Abstract
In patients with spinal cord injury (SCI), patient-reported outcomes (PROMs) and experience of care measures (PREMs) are extremely relevant for the prognosis. However, there is a paucity of research on these topics. We conducted a cross-sectional study to investigate the relationships between these patient outcomes and other demographic and clinical variables in adult SCI patients discharged from the intensive care unit of an Italian tertiary rehabilitation hospital. We administered the Consultation and Relational Empathy (CARE) for perceived relational empathy, the Spinal Cord Independence Measure III self-report (SCIM-SR) for functional autonomy, the Numeric Rating Scale (NRS) for pain, and the Connor–Davidson Resilience Scale (CD-RISC-10) for resilience. Study participants consisted of 148 adults with SCI; 82.4% were male, with a mean age of 49.9 years (SD = 16.6). The lesion was traumatic in 82.4% and complete in 74.3% of cases. The median length of hospital stays was 35 days (interquartile range—IQR = 23–60). Perceived relational empathy was positively associated with resilience (r = 0.229, p = 0.005) and negatively associated with the length of the stay and lesion completeness. Resilience had a weak negative association with pain (r = −0.173, p = 0.035) and was unrelated to other variables. Clinicians should consider the routine assessment of PREMs and PROMs in order to personalize post-discharge therapeutic plans and identify appropriate measures to ensure continuity of care.
Keywords: patient-reported experience measures (PREMs), patient-reported outcome measures (PROMs), resilience, relational empathy, spinal cord injury, acute care
1. Introduction
Over the past 10 years, health services in many EU countries have begun to collect indicators based on patient-reported information such as patient-reported experience measures (PREMs) [1,2] and patient-reported outcome measures (PROMs) [3,4] to assess the quality of care provided and for the accountability and performance evaluation of health systems. PROMs typically represent subjective outcomes that are relevant to patients because they measure the impact of healthcare on their usual activities and self-care. They include, for example, pain, perceived functional capacity, and self-efficacy in managing their disease. PREMs measure users’ experiences of care, such as being involved in treatment decisions, being treated with dignity and respect, and receiving information about available services; they provide a practical way to explore person-centered, integrated models of care. A systematic review has shown that improving patients’ experience of care is often associated with improvements in patient safety, clinical effectiveness, and health outcomes [5]. In people with spinal cord injury (SCI), where personal suffering adds to clinical complexity, perceived relational empathy and resilience are extremely relevant for the prognosis, as treatment experience may influence therapeutic outcomes [6,7,8]. As a matter of fact, the success of a rehabilitation project depends not only on the therapeutic approaches used but also, to a large extent, on the trustful relationship between healthcare professionals and the patient [9,10]. Thus, the assessment with tools measuring the subjective experience of care [11,12,13] should be added to traditional assessments of clinical outcomes such as pain and functioning.
However, there are currently few studies using PROMs, and even fewer using PREMS in people with SCI, and none in the intensive phase of hospitalization.
Among PREMs, the perceived relational empathy of healthcare professionals has received some attention in studies on people with SCI. In a U.S. study of patients receiving care from the U.S. Veterans Health Administration and SCI Model Systems, based on a survey and administrative databases, higher physical and mental health status and tetraplegia were associated with greater perceptions of holistic care and empathy in the therapeutic patient–provider relationship [14]. In a second study conducted in India in patients seen for a follow-up visit at least one year after injury and living in the community, perceived relational empathy was associated with higher levels of quality of life [15].
In addition, resilience, a psychological characteristic, has been reported to be central to the well-being of patients with SCI. Resilience has been considered as a state-like variable that involves behaviors, thoughts, and actions, which can be learned over time, or as a trait-like construct that someone either has or does not have.
Psychological resilience can be conceptualized as the ability to (1) resist the negative effects of stressors, (2) “bounce back” from stressors, and/or (3) grow from stressors [16]. Hence, assessing an individual’s state of resilience and approach to setbacks may provide the development of important interventions that may involve, for example, bolstering resilience through external support systems such as social support and good relationships. This kind of resilience-specific intervention could also be important in addressing rehospitalization and extending benefits after discharge as well, such as through the adoption of new resilient coping strategies [17,18,19].
According to recent research, high levels of resilience are linked to emotional regulation, cognitive coping (e.g., problem-solving skills, reappraisal of the meaning of setbacks), and positive mental health [20]. Resilience was also found to be consistently related to acceptance of disability and high self-efficacy and, in general, to a better and satisfactory quality of life [21,22,23,24,25].
To our knowledge, no research study has investigated the relationship between resilience and patient-perceived relational empathy of doctors at discharge from acute hospital care.
Our results have the potential to contribute to the future development of strategies to improve and personalize the care provided to patients with SCI.
The primary aim of this study is to describe the perceived relational empathy of doctors and the resilience of patients with SCI at discharge from the intensive care unit (ICU) of the Montecatone Rehabilitation Institute.
The secondary aims are to analyze the association of perceived relational empathy and resilience with pain intensity, functional autonomy achieved by the patient, and the medical history of patients at discharge.
