Abstract
Background
To compare the visual efficacy and patient satisfaction between 2 toric IOLs (TIOL), enhanced for intermediate vision or monofocal.
Methods
A retrospective chart review was performed of 100 eyes from 68 astigmatic patients who underwent cataract surgery with implantation of a Tecnis Eyhance Toric II IOL (Johnson & Johnson Vision, Irvine, CA, USA) (Group 1, 50 eyes) or Tecnis TIOL (Group 2, 50 eyes). The uncorrected distant (UDVA), intermediate (UIVA), and near (UNVA) visual acuities; residual refractive astigmatism; defocus curve; and IOL axis rotation were evaluated at 1 week, 1 month, 2 months, and 3 months postoperatively.
Results
The postoperative UDVA and UNVA refractive astigmatism values of the two groups were better than the preoperative measurements (P < 0.05), but there was no statistical difference between the two groups (P > 0.05). The postoperative UIVA of group 1 (0.18 ± 0.15 logMAR) was significantly better than that of group 2 (0.30 ± 0.25) (P < 0.05). The mean postoperative IOL rotation of group 1 (2.51 ± 0.79°) was lower than that of group 2 (3.02 ± 0.84°) (P < 0.05). Overall satisfaction of group 1 (1.27 ± 0.47) was better than that of group 2 (2.02 ± 0.53) (P < 0.05).
Conclusions
The Tecnis Eyhance Toric II IOL demonstrated less postoperative IOL rotation and excellent uncorrected intermediate vision compared with the Tecnis TIOL. Near visual acuity and overall satisfaction with the Tecnis Eyhance Toric II IOL were also higher than those with the Tecnis TIOL.
Keywords: Enhanced monofocal TIOL, Monofocal TIOL, IOL rotation, Intermediate vision
Introduction
Approximately 60% of patients who have undergone cataract surgery have greater than 0.75 diopters (D) of corneal astigmatism, and 20% have astigmatism of 1.5 D or greater [1, 2]. Even after cataract surgery, patients would have lower visual acuity and increased spectacle dependence if such astigmatism is not corrected [3]. Toric intraocular lenses (TIOLs) can improve uncorrected visual acuity in cataract patients by resolving both the opaque lens and the corneal astigmatism [4]. A 1° rotation of a TIOL results in a 3% decrease of effective cylinder power. When the TIOL is rotated by 30° following cataract surgery, the full corrective impact of astigmatism is lost [5].
In everyday life, intermediate distance tasks such as eating, computer work, and looking at the dashboard of a car are important and must be considered for every patient after cataract surgery [6, 7]. Therefore, IOLs that decrease spectacle dependence for intermediate vision are attractive for cataract patients [8].
An enhanced monofocal TIOL with a modified aspheric anterior surface and a continuous power profile has recently been designed to increase intermediate vision. The lens also has frosted haptics to significantly increase rotational stability after cataract surgery [9].
Several studies have analyzed the rotational stability of the enhanced monofocal TIOL [9, 10]. In the present study, we aim to compare intermediate visual efficacy and patient satisfaction with the enhanced monofocal TIOL and basic monofocal TIOL in cataract patients with corneal astigmatism.
Methods
This study was a retrospective data analysis carried out in accordance with the Declaration of Helsinki and was approved by Bucheon St. Mary Hospital's Institutional Review Board (IRB)/Ethics Committee.
Inclusion and exclusion criteria
A total of 100 eyes from 68 patients with greater than 1.0 D of total corneal astigmatism was included from January 2023 to December 2024. To minimize potential selection biases in a retrospective study, we included patients randomly based on the inclusion criteria. Eligible subjects were those who had total corneal astigmatism from 1.0 to 2.5 D and axial length from 22.0–25.0 mm. Nuclear opacity grades 3–4 were included based on the Lens Opacities Classification System III. Patients with bilateral cataract received the same type of IOL in both eyes. Patients with the following conditions that could affect clinical parameters were excluded: degenerative corneal disease, ectatic corneal disease, lens subluxation/dislocation, or amblyopia. We followed study reporting guidelines and a study flowchart (https://www.equator-network.org/reporting-guidelines/).
