Abstract
Tissue factor (TF) is a transmembrane glycoprotein that represents the fundamental physiological initiator of the coagulation cascade through its interaction with factor VII. TF belongs to the cytokine receptor protein superfamily and contributes to the transduction of cellular signaling. Therefore, TF-related pathways are involved in multiple pathophysiological processes, not only in coagulation/thrombosis but in a wider mechanisms’ panorama, ranging from infective to neoplastic diseases. Consistently, the measurement of TF activity could have a diagnostic and/or prognostic meaning in different clinical conditions. However, the transmembrane localization, the expression on different cellular types and circulating extracellular vesicles, and the different conformations (encrypted and decrypted) and variants (such as the soluble alternatively spliced TF) hamper TF assessment in clinical practice. The activated factor VII-antithrombin (FVIIa–AT) complex is proposed as an indirect biomarker of the TF–FVIIa interaction and, consequently, of the functionally active TF expression. In this narrative review, we evaluate the clinical studies investigating the role of plasma concentration of FVIIa–AT in health and disease. Although without conclusive data, high FVIIa–AT concentrations predict the worst clinical outcomes in different pathologic conditions, such as cardiovascular disease and cancer, thereby suggesting that overactivation of TF-related pathways may play an unfavorable role in various clinical settings.
Keywords: activated factor VII–antithrombin complex (FVIIa–AT), cancer, cardiovascular disease (CAD), coagulation, SARS-CoV-2 infection, preeclampsia, tissue factor (TF), venous thromboembolism (VTE)
1. The Crucial Roles of Tissue Factor: Haemostasis and Beyond
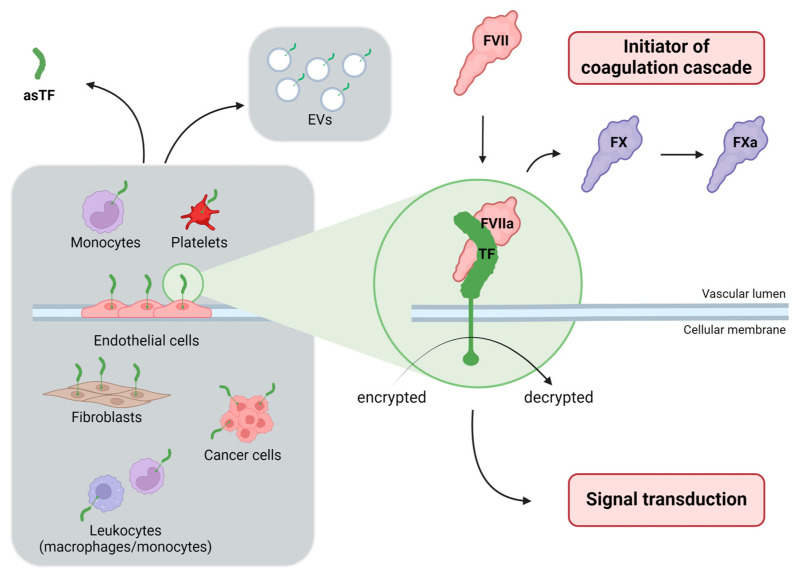
Tissue factor (TF) is a transmembrane glycoprotein belonging to the cytokine receptor protein superfamily, historically known as the initiator of the extrinsic pathway of the coagulation cascade and the major cellular activator of the clotting cascade [1]. The crucial role of TF is well illustrated by the reports that, by attempting to generate TF knock-out mice models, have shown a severe lethality of TF−/− embryos, thus suggesting that TF is biologically indispensable for life [1]. The full-length, transmembrane TF molecule is formed by three different domains: (i) an extracellular domain at the N-terminal involved in the interaction with coagulation factor VII (FVII), (ii) a transmembrane domain anchoring TF to the membrane, and (iii) a cytoplasmatic C-terminal domain involved in signal transduction [2]. The full-length TF is typically expressed on vascular smooth muscle cells, fibroblasts, and perivascular cells, where it forms a haemostatic barrier that leads toward a rapid initiation of the coagulation cascade when the blood vessel is damaged [3]. Moreover, TF is expressed by activated leukocytes (monocytes/macrophages) and by stimulated endothelial cells [4], although there are some controversies on the expression of TF by endothelial cells in vivo [5]. Full-length TF can also be found in blood on extracellular vesicles (EVs) derived from a variety of cell types, including platelets, monocytes, and endothelial cells [6], as well as from malignant tumor cells [7] which are further important sources expressing TF [8]. The cellular sources of TF expression are, therefore, multiple and heterogeneous (for a review see Grover SP & Mackman N, Arterioscler Thromb Vasc Biol. 2018 [9]), as summarized in Figure 1.
Figure 1.
The multifaced expression and role of tissue factor (TF). In the context of the crossroad between coagulation cascade and signal transduction, the various cellular sources of TF (on the left), the different isoforms—encrypted and decrypted—(in the middle), and the alternatively spliced forms (soluble and asTF) are shown. Created with BioRender.com. asTF, alternatively spliced tissue factor; EVs, extracellular vesicles; TF, tissue factor.
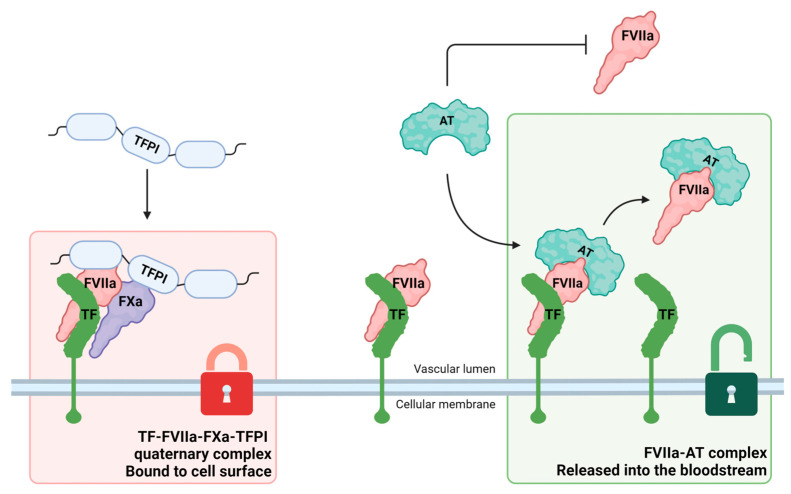
TF is usually expressed on the cellular surface in a quiescent or “encrypted” form, while activation or “decryption” is necessary for procoagulant activity [10]. Experimental observations suggested that decryption involves both the formation of a disulfide bond between unpaired cysteine residues 186 and 209 in encrypted TF and the exposure of phosphatidyl serine on the cellular surface [11]. When functionally active TF is exposed to the bloodstream, it encounters either FVII, converting it to its activated form (FVIIa), or binds FVIIa [12]. Once the TF–FVIIa complex is formed, it can initiate the blood clotting cascade by activating factor X (FX). However, the role of TF is notably not limited to haemostatic function and contributes to signaling in a variety of cells, modulating inflammatory pathways and cellular proliferation [9]. Two different plasmatic inhibitors can interact with the TF–FVIIa complex: tissue factor pathway inhibitor (TFPI) and antithrombin (AT) [12]. The main inhibitor of the TF pathway is TFPI, which first binds to activated FX (FXa) and subsequently forms a tetramolecular complex (TF–FVIIa–TFPI–FXa), which remains stable on the surface of the cell membrane. Moreover, AT can interact with TF–FVIIa forming a FVIIa–AT complex, which detaches from TF and is released from the cell membrane into the bloodstream [12] (Figure 2).
Figure 2.
Modes of action of the main inhibitors of the tissue factor (TF) pathway. Tissue factor pathway inhibitor (TFPI) forms a tetramolecular complex (TF–FVIIa–FXa–TFPI) which remains stable on the surface of the cell membrane (on the left). Antithrombin (AT) reacts with FVIIa only if FVIIa is bound to functionally active TF, thereby forming a FVIIa–AT complex, which is released from the cell membrane into the bloodstream (on the right). Created with BioRender.com. AT, antithrombin; FVIIa, activated factor VII; FXa, activated factor X; FVIIa–AT, activated factor VII-antithrombin; TF, tissue factor; TFPI, tissue factor pathway inhibitor.
Post-transcriptional regulations of TF have also been studied. It is worth noting that an alternatively spliced TF (asTF), which lacks the transmembrane domain and presents an altered C-terminus domain due to the deletion of exon 5, has been described [13]. Alternatively spliced TF is a soluble molecule that can be detected in the bloodstream, although its role remains partially undefined. Remarkably, asTF lacks residues required for interaction with FX and therefore has a reduced procoagulant activity. There is evidence suggesting, however, that asTF may have a greater role in angiogenesis and cancer biology rather than in coagulation and thrombosis [14], thereby favouring tumor growth and metastasis spreading [15,16].