2. Materials and Methods
This observational, cross-sectional study was carried out at the Montecatone Rehabilitation Institute and included people with SCI admitted to the ICU.
Patients in the ICU are mainly referred from the resuscitation services, emergency departments, and trauma centers of other Italian hospitals, usually shortly after the trauma. Referred patients have completed the surgical phase, are still clinically very unstable, and do not have the autonomy to perform basic vital functions. In the ICU, the post-traumatic situation is assessed, and the most appropriate measures are taken to start rehabilitation as early as possible and to ensure a high quality of care, guaranteeing the start of motor and respiratory rehabilitation at a very early stage, when respiratory, metabolic, nutritional, infectious, or other problems are still present and require intensive care, monitoring, and support. In this way, the ICU of the Institute initiates the process of true global rehabilitation for patients who cannot be weaned from the ventilator, thus becoming the link between the period of intensive intervention and the subsequent global rehabilitation phase, including training to promote patient and caregiver autonomy.
2.1. Study Population
Patients were enrolled in this study over a period of 37 months (June 2020–July 2023) and were assessed at discharge from the ICU after signing an informed consent to participate in the study and to have their personal data processed. For patients who were able to consent but were unable to sign, the consent form was signed by an impartial third party who was not involved in the study. The study was approved by the Ethics Committee CE AVEC protocol # 46-2021-OSS-AUSLIM.
Inclusion criteria were adult age, SCI at any neurological level, completeness and etiology, sufficient knowledge of Italian to complete questionnaires, and ability to provide written informed consent. Exclusion criteria were cognitive deficits, brain damage, and ongoing pregnancy.
The demographic variables and the characteristics of the lesion were extracted from electronic clinical records and linked with questionnaire data. These variables included age, gender, neurological level, AIS level (coded as A, complete lesion, and B, incomplete lesion), etiology (coded as traumatic or non-traumatic), comorbidity (coded as present or absent), and length of hospital stay.
2.2. PROMs
The Spinal Cord Independence Measure III self-report (SCIM-SR) [26] is a self-report questionnaire that assesses the individual’s autonomy by evaluating the ability to perform simple daily life tasks. It consists of 16 items organized into 3 groups: self-care (range 0–20), breathing and sphincter management (range 0–40), and mobility (range 0–40). Higher scores denote better functioning. A score of 0 indicates the need for total assistance in performing the task. The total score ranges from 0 to 100.
The Italian version of the SCIM-SR was validated by Bonavita et al. [27] against the interview-based version. A good agreement was found between the domain and total scores of the two versions (r = 0.918 for ‘Self-care’, 0.806 for ‘Respiration and sphincter management’, 0.906 for ‘Mobility’, and 0.934 for the total score).
The Numeric Rating Scale (NRS) measures the intensity of pain. It is a self-rated pain scale ranging from 0 to 10, where 0 indicates ‘no pain’ and 10 indicates the ‘worst pain imaginable’.
2.3. PREMs
The Consultation and Relational Empathy (CARE) measure is a patient-reported experience measure developed in the United Kingdom [11,28,29], which has been extensively validated [14,28,29,30,31,32] and shown to be highly reliable in differentiating between doctors [29,30,31]. It consists of ten items, rated as “poor” = 1, “fair” = 2, “good” = 3, “very good” = 4, “excellent” = 5, or “does not apply”. The total score is obtained as a sum of item scores and ranges from 10 to 50; higher scores reflect greater patient-centeredness, specifically patient perceptions of holistic care and relational empathy in their healthcare. This measure has been used in U.S. patients with spinal cord injury [14]. More information on CARE can be found in the CARE Measure Website [33]. In the Italian version [34], internal consistency was excellent (Cronbach’s α= 0.962), and the exploratory factor analysis confirmed the unidimensional structure of the CARE measure with 74.82% of variance explained by the first factor.
2.4. Resilience
The Connor–Davidson Resilience Scale (CD-RISC-10) is a self-report tool with 10 items scored on a five-point Likert scale from 0 (not at all true) to 4 (true almost all of the time). It measures resilience and the ability to cope with adversity and demonstrates good construct validity and internal consistency (α = 0.85) in an undergraduate sample [13]. Higher scores indicate higher levels of resilience. The total score ranges between 0 and 40. In the Italian version, validated by Di Fabio and Palazzeschi [35] in university students, the scale proved to be unidimensional in confirmatory factor analysis and showed good reliability (Cronbach’s alpha = 0.89) and concurrent validity.
2.5. Statistical Analyses
A sample size of 150 was calculated to detect a correlation ≥ 0.20 between resilience and relational empathy, with an 80% power and a type-I error of 0.05.
Continuous variables were summarized using the mean and standard deviation or the median and interquartile range, and categorical and ordinal variables were summarized using absolute and percentage frequencies. Correlations between continuous or ordinal variables were determined using Spearman’s correlation coefficient, and between a continuous and a dichotomous variable using the point-biserial correlation coefficient. Correlations between 0.10 and 0.29 were considered weak, between 0.30 and 0.49 moderate, and >0.50 strong, using Cohen’s criteria [36].
