Abstract
Background
This case report documents the first worldwide use of the Hybrid System from Spectrum Medical in a heart transplant procedure, focusing on its safety and efficacy. Traditional cardiopulmonary bypass systems often use an open reservoir, which increases the blood’s exposure to air, thereby heightening the risk of an inflammatory response and gas embolism. In contrast, the Hybrid System is designed to improve surgical outcomes by significantly reducing the blood-air interface. This system utilizes a dual-chamber cardiotomy-venous reservoir with a collapsible soft bag, effectively minimizing blood contact with air and foreign materials. However, it is important to note that there is currently no evidence supporting the use of this methodology specifically in heart transplants.
Case presentation
A 41-year-old male managed with a left ventricular assist device because of dilated cardiomyopathy underwent a heart transplant using the Hybrid System. The perioperative and postoperative data provided evidence of the system’s effectiveness. The selection of this patient was due to the absence of significant comorbidities unrelated to his primary cardiac condition, making him an ideal candidate to evaluate the system’s performance.
Conclusion
The Hybrid System is safe and efficient. The successful implementation in this case highlights its advantages over traditional cardiopulmonary bypass systems, suggesting a promising future in cardiac surgery. Further studies with routine cardiac surgery patients are required to validate these findings.
Keywords: Heart transplant, Cardiac surgery, Hybrid system, Inflammatory response, Gas micro-emboli
Introduction
Heart transplantation remains the gold standard treatment for end-stage heart failure, offering significant improvements in survival and quality of life. However, the procedure’s complexity necessitates the use of advanced perfusion technologies to mitigate risks and enhance outcomes, particularly concerning end-organ protection [1, 2]. The Hybrid System incorporates a dual-chamber cardiotomy-venous reservoir with a collapsible soft bag, offering several advantages over traditional hard-shell systems used in cardiopulmonary bypass (CPB), and a hypobaric oxygenator with a negative vacuum line, offering better oxygenation over standard hyperbaric oxygenators [3, 4]. This report describes the innovative application of the Hybrid System from Spectrum Medical in a heart transplant, emphasizing its unique design features intended to reduce blood-air interaction and inflammatory response and to eliminate all gas bubbles from the blood through negative vacuum.
Patient information
A 41-year-old male with a history of dilated cardiomyopathy was referred for heart transplantation. The patient had been managed with a left ventricular assist device (LVAD) HeartMate 3 (Abbott) since september 2018, highlighting the chronic and severe nature of his cardiac condition. His preoperative physical characteristics included a height of 180 cm, weight of 89 kg, body surface area of 2.09 m², and a body mass index of 27.47. The patient’s medical history was notable for the absence of significant comorbidities unrelated to his cardiomyopathy, such as diabetes or chronic kidney disease, making him an ideal candidate for this novel perfusion approach. (Table 1).
Table 1.
Preoperative and Perioperative Technical data
| Patient Characteristics | Value |
|---|---|
| Sex | Male |
| Age (years) | 41 |
| Procedure | Heart Transplant |
| Patology | Hyperthrophie cardiomyopathy with VAD |
| Weight (Kg) | 89 |
| Height (Cm) | 180 |
| Body Surface Area (m2) | 2,09 |
| Cardiopulmonary Bypass Procedure | Value |
| Calculated Blood Flow (l/min) | 5,06 |
| Bypass Time (min) | 176 |
| Cross Clamp Time (min) | 91 |
| Priming Volume (ml) | 1000 |
| Hemofiltration (ml) | 600 |
| Drainage volume (ml) | 1200 |
| Cardioplegia Solution | Del Nido |
Diagnostic assessment
The patient underwent comprehensive preoperative evaluations, including cardiac imaging and laboratory tests, to confirm the suitability for heart transplantation and to plan the use of the Hybrid System during the procedure.
Ethics
The patient has given informed consent to this clinical report. The case report was performed according to the Helsinki Declaration of Human Rights. The case report was approved by the Regional Ethics Review Board at Kosuyolu High Specialization Education and Research Hospital, Istanbul, Türkiye.
