Abstract
The vast majority of gastric cancer (GC) cases are adenocarcinomas including intestinal and diffuse GC. The incidence of diffuse GC, often associated with poor overall survival, has constantly increased in Western countries. Epidemiological studies have reported increased mortality from GC after occupational exposure to pro-carcinogens that are metabolically activated by cytochrome P450 enzymes through aryl hydrocarbon receptor (AhR). However, little is known about the role of AhR and environmental AhR ligands in diffuse GC as compared to intestinal GC in Western patients. In a cohort of 29, we demonstrated a significant increase in AhR protein and mRNA expression levels in GCs independently of their subtypes and clinical parameters. AhR and RHOA mRNA expression were correlated in diffuse GC. Further, our study aimed to characterize in GC how AhR and the AhR-related genes cytochrome P450 1A1 (CYP1A1) and P450 1B1 (CYP1B1) affect the mRNA expression of a panel of genes involved in cancer development and progression. In diffuse GC, CYP1A1 expression correlated with genes involved in IGF signaling, epithelial–mesenchymal transition (Vimentin), and migration (MMP2). Using the poorly differentiated KATO III epithelial cell line, two well-known AhR pollutant ligands, namely 2-3-7-8 tetrachlorodibenzo-p-dioxin (TCDD) and benzo[a]pyrene (BaP), strongly increased the expression of CYP1A1 and Interleukin1β (IL1B), and to a lesser extend UGT1, NQO1, and AhR Repressor (AhRR). Moreover, the increased expression of CYP1B1 was seen in diffuse GC, and IHC staining indicated that CYP1B1 is mainly expressed in stromal cells. TCDD treatment increased CYP1B1 expression in KATO III cells, although at lower levels as compared to CYP1A1. In intestinal GC, CYP1B1 expression is inversely correlated with several cancer-related genes such as IDO1, a gene involved in the early steps of tryptophan metabolism that contributes to the endogenous AhR ligand kynurenine expression. Altogether, our data provide evidence for a major role of AhR in GC, as an environmental xenobiotic receptor, through different mechanisms and pathways in diffuse and intestinal GC. Our results support the continued efforts to clarify the identity of exogenous AhR ligands in diffuse GC in order to define new therapeutic strategies.
Keywords: gastric cancers; aryl hydrocarbon receptor (AhR); diffuse gastric subtype; intestinal gastric subtype; benzo[a]pyrene (BaP); 2,3,7,8-tetrachlorodibenzeno-p-dioxin (TCDD or dioxin); xenobiotic metabolism; tryptophan metabolism
1. Introduction
GC still remains the fifth leading cause of cancer mortality [1,2,3], with high heterogeneity in different subtypes according to the classification proposed by the World Health Organization [4]. Regardless of the country, the majority of gastric tumors are adenocarcinomas, which can be more histologically classified into diffuse and intestinal subtypes according to the Lauren classification [5]. While intestinal-type GC is well differentiated and related to Helicobacter pylori infection, the diffuse GC is poorly differentiated, and can be seen in familial (germline mutation in the E-Cadherin (CDH1) gene) or sporadic settings as an infiltrating and scattered type [6,7] with unknown origin. The prevalence of the diffuse type is increasing worldwide, especially in Western countries [8]. The majority of patients with diffuse GC are usually diagnosed at advanced stages with positive axillary nodes (83%) and peritoneal carcinomatosis (18.6%) [6,9,10].
The hypothesis of a link between exposure to persistent organic pollutants (POPs, including dioxin) and cancers, including GC, is supported by several epidemiological studies of accidentally exposed populations in Seveso [11]. Moreover, it is known that polycyclic polyhalogenated hydrocarbons, like dioxins and polychlorobyphenyls (PCBs) and polycyclic aromatic hydrocarbons (PAHs) (including benzo[a]pyrene from tobacco-smoke and biomass burning), are linked to relatively high health risk including cancers. We have previously shown that environmental chemicals, such as POPs are involved in breast cancers [12], and may accumulate in the Omentum adipose tissue of patients with GC [13]. In addition to TCDD, the prototypical and most potent known environmental ligand in animals and humans, other widespread environmental POP contaminants bind AhR, a basic helix-loop-helix transcription factor, with strong affinities [14,15] and may chronically activate AhR in cancer progression.
For decades, AhR has been studied for its role in environmental chemical toxicity and as a mediator of the unintended consequences of human pollution. AhR is a regulator of xenobiotic metabolic enzymes such as CYP1A1 and CYP1B1 [16]. Further, AhR participates in important cellular and pathological processes, including proliferation, migration, angiogenesis, the control of the immune system, and tumor initiation and progression [12,15,17,18,19,20,21,22,23]. Animal experimental data have provided substantial support for an association between AhR and GCs [23,24,25,26,27,28]. Transgenic mice expressing a constitutively active dioxin/AhR mutant (CA-AhR) due to a deletion in the ligand-binding domain of AhR rapidly developed stomach cancers [24,25]. Several tissues of CA-AhR mice have shown the life-long continuous low-level activity of AhR, and this model is useful to mimic the dioxin exposure of humans in the general population [26]. Mice exposed to the chemical carcinogen BaP [27] also developed gastric tumors. There is evidence for elevated AhR expression in human GC [28,29]. However, the expression levels of AhR and AhR-related signaling pathways have not been investigated in Western patients with diffuse GCs.
In this study, we have analyzed the expression of AhR in a series of diffuse and intestinal gastric tumors, as well as the expression of xenobiotic metabolic enzymes such as cytochromes P450 (CYP1A1 and CYP1B1) and a large panel of genes known to be regulated by AhR in several cancers. The impact of exogenous environmental POPs known as AhR ligands on AhR and AhR-related gene expression was also evaluated in vitro in two GC-derived cell lines.
2. Materials and Methods
2.1. Patients and Tissue Samples
A total of 29 patients underwent partial gastrectomy for histopathologically confirmed gastric adenocarcinoma primary tumor tissue in the Lariboisiere Hospital (Paris, France) from 2005 to 2014. All the patients provided written informed consent prior to their inclusion in the study. Biopsies (provided before 2014) were taken for diagnostic and research purposes, and analysis was permitted by the Ethical Committee of Lariboisiere Hospital (Paris). Eligibility criteria included (1) gastric carcinoma identified by histopathological examination, (2) no other malignancy, (3) no pre-operative chemotherapy or radiotherapy, and (4) the availability of complete clinical, histological, and biological data. Normal (non-malignant) samples refer to the samples harvested from the stomach from sites distant from the tumor. Immediately after surgery, fresh gastric tumors and their matched normal mucosa were stored in liquid nitrogen until mRNA extraction; other tumor samples and their adjacent normal tissues were routinely fixed in 10% buffered formalin and embedded in paraffin for histological analysis. As previously described [10], the population was divided into two groups according to the histological status of GC: diffuse adenocarcinoma (a poorly differentiated, infiltrating, and scattered type) or intestinal adenocarcinoma (a well-differentiated and clustered subtype) according to the Lauren classification (see Table 1). The malignancy of infiltrating carcinomas was scored according to the TNM staging system (stages I to IV) as previously described [10]: first, according to American Joint Committee on Cancer (AJCC) 7 [30], revised from International Gastric Cancer Association [31,32] and AJCC 8 [33]. This TNM staging includes T scores for the primary tumor (T1–T4), N scores (lymph node metastasis), and M scores (metastasis). The clinicopathological characteristics of the 29 patients were already reported in reference [29].
Table 1.
Clinicopathological characteristics of gastric carcinoma patients accordingly with histopathological subtype.
| Total GC (n = 29) | Diffuse/Poorly Cohesive GC * (n = 13) (45%) | Intestinal-Subtype GC ** (n = 16) (55%) |
p Value a | |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Male | 13/29 | 6/13 (46%) | 7/16 (43%) | 0.90 (NS) |
| Female | 16/29 | 7/13 (54%) | 9/16 (56%) | |
| Age (years, median) | 63 ± 17 | 57 (27–71) | 75 (59–82) | 0.0004 b |
| Smoking | ||||
| Negative | 12/22 | 4/12 | 8/12 | 0.77 (NS) |
| Positive | 10/22 | 3/10 | 7/10 | |
| Tumor size (mm), n (%) | ||||
| <50 | 10/27 | 4/11 (36%) | 6/16 (37%) | 0.10 (NS) b |
| ≥50 | 17/27 | 7/11 (64%) | 10/16 (63%) | 0.95 (NS) |
| Depth tumor invasion (T) | ||||
| T1–T2 | 6/29 | 2/13 (15%) | 4/16 (33%) | 0.5 (NS) |
| T3–T4 | 23/29 | 11/13 (85%) | 12/16 (67%) | |
| Lymphatic invasion (N) | ||||
| Negative | 11/28 | 1/13 (7%) | 10/15 (67%) | 0.0014 |
| Positive | 17/28 | 12/13 (92%) | 5/15 (33%) | |
| Metastasis (M), n (%) | ||||
| Negative | 24/29 | 9/13 (69%) | 15/16 (94%) | 0.14 (NS) |
| Positive | 5/29 | 4/13 (31%) | 1/16 (6%) | |
| TNM status | ||||
| I–II | 16/29 | 5/13 (38.5%) | 11/16 (69%) | 0.10 (NS) |
| III–IV | 13/29 | 8/13 (61.5%) | 5/16 (31%) | |
| Vascular invasion, n + (%) | ||||
| Negative | 9/29 | 3/13 (23%) | 6/16 (38%) | 0.67 (NS) |
| Positive | 20/29 | 10/13 (77%) | 10/16 (62%) | |
| Neural invasion, n (%) | ||||
| Negative | 23/29 | 2/13 (15%) | 4/16 (25%) | 0.66 (NS) |
| Positive | 6/29 | 11/13 (68%) | 12/16 (75%) |
* poorly cohesive adenocarcinoma/diffuse-type carcinoma; ** intestinal-type adenocarcinoma. a, Chi-square test, Yates’ continuity corrected chi-square test, or Fisher’s exact test if appropriate; b, Mann–Whitney. NS = not statistically different. The characteristics of the patients included in the cohort were already reported in ref. [29].
