Abstract
Adenomyosis, endometriosis of the uterus, is associated with an increased likelihood of abnormal endometrial molecular expressions thought to impair implantation and early embryo development, resulting in disrupted fertility, including the local effects of sex steroid and pituitary hormones, immune responses, inflammatory factors, and neuroangiogenic mediators. In the recent literature, all of the proposed pathogenetic mechanisms of adenomyosis reduce endometrial receptivity and alter the adhesion molecule expression necessary for embryo implantation. The evidence so far has shown that adenomyosis causes lower pregnancy and live birth rates, higher miscarriage rates, as well as adverse obstetric and neonatal outcomes. Both pharmaceutical and surgical treatments for adenomyosis seem to have a positive impact on reproductive outcomes, leading to improved pregnancy and live birth rates. In addition, adenomyosis has negative impacts on reproductive outcomes in patients undergoing assisted reproductive technology. This association appears less significant after patients follow a long gonadotropin-releasing hormone agonist (GnRHa) protocol, which improves implantation rates. The pre-treatment of GnRHa can also be beneficial before engaging in natural conception attempts. This review aims to discover adenomyosis-associated infertility and to provide patient-specific treatment options.
Keywords: adenomyosis, infertility, endometrial receptivity, embryo implantation, pregnancy, assisted reproductive technology
1. Introduction
Adenomyosis is an estrogen-dependent uterine disorder characterized by ectopic endometrial-like tissue (stroma, glands, and fibroblasts) pathologically demonstrated in the myometrium, causing hyperplasia and hypertrophy in the surrounding smooth muscle cells and local inflammatory responses [1]. Women affected by adenomyosis may present with an enlarged uterus, heavy menstrual bleeding, dysmenorrhea, dyspareunia, chronic pelvic pain, and infertility, but one-third of them are asymptomatic [2].
Historically, adenomyosis was diagnosed by a histopathological finding after hysterectomy [3]. The epidemiological scenario has changed; introducing new medical compounds and surgical techniques has allowed clinicians to treat the disease conservatively. A 20.9% prevalence of adenomyosis in the general population was shown from ultrasound units [4], whereas the data range from 10% to 35% in histological reports after hysterectomy [5]. Noninvasive methods, such as ultrasounds and magnetic resonance imaging (MRI), now allow for the clinical diagnosis of adenomyosis in infertile women [6,7], leading to a better understanding of the epidemiology, natural history, and consequences on fertility and obstetric outcomes. Four subtypes of adenomyosis assessed by MRI were classified as follows: subtypes I-III were suggested as causes of direct endometrial invasion, ectopic endometriotic invasion from the outside, and de novo metaplasia, respectively, whereas subtype IV was a heterogeneous mixture of far advanced disease [8]. Although the most common risk factor profile [9] included an age of more than 40 years, multiparity, prior cesarean delivery, or uterine surgery [9,10], over the past decade, adenomyosis has been increasingly identified in young fertile-aged women [11], in infertility patients [12], and those with pain, abnormal uterine bleeding, or both [13]. Because of recent advancements in imaging techniques [14], improved diagnostic tools have raised awareness of the condition in adenomyosis-associated infertility. Additionally, adenomyosis usually coexists with other gynecological disorders, such as uterine fibroids and endometriosis. Adenomyosis and endometriosis share several features; for a long time, adenomyosis has been called endometriosis interna [15], which the International Statistical Classification of Diseases and Related Health Problems (ICD) coded as “endometriosis of uterus” https://www.icd10data.com/ICD10CM/Codes/N00-N99/N80-N98/N80-/N80.0 (accessed on 1 October 2023). Although they often coexist in the same patients, they are considered two distinct entities due to different pathogenic pathways and clinical characteristics [16,17].
Among women receiving assisted reproductive technology (ART), the prevalence of endometriosis is widely variable, ranging from 20% to 80% [16,17], whereas in those with a history of adenomyosis, it is 20% to 25% [12]. Endometriosis influences up to 40% of infertile women and is associated with poorer ART outcomes, including a decreased yield of mature oocytes [18], lower implantation rates [19,20], and reduced pregnancy rates [19,20]. Adenomyotic foci impair the molecular factors of embryo attachment and endometrial decidualization, resulting in altered expressions of endometrial receptivity genes, growth factors, cytokines, and myometrial contractility in a fashion that disrupts implantation [21,22]. Recently, the development of imaging resolution has led to an increased number of women being diagnosed with adenomyosis, strengthening the interest in more conservative treatment options [23]. Regarding the scarcity of high-quality studies in fertility-preserving management, a shared guideline of ART strategies will be important in the future as the disease requires a lifelong plan for symptom control and reproductive outcomes. This review aims to discover adenomyosis-associated infertility and to provide clarified guidance for managing infertile women with adenomyosis.
2. Pathophysiologic Aspects of Adenomyosis-Associated Infertility
Adenomyosis is the presence of ectopic endometrial glands and stroma surrounded by hypertrophic and hyperplastic myometrium, subsequently establishing dysfunction in embryo transport and implantation [21,22]. The pathogenesis of adenomyosis remains unclear; in the past decade, several hypotheses have been proposed [24], and an increasing number of studies have demonstrated that sex steroid hormone receptors, inflammatory molecules, extracellular matrix enzymes, growth factors, and neuroangiogenic factors act as pathogenic mediators of adenomyosis [21].
2.1. Myometrium Structure and Physiology in Fecundity
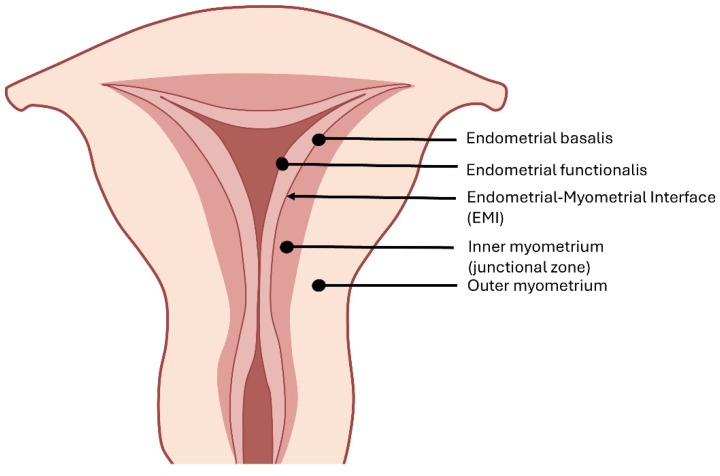
Histologically, the myometrium comprises an outer longitudinal layer and an inner circular layer of smooth muscle cells between the endometrium and uterine serosa [25]. Differing from other mucosal tissues (e.g., intestine), the endometrial–myometrial interface (EMI) is a mucosal–muscular interface without an intervening basement membrane, where the endometrial basalis directly contacts the myometrium [26,27] (Figure 1). MRI provides definitions of high-signal intensity endometrium, medium-signal intensity outer myometrium, and low-signal intensity inner myometrium (also called the “junctional zone”) on T2-weighted images [28]. With a poor histological correlation, the junctional zone is identified in MRI studies of the uterus as the subendometrial halo or in ultrasonography as the hypoechoic tissue identified beyond the endometrial basal layer [28,29]. Additionally, their embryologic origins and physiological roles differ markedly. During embryogenic development, the junctional zone arises from the Mullerian ducts, as does the endometrium, whereas the outer myometrium is mesenchymal in origin. The inner myometrium, endowed with estrogen and progesterone receptors, displays cycle-dependent directional contractions throughout menstruation [30,31]. In the follicular phase, retrograde contractions (uterine cervix to fundus) of the inner myometrium facilitate sperm transport. The contractile frequency and amplitude decrease markedly in the mid-luteal phase to promote embryo implantation. During menses, antegrade-propagated (uterine fundus to cervix) contractions with increased peristalsis amplitude assist the desquamation of the shed endometrium [30,32]. In contrast, the outer myometrium protects the fetus throughout pregnancy and mechanically facilitates the expulsion of the fetus at parturition under the regulation of oxytocin and steroid hormones [33,34].
Figure 1.
The structure of the uterus. The endometrial–myometrial interface (EMI) is a mucosal–muscular interface where the endometrial basalis directly contacts the myometrium.
2.2. Theories and Potential Mechanisms of Adenomyosis
2.2.1. Invagination Theory
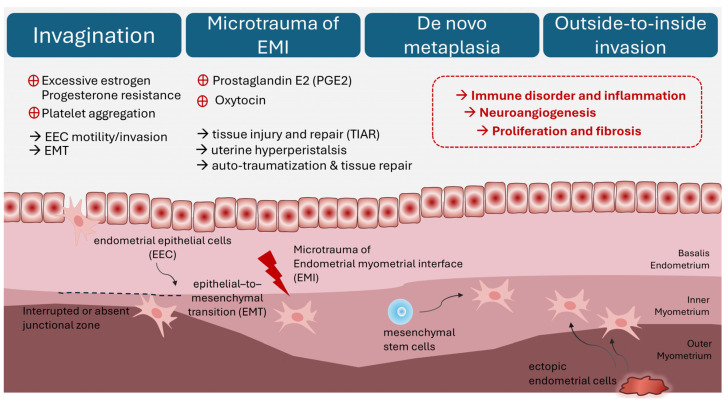
As one of the most accepted theories, adenomyotic lesions grow from an enhanced invasion of the endometrium into the myometrium through an interrupted or absent junctional zone [35] (Figure 2). Studies have postulated the dysregulation of extracellular matrix function in the eutopic endometria of women with adenomyosis compared with healthy controls, facilitating endometrial cell proliferation, epithelial-to-mesenchymal transition (EMT), resistance to apoptosis, migration and invasion into the myometrium, and the establishment of adenomyosis [36,37]. Excessive estradiol in the eutopic endometria of women with adenomyosis drives molecular mechanisms of proliferation and apoptosis dysfunctionalities in adenomyotic lesions [37,38,39]. EMT, a process wherein epithelial cells acquire an invasive and metastatic phenotype, is characterized by the loss of E-cadherin and enhanced mesenchymal marker expression, which occur concomitantly with the up-regulation of N-cadherin and vimentin in the eutopic and ectopic endometrium of patients with adenomyosis compared with healthy controls [40], contributing to endometrial cell migration into the myometrium. Platelet aggregation [39] and high estrogen levels [40] have been considered possible causes of endometrial EMT in the development of adenomyosis. Moreover, the dysregulation of extracellular cell matrix function, which is mediated by the downregulated Lysyl oxidase gene [41] or the up-regulated matrix metalloproteinases [42,43], presented in the eutopic endometrium in women with adenomyosis, supporting the invagination theory.
Figure 2.
Theories and potential mechanisms of adenomyosis. (1) Invasion of endometrial basalis into myometrium. (2) Microtrauma of endometrial–myometrial interface. (3) De novo metaplasia from stem cells. (4) Outside-to-inside invasion induced by ectopic endometrial cells.
2.2.2. Microtrauma of Endometrial–Myometrial Interface
The theory of tissue injury and repair (TIAR) as the primary mechanism in the initiation process of adenomyosis [44] stresses the importance of tissue damage in the endometrial–myometrial interface (EMI). In support of this hypothesis are the clinical observations that adenomyosis is associated with multiparity, repeated endometrial curettage, previous cesarean section, and prior uterine surgery wherein the endometrial–myometrial interface is breached [24,45]. However, nulliparous women without a history of uterine surgeries also develop adenomyosis. The proposal is that physiologic trauma (“microtrauma”) to the EMI results from the course of proliferation and inflammation at the EMI by chronic uterine auto-traumatization (tissue injury) and, subsequently, tissue repair [14]. Continuous cyclic uterine peristaltic activity induces repeated cycles of auto-traumatization, damaging the EMI and migrating basal endometrium fragments into the myometrium throughout a woman’s reproductive lifetime [46]. Increased estrogen levels in the eutopic endometrium promote microtrauma to the EMI following TIAR and the peristaltic activity of the subendometrial myometrium [47]. Studies have demonstrated that microtrauma activates the TIAR process and produces prostaglandin E2 (PGE2) through interleukin-1 (IL-1)-induced cyclo-oxygenase-2 (COX-2) expression, facilitating local estrogen production through STAR and aromatase P450 [22]. While increased estrogen promotes healing through estrogen receptor β, it also supports oxytocin-mediated hyperperistalsis through estrogen receptor α, which inhibits the healing course and augments further microtrauma to EMI, eventually leading to the establishment of adenomyotic lesions [14,47].
