliness during the pandemic, as this age cohort shows the highest loneliness levels compared to any other age group (Luchetti et al., 2020; McGinty et al., 2020). Higher levels of loneliness are associated with depressive symptoms and suicidal ideation (Killgore et al., 2020). During the pandemic, there has been a perceived reduction in the quality of social relationships (Buecker & Horstmann, 2021) and college students with less social support and less sense of connectedness to their peer groups report greater symptoms of depression (Graupensperger, Benson, Kilmer, & Evans, 2020), putting individuals further at risk for loneliness and co-occurring negative mental health symptoms during this time.
Loneliness and substance use
The association between loneliness and substance use is inconsistent, and differences may be dependent on type of substance used. Some studies show positive associations between loneliness and substance use (Ingram et al., 2020; Stickley et al., 2014), including the finding those who have substance use problems are seven times more likely to report loneliness than those in the general population (Ingram, Kelly, Deane, Baker & Raftery, 2018). Substance use may be used as a method of coping with, or avoiding, negative affective states (Kuntsche, Knibbe, Gmel, & Engels, 2005), including feelings of loneliness.
Although not entirely consistent, studies, most of which have been cross-sectional, suggest that loneliness may be associated with adolescent and young adult alcohol use (Bonin, McCreary, & Sadava, 2000; McKay, Konowalczyk, Andretta, & Cole, 2017), although other studies suggest a negative association between alcohol use and loneliness (Diehl et al., 2018; McBroom, Fife, & Nelson, 2008) as greater alcohol is consumed when individuals feel less lonely. Research also suggests that loneliness is associated with cannabis use (Holmes, Popova, & Ling, 2016; Rhew, Cadigan & Lee, 2021). However, there may be differences in loneliness depending on type of substance use (i.e., alcohol or cannabis) (Cacioppo et al., 2000). Rhew, Cadigan, and Lee (2021) found greater frequency of cannabis use, especially daily cannabis use, was associated with higher levels of loneliness and higher levels of depression and anxiety; however, alcohol use frequency was not associated with loneliness. Given this as well as the fact that the vast majority of studies of loneliness and substance use have been cross-sectional, longitudinal studies that assess both alcohol and cannabis would be important in bringing greater clarity into the role of loneliness in different forms of substance use.
Loneliness and substance use during COVID-19 pandemic
Alcohol and cannabis use are common among young adults, with national surveys indicating 82% have used alcohol and 42% have used cannabis in the past year (Schulenberg et al., 2021). Patterns of young adults’ alcohol use during the pandemic (January 2020 to April/May 2020) show an increase in alcohol use frequency, but decrease in per day drinking consumption, with no changes in cannabis use (Graupensperger et al., 2021). Other studies have shown greater COVID-related distress associated with increased alcohol consumption (Rodriguez et al., 2020), especially among those with social/relationship stressors (Graupensperger, Cadigan, Einberger, & Lee, 2021).
During the pandemic, impacts of social interaction and loneliness on alcohol use have been examined. Bartel et al (2021) observed in a sample of Canadian young adults that self-isolation due to the pandemic was associated with greater quantity and frequency of cannabis use, adjusting for pre-pandemic levels of use. Bragard and colleagues (2021) found that among those with less face-to-face interaction, more feelings of loneliness were associated with greater alcohol consumption during the pandemic. But, among those with more face-to-face interaction, they found that loneliness was associated with less alcohol consumption, suggesting that individuals may be less lonely when surrounded by others and not rely on alcohol use. However, less is known about the relationship between loneliness and cannabis use, and the trajectories of loneliness throughout the pandemic in relation to substance use.
Consistent with Cacioppo and colleagues’ Theory of Loneliness, lonely individuals tend to perceive the world as more threatening, expect more negative social interactions, and have greater mistrust and higher levels of self-blame (Cacioppo, Cacioppo, & Boomsma, 2014; Hawkley & Cacioppo, 2010). Subsequently, they experience more negative affect and can further isolate from others, which can serve to maintain and exacerbate loneliness. Affective-motivational and affect-regulation theories assert some young adults use substances to cope with negative affect and psychological distress (e.g., depression, anxiety), a finding which has been supported by daily-level studies showing associations between negative affect and coping motives for substance use (Arbeau et al., 2011; Park, et al., 2004). Therefore, young adults who are lonely may engage in substance use (particularly cannabis) to cope with feelings of negative affect and loneliness.
Present Study
The present study examined patterns of longitudinal trajectories of loneliness during 2020 and into 2021, incorporating six time points including pre-pandemic (January 2020), early acute pandemic period in Spring 2020 (April 2020), and in September/October 2020, November/December 2020, January/February 2021, and March/April 2021, and whether loneliness trajectory classes were associated with psychological distress and substance use the Spring of 2021 (March/April 2021). As prior work has found sharper increases in loneliness throughout the pandemic among those who had greater levels of perceived social support before the pandemic (Lee, Cadigan, & Rhew, 2020), in addition to differences based on gender, LGBTQ status, and race with regards to levels of both loneliness and substance use (Bonin, McCreary, & Sadava, 2000; Evans et al., 2017; Lee, Cadigan, & Rhew, 2020; Schuler & Collins, 2020), we also explored how demographic factors and social support were associated with trajectories of loneliness.
Our aims were to examine: 1) What are the trajectories of loneliness during the Covid-19 pandemic? 2) What demographic factors (student status; gender; age; race; LGBTQ status) and baseline social support are associated with trajectories of loneliness? 3) How are trajectories of loneliness associated with psychological distress (i.e., depressive and anxiety symptoms) and substance use (i.e., alcohol and cannabis use) approximately one year after the start of the physical distancing mandates in the United States (in March/April 2021)? Consistent with prior research examining trajectories of loneliness, we hypothesized that trajectories of loneliness would vary, with some experiencing higher levels of loneliness and a return to baseline level and other reporting more moderate levels throughout the pandemic. Consistent with theories of affect-motivation, affect-regulation, and prior research, we generally hypothesized that higher patterns of loneliness would be associated with greater psychological distress and greater cannabis, but not alcohol, use.