2.2. Total RNA Preparation and qRT-PCR
Total RNA extraction, complementary cDNA synthesis, and qRT-PCR conditions were as previously described [12,34]. Primers for AhR, AhRR, and other genes were selected using the Oligo 6.0 program (National Biosciences, Plymouth, MN) [12,29]. Each sample was normalized on the basis of its TBP content as previously described [10,12]. The results, expressed as N-fold difference in target gene expression relative to the TBP gene (and termed “Ntarget”), were determined as Ntarget = 2ΔCtsample, where the ΔCt value of the sample was determined by subtracting the average Ct value of the specific target gene from the average Ct value of the TBP gene. The Ntarget values of the samples were subsequently normalized so that the median of the Ntarget values for normal gastric tissues (n = 11) was 1. Target gene expression was normalized to their transcription level of house-keeping genes TATA-Box Binding Protein (TBP), Po, and Peptidylprolyl Isomerase A (PPIA). The preliminary analysis of gene expression did not indicate changes in the median basal levels in normal samples in the same patients (with either diffuse or intestinal GC). For each gene expression, the normalized RNA values of 3 (or more) were considered to represent gene overexpression in tumor samples, and values 0.33 (or less) represented gene under expression.
2.3. Immunohistochemistry
Immunohistochemical staining (IHC) was performed on paraffin sections (4 μm) as previously described [12,29]. Immunohistochemical staining for AhR (Santa Cruz Biotechnology, Dallas, TX, USA, H-211, sc-5579, dilution 1/50) and CYP1B1 (Santa Cruz Biotechnology, H-105, sc-32882, dilution 1/200) was performed using the Ventana Autostainer (Export, PA, USA). Specificity was checked by control staining performed in the absence of primary antibodies and with positive tissue [12]. The antigen–antibody complex was visualized using DAB as the chromogen. Immunostaining was analyzed blindly in duplicate by two specialists including a certified pathologist.
2.4. Cell Culture
The two human gastric cell lines were obtained from ATCC (Manassas, VA, USA). KATO-III is derived from a poorly differentiated gastric adenocarcinoma, and AGS from moderately differentiated GC were acquired from ATCC (Manassas, VA, USA). The cells were grown in Dulbecco’s modified Eagle medium supplemented with 10% heat-inactivated fetal bovine serum, 0.5% penicillin-streptomycin, and 2 nM of L-glutamine (Gibco, Saint Aubin, France at 37 °C in a humidified 5% CO2/95% air atmosphere. Exponentially growing cells were trypsinized and seeded in flasks; the medium was replaced every 24 h; when cells reached 70–80% of confluence as evaluated by microscopic examination, the medium was changed, and either TCDD (1–30 nM) or BaP (10 μM) (gift from P Balaguer, Montpellier, France) was added for 16 h to 24 h. Control experiments included the addition of CHH 223191 (10 μM), a full AhR antagonist (a gift from P Balaguer, Montpellier, France).
2.5. Statistical Analysis
As mRNA expression levels did not fit a Gaussian distribution, the relative expression of genes was characterized by the median and the range rather than by their mean values and coefficient of variation [10,12,29]. For each gene, the differences in expression between tumors versus normal tissues (fold change) were analyzed as previously described [10,12]. Differences in the number of samples that over- (>3-fold) or under- (<3-fold) expressed were analyzed using the Chi2-square test [29]. The relationships between the expressions of genes in GC were determined using non parametric Spearman’s rank correlation test. Relationships between the expression levels and clinical parameters were analyzed using non parametric Kruskal–Wallis (or Mann–Whitney) and Chi-square tests, as indicated in each Table. Statistical analyses were performed using the Prism 5.03 software (GraphPad, San Diego, CA, USA). The differences were considered significant at confidence levels greater than 95% (p < 0.05).
3. Results
3.1. Patient Characteristics
The clinical characteristics of the patients are shown in Table 1. The patients with diffuse GC were younger than the patients with intestinal GC (n = 57, 27–71 years and n = 75, 59–82 years, respectively, p = 0.0004). Both subtypes of carcinoma had large tumors (>50 mm) and tumor invasion (T3–T4) [10]. Within each subtype, half of the patients smoked. The patients with diffuse adenocarcinoma had more lymphatic invasion (p = 0.0014) and metastasis (31% vs. 6%) than the patients with intestinal GC. Most diffuse GC had a TNM stage III–IV, while the patients with intestinal GC were stage I, II, and III. Vascular and neural invasion did not differ among different GC subtypes.
3.2. High AhR Expression in Gastric Tumors Both at the mRNA and Protein Levels
The cohort of GC specimens was first used to assess AhR mRNA expression levels. As compared to the normal gastric tissue samples, AhR expression was significantly increased in gastric tumors (×1.94, p = 0.002), both diffuse and intestinal GC (×2.12, p = 0.001 and ×1.60, p = 0.003, respectively) (Table 2). Moreover, AhR mRNA expression was independent of classical clinical parameters, i.e., gender, age, tumor grade, lymphatic invasion, metastasis status, TNM stage, vascular or neural invasion, and the GC subtype (Supplementary Table S1).
Table 2.
Statistical analysis of mRNA expression levels of AhR, CYP1B1, CYP1A1, and AhRR in gastric cancers (all GC, diffuse and intestinal subtypes).
| Genes | Nontumoral Gastric Tissues (n = 11) | All Tumors (n = 29) | p Value a | Diffuse GC vs. PT (n = 13) |
p Value a | Intestinal GC vs. PT (n = 16) |
p Value a | p Value (GC Subtypes) |
|---|---|---|---|---|---|---|---|---|
| AhR and Target Genes | ||||||||
| AhR | 1 (0.37–1.64) | 1.94 (0.55–3.53) | 0.002 | 2.12 (0.55–3.35) | 0.001 | 1.60 (0.65–3.53) | 0.003 | 0.13 (NS) |
| CYP1B1 | 1 (0.52–2.90) | 1.45 (0.13–4.90) | 0.91 (NS) | 1.62 (0.43–4.90) | 0.014 | 1.22 (0.13–4.0) | 0.82 (NS) | 0.19 (NS) |
| CYP1A1 | 0 (0–5.6) | 1.37 (0–86) | 0.26 (NS) | 0.43 (0–30) | 0.73 (NS) | NS | ||
| AhRR | 1 (0.23–1.66) | 1.25 (0.19–3.93) | >0.999 (NS) | 2.65 (0.74–3.96) | 0.007 | 0.89 (0.19–3.85) | 0.88 (NS) | 0.017 |
Median (range) of gene mRNA expression levels; p value (a Mann–Whitney). Significant p value in bold. Comparative basal levels of genes in normal gastric tissue (×1) are as follows: AhR (71), CYP1A1 (0), CYP1B1 (372), and AhRR (21). NS = not statistically different. AhR expression was already reported in ref. [29].
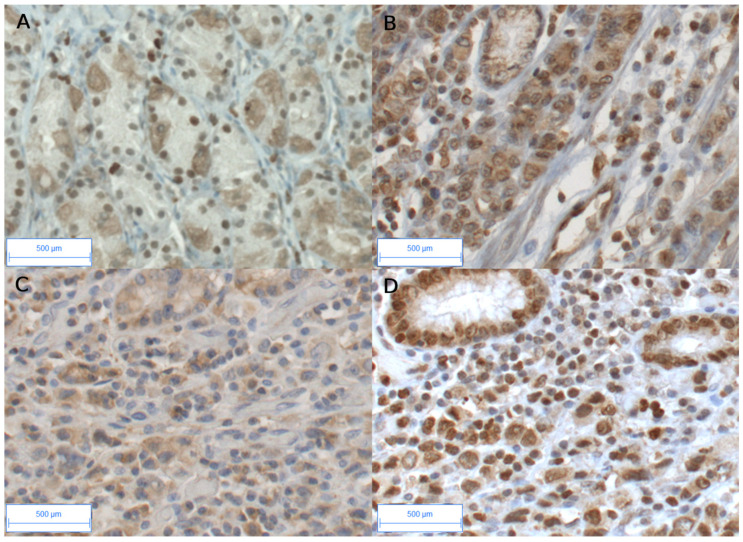
Most importantly, at the protein expression levels in GC, strong nuclear AhR staining was observed (Figure 1B,D) in epithelial and stromal cells, including fibroblasts and endothelial and immune cells [29], as compared to the weak cytoplasmic and nuclear staining observed in the epithelial cells in non-tumoral tissue (Figure 1A).
Figure 1.
Immunohistochemical staining of AhR and CYP1B1 in peritumoral and diffuse GCs. AhR in peritumoral gastric tissue (A); weak cytoplasmic and/or nuclear staining were observed in glandular tissue and stroma. In tumoral tissue (B,D), strong AhR immunostaining is observed in most cells, both epithelial and stromal compartments. CYP1B1 (C) and AhR (D) immunostaining are shown on the same tumor (diffuse GC). CYP1B1 was mainly observed in the stromal compartment in diffuse GC (C). Original magnification ×20. Bar scale, 500 μm.
Altogether, these results indicate that AhR (mRNA and protein) is significantly increased in GCs, both in diffuse and intestinal adenocarcinoma, as compared to the control samples.
3.3. Expression of AhR-Target Genes Encoding Xenobiotic Metabolizing Enzymes in Gastric Cancers
As GC expresses high AhR expression levels (mRNA and protein), we analyzed the changes in the expression of the classic target genes of AhR, such as CYP1A1 and CYP1B1, two genes involved in xenobiotic metabolism [16]. CYP1A1 was expressed at a low level in normal tissues (Table 2). As compared to the non-tumoral tissue, the enhanced expression of CYP1A1 was attained with an increase of more than 3-fold observed in 5/29 of GC cases (17%) and in 23% diffuse GC. CYP1B1 expression was significantly increased in diffuse GC (p = 0.014, 92% lymphatic invasion, Table 2 and Table 3). At the protein level, CYP1B1 was mainly observed in the stromal compartment in diffuse GC (Figure 1C). In all the tumors, CYP1B1 expression was independent of clinical parameters (gender, age, smoking, and tumor grade (T), except for an increase with lymphatic invasion (p < 0.02) and TNM (p < 0.05 respectively) (Table 3).
Table 3.