Comparisons between groups were performed using the t-test or Mann–Whitney’s test for continuous variables, and the χ2 test or Fisher’s exact test for categorical variables, as appropriate.
Multivariable stepwise linear regression was used to identify the variables associated with a better perception of relational empathy during healthcare encounters. Two continuous variables, the CD-RISC score and the length of hospital stay, and one categorical variable, the completeness of the lesion (coded as complete/incomplete), were included as independent variables in the model.
3. Results
This study sample included 148 patients (82.4% male, mean age of 49.9 years, SD = 16.6). The etiology of the lesion was traumatic in the majority of cases (82.4%) and the AIS level was A (complete lesion) in 74.3%. The median length of hospitalization was 35 days (range 7–738, IQR = 23–60) (Table 1).
Table 1.
Characteristics of the sample (N = 148).
| Variables | |
|---|---|
| Sex, n (%) | |
| M | 122 (82.4) |
| F | 26 (17.6) |
| Age, mean (SD) | 49.9 (16.6) |
| Age, median (IQR) | 52 (35.9–63.2) |
| Etiology, n (%) | |
| Traumatic | 122 (82.4) |
| Non-traumatic | 26 (17.6) |
| ASIA Impairment Scale (AIS), n (%) | |
| A | 110 (74.3) |
| B | 38 (25.7) |
| Length of hospitalization, mean (SD) | 55.8 (83.8) |
| Length of hospitalization, median (IQR)) | 35 (23–60) |
ASIA Impairment Scale (AIS).
Patients reported a minimal level of pain at discharge (median NRS = 1, IQR 0–3). Descriptive statistics of SCIM subscales and the total score, and of CARE and the CD-RISC scores are provided in Table 2.
Table 2.
Descriptive statistics of scaled variables.
| Variables | |
|---|---|
| NRS 1 score, mean (SD) | 1.52 (1.76) |
| NRS 1 score, median (IQR) | 1 (0–3) |
| NRS classes, n (%) | |
| 1–3 | 129 (87.2) |
| 4–6 | 19 (12.8) |
| 7–10 | 0 |
| SCIM 2 Self-care scale, mean (SD) | 1.09 (2.45) |
| SCIM 2 Self-care scale, median (IQR) | 0 (0–0.75) |
| SCIM sphinct-respiratory scale, mean (SD) | 3.05 (4.40) |
| SCIM sphinct-respiratory scale, median (IQR) | 2 (0–4) |
| SCIM mobility scale, mean (SD) | 0.20 (0.96) |
| SCIM mobility scale, median (IQR) | 0 (0–0) |
| SCIM total score, mean (SD) | 4.33 (6.96) |
| SCIM total score, median (IQR) | 2 (0–6.75) |
| CARE 3 score, mean (SD) | 40.15 (7.39) |
| CARE 3 score, median (IQR) | 41 (34–46) |
| CD-RISC 4 score, mean (SD) | 24.44 (7.42) |
| CD-RISC 4 score, median (IQR) | 26 (17–30) |
1 NRS, Numerical Rating Scale; 2 SCIM Spinal Cord Independence Measure; 3 CARE, Consultation and Relational Empathy Measure; 4 CD-RISC-10, 10-item Connor–Davidson Resilience Scale.
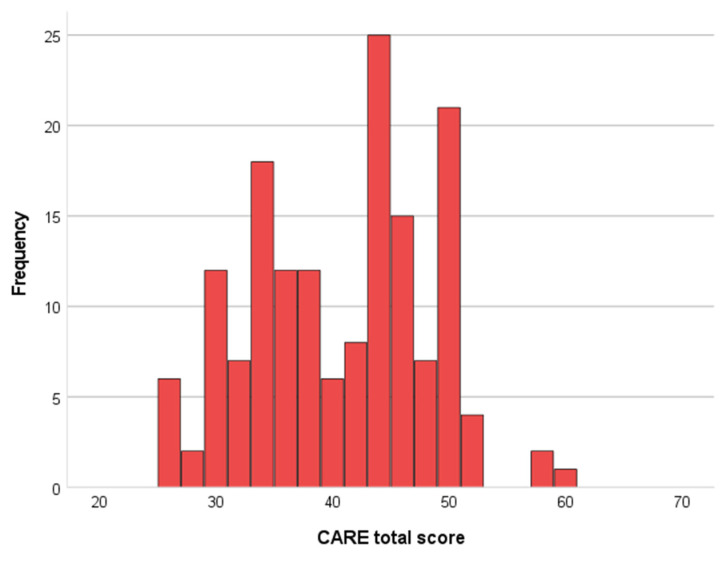
The mean CARE score was 40.2 (SD = 7.4), a value located between the 10th and 25th percentile, i.e., in the lower quartile of normative scores, 39.9% of patients had a score exceeding the normative value of 43 (Figure 1).
Figure 1.
Histogram of the frequency distribution of CARE scores. Mean 40.47, SD = 7.496, N = 148.