At a post-transcriptional level, several microRNAs (miRNAs) have been reported to modulate TF synthesis in physiological but mostly pathological conditions. Interestingly, miRNAs targeting TF have been then proposed as biomarkers of TF pathway with even potential therapeutic application [17,18].
2. The Difficulty of Evaluating Tissue Factor Activity: Biomarkers Searching for an Elusive Molecule
The multiform and differentiated TF expression explains the difficulties of the laboratory assessment of its activity. According to its transmembrane cellular localization, the direct determination of TF in plasma is not and cannot be a routine assessment in clinical practice. Notably, blood-born TF, if present, is at very low concentration and without procoagulant functional activity [9]. The soluble asTF can be detected in plasma but has negligible procoagulant activity [19]. On the other hand, the full-length TF can be isolated and assessed from EVs released into the bloodstream [20]. Importantly, antigen-based assays cannot differentiate between the two conformational forms of the full-length TF, encrypted (with low procoagulant activity) or decrypted (with high procoagulant activity), and therefore is not an accurate way to measure TF activity [20].
3. Activated Factor VII-Antithrombin Complex as an Indirect Biomarker of Tissue Factor Pathway
The plasma levels of FVIIa–AT have been proposed to indirectly reflect TF–FVIIa interaction and thus TF expression/activity. The biological basis of this assumption refers to biochemical studies that documented the molecular mechanisms by which AT can inhibit the TF–FVIIa complex. The AT reaction with FVIIa was first reported in 1974 [21]. Later, in 1993, it was shown that the interaction between TF–FVIIa greatly enhances the susceptibility of FVIIa to inhibition by AT, thereby suggesting that AT reacts with FVIIa only if FVIIa is bound to functionally active TF [22]. In 1995 it was shown that the decrease in FVIIa levels associated with TF in the presence of AT was the result of the accelerated dissociation of FVIIa from TF after the binding of AT to the TF–FVIIa complexes, thereby suggesting that FVIIa–AT complexes released into the blood correlate directly with functionally active TF expressed [23]. Notably, AT inhibition of TF–FVIIa interaction does not require the presence of FXa, while TFPI cannot inhibit TF–FVIIa interaction without the presence of FXa.
Consistent with these biochemical premises, the FVIIa–AT complex could be considered as an indirect biomarker of the overall TF expression and was seen as a hypothetically useful tool for the assessment of TF activity in health and disease [12]. In 2003, the first patent of an enzyme-linked immunosorbent assay (ELISA) for measuring FVIIa–AT plasma levels was published [24]. Subsequently, some companies developed and commercialized specific ELISA assays with this aim, thus paving the way for more extensive population-based studies in order to assess the clinical significance of the measurement of FVIIa–AT plasma levels.
4. Plasma Concentration of Activated Factor VII-Antithrombin Complex in Different Clinical Settings in Humans
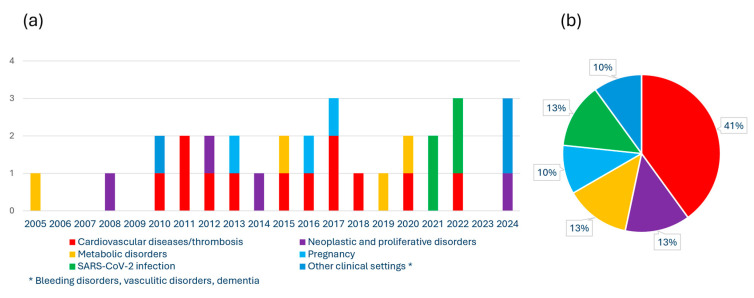
Thirty studies during the last two decades (Figure 3a) have assessed FVIIa–AT plasma concentration in humans, investigating the possible diagnostic and/or prognostic role of this biomarker in different clinical settings.
Figure 3.
Studies investigating plasma-activated factor VII–antithrombin complex (FVIIa–AT) in humans. (a) Distribution of the literature across timeline (20 years); (b) representation of prevalence (%) of the studies according to the different clinical settings.
The majority of these studies focused on cardiovascular diseases/thrombosis and neoplastic disorders (Figure 3b). A detailed description of the main results of these research papers is presented in the following paragraphs and summarized in Table 1.
4.1. Thrombosis and Cardiovascular Disease
The first paper highlighting the indeed plausible association between FVIIa–AT plasma concentrations and thrombotic diseases was published in 2010 by Spiezia and colleagues who found that FVIIa–AT complex levels were lower in patients with acute thrombosis, either arterial or venous, than in those with previous thrombosis or in healthy controls [25]. FVIIa–AT levels correlated strongly and positively with plasma FVIIa activity, which is considered more specific and reliable than FVII coagulant activity [26]. On the other hand, no relevant role of AT plasma levels was observed in predicting FVIIa–AT variability [25]. In a subsequent study conducted on patients with acute deep vein thrombosis (DVT) by using an in-house assay, the FVIIa–AT complex was detected only in a minority of patients (about 10%) and controls (about 30%). In this small subgroup of subjects with detectable FVIIa–AT, the related levels were substantially higher in patients with DVT than in controls [27].
In the setting of portal vein thrombosis (PVT), with or without concomitant liver cirrhosis, it was shown that non-cirrhotic patients with PVT had higher FVIIa–AT levels than healthy controls. On the other hand, no significant differences in FVIIa–AT levels were found between cirrhotic patients with or without PVT, with both groups characterized by lower levels of FVIIa–AT as compared with non-cirrhotic subjects [28]. Noteworthily, in the group of cirrhotic patients characterized by low synthesis of plasma proteins, including FVII and AT, there was a significant positive correlation of FVIIa–AT with both FVII and AT [28]. Similarly, another study investigating HCV-related cirrhosis with or without PVT showed no significant difference in FVIIa–AT levels between cirrhotic patients with or without PVT. Cirrhotic patients with PVT had significantly lower FVIIa–AT levels compared to either non-cirrhotic patients with PVT or healthy controls [29]. These results indicated mainly the presence of low levels of FVIIa–AT in patients with acute thrombotic complications, as well as in those with liver cirrhosis. There was also a strong correlation between FVIIa–AT and FVII/FVIIa levels. Therefore, it appears biologically plausible that conditions which are associated with low FVII/FVIIa levels because of either reduced synthesis (like liver cirrhosis) or increased consumption (like acute thrombosis) can affect FVIIa–AT plasma concentration. Moreover, it is tempting to speculate that such conditions may represent a major confounding factor in the interpretation of FVIIa–AT plasma levels as an indirect biomarker of TF expression and activity.
In 2012, the investigations on the potential clinical significance and prognostic role of FVIIa–AT were extended to cardiovascular disease (CVD). The Stockholm Coronary Atherosclerosis Risk Factor (SCARF) study analysed 200 patients with ischemic heart disease and previous (3–6 months before) myocardial infarction (MI). FVIIa–AT levels were slightly higher in patients with previous MI than in controls even though with a substantial overlap of values [30]. Furthermore, in the Stockholm prospective study of CVD, FVIIa–AT levels had no predictive value for the development of future CVD during a 5-to-7-year follow-up in 60-year-old individuals [30]. Afterwards, in the Italian observational study cohort of the Verona Heart Study (VHS), investigating subjects with or without angiographically demonstrated coronary artery disease (CAD), no difference in FVIIa–AT levels between CAD and CAD-free subjects was found. However, within the group of 546 patients with clinically stable CAD (acute coronary syndrome, as well as any recent acute illness, were exclusion criteria for VHS), during a 64-month median follow-up, subjects with high FVIIa–AT levels (higher than the median value at baseline) had a two-fold greater risk of both total and cardiovascular mortality, independent of traditional confounding factors [31]. Moreover, high FVIIa–AT levels were associated with increased thrombin generation, thereby indicating FVIIa–AT as a marker of prothrombotic diathesis [31]. In a subgroup analysis within the same population, consistent with its role as a thrombophilic biomarker, high FVIIa–AT plasma levels also correlated directly with FXa generation and, notably, the characteristics of hypercoagulability related to FVIIa–AT were specifically detectable in the initiation phase of coagulation [32]. The potential role of FVIIa–AT as a prognostic biomarker was confirmed in the larger cohort of the Cardiovascular Health Study (CHS), a prospective cohort study investigating risk factors for coronary heart disease and stroke [33]. Within the CHS cohort, high levels of FVIIa–AT were associated with an increased risk of mortality from all causes in adults aged 65 years and older. The almost 3500 subjects of the CHS also allowed for a genome-wide association study (GWAS) on genetic determinants of FVIIa and FVIIa–AT in European Americans. The most significant SNP for FVIIa–AT (and also FVIIa) was rs1755685 in the F7 promoter region on chromosome 13, while there was also an association with rs867186 located in PROCR on chromosome 20 [33].