Relationship between CYP1B1, CYP1A1, and AhRR expression with clinical parameters in gastric adenocarcinomas (including sub-populations in all tumors (A) and diffuse and intestinal GC subtypes (B).
| (A) | ||||||||
| All tumors, n = 29 | ||||||||
| AhRR | CYP1B1 | CYP1A1 | ||||||
| Gender | p = 0.75 | p = 0.47 | p = 0.063 | |||||
| Male (n = 13) | 1.63 (0.29–3.96) | 1.62 (0.13–4.03) | 1.37 (0–30.1) | |||||
| Female (n = 16) | 1.18 (0.29–3.85) | 1.34 (0.32–4.9) | 0 (0–86) | |||||
| Age | p = 0.27 | p = 0.18 | p = 0.97 | |||||
| <60 years (n = 9) | 1.66 (0.74–3.96) | 1.47 (1.23–4.9) | 0.67 (0–30.1) | |||||
| >60 years(n = 20) | 1.17 (0.19–3.85) | 1.21 (0.13–4) | 0.65 (0–86) | |||||
| Smoking | p = 0.54 | p = 0.34 | p = 0.42 | |||||
| Negative (n = 12) | 1.21 (0.42–1.67) | 1.63 (0.36–4) | 0.33 (0–1.98) | |||||
| Positive (n = 10) | 1.65 (0.29–3.85) | 0.98 (0.13–5) | 0.43 (0–86) | |||||
| Tumor invasion (T) | p = 0.11 | p = 0.18 | p = 0.63 | |||||
| T1–T2 (n = 6) | 0.43 (0.19–3.5) | 0.94 (0.13–2.44) | 0.47 (0–86) | |||||
| T3–T4 (n = 23) | 1.31 (0.42–3.87) | 1.47 (0.32–4.9) | 0.67 (0–30.1) | |||||
| Lymphatic invasion | p = 0.032 | p = 0.014 | p = 0.06 | |||||
| Negative (n = 11) | 0.74 (0.19–3.85) | 0.5 (0.3–2.5) | 0 (0–1.39) | |||||
| Positive (n = 17) | 1.67 (0.42–3.96) | 1.6 (0.4–4.9) | 1 (0–86) | |||||
| Metastasis (M) | p = 0.59 | p = 0.55 | p = 0.59 | |||||
| Negative (n = 24) | 1.28 (0.19–4.0) | 1.39 (0.13–4) | 0.68 (0–86) | |||||
| Positive (n = 5) | 1.15 (0.74–2.38) | 1.45 (0.43–4.9) | 0 (0–30.1) | |||||
| TNM | p = 0.35 | p = 0.045 | p = 0.10 | |||||
| I–II (n = 16) | 1.06 (0.19–3.96) | 1.19 (0.13–3) | 0.12 (0–4.01) | |||||
| III–IV (n = 13) | 1.63 (0.42–3.66) | 1.62 (0.43–4.9) | 1.37 (0–86) | |||||
| Vascular invasion, | p = 0.09 | p = 0.39 | p = 0.45 | |||||
| Negative (n = 9) | 0.74 (0.2–4) | 1.27 (0.36–2.32) | 0.61 (0–4.01) | |||||
| Positive (n = 20) | 1.65 (0.3–3.8) | 1.54 (0.13–4.9) | 0.71 (0–86) | |||||
| Neural invasion | p = 0.38 | p = 0.41 | p = 0.38 | |||||
| Negative (n = 6) | 0.79 (0.19–3.53) | 1.76 (0.72–2.51) | 1.04 (0–86) | |||||
| Positive (n = 23) | 1.31 (0.29–3.96) | 1.4 (0.13–4.9) | 0.61 (0–30.1) | |||||
| (B) | ||||||||
| Diffuse subtype GC, n = 13 | Intestinal subtype GC, n = 16 | |||||||
| n= | AhRR | CYP1B1 | CYP1A1 | n = | AhRR | CYP1B1 | CYP1A1 | |
| Gender | p = 0.42 | p = 0.92 | p = 0.83 | p = 0.88 | p = 0.67 | p = 0.058 | ||
| Male | 6 | 2.2 (1.23–3.96) | 1.76 (1.15–2.32) | 1.38 (0–4) | 7 | 0.93 (0.29–2.38) | 1.45 (0.13–4) | 0.76 (0–30.1) |
| Female | 7 | 2.65 (0.74–3.5) | 1.47 (0.43–4.9) | 0 (0–86) | 9 | 0.85 (0.19–3.85) | 1.16 (0.32–2.5) | 0 (0–1.39) |
| Age | p = 0.27 | p = 0.49 | p = 0.16 | ND | ND | ND | ||
| <60 years | 8 | 1.64 (0.74–3.96) | 1.68 (1.23–4.9) | 0.33 (0–4) | 1 | 2.38 | 1.45 | 30.1 |
| >60 years | 5 | 3.17 (1.15–3.66) | 1.62 (0.43–2.44) | 1.51 (0–86) | 15 | 0.85 (0.19–3.85) | 1.16 (0.13–4) | 0.25 (0–3.31) |
| Smoking | p = 0.46 | p = 0.23 | p = 0.40 | p = 0.84 | p = 0.054 | p = 0.86 | ||
| Negative | 4 | 1.43 (0.74–1.66) | 1.78 (1.31–2.32) | 0.33 (0–1.37) | 8 | 1.02 (0.42–1.67) | 1.63 (0.36–4) | 0.38 (0–1.98) |
| Positive | 3 | 3.17 (0.74–3.53) | 2.44 (1.85–4.9) | 62.55 (0–86) | 7 | 0.93 (0.29–3.85) | 0.49 (0.13–3) | 0.25 (0–30.1) |
| Tumor invasion | ND | ND | ND | p = 0.002 | p = 0.055 | p = 0.36 | ||
| T1–T2 | 2 | 3.35 (3.17–3.53) | 2.14 (1.85–2.44) | 74.3 (62.5–86) | 4 | 0.31 (0.19–0.53) | 0.46 (0.13–1.2) | 0.12 (0–0.7) |
| T3–T4 | 11 | 1.66 (0.74–3.96) | 1.47 (0.43–4.9) | 0.67 (0–4) | 12 | 1.22 (0.42–3.85) | 1.52 (0.32–4) | 0.68 (0–30.1) |
| Lymphatic invasion | ND | ND | ND | p = 0.25 | p = 0.019 | p = 0.04 | ||
| Negative | 1 | 1.63 | 2.32 | 1.37 | 10 | 0.73 (0.19–3.85) | 0.52 (0.13–2.5) | 0 (0–1.39) |
| Positive | 12 | 2.7 (0.74–3.96) | 1.54 (0.43–4.9) | 1.03 (0–86) | 5 | 1.31 (0.42–2.38) | 1.59 (1.27–4) | 1 (0–30.1) |
| Metastasis | p = 0.006 | p = 0.82 | p = 0.06 | ND | ND | ND | ||
| Negative | 9 | 3.17 (1.23–3.96) | 1.62 (1.15–2.44) | 1.51 (0–86) | 15 | 0.85 (0.19–3.85) | 1.16 (0.13–4) | 0.25 (0–3.31) |
| Positive | 4 | 0.94 (0.74–1.63) | 1.86 (0.43–4.9) | 0 (0–1.37) | 1 | 2.38 | 1.45 | 30.1 |
| TNM | p = 0.50 | p = 0.68 | p = 0.83 | p = 0.22 | p = 0.038 | p = 0.097 | ||
| I–II | 5 | 2.65 (1.23–3.96) | 1.47 (1.23–2.17) | 0.67 (0–4) | 11 | 0.74 (0.19–3.85) | 0.52 (0.13–3) | 0 (0–3.31) |
| III–IV | 8 | 2.19 (0.74–3.66) | 1.73 (0.43–4.9) | 1.38 (0–86) | 5 | 1.31 (0.42–2.38) | 1.59 (1.27–4) | 1 (0–30.1) |
| Vascular invasion | p = 0.84 | p = 0.57 | p > 0.9999 | p = 0.17 | p = 0.53 | p = 0.41 | ||
| Negative | 3 | 1.63 (0.74–3.96) | 1.9 (1.4–2.32) | 1.37 (0–4) | 6 | 0.62 (0.19–1.31) | 0.94 (0.36–1.6) | 0.30 (0–1) |
| Positive | 10 | 2.70 (0.74–3.66) | 1.54 (0.43–4.9) | 1.03 (0–86) | 10 | 1.09 (0.29–3.85) | 1.56 (0.13–4) | 0.5 (0–30.1) |
| Neural invasion | ND | ND | ND | p = 0.12 | p = 0.52 | p = 0.76 | ||
| Negative | 2 | 3.35 (3.17–3.53) | 2.14 (1.85–2.44) | 74.3 (62.5–86) | 4 | 0.63 (0.19–0.85) | 1.41 (0.72–2.5) | 0.35 (0–1.39) |
| Positive | 11 | 1.66 (0.74–3.96) | 1.47 (0.43–4.9) | 0.67 (0–4) | 12 | 1.22 (0.29–3.85) | 0.89 (0.13–4) | 0.43 (0–30.1) |
Median (range) of gene mRNA expression levels; p value (Mann–Whitney). Significant p value in bold; tendency in italic. ND = not determined.
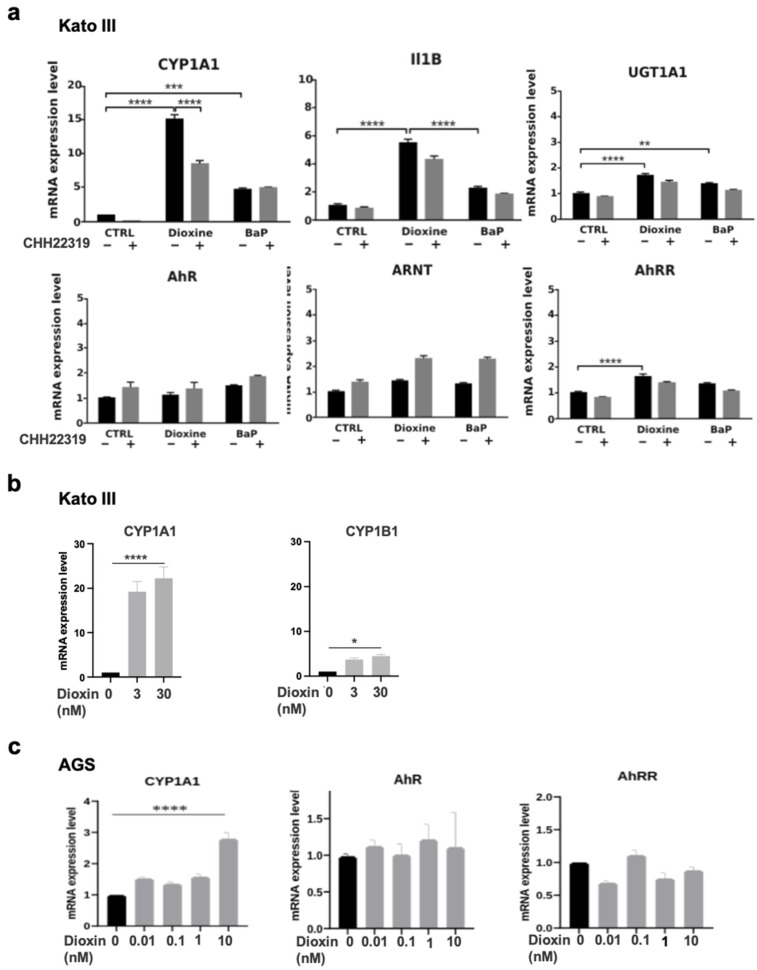
3.4. AhR Ligands Such as Environmental Ligands Induced mRNA Expression of CYP1A, IL1B, UGT1A1, and AhRR in Gastric Epithelial Cell Lines
Next, it was important to directly evaluate how exposure to POPS impacted the expression of AhR and AhR-related genes. We thus examined how TCDD, the most potent known environmental AhR ligand, and BaP impacted the mRNA expression levels of AhR and AhR-related genes in two epithelial gastric cell lines (KATO III and AGS). These cells are poorly (KATO III) and moderately (AGS) differentiated, with high AhR expression.