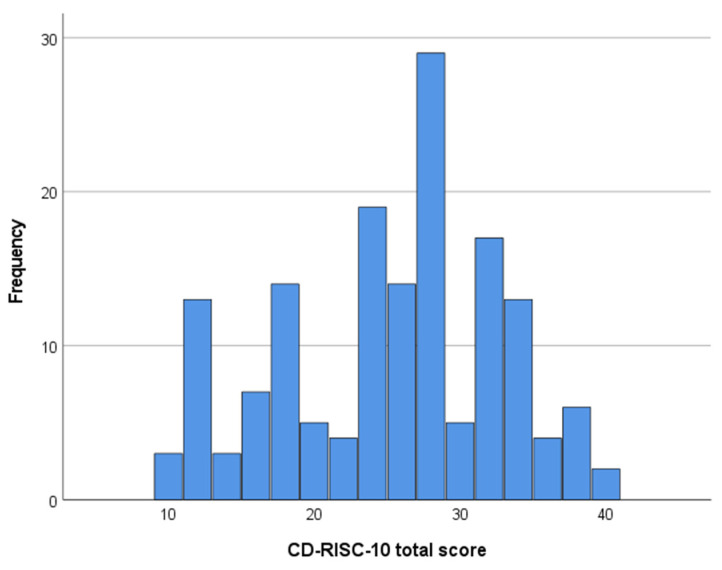
The CD-RISC scale had a mean total score of 24.5 and a range from 0 to 40, showing that the participants exhibited significant variability, from very poor to excellent perceived resilience (Figure 2).
Figure 2.
Frequency distribution of CD-RISC total score. Mean 24.9, SD = 7.53, N = 148.
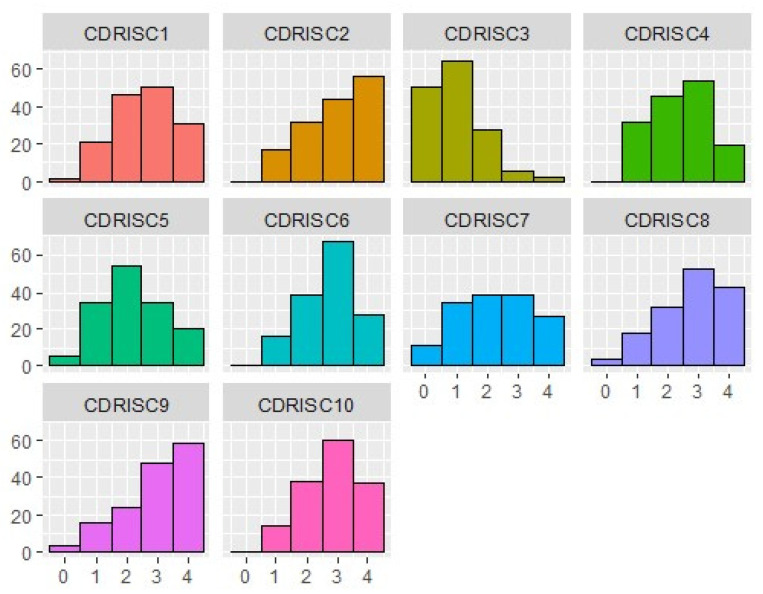
The frequency distribution of the CD-RISC items (Figure 3) indicated variability in responses according to the aspect of resilience investigated; higher scores were found in the ability to cope with adversities (item 2), not being easily discouraged by failure (item 8), and thinking about themselves as strong persons (item 9), while the ability to find the humorous side of the problem was very low (item 3).
Figure 3.
Frequency distribution of CD-RISC items. The x-axis reports the response options to the CD-RISC items on a 5-point Likert scale (0 = “not true”, 4 = “true nearly all the time”); the y-axis reports the percentage of responses.
The SCIM functional scores were indicative of the high severity of these patients’ conditions, with median scores of 0 for self-care and mobility, with 75% requiring total assistance with self-care, 45.3% with managing respiratory and sphincter function, and 92.6% with mobility.
3.1. Correlations between Perceived Relational Empathy, Resilience, Pain, and Functioning
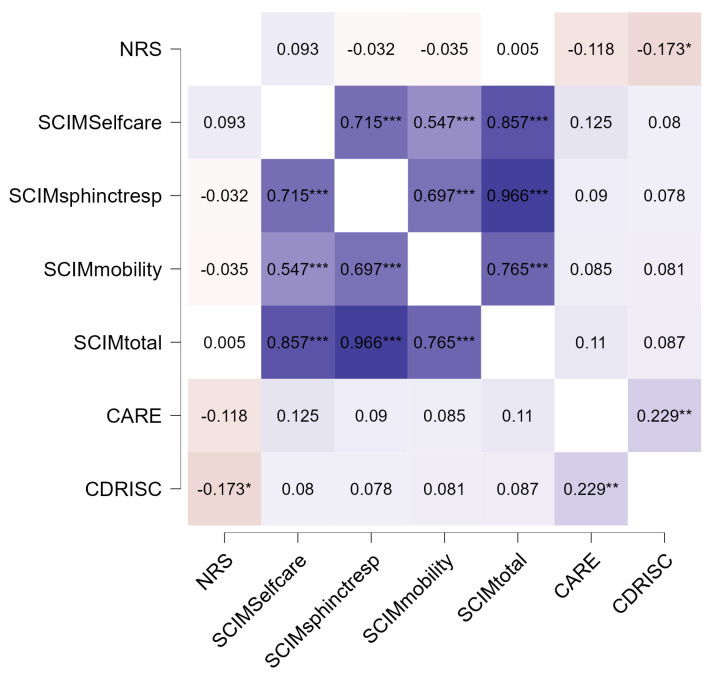
The total CARE score was positively related to the CD-RISC score (r = 0.229, p = 0.005, Figure 4), indicating that higher perceived empathy in the relationship with the doctors was associated with higher resilience. Pain was negatively associated with resilience (r = −0.173, p < 0.05), suggesting that patients experiencing high levels of pain were less resilient. The SCIM scales were strongly associated with each other and with the total score of the scale, as expected.