Method
Procedures and Participants
Participants were originally from a community sample of young adults enrolled in a longitudinal study on social role transitions and alcohol use in Seattle, WA. Study recruitment occurred during 2015–2016 mainly via social media, newspaper, and community advertisements. To be eligible for the study, participants must have been between 18 and 23 years old at screening, reporting alcohol use in the past year, living within 60 miles of study offices, and available to attend an in-person identification verification and consent study visit (see Patrick et al., 2018 for complete procedures of the original study). As part of the original study procedures, participants completed a baseline survey, 24 consecutive months of online surveys, and a final online survey 30 months post-baseline (completed between August 2017–July 2018, depending on the enrollment date). More recently, 767 participants (out of 778 who were originally enrolled) were invited to complete supplemental online assessments in January 2020 and then in April/May 2020. With additional supplemental funding, additional assessment points were conducted between September/October 2020 and March/April 2021, occurring bimonthly. Participants were randomly assigned to begin assessments in either September or October 2020. The randomized bi-monthly design was selected to approximate the original data collection design (monthly) of the parent study, but to also maximize the total length of the follow-up period to study impacts of the pandemic up to one year after first assessment and to have adequate power for study aims and to be able to have continuous coverage of months in the event of rapid changes in COVID-19 pandemic responses and policies. Data for this study were from the January 2020 (N = 594), April/May 2020 (N = 552), September/October 2020 (N = 565), November/December 2020 (N = 500), January/February 2021 (N = 475), and March/April 2021 (N = 469) assessments. Participants were compensated $15 for completion of each survey. Completion rates were 77.4% in January 2020 (conducted on January 6–30 to get updated contact information, current social role statuses, substance use, and mental health) and 72.0% in April/May 2020 (conducted on April 21-May 18 to get an update during the COVID-19 pandemic). Completion rates for the bimonthly surveys were as follows: September/October 2020 (73.7%), November/December 2020 (65.2%), January/February 2021 (61.9%), and March/April 2021 (61.1%).
A total of 644 young adults (mean age = 25.57 [standard deviation = 1.81]; 61.0% female; 30.1% LBGTQ; 54.4% white non-Hispanic, 18.2% Asian non-Hispanic) were included in the present analyses. The institutional review board of the University of Washington approved the human subjects research, and information statements with all elements of consent were included at the beginning of the January and April/May and September/October surveys.
Measures
Loneliness.
Loneliness was assessed at six time points (January 2020, April/May 2020, September/October 2020, November/December 2020, January/February 2021, and March/April 2021) using the Three-Item Loneliness Scale (Hughes et al., 2004), which is a short version of the Revised UCLA Loneliness Scale (R-UCLA; Russell et al., 1980). Participants completed three items asking how often they felt “that they lacked companionship,” “left out,” or “isolated from others.” Response options were “hardly ever” (1), “some of the time” (2), and “often” (3). Responses from each item were summed to create a total score that ranged from 3 to 9. Internal consistency in this study sample was high (α ≥ .78 at all time points).
Depression Symptoms.
Depression severity was assessed in March/April 2021 using the 8-item version of the Patient Health Questionnaire (PHQ-8; Kroenke et al., 2009). Participants were asked “how often have you been bothered by any of the following problems?” regarding the previous month (February or March 2021) and then responded to eight items containing symptoms of depression. Response options ranged from “not at all” (0) to “nearly every day” (3). The eight items were summed to create a total score ranging from 0 to 24. The PHQ has shown strong criterion validity when compared against clinical diagnosis of depressive disorders in a wide range of study populations. The internal consistency of the scale was high in the sample (α = .90). The two-item version of the PHQ consisting of the first two questions of the full PHQ (“Little interest or pleasure in doing things; “Feeling down, depressed or hopeless”) (PHQ-2; Kroenke et al., 2003) was given in January 2020. Responses for the two items were summed to create total scores ranging from 0 to 6. This short version of the PHQ was included in models predicting PHQ-8 scores to control for pre-pandemic levels of depression severity. The full PHQ-8 and the brief PHQ-2 were strongly correlated (τ = 0.77, p < .01 in March/April 2021).
Anxiety Symptoms.
Anxiety severity was assessed in March/April 2021 using the Generalized Anxiety Disorder Screener (GAD-7; Löwe et al., 2008; Spitzer et al., 2006). Similar to the PHQ, participants were asked “how often have you been bothered by any of the following problems?” regarding the previous month (February or March 2021) and then responded to seven items containing symptoms of anxiety. Response options similarly ranged from “not at all” (0) to “nearly every day” (3). The seven items were summed to create a total score ranging from 0 to 21. The GAD-7 has been well-validated against clinician-based diagnoses of generalized anxiety. In this study, Cronbach’s alpha was .93. The two-item version of the GAD consisting of the first two items of the full GAD-7 (“Feeling nervous, anxious or on edge”; Not being able to stop or control worrying”) (GAD-2; Kroenke et al., 2007) was given in January 2020. Responses for the two items were summed to create a total score ranging from 0 to 6. This short version of the GAD was included in models predicting GAD-7 scores to control for pre-pandemic levels of anxiety severity. The full GAD-7 and the brief GAD-2 were strongly correlated (τ = 0.83, p < .01 in March/April 2021).
Alcohol Use.
Two indices of past-month alcohol use were assessed in January 2020 and in March/April 2021: typical number of drinking days per week and any binge drinking (4+/5+ drinks within a two-hour period). Typical number of drinking days per week was assessed using the Daily Drinking Questionnaire (DDQ; Collins et al., 1985), which asks participants to report the number of drinks they typically consume on each day of the week. The DDQ was asked in reference to the previous month. Participants also completed an item asking how often they had 4+/5+ drinks (women/men) containing alcohol within a two-hour period, with response options ranging from “never” (0) to “every day” (7) (NIAAA, 2003). Responses were dichotomized to reflect any past-month binge drinking (1; responses of “once a month” to “every day”) and no past-month binge drinking (0; “never”).
Cannabis Use.
Cannabis use was assessed in January 2020 and in March/April 2021 with a single item asking, “In the past 30 days, how many days did you use marijuana?” Participants entered the number of days in a free-response text box. Similar to binge drinking, this variable was dichotomized to reflect any (1) and no (0) past-month cannabis use.
Perceived Social Support.
Perceived social support was assessed in January 2020 using the Multidimensional Scale of Perceived Social Support (Zimet et al., 1988). Participants responded to 12 statements about their perceived social support with response options ranging from “very strongly disagree” (1) to “very strongly agree” (7). Responses from all items were averaged to create a total score that ranged from 1 to 7. Internal consistency in this sample was high (α = .91).
Student Status.
In January 2020, participants were asked, “What is your educational status?” Response options were “High school student,” “General Education Development (GED) student,” “Trade or vocational student,” “2-year or community college student,” “4-year college or university student,” “Graduate or professional school student,” “Other certifications or coursework,” and “I am currently not a student.” A binary indicator variable was created based on participants’ responses to this item to differentiate between participants who were and were not 4-year college students. Participants who selected “4-year college or university student” were coded as 0, and all other participants (i.e., those who were not currently 4-year students) were coded as 1.