In the KATO III cells, TCDD (30 nM) strongly increased the expression of CYP1A1 mRNA levels as compared to untreated cells (×15, p < 0.0001) (Figure 2a). The TCDD-induced CYPA1 expression was reversed by CHH 223191, a full AhR antagonist (p < 0.001) (Figure 2a). BaP (10 μM), a well-studied pro-carcinogen, also increased CYP1A expression (×5, p < 0.001) (Figure 2a). Further, TCDD (30 nM) also significantly increased the expression of IL1B (×5.5, p < 0.0001), UDP Glucuronosyltransferase Family 1 Member A complex Locus (UGT1A), and AhRR (×2, p < 0.0001) (Figure 2a). We did not detect significant effects of TCDD (or BaP) on AhR and AhRR nuclear translocator (ARNT) expression in the KATO III cells (Figure 2a). Just as what was seen in the diffuse GC patients, the CYP1B1 expression levels were increased in the Kato III cells upon TCDD treatment, although to a lesser extent compared to what was seen for CYP1A1. (Figure 2b). Of note, the levels of CYP1B1 were low in the epithelial KATO III cells and undetectable (qPCR threshold > CT50) in the AGS cells. In AGS cells, the expression of CYP1A but not AhR or AhRR was significantly increased following the TCDD treatment (Figure 2c).
Figure 2.
mRNA expression levels of AhR and AhR-related genes in KATO III and AGS gastric cells upon treatment with either TCDD or BaP. (a) The KATO III cells were cultivated in the absence (Ctrl) or presence of either TCDD (dioxin) 30 nM or BaP (10 µM) for 16 h. The cells were incubated with (gray column) or without (black column) CHH223191 (10 μM). The expression of the indicated genes was determined by qRT-PCR. All the experiments were performed in triplicate. The results are expressed as means +/− S.E.M and normalized so that the mean of the control cells was 1. * p value < 0.005, ** p value < 0.01; *** p value < 0.001; **** p value < 0.0001. (b) The KATO III cells were cultivated in the presence or absence of dioxin at the indicated concentrations. The expression levels of CYP1A1 and CYP1B1 were determined by qRT-PCR in the same experiment. The results were expressed as in (a). (c) The AGS cells were cultivated in the absence (Ctrl in black) or presence of (dioxin) (0.01–10 nM, in gray). The expression levels of the indicated genes were determined by qRT-PCR in the same experiment. All the experiments were performed in triplicate. The results were expressed as in (a).
3.5. Correlations of Expression of AhR, CYP1A1 and CYP1B1, AhRR with a Panel of Genes Involved in AhR-Related Signaling Pathways
AhR is known to activate several signaling pathways governing proliferation, epithelial–mesenchymal transition (EMT), cell migration, inflammation, immunity, and angiogenesis in cancers [12,15,17,18,19,20,21,22,23]. We then compared the mRNA expression levels of AhR, CYP1A1, and CYP1B1 with the expression of 36 genes involved in EMT, cell proliferation and migration, immunity, and angiogenesis that we previously described in our cohort of GCs [10,29]. AhR expression was correlated with Ras Homolog Family MemberA (RHOA) expression in intestinal and diffuse GC (Table 4). In diffuse GC, CYP1A1 expression correlated with several genes such as growth factors (Insulin-Like Growth Factor 1 (IGF1), p = 0.001, and IGF Receptor (IGFR2), p = 0.015); genes involved in EMT such as Vimentin (VIM) (p = 0.007), Snail Family Transcriptional Repressor (SNAI2) and Zinc Finger E-Box Binding Homeobx 2 (ZEB2) (p = 0.04); and migration (Matrix Metallopeptidase 2 (MMP)2, p = 0.01) (Table 4). CYP1B1 expression was only inversely correlated with Erb-B2 Receptor Tyrosine Kinase 2 (ERRB2) (p = 0.01). Moreover, significantly increased AhRR expression (×2.65, p < 0.01) positively correlated with IGF1 (p = 0.0001), Twist Family BHLH Transcription Factor 2 (TWIST2), ZEB2 (p < 0.02), MMP2 (p < 0.002), and Neuropilin 1 (NRP1) (p = 0.02) in diffuse, but not intestinal GC (Table 4). In intestinal GC, the low expression of CYP1A1 and CYPB1 inversely correlated with Indoleamine 2,3-Dioxygenase 1 (IDO1) (p = 0.014 and p = 0.001, respectively, Table 4). Low CYP1B1 expression also correlated with genes that were not significantly increased including growth factors and receptors, EMT (VIM, SNAI2, and TWIST2), VEGF, and NRP1 (Table 4).
Table 4.
Correlations of the selected genes analyzed in the study in relation to AhR and “AhR-related signalling pathways” in diffuse (A) and intestinal (B) GC.
| (A) | ||||||||
| Diffuse GC | ||||||||
| Genes | AhR | AhR | AhRR | AhRR | CYP1B1 | CYP1B1 | CYP1A1 | CYP1A1 |
| r | p value | r | p value | r | p value | r | p value | |
| AhR | x | −0.031 | 0.92 | −0.066 | 0.83 | 0.181 | 0.553 | |
| AhRR | −0.031 | 0.92 | x | −0.107 | 0.73 | 0.711 | 0.007 | |
| CYP1B1 | −0.066 | 0.83 | −0.107 | 0.73 | x | 0.342 | 0.253 | |
| Growth factors and receptors (n = 10) | ||||||||
| IGF1 | 0.184 | 0.55 | 0.865 | 0.0001 | 0.155 | 0.71 | 0.846 | 0.001 |
| IGF1R | 0.596 | 0.032 | 0.267 | 0.38 | −0.159 | 0.6 | 0.345 | 0.24 |
| FGFR1 | −0.234 | 0.441 | 0.542 | 0.055 | 0.269 | 0.37 | 0.444 | 0.13 |
| FGF7 | 0 | 1 | 0.576 | 0.04 | −0.055 | 0.86 | 0.424 | 0.15 |
| IGF2 | 0.041 | 0.89 | 0.119 | 0.7 | −0.033 | 0.91 | −0.043 | 0.69 |
| IGFR2 | 0.562 | 0.046 | 0.375 | 0.21 | −0.06 | 0.84 | 0.655 | 0.015 |
| IRS1 | −0.259 | 0.39 | 0.457 | 0.12 | −0.121 | 0.69 | 0.384 | 0.19 |
| IRS2 | 0.259 | 0.39 | 0.501 | 0.08 | 0.005 | 0.99 | 0.623 | 0.02 |
| ERBB2 | 0.341 | 0.25 | 0.529 | 0.06 | −0.676 | 0.01 | 0.291 | 0.34 |
| EMT and migration (n = 10) | ||||||||
| VIM | 0.135 | 0.66 | 0.518 | 0.07 | 0.280 | 0.35 | 0.709 | 0.007 |
| CDH1 | 0.501 | 0.08 | 0.57 | 0.09 | −0.264 | 0.38 | 0.592 | 0.03 |
| SNAI1 | 0.239 | 0.43 | 0.102 | 0.74 | 0.066 | 0.83 | 0.131 | 0.67 |
| TGFB1 | 0.297 | 0.32 | 0.182 | 0.55 | −0.511 | 0.83 | −0.165 | 0.59 |
| RUNX3 | −0.771 | 0.8 | 0.202 | 0.51 | −0.313 | 0.30 | −0.065 | 0.83 |
| SNAI2 | 0.317 | 0.29 | 0.441 | 0.13 | 0.044 | 0.89 | 0.605 | 0.04 |
| TWIST2 | −0.005 | 0.99 | 0.667 | 0.013 | 0.115 | 0.71 | 0.504 | 0.08 |
| ZEB2 | 0.033 | 0.91 | 0.661 | 0.014 | −0.038 | 0.90 | 0.602 | 0.04 |
| RHOA | 0.600 | 0.034 | 0.176 | 0.56 | −0.203 | 0.50 | 0.484 | 0.09 |
| RHOB | −0.215 | 0.48 | 0.295 | 0.23 | 0.429 | 0.14 | 0.444 | 0.13 |
| Cell proliferation and migration (n = 3) | ||||||||
| Ki67 | 0.463 | 0.11 | 0.328 | 0.27 | −0.176 | 0.56 | 0.537 | 0.26 |
| MMP2 | −0.099 | 0.74 | 0.774 | 0.002 | 0.164 | 0.59 | 0.701 | 0.01 |
| MMP9 | 0.193 | 0.53 | 0.005 | 0.99 | −0.511 | 0.07 | −0.271 | 0.32 |
| Immunity (n = 5) | ||||||||
| IDO1 | 0.528 | 0.07 | −0.228 | 0.44 | −0.440 | 0.13 | −0.245 | 0.42 |
| TDO2 | 0.267 | 0.38 | 0.330 | 0.27 | −0.280 | 0.35 | 0.048 | 0.87 |
| PD1 | 0.534 | 0.06 | 0.033 | 0.92 | 0.115 | 0.71 | 0.209 | 0.49 |
| CD274 | 0.446 | 0.13 | −0.437 | 0.13 | −0.060 | 0.85 | −0.435 | 0.11 |
| PDL2 | 0.332 | 0.26 | 0.080 | 0.79 | 0.091 | 0.77 | 0.266 | 0.38 |
| Angiogenesis (n = 6) | ||||||||
| FLT1 | 0.559 | 0.047 | 0.303 | 0.31 | 0.214 | 0.48 | 0.319 | 0.29 |
| VEGF165 | 0.402 | 0.17 | 0.358 | 0.23 | 0.011 | 0.97 | 0.364 | 0.22 |
| VEGF189 | 0.306 | 0.31 | 0.088 | 0.77 | −0.137 | 0.65 | 0.114 | 0.71 |
| KDR | −0.187 | 0.54 | −0.151 | 0.62 | −0.368 | 0.22 | −0.387 | 0.19 |
| VEGFC | 0.179 | 0.56 | 0.328 | 0.27 | 0 | 1 | 0.199 | 0.51 |
| NRP1 | 0.185 | 0.55 | 0.614 | 0.02 | 0.033 | 0.91 | 0.411 | 0.16 |
| (B) | ||||||||
| Intestinal GC | ||||||||
| Genes | AhR | AhR | AhRR | AhRR | CYP1B1 | CYP1B1 | CYP1A1 | CYP1A1 |
| r | p value | r | p value | r | p value | r | p value | |