In a further smaller cohort study on 120 CAD patients, FVIIa–AT levels were positively associated with current smoking and multivessel CAD. More relevant from a clinical point of view, CAD patients with a high baseline FVIIa–AT plasma concentration had an increased risk of both ischemic stroke/systemic thromboembolism and the composite endpoint of myocardial infarction, stroke/systemic thromboembolism, and cardiovascular death during a median follow-up of 106 months [34]. FVIIa–AT levels have also been assessed in the setting of cardiac surgery. In a small study of 13 adult patients undergoing cardiac surgery with cardiopulmonary bypass, the pre-surgery concentrations of FVIIa–AT rose about twice as much post-heparin bolus and those higher concentrations were maintained throughout the cardiopulmonary bypass and post-protamine administration time so that it was suggested that AT appeared to play an active role in FVIIa inhibition during cardiac surgery [35]. This small study was not able to distinguish between an increase in TF exposure due to surgery and an increase in the AT binding to FVIIa mediated by heparin, although the latter hypothesis seems suggestive. On the other hand, no definite conclusions could be drawn on a possible prognostic significance of FVIIa–AT levels in this clinical setting. As it refers to cerebrovascular disease, in a study on paediatric patients including 54 children with ischemic stroke (IS) and 7 children with cerebral vein thrombosis (CVT), FVIIa–AT levels were lower in children with acute IS (n = 38) than in healthy children, while those with previous IS (n = 16) or CVT had levels of FVIIa–AT not significantly higher than healthy children [36]. In this paediatric population, FVIIa activity plasma levels were directly correlated with FVIIa–AT plasma levels [36]. FVIIa–AT levels were significantly lower also in 33 adult subjects with acute ischemic stroke (of whom 13 underwent thrombolysis with rtPA) than in age-matched controls [37].
4.2. Neoplastic and Proliferative Disorders
A study assessing 93 patients with haematological malignancies (acute myeloid leukaemia, chronic lymphatic leukaemia, multiple myeloma, non-Hodgkin’s lymphoma) found no difference in baseline FVIIa–AT plasma concentrations between haematological cases and healthy controls. On the other hand, FVIIa–AT levels increased during the follow-up after cancer treatment [38]. In the few haematological patients (n = 4) who had a previous venous thrombosis (VT), FVIIa–AT levels were lower at baseline, while those with VT after diagnosis of malignancy (n = 8) had no difference in FVIIa–AT levels as compared with patients without malignancy [38]. In contrast, a study on essential thrombocythemia, a well-known chronic myeloproliferative neoplasm, showed different results [39]. FVIIa–AT levels were significantly higher in 73 patients with essential thrombocythemia, in particular in those positive for the JAK2V617F mutation (n = 37), as compared with controls [39]. With regard to solid cancers, a study including 60 patients with different types of active cancer (gastro-intestinal, breast, pancreatic, prostatic, lung, liver, cerebral) with or without acute venous thromboembolism (VTE) showed that patients with active cancer and without acute VTE had significantly higher FVIIa–AT levels than controls, while patients with acute VTE, either unprovoked or with active cancer, had lower FVIIa–AT levels than controls [40].
In a recent study on 136 Italian patients with different types of liver cancer, i.e., hepatocellular carcinoma, cholangiocarcinoma, and metastasis of colon cancer, FVIIa–AT plasma concentrations were more elevated in cancer patients than among sex- and age-matched controls and differed among the specific types of cancer with the highest levels in patients with cholangiocarcinoma [41]. Most importantly, high FVIIa–AT levels were associated with high TF mRNA levels in cancer tissue, thus supporting the concept of FVIIa–AT as a reliable marker of TF expression at the cellular level [41]. Finally, high FVIIa–AT levels predicted an increased risk of mortality in the cancer population during a 34-month median follow-up, thereby suggesting that FVIIa–AT may allow the identification of patients with cancer characterized by an enhanced TF expression and a greater risk of mortality [41].
4.3. Metabolic Disorders
A series of studies assessed FVIIa–AT levels also in the setting of metabolic disorders, which are well recognized as traditional cardiovascular risk factors. A study evaluating both FVIIa–AT and thrombin generation was performed in 80 overweight and obese patients, asymptomatic for thrombotic events, i.e., 20 overweight subjects (BMI range 25–29.9 kg/m2), 20 subjects with I degree obesity (BMI range 30–34.9 kg/m2), 20 subjects with II degree obesity (BMI range 35–39.9 kg/m2), and 20 subjects with III degree obesity (BMI ≥ 40 kg/m2). No significant difference in FVIIa–AT levels was found between overweight/obese patients and controls [42]. On the other hand, the obese patients showed higher peak thrombin as compared to controls [42]. In a small controlled cross-over study on 20 obese patients, in whom high-fat and low-fat meals were served, FVIIa–AT levels, along with FVIIa and triglycerides, increased significantly after high-fat meals and low-fat meals with the largest increase after high-fat meals [43].
Within the frame of the Italian angiographically-controlled study cohort of the Verona Heart Study (VHS), the plasma concentration of FVIIa–AT significantly and directly correlated with total and high-density lipoprotein cholesterol, triglycerides, ApoA-I, ApoC-III, and ApoE levels [44]. More precisely, ApoC-III showed the strongest correlation with FVIIa–AT levels, even in multiple adjusted models [44]. FVIIa–AT complex was also used as a tool to explore TF expression in different experimental settings. In a study including nine patients with type 1 diabetes who received 20 infusions of isolated human islets of Langerhans, FVIIa–AT levels increased rapidly within 15–60 min after islet infusion and correlated negatively with the change in C-peptide over 7 days [45]. Based on these data and further results, it was hypothesized that TF produced by the cells of the islets of Langerhans elicited an instant blood-mediated inflammatory reaction, thereby being associated with a negative outcome of clinical islet transplantation [45].
4.4. SARS-CoV-2 Infection
In the last years, the pandemic caused by SARS-CoV-2 infection renewed interest in a better understanding of the complex interconnections between immune response, inflammation, clotting, and thrombosis, which are now collected under the term immunothrombosis. Acute and severe infections, like those leading to septic shock, are well known to be generally associated with several alterations in coagulation mechanisms, including an increase in the expression and activity of TF [46,47]. However, to the best of our knowledge, the specific assessment of FVIIa–AT during infectious diseases was performed just in patients with SARS-CoV-2 infection so far. Francischetti and colleagues analysed 66 adult COVID-19 patients at the Johns Hopkins Hospital having moderate (n = 40) and severe disease (n = 26). FVIIa–AT levels were significantly higher in COVID-19 patients with severe disease than in controls negative for SARS-CoV-2 infection, with intermediate levels in COVID-19 patients with moderate disease [48]. Similar results were shown in an Italian case-control study on 40 subjects with SARS-CoV-2 pneumonia during the first pandemic wave, compared to 40 historic non-COVID-19 controls with inflammation and 40 historic non-COVID-19 controls without inflammation [49]. FVIIa–AT levels were higher in COVID-19 patients than in non-COVID-19 subjects, either with or without inflammation, while no difference was observed among non-COVID-19 subjects [49]. In 203 Dutch patients with previous acute COVID-19, FVIIa–AT levels were still increased in a third of the patients (35%) 6–20 weeks after recovery, confirming a sustained and long-term activation of coagulation mechanisms in COVID-19 [50]. FVIIa–AT plasma concentration was also measured, by means of an in-house developed assay, in 40 adult healthcare workers before and after (1–2 days) the first dose of ChAdOx1 vaccination against SARS-CoV-2 [51]. FVIIa–AT levels were significantly decreased after vaccination suggesting that, generally, the first dose of ChAdOx1 vaccination does not lead to an activation of the TF pathway [51].
Table 1.