Therapeutic intervention
Premedication, induction and maintenance of anaesthesia was standardised as per the hospital protocol. Before cannulation, heparin was administered IV with a targeted activated clotting time (ACT) of 400 s,, which is within the lower range of acceptable values for this novel system (in relation toi the reduction of air blood interface) but may need adjustment in future cases based on broader clinical experience, A. Bauer et al. showed in literature in the context of the minimal invasive extracorporeal that ACT level of 300 s can be safely applied without thromboembolic complications [5]. The surgical procedure was performed using the standard technique for aortic cannula placed in the ascending aorta before the brachiocephalic artery and bicaval cannulae inserted in the inferior vena and superior vena cava The extracorporeal circuit was primed with 1000 mL of Ringer solution and 200 mL of Mannitol. The total CPB time was 176 min, the aortic cross-clamp time was 91 min (Table 1) and the perioperative data were reported in (Tables 2 and 3).
Table 2.
Monitoring parameters during cardiopulmonary bypass
| Parameter | Mean Value |
|---|---|
| Pump Flow (L/min) | 5.35 |
| Pressure Outlet (mmHg) | 178.0 |
| Mean Art Pressure (mmHg) | 57.1 |
| Ven Temp (°C) | 33.3 |
| Hct (%) | 30.0 |
| PaO2 (mmHg) | 168.3 |
| PCO2 (mmHg) | 37.0 |
| Art. Sat (%) | 97.7 |
| SVO2 (%) | 80.2 |
| DO2i (mL/min/m²) | 312.1 |
| VO2i (mL/min/m²) | 90.2 |
| VCO2i (mL/min/m²) | 68.7 |
| O2 Extraction rate | 1.4 |
| Perfusion Rate (L/min/m²) | 4.9 |
Data Expression: The values for each parameter are expressed as median values
Hct: Hematocrit; PaO2: Partial Pressure of Oxygen; PCO2: Partial Pressure of Carbon Dioxide; Art. Sat: Arterial Saturation; SVO2: Mixed Venous Oxygen Saturation; DO2i: Indexed Oxygen Delivery; VO2i: Indexed Oxygen Consumption; VCO2i: Indexed Carbon Dioxide Production; O2 Extraction rate: Oxygen Extraction Rate
Table 3.
Laboratory values Trend
| Parameter | Preoperative | CPB | 6 h | 12 h | 24 h |
|---|---|---|---|---|---|
| Hemoglobin (g/ml) | 13.3 | 10.8 | 11.7 | 10.6 | 8.5 |
| Hematocrit (%) | 40.8 | 33 | 36 | 32.5 | 26.2 |
| Platelets (K/mm³) | 132 | 154 | 89 | 160 | 110 |
| Leucocyte (K/µL) | 3.29 | 5.81 | 12.2 | 10.06 | 9.67 |
| LDH (U/L) | 236 | 126 | 191 | 198 | 190 |
| Urea (mg/dL) | 27.3 | 25.7 | 26.1 | 33 | 41.8 |
| Creatinin (mg/dL) | 0.63 | 0.86 | 0.83 | 1.25 | 1.05 |
| Direct Bilb (mg/dL) | 0.37 | 0.1 | 0.18 | 1.1 | 0.15 |
| Troponin (ng/mL) | 0.003 | 0.055 | 3.255 | 1.809 | 0.99 |
| CRP (mg/L) | 0.37 | 0.32 | 3.36 | 50.29 | 162 |
| Pro-BNP (pg/mL) | 41 | 17 | 42 | 111 | 125 |
| Haptoglobin (mg/dL) | 100 | 69 | 8 | 22.4 | 53.8 |
| Lactate (mmol/L) | 2.1 | 2.3 | 5.8 | 3.3 | 2.7 |
| pH | 7.44 | 7.32 | 7.34 | 7.35 | 7.44 |
| PaO2 (mmHg) | 487 | 252 | 173 | 162 | 114 |
| PCO2 (mmHg) | 37.4 | 36.7 | 34 | 34 | 33.6 |
| Red Blood Cells (Unit) | 0 | 0 | 0 | 0 | 1 |
Data Expression: The values for each parameter are expressed as median values
CPB: Cardiopulmonary Bypass LDH: Lactate Dehydrogenase, CRP: C-Reactive Protein, Pro-BNP: Pro-B-Type Natriuretic Peptide; PaO2: Partial Pressure of Oxygen; PCO2: Partial Pressure of Carbon Dioxide
Hybrid system components
The Hybrid System from Spectrum Medical was employed for its advanced features designed to enhance patient outcomes:
-
Hybrid Venous Reservoir: This system includes a dual chamber for managing blood suction and a collapsible soft bag to minimize blood contact with foreign materials and reduce air exposure (Fig. 1).