2.2.3. De Novo Metaplasia Theory
The alternative hypothesis of adenomyosis proposes a de novo process of embryonic or adult endometrial stem cell metaplasia into the myometrium [48]. During Müllerian duct development and fusion, some embryonic pluripotent Müllerian remnants may be misplaced in the myometrium, subsequently resulting in metaplastic changes in the adult myometrium and the development of de novo adenomyotic foci [49]. Furthermore, endometrial epithelial progenitor and mesenchymal stem cells have been reported in the endometrial basalis, playing a critical role in the cyclic repair of the endometrium [50]. These adult stem cells can be activated after tissue injury at the EMI, promoting uncontrolled growth into the myometrium and differentiating into adenomyotic lesions [21].
2.2.4. Outside-to-Inside Invasion
Apart from invasion directly into the myometrium, adult endometrial and stromal stem cells may be deposited into the myometrium through retrograde menstruation [24]. Chapron et al. proposed the “outside-to-inside invasion” theory that endometrial cells in retrograde menstrual blood potentially infiltrate pelvic organs and the uterine serosa [15]. The posterior focal adenomyosis of the outer myometrium in patients with deep infiltrating endometriosis nodules in the posterior compartment supports this hypothesis. Similarly, through outside-to-inside trans-serosa invasion, the high concurrence of anterior focal adenomyosis of the outer myometrium and deep infiltrating endometriosis nodules in the vesicouterine pouch have been reported [51].
Nevertheless, existing theories may not fully explain the heterogeneous phenotypes of adenomyosis. Most importantly, elucidating the adenomyosis pathogenesis may help us better understand clinical symptoms and the association of imaging presentations.
2.3. Pathogenesis of Adenomyosis
2.3.1. Genetic and Epigenetic Alteration
Thousands of abnormally up- or downregulated genes have been reported in the eutopic endometria of women with adenomyosis compared to controls [41]. Studies have found that the variants of the Cytochrome P450 (CYP) gene and catechol-O-methyltransferase (COMT) gene affect enzyme activity and promote estrogen-dependent diseases, including adenomyosis [52,53]. Current evidence has demonstrated the role of genetic polymorphisms involved in the adenomyosis pathogenesis through alterations in the metabolism and functions of steroid hormones and their receptors [54,55], extracellular matrix dysregulation [56], angiogenesis [57], and inflammatory mediators [58]. A recent next-generation sequencing study detected KRAS and PIK3CA mutations in adenomyotic lesions and the adjacent eutopic endometrium, suggesting that these mutations most likely arose in the eutopic endometrial epithelial cells before they invaded the myometrium, promoting invasive and survival capacities that facilitate their invasion and growth within the myometrial tissue, thereby establishing adenomyosis [59].
Epigenetic abnormalities can be equally applied to adenomyosis, including DNA methylation, histone modification, and microRNA expression, which give rise to aberrant mRNA and the protein expression of genes [21]. The aberrant expression of deoxyribonucleic acid methyltransferases (DNMTs), a family of enzymes that catalyze the transfer of a methyl group to DNA, was detected in patients with adenomyosis compared with controls [60]. The hypomethylation of DNA and increased expression of the CCAAT/enhancer-binding protein β, a transcription factor regulating cellular proliferation and differentiation, have been demonstrated in adenomyosis [61]. The promoter hypermethylation of progesterone receptor β can lead to progesterone resistance in adenomyotic tissue [62]. The increased expression of class I histone deacetylases (HDACs) was also associated with the development of adenomyosis [63]. Methyltransferase-like 3 (METTL3), a writer promoting the methylation of RNA, and the total N6-methyladenosine (m6A) levels were decreased in the eutopic endometria of patients with adenomyosis compared with controls, suggesting that m6A RNA methylation regulators may be involved in the pathogenesis of adenomyosis [64].
2.3.2. Hyperestrogenism and Progesterone Resistance
As an estrogen-dependent uterine disorder, adenomyosis is associated with local steroid hormone aberration. Aromatase enzyme activity and protein expression are up-regulated in adenomyotic tissue [65]. The epigenetic-regulated NR5A1 (a nuclear receptor) binding to the proximal promoter of the aromatase (CYP19A1) gene seems to be the critical mechanism for its suppression in normal endometrial stromal cells and its expression in endometriotic stromal cells [66]. Moreover, a lower expression of 17-β hydroxysteroid dehydrogenase type 2 (HSD17-β2), which converts estradiol (E2) to the less potent estrone (E1), was detected in the eutopic and ectopic endometria of patients with adenomyosis compared with controls [67]. Lastly, increased biosynthesis and decreased conversion of E2 contribute to a local hyperestrogenic milieu in adenomyosis, promoting the excessive production of prostaglandins driven by estrogen receptor β that causes an inflammatory process [52].
The expression of uterine estrogen and progesterone receptors in patients with adenomyosis differs from that in healthy controls [68]. Estrogen receptor β (ERβ) is overexpressed in adenomyotic tissue during the proliferative phase and throughout the myometrium across the menstrual cycle. In contrast, compared with controls, estrogen receptor α (ERα) is downregulated in the eutopic endometria of patients with adenomyosis during the secretory phase. Additionally, lower progesterone receptor (PRα and PRβ) expression is discovered in adenomyotic tissue as a clue of progesterone resistance [69,70].
2.3.3. Immune Disorder and Inflammatory Mediators
Specific human leukocyte antigen (HLA) classes and increased numbers of macrophages and other immune cells in the endometria of women with adenomyosis have been proposed to activate the autoimmune system, causing a dysregulated immune response [71,72]. Altered COX-2 and PGE2 synthesis, correlating with an increased expression of corticotropin-releasing hormone (CRH), facilitates the inflammatory pathway [73]. The increased expression of inflammatory mediators, including IL-1β, the IL-18/IL-18R complex, and tumor necrosis factor-α,β (TNF-α,β), in the endometria of women with adenomyosis further implicate the activation of the nuclear factor kappa light-chain enhancer of activated B cell (NF-κB) pathways in developing adenomyotic lesions [74,75].
2.3.4. Neuroangiogenesis and Fibrosis
Particularly in symptomatic women, higher expressions of neurogenic factors, including nerve growth factors (NGFs), synaptophysin (SYN), and microtubule-associated protein 2 (MAP2), have been reported in adenomyotic lesions compared with controls [76]. Inflammatory mediators, known as PGE2 and prostacyclin, may stimulate sensory unmyelinated C nerve fibers in the functional layer of the endometrium, causing neurogenic inflammation in adenomyotic lesions. The glycoprotein neural cell adhesion molecule, such as CD56, and other neurotrophic factors found in the endometrium and adenomyotic lesions further stimulate nerve growth, increasing the sensitivity of nociceptors in the myometrium, thus triggering pelvic pain [77,78].
The overexpression of angiogenic factors, such as VEGF, annexinA2 (ANXA2), follistatin, and activin A, members of the TGF-β family, has been detected in the ectopic and eutopic endometria of patients with adenomyosis, promoting vascular sprouting and augmenting vascular permeability in angiogenesis [79,80,81]. Due to repeated cycles of TIAR, TGF-β signaling drives EMT and collagen production, ultimately leading to a certain degree of fibrosis in adenomyosis [39].
2.3.5. Pituitary Hormones and Endocrine-Disrupting Chemicals
Prolactin (PRL) expression has increased in women with adenomyosis compared to those without adenomyosis [82]. In animal studies, hyperprolactinemia-triggered adenomyosis was demonstrated in a mouse model [83,84], and the overexpression of PRL receptor mRNA was detected in the uteri of mice with versus those without adenomyosis [84]. PRL directly influences the myometrium and induces adenomyosis by the degeneration of smooth muscle cells [85]; however, the mechanisms still await further delineation.
The oxytocin receptor (OTR) is expressed in the normal endometrium and myometrium and is regulated by the cyclic steroid hormone [86]. The overexpression of OTR in adenomyosis-affected uteri may induce hyperperistalsis and microtrauma in the EMI, thus positively correlating with the severity of the disease. Moreover, there is a significantly higher expression of myometrial OTR in the fundal region of adenomyosis-affected uteri than in the isthmic region, causing disorientation of the EMI contractions and subsequently interfering with sperm transport and fertility [87].
Endocrine-disrupting chemicals (EDCs), such as estrogen-mimetic bisphenol A and diethylstilbestrol, have been reported as the effects of gene–environment interaction during embryogenesis and neonatal development in animal studies [88,89], giving rise to adenomyosis development. Furthermore, phthalates, a kind of EDC that have antiandrogenic effects, are reported to increase the risk of adenomyosis [90].
2.3.6. Microbiota Composition
An alteration in the microbiota composition has been postulated in the pathogenesis of adenomyosis by affecting the host’s epigenetic, immunologic, metabolic, and biochemical functions. Distinct bacterial taxa were identified in the endometrial, vaginal, and gut microbiota of patients with adenomyosis compared with the controls, suggesting a potential link between the microbiota profile and adenomyosis [91].
3. Pathologic Mechanisms in Adenomyosis-Associated Infertility
Adenomyosis has been regarded as a typical uterine disorder in multiparous women; however, increasing evidence declares an association with infertility and reproductive failure [92]. Recently, a cross-sectional study showed that the prevalence of adenomyosis was 24.4% in infertile women over 40 years old and 22% in those under 40 years old. The percentage increased to 38.2% in women with recurrent miscarriages and 34.7% with previous artificial reproductive treatment failure [12]. The effects of adenomyosis on eutopic endometrial function, uterine environment, and contractility alter the capacity to receive the embryo and accept proper development, causing infertility and poor implantation outcomes [12,93] (Figure 3). However, it is not easy to precisely understand the specific role of adenomyosis due to the frequent coexistence of endometriosis and adenomyosis [94].
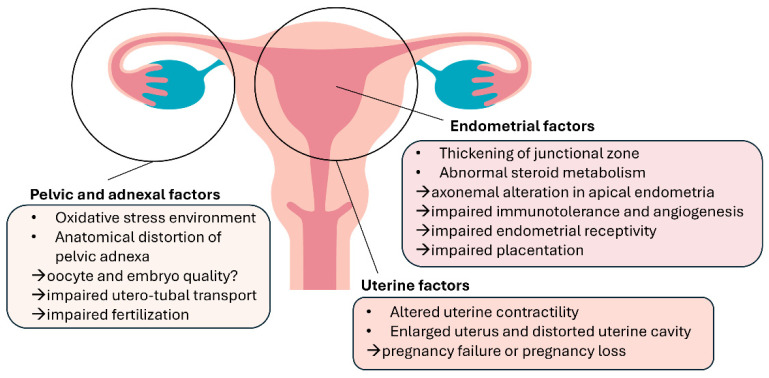
Figure 3.
Pathologic mechanisms in adenomyosis-associated infertility.
3.1. Oocyte Quality and Embryo Euploidy
An impaired follicular environment has been advocated in endometriosis, which makes oogenesis more susceptible to meiotic errors and chromosomal instability [19]. Toxic pelvic factors directly and persistently affect the quality of the gametes in the local environment and temporarily affect the embryos while passing through the fallopian tube. Some studies demonstrated that an alteration in the meiotic spindle could increase the embryo aneuploidy rate and thus cause higher miscarriage rates and pregnancy losses in patients with endometriosis [95,96]. In ART, in bypassed tubal and pelvic environments, Juneau et al. [97] reported equal euploidy rates in women with endometriosis and age-matched controls. Regardless of the high correlation with endometriosis, the negative impact on oocytes in women with adenomyosis remains elusive.
3.2. Utero-Tubal Transport
As described earlier, the opposite pattern of OTR expression in fundal and isthmic regions could disturb the direction of EMI contractions, interfering with gametes or embryo transport and subsequent implantation into the endometrium [87]. Additionally, adenomyosis seems to destroy the normal architecture of the myometrium, resulting in the anatomical distortion of the uterine cavity and disturbing uterine peristalsis [98].
3.3. Endometrial Receptivity
The implantation process requires coordinated and synchronous embryo development and a decidualized endometrium receptive to implantation [99]. Aberrant endometrial shifts during the window of implantation (WOI), including impaired decidual transformation, increased inflammatory mediators, the dysregulation of immune factors, and oxidative stress, ultimately contributed to defective endometrial receptivity. Dysregulated implantation-associated factors, such as HOXA10 [100,101], the leukemia inhibitory factor [102], NR4A and FOXO1A [103], and MMP2 [42], leading to a shift in gene expression during the WOI, have been reported to promote progesterone resistance and impair decidualization. The decreased expression of cell adhesion receptors, including glycodelin, the integrin family, Mucin-1, and osteopontin, further reduces embryo-to-endometrial interaction in implantation [104,105].