Studies assessing plasma levels of FVIIa–AT in humans in different clinical settings.
| Thrombosis and Cardiovascular Disorders (CVD) | |||
| Type of Study | Study Population | FVIIa–AT-Related Main Results | Reference |
| Case-control study |
|
|
Spiezia L et al., 2010 [25] |
| Case-control study |
|
|
Spiezia L et al., 2011 [36] |
| Cohort study |
|
|
Davidson SJ and Woodhams B, 2011 [35] |
| Case-control study and Cohort Study with nested case-control design |
Stockholm Coronary Atherosclerosis Risk Factor (SCARF) study
Stockholm prospective study of 60-year-olds individuals
|
|
Silveira A et al., 2012 [30] |
| Case-control study |
|
|
Rossetto V et al., 2013 [28] |
| Case-control study |
|
FVIIa–AT plasma concentration was measured using an in-house developed assay and was detected only in a minority of patients (n = 16, 11%) and controls (n = 58, 33%). In these individuals the related levels were substantially higher in patients with DVT than in controls. | Schut AM et al., 2015 [27] |
| Case-control study and Longitudinal Cohort study |
Verona Heart Study (VHS)
|
|
Martinelli N et al., 2016 [31] |
| Case-control study |
|
FVIIa–AT levels were significantly lower in patients with IS than in controls. | Slomka A et al., 2017 [37] |
| Case-control study |
|
|
Abu El-Makarem MA et al., 2017 [29] |
| Prospective Cohort studyGenome-wide association study (GWAS) of FVIIa and FVIIa–AT |
Cardiovascular Health Study (CHS) in European-Americans adults aged 65-years and older
|
|
Olson NC et al., 2018 [33] |
| Observational study |
|
|
Baroni M et al., 2020 [32] |
| Longitudinal Cohort study |
|
|
Paszek E et al., 2022 [34] |
| Neoplastic and Proliferative Disorders | |||
| Type of Study | Study Population | FVIIa–AT-Related Main Results | Reference |
| Case-control study |
|
|
Negaard HFS et al., 2008 [38] |
| Retrospective case-control study |
|
|
Spiezia L et al., 2012 [40] |
| Case-control study |
|
FVIIa–AT levels were significantly elevated in patients with essential thrombocythemia, in particular those positive for the JAK2V617F mutation, as compared with controls. | Marchetti M et al., 2014 [39] |
| Case-control study and Longitudinal Cohort study |
|
|
Martinelli N et al., 2024 [41] |
| Metabolic Disorders | |||
| Type of Study | Study Population | FVIIa–AT-Related Main Results | Reference |
| Experimental study |
|
|
Johansson H et al., 2005 [45] |
| Case-control study |
|
|
Campello E et al., 2015 [42] |
| Observational study |
Verona Heart Study (VHS)
|
|
Martinelli N et al., 2019 [44] |
| Controlled cross-over study | 20 obese patients, in whom high-fat and low-fat meals were served |
|
Landgrebe LE et al., 2020 [43] |
| SARS-CoV-2 Infection | |||
| Type of Study | Study Population | FVIIa–AT-Related Main Results | Reference |
| Case-control study |
|
FVIIa–AT levels were significantly higher in COVID-19 patients with severe disease than in controls, with intermediate levels in COVID-19 patients with moderate disease. | Francischetti IMB et al., 2021 [48] |
| Cohort study |
|
FVIIa–AT plasma levels (measured using an in-house developed assay) were significantly decreased after vaccination. | Willems LH et al., 2021 [51] |
| Cross-sectional Cohort study |
|
FVIIa–AT levels were increased in a third of the patients (35%) 6–20 weeks after recovery of acute COVID-19. | Willems LH et al., 2022 [50] |
| Case-control study |
|
FVIIa–AT levels were higher in COVID-19 patients than in non-COVID-19 subjects, either with or without inflammation, while no difference was observed among non-COVID-19 subjects. | Martinelli N et al., 2022 [49] |
| Pregnancy and Preeclampsia | |||
| Type of Study | Study Population | FVIIa–AT-Related Main Results | Reference |
| Case-control study |
|
|
Spiezia L. et al., 2013 [52] |
| Case-control study |
|
FVIIa–AT levels were not different between severe preeclamptic and normotensive pregnant women. | Alpoim PN et al., 2016 [53] |
| Cohort study |
|
Increased FVIIa–AT levels were found in early severe preeclampsia compared to late severe preeclampsia. | Dusse LMS et al., 2017 [54] |
| Other Clinical Settings | |||
| Type of Study | Study Population | FVIIa–AT-Related Main Results | Reference |
| Cohort study for a population pharmacokinetic model |
|
The rFVII–AT complex formation was responsible for 65% of the total rFVIIa clearance. The formation of rFVIIa–AT complex was able to explain the difference observed between the rFVIIa:C and the rFVII:Ag concentration. | Agerso H et al., 2010 [55] |
| Longitudinal Cohort study |
|
|
Busch MH et al., 2024 [56] |
| Prospective Cohort study | Cardiovascular Health Study (CHS) in adults—3185 older adults (aged 65-years and older) free of dementia in 1992/1993 | There was no evidence of linear associations between FVIIa–AT levels with any dementia risk. | Harrington LB et al., 2024 [57] |
Abbreviations: CVD, Cardiovascular Disorders; AT, Antithrombin; IS, Ischemic Stroke; CVT, cerebral vein thrombosis; MI, myocardial infarction; PVT, portal vein thrombosis; DVT, deep venous thrombosis; CAD, coronary artery disease; VT, venous thrombosis; VTE, acute venous thromboembolism; rFVIIa, recombinant human factor VIIa.
4.5. Pregnancy and Preeclampsia
The modifications of coagulation during pregnancy, usually involving a shift toward a hypercoagulable state, are well known, as well as the potential role of blood clotting in many pregnancy-related diseases. The first study investigating FVIIa–AT levels in pregnancy analysed 105 pregnant women, 30 in the first trimester, 30 in the second trimester, 30 in the third trimester, and 15 with pre-eclampsia [52]. Higher FVIIa–AT plasma levels were found in pregnant women than in healthy non-pregnant women. Women with pre-eclampsia had a significantly higher FVIIa–AT/FVIIa ratio than pregnant women in the third trimester, but no significant difference in FVIIa–AT levels between pregnant women in the third trimester and those with pre-eclampsia was found [52]. Similarly, in a cohort study comparing the concentration of FVIIa–AT between 108 severe preeclamptic women and 104 normotensive pregnant women, FVIIa–AT levels were not different between severe preeclamptic and normotensive pregnant women [53]. Finally, increased FVIIa–AT levels have been detected in 26 pregnant women with early (gestational age < 34 weeks) severe preeclampsia compared to 19 with late (gestational age ≥ 34 weeks) severe preeclampsia, thus suggesting a higher TF-related hypercoagulability in early preeclampsia [54].
4.6. Other Clinical Settings
The assessment of FVIIa–AT plasma levels has also been used in other clinical contexts and diseases. In a cohort study which aimed to characterize the pharmacokinetics of recombinant human factor VIIa (rFVIIa) in haemophilia patients, 10 subjects with severe FVIII or FIX deficiency were treated with rFVIIa [55]. The rFVIIa–AT complex formation was responsible for 65% of the total rFVIIa clearance. The formation of the FVII–AT complex was able to explain the difference observed between the recombinant FVIIa activity (rFVIIa:C) and the antigen (rFVII:Ag) concentration [55]. In a recent study on venous thrombotic risk in patients with antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis, coagulation parameters were assessed at presentation with active disease and at follow-up after 6 months of treatment in 71 patients [56]. FVIIa–AT levels were normal in the majority of patients (90%) at baseline and further slightly decreased over time. Four of 71 (6%) had a history of VTE and five had VTE symptomatic after presentation. No difference in FVIIa–AT levels was found between patients with or without VTE [56]. Finally, within the frame of the previously mentioned Cardiovascular Health Study (CHS), in a cohort of adults aged 65 years and older and free of dementia in 1992/1993 (n = 3185), there was no evidence of linear associations of FVIIa–AT levels with any dementia risk [57].
5. Correlations with Other Clinical and Laboratory Parameters
FVIIa–AT levels have been found to correlate directly with peak and endogenous thrombin potential (ETP) levels by thrombin generation analysis, with high FVIIa–AT plasma concentration associated with increased peak and ETP levels [31]. Similarly, high FVIIa–AT plasma levels were related to increased FXa generation, with hypercoagulability features specifically detectable in the coagulation initiation phase [32]. Such results consistently indicate FVIIa–AT as a thrombophilic biomarker, with high levels correlated with a procoagulant/prothrombotic diathesis. Beyond the expected and strong correlation with FVII/FVIIa, which was often the main predictor of FVIIa–AT variability [31,33], FVIIa–AT plasma levels have been found to relate to other clinical and laboratory parameters. An inverse correlation with renal function (the lowest the renal function, the highest the FVIIa–AT levels) has been described [31]. Similarly, chronic kidney disease is well known to be associated with an increase in FVII activity due not only to altered renal clearance but also to potentially procoagulant endothelial dysfunction [58]. Multiple direct correlations of FVIIa–AT with plasma lipid and apolipoprotein profile (total and high-density lipoprotein cholesterol, triglycerides, ApoA-I, ApoC-III, and ApoE) have been reported [31,33,44] and, notably, low-density lipoprotein (LDL) receptor-related protein 1 (LRP1) may contribute to the clearance of FVIIa–AT complex in vivo [59]. Direct correlation with inflammatory markers, like C reactive protein (CRP), has been also reported, as well as direct associations with current smoking, systolic blood pressure, and female gender [33]. On the one hand, all these associations support the concept that different conditions, including many traditional cardiovascular risk factors, are associated with an overall increased TF expression/activity. On the other hand, such associations should remind us how FVIIa–AT plasma levels can be influenced by multiple conditions that can act as possible confounding factors in evaluating its real clinical significance and prognostic impact. However, it is worth noting that, in the prospective and longitudinal studies evaluating the prognosis in patients with cardiovascular disease or cancer, high FVIIa–AT plasma levels remained a significant and independent predictor of mortality, even after multiple adjustments for potential concomitant risk factors [31,33,41].