Plan of Analysis
To identify classes of latent trajectories of loneliness during the COVID-19 pandemic and to investigate whether membership in these latent trajectory classes was associated with (1) demographic covariates and perceived social support before the pandemic and (2) substance use and psychological distress distal outcomes in March and April of 2021, the classify-analyze approach was used (Bray, Lanza, & Tan, 2015). This approach involved three stages of analysis. First, latent loneliness trajectory classes were identified using six measurements of loneliness from January 2020 (pre-pandemic) to March and April of 2021 using growth mixture models. Growth mixture models allow for unobserved groups (often called classes) with different growth trajectories to be identified, rather than estimating a single average growth trajectory or estimating different trajectories in observed groups (e.g., a multi-group growth model) (Grimm, Ram, & Estabrook, 2017). This is achieved by incorporating a categorical latent variable into a growth model. These models estimate growth parameters (intercepts and slopes) for each latent class and provide posterior estimates of the probability that each individual belongs to each latent class. Second, based on these posterior probabilities, participants were assigned to their most-likely latent loneliness trajectory class (i.e., the class they had the highest probability of belonging to), and then class membership was regressed on pre-pandemic measurements of the demographic covariates and perceived social support (Bray et al., 2015). Third, substance use and psychological distress distal outcomes, measured in March and April of 2021, were regressed on the most-likely loneliness trajectory class variable with pre-pandemic measurements of each distal outcome and the demographic covariates included as covariates.
For the first stage, a “one-class” latent growth curve model and two- through five-class growth mixture models were run in Mplus (Version 8; Muthén & Muthén, 2017) to identify distinct trajectories of loneliness during the pandemic. The time metric was months (since January 2020), and time was coded as follows: January 2020 (0), April/May 2020 (4), September/October 2020 (8.5), November/December 2020 (10.5), January/February 2021 (12.5), and March/April 2021 (14.5). Intercepts, linear slopes, and quadratic slopes were estimated for each latent class. Models were estimated using maximum likelihood estimation with robust standard errors. This estimation technique can accommodate missing data in outcome (i.e., endogenous) variables and will generally provide unbiased parameter estimates under the assumption that data are missing at random (Grimm et al., 2017). The optimal number of classes was determined by comparing several fit indices (i.e., AIC, BIC, sample-size adjusted BIC, entropy, Vuong-Lo-Mendell-Rubin likelihood ratio test [LRT], Lo-Mendell-Rubin LRT, and the bootstrap LRT), inspecting descriptive statistics, and evaluating the substantive meaning of the latent trajectories across models (Grimm et al., 2017).
For the second stage, individuals were assigned to their most-likely loneliness trajectory class according to posterior probabilities of membership based on the best-fitting growth mixture model. The categorical latent trajectory variable was then regressed on pre-pandemic (January 2020) measurements of the demographic covariates (i.e., sex, age, race/ethnicity, sexual orientation, and student status) and perceived social support using multinomial logistic regression in the nnet package (Venables & Ripley, 2002) of R 4.2.1 (R Core Team, 2022). To enable all comparisons among loneliness trajectories to be made, two models were estimated for each outcome: one with the low loneliness trajectory as the reference group and one with the moderate loneliness trajectory as the reference group.
For the third stage, in separate models, the substance use and psychological distress distal outcomes from March and April of 2021 were regressed on indicator variables for latent trajectory classes using binomial logistic and negative binomial regression in the stats (R Core Team, 2020) and MASS (Venables & Ripley, 2002) packages, respectively, in R. Pre-pandemic (i.e., January 2020) measurements of the distal outcomes and the demographic variables used in the previous stage were included as covariates. Thus, these models assessed whether proportional change in substance use and psychological distress during the pandemic was predicted by individuals’ most-likely latent loneliness trajectory. As with the second stage, two models were estimated for each outcome: one with the low loneliness trajectory as the reference group and one with the moderate loneliness trajectory as the reference group.
Multiple imputation performed in the MICE package (van Buuren & Groothuis-Oudshoorn, 2011) was used to account for missing data in outcomes assessed in March and April of 2021 and in baseline covariates assessed in January 2020. Multiple imputation is expected to produce unbiased estimates when data are missing at random. Five-hundred imputed datasets were created, and all variables included in the regressions in the third stage of analysis were included as covariates in the imputation model. Summary parameters and standard errors were estimated based on Rubin’s Rules, which account for uncertainty between and within imputed datasets (Rubin, 2014).
Results
Identification of Latent Loneliness Trajectory Classes
Table 1 shows the distribution of the loneliness indicators across the survey waves, demographic covariates, perceived social support, and distal outcomes. Class sizes and fit indices for the two- through four-class loneliness growth mixture models are provided in Table 2. The five-class model did not converge and was not included in Table 2. Based on the fit indices and substantive evaluation of the size and meaningfulness of the latent trajectory classes, the 3-class model was selected. Intercept and slope estimates for the three latent loneliness trajectory classes are presented in Table 3, and the trajectories are depicted visually in Figure 1. Approximately 39% of participants were assigned to the “low” latent loneliness trajectory as their most-likely trajectory. These participants had average loneliness scores of 3.54 in January 2020, prior to the onset of the pandemic, and their loneliness scores increased linearly by 0.20 units per month (linear slope) and decelerated at a rate of 0.01 units per month squared (quadratic slope). This resulted in a curvilinear loneliness trajectory that was consistently low but increased during the early months of the pandemic. Approximately 47% of participants were assigned to the “moderate” latent loneliness trajectory as their most-likely trajectory. These participants had average loneliness scores of 5.80 in January 2020 that did not change significantly across the 15-month study period. Approximately 14% of participants were assigned to the “high” latent loneliness trajectory as their most-likely latent trajectory. These participants had average loneliness scores of 8.55 in January 2020, and their loneliness scores decreased linearly by 0.24 units per month and accelerated at a rate of 0.01 units per month squared. This resulted in a curvilinear loneliness trajectory that was consistently very high but decreased during the early months of the pandemic.
Table 1.