Patient examination
Data from astigmatic patients who underwent cataract surgery with implantation of a Tecnis Eyhance Toric II IOL (Johnson & Johnson Vision, Irvine, CA, USA) (Group 1: DIU IOL, 50 eyes) or Tecnis TIOL (Group 2: ZCT IOL, 50 eyes) were collected retrospectively. Every patient underwent a total ophthalmological examination, and their perioperative information was recorded. Uncorrected and corrected distant, intermediate, and near visual acuities were recorded as logMAR at 1 week, 1 month, 2 months, and 3 months after surgery. Manifest refraction, keratometry, and biometry with the IOLMaster partial coherence interferometry device (Carl Zeiss Meditec AG); corneal topography (Pentacam®, Oculus, Germany); slit lamp examination; and dilated funduscopy were performed. The web-based toric calculator provided by the IOL manufacturer was used to calculate the required cylinder power and axis for each implanted IOL. Surgically-induced astigmatism was set at 0.5 diopters. The Scheimpflug system (Pentacam®, Oculus, Germany) was used to determine total corneal astigmatism. Patient satisfaction was assessed with a Cataract TyPE Specification questionnaire at 3 months after cataract surgery [11]. The subjective questionnaire was completed for each eye in patients who underwent bilateral cataract surgery. A score ranging from 0 to 100 was calculated for each dimension, and individual scores were combined to produce an unweighted overall score, also with a range of 0 to 100. The axis of toric IOL was measured with PicPickTools (NGWIN, Seoul, Korea) using a photograph of the anterior segment under pupil dilation from postoperative 1 day to 3 months. The mean angle rotation was calculated as the average of TIOL rotation values from postoperative 1 day to 3 months.
Operative procedures
With the patient sitting, the corneal limbus was marked at 0°, 90°, and 180° meridian after topical anesthetic eye drops were instilled. All patients received topical anesthetic by a single trained surgeon (E. C. K) utilizing a CENTURION® (Alcon Laboratories, Inc., Fort Worth, TX, USA). Gentian violet was used to mark the corneal steep axis and 6.0 mm capsulotomy. A continuous curvilinear capsulotomy, hydrodissection, and hydrodelineation were performed. Phacoemulsification was performed using 2.75-mm-sized phacotips and infusion/aspiration (I/A) cannulas. A TIOL (Tecnis ZCT or DIU; Johnson & Johnson Vision, Irvine, CA, USA) was implanted in the capsular bag and was rotated to the total corneal astigmatism axis. The wound was hydrated with BSS. Gatifloxacin 0.3% (Gatiflo, Handok, Chungbuk, Korea) and fluorometholone acetate 0.01% (Ocumetholone, Samil, Seoul, Korea) eye drops were instilled postoperatively 4 times a day for 4 weeks.
Statistical analysis
SPSS for Windows, version 21.0.1 (SPSS Inc., Chicago, IL) was used to perform statistical analyses. A power analysis was conducted to estimate minimum needed sample size. To compare pre- and postoperative VA, as well as refractive and keratometer astigmatism values, the Wilcoxon signed rank test was performed. Mann–Whitney tests were used to compare the two groups. P values less than 0.05 were deemed statistically significant.
Results
The preoperative characteristics of patients in each group are demonstrated in Table 1. There were no significant differences between the two groups in age, preoperative UCVA or CDVA, refractive astigmatism, or total corneal astigmatism (p > 0.05).
Table 1.
Preoperative data of patients
| Parameter | Group 1 (TECNIS Eyhance Toric II) | Group 2 (TECNIS Toric) | P value |
|---|---|---|---|
| Mean age (Years) | 71.3 ± 9.7 | 67.5 ± 7.2 | 0.48 |
| Gender (F:M) | 36:14 | 38:12 | 0.59 |
| Mean corneal power | 44.58 ± 1.47 | 44.50 ± 1.53 | 0.71 |
| Anterior chamber depth (mm) | 3.75 ± 0.89 | 3.80 ± 0.91 | 0.46 |
| IOL Diopter | 20.25 ± 1.81 | 20.73 ± 1.95 | 0.24 |
| Total corneal Astigmatism (D) | 1.85 ± 0.52 | 1.93 ± 0.79 | 0.36 |
| Refractive Astigmatism (D) | 2.23 ± 0.84 | 2.31 ± 0.94 | 0.15 |
| UDVA (LogMAR) | 0.34 ± 0.18 | 0.41 ± 0.26 | 0.26 |
| CDVA (logMAR) | 0.23 ± 0.12 | 0.25 ± 0.15 | 0.68 |
| Eyes (n) | 50 | 50 |
There was no statistical difference between two groups (p > 0.05)
Values are presented as mean ± SD. D; diopter
Statistical comparisons between two groups were performed using the Mann–Whitney U test
The categorical data were compared between groups with the χ2 test
Postoperative visual acuity
There were no significant differences between the two groups according to postoperative UDVA, CDVA, uncorrected near visual acuity (UNVA), or residual astigmatism at 3 months after cataract surgery (p > 0.05). However, the uncorrected intermediate visual acuity (UIVA) of group 1 (0.18 ± 0.15 logMAR) was significantly better than that of group 2 (0.30 ± 0.25) (p < 0.05) (Table 2).