Steroid metabolism and biosynthesis in the endometrium also alter endometrial receptivity. The overexpression of aromatase, coupled with the downregulation of the E2 metabolizing enzyme HSD17-β2, enhances bioavailable E2 in the endometrium, accounting for aberrantly high estrogen receptor levels and proliferation, interfering embryo attachment and invasion [65]. E2-regulated COX-2 and hypoxia-induced factor-1 are involved in inflammation associated with implantation failure [106].
Recently, Khan et al. [107] demonstrated microvilli malformation and axonemal arrangement disruption in the apical endometria derived from women with focal and diffuse adenomyosis. These ultra-structural endometrial abnormalities in response to tissue inflammation with abundant macrophage infiltration may negatively affect fertility outcomes in women with symptomatic adenomyosis.
In addition, women with adenomyosis have a higher concurrent rate of chronic endometritis [108]. A variable presence of chronic endometritis in women with adenomyosis could be an additional factor that worsens the endometrial receptivity by distorting the functional and structural integrity of the endometrium [109].
3.4. Immunotolerance and Angiogenesis
During the WOI, natural killer (NK) cells and macrophages are the dominant immune cells that regulate trophoblast invasion macrophages [110]. In addition, the vascular endothelial growth factor and placental growth factor are also important in promoting angiogenesis [111] in early pregnancy. In endometriosis, activated macrophages can secrete pro-inflammatory cytokines, such as IL-1β, IL-6, IL-8, interferon-γ (IFN-γ), and TNF-α in the peritoneal cavity [112] and pro-inflammatory cytokines that trigger venous thromboembolism during pregnancy [113]. Several mechanisms appear to be implicated in the association between adenomyosis and obstetric complications, including activated local and systemic inflammation, increased prostaglandin production in myometrium, aberrant uterine contractility, and defective spiral artery remodeling at the basis of placentation, resulting in several detrimental obstetric consequences, including early pregnancy losses and possibly repeated pregnancy loss (RPL) [114,115].
3.5. Uterine Peristaltic Wave
Studies have shown that higher uterine contraction frequencies in natural [116] and stimulated cycles [117] are associated with reduced conception, implantation, and live birth rates. In adenomyosis, ultrastructural myometrial abnormalities distort the uterine cavity and cause a disturbance in the normal rhythmic muscle contractility [118]. In addition, subendometrial myometrium (inner myometrium or junctional zone) presents with dysfunctional hyperperistalsis and increased intrauterine pressure in women with adenomyosis, amplified by local hyperestrogenism, leading to defective implantation and placentation and, in turn, miscarriages and RPL [119].
4. Assisted Reproductive Technology for Adenomyosis-Associated Infertility
The management of adenomyosis-associated infertility has been conflicting. The current medical treatments for symptomatic adenomyosis, including nonsteroidal anti-inflammatory drugs (NSAIDs), progestins, oral contraceptives, a levonorgestrel-releasing intrauterine system (LNG-IUS), as well as both gonadotropin-releasing hormone (GnRH) agonists and antagonists, are based on anti-proliferative and anti-inflammatory effects by controlling the hormonal medium. Regardless of the modality, the treatment of adenomyosis can temporarily improve symptoms and quality of life, consistently improving conception chances [120,121,122]. The adverse effects of adenomyosis on ART outcomes have also been reported [92,123,124]. However, there are limited data evaluating the impact of ART with medical or surgical intervention on women with adenomyosis-associated infertility.
4.1. Ovarian Stimulation Protocol
According to the pathogenic mechanisms of adenomyosis, several ovarian stimulation protocols have been attempted to improve reproductive outcomes. The use of long-acting or continuous gonadotropin-releasing hormone agonist (GnRHa) administration in an ovarian stimulation protocol, which suppresses premature LH surge and avoids spontaneous ovulation, was more extensive, possibly because of a hypoestrogenic state and an anti-proliferative effect in adenomyotic tissue [125].
Regarding the duration of GnRHa downregulation, the GnRHa protocol was classified as an ultra-long (a monthly long-acting GnRHa injection with a duration varying from one to six cycles), long (a daily dose of GnRHa starting from the previous luteal phase until hCG is triggered), or short (a daily dose of GnRHa given on days 2–4 of the menstrual cycle until hCG is triggered) protocol. In a previous systematic review of 10 studies [126], a pooled analysis showed that a long protocol had better reproductive outcomes than a short protocol regarding the pregnancy, live birth, and miscarriage rates. Several studies have demonstrated positive results with an increased clinical pregnancy rate (CPR) [127] and implantation rate (IR) [127] and a decreased miscarriage rate (MR) [128] in the ultra-long protocol when compared with the long protocol. However, the ultra-long protocol causes the profound inhibition of ovarian function by the downregulation of its receptors, thus reducing the sensitivity of pituitary glands, usually causing an increase in the duration and dosage of gonadotropin, resulting in poor ovarian response and decreased oocyte retrieval [127].
Ge et al. systematically evaluated the reproductive outcomes of different ovarian stimulation protocols in fresh embryo transfer (ET) cycles [129]. The intragroup comparison showed no statistical differences in the number of retrieved oocytes and maturation rate. The results elucidate that an ultra-long or long protocol might benefit women with adenomyosis receiving ART with fresh ET compared to a short protocol. In fresh ET in women aged ≥35, the CPR was higher in the ultra-long and long protocols than in the antagonist and short protocols (52.1%, 50.0% vs. 20.0%, 27.5%; p = 0.031) [129]. Nevertheless, embryos derived from protocols, such as long, short, and antagonist protocols, had no impact on pregnancy outcomes in frozen embryo transfer (FET) cycles (Table 1).
Table 1.
Ovarian stimulation protocol and embryo transfer strategy for adenomyosis.
| Ovarian Stimulation Protocol | ||
|---|---|---|
| Study | Intervention | Results |
| Rocha et al. (2018) [126] |
Pooled long protocols (N = 482) |
|
| Hou et al. (2020) [127] |
Patients in long protocol (N = 127) Patients in ultra-long protocol (N = 362) |
|
| Lan et al. (2021) [128] |
Long GnRHa protocol (N = 116) |
|
| Wu et al. (2022) [130] |
Group B: fresh ET with ultra-long protocol (N = 241) Group C: fresh ET with long protocol (N = 104) |
|
| Ge et al. (2023) [129] |
Total of 305 FET cycles with embryos from ultra-long (N = 98), long (N = 101), short (N = 52), and antagonist (N = 54) protocols |
|
| Embryo Transfer Strategy | ||
| Study | Intervention | Results |
| Niu et al. (2013) [122] |
|
|
| Park et al. (2016) [121] |
Group B: fresh ET with GnRHa pre-treatment (N = 105) Group C: FET with GnRHa pre-treatment (N = 43) |
|
| Liang et al. (2019) [131] |
|
|
| Chen et al. (2020) [132] |
|
|
| Li et al. (2021) [133] |
|
|
| Zhang et al. (2022) [134] |
|
|
| Feng et al. (2022) [135] |
|
|
| Yang et al. (2023) [136] |
(Subgroups in GnRHa-HRT protocol: one, two, and three or more GnRHa injections) |
|
| Ge et al. (2023) [129] |
|
|
| Li et al. (2023) [137] |
(Subgroups in downregulation group: GnRHa for 1 month, 2 months, or ≥3 months) |
|
CPR: clinical pregnancy rate; LBR: live birth rate; MR: miscarriage rate; IR: implantation rate; OR: odd ratio; CI: confidence interval; ET: embryo transfer; FET: frozen embryo transfer; HRT: hormonal replacement therapy; OI: ovulation induction; NC: natural cycle.
4.2. Embryo Transfer Strategy
Frozen embryo transfer (FET) is commonly used when the endometrial characteristics are unsuitable for fresh cycle transfer, when there is a high risk of ovarian hyperstimulation syndrome, and when there is further promotion of the cumulative live birth rate [138]. FET with artificial endometrial preparation is widely accepted due to the mechanism that ovarian suppression induced by the hormone replacement regimen possibly plays a role in reducing endometrial alterations linked to ovarian function in adenomyosis [129,130]. With the pre-treatment of long-term GnRHa downregulation, FET was a protective factor for the LBR and a cost-effective method with a lower total gonadotrophin dosage and shorter stimulation duration than fresh ET with an ultra-long protocol [130].
4.2.1. Segmentation of Embryo Transfer
The pre-treatment of hormonal suppression, such as through GnRHa or progestins, 3–6 months before FET, also known as deferred ET or segmental ET, was thought to produce a hypo-estrogen status, causing the regression of adenomyotic lesions and the correction of endometrial alterations, thus improving the ART outcomes. Based on these theories, a freeze-all cycle with a deferred embryo transfer strategy is recommended for patients with endometriosis [139], a treatment of choice that does not increase the risk of endometriosis flare [140,141,142,143]. Studies have shown that reproductive outcomes significantly improved in women with adenomyosis undergoing deferred ET with long-term GnRHa preparation for 2 to 4 months [92,122,134]. Interestingly, Zhang et al. found that the uterine volume did not change before or after the GnRHa treatment (82.0 ± 13.4 cm3 vs. 79.3 ± 14.0 cm3; p = 0.123), suggesting that the downregulation effect of GnRHa may improve pregnancy outcomes in other ways [134]. Also, women undergoing in vitro fertilization (IVF) with LNG-IUS pre-treatment for three months before FET have higher clinical pregnancy, implantation, and ongoing pregnancy rates [131]. Another case report showed that a patient receiving deferred ET after dienogest pre-treatment for three months achieved pregnancy with reduced adenomyotic lesions and serum marker cancer antigen-125 (CA-125) [135].
4.2.2. GnRHa Pre-Treatment
FET following long-term GnRHa pre-treatment has a better ART outcome and a potential benefit in terms of a lower gonadotrophin dose and a shorter stimulation duration than fresh ET combined with a long or ultra-long GnRHa protocol [130]. GnRHa has been found to markedly suppress the hypothalamus–pituitary–ovarian axis and reduce the angiogenesis and inflammatory response of adenomyotic foci, leading to the regression of adenomyosis as well as symptom relief [121,144]. Regarding the effect of GnRHa on endometrial receptivity in women with adenomyosis, Tian et al. proposed a transcriptome analysis of the eutopic endometrium, which identified the systemic role and underlying cellular regulatory mechanisms of GnRHa treatment in adenomyosis-associated infertility [145]. After GnRHa treatment, the study elucidated 132 differentially expressed genes in the eutopic endometria of women with adenomyosis. Chemokine (C-C motif) ligand 21 (CCL21), related to immune system-associated signal transduction, was highly expressed after the GnRHa treatment, indicating that a molecular regulation may be involved in the improvement of endometrial receptivity in adenomyosis. Nevertheless, the routine use of GnRHa before fertility management in infertile women with adenomyosis remains conflicting. According to some retrospective studies [121,129,133,146], pre-treatment with GnRHa before FET has not shown a beneficial effect on IVF outcomes in women with adenomyosis. Moreover, a higher miscarriage rate (MR) was found in women with adenomyosis undergoing IVF with GnRHa pre-treatment [132,136,137]. A recent retrospective study revealed that the GnRHa downregulation group had a larger mean diameter of the uterus and a higher proportion of severe dysmenorrhea at baseline than the non-downregulation group [137]. The pregnancy outcomes had no difference between the two groups, except for a higher MR in the GnRHa downregulation group, suggesting that the MR was difficult to reverse through GnRHa treatment in severe adenomyosis. Randomized controlled trials with more cases should be designed to verify the correlation between a higher MR and GnRHa treatment in adenomyosis. Conflicting results may be attributed to a mixed variety of adenomyosis features without a proper classification and a lack of consensus on ART protocols.