6. Strengths, Limitations, and Perspectives for Using FVIIa–AT to Explore the TF-Related Pathway
FVIIa–AT plasma concentrations, as an indirect marker of TF–FVIIa interaction, may overcome the difficulties related to the evaluation of a transmembrane molecule like TF, which is usually not directly detected in plasma (with the notable exception of EV-associated TF), has alternatively spliced forms (like the soluble asTF), and exists in different (encrypted and decrypted) conformations. As regards the last issue, it should be noted that TF conformations are not discriminated by antigenic assays which cannot distinguish the different isoforms and measure all forms of TF without giving functional information.
However, there are certainly many significant limitations which should be taken into account when considering FVIIa–AT as a potential biomarker of the TF pathway:
-
(i)
FVIIa–AT plasma levels can be informative on the global TF–FVIIa interaction but are unable to disentangle the different cellular origins of TF expression/activity (e.g., EVs, platelets, monocytes, activated endothelial cells, neoplastic cells, etc.) which may have significant pathophysiological and different clinical implications;
-
(ii)
The method for measuring FVIIa–AT complex concentration requires standardisation, for the pre-analytical and analytical phases, in order to ensure greater reproducibility and comparability of the results. Taking into account that activated platelets can express TF [60] and how platelets can be triggered/activated during blood drawn [61], the compliance with procedures to limit platelet activation during blood sampling and the appropriate preparation of platelet-poor plasma (PPP) samples would be crucial to avoid further confounding elements in FVIIa–AT evaluation;
-
(iii)
Up to now, all the studies in humans showed a large range of overall distribution of FVIIa–AT plasma levels, as well as a substantial overlap of values between pathological cases and healthy controls. Therefore, any potential for diagnostic sensitivity and specificity appears to be limited;
-
(iv)
The plasma levels of FVIIa–AT are strongly influenced by those of FVII/FVIIa, which have been indicated among the main determinants of FVIIa–AT concentration in many studies [25,31,33]. Consistently, several clinical conditions are recognized to be related to low levels of FVII/FVIIa by means of either reduced synthesis (e.g., genetic variants leading to low FVII expression, liver cirrhosis, VKAs therapy) or increased consumption (e.g., acute thrombosis, disseminated intravascular coagulation), and have been also associated with low levels of FVIIa–AT [25,28,29,30,33]. Such decrease, which is mediated predominantly by FVII levels (and not by TF–FVIIa interaction), could affect the value of the FVIIa–AT assay as an efficacious biomarker of TF activity and likely limits its prognostic role. For instance, in previous studies, FVIIa–AT discriminated between subjects with or without portal vein thrombosis only among non-cirrhotic subjects, while cirrhotic patients with or without portal vein thrombosis had similarly very low levels of FVIIa–AT [28,29];
-
(v)
Many traditional laboratory parameters, from renal function to plasma lipid profile, have been shown to predict FVIIa–AT variability, also consistently with the effects on FVII/FVIIa, thus raising the clinical suspicion that the FVIIa–AT-related prognostic role may be merely an epiphenomenon of the changes and imbalances of other traditional and crucial cardiovascular risk factors [31,43,44].
According to all these considerations, it could be hypothesized that, in order to optimise the relevance of FVIIa–AT as an indirect marker of TF activity, the sampling time for plasma assays should be after a night of fasting (to avoid the potential interference of fat-containing meals) in clinically stable subjects (without any acute thrombotic events), not taking drugs reducing FVII levels (like VKAs) or with concomitant medical condition reducing FVII and FVIIa–AT levels (like advanced liver disease or disseminated intravascular coagulation). The potential influence related to renal failure and hyperlipidaemia, both associated with higher FVIIa–AT levels, should also be taken into account.
Nonetheless, in spite of all these limitations and confounding factors, it is intriguing to observe that the levels of FVIIa–AT are increased in many different illnesses, from cardiovascular to thrombotic diseases, from cancer to infection, and—most importantly—such an increase could predict a worse prognosis in the specific clinical settings [31,33,41]. Actually, it appears biologically plausible that TF overexpression could be unfavourable and potentially detrimental in pathophysiological pathways characterized by prothrombotic diathesis, excessive stimulation of inflammatory pathways, or inappropriate cellular proliferation. From a pragmatic point of view, the capability of the FVIIa–AT complex to be a global marker of the TF–FVIIa interaction, even if not able to better characterize and differentiate the cellular origins of such an interaction, could allow us to intercept a background signal of hyperactivation of the TF pathway and potentially overcome the limitations related to a restricted assessment of TF activity (e.g., that related to extracellular vesicles (EVs)). In our previous work in patients with liver cancer, FVIIa–AT levels but not EV-associated TF-dependent procoagulant activity predicted the risk of overall mortality and no correlation was found between FVIIa–AT levels and EV-associated TF-dependent procoagulant activity, thus suggesting that, in this study population, TF-positive EVs were not the main source of TF–FVIIa interaction [41].
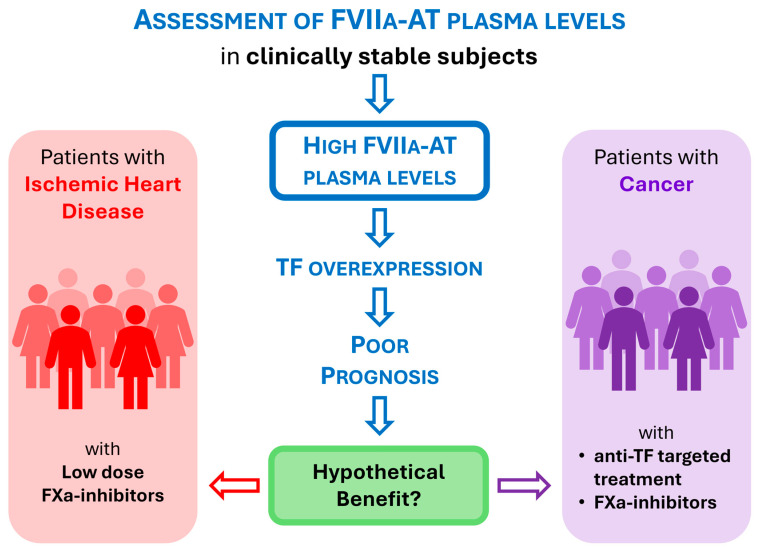
Notably, a laboratory biomarker able to identify patients with high expression/TF activity may have not only prognostic but also therapeutic implications and may pave the way for more patient-tailored management of disease. In 2016, according to the prognostic role of FVIIa–AT in our cohort of patients with clinically stable CAD, we hypothesized the possible beneficial use of oral direct FXa inhibitors in patients with high FVIIa–AT levels, by blocking the excess of FX activation mediated by the FVIIa–TF pathway [31]. In 2017, the COMPASS trial showed that low doses of the FXa-inhibitor rivaroxaban, 2.5 mg twice daily, plus aspirin, led to better cardiovascular outcomes than aspirin alone in patients with stable atherosclerotic vascular disease; although, it also increased the risk of major bleeding [62]. Now, we could further speculate that FVIIa–AT assessment may allow the identification of the subgroup of stable CAD patients who can have the major benefit from a more aggressive antithrombotic treatment associating antiplatelet agents and FXa-inhibitors (Figure 4).
FXa-inhibitors have been also proposed to have an anti-neoplastic role, consistent with the observation that coagulation factors contribute to cancer immune evasion [63,64]. The FXa-inhibitor rivaroxaban has been shown to have anti-neoplastic synergistic effects with immune checkpoint inhibitors (ICIs) in a real-world cohort of patients with metastatic melanoma [65]. According to these considerations, also in the setting of neoplastic disease, we could hypothesize that high FVIIa–AT plasma levels may allow us to identify patients with cancer overexpressing TF who can receive major benefits from such treatment approaches or specifically from anti-TF molecularly targeted treatment against malignant cells (Figure 4). With regards to the latter issue, it is worth noting that tisotumab vedotin, an antibody–drug conjugate combining an anti-TF monoclonal antibody and an inhibitor of cell division, has been approved for the treatment of cervical cancer as a first-in-class medication [66,67].
Figure 4.
Potential benefit of plasmatic FVIIa–AT assessment in clinical practice. Hypothesis of the use of plasma FVIIa–AT levels in the management of patients with different medical conditions (cardiovascular disease/cancer). Speculatively, cardiovascular patients with high FVIIa-AT levels could have a more favourable benefit/risk ratio from treatment with low dose of FXa-inhibitors [62]. Similarly, cancer patients with high FVIIa-AT levels could have a more favourable benefit/risk ratio from treatment with FXa-inhibitors [65] or with specific anti-TF targeted therapies [66].