Table 2.
Postoperative outcomes after 3 months
| Parameter | Group 1 (Tecnis Eyhance Toric II) | Group 2 (Tecnis Toric) | P-value |
|---|---|---|---|
| UDVA (logMAR) | 0.04 ± 0.03 | 0.08 ± 0.07 | 0.12 |
| CDVA (logMAR) | 0.04 ± 0.02 | 0.04 ± 0.03 | 0.64 |
| UIVA (logMAR) | *0.18 ± 0.15 | 0.30 ± 0.25 | 0.02 |
| UNVA (logMAR) | 0.75 ± 0.52 | 0.81 ± 0.65 | 0.07 |
| Mean sphere refraction (D) | 0.14 ± 0.18 | 0.15 ± 0.16 | 0.54 |
| Cylinder refraction (D) | -0.55 ± 0.33 | -0.61 ± 0.31 | 0.20 |
| Mean refraction spherical equivalent (D) | -0.13 ± 0.39 | -0.15 ± 0.45 | 0.32 |
| Residual Astigmatism (D) | 1.85 ± 0.52 | 1.93 ± 0.79 | 0.28 |
| Eyes (n) | 50 | 50 |
The postoperative UIVA of group 1 was significantly better than that of group 2 (P < 0.05)
Values are presented as mean ± SD. D; diopter
Statistical comparisons between two groups were performed using the Mann–Whitney U test
The categorical data were compared between groups with the χ2 test
UDVA Uncorrected distant visual acuity, CDVA Corrected distant visual acuity, UIVA Uncorrected intermediate visual acuity, UNVA Uncorrected near visual acuity
*P < 0.05
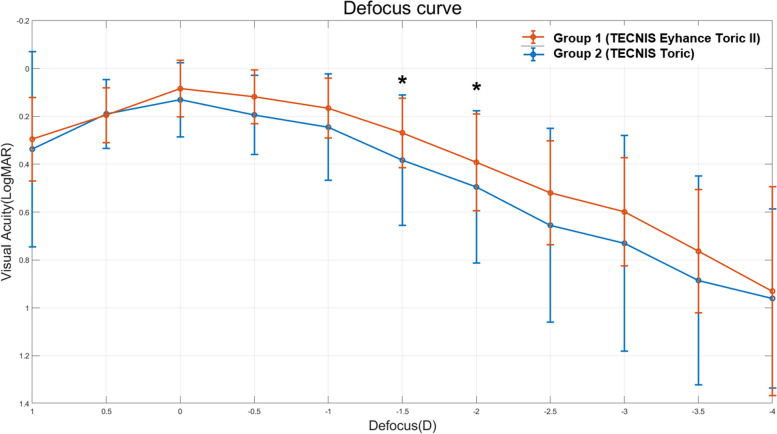
Defocus curve
The defocus curves observed in both groups at 3 months after cataract surgery are shown in Fig. 1. Both curves indicate a peak at defocus of 0.00 D (4 m) and a decrease in visual acuity as negative defocus increased. The Tecnis Eyhance Toric II IOL showed significantly better defocus at -1.5 D and -2.0 D (corresponding to 66–50 cm) compared with the Tecnis Toric IOL (P < 0.05) (Fig. 1).
Fig. 1.