4.2.3. Oxytocin Antagonists
Uterine hyperperistalsis with higher serum oxytocin levels was found in women with endometriosis compared to healthy controls [147,148], which may contribute to the development of endometriosis as well as to adverse effects on IVF outcomes in women with endometriosis. The increased immunoreactivity of oxytocin receptors has been found in eutopic endometrial stromal and epithelial cells and in myometrial and vascular cells in ectopic adenomyosis foci, correlating with the severity of dysmenorrhea [149]. Atosiban, an oxytocin receptor antagonist, can decrease myometrial contractility and preferentially relax uterine arteries, enhancing endometrial perfusion and supporting embryo implantation [150]. A randomized controlled study has shown that Atosiban treatment before FET provides better clinical efficacy in the priming of the uterus in patients with endometriosis [147]. Lin et al. reported that atosiban increased the pregnancy rate among patients with endometriosis without coexisting adenomyosis but not for those with coexisting adenomyosis [151]. They stratified the analyses by adenomyosis features and found an insignificant benefit of atosiban therapy among patients with more extensive adenomyosis. Further evidence is required to prove that atosiban has a therapeutic role in adenomyosis-associated infertility.
4.3. Uterus Sparing Surgery
Fertility-preserving adenomyomectomy plans to balance the advantages of removing the pathology against the disadvantages of possibly destroying the uterine structure. Proper conservative surgery seems to restore fertility in women with adenomyosis, as successful pregnancies have been reported in a systematic review [126]. Many methods and techniques have been demonstrated for proper excision of the affected area and reconstruction of the myometrial defect, either by laparoscopy, laparotomy, or hysteroscopy.
In a systematic review study, Grimbizis et al. reported pregnancy rates of 60.5% after complete excision, 46.9% after partial excision of adenomyosis, and 55.6% after non-excisional techniques [152]. Rocha et al. reported a higher spontaneous pregnancy rate in the group with GnRHa for 24 weeks after surgery compared with surgery alone (40.7% vs. 15.0%; p = 0.002) [126]. Younes et al. reported that the odds ratio of clinical pregnancy rates after surgery for adenomyosis was 6.22 (95% CI 2.34–16.54) in a meta-analysis [92] and reported successful pregnancies after fertility-preserving surgery in three-fourths of the cases treated for adenomyosis in another review [153]. Tan et al. compared the reproductive outcomes in diffuse versus focal adenomyosis following surgical or combined medical management. Their results show that women with focal adenomyosis have higher pregnancy rates (54.8% versus 31.3%), live birth rates (45.1% versus 23.8%), and surprisingly higher miscarriage rates (21.8% versus 19.6%) than those with diffuse adenomyosis [154]. In a recent meta-analysis, Jiang suggested excisional treatment as a consideration for patients with symptomatic adenomyosis and infertility for several years or repeated failure with ART [155]. However, there is a lack of consensus on the rationale for removing the adenomyotic foci to improve fertility due to the high heterogenicity between studies. The surgeon’s experience is important in managing an optimal surgical method for adenomyosis; several surgical techniques (open or laparoscopic), excision techniques (complete or partial adenomyomectomy), and modified closure techniques (U-shaped suturing, overlapping flaps, double-/triple-flap method, and transverse H-incisions) have been proposed [156,157].
Fertility-preserving surgical treatment for adenomyosis is associated with a higher risk of adverse obstetric outcomes in future pregnancies. The removal of adenomyotic foci with significant amounts of myometrium may cause the formation of uterine scars and a reduction in uterine capacity, which results in the uterus having a lack of ability to grow during pregnancy, thus increasing the risk of uterine rupture. The risk of uterine rupture during pregnancy is more than 1.0% versus 0.26% in women receiving uterine adenomyomectomy and myomectomy, respectively [158]. Otsubo et al. suggested that preserving a 9 to 15 mm uterine wall thickness after an adenomyotic foci excision is safe for future pregnancies [159]. In addition, the destruction of the endometrium, together with the junctional zone, may cause serial obstetric complications, including miscarriage, preterm birth, and placentation disorders. Although the presented studies favored the safety of the obstetric outcomes in women treated with adenomyomectomy, it is uncertain whether surgery is involved in better reproductive performance or not.
5. Prognostic Tools for Adenomyosis-Associated Infertility
An increasing number of studies have reported the impact of adenomyosis features on successful pregnancy outcomes after fertility treatment, including the extent or severity of adenomyosis lesions, based on images and clinical presentation. As adenomyosis becomes more prevalent in older women, a degree of confounding factors, such as declining ovarian reserve and an older age, harms reproductive outcomes.
5.1. Imaging Features of Adenomyosis
Adenomyosis is expressed as several morphologic characteristics, including asymmetrical myometrial thickening, intramyometrial cysts or hyperechoic islands, linear striae, fan-shaped shadowing, myometrial echogenic subendometrial lines and buds, translesional vascularity, and the disruption of the endometrial myometrial junction, which increases the magnitude of the adverse effect [160]. With the evolution of imaging techniques, such as high-resolution ultrasound and magnetic resonance imaging (MRI), we can now diagnose adenomyosis relatively reliably in women undergoing conservative treatments. Although no uniform standardized reporting system exists for image-based adenomyosis diagnostic criteria, the International Morphological Uterus Sonographic Assessment (MUSA) group agreed on terminology for describing myometrial lesions in ultrasonography. The sonographic features of adenomyosis could be described and classified according to their lesion size, location, differentiation (focal/diffuse), appearance (cystic/non-cystic), uterine myometrium involvement (depth of invasion), disease extent (<25%, 25–50%, and >50% of uterine volume), and number of foci [161]. Recently, several studies proposed a positive correlation between the cumulative impact of ultrasound parameters and the clinical features of adenomyosis [162].
Furthermore, the presence of numerous sonographic features of adenomyosis worsens fertility outcomes. According to a multicenter prospective study, the clinical pregnancy rate decreased from 42.7% in the control group to 22.9% and 13.0% in women with four and seven ultrasound diagnostic features of adenomyosis, respectively [163]. Additionally, the focal type of adenomyosis seems to have a more significant negative effect than other types [128,164]. A significant lower cumulative pregnancy rate and severe obstetric complications, such as placenta previa, placenta accreta, preeclampsia, and preterm birth, were associated with adenomyosis located in the posterior uterine wall, possibly due to a higher concurrence rate of ovarian endometrioma, pelvic adhesion, and revised American Society for Reproductive Medicine (rASRM) scores [165]. However, a recent systematic review and meta-analysis revealed that women with focal adenomyosis do not significantly affect the reproductive outcome compared to those with diffuse lesions [124]. A validated model that includes sonographic predictors and symptoms of adenomyosis may enrich clinical practice regarding adenomyosis.
5.2. Serum Marker
The serum marker cancer antigen 125 (CA-125) is positively correlated with the severity of adenomyosis. It indicates concomitant mixed endometriosis, suggesting that CA-125 may be a valuable indicator for monitoring the efficacy of adenomyosis treatment and future fertility outcomes [166,167,168]. A retrospective study of women with severe adenomyosis treated with a six-month course of GnRH agonist following conservative surgery showed that the severity of dysmenorrhea was significantly improved with a decline in the serum level of CA-125 [167]. A higher spontaneous pregnancy rate was found in women with a postoperative serum level of CA-125 of less than 10.00 IU/mL. Another retrospective study found that patients with a greater than sevenfold decrease in the CA-125 level after GnRH agonist treatment might have better IVF outcomes [166]. Chang et al. showed that patients with adenomyosis who had a successful live birth during the three-year follow-up after surgical–medical therapy tended to be younger and nulliparous with a lower body mass index, lower baseline analgesic usage score, lower preoperative serum CA-125, and with an anterior adenoma location [168]. However, to evaluate the pregnancy-associated factors, a stepwise multivariate linear regression analysis showed that only age and the baseline analgesic usage score were independent predictors of future pregnancy in women with adenomyosis who underwent treatment.
6. Conclusions
Adenomyosis, defined as endometrial cell invasion into the myometrium, usually presents with pelvic pain, heavy menstrual bleeding, and reproductive failure, which may be associated with abnormal local effects of sex steroid and pituitary hormones, immune response, inflammatory factors, and neuroangiogenic mediators. The proposed pathogenetic mechanisms affect the uterine cavity’s receptivity and the endometrial molecular expression necessary for embryo implantation, resulting in decreased pregnancy rates, higher miscarriage rates, and obstetric complications. According to current evidence, the management of adenomyosis, either through medical or surgical approaches, may positively affect reproductive outcomes. Women receiving assisted reproductive treatments with a downregulation protocol or segmental embryo transfer appear to have better pregnancy results. More research is necessary to evaluate the management of adenomyosis-associated infertility and provide treatment guidance for the challenging condition of adenomyosis.
Author Contributions
H.-M.W., T.-C.T., S.-M.L., A.H.-Y.P. and L.-H.C. contributed to the concept, design, literature review, draft, and final approval of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research was funded by the Chang Gung Foundation (CMRPG3I0423; CMRPG3L0803; CMRPG3M0872).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Kennedy S., Bergqvist A., Chapron C., D’Hooghe T., Dunselman G., Greb R., Hummelshoj L., Prentice A., Saridogan E. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum. Reprod. 2005;20:2698–2704. doi: 10.1093/humrep/dei135. [DOI] [PubMed] [Google Scholar]
- 2.Peric H., Fraser I.S. The symptomatology of adenomyosis. Best. Pract. Res. Clin. Obstet. Gynaecol. 2006;20:547–555. doi: 10.1016/j.bpobgyn.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Taran F.A., Wallwiener M., Kabashi D., Rothmund R., Rall K., Kraemer B., Brucker S.Y. Clinical characteristics indicating adenomyosis at the time of hysterectomy: A retrospective study in 291 patients. Arch. Gynecol. Obstet. 2012;285:1571–1576. doi: 10.1007/s00404-011-2180-7. [DOI] [PubMed] [Google Scholar]