| AhR | 1 | 0.679 | 0.004 | 0.018 | 0.95 | 0.112 | 0.68 | |
| AhRR | 0.679 | 0.004 | 1 | 0.253 | 0.34 | 0.241 | 0.368 | |
| CYP1B1 | 0.018 | 0.95 | 0.253 | 0.34 | 1 | 0.655 | 0.006 | |
| Growth factors and receptors (n = 10) | ||||||||
| IGF1 | −0.113 | 0.68 | 0.168 | 0.53 | 0.765 | 0.001 | 0.371 | 0.16 |
| IGF1R | −0.053 | 0.84 | 0.077 | 0.78 | 0.667 | 0.005 | 0.521 | 0.04 |
| FGFR1 | −0.021 | 0.94 | 0.132 | 0.62 | 0.794 | <0.0001 | 0.455 | 0.08 |
| FGF7 | −0.127 | 0.64 | 0.047 | 0.86 | 0.721 | 0.002 | 0.401 | 0.12 |
| IGF2 | −0.093 | 0.73 | 0.144 | 0.59 | 0.774 | <0.0001 | 0.337 | 0.2 |
| IGFR2 | 0.169 | 0.53 | 0.018 | 0.95 | 0.524 | 0.037 | 0.364 | 0.15 |
| IRS1 | 0.056 | 0.84 | 0.471 | 0.07 | 0.915 | <0.0001 | 0.531 | 0.05 |
| IRS2 | 0.113 | 0.68 | 0.203 | 0.45 | 0.582 | 0.018 | 0.05 | 0.83 |
| ERBB2 | 0.533 | 0.03 | 0.288 | 0.28 | −0.141 | 0.602 | 0.097 | 0.72 |
| EMT and migration (n = 10) | ||||||||
| VIM | 0.186 | 0.49 | 0.132 | 0.62 | 0.812 | <0.0001 | 0.379 | 0.15 |
| CDH1 | 0.284 | 0.286 | 0.085 | 0.75 | 0.051 | 0.85 | 0.214 | 0.43 |
| SNAI1 | 0.087 | 0.75 | 0.068 | 0.8 | 0.577 | 0.02 | 0.241 | 0.37 |
| TGFB1 | 0.21 | 0.39 | −0.091 | 0.74 | 0.453 | 0.08 | 0.118 | 0.66 |
| RUNX3 | 0.195 | 0.47 | 0.081 | 0.76 | −0.199 | 0.46 | −0.071 | 0.8 |
| SNAI2 | 0.282 | 0.29 | 0.171 | 0.53 | 0.711 | 0.002 | 0.131 | 0.63 |
| TWIST2 | 0.121 | 0.66 | 0.109 | 0.69 | 0.827 | <0.0001 | 0.307 | 0.25 |
| ZEB2 | 0.133 | 0.62 | 0.242 | 0.37 | 0.477 | 0.001 | 0.462 | 0.07 |
| RHOA | 0.693 | 0.003 | 0.324 | 0.22 | −0.056 | 0.84 | 0.171 | 0.53 |
| RHOB | −0.094 | 0.73 | 0.041 | 0.88 | 0.559 | 0.02 | 0.201 | 0.45 |
| Cell proliferation and migration (n = 3) | ||||||||
| Ki67 | 0.277 | 0.3 | −0.135 | 0.61 | −0.665 | 0.006 | −0.381 | 0.1 |
| MMP2 | 0.121 | 0.65 | 0.118 | 0.66 | 0.800 | <0.0001 | 0.335 | 0.2 |
| MMP9 | 0.139 | 0.61 | 0.041 | 0.88 | 0.185 | 0.49 | 0.07 | 0.8 |
| Immunity (n = 5) | ||||||||
| IDO1 | 0.272 | 0.3 | −0.025 | 0.94 | −0.727 | 0.001 | −0.601 | 0.014 |
| TDO2 | 0.046 | 0.87 | 0.103 | 0.7 | 0.218 | 0.41 | 0.163 | 0.54 |
| PD1 | −0.155 | 0.56 | −0.132 | 0.62 | 0.056 | 0.84 | −0.261 | 0.25 |
| CD274 | 0.199 | 0.46 | 0.156 | 0.56 | −0.251 | 0.34 | −0.332 | 0.15 |
| PDL2 | −0.015 | 0.95 | −0.172 | 0.517 | 0.455 | 0.08 | −0.032 | 0.76 |
| Angiogenesis (n = 6) | ||||||||
| FLT1 | −0.407 | 0.12 | −0.394 | 0.13 | 0.032 | 0.91 | −0.176 | 0.51 |
| VEGF165 | −0.531 | 0.03 | −0.641 | 0.01 | −0.321 | 0.23 | −0.013 | 0.68 |
| VEGF189 | −0.181 | 0.51 | −0.238 | 0.37 | −0.156 | 0.56 | −0.046 | 0.86 |
| KDR | −0.081 | 0.77 | −0.079 | 0.77 | 0.482 | 0.06 | 0.061 | 0.82 |
| VEGFC | 0.01 | 0.88 | 0.132 | 0.63 | 0.788 | 0.0001 | 0.353 | 0.18 |
| NRP1 | 0.131 | 0.62 | 0.168 | 0.53 | 0.838 | <0.0001 | 0.324 | 0.22 |
r, Spearman’s rank test (relationship between two quantitative parameters). Values in bold type are statistically significant at confidence level greater than 99% (p value < 0.01) and r > 0.6. CYP1B1 and AhRR were not significantly increased in intestinal GC and statistical correlations should be considered with caution (see Table 2). x, maximum correlation = 1.
4. Discussion
Although AhR is well reported for its role in environmental chemical toxicity, as a mediator of the unintended consequences of human pollution, and its involvement in tumor initiation and progression [24,25,26,28,35], the relationship between AhR expression, pollution-linked AhR-dependent function, and Western patients with GCs remains unexplored. Because diffuse GC is increasing in prevalence in Western countries, usually diagnosed at advanced stages, and has no efficacious treatment options, the exploration of its cellular and molecular causes is crucial. We reported significantly high expression of AhR in our Western cohort of GC independently of their clinical subtypes [29]. A link between exposure to POPs and diffuse GC is supported by the study of accidentally exposed populations in Seveso [11]. In the study presented here, we have analyzed the expression of AhR and several AhR-regulated genes in a series of gastric tumors including diffuse and intestinal GC. Furthermore, we have studied the impact of two AhR ligands well known for their critical role in cancer development linked to pollution on AhR and AhR-related gene expression [26,27].
Expression of AhR and RHOA: Using RT-PCR, we found a correlation between the expression of AhR and RHOA in GCs independently of their subtypes (Table 4), as previously documented for other types of cancers [12,36,37]. A higher expression of RHOA has been found in diffuse GC with 85% overexpression (>3 fold) as compared to normal samples, along with 50% in intestinal subtype) [10]. The functional and coordinated role of RHOA in the development of cancers involves several processes such as cell proliferation, migration, invasion, and angiogenesis [36,37,38,39,40]. Increased RHOA activity is correlated with worse overall survival in diffuse patients [41]. Interestingly, RHOA transcription has recently been shown to be initiated by a ligand-AhR-ARNT complex. Somatic alterations in RHOA and CDH1 have been reported in aggressive diffuse GC and are generally associated with familial disease [4,42]. However, our Western cohort of diffuse GC as defined by the Lauren classification did not include familial GC.
Expression and distribution of CYP1A1 and CYP1B1: Cytochrome P450-1 enzymes are inducible forms of the cytochrome P450 family of xenobiotic metabolizing enzymes [43,44]. In our study, CYP1A1 was detected at a very low level in the stomach, but overexpressed (>3 fold) in 23% of diffuse GC as compared to non-tumoral tissue. CYP1A1 was also highly induced by TCDD, a non-genotoxic AhR ligand, in undifferentiated diffuse GC (Kato III) cells. CYP1B1 was the most significantly expressed form in diffuse GC, as previously reported in a wide range of human cancers including breast, colon, lung, and others [43], mainly in the cytoplasm in GC which is expected for an enzyme involved in xenobiotic metabolism. CYP1A1 and CYP1B1 have a central role in tumor development and the activation step of pro-carcinogen compounds such as BaP [16,44,45,46,47,48]. BaP is a prototypical PAH found in tobacco and combustion processes such as biomass burning [49,50].
Our in vitro experiments using two GC cell lines (KATO III and AGS) indicated that TCDD, and to a lesser extent BaP, strongly induced CYP1A1, UGT1A1, and NQO1 in KATO III epithelial cells. The expression of CYP1B1 was also induced upon TCDD treatment, even though at a much lower level as compared to CYP1A1. CYP1A1 was also increased following TCDD treatment in AGS cells as compared to unexposed cells. Functional DRE enhancer elements have been identified in vitro and in vivo for AhR target genes including CYP1A1, CYP1B1, and NQO1, which encode phase I and II xenobiotic metabolizing enzymes [51]. Our in vivo study also shows that CYP1B1 expression is significantly increased (p = 0.014) in diffuse GC as compared to intestinal GC. At the protein level, CYP1B1 was mainly observed in the stromal compartment in diffuse GC (Figure 1C). It is well known that stromal cells, such as fibroblasts and macrophages, express CYP1B1, but not CYP1A1, in response to TCDD or benzopyrene [52,53]. Taken together, our results suggest a cell-specific distribution of CYP1B1 and CYP1A1 in diffuse GC. Our results also suggest that activated AhR may contribute to the tumor–stroma interaction (through CYP1A1 and CYP1B1) in diffuse GC.