Figure 4.
Heatmap showing the relationships of PROMs variables with perceived relational empathy and resilience. This heatmap uses a warm to cold color spectrum in which the warm areas’ values are high and the cold areas’ values are low. NRS, Numerical Rating Scale; SCIM, Spinal Cord Independence Measure; CARE, Consultation and Relational Empathy Measure; CD-RISC-10, 10-item Connor–Davidson Resilience Scale. * p < 0.05, ** p < 0.01, *** p < 0.001.
3.2. Correlations of Perceived Relational Empathy Resilience, Pain, and Functioning with Age, Gender, Length of Stay, Etiology, and Neurological Level of Lesion
The level of perceived relational empathy with the doctors was negatively correlated with the length of stay and the completeness of the lesion, indicating that a longer stay and having a complete lesion were associated with poorer perceived empathy. Still, perceived empathy and pain were unrelated to demographic factors and the etiology and neurological level of the lesion (Table 3). The SCIM total score was negatively associated with the length of stay, tetraplegia, and lesion completeness, indicating that patients with better functioning had a shorter ICU stay and were less likely to have tetraplegia and a complete lesion. In addition, the total SCIM score was positively associated with traumatic etiology and comorbidity. Self-care and mobility scores were lower in males than in females.
Table 3.
Correlation of PREM/PROM scores and resilience with demographic and clinical factors.
| Variables | Gender | Age | Length of Stay | Traumatic Etiology | Tetraplegia | Comorbidity | Complete Lesion |
|---|---|---|---|---|---|---|---|
| CARE 1 | −0.003 | −0.066 | −0.186 * | 0.054 | −0.057 | −0.055 | −0.176 * |
| CD-RISC 2 | −0.082 | −0.017 | −0.132 | −0.125 | 0.013 | −0.098 | −0.095 |
| NRS 3 | −0.056 | 0.076 | 0.041 | −0.036 | −0.135 | 0.039 | −0.029 |
| SCIM 4 Self-care | −0.211 * | 0.041 | −0.248 ** | 0.109 | −0.617 ** | 0.201 * | −0.378 ** |
| SCIM sphinct-resp | −0.067 | 0.064 | −0.344 ** | 0.227 ** | −0.592 ** | 0.259 ** | −0.303 ** |
| SCIM mobility | −0.212 ** | −0.136 | −0.091 | 0.068 | −0.325 ** | 0.012 | −0.251 ** |
| SCIM total score | −0.090 | 0.080 | −0.329 ** | 0.263 ** | −0.598 ** | 0.273 ** | −0.338 ** |
* Correlation is significant at the 0.05 level (2-tailed). ** Correlation is significant at the 0.01 level (2-tailed). 1 CARE, Consultation and Relational Empathy Measure; 2 CD-RISC-10, 10-item Connor–Davidson Resilience Scale; 3 NRS, Numerical Rating Scale; 4 SCIM, Spinal Cord Independence Measure.
When we performed a multivariable stepwise linear regression to identify the variables independently associated with a better perception of the relational empathy of doctors, only resilience (the CD-RISC score) emerged as a significant predictor and entered the model (b = 0.225, SE(b) = 0.081, p = 0.006).
4. Discussion
To our knowledge, few studies have used PREMs in this patient population [14,37,38,39,40,41], and this is the first study to provide information on PREMs, PROMs, and resilience. Our findings indicated that the ability of the doctors to build an empathic relationship with the patient was associated with resilience. Although no causal relationship was investigated in this cross-sectional study, it is reasonable to assume that relational empathy affects patients’ resilience and not vice versa. Notably, relational empathy was unrelated to functional outcomes and pain. However, we found a weak negative relationship between relational empathy and the length of stay and completeness of the lesion, suggesting that it may be more challenging to establish a positive relationship between a patient and clinician when the clinical condition is more serious, and hospitalization is of a longer duration. A recent study using the CARE measure in Indian patients with SCI found that quality of life was closely associated with greater perceptions of holistic care and empathy in the therapeutic patient–provider relationship and concluded that the lack of coordination, poor quality of life, and limited communication between a patient and clinician may occur when the latter focuses only on treating the disease rather than treating the patient as a “whole person” [15]. In addition, it has been shown that a good nurse–patient relationship reduces the length of hospital stay and improves the quality and satisfaction of both [10].