7. Conclusions
In summary, FVIIa–AT plasma concentrations appear so far as an imperfect though biologically sound biomarker of a TF-related pathway that can be clinically useful given that elevated levels are associated with procoagulant diathesis and worse clinical outcomes. Current data so far do not suggest diagnostic relevance, consistently with the lack of specificity and the wide distribution range of this biomarker, but rather a potential role in the prognostic stratification of patients with well-defined clinical conditions in whom TF overexpression may have harmful effects (like cardiovascular disease or cancer). Certainly, the biological and clinical role of FVIIa–AT should be further investigated and eventually validated by future larger studies, preferentially with prospective design and taking into account the large variability and the multiple conditions potentially influencing this biomarker. Nonetheless, the present data suggest that the assessment of FVIIa–AT, when properly weighed according to the clinical settings and avoiding potential confounding factors, may contribute to shedding light on the relevance of the TF-related pathway in health and disease and, thereby, better and more patient-tailored disease management. This could be obtained, speculatively, by identifying subjects with high TF expression/activity who may have the most favourable benefit–risk ratio when considering treatment with—for instance—either FXa inhibitors or TF-directed therapies (Figure 4).
Acknowledgments
This work was performed (in part) in the LURM (Laboratorio Universitario di Ricerca Medica) Research Center, University of Verona (Italy).
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research was funded by Italian Ministry of University and Research (MUR), PRIN 2022, grant number 2022XZBHYS, CUP B53D23008450006.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Mackman N. Role of Tissue Factor in Hemostasis, Thrombosis, and Vascular Development. Arterioscler. Thromb. Vasc. Biol. 2004;24:1015–1022. doi: 10.1161/01.ATV.0000130465.23430.74. [DOI] [PubMed] [Google Scholar]
- 2.Butenas S. Tissue Factor Structure and Function. Scientifica (Cairo) 2012;2012:964862. doi: 10.6064/2012/964862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drake T.A., Morrissey J.H., Edgington T.S. Selective Cellular Expression of Tissue Factor in Human Tissues. Implications for Disorders of Hemostasis and Thrombosis. Am. J. Pathol. 1989;134:1087–1097. [PMC free article] [PubMed] [Google Scholar]
- 4.Kaneko T., Fujii S., Matsumoto A., Goto D., Makita N., Hamada J., Moriuchi T., Kitabatake A. Induction of Tissue Factor Expression in Endothelial Cells by Basic Fibroblast Growth Factor and Its Modulation by Fenofibric Acid. Thromb. J. 2003;1:6. doi: 10.1186/1477-9560-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steffel J., Lüscher T.F., Tanner F.C. Tissue Factor in Cardiovascular Diseases. Circulation. 2006;113:722–731. doi: 10.1161/CIRCULATIONAHA.105.567297. [DOI] [PubMed] [Google Scholar]
- 6.Owens A.P., Mackman N. Microparticles in Hemostasis and Thrombosis. Circ. Res. 2011;108:1284–1297. doi: 10.1161/CIRCRESAHA.110.233056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baroni M., Pizzirani C., Pinotti M., Ferrari D., Adinolfi E., Calzavarini S., Caruso P., Bernardi F., Di Virgilio F. Stimulation of P2 (P2X 7) Receptors in Human Dendritic Cells Induces the Release of Tissue Factor-bearing Microparticles. FASEB J. 2007;21:1926–1933. doi: 10.1096/fj.06-7238com. [DOI] [PubMed] [Google Scholar]
- 8.Koizume S., Miyagi Y. Tissue Factor in Cancer-Associated Thromboembolism: Possible Mechanisms and Clinical Applications. Br. J. Cancer. 2022;127:2099–2107. doi: 10.1038/s41416-022-01968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grover S.P., Mackman N. Tissue Factor: An Essential Mediator of Hemostasis and Trigger of Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2018;38:709–725. doi: 10.1161/ATVBAHA.117.309846. [DOI] [PubMed] [Google Scholar]
- 10.Bach R.R. Tissue Factor Encryption. Arterioscler. Thromb. Vasc. Biol. 2006;26:456–461. doi: 10.1161/01.ATV.0000202656.53964.04. [DOI] [PubMed] [Google Scholar]
- 11.Chen V.M., Hogg P.J. Encryption and Decryption of Tissue Factor. J. Thromb. Haemost. 2013;11:277–284. doi: 10.1111/jth.12228. [DOI] [PubMed] [Google Scholar]
- 12.Spiezia L., Campello E., Valle F.D., Woodhams B., Simioni P. Factor VIIa-Antithrombin Complex: A Possible New Biomarker for Activated Coagulation. Clin. Chem. Lab. Med. 2017;55:484–488. doi: 10.1515/cclm-2016-0399. [DOI] [PubMed] [Google Scholar]
- 13.Bogdanov V.Y., Balasubramanian V., Hathcock J., Vele O., Lieb M., Nemerson Y. Alternatively Spliced Human Tissue Factor: A Circulating, Soluble, Thrombogenic Protein. Nat. Med. 2003;9:458–462. doi: 10.1038/nm841. [DOI] [PubMed] [Google Scholar]
- 14.Böing A.N., Hau C.M., Sturk A., Nieuwland R. Human Alternatively Spliced Tissue Factor Is Not Secreted and Does Not Trigger Coagulation. J. Thromb. Haemost. 2009;7:1423–1426. doi: 10.1111/j.1538-7836.2009.03521.x. [DOI] [PubMed] [Google Scholar]
- 15.van den Berg Y.W., van den Hengel L.G., Myers H.R., Ayachi O., Jordanova E., Ruf W., Spek C.A., Reitsma P.H., Bogdanov V.Y., Versteeg H.H. Alternatively Spliced Tissue Factor Induces Angiogenesis through Integrin Ligation. Proc. Natl. Acad. Sci. USA. 2009;106:19497–19502. doi: 10.1073/pnas.0905325106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kocatürk B., Van den Berg Y.W., Tieken C., Mieog J.S.D., de Kruijf E.M., Engels C.C., van der Ent M.A., Kuppen P.J., Van de Velde C.J., Ruf W., et al. Alternatively Spliced Tissue Factor Promotes Breast Cancer Growth in a Β1 Integrin-Dependent Manner. Proc. Natl. Acad. Sci. USA. 2013;110:11517–11522. doi: 10.1073/pnas.1307100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tavares V., Neto B.V., Marques I.S., Assis J., Pereira D., Medeiros R. Cancer-Associated Thrombosis: What about MicroRNAs Targeting the Tissue Factor Coagulation Pathway? Biochim. Biophys. Acta (BBA)-Rev. Cancer. 2024;1879:189053. doi: 10.1016/j.bbcan.2023.189053. [DOI] [PubMed] [Google Scholar]
- 18.Morelli V.M., Snir O., Hindberg K.D., Hveem K., Brækkan S.K., Hansen J.-B. High MicroRNA-145 Plasma Levels Are Associated with Decreased Risk of Future Incident Venous Thromboembolism: The HUNT Study. Blood. 2024;143:1773–1781. doi: 10.1182/blood.2023022285. [DOI] [PubMed] [Google Scholar]
- 19.Bogdanov V.Y., Versteeg H.H. “Soluble Tissue Factor” in the 21st Century: Definitions, Biochemistry, and Pathophysiological Role in Thrombus Formation. Semin. Thromb. Hemost. 2015;41:700–707. doi: 10.1055/s-0035-1556049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mackman N., Sachetto A.T.A., Hisada Y. Measurement of Tissue Factor-Positive Extracellular Vesicles in Plasma: Strengths and Weaknesses of Current Methods. Curr. Opin. Hematol. 2022;29:266–274. doi: 10.1097/MOH.0000000000000730. [DOI] [PubMed] [Google Scholar]
- 21.Godal H.C., Rygh M., Laake K. Progressive Inactivation of Purified Factor VII by Heparin and Antithrombin III. Thromb. Res. 1974;5:773–775. doi: 10.1016/0049-3848(74)90120-0. [DOI] [PubMed] [Google Scholar]
- 22.Lawson J.H., Butenas S., Ribarik N., Mann K.G. Complex-Dependent Inhibition of Factor VIIa by Antithrombin III and Heparin. J. Biol. Chem. 1993;268:767–770. doi: 10.1016/S0021-9258(18)53998-3. [DOI] [PubMed] [Google Scholar]