Expression and functional role of AhR, CYP1A1 and CYP1B1: Animal and clinical data provide evidence for the role of AhR in gastric tumorigenesis, implicating the receptor in the regulation of tumor growth, EMT, migration, invasion, and cancer aggression [24,25,28,35]. We observed a significant increase in AhR mRNA expression levels in GC independently of intestinal or diffuse GC subtypes and clinical parameters. In addition, strong nuclear AhR is observed in GC tumors (Figure 1B,D), a subcellular distribution for a transcription factor indicative of its constitutive activation in GC. Altogether, these observations strongly suggest the activation of AhR in GC, as previously reported in breast cancer [12]. The connection between EMT and tumorigenesis has been established in human cancers involving several pathways such as the activation of Wnt/β-catenin signaling through CYP1s [54,55], or hedgehog signaling [56,57]. It is also well known that CYP1A1 and CYP1B1 have important roles in tumor development (cell invasion, migration, and disease progression), in part linked to their metabolic activation by BaP. The analysis of CYP1s and co-regulated genes using large-scale analysis may also be helpful for functional studies [58]. Using qRT-PCR, we compared the expression of CYP1s with the expression levels of 36 genes coding for proteins that have been previously studied in the same cohort of patients [10,29]. These genes were selected on the basis of their roles in proliferation, the IGF pathway, the EMT signature, migration, angiogenesis, or immunity. In diffuse GC, but not intestinal GC, CYP1A1 expression was strongly correlated with the expression of genes involved in proliferation (IGF1, p = 0.001), EMT signature such as VIM, p = 0.007; SLUG and ZEB2 (p = 0.04); and migration (MMP2, p = 0.01); these genes were previously shown to be correlated with IGF1 [10]. Interestingly, the promoters of CYP1A1, VIM, and SNAI2/SLUG contain a xenobiotic responsive element (DRE) sequence that when bound by AhR-ARNT heterodimers (canonical pathway) leads to their transcription. The activation of the AhR pathway by TCDD has been previously shown to enhance cancer cell invasion through metalloproteinases [59,60]. Environmental pollutants have been found to contribute to EMT and mesenchymal markers that provide invasion, migration, and subsequent metastasis [60,61,62]. In contrast to diffuse GC, the low expression of CYP1A1 and CYP1B1 in intestinal GC inversely correlated with IDO1 expression (p < 0.02). The IDO enzyme mediates the early steps of tryptophan metabolism leading to kynurenine, an endogenous AhR ligand produced in the intestinal but not diffuse GC [29]. Thus, environmental pollutants vs. endogenous kynurenin may have different effects on AhR-dependent gene expression in GCs.
Whether the increased expression of CYP1s that we observed in diffuse as compared to intestinal GC is due to exposure to a specific or multiple POPs remains to be established [63]. We have previously reported the significant and widespread increase in a substantial set of POPs such as polychlorinated dioxins (PCDDs/PCDFs), PCBs, and polybrominated flame retardants (such as PBDE 209, a carcinogenic intermediate of BaP) in human omental tissue (fat deposits) from French patients with diffuse GC as compared to control biopsies [13]. The co-exposure of TCDD and PBDE 209 was observed in 33% of the omentum from diffuse GC patients. Interestingly, an increased incidence of hepatocellular carcinomas was observed in rodents upon exposure to PBDE 209 as well as increased CYP1A1 mRNA expression levels in Caco-2 cells [64].
Expression of AhRR: Our results reveal that AhRR mRNA expression levels are strongly increased in the cohort of diffuse GC as compared to normal tissues of the same anatomical origin (×2.65, p = 0.007) (Table 2). The effect of dioxin on CYP1A1 and AhRR expression in the undifferentiated KATO III as compared to the AGS gastric epithelial cells also supports the role of xenobiotic compounds in vivo. The expression of AhRR correlated with CYP1A1 (p = 0.007), IGF1 (p < 0.0001), and with genes involved in EMT (TWIST2 and ZEB2) and cell migration (MMP2, p = 0.002). Our observations in patients with metastatic diffuse GC further indicate a significant decrease in AhRR expression. Our results suggest that AhRR may represent an independent prognosis factor in diffuse GC, as we previously reported for breast cancer [12]. Poor prognosis was previously correlated with a decreased expression of AhRR in GCs from an Asian gastric cohort, but without discrimination between subtypes [65]. Moreover, the loss of AhRR correlates with an aggressive tumorigenic phenotype in several tumors including colon, cervical, and ovarian carcinoma [66].
In conclusion, this pilot study explores two forms of GCs, diffuse and intestinal, which lead to metastases in the peritoneal cavity. The induction of CYP1s through AhR activation may potentially serve as a biomarker for exposure to xenobiotics in diffuse GC. In vitro experiments indicate that TCDD strongly induces CYP1A1 in epithelial cells. The expression of CYP1A1 strongly correlated with genes involved in EMT and migration, and the IGF pathway. The increased expression of CYP1B1 was observed in diffuse GC. CYP1B1 activates a large number of pollutants which may result in the activation of pro-cancer signaling pathways. AhR may contribute to the tumor–stroma interaction (through CYP1A1 and CYP1B1) in diffuse GC. Whether clinical factors such as smoking are prognostic factors remains to be investigated in GC. We argue that reduction in exposure to subsets of environmental ligands could be important to prevent primary diffuse GC. A recent study revealed that exposure to environmental pollutants such as POPs and BaP may reduce the efficacy of chemotherapy [67].
We acknowledge that our study has limitations. Because of the relatively low sample size in this report (n = 29), certainly, the results need to be confirmed using a larger cohort of gastric tumor samples with different clinical characteristics (including early and advanced stages). Nonetheless, our pilot study shed light on the impact of AhR and related signaling pathways in Western patients with GC. In addition, it will be interesting to extend the coverage to different geographical population settings. This will allow us to understand if the signaling pathways identified in GC subtypes are characteristic of Western patients or can also be observed in patients from other geographical locations. Further in vitro and in vivo studies with a larger cohort of gastric tumor samples will provide a better understanding of the complexity of the effect of different ligands on the regulation of the AhR pathways and may contribute to the development of novel clinically relevant agonists or antagonists.
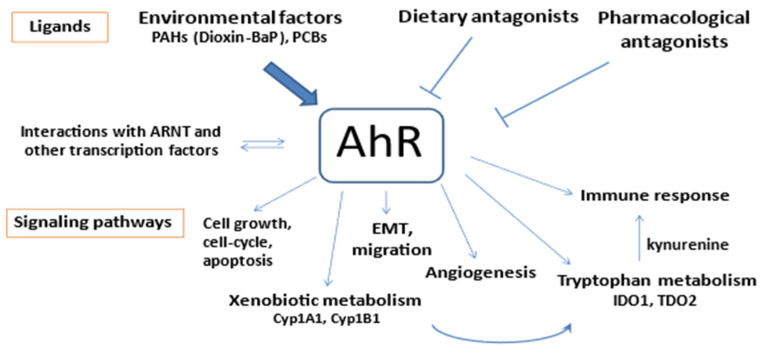
As summarized in Figure 3, the present study provides new insights into the diversity of AhR functions in the development of cancer including GC. It is likely that the binding of various ligands is central to this carcinogenesis. The gastric epithelium is constantly exposed to exogenous AhR ligands such as dietary compounds and environmental toxins (PAH and other dioxin-like compounds), which enable the strong activation of AhR. Furthermore, the endogenous AhR kynurenine is produced through the metabolism of tryptophan by IDO1 which is induced in stromal cells, or by TDO2 which can be up-regulated in tumor cells and the tumor stroma. Our findings merit further studies with a larger cohort of gastric tumor samples with different clinical characteristics, including early and advanced tumor stages.
Figure 3.
AhR role in cancer biology; environmental compounds at the crossroads of toxicity and several signaling pathways.
Acknowledgments
The authors greatly thank Matti Ullah and Iman Aldybiat (INSERM U1275, Lariboisiere Hospital), P Castagnet (Department of Pathology, Lariboisiere Hospital, Paris, France), and Ivan Bieche (Department of Genetics, Pharmacogenomics Unit, Institut Curie, University Paris Cité, Paris 75005). We also thank Peter Brooks for assistance in editing the English language of the manuscript.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines12081905/s1, Table S1: Relationship between AhR mRNA expression and clinical biological parameters in a series of 29 gastric cancers including diffuse and intestinal subtypes.
Author Contributions
Conceptualization: M.P.-A.; methodology: C.P., S.V. and M.P.-A.; software: C.P., M.P.-A., and V.B., data curation: M.P. collected the clinical samples and data from patients. Writing—original draft: M.P.-A.; rewriting: V.B. Funding acquisition: M.P.-A. and M.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The studies involving human participants were approved by the Ethical Committee of Lariboisiere Hospital (Paris, France). The patients/participants provided their written informed consent to participate in scientific studies. Written informed consent was obtained from the participants before the collection of any samples, and the specimens were irreversibly de-identified. All the experiments involving the handling of human tissues were performed in accordance with the Tenets of the Declaration of Helsinki. Biopsies were taken from patients who underwent partial gastrectomy for gastric adenocarcinoma tumor tissue from 2005 to 2014. The cohort of patients was previously described in [13,29].
Informed Consent Statement
The patients/participants provided their written informed consent to participate in this study and associated publications.