Mean defocus curves of the two intraocular lens groups logMAR = logarithm of the minimum angle of resolution. The TECNIS Eyhance Toric II IOL (DIU) provided significantly better defocus results at -1.5 D and -2.0 D of defocus range (corresponding to 66 ~ 50 cm) compared with the TECNIS Toric IOL (ZCT) (P < 0.05). *: P < 0.05. Values are presented as mean ± SD
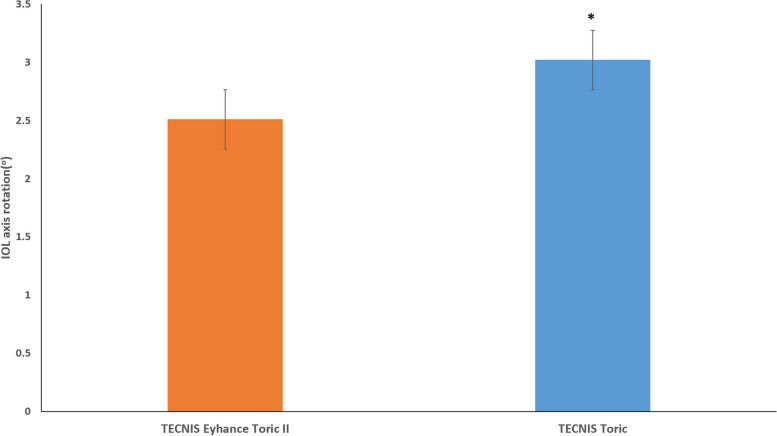
IOL axis rotation
The IOL axis rotation of group 1 was significantly smaller than that of group 2 from postoperative 1 day to 3 months (P < 0.05) (Fig. 2). There was no significant difference in the percentage of eyes with misalignment > 10° in the groups (group 1: 2%, group 2: 3%, P > 0.05).
Fig. 2.
Amount of IOL axis rotation after cataract surgery from 1 day to 3 months. IOL axis rotation was significantly smaller with the TECNIS Eyhance Toric II IOL (DIU) than with the TECNIS Toric IOL (ZCT) (p < 0.05). *: P < 0.05. Values are presented as mean ± SD
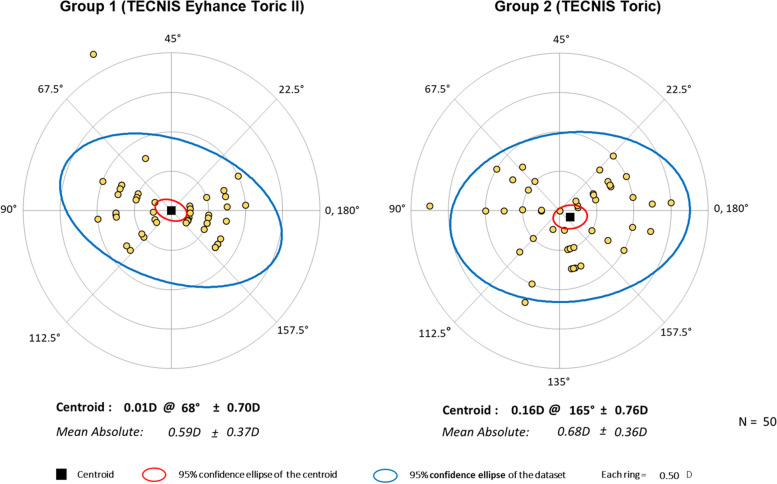
The average deviation from the planned axis was similar for the IOLs (group 1: 2.51 ± 1.35 and group 2: 3.02 ± 1.52, P > 0.05). No difference in misalignment direction was found (group 1: 72% and group 2: 68% clockwise [CW] deviation, respectively, P > 0.05) (Table 3). The number of lenses precisely on located on the planed axis (group 1: 16%, and group 2: 10%) was (or was not) significantly different between the groups. Double angle plots of the misalignment of each IOL model are presented in Fig. 3.
Table 3.
The TIOL deviation and its direction of the different TIOLs
| Parameter | Group 1 (Tecnis Eyhance Toric II) | Group 2 (Tecnis Toric) | P-value |
|---|---|---|---|
| misalignment (°), absolute mean ± SD [range] | 2.51 ± 0.35 [0, 11] | 3.02 ± 0.52 [0, 15] | 0.03 |
| CW misalignment, n (%*) | 36 (72) | 35 (70) | |
| CCW misalignment, n (%*) | 6 (12) | 10 (20) |
Statistical comparisons between two groups were performed using the Mann–Whitney U test
TIOL Toric intraocular lens, CW Clockwise, CCW Counterclockwise
*IOLs that were precisely on the planned axis were excluded
Fig. 3.