Overall, resilience levels in our sample were lower than those of a recent study on patients with SCI participating in a survey (the mean and SD for CD-RISC-10 were M = 29.68, SD = 5.71). This result can be explained by the greater severity of the patients’ conditions in our study, assessed on discharge from intensive care. Resilience was negatively associated with pain, indicating that patients suffering from pain perceived themselves as less capable of coping with their condition. We did not find a significant association between resilience and functioning in SCI. This is consistent with a study carried out in axial spondylarthritis, showing that levels of resilience did not contribute to patients’ perception of their disease activities [42]. Possible explanations are that resilience does not only depend on an individual’s ability to cope with adversities, but also on the strength of interpersonal relationships, the resources available in the community and family circles that can be used to facilitate resilience, biological factors, and stressors, as well as an individual’s level of self-awareness [43,44,45,46]. However, another study conducted on patients with SCI during the COVID-19 pandemic [47] found that autonomy, in addition to psychological health and participation, were determinants of resilience.
One limitation of our study is the cross-sectional design that does not allow us to determine the presence and the direction of causal links among variables.
Patients were recruited from a tertiary hospital in which cases of SCI are more severe than those managed in the community. The mean resilience score for our sample was 24.2, which was slightly lower than that of other cohort studies and might limit the generalizability of the results.
Possible determinants of resilience such as religiousness, depression, life satisfaction, and social support were not collected, thus leaving an important source of variability unexplained.
5. Conclusions
In summary, our study demonstrated that resilience and the perceived relational empathy of doctors are related to each other, but not resilience and functioning. Therefore, the experience of a positive and empathic relationship with doctors is beneficial to the patients and may empower them during rehabilitation. Our results can be generalized only to patients in the initial phase of rehabilitation, shortly after the lesion. Hence, it would be useful for clinicians to collect these subjective measures in order to have a clearer picture of the quality of care provided and of the patients’ psychological strengths; this may be used to accelerate potential clinical improvement during the rehabilitation period and after the transition to community care.
Author Contributions
Conceptualization, M.Z. and P.R.; methodology, M.Z. and P.R.; validation, M.Z., P.R. and E.D.; formal analysis, P.R. and R.D.S.; investigation, S.C., G.B. and E.D.; resources, M.Z.; data curation, P.R. and R.D.S.; writing—original draft preparation, M.Z. and P.R; writing—review and editing, M.Z. and P.R.; visualization, M.Z. and P.R.; supervision, M.Z. and P.R.; project administration, M.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved on 21 January 2021 by the Institutional Review Board (IRB)—Comitato Etico Indipendente Area Vasta Emilia Centro (approval no. 46-2021-OSS-AUSLIM).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Department of Health High Quality Care for All: NHS Next Stage Review Final Report. The Stationery Office. [(accessed on 7 December 2023)];2008 Available online: https://assets.publishing.service.gov.uk/media/5a7c3a5b40f0b67d0b11fbaf/7432.pdf.
- 2.Manary M.P., Boulding W., Staelin R., Glickman S.W. The patient experience and health outcomes. N. Engl. J. Med. 2013;368:201–203. doi: 10.1056/NEJMp1211775. [DOI] [PubMed] [Google Scholar]
- 3.Gleeson H., Calderon A., Swami V., Deighton J., Wolpert M., Edbrooke-Childs J. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open. 2016;6:e011907. doi: 10.1136/bmjopen-2016-011907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oliver R.L. Cognitive, Affective, and Attribute Bases of the Satisfaction Response. J. Consum. Res. 1993;20:418–430. doi: 10.1086/209358. [DOI] [Google Scholar]
- 5.Doyle C., Lennox L., Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davies N., Gibbons E., Fitzpatrick R. A Structured Review of Patient-Reported Outcome Measures for COPD: An Update 2009. University of Oxford; London, UK: 2009. [Google Scholar]
- 7.Fitzpatrick R., Bowling A., Gibbons E. A Structured Review of Patient-Reported Measures in Relation to Selected Chronic Condition, Perceptions of Quality of Life and Carer Impact. University of Oxford and the Department of Health; London, UK: 2009. [Google Scholar]
- 8.Coulter A., Fitzpatrick R., Cornwall J. The Point of Care: Measures of Patients’ Experience of Hospital: Purpose, Methods and Uses. The Kings Fund. 2009. [(accessed on 7 December 2023)]. Available online: https://www.researchgate.net/publication/230687403_The_Point_of_Care_Measures_of_Patients%27_Experience_in_Hospital_Purpose_Methods_and_Uses.