Descriptive Statistics for the Loneliness Indicators, Demographic Covariates, Perceived Social Support, and Distal Outcomes
| Loneliness Indicators | |||||
|---|---|---|---|---|---|
| Month/Year | Time Metric | n | M (SD) | Median | Range |
| January 2020 | 0 | 578 | 5.26 (1.84) | 5 | 3–9 |
| April/May 2020 | 4 | 547 | 5.53 (1.89) | 6 | 3–9 |
| September/October 2020 | 8.5 | 540 | 5.56 (1.88) | 5.5 | 3–9 |
| November/December 2020 | 10.5 | 482 | 5.58 (1.82) | 6 | 3–9 |
| January/February 2021 | 12.5 | 460 | 5.59 (1.81) | 6 | 3–9 |
| March/April 2021 | 14.5 | 543 | 5.62 (1.86) | 6 | 3–9 |
| Covariates (January 2020) | M (SD) or % | Range |
|---|---|---|
| Male sex | 40.2% | 0–1 |
| Age in years | 25.57 (1.81) | 22.03–28.89 |
| Race/ethnicity | ||
| Asian Non-Hispanic (NH) | 18.2% | 0–1 |
| Other NH | 18.9% | 0–1 |
| Hispanic | 8.2% | 0–1 |
| White NH | 54.4% | 0–1 |
| Non-4-year college student status | 68.6% | 0–1 |
| LGBTQ status | 30.1% | 0–1 |
| Perceived social support | 5.33 (1.15) | 1–7 |
| Distal Outcomes (March/April 2021) | M (SD) or % | Range |
| Typical drinking days per week | 1.67 (1.92) | 0–7 |
| Any past-month binge drinking | 28.2% | 0–1 |
| Any past-month cannabis use | 30.6% | 0–1 |
| Depression severity (PHQ-8) | 6.88 (5.66) | 0–24 |
| % with depressive symptoms | 25.2% | - |
| Anxiety severity (GAD-7) | 5.82 (5.44) | 0–21 |
| % with anxiety symptoms | 20.2% | - |
Note. N = 644. PHQ-8 = Patient Health Questionnaire-8; GAD-7 = Generalized Anxiety Disorder Screener; % with depressive/anxiety symptoms = PHQ-8 ≥ 10; GAD-7 ≥ 10.
Table 2.
Fit Statistics and Class Proportions for a “One-Class” Latent Curve Model and 2- through 4-Class Growth Mixture Models
| Latent Curve Model | Growth Mixture Models | |||
|---|---|---|---|---|
| Fit Statistic | One-Class | Two-Classes | Three-Classes | Four-Classes |
| AIC | 10,746 | 10,700 | 10,571 | 10,552 |
| BIC | 10,813 | 10,785 | 10,674 | 10,673 |
| Adjusted BIC | 10,765 | 10,724 | 10,601 | 10,587 |
| Entropy | - | .66 | .85 | .80 |
| VLMR p-value | - | .05 | < .001 | < .001 |
| LMR p-value | - | .06 | < .001 | < .001 |
| Bootstrap p-value | - | < .001 | < .001 | < .001 |
| Class proportions | 1.00 | .76/.24 | .44/.41/.15 | .37/.31/.18/.15 |
Note. N = 644. AIC = Akaike Information Criterion, BIC = Bayesian Information Criterion, VLMR = Vuong-Lo-Mendell-Rubin Likelihood Ratio Test, LMR = Lo-Mendell-Rubin Likelihood Ratio Test.
Table 3.
Estimates of Growth Parameters from 3-Class Growth Mixture Model
| Estimate | SE | p | |
|---|---|---|---|
| Low Loneliness Trajectory (n = 250) | |||
| Intercept | 3.54 | 0.05 | 0.00 |
| Linear slope | 0.20 | 0.02 | 0.00 |
| Quadratic slope | −0.01 | 0.00 | 0.00 |
| Moderate Loneliness Trajectory (n = 301) | |||
| Intercept | 5.80 | 0.05 | 0.00 |
| Linear slope | 0.01 | 0.03 | 0.72 |
| Quadratic slope | 0.00 | 0.00 | 0.84 |
| High Loneliness Trajectory (n = 93) | |||
| Intercept | 8.55 | 0.07 | 0.00 |
| Linear slope | −0.24 | 0.04 | 0.00 |
| Quadratic slope | 0.01 | 0.00 | 0.00 |
Note. NTotal = 644.
Figure 1.
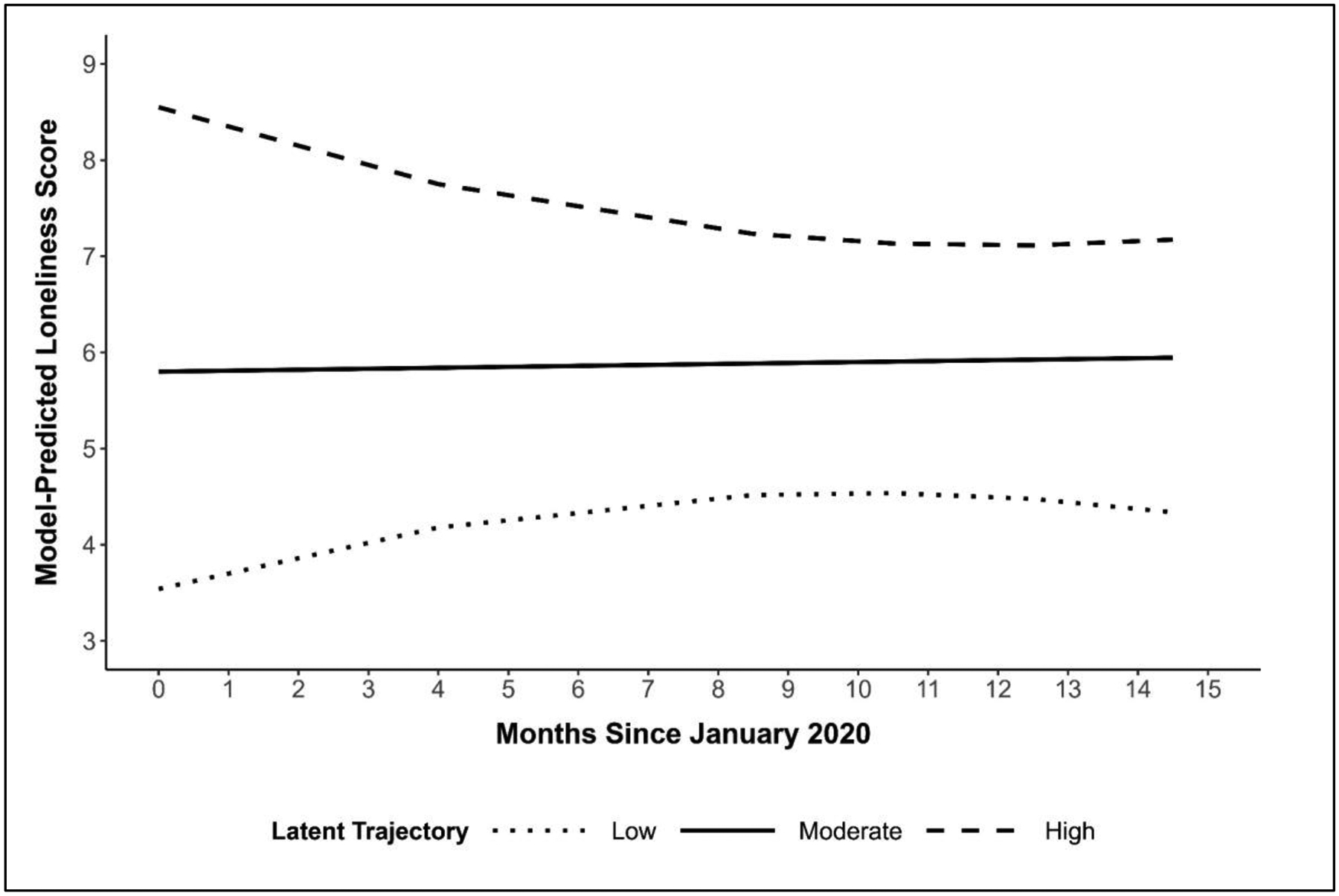
Loneliness latent trajectory classes.