- 4.Naftalin J., Hoo W., Pateman K., Mavrelos D., Holland T., Jurkovic D. How common is adenomyosis? A prospective study of prevalence using transvaginal ultrasound in a gynaecology clinic. Hum. Reprod. 2012;27:3432–3439. doi: 10.1093/humrep/des332. [DOI] [PubMed] [Google Scholar]
- 5.Yeniel O., Cirpan T., Ulukus M., Ozbal A., Gundem G., Ozsener S., Zekioglu O., Yilmaz H. Adenomyosis: Prevalence, risk factors, symptoms and clinical findings. Clin. Exp. Obstet. Gynecol. 2007;34:163–167. [PubMed] [Google Scholar]
- 6.Bazot M., Darai E. Role of transvaginal sonography and magnetic resonance imaging in the diagnosis of uterine adenomyosis. Fertil. Steril. 2018;109:389–397. doi: 10.1016/j.fertnstert.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 7.Andres M.P., Borrelli G.M., Ribeiro J., Baracat E.C., Abrao M.S., Kho R.M. Transvaginal Ultrasound for the Diagnosis of Adenomyosis: Systematic Review and Meta-Analysis. J. Minim. Invasive Gynecol. 2018;25:257–264. doi: 10.1016/j.jmig.2017.08.653. [DOI] [PubMed] [Google Scholar]
- 8.Kishi Y., Suginami H., Kuramori R., Yabuta M., Suginami R., Taniguchi F. Four subtypes of adenomyosis assessed by magnetic resonance imaging and their specification. Am. J. Obstet. Gynecol. 2012;207:114.e1–114.e7. doi: 10.1016/j.ajog.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 9.Vercellini P., Vigano P., Somigliana E., Daguati R., Abbiati A., Fedele L. Adenomyosis: Epidemiological factors. Best. Pract. Res. Clin. Obstet. Gynaecol. 2006;20:465–477. doi: 10.1016/j.bpobgyn.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 10.Li X., Liu X., Guo S.W. Clinical profiles of 710 premenopausal women with adenomyosis who underwent hysterectomy. J. Obstet. Gynaecol. Res. 2014;40:485–494. doi: 10.1111/jog.12211. [DOI] [PubMed] [Google Scholar]
- 11.Pinzauti S., Lazzeri L., Tosti C., Centini G., Orlandini C., Luisi S., Zupi E., Exacoustos C., Petraglia F. Transvaginal sonographic features of diffuse adenomyosis in 18-30-year-old nulligravid women without endometriosis: Association with symptoms. Ultrasound Obstet. Gynecol. 2015;46:730–736. doi: 10.1002/uog.14834. [DOI] [PubMed] [Google Scholar]
- 12.Puente J.M., Fabris A., Patel J., Patel A., Cerrillo M., Requena A., Garcia-Velasco J.A. Adenomyosis in infertile women: Prevalence and the role of 3D ultrasound as a marker of severity of the disease. Reprod. Biol. Endocrinol. 2016;14:60. doi: 10.1186/s12958-016-0185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naftalin J., Hoo W., Pateman K., Mavrelos D., Foo X., Jurkovic D. Is adenomyosis associated with menorrhagia? Hum. Reprod. 2014;29:473–479. doi: 10.1093/humrep/det451. [DOI] [PubMed] [Google Scholar]
- 14.Leyendecker G., Bilgicyildirim A., Inacker M., Stalf T., Huppert P., Mall G., Bottcher B., Wildt L. Adenomyosis and endometriosis. Re-visiting their association and further insights into the mechanisms of auto-traumatisation. An MRI study. Arch. Gynecol. Obstet. 2015;291:917–932. doi: 10.1007/s00404-014-3437-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chapron C., Tosti C., Marcellin L., Bourdon M., Lafay-Pillet M.C., Millischer A.E., Streuli I., Borghese B., Petraglia F., Santulli P. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum. Reprod. 2017;32:1393–1401. doi: 10.1093/humrep/dex088. [DOI] [PubMed] [Google Scholar]
- 16.Di Donato N., Montanari G., Benfenati A., Leonardi D., Bertoldo V., Monti G., Raimondo D., Seracchioli R. Prevalence of adenomyosis in women undergoing surgery for endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;181:289–293. doi: 10.1016/j.ejogrb.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Eisenberg V.H., Arbib N., Schiff E., Goldenberg M., Seidman D.S., Soriano D. Sonographic Signs of Adenomyosis Are Prevalent in Women Undergoing Surgery for Endometriosis and May Suggest a Higher Risk of Infertility. Biomed. Res. Int. 2017;2017:8967803. doi: 10.1155/2017/8967803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma R.K., Azeem A., Agarwal A. Spindle and chromosomal alterations in metaphase II oocytes. Reprod. Sci. 2013;20:1293–1301. doi: 10.1177/1933719113483018. [DOI] [PubMed] [Google Scholar]
- 19.Pellicer A., Oliveira N., Ruiz A., Remohi J., Simon C. Exploring the mechanism(s) of endometriosis-related infertility: An analysis of embryo development and implantation in assisted reproduction. Hum. Reprod. 1995;10((Suppl. 2)):91–97. doi: 10.1093/humrep/10.suppl_2.91. [DOI] [PubMed] [Google Scholar]
- 20.Arici A., Oral E., Bukulmez O., Duleba A., Olive D.L., Jones E.E. The effect of endometriosis on implantation: Results from the Yale University in vitro fertilization and embryo transfer program. Fertil. Steril. 1996;65:603–607. doi: 10.1016/S0015-0282(16)58162-X. [DOI] [PubMed] [Google Scholar]
- 21.Vannuccini S., Tosti C., Carmona F., Huang S.J., Chapron C., Guo S.W., Petraglia F. Pathogenesis of adenomyosis: An update on molecular mechanisms. Reprod. Biomed. Online. 2017;35:592–601. doi: 10.1016/j.rbmo.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 22.Zhai J., Vannuccini S., Petraglia F., Giudice L.C. Adenomyosis: Mechanisms and Pathogenesis. Semin. Reprod. Med. 2020;38:129–143. doi: 10.1055/s-0040-1716687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vannuccini S., Petraglia F. Recent advances in understanding and managing adenomyosis. F1000Research. 2019;8:283. doi: 10.12688/f1000research.17242.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Solares J., Donnez J., Donnez O., Dolmans M.M. Pathogenesis of uterine adenomyosis: Invagination or metaplasia? Fertil. Steril. 2018;109:371–379. doi: 10.1016/j.fertnstert.2017.12.030. [DOI] [PubMed] [Google Scholar]
- 25.Brosens J.J., de Souza N.M., Barker F.G. Uterine junctional zone: Function and disease. Lancet. 1995;346:558–560. doi: 10.1016/S0140-6736(95)91387-4. [DOI] [PubMed] [Google Scholar]
- 26.Naftalin J., Jurkovic D. The endometrial-myometrial junction: A fresh look at a busy crossing. Ultrasound Obstet. Gynecol. 2009;34:1–11. doi: 10.1002/uog.6432. [DOI] [PubMed] [Google Scholar]
- 27.Uduwela A.S., Perera M.A., Aiqing L., Fraser I.S. Endometrial-myometrial interface: Relationship to adenomyosis and changes in pregnancy. Obstet. Gynecol. Surv. 2000;55:390–400. doi: 10.1097/00006254-200006000-00025. [DOI] [PubMed] [Google Scholar]
- 28.Hricak H., Alpers C., Crooks L.E., Sheldon P.E. Magnetic resonance imaging of the female pelvis: Initial experience. AJR Am. J. Roentgenol. 1983;141:1119–1128. doi: 10.2214/ajr.141.6.1119. [DOI] [PubMed] [Google Scholar]
- 29.Rasmussen C.K., Hansen E.S., Dueholm M. Two- and three-dimensional ultrasonographic features related to histopathology of the uterine endometrial-myometrial junctional zone. Acta Obstet. Gynecol. Scand. 2019;98:205–214. doi: 10.1111/aogs.13484. [DOI] [PubMed] [Google Scholar]
- 30.Ijland M.M., Evers J.L., Dunselman G.A., van Katwijk C., Lo C.R., Hoogland H.J. Endometrial wavelike movements during the menstrual cycle. Fertil. Steril. 1996;65:746–749. doi: 10.1016/S0015-0282(16)58207-7. [DOI] [PubMed] [Google Scholar]
- 31.Noe M., Kunz G., Herbertz M., Mall G., Leyendecker G. The cyclic pattern of the immunocytochemical expression of oestrogen and progesterone receptors in human myometrial and endometrial layers: Characterization of the endometrial-subendometrial unit. Hum. Reprod. 1999;14:190–197. doi: 10.1093/humrep/14.1.190. [DOI] [PubMed] [Google Scholar]
- 32.Lyons E.A., Taylor P.J., Zheng X.H., Ballard G., Levi C.S., Kredentser J.V. Characterization of subendometrial myometrial contractions throughout the menstrual cycle in normal fertile women. Fertil. Steril. 1991;55:771–774. doi: 10.1016/S0015-0282(16)54246-0. [DOI] [PubMed] [Google Scholar]
- 33.Aguilar H.N., Mitchell B.F. Physiological pathways and molecular mechanisms regulating uterine contractility. Hum. Reprod. Update. 2010;16:725–744. doi: 10.1093/humupd/dmq016. [DOI] [PubMed] [Google Scholar]
- 34.Kurowicka B., Franczak A., Oponowicz A., Kotwica G. In vitro contractile activity of porcine myometrium during luteolysis and early pregnancy: Effect of oxytocin and progesterone. Reprod. Biol. 2005;5:151–169. [PubMed] [Google Scholar]
- 35.Bergeron C., Amant F., Ferenczy A. Pathology and physiopathology of adenomyosis. Best. Pract. Res. Clin. Obstet. Gynaecol. 2006;20:511–521. doi: 10.1016/j.bpobgyn.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 36.Mehasseb M.K., Taylor A.H., Pringle J.H., Bell S.C., Habiba M. Enhanced invasion of stromal cells from adenomyosis in a three-dimensional coculture model is augmented by the presence of myocytes from affected uteri. Fertil. Steril. 2010;94:2547–2551. doi: 10.1016/j.fertnstert.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 37.Li J., Yanyan M., Mu L., Chen X., Zheng W. The expression of Bcl-2 in adenomyosis and its effect on proliferation, migration, and apoptosis of endometrial stromal cells. Pathol. Res. Pract. 2019;215:152477. doi: 10.1016/j.prp.2019.152477. [DOI] [PubMed] [Google Scholar]
- 38.Guo J., Chen L., Luo N., Li C., Chen R., Qu X., Liu M., Kang L., Cheng Z. LPS/TLR4-mediated stromal cells acquire an invasive phenotype and are implicated in the pathogenesis of adenomyosis. Sci. Rep. 2016;6:21416. doi: 10.1038/srep21416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu X., Shen M., Qi Q., Zhang H., Guo S.W. Corroborating evidence for platelet-induced epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation in the development of adenomyosis. Hum. Reprod. 2016;31:734–749. doi: 10.1093/humrep/dew018. [DOI] [PubMed] [Google Scholar]
- 40.Chen Y.J., Li H.Y., Huang C.H., Twu N.F., Yen M.S., Wang P.H., Chou T.Y., Liu Y.N., Chao K.C., Yang M.H. Oestrogen-induced epithelial-mesenchymal transition of endometrial epithelial cells contributes to the development of adenomyosis. J. Pathol. 2010;222:261–270. doi: 10.1002/path.2761. [DOI] [PubMed] [Google Scholar]
- 41.Herndon C.N., Aghajanova L., Balayan S., Erikson D., Barragan F., Goldfien G., Vo K.C., Hawkins S., Giudice L.C. Global Transcriptome Abnormalities of the Eutopic Endometrium From Women With Adenomyosis. Reprod. Sci. 2016;23:1289–1303. doi: 10.1177/1933719116650758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tokyol C., Aktepe F., Dilek F.H., Sahin O., Arioz D.T. Expression of cyclooxygenase-2 and matrix metalloproteinase-2 in adenomyosis and endometrial polyps and its correlation with angiogenesis. Int. J. Gynecol. Pathol. 2009;28:148–156. doi: 10.1097/PGP.0b013e318187033b. [DOI] [PubMed] [Google Scholar]
- 43.Li T., Li Y.G., Pu D.M. Matrix metalloproteinase-2 and -9 expression correlated with angiogenesis in human adenomyosis. Gynecol. Obstet. Investig. 2006;62:229–235. doi: 10.1159/000094426. [DOI] [PubMed] [Google Scholar]
- 44.Leyendecker G., Wildt L. A new concept of endometriosis and adenomyosis: Tissue injury and repair (TIAR) Horm. Mol. Biol. Clin. Investig. 2011;5:125–142. doi: 10.1515/HMBCI.2011.002. [DOI] [PubMed] [Google Scholar]