- 9.Morera-Balaguer J., Botella-Rico J.M., Catalán-Matamoros D., Martínez-Segura O.R., Leal-Clavel M., Rodríguez-Nogueira Ó. Patients’ experience regarding therapeutic person-centered relationships in physiotherapy services: A qualitative study. Physiother. Theory Pract. 2021;37:17–27. doi: 10.1080/09593985.2019.1603258. [DOI] [PubMed] [Google Scholar]
- 10.Molina-Mula J., Gallo-Estrada J. Impact of Nurse-Patient Relationship on Quality of Care and Patient Autonomy in Decision-Making. Int. J. Env. Res. Public Health. 2020;17:835. doi: 10.3390/ijerph17030835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mercer S.W., Maxwell M., Heaney D., Watt G.C. The consultation and relational empathy (CARE) measure: Development and preliminary validation and reliability of an empathy-based consultation process measure. Fam. Pract. 2004;21:699–705. doi: 10.1093/fampra/cmh621. [DOI] [PubMed] [Google Scholar]
- 12.Kersten P., White P.J., Tennant A. The consultation and relational empathy measure: An investigation of its scaling structure. Disabil. Rehabil. 2012;34:503–509. doi: 10.3109/09638288.2011.610493. [DOI] [PubMed] [Google Scholar]
- 13.Campbell-Sills L., Stein M.B. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress. 2007;20:1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 14.LaVela S.L., Heinemann A.W., Etingen B., Miskovic A., Locatelli S.M., Chen D. Relational empathy and holistic care in persons with spinal cord injuries. J. Spinal Cord Med. 2017;40:30–42. doi: 10.1080/10790268.2015.1114227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohan M., Singh V.V., Deb R. Relational Empathy, Holistic Care, and Quality of Life in Persons With Spinal Cord Injuries: A Cross-sectional Study. Am. J. Phys. Med. Rehabil. 2023;102:1000–1007. doi: 10.1097/PHM.0000000000002261. [DOI] [PubMed] [Google Scholar]
- 16.den Hartigh R., Hill Y. Conceptualizing and measuring psychological resilience: What can we learn from physics? New Ideas Psychol. 2022;66:100934. doi: 10.1016/j.newideapsych.2022.100934. [DOI] [Google Scholar]
- 17.Anderson N.B., Anderson P.E. Emotional Longevity: What Really Determines How Long You Live. Viking Penguin; New York, NY, USA: 2003. [Google Scholar]
- 18.Connor K.M., Davidson J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depress. Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 19.Luthar S.S., Cicchetti D., Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khosla M. Resilience and health: Implications for interventions and policy making. Psychol. Stud. 2017;62:233–240. doi: 10.1007/s12646-017-0415-9. [DOI] [Google Scholar]
- 21.Driver S., Warren A.M., Reynolds M., Agtarap S., Hamilton R., Trost Z., Monden K. Identifying predictors of resilience at inpatient and 3-month post-spinal cord injury. J. Spinal Cord Med. 2016;39:77–84. doi: 10.1179/2045772314Y.0000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guest R., Craig A., Perry K.N., Tran Y., Ephraums C., Hales A., Dezarnaulds A., Crino R., Middleton J. Resilience following spinal cord injury: A prospective controlled study investigating the influence of the provision of group cognitive behavior therapy during inpatient rehabilitation. Rehabil. Psychol. 2015;60:311–321. doi: 10.1037/rep0000052. [DOI] [PubMed] [Google Scholar]
- 23.Guest R., Craig A., Tran Y., Middleton J. Factors predicting resilience in people with spinal cord injury during transition from inpatient rehabilitation to the community. Spinal Cord. 2015;53:682–686. doi: 10.1038/sc.2015.32. [DOI] [PubMed] [Google Scholar]
- 24.Kilic S.A., Dorstyn D.S., Guiver N.G. Examining factors that contribute to the process of resilience following spinal cord injury. Spinal Cord. 2013;51:553–557. doi: 10.1038/sc.2013.25. [DOI] [PubMed] [Google Scholar]
- 25.White B., Driver S., Warren A.M. Resilience and indicators of adjustment during rehabilitation from a spinal cord injury. Rehabil. Psychol. 2010;55:23–32. doi: 10.1037/a0018451. [DOI] [PubMed] [Google Scholar]
- 26.Fekete C., Eriks-Hoogland I., Baumberger M., Catz A., Itzkovich M., Lüthi H., Post M.W., von Elm E., Wyss A., Brinkhof M.W. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III) Spinal Cord. 2013;51:40–47. doi: 10.1038/sc.2012.87. [DOI] [PubMed] [Google Scholar]
- 27.Bonavita J., Torre M., China S., Bressi F., Bonatti E., Capirossi R., Tiberti S., Olivi S., Musumeci G., Maietti E., et al. Validation of the Italian version of the Spinal Cord Independence Measure (SCIM III) Self-Report. Spinal Cord. 2016;54:553–560. doi: 10.1038/sc.2015.187. [DOI] [PubMed] [Google Scholar]
- 28.Mercer S.W., Reynolds W.J. Empathy and quality of care. Br. J. Gen. Pract. 2002;52:S9–S12. [PMC free article] [PubMed] [Google Scholar]
- 29.Mercer S.W., McConnachie A., Maxwell M., Heaney D., Watt G.C. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam. Pract. 2005;22:328–334. doi: 10.1093/fampra/cmh730. [DOI] [PubMed] [Google Scholar]
- 30.Mercer S.W., Hatch D.J., Murray A., Murphy D.J., Eva K.W. Capturing patients’ views on communication with anaesthetists: The CARE Measure. Clin. Gov. Int. J. 2008;13:128–137. doi: 10.1108/14777270810867320. [DOI] [Google Scholar]
- 31.Mercer S.W., Murphy D.J. Validity and reliability of the CARE Measure in secondary care. Clin. Gov. Int. J. 2008;13:269–283. doi: 10.1108/14777270810912969. [DOI] [Google Scholar]
- 32.Mercer S.W., Neumann M., Wirtz M., Fitzpatrick B., Vojt G. General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland—a pilot prospective study using structural equation modeling. Patient Educ. Couns. 2008;73:240–245. doi: 10.1016/j.pec.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 33.Consultation and Relational Empathy (CARE) Measure. [(accessed on 6 April 2024)]. Available online: https://caremeasure.stir.ac.uk.