Testing Differences among the Trajectory Classes at Baseline
Table 4 shows the results of a multinomial logistic regression testing whether pre-pandemic measurements of demographic covariates and perceived social support were associated with participants’ most-likely latent loneliness trajectory class. Each one-unit increase in pre-pandemic perceived social support was associated with 47% lower odds of being in the Moderate loneliness trajectory class (Odds Ratio [OR] = .53, 95% CI: .43, .66) and 73% lower odds of being in the High trajectory class (OR = .27, 95% CI: .19, .39) compared to the Low trajectory class. Each one-unit increase in pre-pandemic perceived social support was associated with 50% lower odds of being in the High loneliness trajectory class compared to the Moderate trajectory class (OR = 0.50, 95% CI: 0.37, 0.69). None of the demographic covariates were significantly associated with latent loneliness trajectory class membership.
Table 4.
Multinomial Logistic Regression of the Most Likely Latent Trajectory Variable on Pre-Pandemic Demographic Covariates and Perceived Social Support
| Moderate (vs. Low) | High (vs. Low) | High (vs. Moderate) | |
|---|---|---|---|
| Predictor | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Male sex | 0.88 [0.61, 1.28] | 0.71 [0.40, 1.24] | 0.80 [0.47, 1.35] |
| Age | 1.02 [0.92, 1.13] | 0.99 [0.85, 1.16] | 0.97 [0.84, 1.12] |
| Non-4-year college student | 0.73 [0.48, 1.09] | 1.13 [0.59, 2.17] | 1.56 [0.86, 2.84] |
| LGBTQ | 1.44 [0.94, 2.20] | 1.10 [0.57, 2.12] | 0.76 [0.42, 1.39] |
| Race/ethnicity | |||
| Asian Non-Hispanic (NH) | 0.99 [0.61, 1.62] | 0.84 [0.41, 1.73] | 0.85 [0.44, 1.64] |
| Other NH | 0.76 [0.47, 1.23] | 0.73 [0.36, 1.48] | 0.96 [0.50, 1.85] |
| Hispanic | 1.17 [0.61, 2.23] | 0.44 [0.12, 1.53] | 0.37 [0.12, 1.21] |
| White NH (Reference) | - | - | |
| Perceived social support | 0.53 [0.43, 0.66] | 0.27 [0.19, 0.39] | 0.51 [0.37, 0.69] |
Note. NTotal = 644; nLow = 250, nModerate = 301, nHigh = 93. Bold typeface denotes statistically significant findings (i.e., p < .05). OR = Odds ratio; CI = Confidence interval.
Testing Whether Loneliness Trajectory Classes Predicted Distal Outcomes
Table 5 shows the results of binomial logistic and negative binomial regression models testing whether participants’ most-likely loneliness trajectory class was associated with substance use and psychological distress distal outcomes in March and April of 2021. Prior to adding pre-pandemic (i.e., January 2020) measurements of each distal outcome as covariates, participants assigned to the Moderate and High loneliness trajectory classes tended to have higher depression (PHQ-8) and anxiety (GAD-7) severity scores compared with those in the Low trajectory class. There were no significant differences in depression or anxiety severity scores between participants assigned to the Moderate and High loneliness trajectory classes. Participants assigned to the High loneliness trajectory class had greater odds of past-month cannabis use than those in the Low and Moderate trajectory classes, but there was no significant difference in the odds of past-month cannabis use between those assigned to the Low and Moderate trajectory classes. There were no significant associations between most-likely latent loneliness trajectory class and typical number of drinking days per week or odds of past-month binge drinking.
Table 5.
Negative Binomial and Binomial Logistic Regressions of Distal Outcomes (March/April 2021) on Most Likely Latent Trajectory Variable
| Without Controlling for Pre-Pandemic Measurement of Outcome | |||||
|---|---|---|---|---|---|
| Typical Number of Drinking Days per Week (DDQ) | Any Past-Month Binge Drinking | Any Past-Month Cannabis Use | Depression Severity (PHQ-8) | Anxiety Severity (GAD-7) | |
| Parameter | CR [95% CI] | OR [95% CI] | OR [95% CI] | CR [95% CI] | CR [95% CI] |
| Latent Trajectory | |||||
| Low (Ref.) | - | - | - | - | - |
| Moderate | 1.01 [0.79, 1.28] | 1.46 [0.90, 2.40] | 1.42 [0.86, 2.33] | 1.26 [1.06, 1.49] | 1.32 [1.08, 1.62] |
| High | 1.09 [0.45, 2.65] | 1.12 [0.38, 3.29] | 3.06 [1.41, 6.64] | 1.84 [1.00, 3.40] | 2.13 [1.08, 4.21] |
| Latent Trajectory | |||||
| Low | 0.99 [0.78, 1.26] | 0.68 [0.42, 1.11] | 0.71 [0.43, 1.16] | 0.80 [0.67, 0.94] | 0.76 [0.62, 0.92] |
| Moderate (Ref.) | - | - | - | - | - |
| High | 1.09 [0.45, 2.63] | 0.77 [0.28, 2.10] | 2.16 [1.08, 4.32] | 1.47 [0.81, 2.65] | 1.61 [0.83, 3.11] |
| Controlling for Pre-Pandemic Measurement of Outcome | |||||
| Typical Number of Drinking Days per Week (DDQ) | Any Past-Month Binge Drinking | Any Past-Month Cannabis Use | Depression Severity (PHQ-8) | Anxiety Severity (GAD-7) | |
| Parameter | CR [95% CI] | OR [95% CI] | OR [95% CI] | CR [95% CI] | CR [95% CI] |
| Latent Trajectory | |||||
| Low (Ref.) | - | - | - | - | - |
| Moderate | 0.95 [0.77, 1.19] | 1.37 [0.83, 2.29] | 1.41 [0.80, 2.51] | 1.12 [0.94, 1.32] | 1.19 [0.98, 1.45] |
| High | 1.23 [0.48, 3.12] | 1.11 [0.36, 3.44] | 3.21 [1.26, 8.15] | 1.32 [0.69, 2.52] | 1.53 [0.70, 3.33] |
| Latent Trajectory | |||||
| Low | 1.04 [0.84, 1.30] | 0.73 [0.44, 1.21] | 0.71 [0.40, 1.26] | 0.90 [0.76, 1.06] | 0.84 [0.69, 1.02] |
| Moderate (Ref.) | - | - | - | - | - |
| High | 1.28 [0.51, 3.25] | 0.81 [0.28, 2.36] | 2.27 [0.97, 5.32] | 1.18 [0.64, 2.20] | 1.28 [0.61, 2.70] |
Note. NTotal = 644; nLow = 250, nModerate = 301, nHigh = 93. Bold typeface denotes statistically significant findings (i.e., p < .05). All models control for sex, age, race/ethnicity, college student status, sexual orientation, and perceived social support in January 2020. DDQ = Daily Drinking Questionnaire; PHQ-8 = Patient Health Questionnaire-8; GAD-7 = Generalized Anxiety Disorder Screener; CR = Count ratio; OR = Odds ratio; CI = Confidence interval.