- Dual Chamber: Separates vented and suctioned blood, allowing for more efficient management.
Oxygenator: Spectrum Medical VT200, providing efficient oxygenation throughout the procedure.
Heat Exchanger: Quantum Standard Heat Exchanger High Flow 3/8, ensuring precise thermal control.
Perfusion System: Quantum perfusion system, delivering reliable and consistent blood flow, with online continuous blood measurement, with all the physiological indices, all data collected through the VIPER (Perfusion Record) (Fig. 2) (Table 2).
Ventilation Module: Quantum ventilation module, supporting optimal gas blending, the management of Vacuum, providing atmospheric and hypobaric ventilation.
Fig. 1.

Features of the Hybrid Cardiotomy-Venous Reservoir
Fig. 2.
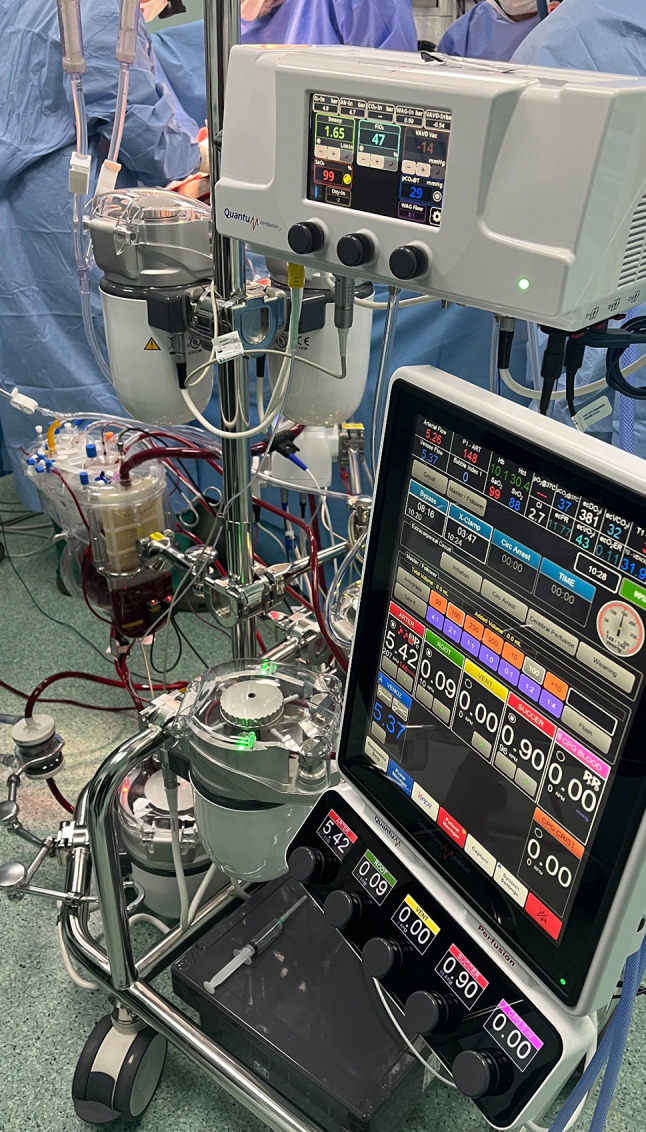
Use of the Hybrid Reservoir in the Operating Room with the Quantum Heart-Lung Machine
Follow-up and outcomes
The patient was extubated after 78 h of mechanical ventilation as cautional approach in relation to the the clinical and adaptive conditions (in relation to pulmonary artery catheter (PAC) parameters cardiac index and Pulmonary Vascular Resistance) of the new transplanted heart on the patient, no alteration in the myocardial biopsy was found. His intensive care unit stay lasted 8 days, during which he showed steady improvement with no signs of neurological deficits or serious complications and without alteration on laboratory tests (Table 3). The total hospital stay was 20 days, reflecting a smooth postoperative recovery. No adverse events or significant inflammatory responses for C-reactive protein (CRP) were observed, underscoring the safety and efficacy of the Hybrid System. However, further investigation ans samples are needed optimizing the system’s protocols of the Hybrid System.