Data Availability Statement
A total of 29 patients underwent partial gastrectomy for histopathologically confirmed gastric adenocarcinoma primary tissue in the Lariboisiere Hospital (Paris, France) from 2005 to 2014.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This work was supported by INSERM (Institut National de la Santé et de la Recherche Medicale, Paris) and CNRS (Centre national de la Recherche Scientifique (M.P.-A.)), and INSERM, Université Paris Cité and Fondation Nelia et Amadeo Barletta, Switzerland (V.B.).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bray F., Laversanne M., Sung H., Ferlay J., Siegel R.L., Soerjomataram I., Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024;73:229–263. doi: 10.3322/caac.21834. [DOI] [PubMed] [Google Scholar]
- 2.Thrift A.P., Wenker T.N., El-Serag H.B. Global burden of gastric cancer: Epidemiological trends, risk factors, screening and prevention. Nat. Rev. Clin. Oncol. 2023;20:338–349. doi: 10.1038/s41571-023-00747-0. [DOI] [PubMed] [Google Scholar]
- 3.Díaz Del Arco C., Estrada Muñoz L., Ortega Medina L., Molina Roldán E., Cerón Nieto M.Á., García Gómez de Las Heras S., Fernández Aceñero M.J. Clinicopathological differences, risk factors and prognostic scores for western patients with intestinal and diffuse-type gastric cancer. World J. Gastrointest Oncol. 2022;14:1162–1174. doi: 10.4251/wjgo.v14.i6.1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Cancer Genome Atlas Research Network Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lauren P. The Two Histological Main Types of Gastric Carcinoma: Diffuse and So-Called Intestinal-Type Carcinoma. An Attempt at a Histo-Clinical Classification. Acta Pathol. Microbiol. Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 6.Piessen G., Messager M., Leteurtre E., Jean-Pierre T., Mariette C. Signet ring cell histology is an independent predictor of poor prognosis in gastric adenocarcinoma regardless of tumoral clinical presentation. Ann. Surg. 2009;250:878–887. doi: 10.1097/SLA.0b013e3181b21c7b. [DOI] [PubMed] [Google Scholar]
- 7.Piessen G., Messager M., Le Malicot K., Robb W.B., Di Fiore F., Guilbert M., Moreau M., Christophe V., Adenis A., Mariette C. Phase II/III multicentre randomised controlled trial evaluating a strategy of primary surgery and adjuvant chemotherapy versus peri-operative chemotherapy for resectable gastric signet ring cell adenocarcinomas-PRODIGE 19-FFCD1103-ADCI002. BMC Cancer. 2013;13:281. doi: 10.1186/1471-2407-13-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henson D.E., Dittus C., Younes M., Nguyen H., Albores-Saavedra J. Differential trends in the intestinal and diffuse types of gastric carcinoma in the United States, 1973–2000: Increase in the signet ring cell type. Arch. Pathol. Lab. Med. 2004;128:765–770. doi: 10.5858/2004-128-765-DTITIA. [DOI] [PubMed] [Google Scholar]
- 9.Taghavi S., Jayarajan S.N., Davey A., Willis A.I. Prognostic significance of signet ring gastric cancer. J. Clin. Oncol. 2012;30:3493–3498. doi: 10.1200/JCO.2012.42.6635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perrot-Applanat M., Vacher S., Pimpie C., Chemlali W., Derieux S., Pocard M., Bieche I. Differential gene expression in growth factors, epithelial mesenchymal transition and chemotaxis in the diffuse type compared with the intestinal type of gastric cancer. Oncol. Lett. 2019;18:674–686. doi: 10.3892/ol.2019.10392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pesatori A.C., Consonni D., Rubagotti M., Grillo P., Bertazzi P.A. Cancer incidence in the population exposed to dioxin after the “Seveso accident”: Twenty years of follow-up. Environ. Health. 2009;8:39. doi: 10.1186/1476-069X-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vacher S., Castagnet P., Chemlali W., Lallemand F., Meseure D., Pocard M., Bieche I., Perrot-Applanat M. High AHR expression in breast tumors correlates with expression of genes from several signaling pathways namely inflammation and endogenous tryptophan metabolism. PLoS ONE. 2018;13:e0190619. doi: 10.1371/journal.pone.0190619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perrot-Applanat M., Pimpie C., Cano-Sancho G., Antignac J.P., Pocard M. Detection of Persistent Organic Pollutants in Omental Adipose Tissue from Patients with Diffuse-Gastric Cancer: A Pilot Study. Cancers. 2021;13:4874. doi: 10.3390/cancers13194874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Denison M.S., Nagy S.R. Activation of the aryl hydrocarbon receptor by structurally diverse exogenous and endogenous chemicals. Annu. Rev. Pharmacol. Toxicol. 2003;43:309–334. doi: 10.1146/annurev.pharmtox.43.100901.135828. [DOI] [PubMed] [Google Scholar]
- 15.Denison M.S., Soshilov A.A., He G., DeGroot D.E., Zhao B. Exactly the same but different: Promiscuity and diversity in the molecular mechanisms of action of the aryl hydrocarbon (dioxin) receptor. Toxicol. Sci. 2011;124:1–22. doi: 10.1093/toxsci/kfr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Go R.E., Hwang K.A., Choi K.C. Cytochrome P450 1 family and cancers. J. Steroid Biochem. Mol. Biol. 2015;147:24–30. doi: 10.1016/j.jsbmb.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez-Salguero P., Pineau T., Hilbert D.M., McPhail T., Lee S.S., Kimura S., Nebert D.W., Rudikoff S., Ward J.M., Gonzalez F.J. Immune system impairment and hepatic fibrosis in mice lacking the dioxin-binding Ah receptor. Science. 1995;268:722–726. doi: 10.1126/science.7732381. [DOI] [PubMed] [Google Scholar]
- 18.Safe S. Molecular biology of the Ah receptor and its role in carcinogenesis. Toxicol. Lett. 2001;120:1–7. doi: 10.1016/S0378-4274(01)00301-0. [DOI] [PubMed] [Google Scholar]
- 19.Roman A.C., Carvajal-Gonzalez J.M., Rico-Leo E.M., Fernandez-Salguero P.M. Dioxin receptor deficiency impairs angiogenesis by a mechanism involving VEGF-A depletion in the endothelium and transforming growth factor-beta overexpression in the stroma. J. Biol. Chem. 2009;284:25135–25148. doi: 10.1074/jbc.M109.013292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng S., Cao Z., Wang X. Role of aryl hydrocarbon receptor in cancer. Biochim. Biophys. Acta. 2013;1836:197–210. doi: 10.1016/j.bbcan.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Quintana F.J., Sherr D.H. Aryl hydrocarbon receptor control of adaptive immunity. Pharmacol. Rev. 2013;65:1148–1161. doi: 10.1124/pr.113.007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stockinger B., Di Meglio P., Gialitakis M., Duarte J.H. The aryl hydrocarbon receptor: Multitasking in the immune system. Annu. Rev. Immunol. 2014;32:403–432. doi: 10.1146/annurev-immunol-032713-120245. [DOI] [PubMed] [Google Scholar]
- 23.Litzenburger U.M., Opitz C.A., Sahm F., Rauschenbach K.J., Trump S., Winter M., Ott M., Ochs K., Lutz C., Liu X., et al. Constitutive IDO expression in human cancer is sustained by an autocrine signaling loop involving IL-6, STAT3 and the AHR. Oncotarget. 2014;5:1038–1051. doi: 10.18632/oncotarget.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andersson P., McGuire J., Rubio C., Gradin K., Whitelaw M.L., Pettersson S., Hanberg A., Poellinger L. A constitutively active dioxin/aryl hydrocarbon receptor induces stomach tumors. Proc. Natl. Acad. Sci. USA. 2002;99:9990–9995. doi: 10.1073/pnas.152706299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersson P., Rubio C., Poellinger L., Hanberg A. Gastric hamartomatous tumours in a transgenic mouse model expressing an activated dioxin/Ah receptor. Anticancer Res. 2005;25:903–911. [PubMed] [Google Scholar]
- 26.Brunnberg S., Andersson P., Lindstam M., Paulson I., Poellinger L., Hanberg A. The constitutively active Ah receptor (CA-Ahr) mouse as a potential model for dioxin exposure--effects in vital organs. Toxicology. 2006;224:191–201. doi: 10.1016/j.tox.2006.04.045. [DOI] [PubMed] [Google Scholar]
- 27.Labib S., Guo C.H., Williams A., Yauk C.L., White P.A., Halappanavar S. Toxicogenomic outcomes predictive of forestomach carcinogenesis following exposure to benzo(a)pyrene: Relevance to human cancer risk. Toxicol. Appl. Pharmacol. 2013;273:269–280. doi: 10.1016/j.taap.2013.05.027. [DOI] [PubMed] [Google Scholar]
- 28.Peng T.L., Chen J., Mao W., Song X., Chen M.H. Aryl hydrocarbon receptor pathway activation enhances gastric cancer cell invasiveness likely through a c-Jun-dependent induction of matrix metalloproteinase-9. BMC Cell Biol. 2009;10:27. doi: 10.1186/1471-2121-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perrot-Applanat M., Pimpie C., Vacher S., Bieche I., Pocard M., Baud V. Differential Expression of Genes Involved in Metabolism and Immune Response in Diffuse and Intestinal Gastric Cancers, a Pilot Ptudy. Biomedicines. 2022;10:240. doi: 10.3390/biomedicines10020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Washington K. 7th edition of the AJCC cancer staging manual: Stomach. Ann. Surg. Oncol. 2010;17:3077–3079. doi: 10.1245/s10434-010-1362-z. [DOI] [PubMed] [Google Scholar]
- 31.Sano T., Coit D.G., Kim H.H., Roviello F., Kassab P., Wittekind C., Yamamoto Y., Ohashi Y. Proposal of a new stage grouping of gastric cancer for TNM classification: International Gastric Cancer Association staging project. Gastric Cancer. 2017;20:217–225. doi: 10.1007/s10120-016-0601-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shu P., Qin J., Shen K., Chen W., Liu F., Fang Y., Wang X., Wang H., Shen Z., Sun Y., et al. The IGCA staging system is more accurate than AJCC7 system in stratifying survival of patients with gastric cancer in stage III. BMC Cancer. 2017;17:238. doi: 10.1186/s12885-017-3235-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ji X., Bu Z.D., Yan Y., Li Z.Y., Wu A.W., Zhang L.H., Zhang J., Wu X.J., Zong X.L., Li S.X., et al. The 8th edition of the American Joint Committee on Cancer tumor-node-metastasis staging system for gastric cancer is superior to the 7th edition: Results from a Chinese mono-institutional study of 1663 patients. Gastric Cancer. 2017;21:643–652. doi: 10.1007/s10120-017-0779-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bieche I., Onody P., Laurendeau I., Olivi M., Vidaud D., Lidereau R., Vidaud M. Real-time reverse transcription-PCR assay for future management of ERBB2-based clinical applications. Clin. Chem. 1999;45:1148–1156. doi: 10.1093/clinchem/45.8.1148. [DOI] [PubMed] [Google Scholar]