- 34.Natali F., Corradini L., Sconza C., Taylor P., Furlan R., Mercer S.W., Gatti R. Development of the Italian version of the Consultation and Relational Empathy (CARE) measure: Translation, internal reliability, and construct validity in patients undergoing rehabilitation after total hip and knee arthroplasty. Disabil. Rehabil. 2023;45:703–708. doi: 10.1080/09638288.2022.2037742. [DOI] [PubMed] [Google Scholar]
- 35.Di Fabio A., Palazzeschi L. Connor-Davidson Resilience Scale: Proprietà psicometriche della versione italiana. Couns. G. Ital. Ric. Appl. 2012;5:101–110. [Google Scholar]
- 36.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Routledge; London, UK: 1988. [DOI] [Google Scholar]
- 37.Scholten E.W.M., POWER Group. Simon J.D.H.P., van Diemen T., Hillebregt C.F., Ketelaar M., Woldendorp K.H., Osterthun R., Visser-Meily J.M.A., Post M.W.M. Appraisals and coping mediate the relationship between resilience and distress among significant others of persons with spinal cord injury or acquired brain injury: A cross-sectional study. BMC Psychol. 2020;8:51. doi: 10.1186/s40359-020-00419-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shin J.-I., Chae J.-H., Min J.-A., Lee C.-U., Hwang S.-I., Lee B.-S., Han S.-H., Ju H.-I., Lee C.-Y. Resilience as a possible predictor for psychological distress in chronic spinal cord injured patients living in the community. Ann. Rehabil Med. 2012;36:815–820. doi: 10.5535/arm.2012.36.6.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhattarai M., Maneewat K., Sae-Sia W. Psychosocial factors affecting resilience in Nepalese individuals with earthquake-related spinal cord injury: A cross-sectional study. BMC Psychiatry. 2018;18:60. doi: 10.1186/s12888-018-1640-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Battalio S.L., Tang C.L., Jensen M.P. Resilience and Function in Adults with Chronic Physical Disabilities: A Cross-Lagged Panel Design. Ann. Behav. Med. 2020;54:297–307. doi: 10.1093/abm/kaz048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Divanoglou A., Tasiemski T., Jörgensen S. INTERnational Project for the Evaluation of “activE Rehabilitation” (inter-PEER)-a protocol for a prospective cohort study of community peer-based training programmes for people with spinal cord injury. BMC Neurol. 2020;20:14. doi: 10.1186/s12883-019-1546-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chung D.X.Y., Loo Y.E., Kwan Y.H., Phang J.K., Woon T.H., Goh W.R., Angkodjojo S., Fong W. Association of anxiety, depression and resilience with overall health and functioning in axial spondyloarthritis (axSpA): A cross-sectional study. BMJ Open. 2023;13:e071944. doi: 10.1136/bmjopen-2023-071944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuzu D., Kallen M.A., Kratz A.L. Psychometric Properties of the Spinal Cord Injury-Quality of Life (SCI-QOL) Resilience Short Form in a Sample with Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2023;105:59–66. doi: 10.1016/j.apmr.2023.10.002. [DOI] [PubMed] [Google Scholar]
- 44.Windle G., Bennett K.M., Noyes J. A methodological review of resilience measurement scales. Health Qual. Life Outcomes. 2011;9:8. doi: 10.1186/1477-7525-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Donoghue E.M., Sturtevant V.E. Social science constructs in ecosystem assessments: Revisiting community capacity and community resiliency. Soc. Nat. Resour. 2007;20:899–912. doi: 10.1080/08941920701561114. [DOI] [Google Scholar]
- 46.Sisto A., Vicinanza F., Campanozzi L.L., Ricci G., Tartaglini D., Tambone V. Towards a Transversal Definition of Psychological Resilience: A Literature Review. Medicina. 2019;55:745. doi: 10.3390/medicina55110745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lakhani A., Dema S., Hose J., Erdem N., Wollersheim D., Grindrod A., Grimbeek P., Charlifue S. Predictors of resilience for people with spinal cord injury over two periods of COVID-19 social distancing restrictions: A 12-month longitudinal study using structural equation modelling. BMC Public Health. 2023;23:1334. doi: 10.1186/s12889-023-16238-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.