Double-angle plots of refractive astigmatism prediction errors evaluated with centroids, standard deviation of the centroids, and 95% confidence ellipses of the prediction errors. There was no significant difference of prediction errors in both groups (P > 0.05). Each ring = 0.50 diopters (D)
Subjective satisfaction score
There were no significant differences in far vision satisfaction, glare, or halo between the two groups (P > 0.05). However, the near vision and overall satisfaction ratings of group 1 (1.53 ± 0.65, 1.27 ± 0.47, respectively) were significantly better than those of group 2 (1.97 ± 0.97, 2.02 ± 0.53, respectively) (P < 0.05) (Table 4).
Table 4.
Subjective satisfaction score
| Parameter | Group 1 (Tecnis Eyhance Toric II) | Group 2 (Tecnis Toric) | P-value |
|---|---|---|---|
| Overall satisfaction | *1.27 ± 0.47 | 2.02 ± 0.53 | 0.02 |
| Far vision satisfaction | 1.62 ± 0.87 | 1.66 ± 0.73 | 0.43 |
| Near vision satisfaction | *1.53 ± 0.65 | 1.97 ± 0.97 | 0.03 |
| Glare, Halo | 1.75 ± 0.81 | 1.62 ± 0.51 | 0.26 |
Low score means high satisfaction. (Range of score: 0 ~ 100)
Near vision and overall satisfactions of group 1 were significantly better than those of group 2 (P < 0.05)
Values are presented as mean ± SD. D; diopter
*P < 0.05
Discussion
Correction of astigmatism and presbyopia after cataract surgery is becoming more prevalent and popular among patients [8]. Because of the good clinical outcomes and increasing patient demand, the use of TIOLs in cataract surgery to correct corneal astigmatism has increased in popularity [12, 13]. Uncorrected vision after TIOL implantation, on the other hand, varies according to postoperative residual astigmatism change due to IOL axis rotation [3, 14]. To treat presbyopia in cataract patients, implantation of a multifocal IOL has been popular due to its excellent near vision; however, this type of lens causes a larger halo that is associated with a worse low-contrast UDVA and visual acuity [15]. The Tecnis Eyhance IOL can provide good intermediate vision while maintaining a visual acuity similar to that of a monofocal IOL [8].
The rotational stability of the Tecnis TIOL (Johnson & Johnson Vision Care, Inc., Santa Ana, CA, US) has been reported, but the methodology used to assess “rotational stability” was not disclosed in the studies [16–18]. In addition, some patients required repositioning surgery [19, 20]. The Tecnis Eyhance Toric II IOL has frosted haptics to increase surface friction between the capsular bag and the lens, as well as a constant power profile optic to improve intermediate vision [10, 21–23].
Takaku R et al. reported higher rotational stability in Toric II IOL than the Toric I IOL, with lower residual manifest astigmatism (p = 0.018), lower axis misalignment (p = 0.04), lower incidence of misalignment > 10º (p = 0.0044), and smaller prediction errors (p= 0.043) [9]. Osawa R. et al. reported the same results with rotational stability and an incidence of misalignment > 10º but showed no significant differences in residual astigmatism. [10]
In our results, the axis rotation of group 1 was significantly smaller than that of group 2 from postoperative 1 day to 3 months (P < 0.05) (Fig. 2). However, there was no significant difference in residual astigmatism or percentage of eyes with misalignment > 10° (group 1: 2%, group 2: 3%) (P > 0.05).
Takaku R. et al. and Osawa R. et al. reported no significant differences in UDVA and CDVA between TECNIS Eyhance Toric II IOL and TECNIS TIOL. [9, 10]
In our results, there were no significant differences between the two IOLs in UDVA, CDVA, and UNVA. However, the UDVA and UNVA of group 1 were numerically higher than those of group 2 (P > 0.05). The uncorrected intermediate visual acuity (UIVA) of group 1 (0.18 ± 0.15 logMAR) was significantly better than that of group 2 (0.30 ± 0.25) (P < 0.05) (Table 2). Mencucci R. et al. reported better monocular and binocular UIVA in the Eyhance nontoric IOL compared with the Tecnis nontoric IOL. [8] In our results, there were no significant differences in far vision satisfaction, glare, and halo between the two groups (p > 0.05). Mencucci R. et al. also described no significant differences in glare and halo perception, photopic contrast sensitivity, MTF cutoff, OSI, and Strehl ratio between the Eyhance nontoric IOL and Tecnis nontoric IOL. [8]
In our results, the near vision and overall satisfaction of group 1 (1.53 ± 0.65, 1.27 ± 0.47, respectively) were significantly better than those of group 2 (1.97 ± 0.97, 2.02 ± 0.53, respectively) (P < 0.05) (Table 4).