- 35.Yin X.F., Chen J., Mao W., Wang Y.H., Chen M.H. Downregulation of aryl hydrocarbon receptor expression decreases gastric cancer cell growth and invasion. Oncol. Rep. 2013;30:364–370. doi: 10.3892/or.2013.2410. [DOI] [PubMed] [Google Scholar]
- 36.Nam S., Lee Y., Kim J.H. RHOA protein expression correlates with clinical features in gastric cancer: A systematic review and meta-analysis. BMC Cancer. 2022;22:798. doi: 10.1186/s12885-022-09904-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kakiuchi M., Nishizawa T., Ueda H., Gotoh K., Tanaka A., Hayashi A., Yamamoto S., Tatsuno K., Katoh H., Watanabe Y., et al. Recurrent gain-of-function mutations of RHOA in diffuse-type gastric carcinoma. Nat. Genet. 2014;46:583–587. doi: 10.1038/ng.2984. [DOI] [PubMed] [Google Scholar]
- 38.Ridley A.J. RhoA, RhoB and RhoC have different roles in cancer cell migration. J. Microsc. 2013;251:242–249. doi: 10.1111/jmi.12025. [DOI] [PubMed] [Google Scholar]
- 39.Song L., Guo Y., Xu B. Expressions of Ras Homolog Gene Family, Member A (RhoA) and Cyclooxygenase-2 (COX-2) Proteins in Early Gastric Cancer and Their Role in the Development of Gastric Cancer. Med. Sci. Monit. 2017;23:2979–2984. doi: 10.12659/MSM.902367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lawson C.D., Ridley A.J. Rho GTPase signaling complexes in cell migration and invasion. J. Cell Biol. 2018;217:447–457. doi: 10.1083/jcb.201612069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoon J.H., Choi W.S., Kim O., Choi B.J., Nam S.W., Lee J.Y., Park W.S. Gastrokine 1 inhibits gastric cancer cell migration and invasion by downregulating RhoA expression. Gastric Cancer. 2017;20:274–285. doi: 10.1007/s10120-016-0617-1. [DOI] [PubMed] [Google Scholar]
- 42.Wang R., Song S., Harada K., Ghazanfari Amlashi F., Badgwell B., Pizzi M.P., Xu Y., Zhao W., Dong X., Jin J., et al. Multiplex profiling of peritoneal metastases from gastric adenocarcinoma identified novel targets and molecular subtypes that predict treatment response. Gut. 2020;69:18–31. doi: 10.1136/gutjnl-2018-318070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murray G.I., Taylor M.C., McFadyen M.C., McKay J.A., Greenlee W.F., Burke M.D., Melvin W.T. Tumor-specific expression of cytochrome P450 CYP1B1. Cancer Res. 1997;57:3026–3031. [PubMed] [Google Scholar]
- 44.Murray G.I., Taylor M.C., Burke M.D., Melvin W.T. Enhanced expression of cytochrome P450 in stomach cancer. Br. J. Cancer. 1998;77:1040–1044. doi: 10.1038/bjc.1998.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shimada T., Hayes C.L., Yamazaki H., Amin S., Hecht S.S., Guengerich F.P., Sutter T.R. Activation of chemically diverse procarcinogens by human cytochrome P-450 1B1. Cancer Res. 1996;56:2979–2984. [PubMed] [Google Scholar]
- 46.Buters J.T., Mahadevan B., Quintanilla-Martinez L., Gonzalez F.J., Greim H., Baird W.M., Luch A. Cytochrome P450 1B1 determines susceptibility to dibenzo[a,l]pyrene-induced tumor formation. Chem. Res. Toxicol. 2002;15:1127–1135. doi: 10.1021/tx020017q. [DOI] [PubMed] [Google Scholar]
- 47.Shiizaki K., Kawanishi M., Yagi T. Modulation of benzo[a]pyrene-DNA adduct formation by CYP1 inducer and inhibitor. Genes Environ. 2017;39:14. doi: 10.1186/s41021-017-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Z., Snyder M., Kenison J.E., Yang K., Lara B., Lydell E., Bennani K., Novikov O., Federico A., Monti S., et al. How the AHR Became Important in Cancer: The Role of Chronically Active AHR in Cancer Aggression. Int. J. Mol. Sci. 2020;22:387. doi: 10.3390/ijms22010387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nebert D.W., Shi Z., Galvez-Peralta M., Uno S., Dragin N. Oral benzo[a]pyrene: Understanding pharmacokinetics, detoxication, and consequences–Cyp1 knockout mouse lines as a paradigm. Mol. Pharmacol. 2013;84:304–313. doi: 10.1124/mol.113.086637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang H., Zhang X., Wang Y., Bai P., Hayakawa K., Zhang L., Tang N. Characteristics and Influencing Factors of Polycyclic Aromatic Hydrocarbons Emitted from Open Burning and Stove Burning of Biomass: A Brief Review. Int. J. Environ. Res. Public Health. 2022;19:3944. doi: 10.3390/ijerph19073944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dere E., Lo R., Celius T., Matthews J., Zacharewski T.R. Integration of genome-wide computation DRE search, AhR ChIP-chip and gene expression analyses of TCDD-elicited responses in the mouse liver. BMC Genom. 2011;12:365. doi: 10.1186/1471-2164-12-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eltom S.E., Larsen M.C., Jefcoate C.R. Expression of CYP1B1 but not CYP1A1 by primary cultured human mammary stromal fibroblasts constitutively and in response to dioxin exposure: Role of the Ah receptor. Carcinogenesis. 1998;19:1437–1444. doi: 10.1093/carcin/19.8.1437. [DOI] [PubMed] [Google Scholar]
- 53.Sparfel L., Pinel-Marie M.L., Boize M., Koscielny S., Desmots S., Pery A., Fardel O. Transcriptional signature of human macrophages exposed to the environmental contaminant benzo(a)pyrene. Toxicol. Sci. 2010;114:247–259. doi: 10.1093/toxsci/kfq007. [DOI] [PubMed] [Google Scholar]
- 54.Kwon Y.J., Baek H.S., Ye D.J., Shin S., Kim D., Chun Y.J. CYP1B1 Enhances Cell Proliferation and Metastasis through Induction of EMT and Activation of Wnt/beta-Catenin Signaling via Sp1 Upregulation. PLoS ONE. 2016;11:e0151598. doi: 10.1371/journal.pone.0151598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mohamed H.T., Gadalla R., El-Husseiny N., Hassan H., Wang Z., Ibrahim S.A., El-Shinawi M., Sherr D.H., Mohamed M.M. Inflammatory breast cancer: Activation of the aryl hydrocarbon receptor and its target CYP1B1 correlates closely with Wnt5a/b-beta-catenin signalling, the stem cell phenotype and disease progression. J. Adv. Res. 2019;16:75–86. doi: 10.1016/j.jare.2018.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ohta H., Aoyagi K., Fukaya M., Danjoh I., Ohta A., Isohata N., Saeki N., Taniguchi H., Sakamoto H., Shimoda T., et al. Cross talk between hedgehog and epithelial-mesenchymal transition pathways in gastric pit cells and in diffuse-type gastric cancers. Br. J. Cancer. 2009;100:389–398. doi: 10.1038/sj.bjc.6604846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Katoh M. Genomic testing, tumor microenvironment and targeted therapy of Hedgehog-related human cancers. Clin. Sci. 2019;133:953–970. doi: 10.1042/CS20180845. [DOI] [PubMed] [Google Scholar]
- 58.Weitzman J.B. Co-regulation of mouse genes predicts function. J. Biol. 2004;3:19. doi: 10.1186/jbiol18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ishida M., Mikami S., Kikuchi E., Kosaka T., Miyajima A., Nakagawa K., Mukai M., Okada Y., Oya M. Activation of the aryl hydrocarbon receptor pathway enhances cancer cell invasion by upregulating the MMP expression and is associated with poor prognosis in upper urinary tract urothelial cancer. Carcinogenesis. 2010;31:287–295. doi: 10.1093/carcin/bgp222. [DOI] [PubMed] [Google Scholar]
- 60.Barouki R., Coumoul X. Cell migration and metastasis markers as targets of environmental pollutants and the Aryl hydrocarbon receptor. Cell Adhes. Migr. 2010;4:72–76. doi: 10.4161/cam.4.1.10313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Otsuki S., Inokuchi M., Enjoji M., Ishikawa T., Takagi Y., Kato K., Yamada H., Kojima K., Sugihara K. Vimentin expression is associated with decreased survival in gastric cancer. Oncol. Rep. 2011;25:1235–1242. doi: 10.3892/or.2011.1185. [DOI] [PubMed] [Google Scholar]
- 62.Ochieng J., Nangami G.N., Ogunkua O., Miousse I.R., Koturbash I., Odero-Marah V., McCawley L.J., Nangia-Makker P., Ahmed N., Luqmani Y., et al. The impact of low-dose carcinogens and environmental disruptors on tissue invasion and metastasis. Carcinogenesis. 2015;36:S128–S159. doi: 10.1093/carcin/bgv034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lagunas-Rangel F.A., Linnea-Niemi J.V., Kudlak B., Williams M.J., Jonsson J., Schioth H.B. Role of the Synergistic Interactions of Environmental Pollutants in the Development of Cancer. Geohealth. 2022;6:e2021GH000552. doi: 10.1029/2021GH000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li S., Yuan J., Che S., Zhang L., Ruan Z., Sun X. Decabromodiphenyl ether induces ROS-mediated intestinal toxicity through the Keap1-Nrf2 pathway. J. Biochem. Mol. Toxicol. 2022;36:e22995. doi: 10.1002/jbt.22995. [DOI] [PubMed] [Google Scholar]
- 65.Li Y.F., Wang D.D., Zhao B.W., Wang W., Yuan S.Q., Huang C.Y., Chen Y.M., Zheng Y., Keshari R.P., Xia J.C., et al. Poor prognosis of gastric adenocarcinoma with decreased expression of AHRR. PLoS ONE. 2012;7:e43555. doi: 10.1371/journal.pone.0043555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zudaire E., Cuesta N., Murty V., Woodson K., Adams L., Gonzalez N., Martinez A., Narayan G., Kirsch I., Franklin W., et al. The aryl hydrocarbon receptor repressor is a putative tumor suppressor gene in multiple human cancers. J. Clin. Investig. 2008;118:640–650. doi: 10.1172/JCI30024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lagunas-Rangel F.A., Liu W., Schioth H.B. Can Exposure to Environmental Pollutants Be Associated with Less Effective Chemotherapy in Cancer Patients? Int. J. Environ. Res. Public Health. 2022;19:2064. doi: 10.3390/ijerph19042064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
A total of 29 patients underwent partial gastrectomy for histopathologically confirmed gastric adenocarcinoma primary tissue in the Lariboisiere Hospital (Paris, France) from 2005 to 2014.