In further models, we controlled for pre-pandemic measurements of the distal outcome variable in each model. Although they remained in the same direction, associations of loneliness with depressive and anxiety symptoms were attenuated and no longer statistically significant. Participants assigned to the High loneliness trajectory class had over 3 times greater odds of past-month cannabis use (OR = 3.21; 95% CI: 1.26, 8.15) compared to those assigned to the Low trajectory class. However, there were no differences in odds of past-month cannabis use between those in the High and Moderate trajectory classes or between those in the Moderate and Low trajectory classes. There remained no statistically significant differences in typical number of drinking days per week and odds of past-month binge drinking among the three loneliness trajectory classes.
Discussion
Addressing loneliness and improving social connections is a public health priority (U.S. Surgeon General, 2021). Among young adults, the prevalence of depression and anxiety have increased rapidly, loneliness continues to rise, and alcohol and cannabis use are common. Extending our prior work examining increases in loneliness during the pandemic (Lee, Cadigan, & Rhew, 2020), we examined the longitudinal trajectory of loneliness from January 2020 (pre-pandemic) to March/April 2021 (pandemic) and assessed how loneliness trajectory classes were associated with later psychological distress and substance use. Trajectories of loneliness varied from lower to higher levels. When controlling for pre-pandemic levels, higher trajectories of loneliness were associated with greater odds of past-month cannabis use compared to Low trajectories, but not significantly associated with psychological distress (i.e., depression and anxiety symptoms), or alcohol use, in March/April 2021.
The three loneliness trajectories show that young adults who were more lonely prior to the pandemic continued to show higher levels of loneliness throughout the pandemic (High), those who had moderate levels of loneliness remained relatively stable throughout the pandemic (Moderate), and those who had low levels of loneliness increased slightly during the pandemic (Low), suggesting young adults followed a similar trajectory in terms of their loneliness at pre-pandemic levels. This highlights that those who were already struggling in terms of loneliness before the pandemic continued to struggle as the pandemic continued, suggesting the importance of universal screening for loneliness and brief intervention to perhaps alter this trajectory.
These findings are similar to those from an adult sample in the UK where loneliness was assessed from March 2020 to May 2020 and trajectories of loneliness also ranged from low to high (Bu, Steptoe, & Fancourt, 2020). Our finding that pre-pandemic social support appears to be a protective factor against elevated levels of loneliness is consistent with findings from Bu et al., (2020) showing social support is associated with lower odds of being in a higher loneliness trajectory, and from Lee et al. (2020) showing those with lower social support report consistently higher levels of loneliness compared to those with higher social support. Young adults with higher perceived social support may have relied on their social network during internment periods of loneliness, which may prevented development of a more chronic, higher trajectory of loneliness. The finding that none of the demographic covariates (e.g., student status; gender; age; race; LGBTQ status) were associated with loneliness trajectory class membership was surprising, as research has shown differences in loneliness levels among these groups (Bonin, McCreary, & Sadava, 2000; Evans et al., 2017; Fish et al., 2021). We encourage future work to examine these demographic groups with larger sample sizes.
Although it is well documented that loneliness is associated with poor mental health (Cacioppo et al., 2006), this study is the first, to our knowledge, to examine a year of loneliness trajectories during the pandemic and whether these distinct trajectories were associated with substance use and psychological distress. Prior to adjusting for pre-pandemic levels, young adults with higher levels of loneliness during the pandemic showed greater levels of depressive and anxiety symptoms in March/April 2021. However, after further adjusting for pre-pandemic symptom scores, associations became attenuated and, although they remained in the same direction, there were no longer any statistically significant differences among loneliness trajectory classes for depressive or anxiety symptoms. It may be that those who were already showing higher levels of loneliness were also initially high in psychological distress. The distress may have remained elevated during the pandemic and shaped loneliness. This is somewhat consistent with findings showing that loneliness and depression may be mutually occurring (Cacioppo et al. 2006). However, other rigorous longitudinal studies have observed that loneliness is related to subsequent depressive symptoms (VanderWeele et al., 2011). It may be that we had limited statistical power to observe an association especially when comparing the high loneliness trajectory class, which consisted of relatively few participants, to the low trajectory class.
Our findings also show that young adults with higher levels of loneliness may be more likely to engage in cannabis use, although not alcohol use. We found young adults in the High loneliness trajectory had greater odds of past-month cannabis use compared those in the Low trajectory; however, there were no statistically significant differences among the loneliness trajectory classes in either of the alcohol outcomes. This finding is consistent with previous work observing that greater frequency of cannabis, but not alcohol use, was cross-sectionally associated with higher levels of loneliness (Rhew, Cadigan, & Lee, 2021). Consistent with theories of affect-motivation, cannabis may have been used to cope with chronic feelings of negative affect (including loneliness) throughout the pandemic. As frequent cannabis users are more likely to experience emotion dysregulation than non-users (Bonn-Miller et al., 2008), heightened levels of loneliness may have sustained or increased cannabis use to cope with this distress. The lack of association between loneliness trajectory and alcohol outcomes may be suggestive of historical trends indicating the strength of the relationship between psychological distress and alcohol use is weakening (Keyes, Hamilton, Patrick & Schulenberg, 2020), and consistent with literature showing negative associations between loneliness and alcohol use (Diehl et al., 2018; McBroom, Fife, & Nelson, 2008) as more alcohol is consumed when individuals feel less lonely, suggesting alcohol may be used as means of social facilitation and not for affect-regulation.