- 23.Rao L.V., Nordfang O., Hoang A.D., Pendurthi U.R. Mechanism of Antithrombin III Inhibition of Factor VIIa/Tissue Factor Activity on Cell Surfaces. Comparison with Tissue Factor Pathway Inhibitor/Factor Xa-Induced Inhibition of Factor VIIa/Tissue Factor Activity. Blood. 1995;85:121–129. doi: 10.1182/blood.V85.1.121.bloodjournal851121. [DOI] [PubMed] [Google Scholar]
- 24.Morrissey J.H. Assay for Measuring Factor VIIa-Antithrombin Complexes. WO 03/004694. 2003 January 16;
- 25.Spiezia L., Rossetto V., Campello E., Gavasso S., Woodhams B., Tormene D., Simioni P. Factor VIIa-Antithrombin Complexes in Patients with Arterial and Venous Thrombosis. Thromb. Haemost. 2010;103:1188–1192. doi: 10.1160/TH09-08-0606. [DOI] [PubMed] [Google Scholar]
- 26.Scharling B., Nielsen G.G., Klitgaard T., Skovsted T.A., Møss J., Segel S., Larsen L.F. Comparison of Coagulant Activity of Factor VII and Activated Factor VII Activity Assays When Used for Determination of Recombinant Activated Factor VII Levels in Plasma. Blood Coagul. Fibrinolysis. 2007;18:677–684. doi: 10.1097/MBC.0b013e3282e7febb. [DOI] [PubMed] [Google Scholar]
- 27.Schut A.M., Meijers J.C.M., Lisman-van Leeuwen Y., van Montfoort M.L., Roest M., de Groot P.G., Urbanus R.T., Coppens M., Lisman T. Decreased Plasma Levels of Activated Factor VII in Patients with Deep Vein Thrombosis. J. Thromb. Haemost. 2015;13:1320–1324. doi: 10.1111/jth.12980. [DOI] [PubMed] [Google Scholar]
- 28.Rossetto V., Spiezia L., Senzolo M., Rodriguez K., Gavasso S., Woodhams B., Simioni P. Factor VIIa-Antithrombin Complexes in Patients with Non-Neoplastic Portal Vein Thrombosis with and without Cirrhosis. Int. J. Lab. Hematol. 2013;35:101–105. doi: 10.1111/ijlh.12003. [DOI] [PubMed] [Google Scholar]
- 29.Abu El-Makarem M.A., El-Akad A.F., Elian M.M., Sherif T.M., El-shaheed R.A., Abd EL Fatah A.S., Sayed D.M., Bakry R.M., Mahmoud A.M. Non-Neoplastic Portal Vein Thrombosis in HCV Cirrhosis Patients: Is It an Immuno-Inflammatory Disorder? Ann Hepatol. 2017;16:574–583. doi: 10.5604/01.3001.0010.0296. [DOI] [PubMed] [Google Scholar]
- 30.Silveira A., Scanavini D., Boquist S., Ericsson C.-G., Hellénius M.-L., Leander K., de Faire U., Ohrvik J., Woodhams B., Morrissey J.H., et al. Relationships of Plasma Factor VIIa-Antithrombin Complexes to Manifest and Future Cardiovascular Disease. Thromb. Res. 2012;130:221–225. doi: 10.1016/j.thromres.2011.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martinelli N., Girelli D., Baroni M., Guarini P., Sandri M., Lunghi B., Tosi F., Branchini A., Sartori F., Woodhams B., et al. Activated Factor VII-Antithrombin Complex Predicts Mortality in Patients with Stable Coronary Artery Disease: A Cohort Study. J. Thromb. Haemost. 2016;14:655–666. doi: 10.1111/jth.13274. [DOI] [PubMed] [Google Scholar]
- 32.Baroni M., Martinelli N., Lunghi B., Marchetti G., Castagna A., Stefanoni F., Pinotti M., Woodhams B., Olivieri O., Bernardi F. Aptamer-Modified FXa Generation Assays to Investigate Hypercoagulability in Plasma from Patients with Ischemic Heart Disease. Thromb. Res. 2020;189:140–146. doi: 10.1016/j.thromres.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 33.Olson N.C., Raffield L.M., Lange L.A., Lange E.M., Longstreth W.T., Chauhan G., Debette S., Seshadri S., Reiner A.P., Tracy R.P. Associations of Activated Coagulation Factor VII and Factor VIIa-Antithrombin Levels with Genome-Wide Polymorphisms and Cardiovascular Disease Risk. J. Thromb. Haemost. 2018;16:19–30. doi: 10.1111/jth.13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paszek E., Pociask E., Ząbczyk M., Butenas S., Undas A. Activated Factor XI Is Associated with Increased Factor VIIa—Antithrombin Complexes in Stable Coronary Artery Disease: Impact on Cardiovascular Outcomes. Eur. J. Clin. Investig. 2022;52:e13857. doi: 10.1111/eci.13857. [DOI] [PubMed] [Google Scholar]
- 35.Davidson S.J., Woodhams B. Factor VIIa-Antithrombin Complexes during Cardiac Surgery Using Cardiopulmonary Bypass. Int. J. Lab. Hematol. 2011;33:614–616. doi: 10.1111/j.1751-553X.2011.01331.x. [DOI] [PubMed] [Google Scholar]
- 36.Spiezia L., Campello E., Gentilomo C., Gavasso S., Woodhams B., Laverda A.M., Simioni P. Factor VIIa-Antithrombin Complexes in Children with Ischemic Stroke. Thromb. Res. 2011;128:303–304. doi: 10.1016/j.thromres.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 37.Słomka A., Świtońska M., Sinkiewicz W., Żekanowska E. Assessing Circulating Factor VIIa-Antithrombin Complexes in Acute Ischemic Stroke: A Pilot Study. Clin. Appl. Thromb. Hemost. 2017;23:351–359. doi: 10.1177/1076029616631424. [DOI] [PubMed] [Google Scholar]
- 38.Negaard H.F.S., Iversen P.O., Østenstad B., Iversen N., Holme P.A., Sandset P.M. Hypercoagulability in Patients with Haematological Neoplasia: No Apparent Initiation by Tissue Factor. Thromb. Haemost. 2008;99:1040–1048. doi: 10.1160/TH07-09-0541. [DOI] [PubMed] [Google Scholar]
- 39.Marchetti M., Tartari C.J., Russo L., Panova-Noeva M., Leuzzi A., Rambaldi A., Finazzi G., Woodhams B., Falanga A. Phospholipid-Dependent Procoagulant Activity Is Highly Expressed by Circulating Microparticles in Patients with Essential Thrombocythemia. Am. J. Hematol. 2014;89:68–73. doi: 10.1002/ajh.23590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spiezia L., Campello E., Bon M., Gavasso S., Woodhams B., Simioni P. Factor VIIa-Antithrombin Complexes Plasma Levels in Cancer Patients with and without Thrombosis. Thromb. Res. 2012;129:818–819. doi: 10.1016/j.thromres.2012.02.046. [DOI] [PubMed] [Google Scholar]
- 41.Martinelli N., Moruzzi S., Udali S., Castagna A., Di Santo L., Ambrosani F., Baroni M., Pattini P., Pizzolo F., Ruzzenente A., et al. Tissue Factor Pathway-Related Biomarkers in Liver Cancer: Activated Factor VII-Antithrombin Complex and Tissue Factor MRNA Levels Are Associated with Mortality. Res. Pract. Thromb. Haemost. 2024;8:102310. doi: 10.1016/j.rpth.2023.102310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Campello E., Zabeo E., Radu C.M., Spiezia L., Gavasso S., Fadin M., Woodhams B., Vettor R., Simioni P. Hypercoagulability in Overweight and Obese Subjects Who Are Asymptomatic for Thrombotic Events. Thromb. Haemost. 2015;113:85–96. doi: 10.1160/TH14-02-0156. [DOI] [PubMed] [Google Scholar]
- 43.Landgrebe L.E., Juhl C.B., Andersen V., Moitinho-Silva L., Bang C., Bladbjerg E.M. Postprandial Factor VII Activation Does Not Increase Plasma Concentrations of Prothrombin Fragment 1 + 2 in Patients with Morbid Obesity. Thromb. Res. 2020;196:260–267. doi: 10.1016/j.thromres.2020.08.044. [DOI] [PubMed] [Google Scholar]
- 44.Martinelli N., Baroni M., Castagna A., Lunghi B., Stefanoni F., Tosi F., Croce J., Udali S., Woodhams B., Girelli D., et al. Apolipoprotein C-III Strongly Correlates with Activated Factor VII-Anti-Thrombin Complex: An Additional Link between Plasma Lipids and Coagulation. Thromb. Haemost. 2019;119:192–202. doi: 10.1055/s-0038-1676817. [DOI] [PubMed] [Google Scholar]
- 45.Johansson H., Lukinius A., Moberg L., Lundgren T., Berne C., Foss A., Felldin M., Källen R., Salmela K., Tibell A., et al. Tissue Factor Produced by the Endocrine Cells of the Islets of Langerhans Is Associated with a Negative Outcome of Clinical Islet Transplantation. Diabetes. 2005;54:1755–1762. doi: 10.2337/diabetes.54.6.1755. [DOI] [PubMed] [Google Scholar]