The results of UNVA and satisfaction score for near vision do not coincide in this study. As the UNVA of the Tecnis Eyhance Toric II was numerically but not statistically higher than that of the Tecnis Toric, we thought that the subjective near vision satisfaction of the Tecnis Eyhance Toric II might be better than that of the Tecnis Toric. Because the TECNIS Eyhance Toric II has been shown to be better for intermediate vision, we wanted to compare the differences of far and near vision satisfaction between the IOLs. The non-significantly higher glare and halo score of group 1 was indicates that some patients are concerned about night driving and TV viewing in a dark environment after implantation of the Tecnis Eyhance Toric II.
The time differences between the first eye and the second eye cannot influence the subjective aspect of the study because the time difference was just from 1 day to 1 week.
In this study, we compared the intermediate visual efficacy and patient satisfaction of the enhanced monofocal TIOL and original monofocal TIOL in cataract patients with corneal astigmatism.
Limitations of our investigation were use of data from a single center, use of a small number of patients, and a short follow-up period. Further studies are needed to verify the efficacy of the Tecnis Eyhance TIOL compared to the Tecnis TIOL.
In conclusion, the Tecnis Eyhance TIOL may be a better option in cataract patients with astigmatism. This TIOL shows better spectacle independence for intermediate vision and higher rotational stability than the original Tecnis TIOL while maintaining similar visual acuity.
Acknowledgements
None.
Abbreviations
- BCVA
Best corrected visual acuity
- LogMAR
Logarithm of the Minimum Angle of Resolution
- TIOL
Toric intraocular lens
- UCVA
Uncorrected visual acuity
Authors’ contributions
HSH was involved in analysis and interpretation of data and drafting the manuscript. HSH, DA, HSK, ECK made contribution to acquisition of data and drafting. ECK contributed to conception and design, analysis and interpretation of data, drafting and revising the manuscript. All authors read and approved the final manuscript.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2022R1F1A1069218, 2017R1A1A2A10000681, and 2020R1A2C1005009) and the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (HI17C0659). The funding offered support in the design of the study and collection, analysis, interpretation of data, and publication fee.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the institutional review board at Bucheon St. Mary’s Hospital (HC22RASI0095); the informed consent was waived. All clinical investigations have been conducted according to the principles expressed in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36(9):1479–85. 10.1016/j.jcrs.2010.02.025 [DOI] [PubMed] [Google Scholar]
- 2.Ostri C, Falck L, Boberg-Ans G, Kessel L. The need for toric intra-ocular lens implantation in public ophthalmology departments. Acta Ophthalmol. 2015;93(5):e396–7. 10.1111/aos.12584 [DOI] [PubMed] [Google Scholar]
- 3.Hwang HS, Kim HS, Kim MS, Kim EC. The Effect of toric intraocular lens implantation in irregular corneal steep and flat meridian. J Ophthalmol. 2021;2021:3630668. 10.1155/2021/3630668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agresta B, Knorz MC, Donatti C, Jackson D. Visual acuity improvements after implantation of toric intraocular lenses in cataract patients with astigmatism: a systematic review. BMC Ophthalmol. 2012;12:41. 10.1186/1471-2415-12-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34(10):1631–6. 10.1016/j.jcrs.2008.04.041 [DOI] [PubMed] [Google Scholar]
- 6.Shen Z, Lin Y, Zhu Y, Liu X, Yan J, Yao K. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: a systematic review and meta-analysis. Sci Rep. 2017;7:45337. 10.1038/srep45337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breyer DRH, Kaymak H, Ax T, Kretz FTA, Auffarth GU, Hagen PR. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia Pac J Ophthalmol (Phila). 2017;6(4):339–49. [DOI] [PubMed] [Google Scholar]