Lonely young adults may use cannabis in a solitary way to enhance their daily activities (e.g., make every day activities more interesting), especially during the pandemic when more individuals are spending time alone and social distancing from others. Using cannabis to enhance activities (e.g. music sounds better, every day activities more interesting) has been associated with greater cannabis use (Lee, Neighbors, & Woods, 2007). Future work could examine associations between loneliness and solitary (compared to social) substance use. Prior work has found loneliness to be associated with more solitary alcohol use (Gonzalez & Skewes, 2013) and less social drinking (Arpin et al., 2015). Young adults with higher loneliness trajectories may be more likely to engage in solitary substance use compared to those in a ‘lower’ loneliness class, also negatively impacting mental health.
Limitations
Study findings should be considered in light of limitations. The study was a convenience sample that originated from an urban region of the Pacific Northwest in the U.S. recruited via social media and other methods. Thus, the findings may not be representative of the broader young adult population. However, online strategies for recruitment may aid in enrollment of harder-to-reach populations. There may be important unmeasured confounders that were unaccounted for. However, this study did adjust for various covariates including pre-pandemic levels of the outcome and other important sociodemographic characteristics. Study measures were based on self-report, which may be a concern particularly for substance use outcomes. However, substance use measures as well as the psychological distress measures have been widely used in research. Further, there may be less concern about under-reporting of substance use in a state where cannabis is legal. In addition to assessing solitary substance use, context of use, and motivations for use, future work could examine within-person variability in loneliness throughout the pandemic and associations with mental health and substance use outcomes. Similarly, our models do not account for potential non-linear changes in substance use and mental health outcomes across the study period or for differential change trajectories in these outcome variables among the latent loneliness classes. Future work could test multi-group growth models and/or multivariate growth models to account for such changes in both loneliness and substance use and mental health outcomes. We also encourage future research to examine associations between motives for substance use (particularly coping) and loneliness, including directionality.
Conclusions
Consistent with the U.S. Surgeon General Mental Health’s Advisory (2021) there is an urgent public health need to support the mental health of young adults. In March/April 2021, psychological distress among young adults in a national sample was alarmingly high, with 52.9% reporting symptoms of depression or anxiety in the past week (Centers for Disease Control and Prevention, 2022). Our findings show trajectories of loneliness to vary from low to high, however these trajectories were relatively stable from January 2020 to January 2021. For example, young adults who were lonely pre-pandemic continued to report high levels of loneliness throughout the pandemic. Likewise, those with low loneliness pre-pandemic continued to have consistently low levels, although increasing slightly. Young adults with moderate loneliness scores remained relatively stable throughout the pandemic. This suggests that for many young adults, patterns of loneliness remained somewhat consistent.
Addressing loneliness and the mental health of young adults continues to be a public health priority. Screening for loneliness (in addition to standard depression and anxiety screening) could be one effective tool that primary care facilities could incorporate. Increasing adaptive coping skills could be especially helpful, including increasing connection and feelings of connectedness, both shown to improve wellbeing (Cacioppo et al., 2015). Interventions targeting loneliness have primarily focused on four strategies: (1) improving social skills, (2) enhancing social support, (3) increasing social contact, and (4) addressing maladaptive thoughts related to social isolation (Masi, Chen, Hawkley, & Cacioppo, 2011), all of which could be useful for young adults. As our findings show perceived social support to be protective against loneliness, interventions could directly address ways of increasing support and social connections. Given that young adults in higher loneliness trajectories are at risk for cannabis use, clinicians could also screen for substance use, motivations for using, and provide brief intervention when appropriate.
Acknowledgments
Data collection and manuscript preparation were supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA R01AA027496-02S1 to C. Lee). Manuscript preparation was also supported by R34AA028074 to J. Cadigan. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism and the National Institutes of Health.
References
- Arbeau KJ, Kuiken D, & Wild TC (2011). Drinking to enhance and to cope: A daily process study of motive specificity. Addictive Behaviors, 36(12), 1174–1183. [DOI] [PubMed] [Google Scholar]
- Arpin SN, Mohr CD, & Brannan D (2015). Having friends and feeling lonely: A daily process examination of transient loneliness, socialization, and drinking behavior. Personality and Social Psychology Bulletin, 41(5), 615–628. [DOI] [PubMed] [Google Scholar]
- Bartel SJ, Sherry SB, & Stewart SH (2020). Self-isolation: A significant contributor to cannabis use during the COVID-19 pandemic. Substance Abuse, 41(4), 409–412. [DOI] [PubMed] [Google Scholar]
- Buecker S, Horstmann KT, Krasko J, Kritzler S, Terwiel S, Kaiser T, & Luhmann M (2020). Changes in daily loneliness for German residents during the first four weeks of the COVID-19 pandemic. Social science & medicine, 265, 113541. [DOI] [PubMed] [Google Scholar]
- Bonin MF, McCreary DR, & Sadava SW (2000). Problem drinking behavior in two community-based samples of adults: Influence of gender, coping, loneliness, and depression. Psychology of Addictive Behaviors, 14(2), 151. [DOI] [PubMed] [Google Scholar]
- Bragard E, Giorgi S, Juneau P, & Curtis BL (2021). Loneliness and Daily Alcohol Consumption During the COVID-19 Pandemic. Alcohol and Alcoholism [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray BC, Lanza ST, & Tan X (2015). Eliminating bias in classify-analyze approaches for latent class analysis. Structural Equation Modeling, 22, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, & Zvolensky MJ (2008). Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Substance Use & Misuse, 43(11), 1653–1665. [DOI] [PubMed] [Google Scholar]
- Bu F, Steptoe A, & Fancourt D (2020). Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Social Science & Medicine, 265, 113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buecker S, & Horstmann KT (2021). Loneliness and social isolation during the COVID-19 pandemic: A systematic review enriched with empirical evidence from a large-scale diary study. European Psychologist, 26(4), 272. [Google Scholar]
- Cacioppo JT, Cacioppo S, & Boomsma DI (2014). Evolutionary mechanisms for loneliness. Cognition & emotion, 28(1), 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Ernst JM, Burleson MH, McClintock MK, Malarkey WB, Hawkley LC, … & Berntson GG (2000). Lonely traits and concomitant physiological processes: The MacArthur social neuroscience studies. International Journal of Psychophysiology, 35(2–3), 143–154. [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015). Loneliness: Clinical import and interventions. Perspectives on Psychological Science, 10, 238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, & Thisted RA (2006). Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and aging, 21(1), 140. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2022). Retrieved from https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53, 189–200. [DOI] [PubMed] [Google Scholar]