Discussion
The Hybrid system’s design, featuring a dual chamber and collapsible soft bag, the perspective of this system is the reduce the blood-air interface and exposure to foreign materials, which are critical factors in managing the inflammatory response during CPB, this case report is the first one reported in literature, about the Hybrid system clinical use. This approach open new perspective in complex cardiac surgery procedures and scenarios which could be difficult to address in terms of practical reproducibility with the minimal invasive extracorporeal circulation (MiECC) use. C-reactive protein (CRP), play a crucial role in evaluating the patient’s response to CPB systems [1, 2]. Eisenberg MS et al. in their article presented that elevated levels of plasma CRP have been associated with decreased graft survival in cardiac transplant recipients [10]. Our experience with cardiac transplant cases using conventional CPB systems indicates that median CRP levels typically peak on the first and second postoperative days (259 and 270 mg/dL, respectively). In this case report, CRP levels peaked at 162 mg/dL. This reduction in inflammatory marker is critical, as it correlates with improved clinical outcomes and reduced complication rates. The Hybrid System’s innovative design could play a crucial role in managing systemic inflammatory response syndrome (SIRS), a common complication in patients undergoing CPB. SIRS is characterized by widespread inflammation that can lead to multiple organ dysfunction and increased morbidity [5, 6]. One of the primary triggers of SIRS during CPB is the exposure of blood to foreign surfaces and air, which activates the body’s inflammatory pathways [7, 8]. By incorporating a dual chamber and collapsible soft bag, the Hybrid System significantly reduces the blood-air interface and the exposure to foreign materials [9]. This reduction in inflammatory response can be particularly beneficial in heart transplant patients, who are already at high risk for complications due to the extensive nature of the surgery and the immunosuppressive therapy required post-transplant [10, 11]. The role of IL-6 as the major regulator of acute-phase protein synthesis, including CRP, has been extensively studied. For instance, Castell et al. (1989) demonstrated that IL-6 is the primary cytokine responsible for inducing CRP production in adult human hepatocytes [12]. However, no inflammatory markers were measured and compared in this case report, limiting the strength of this conclusion. Future studies should include such data to validate these findings. Micro-bubble embolization is another critical concern during CPB, especially in heart transplant procedures where the heart is resected, leaving all inflows and outflows open to air. Micro-bubbles can enter the bloodstream during surgery, potentially leading to embolic events that can cause neurological damage, myocardial injury, or other serious complications [4]. The Hybrid System addresses this risk through its efficient air removal capabilities. The system’s design allows for precise volume control and effective management of vented and suctioned blood, significantly reducing the incidence of micro-bubble formation. By minimizing micro-bubble embolization, the Hybrid System enhances patient safety and could contributes to better neurological outcomes post-surgery. This feature is particularly crucial in heart transplantation, where maintaining optimal cerebral perfusion and minimizing embolic risks are essential for successful recovery. In addition to the innovative design features of the Hybrid System, we used in this case report the hypobaric oxygenator. The Hypobaric Oxygenation (HBO) therapy involves the administration of oxygen at lower than atmospheric pressures, which enhances the body’s oxygenation without the risks associated with high-pressure environments [4, 5]. Hypobaric conditions can improve tissue oxygenation, promote better gas exchange, and reduce inflammation. Importantly, the hypobaric oxygenator is highly effective in eliminating gaseous micro-emboli, which are a significant risk factor during CPB and particularly in heart transplant procedures [5]. The reduced pressure environment helps in the dissolution and removal of micro-bubbles from the blood, thereby decreasing the risk of embolic events that can cause neurological and other systemic complications [11]. By eliminating gaseous micro-embolic activity, the hypobaric oxygenator significantly enhances patient safety and clinical outcomes. The dual benefits of managing SIRS and reducing micro-bubble embolization make the Hybrid System, along with the hypobaric oxygenator, valuable assets in complex cardiac surgeries. Their adoption could represent a significant step forward in the evolution of CPB technology, offering a safer and more efficient option for managing the unique challenges of these surgeries. Study limitations, this case report is limited by its single-case design. Future research should involve larger patient cohorts and include comprehensive data on inflammatory markers, pump data and other data and comparisons with standard heart-lung machines and circuits.
Conclusion
The initial application of the Hybrid System and Hypobaric Oxygenator in this heart transplant case demonstrated its potential to enhance safety and efficacy without iatrogenic complications in complex cardiac surgeries. Further research, including case series and clinical trials, is recommended to validate these findings in relation to inflammation and patient outcomes correlations and expand the use of this innovative system in broader cardiac surgical applications.