- 8.Mencucci R, Favuzza E, Caporossi O, Savastano A, Rizzo S. Comparative analysis of visual outcomes, reading skills, contrast sensitivity, and patient satisfaction with two models of trifocal diffractive intraocular lenses and an extended range of vision intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2018;256(10):1913–22. 10.1007/s00417-018-4052-3 [DOI] [PubMed] [Google Scholar]
- 9.Takaku R, Nakano S, Iida M, Oshika T. Influence of frosted haptics on rotational stability of toric intraocular lenses. Sci Rep. 2021;11(1):15099. 10.1038/s41598-021-94293-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osawa R, Sano M, Yuguchi T, Kaiya T, Oshika T. Effects of modified haptics on surgical outcomes and rotational stability of toric intraocular lens implantation. J Refract Surg. 2022;38(10):648–53. 10.3928/1081597X-20220715-02 [DOI] [PubMed] [Google Scholar]
- 11.Gothwal VK, Wright TA, Lamoureux EL, Pesudovs K. Using Rasch analysis to revisit the validity of the Cataract TyPE Spec instrument for measuring cataract surgery outcomes. J Cataract Refract Surg. 2009;35(9):1509–17. 10.1016/j.jcrs.2009.03.056 [DOI] [PubMed] [Google Scholar]
- 12.Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses: historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg. 2013;39(4):624–37. 10.1016/j.jcrs.2013.02.020 [DOI] [PubMed] [Google Scholar]
- 13.Yoon CH, Kim MK. Improving the toric intraocular lens calculation by considering posterior corneal astigmatism and surgically-induced corneal astigmatism. Korean J Ophthalmol. 2018;32(4):265–72. 10.3341/kjo.2017.0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim MH, Chung TY, Chung ES. Long-term efficacy and rotational stability of AcrySof toric intraocular lens implantation in cataract surgery. Korean J Ophthalmol. 2010;24(4):207–12. 10.3341/kjo.2010.24.4.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puell MC, Pérez-Carrasco MJ, Hurtado-Ceña FJ, Álvarez-Rementería L. Disk halo size measured in individuals with monofocal versus diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2015;41(11):2417–23. 10.1016/j.jcrs.2015.04.030 [DOI] [PubMed] [Google Scholar]
- 16.Lee BS, Chang DF. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology. 2018;125(9):1325–31. 10.1016/j.ophtha.2018.02.012 [DOI] [PubMed] [Google Scholar]
- 17.Jung NY, Lim DH, Hwang SS, Hyun J, Chung TY. Comparison of clinical outcomes of toric intraocular lens, Precizon vs Tecnis: a single center randomized controlled trial. BMC Ophthalmol. 2018;18(1):292. 10.1186/s12886-018-0955-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kramer BA, Hardten DR, Berdahl JP. Rotation characteristics of three toric monofocal intraocular lenses. Clin Ophthalmol. 2020;14:4379–84. 10.2147/OPTH.S285818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oshika T, Fujita Y, Hirota A, et al. Comparison of incidence of repositioning surgery to correct misalignment with three toric intraocular lenses. Eur J Ophthalmol. 2020;30(4):680–4. 10.1177/1120672119834469 [DOI] [PubMed] [Google Scholar]
- 20.Lee BS, Onishi AC, Chang DF. Comparison of rotational stability and repositioning rates of 2 presbyopia-correcting and 2 monofocal toric intraocular lenses. J Cataract Refract Surg. 2021;47(5):622–6. 10.1097/j.jcrs.0000000000000497 [DOI] [PubMed] [Google Scholar]
- 21.Quesada GA, Quesada RA, Jones JJ, et al. Reproducibility of the magnitude of lens rotation following implantation of a toric intraocular lens with modified haptics. Clin Ophthalmol. 2022;16:3213–24. 10.2147/OPTH.S373976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeilinger J, Hienert J, Ruiss M, Pilwachs C, Findl O. Rotational stability of a new toric intraocular lens with an advanced optical profile. J Cataract Refract Surg. 2023;49(6):584–8. 10.1097/j.jcrs.0000000000001158 [DOI] [PubMed] [Google Scholar]
- 23.Chang DH, Hu J, Miller KM, Vilupuru S, Zhao W. Post-market evaluation of rotational stability and visual performance of a new toric intraocular lens with frosted haptics. Clin Ophthalmol. 2022;16:4055–64. 10.2147/OPTH.S389304 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.