- 46.Sachetto A.T.A., Mackman N. Monocyte Tissue Factor Expression: Lipopolysaccharide Induction and Roles in Pathological Activation of Coagulation. Thromb. Haemost. 2023;123:1017–1033. doi: 10.1055/a-2091-7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lehner G.F., Tobiasch A.K., Perschinka F., Mayerhöfer T., Waditzer M., Haller V., Zassler B., Maier S., Ulmer H., Joannidis M. Associations of Tissue Factor and Tissue Factor Pathway Inhibitor with Organ Dysfunctions in Septic Shock. Sci. Rep. 2024;14:14468. doi: 10.1038/s41598-024-65262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Francischetti I.M.B., Toomer K., Zhang Y., Jani J., Siddiqui Z., Brotman D.J., Hooper J.E., Kickler T.S. Upregulation of Pulmonary Tissue Factor, Loss of Thrombomodulin and Immunothrombosis in SARS-CoV-2 Infection. EClinicalMedicine. 2021;39:101069. doi: 10.1016/j.eclinm.2021.101069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martinelli N., Rigoni A.M., De Marchi S., Osti N., Donini M., Montagnana M., Castagna A., Pattini P., Udali S., De Franceschi L., et al. High Plasma Levels of Activated Factor VII-Antithrombin Complex Point to Increased Tissue Factor Expression in Patients with SARS-CoV-2 Pneumonia: A Potential Link with COVID-19 Prothrombotic Diathesis. Diagnostics. 2022;12:2792. doi: 10.3390/diagnostics12112792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Willems L.H., Nagy M., Ten Cate H., Spronk H.M.H., Groh L.A., Leentjens J., Janssen N.A.F., Netea M.G., Thijssen D.H.J., Hannink G., et al. Sustained Inflammation, Coagulation Activation and Elevated Endothelin-1 Levels without Macrovascular Dysfunction at 3 Months after COVID-19. Thromb. Res. 2022;209:106–114. doi: 10.1016/j.thromres.2021.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Willems L.H., Nagy M., Ten Cate H., Spronk H.M.H., Jacobs L.M.C., Kranendonk J., van Leeuwen M., Meijer D., Middeldorp S., Groh L.A., et al. ChAdOx1 Vaccination, Blood Coagulation, and Inflammation: No Effect on Coagulation but Increased Interleukin-6. Res. Pr. Thromb. Haemost. 2021;5:e12630. doi: 10.1002/rth2.12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Spiezia L., Visentin S., Radu C., Bon M., Woodhams B., Cosmi E., Simioni P. Association between Increased FVIIa-Antithrombin Complex/FVIIa Ratio and Pre-Eclampsia. J. Matern. Fetal Neonatal Med. 2013;26:1352–1354. doi: 10.3109/14767058.2013.784265. [DOI] [PubMed] [Google Scholar]
- 53.Alpoim P.N., Godoi L.C., Pinheiro M.D.B., Freitas L.G., Carvalho M.d.G., Dusse L.M. The Unexpected Beneficial Role of Smoking in Preeclampsia. Clin. Chim. Acta. 2016;459:105–108. doi: 10.1016/j.cca.2016.05.030. [DOI] [PubMed] [Google Scholar]
- 54.Dusse L.M.S., Godoi L.C., Alpoim P.N., Gomes K.B., Sousa L.P., Perucci L.O., Lwaleed B., Carvalho M.G. FVIIa-Antithrombin Levels in Early and Late Preeclampsia. Clin. Chim. Acta. 2017;474:67–69. doi: 10.1016/j.cca.2017.08.040. [DOI] [PubMed] [Google Scholar]
- 55.Agersø H., Brophy D.F., Pelzer H., Martin E.J., Carr M., Hedner U., Ezban M. Recombinant Human Factor VIIa (RFVIIa) Cleared Principally by Antithrombin Following Intravenous Administration in Hemophilia Patients. J. Thromb. Haemost. 2011;9:333–338. doi: 10.1111/j.1538-7836.2010.04152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Busch M.H., Ysermans R., Aendekerk J.P., Timmermans S.A.M.E.G., Potjewijd J., Damoiseaux J.G.M.C., Spronk H.M.H., Ten Cate H., Reutelingsperger C.P., Nagy M., et al. The Intrinsic Coagulation Pathway Plays a Dominant Role in Driving Hypercoagulability in ANCA-Associated Vasculitis. Blood Adv. 2024;8:1295–1304. doi: 10.1182/bloodadvances.2023011937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harrington L.B., Ehlert A.N., Thacker E.L., Jenny N.S., Lopez O., Cushman M., Olson N.C., Fitzpatrick A., Mukamal K.J., Jensen M.K. Levels of Procoagulant Factors and Peak Thrombin Generation in Relation to Dementia Risk in Older Adults: The Cardiovascular Health Study. Thromb. Res. 2024;235:148–154. doi: 10.1016/j.thromres.2024.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huang M.-J., Wei R., Wang Y., Su T., Di P., Li Q., Yang X., Li P., Chen X. Blood Coagulation System in Patients with Chronic Kidney Disease: A Prospective Observational Study. BMJ Open. 2017;7:e014294. doi: 10.1136/bmjopen-2016-014294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fazavana J.G., Muczynski V., Proulle V., Wohner N., Christophe O.D., Lenting P.J., Denis C.V. LDL Receptor-related Protein 1 Contributes to the Clearance of the Activated Factor VII–Antithrombin Complex. J. Thromb. Haemost. 2016;14:2458–2470. doi: 10.1111/jth.13502. [DOI] [PubMed] [Google Scholar]
- 60.Brambilla M., Becchetti A., Rovati G.E., Cosentino N., Conti M., Canzano P., Giesen P.L.A., Loffreda A., Bonomi A., Cattaneo M., et al. Cell Surface Platelet Tissue Factor Expression: Regulation by P2Y 12 and Link to Residual Platelet Reactivity. Arterioscler. Thromb. Vasc. Biol. 2023;43:2042–2057. doi: 10.1161/ATVBAHA.123.319099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mani H., Kirchmayr K., Kläffling C., Schindewolf M., Luxembourg B., Linnemann B., Lindhoff-Last E. Influence of Blood Collection Techniques on Platelet Function. Platelets. 2004;15:315–318. doi: 10.1080/09537100410001711505. [DOI] [PubMed] [Google Scholar]
- 62.Eikelboom J.W., Connolly S.J., Bosch J., Dagenais G.R., Hart R.G., Shestakovska O., Diaz R., Alings M., Lonn E.M., Anand S.S., et al. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. N. Engl. J. Med. 2017;377:1319–1330. doi: 10.1056/NEJMoa1709118. [DOI] [PubMed] [Google Scholar]
- 63.Versteeg H.H., Schaffner F., Kerver M., Petersen H.H., Ahamed J., Felding-Habermann B., Takada Y., Mueller B.M., Ruf W. Inhibition of Tissue Factor Signaling Suppresses Tumor Growth. Blood. 2008;111:190–199. doi: 10.1182/blood-2007-07-101048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Graf C., Wilgenbus P., Pagel S., Pott J., Marini F., Reyda S., Kitano M., Macher-Göppinger S., Weiler H., Ruf W. Myeloid Cell–Synthesized Coagulation Factor X Dampens Antitumor Immunity. Sci. Immunol. 2019;4:eaaw8405. doi: 10.1126/sciimmunol.aaw8405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Haist M., Stege H., Pemler S., Heinz J., Fleischer M.I., Graf C., Ruf W., Loquai C., Grabbe S. Anticoagulation with Factor Xa Inhibitors Is Associated with Improved Overall Response and Progression-Free Survival in Patients with Metastatic Malignant Melanoma Receiving Immune Checkpoint Inhibitors—A Retrospective, Real-World Cohort Study. Cancers. 2021;13:5103. doi: 10.3390/cancers13205103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Coleman R.L., Lorusso D., Gennigens C., González-Martín A., Randall L., Cibula D., Lund B., Woelber L., Pignata S., Forget F., et al. Efficacy and Safety of Tisotumab Vedotin in Previously Treated Recurrent or Metastatic Cervical Cancer (InnovaTV 204/GOG-3023/ENGOT-Cx6): A Multicentre, Open-Label, Single-Arm, Phase 2 Study. Lancet Oncol. 2021;22:609–619. doi: 10.1016/S1470-2045(21)00056-5. [DOI] [PubMed] [Google Scholar]
- 67.Heitz N., Greer S.C., Halford Z. A Review of Tisotumab Vedotin-Tftv in Recurrent or Metastatic Cervical Cancer. Ann. Pharmacother. 2023;57:585–596. doi: 10.1177/10600280221118370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.