- 45.Curtis K.M., Hillis S.D., Marchbanks P.A., Peterson H.B. Disruption of the endometrial-myometrial border during pregnancy as a risk factor for adenomyosis. Am. J. Obstet. Gynecol. 2002;187:543–544. doi: 10.1067/mob.2002.124285. [DOI] [PubMed] [Google Scholar]
- 46.Shaked S., Jaffa A.J., Grisaru D., Elad D. Uterine peristalsis-induced stresses within the uterine wall may sprout adenomyosis. Biomech. Model. Mechanobiol. 2015;14:437–444. doi: 10.1007/s10237-014-0614-4. [DOI] [PubMed] [Google Scholar]
- 47.Kunz G., Noe M., Herbertz M., Leyendecker G. Uterine peristalsis during the follicular phase of the menstrual cycle: Effects of oestrogen, antioestrogen and oxytocin. Hum. Reprod. Update. 1998;4:647–654. doi: 10.1093/humupd/4.5.647. [DOI] [PubMed] [Google Scholar]
- 48.Gargett C.E., Schwab K.E., Deane J.A. Endometrial stem/progenitor cells: The first 10 years. Hum. Reprod. Update. 2016;22:137–163. doi: 10.1093/humupd/dmv051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gargett C.E. Uterine stem cells: What is the evidence? Hum. Reprod. Update. 2007;13:87–101. doi: 10.1093/humupd/dml045. [DOI] [PubMed] [Google Scholar]
- 50.Gargett C.E., Schwab K.E., Zillwood R.M., Nguyen H.P., Wu D. Isolation and culture of epithelial progenitors and mesenchymal stem cells from human endometrium. Biol. Reprod. 2009;80:1136–1145. doi: 10.1095/biolreprod.108.075226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Marcellin L., Santulli P., Bortolato S., Morin C., Millischer A.E., Borghese B., Chapron C. Anterior Focal Adenomyosis and Bladder Deep Infiltrating Endometriosis: Is There a Link? J. Minim. Invasive Gynecol. 2018;25:896–901. doi: 10.1016/j.jmig.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 52.Artymuk N., Zotova O., Gulyaeva L. Adenomyosis: Genetics of estrogen metabolism. Horm. Mol. Biol. Clin. Investig. 2019;37:20180069. doi: 10.1515/hmbci-2018-0069. [DOI] [PubMed] [Google Scholar]
- 53.Tong X., Li Z., Wu Y., Fu X., Zhang Y., Fan H. COMT 158G/A and CYP1B1 432C/G polymorphisms increase the risk of endometriosis and adenomyosis: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;179:17–21. doi: 10.1016/j.ejogrb.2014.04.039. [DOI] [PubMed] [Google Scholar]
- 54.Hong D.G., Park J.Y., Chong G.O., Lee Y.H., Lee H.J., Shinn J.U., Lee Y.S., Seong W.J. Transmembrane G protein-coupled receptor 30 gene polymorphisms and uterine adenomyosis in Korean women. Gynecol. Endocrinol. 2019;35:498–501. doi: 10.1080/09513590.2018.1540572. [DOI] [PubMed] [Google Scholar]
- 55.Kitawaki J., Obayashi H., Ishihara H., Koshiba H., Kusuki I., Kado N., Tsukamoto K., Hasegawa G., Nakamura N., Honjo H. Oestrogen receptor-alpha gene polymorphism is associated with endometriosis, adenomyosis and leiomyomata. Hum. Reprod. 2001;16:51–55. doi: 10.1093/humrep/16.1.51. [DOI] [PubMed] [Google Scholar]
- 56.Ye H., He Y., Wang J., Song T., Lan Z., Zhao Y., Xi M. Effect of matrix metalloproteinase promoter polymorphisms on endometriosis and adenomyosis risk: Evidence from a meta-analysis. J. Genet. 2016;95:611–619. doi: 10.1007/s12041-016-0675-5. [DOI] [PubMed] [Google Scholar]
- 57.Kang S., Zhao J., Liu Q., Zhou R., Wang N., Li Y. Vascular endothelial growth factor gene polymorphisms are associated with the risk of developing adenomyosis. Environ. Mol. Mutagen. 2009;50:361–366. doi: 10.1002/em.20455. [DOI] [PubMed] [Google Scholar]
- 58.Wang Y., Qu Y., Song W. Genetic variation in COX-2 -1195 and the risk of endometriosis and adenomyosis. Clin. Exp. Obstet. Gynecol. 2015;42:168–172. doi: 10.12891/ceog1747.2015. [DOI] [PubMed] [Google Scholar]
- 59.Inoue S., Hirota Y., Ueno T., Fukui Y., Yoshida E., Hayashi T., Kojima S., Takeyama R., Hashimoto T., Kiyono T., et al. Uterine adenomyosis is an oligoclonal disorder associated with KRAS mutations. Nat. Commun. 2019;10:5785. doi: 10.1038/s41467-019-13708-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu X., Guo S.W. Aberrant immunoreactivity of deoxyribonucleic acid methyltransferases in adenomyosis. Gynecol. Obstet. Investig. 2012;74:100–108. doi: 10.1159/000337718. [DOI] [PubMed] [Google Scholar]
- 61.Xiang Y., Sun Y., Yang B., Yang Y., Zhang Y., Yu T., Huang H., Zhang J., Xu H. Transcriptome sequencing of adenomyosis eutopic endometrium: A new insight into its pathophysiology. J. Cell Mol. Med. 2019;23:8381–8391. doi: 10.1111/jcmm.14718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jichan N., Xishi L., Guo S.W. Promoter hypermethylation of progesterone receptor isoform B (PR-B) in adenomyosis and its rectification by a histone deacetylase inhibitor and a demethylation agent. Reprod. Sci. 2010;17:995–1005. doi: 10.1177/1933719110377118. [DOI] [PubMed] [Google Scholar]
- 63.Liu X., Guo S.W. Valproic acid alleviates generalized hyperalgesia in mice with induced adenomyosis. J. Obstet. Gynaecol. Res. 2011;37:696–708. doi: 10.1111/j.1447-0756.2011.01655.x. [DOI] [PubMed] [Google Scholar]
- 64.Zhai J., Li S., Sen S., Opoku-Anane J., Du Y., Chen Z.J., Giudice L.C. m(6)A RNA Methylation Regulators Contribute to Eutopic Endometrium and Myometrium Dysfunction in Adenomyosis. Front. Genet. 2020;11:716. doi: 10.3389/fgene.2020.00716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yamamoto T., Noguchi T., Tamura T., Kitawaki J., Okada H. Evidence for estrogen synthesis in adenomyotic tissues. Am. J. Obstet. Gynecol. 1993;169:734–738. doi: 10.1016/0002-9378(93)90654-2. [DOI] [PubMed] [Google Scholar]
- 66.Xue Q., Xu Y., Yang H., Zhang L., Shang J., Zeng C., Yin P., Bulun S.E. Methylation of a novel CpG island of intron 1 is associated with steroidogenic factor 1 expression in endometriotic stromal cells. Reprod. Sci. 2014;21:395–400. doi: 10.1177/1933719113497283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kitawaki J., Koshiba H., Ishihara H., Kusuki I., Tsukamoto K., Honjo H. Progesterone induction of 17beta-hydroxysteroid dehydrogenase type 2 during the secretory phase occurs in the endometrium of estrogen-dependent benign diseases but not in normal endometrium. J. Clin. Endocrinol. Metab. 2000;85:3292–3296. doi: 10.1210/jcem.85.9.6829. [DOI] [PubMed] [Google Scholar]
- 68.Mehasseb M.K., Panchal R., Taylor A.H., Brown L., Bell S.C., Habiba M. Estrogen and progesterone receptor isoform distribution through the menstrual cycle in uteri with and without adenomyosis. Fertil. Steril. 2011;95:2228–2235.e1. doi: 10.1016/j.fertnstert.2011.02.051. [DOI] [PubMed] [Google Scholar]
- 69.Sztachelska M., Ponikwicka-Tyszko D., Martinez-Rodrigo L., Bernaczyk P., Palak E., Polchlopek W., Bielawski T., Wolczynski S. Functional Implications of Estrogen and Progesterone Receptors Expression in Adenomyosis, Potential Targets for Endocrinological Therapy. J. Clin. Med. 2022;11:4407. doi: 10.3390/jcm11154407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bulun S.E., Cheng Y.H., Pavone M.E., Xue Q., Attar E., Trukhacheva E., Tokunaga H., Utsunomiya H., Yin P., Luo X., et al. Estrogen receptor-beta, estrogen receptor-alpha, and progesterone resistance in endometriosis. Semin. Reprod. Med. 2010;28:36–43. doi: 10.1055/s-0029-1242991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ota H., Igarashi S., Hatazawa J., Tanaka T. Is adenomyosis an immune disease? Hum. Reprod. Update. 1998;4:360–367. doi: 10.1093/humupd/4.4.360. [DOI] [PubMed] [Google Scholar]
- 72.Wang F., Wen Z., Li H., Yang Z., Zhao X., Yao X. Human leukocyte antigen-G is expressed by the eutopic and ectopic endometrium of adenomyosis. Fertil. Steril. 2008;90:1599–1604. doi: 10.1016/j.fertnstert.2007.06.073. [DOI] [PubMed] [Google Scholar]
- 73.Carrarelli P., Yen C.F., Funghi L., Arcuri F., Tosti C., Bifulco G., Luddi A., Lee C.L., Petraglia F. Expression of Inflammatory and Neurogenic Mediators in Adenomyosis. Reprod. Sci. 2017;24:369–375. doi: 10.1177/1933719116657192. [DOI] [PubMed] [Google Scholar]
- 74.Li B., Chen M., Liu X., Guo S.W. Constitutive and tumor necrosis factor-alpha-induced activation of nuclear factor-kappaB in adenomyosis and its inhibition by andrographolide. Fertil. Steril. 2013;100:568–577. doi: 10.1016/j.fertnstert.2013.04.028. [DOI] [PubMed] [Google Scholar]
- 75.Chen L.H., Chan S.H., Li C.J., Wu H.M., Huang H.Y. Altered Expression of Interleukin-18 System mRNA at the Level of Endometrial Myometrial Interface in Women with Adenomyosis. Curr. Issues Mol. Biol. 2022;44:5550–5561. doi: 10.3390/cimb44110376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang X., Lu B., Huang X., Xu H., Zhou C., Lin J. Innervation of endometrium and myometrium in women with painful adenomyosis and uterine fibroids. Fertil. Steril. 2010;94:730–737. doi: 10.1016/j.fertnstert.2009.03.026. [DOI] [PubMed] [Google Scholar]
- 77.Wang F., Shi X., Qin X., Wen Z., Zhao X., Li C. Expression of CD56 in patients with adenomyosis and its correlation with dysmenorrhea. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015;194:101–105. doi: 10.1016/j.ejogrb.2015.08.027. [DOI] [PubMed] [Google Scholar]
- 78.Nie J., Liu X., Zheng Y., Geng J.G., Guo S.W. Increased immunoreactivity to SLIT/ROBO1 and its correlation with severity of dysmenorrhea in adenomyosis. Fertil. Steril. 2011;95:1164–1167. doi: 10.1016/j.fertnstert.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 79.Carrarelli P., Yen C.F., Arcuri F., Funghi L., Tosti C., Wang T.H., Huang J.S., Petraglia F. Myostatin, follistatin and activin type II receptors are highly expressed in adenomyosis. Fertil. Steril. 2015;104:744–752.e1. doi: 10.1016/j.fertnstert.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 80.Zhou S., Yi T., Liu R., Bian C., Qi X., He X., Wang K., Li J., Zhao X., Huang C., et al. Proteomics identification of annexin A2 as a key mediator in the metastasis and proangiogenesis of endometrial cells in human adenomyosis. Mol. Cell Proteomics. 2012;11:M112 017988. doi: 10.1074/mcp.M112.017988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Huang T.S., Chen Y.J., Chou T.Y., Chen C.Y., Li H.Y., Huang B.S., Tsai H.W., Lan H.Y., Chang C.H., Twu N.F., et al. Oestrogen-induced angiogenesis promotes adenomyosis by activating the Slug-VEGF axis in endometrial epithelial cells. J. Cell Mol. Med. 2014;18:1358–1371. doi: 10.1111/jcmm.12300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andersson J.K., Khan Z., Weaver A.L., Vaughan L.E., Gemzell-Danielsson K., Stewart E.A. Vaginal bromocriptine improves pain, menstrual bleeding and quality of life in women with adenomyosis: A pilot study. Acta Obstet. Gynecol. Scand. 2019;98:1341–1350. doi: 10.1111/aogs.13632. [DOI] [PubMed] [Google Scholar]
- 83.Singtripop T., Mori T., Park M.K., Sakamoto S., Kawashima S. Development of uterine adenomyosis after treatment with dopamine antagonists in mice. Life Sci. 1991;49:201–206. doi: 10.1016/0024-3205(91)90004-U. [DOI] [PubMed] [Google Scholar]
- 84.Yamashita M., Matsuda M., Mori T. Increased expression of prolactin receptor mRNA in adenomyotic uterus in mice. Life Sci. 1997;60:1437–1446. doi: 10.1016/S0024-3205(96)00649-2. [DOI] [PubMed] [Google Scholar]
- 85.Mori T., Singtripop T., Kawashima S. Animal model of uterine adenomyosis: Is prolactin a potent inducer of adenomyosis in mice? Am. J. Obstet. Gynecol. 1991;165:232–234. doi: 10.1016/0002-9378(91)90258-S. [DOI] [PubMed] [Google Scholar]