Acknowledgements
We acknowledge the support of the surgical team and the patient’s family for their cooperation and trust.
Abbreviations
- CPB
Cardiopulmonary Bypass
- LVAD
Left Ventricular Assist Device
- SIRS
Systemic Inflammatory Response Syndrome
- HBO
Hypobaric Oxygenation
- CRP
C-reactive protein
Author contributions
KK and MA participated in manuscript writing, revision and conception. OA participated in conception and manuscript vision. MEG and SA participated in support and conception. All authors read and approved the final manuscript.
Funding
No specific funding was received for this case report.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Ethical approval was obtained for this study, and informed consent was acquired from the patient.
Consent for publication
The patient provided consent for the publication of this case report.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Velho TR, Pereira RM, Guerra NC, Ferreira R, Pedroso D, Neves-Costa A, Nobre Â, Moita LF. The impact of cardiopulmonary bypass time on the sequential organ failure Assessment score after cardiac surgery. Interdiscip Cardiovasc Thorac Surg. 2024;38(5). 10.1093/icvts/ivae082. [DOI] [PMC free article] [PubMed]
- 2.Condello I, Santarpino G, Nasso G, Fiore F, Moscarelli M, Mastroroberto P, Speziale G. Air, inflammation and biocompatibility of the extracorporeal circuits. Perfusion. 2021;36(8):781–5. 10.1177/0267659120968364. 10.1177/0267659120968364 [DOI] [PubMed] [Google Scholar]
- 3.Sibel Aydin D, Cekmecelioglu S, Celik I, Yerli. Kaan Kirali the effect of vacuum-assisted venous drainage on hemolysis during cardiopulmonary bypass. Am J Cardiovasc Dis. 2020;10(4):473–8. PMID: 33224598. [PMC free article] [PubMed] [Google Scholar]
- 4.Stehouwer MC, de Vroege R, Bruggemans EF, Hofman FN, Molenaar MA, van OeverenW BA, Bruins P. The influence of gaseous microemboli on various biomarkers after minimized cardiopulmonary bypass. Perfusion. 2020;35(3):202–8. 10.1177/0267659119867572. 10.1177/0267659119867572 [DOI] [PubMed] [Google Scholar]
- 5.Bauer A, Hausmann H, Schaarschmidt J, et al. Is 300 seconds ACT safe and efficient during MiECC procedures? Thorac Cardiovasc Surg. 2019;67(3):191–202. 10.1055/s-0037-1609019. 10.1055/s-0037-1609019 [DOI] [PubMed] [Google Scholar]
- 6.Elwatidy A, et al. Comparison of miniaturized and conventional cardiopulmonary bypass circuits regarding inflammatory response and clinical outcomes: a systematic review and meta-analysis. Perfusion. 2020;35(4):323–33.31608760 [Google Scholar]
- 7.Murphy GJ, et al. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116(22):2544–52. 10.1161/CIRCULATIONAHA.107.698977 [DOI] [PubMed] [Google Scholar]
- 8.Karkouti K, et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation. 2009;119(4):495–502. 10.1161/CIRCULATIONAHA.108.786913 [DOI] [PubMed] [Google Scholar]
- 9.Cardiopulmonary Bypass Advances in Extracorporeal Life Support, 1st Edition - November 30, 2022, Editors: Kaan Kırali, Joseph S, Coselli. Afksendiyos Kalangos, Paperback ISBN: 9780443189180.
- 10.Eisenberg MS, Chen HJ, Warshofsky MK, et al. Elevated levels of plasma C-reactive protein are associated with decreased graft survival in cardiac transplant recipients. Circulation. 2000;102(17):2100–4. 10.1161/01.cir.102.17.2100. 10.1161/01.cir.102.17.2100 [DOI] [PubMed] [Google Scholar]
- 11.Chotimol P, Lansdowne W, Machin D, Binas K, Angelini GD, Gibbison B. Hypobaric type oxygenators – physics and physiology. Perfusion. 2024;0(0). 10.1177/02676591241232824. [DOI] [PubMed]
- 12.Castell JV, Gómez-Lechón MJ, David M, et al. Interleukin-6 is the major regulator of acute phase protein synthesis in adult human hepatocytes. FEBS Lett. 1989;242(2):237–9. 10.1016/0014-5793(89)80476-4. 10.1016/0014-5793(89)80476-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