- Diehl K, Jansen C, Ishchanova K, & Hilger-Kolb J (2018). Loneliness at Universities: Determinants of Emotional and Social Loneliness among Students. International Journal of Environmental Research and Public Health, 15(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EA, Grella CE, Washington DL, & Upchurch DM (2017). Gender and race/ethnic differences in the persistence of alcohol, drug, and poly-substance use disorders. Drug and alcohol dependence, 174, 128–136. [DOI] [PubMed] [Google Scholar]
- Fish JN, Salerno J, Williams ND, Rinderknecht RG, Drotning KJ, Sayer L, & Doan L (2021). Sexual minority disparities in health and well-being as a consequence of the COVID-19 pandemic differ by sexual identity. LGBT health, 8, 263–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, & Skewes MC (2013). Solitary heavy drinking, social relationships, and negative mood regulation in college drinkers. Addiction Research & Theory, 21(4), 285–294. [Google Scholar]
- Graupensperger S, Benson AJ, Kilmer JR, & Evans MB (2020). Social (un) distancing: teammate interactions, athletic identity, and mental health of student-athletes during the COVID-19 pandemic. Journal of Adolescent Health, 67(5), 662–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger S, Fleming CB, Jaffe AE, Rhew IC, Patrick ME, & Lee CM (2021). Changes in young adults’ alcohol and marijuana use, norms, and motives from before to during the COVID-19 pandemic. Journal of Adolescent Health, 68(4), 658–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger S, Cadigan JM, Einberger C, & Lee CM (2021). Multifaceted COVID-19-related stressors and associations with indices of mental health, well-being, and substance use among young adults. International Journal of Mental Health and Addiction, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm KJ, Ram N, & Estabrook R (2017). Growth modeling: Structural equation and multilevel modeling approaches. Guilford Publications. [Google Scholar]
- Hawes MT, Szenczy AK, Olino TM, Nelson BD, & Klein DN [2021]. Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatry Research, 298, 113778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of behavioral medicine, 40(2), 218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes LM, Popova L, & Ling PM (2016). State of transition: Marijuana use among young adults in the San Francisco Bay Area. Preventive Medicine, 90, 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, & Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on psychological science, 10(2), 227–237. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26, 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram I, Kelly PJ, Deane FP, Baker AL, & Raftery DK (2018). Loneliness in Treatment-Seeking Substance-Dependent Populations: Validation of the Social and Emotional Loneliness Scale for Adults–Short Version. Journal of dual diagnosis, 14(4), 211–219. [DOI] [PubMed] [Google Scholar]
- Ingram I, Kelly PJ, Deane FP, Baker AL, Goh MC, Raftery DK, & Dingle GA (2020). Loneliness among people with substance use problems: A narrative systematic review. Drug and alcohol review, 39(5), 447–483. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hamilton A, Patrick ME, & Schulenberg J (2020). Diverging trends in the relationship between binge drinking and depressive symptoms among adolescents in the US from 1991 through 2018. Journal of Adolescent Health, 66(5), 529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WD, Cloonen SA, Taylor EC, & Dailey NS (2020). Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Research, 113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114, 163–173. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care, 1284–1292. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, & Löwe B (2007). Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Annals of internal medicine, 146(5), 317–325. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical psychology review, 25(7), 841–861. [DOI] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, & Woods BA (2007). Marijuana motives: Young adults’ reasons for using marijuana. Addictive behaviors, 32(7), 1384–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Cadigan JM & Rhew IC (2020). Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. Journal of Adolescent Health, 67, 714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, & Herzberg PY (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46, 266–274. [DOI] [PubMed] [Google Scholar]
- Luchetti M, Lee JH, Aschwanden D, Sesker A, Strickhouser JE, Terracciano A, & Sutin AR (2020). The trajectory of loneliness in response to COVID-19. American Psychologist, 75, 897–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi CM, Chen HY, Hawkley LC, & Cacioppo JT (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBroom E, Fife E, & Nelson C (2008). “ Risky Business”: The College Transition, Loneliness, and Alcohol Consumption. Journal of the First-Year Experience & Students in Transition, 20(2), 45–64. [Google Scholar]
- McGinty EE, Presskreischer R, Han H, & Barry CL (2020). Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA, 324, 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay MT, Konowalczyk S, Andretta JR, & Cole JC (2017). The direct and indirect effect of loneliness on the development of adolescent alcohol use in the United Kingdom. Addictive behaviors reports, 6, 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2021). Mplus user’s guide (7th ed.). Muthén & Muthén. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2003). Underage drinking: A major public health challenge. Alcohol Alert, 59, 1–4 [Google Scholar]
- Office of the Surgeon General (2021). Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory (2021). https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
- Park CL, Armeli S, & Tennen H (2004). The daily stress and coping process and alcohol use among college students. Journal of studies on Alcohol, 65(1), 126–135. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Rhew IC, Lewis MA, Abdallah DA, Larimer ME, Schulenberg JE, & Lee CM (2018). Alcohol motivations and behaviors during months young adults experience social role transitions: Microtransitions in early adulthood. Psychology of Addictive Behaviors, 32(8), 895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Rhew IC, Cadigan JM, & Lee CM (2021). Marijuana, but not alcohol, use frequency associated with greater loneliness, psychological distress, and less flourishing among young adults. Drug and alcohol dependence, 218, 108404. 10.1016/j.drugalcdep.2020.108404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez LM, Litt DM, & Stewart SH (2020). Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors, 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB (2014). Multiple imputation for nonresponse in surveys. John Wiley & Sons. [Google Scholar]
- Russell D, Peplau LA, & Cutrona CE (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39, 472–480. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Patrick ME, Johnston LD, O’Malley PM, Bachman JG, & Miech RA (2021). Monitoring the Future National Survey Results on Drug Use, 1975–2020. Volume II, College Students & Adults Ages 19–60. Institute for Social Research. [Google Scholar]
- Schuler MS, & Collins RL (2020). Sexual minority substance use disparities: Bisexual women at elevated risk relative to other sexual minority groups. Drug and alcohol dependence, 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stickley A, Koyanagi A, Koposov R, Schwab-Stone M, & Ruchkin V (2014). Loneliness and health risk behaviours among Russian and US adolescents: a cross-sectional study. BMC public health, 14(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/ [Google Scholar]
- Van Buuren S, & Groothuis-Oudshoorn K (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45, 1–67. [Google Scholar]
- Vahratian A, Blumberg SJ, Terlizzi EP, & Schiller JS (2021). Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic—United States, August 2020–February 2021. Morbidity and Mortality Weekly Report, 70(13), 490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, Hawkley LC, Thisted RA, & Cacioppo JT (2011). A marginal structural model analysis for loneliness: Implications for intervention trials and clinical practice. Journal of Consulting and Clinical Psychology, 79(2), 225–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venables WN, & Ripley BD (2002). Modern applied statistics with S (4th ed.). Springer: New York. [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52, 30–41. [DOI] [PubMed] [Google Scholar]