- 86.Takemura M., Nomura S., Kimura T., Inoue T., Onoue H., Azuma C., Saji F., Kitamura Y., Tanizawa O. Expression and localization of oxytocin receptor gene in human uterine endometrium in relation to the menstrual cycle. Endocrinology. 1993;132:1830–1835. doi: 10.1210/endo.132.4.8384999. [DOI] [PubMed] [Google Scholar]
- 87.Guo S.W., Mao X., Ma Q., Liu X. Dysmenorrhea and its severity are associated with increased uterine contractility and overexpression of oxytocin receptor (OTR) in women with symptomatic adenomyosis. Fertil. Steril. 2013;99:231–240. doi: 10.1016/j.fertnstert.2012.08.038. [DOI] [PubMed] [Google Scholar]
- 88.Newbold R.R., Jefferson W.N., Padilla-Banks E. Long-term adverse effects of neonatal exposure to bisphenol A on the murine female reproductive tract. Reprod. Toxicol. 2007;24:253–258. doi: 10.1016/j.reprotox.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bennett L.M., McAllister K.A., Malphurs J., Ward T., Collins N.K., Seely J.C., Gowen L.C., Koller B.H., Davis B.J., Wiseman R.W. Mice heterozygous for a Brca1 or Brca2 mutation display distinct mammary gland and ovarian phenotypes in response to diethylstilbestrol. Cancer Res. 2000;60:3461–3469. [PubMed] [Google Scholar]
- 90.Huang P.C., Tsai E.M., Li W.F., Liao P.C., Chung M.C., Wang Y.H., Wang S.L. Association between phthalate exposure and glutathione S-transferase M1 polymorphism in adenomyosis, leiomyoma and endometriosis. Hum. Reprod. 2010;25:986–994. doi: 10.1093/humrep/deq015. [DOI] [PubMed] [Google Scholar]
- 91.Valdes-Bango M., Gracia M., Rubio E., Vergara A., Casals-Pascual C., Ros C., Rius M., Martinez-Zamora M.A., Mension E., Quintas L., et al. Comparative analysis of endometrial, vaginal, and gut microbiota in patients with and without adenomyosis. Acta Obstet. Gynecol. Scand. 2024;103:1271–1282. doi: 10.1111/aogs.14847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Younes G., Tulandi T. Effects of adenomyosis on in vitro fertilization treatment outcomes: A meta-analysis. Fertil. Steril. 2017;108:483–490.e3. doi: 10.1016/j.fertnstert.2017.06.025. [DOI] [PubMed] [Google Scholar]
- 93.Campo S., Campo V., Benagiano G. Adenomyosis and infertility. Reprod. Biomed. Online. 2012;24:35–46. doi: 10.1016/j.rbmo.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 94.Horton J., Sterrenburg M., Lane S., Maheshwari A., Li T.C., Cheong Y. Reproductive, obstetric, and perinatal outcomes of women with adenomyosis and endometriosis: A systematic review and meta-analysis. Hum. Reprod. Update. 2019;25:592–632. doi: 10.1093/humupd/dmz012. [DOI] [PubMed] [Google Scholar]
- 95.Liu L., Trimarchi J.R., Navarro P., Blasco M.A., Keefe D.L. Oxidative stress contributes to arsenic-induced telomere attrition, chromosome instability, and apoptosis. J. Biol. Chem. 2003;278:31998–32004. doi: 10.1074/jbc.M303553200. [DOI] [PubMed] [Google Scholar]
- 96.De Santis L., Cino I., Rabellotti E., Calzi F., Persico P., Borini A., Coticchio G. Polar body morphology and spindle imaging as predictors of oocyte quality. Reprod. Biomed. Online. 2005;11:36–42. doi: 10.1016/S1472-6483(10)61296-5. [DOI] [PubMed] [Google Scholar]
- 97.Juneau C., Kraus E., Werner M., Franasiak J., Morin S., Patounakis G., Molinaro T., de Ziegler D., Scott R.T. Patients with endometriosis have aneuploidy rates equivalent to their age-matched peers in the in vitro fertilization population. Fertil. Steril. 2017;108:284–288. doi: 10.1016/j.fertnstert.2017.05.038. [DOI] [PubMed] [Google Scholar]
- 98.Harada T., Khine Y.M., Kaponis A., Nikellis T., Decavalas G., Taniguchi F. The Impact of Adenomyosis on Women’s Fertility. Obstet. Gynecol. Surv. 2016;71:557–568. doi: 10.1097/OGX.0000000000000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Achache H., Revel A. Endometrial receptivity markers, the journey to successful embryo implantation. Hum. Reprod. Update. 2006;12:731–746. doi: 10.1093/humupd/dml004. [DOI] [PubMed] [Google Scholar]
- 100.Fischer C.P., Kayisili U., Taylor H.S. HOXA10 expression is decreased in endometrium of women with adenomyosis. Fertil. Steril. 2011;95:1133–1136. doi: 10.1016/j.fertnstert.2010.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang J., Huang C., Jiang R., Du Y., Zhou J., Jiang Y., Yan Q., Xing J., Hou X., Zhou J., et al. Decreased Endometrial IL-10 Impairs Endometrial Receptivity by Downregulating HOXA10 Expression in Women with Adenomyosis. Biomed. Res. Int. 2018;2018:2549789. doi: 10.1155/2018/2549789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yen C.F., Liao S.K., Huang S.J., Tabak S., Arcuri F., Lee C.L., Arici A., Petraglia F., Wang H.S., Kayisli U.A. Decreased Endometrial Expression of Leukemia Inhibitory Factor Receptor Disrupts the STAT3 Signaling in Adenomyosis During the Implantation Window. Reprod. Sci. 2017;24:1176–1186. doi: 10.1177/1933719116681515. [DOI] [PubMed] [Google Scholar]
- 103.Jiang Y., Jiang R., Cheng X., Zhang Q., Hu Y., Zhang H., Cao Y., Zhang M., Wang J., Ding L., et al. Decreased expression of NR4A nuclear receptors in adenomyosis impairs endometrial decidualization. Mol. Hum. Reprod. 2016;22:655–668. doi: 10.1093/molehr/gaw042. [DOI] [PubMed] [Google Scholar]
- 104.Nie J., Lu Y., Liu X., Guo S.W. Immunoreactivity of progesterone receptor isoform B, nuclear factor kappaB, and IkappaBalpha in adenomyosis. Fertil. Steril. 2009;92:886–889. doi: 10.1016/j.fertnstert.2009.01.084. [DOI] [PubMed] [Google Scholar]
- 105.Xiao Y., Li T., Xia E., Yang X., Sun X., Zhou Y. Expression of integrin beta3 and osteopontin in the eutopic endometrium of adenomyosis during the implantation window. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013;170:419–422. doi: 10.1016/j.ejogrb.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 106.Kim K.H., Kim H.Y., Kim H.H., Lee K.S., Cheong J. Hypoxia induces expression of COX-2 through the homeodomain transcription factor CDX1 and orphan nuclear receptor SHP in human endometrial cells. Mol. Hum. Reprod. 2011;17:710–719. doi: 10.1093/molehr/gar036. [DOI] [PubMed] [Google Scholar]
- 107.Khan K.N., Fujishita A., Suematsu T., Ogawa K., Koshiba A., Mori T., Itoh K., Teramukai S., Matsuda K., Nakashima M., et al. An axonemal alteration in apical endometria of human adenomyosis. Hum. Reprod. 2021;36:1574–1589. doi: 10.1093/humrep/deab090. [DOI] [PubMed] [Google Scholar]
- 108.Khan K.N., Fujishita A., Ogawa K., Koshiba A., Mori T., Itoh K., Nakashima M., Kitawaki J. Occurrence of chronic endometritis in different types of human adenomyosis. Reprod. Med. Biol. 2022;21:e12421. doi: 10.1002/rmb2.12421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kitaya K., Matsubayashi H., Yamaguchi K., Nishiyama R., Takaya Y., Ishikawa T., Yasuo T., Yamada H. Chronic Endometritis: Potential Cause of Infertility and Obstetric and Neonatal Complications. Am. J. Reprod. Immunol. 2016;75:13–22. doi: 10.1111/aji.12438. [DOI] [PubMed] [Google Scholar]
- 110.Tremellen K.P., Russell P. The distribution of immune cells and macrophages in the endometrium of women with recurrent reproductive failure. II: Adenomyosis and macrophages. J. Reprod. Immunol. 2012;93:58–63. doi: 10.1016/j.jri.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 111.Wang C., Umesaki N., Nakamura H., Tanaka T., Nakatani K., Sakaguchi I., Ogita S., Kaneda K. Expression of vascular endothelial growth factor by granulated metrial gland cells in pregnant murine uteri. Cell Tissue Res. 2000;300:285–293. doi: 10.1007/s004410000198. [DOI] [PubMed] [Google Scholar]
- 112.Vallve-Juanico J., Houshdaran S., Giudice L.C. The endometrial immune environment of women with endometriosis. Hum. Reprod. Update. 2019;25:564–591. doi: 10.1093/humupd/dmz018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sugiura-Ogasawara M., Ebara T., Matsuki T., Yamada Y., Omori T., Matsumoto Y., Kato S., Kano H., Kurihara T., Saitoh S., et al. Endometriosis and Recurrent Pregnancy Loss as New Risk Factors for Venous Thromboembolism during Pregnancy and Post-Partum: The JECS Birth Cohort. Thromb. Haemost. 2019;119:606–617. doi: 10.1055/s-0039-1677733. [DOI] [PubMed] [Google Scholar]
- 114.Vannuccini S., Clifton V.L., Fraser I.S., Taylor H.S., Critchley H., Giudice L.C., Petraglia F. Infertility and reproductive disorders: Impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum. Reprod. Update. 2016;22:104–115. doi: 10.1093/humupd/dmv044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhihong N., Yun F., Pinggui Z., Sulian Z., Zhang A. Cytokine Profiling in the Eutopic Endometrium of Adenomyosis During the Implantation Window After Ovarian Stimulation. Reprod. Sci. 2016;23:124–133. doi: 10.1177/1933719115597761. [DOI] [PubMed] [Google Scholar]
- 116.MM I.J., Evers J.L., Dunselman G.A., Volovics L., Hoogland H.J. Relation between endometrial wavelike activity and fecundability in spontaneous cycles. Fertil. Steril. 1997;67:492–496. doi: 10.1016/s0015-0282(97)80075-1. [DOI] [PubMed] [Google Scholar]
- 117.Zhu L., Che H.S., Xiao L., Li Y.P. Uterine peristalsis before embryo transfer affects the chance of clinical pregnancy in fresh and frozen-thawed embryo transfer cycles. Hum. Reprod. 2014;29:1238–1243. doi: 10.1093/humrep/deu058. [DOI] [PubMed] [Google Scholar]
- 118.Mehasseb M.K., Bell S.C., Pringle J.H., Habiba M.A. Uterine adenomyosis is associated with ultrastructural features of altered contractility in the inner myometrium. Fertil. Steril. 2010;93:2130–2136. doi: 10.1016/j.fertnstert.2009.01.097. [DOI] [PubMed] [Google Scholar]
- 119.Pirtea P., Cicinelli E., De Nola R., de Ziegler D., Ayoubi J.M. Endometrial causes of recurrent pregnancy losses: Endometriosis, adenomyosis, and chronic endometritis. Fertil. Steril. 2021;115:546–560. doi: 10.1016/j.fertnstert.2020.12.010. [DOI] [PubMed] [Google Scholar]
- 120.Pados G., Gordts S., Sorrentino F., Nisolle M., Nappi L., Daniilidis A. Adenomyosis and Infertility: A Literature Review. Medicina. 2023;59:1551. doi: 10.3390/medicina59091551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Park C.W., Choi M.H., Yang K.M., Song I.O. Pregnancy rate in women with adenomyosis undergoing fresh or frozen embryo transfer cycles following gonadotropin-releasing hormone agonist treatment. Clin. Exp. Reprod. Med. 2016;43:169–173. doi: 10.5653/cerm.2016.43.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Niu Z., Chen Q., Sun Y., Feng Y. Long-term pituitary downregulation before frozen embryo transfer could improve pregnancy outcomes in women with adenomyosis. Gynecol. Endocrinol. 2013;29:1026–1030. doi: 10.3109/09513590.2013.824960. [DOI] [PubMed] [Google Scholar]
- 123.Vercellini P., Consonni D., Dridi D., Bracco B., Frattaruolo M.P., Somigliana E. Uterine adenomyosis and in vitro fertilization outcome: A systematic review and meta-analysis. Hum. Reprod. 2014;29:964–977. doi: 10.1093/humrep/deu041. [DOI] [PubMed] [Google Scholar]
- 124.Nirgianakis K., Kalaitzopoulos D.R., Schwartz A.S.K., Spaanderman M., Kramer B.W., Mueller M.D., Mueller M. Fertility, pregnancy and neonatal outcomes of patients with adenomyosis: A systematic review and meta-analysis. Reprod. Biomed. Online. 2021;42:185–206. doi: 10.1016/j.rbmo.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 125.Wu H.M., Chang H.M., Leung P.C.K. Gonadotropin-releasing hormone analogs: Mechanisms of action and clinical applications in female reproduction. Front. Neuroendocrinol. 2021;60:100876. doi: 10.1016/j.yfrne.2020.100876. [DOI] [PubMed] [Google Scholar]
- 126.Rocha T.P., Andres M.P., Borrelli G.M., Abrao M.S. Fertility-Sparing Treatment of Adenomyosis in Patients With Infertility: A Systematic Review of Current Options. Reprod. Sci. 2018;25:480–486. doi: 10.1177/1933719118756754. [DOI] [PubMed] [Google Scholar]
- 127.Hou X., Xing J., Shan H., Mei J., Sun Y., Yan G., Sun H., Wang J. The effect of adenomyosis on IVF after long or ultra-long GnRH agonist treatment. Reprod. Biomed. Online. 2020;41:845–853. doi: 10.1016/j.rbmo.2020.07.027. [DOI] [PubMed] [Google Scholar]
- 128.Lan J., Wu Y., Wu Z., Wu Y., Yang R., Liu Y., Lin H., Jiao X., Zhang Q. Ultra-Long GnRH Agonist Protocol During IVF/ICSI Improves Pregnancy Outcomes in Women With Adenomyosis: A Retrospective Cohort Study. Front Endocrinol (Lausanne) 2021;12:609771. doi: 10.3389/fendo.2021.609771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ge L., Li Y., Guan S., Cui L., Chen Z.J. Effects of ovarian stimulation protocols on outcomes of assisted reproductive technology in adenomyosis women: A retrospective cohort study. Front. Endocrinol. 2023;14:1198779. doi: 10.3389/fendo.2023.1198779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wu Y., Huang J., Zhong G., Lan J., Lin H., Zhang Q. Long-term GnRH agonist pretreatment before frozen embryo transfer improves pregnancy outcomes in women with adenomyosis. Reprod. Biomed. Online. 2022;44:380–388. doi: 10.1016/j.rbmo.2021.10.014. [DOI] [PubMed] [Google Scholar]
- 131.Liang Z., Yin M., Ma M., Wang Y., Kuang Y. Effect of pretreatment with a levonorgestrel-releasing intrauterine system on IVF and vitrified-warmed embryo transfer outcomes in women with adenomyosis. Reprod. Biomed. Online. 2019;39:111–118. doi: 10.1016/j.rbmo.2019.03.101. [DOI] [PubMed] [Google Scholar]
- 132.Chen M., Luo L., Wang Q., Gao J., Chen Y., Zhang Y., Zhou C. Impact of Gonadotropin-Releasing Hormone Agonist Pre-treatment on the Cumulative Live Birth Rate in Infertile Women With Adenomyosis Treated With IVF/ICSI: A Retrospective Cohort Study. Front. Endocrinol. 2020;11:318. doi: 10.3389/fendo.2020.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Li M., Xu L., Zhao H., Du Y., Yan L. Effects of artificial cycles with and without gonadotropin-releasing hormone agonist pretreatment on frozen embryo transfer outcomes in patients with adenomyosis. Sci. Rep. 2021;11:19326. doi: 10.1038/s41598-021-98918-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhang W., Han B., Ma C., Qiao J. Effect of GnRH-a pretreatment before frozen-thawed embryo transfer on pregnancy outcome of adenomyosis-associated infertile patients with 56 cm3 ≤ uterine volume ≤ 100 cm3. Ann. Transl. Med. 2022;10:509. doi: 10.21037/atm-21-6247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Feng M., Chen L.H., Hsu L.T., Wu H.M. Segmented in vitro fertilization and frozen embryo transfer in dienogest-treated patient with adenomyosis: A case report and lierature review. Taiwan. J. Obstet. Gynecol. 2022;61:906–908. doi: 10.1016/j.tjog.2021.09.037. [DOI] [PubMed] [Google Scholar]
- 136.Yang J., Wen Y., Li D., Hou X., Peng B., Wang Z. Retrospective analysis of the endometrial preparation protocols for frozen-thawed embryo transfer cycles in women with endometriosis. Reprod. Biol. Endocrinol. 2023;21:83. doi: 10.1186/s12958-023-01132-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li Y., Ge L., Yang X., Cui L., Chen Z.J. Effects of duration of long-acting GnRH agonist downregulation on assisted reproductive technology outcomes in patients with adenomyosis: A retrospective cohort study. Front. Med. 2023;10:1248274. doi: 10.3389/fmed.2023.1248274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Li X., Lin J., Zhang L., Liu Y. Effects of gonadotropin-releasing hormone agonist pretreatment on frozen embryo transfer outcomes in artificial cycles: A meta-analysis. Arch. Gynecol. Obstet. 2023;308:675–683. doi: 10.1007/s00404-022-06823-7. [DOI] [PubMed] [Google Scholar]
- 139.Bourdon M., Santulli P., Maignien C., Gayet V., Pocate-Cheriet K., Marcellin L., Chapron C. The deferred embryo transfer strategy improves cumulative pregnancy rates in endometriosis-related infertility: A retrospective matched cohort study. PLoS ONE. 2018;13:e0194800. doi: 10.1371/journal.pone.0194800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Maignien C., Santulli P., Gayet V., Lafay-Pillet M.C., Korb D., Bourdon M., Marcellin L., de Ziegler D., Chapron C. Prognostic factors for assisted reproductive technology in women with endometriosis-related infertility. Am. J. Obstet. Gynecol. 2017;216:280.e1–280.e9. doi: 10.1016/j.ajog.2016.11.1042. [DOI] [PubMed] [Google Scholar]
- 141.Meng F., Goldsammler M., Wantman E., Buyuk E., Jindal S.K. Live birth rate from euploid blastocysts is not associated with infertility etiology or oocyte source following frozen-thawed embryo transfer (FET): Analysis of 4148 cycles reported to SART CORS. J Assist Reprod Genet. 2021;38:185–192. doi: 10.1007/s10815-020-01996-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Pirtea P., De Ziegler D., Tao X., Sun L., Zhan Y., Ayoubi J.M., Seli E., Franasiak J.M., Scott R.T., Jr. Rate of true recurrent implantation failure is low: Results of three successive frozen euploid single embryo transfers. Fertil. Steril. 2021;115:45–53. doi: 10.1016/j.fertnstert.2020.07.002. [DOI] [PubMed] [Google Scholar]
- 143.Pirtea P., de Ziegler D., Ayoubi J.M. Effects of endometriosis on assisted reproductive technology: Gone with the wind. Fertil. Steril. 2021;115:321–322. doi: 10.1016/j.fertnstert.2020.08.1431. [DOI] [PubMed] [Google Scholar]
- 144.Khan K.N., Kitajima M., Hiraki K., Fujishita A., Sekine I., Ishimaru T., Masuzaki H. Changes in tissue inflammation, angiogenesis and apoptosis in endometriosis, adenomyosis and uterine myoma after GnRH agonist therapy. Hum. Reprod. 2010;25:642–653. doi: 10.1093/humrep/dep437. [DOI] [PubMed] [Google Scholar]
- 145.Tian J., Kang N., Wang J., Sun H., Yan G., Huang C., Mei J. Transcriptome analysis of eutopic endometrium in adenomyosis after GnRH agonist treatment. Reprod. Biol. Endocrinol. 2022;20:13. doi: 10.1186/s12958-021-00881-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li X., Pan N., Zhang W., Wang Y., Ge Y., Wei H., Lin Y., Ma C. Association between uterine volume and pregnancy outcomes in adenomyosis patients undergoing frozen-thawed embryo transfer. Reprod. Biomed. Online. 2021;42:384–389. doi: 10.1016/j.rbmo.2020.10.002. [DOI] [PubMed] [Google Scholar]
- 147.He Y., Wu H., He X., Xing Q., Zhou P., Cao Y., Wei Z. Administration of atosiban in patients with endometriosis undergoing frozen-thawed embryo transfer: A prospective, randomized study. Fertil. Steril. 2016;106:416–422. doi: 10.1016/j.fertnstert.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 148.Leyendecker G., Kunz G., Wildt L., Beil D., Deininger H. Uterine hyperperistalsis and dysperistalsis as dysfunctions of the mechanism of rapid sperm transport in patients with endometriosis and infertility. Hum. Reprod. 1996;11:1542–1551. doi: 10.1093/oxfordjournals.humrep.a019435. [DOI] [PubMed] [Google Scholar]
- 149.Moawad G., Youssef Y., Fruscalzo A., Faysal H., Kheil M., Pirtea P., Guani B., Ayoubi J.M., Feki A. The Present and the Future of Medical Therapies for Adenomyosis: A Narrative Review. J. Clin. Med. 2023;12:6130. doi: 10.3390/jcm12196130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pierzynski P., Reinheimer T.M., Kuczynski W. Oxytocin antagonists may improve infertility treatment. Fertil. Steril. 2007;88:213.e19–213.e22. doi: 10.1016/j.fertnstert.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 151.Lin C.W., Wu M.H., Mau Y.L., Su P.F., Ou H.T. Effect of atosiban on in vitro fertilization pregnancy outcome among women with endometriosis in presence or absence of adenomyosis. Taiwan. J. Obstet. Gynecol. 2023;62:537–542. doi: 10.1016/j.tjog.2022.12.012. [DOI] [PubMed] [Google Scholar]
- 152.Grimbizis G.F., Mikos T., Tarlatzis B. Uterus-sparing operative treatment for adenomyosis. Fertil. Steril. 2014;101:472–487. doi: 10.1016/j.fertnstert.2013.10.025. [DOI] [PubMed] [Google Scholar]
- 153.Younes G., Tulandi T. Conservative Surgery for Adenomyosis and Results: A Systematic Review. J. Minim. Invasive Gynecol. 2018;25:265–276. doi: 10.1016/j.jmig.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 154.Tan J., Moriarty S., Taskin O., Allaire C., Williams C., Yong P., Bedaiwy M.A. Reproductive Outcomes after Fertility-Sparing Surgery for Focal and Diffuse Adenomyosis: A Systematic Review. J. Minim. Invasive Gynecol. 2018;25:608–621. doi: 10.1016/j.jmig.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 155.Jiang L., Han Y., Song Z., Li Y. Pregnancy Outcomes after Uterus-sparing Operative Treatment for Adenomyosis: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2023;30:543–554. doi: 10.1016/j.jmig.2023.03.015. [DOI] [PubMed] [Google Scholar]
- 156.Capezzuoli T., Toscano F., Ceccaroni M., Roviglione G., Stepniewska A., Fambrini M., Vannuccini S., Petraglia F. Conservative surgical treatment for adenomyosis: New options for looking beyond uterus removal. Best. Pract. Res. Clin. Obstet. Gynaecol. 2024;95:102507. doi: 10.1016/j.bpobgyn.2024.102507. [DOI] [PubMed] [Google Scholar]
- 157.Nishida M., Takano K., Arai Y., Ozone H., Ichikawa R. Conservative surgical management for diffuse uterine adenomyosis. Fertil. Steril. 2010;94:715–719. doi: 10.1016/j.fertnstert.2009.03.046. [DOI] [PubMed] [Google Scholar]
- 158.Osada H. Uterine adenomyosis and adenomyoma: The surgical approach. Fertil. Steril. 2018;109:406–417. doi: 10.1016/j.fertnstert.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 159.Otsubo Y., Nishida M., Arai Y., Ichikawa R., Taneichi A., Sakanaka M. Association of uterine wall thickness with pregnancy outcome following uterine-sparing surgery for diffuse uterine adenomyosis. Aust. N. Z. J. Obstet. Gynaecol. 2016;56:88–91. doi: 10.1111/ajo.12419. [DOI] [PubMed] [Google Scholar]
- 160.Chapron C., Vannuccini S., Santulli P., Abrao M.S., Carmona F., Fraser I.S., Gordts S., Guo S.W., Just P.A., Noel J.C., et al. Diagnosing adenomyosis: An integrated clinical and imaging approach. Hum. Reprod. Update. 2020;26:392–411. doi: 10.1093/humupd/dmz049. [DOI] [PubMed] [Google Scholar]
- 161.Van den Bosch T., de Bruijn A.M., de Leeuw R.A., Dueholm M., Exacoustos C., Valentin L., Bourne T., Timmerman D., Huirne J.A.F. Sonographic classification and reporting system for diagnosing adenomyosis. Ultrasound Obstet. Gynecol. 2019;53:576–582. doi: 10.1002/uog.19096. [DOI] [PubMed] [Google Scholar]
- 162.Wang X.L., Xu Z.W., Huang Y.Y., Lin S., Lyu G.R. Different subtypes of ultrasound-diagnosed adenomyosis and in vitro fertilization outcomes: A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2023;102:657–668. doi: 10.1111/aogs.14580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Mavrelos D., Holland T.K., O’Donovan O., Khalil M., Ploumpidis G., Jurkovic D., Khalaf Y. The impact of adenomyosis on the outcome of IVF-embryo transfer. Reprod. Biomed. Online. 2017;35:549–554. doi: 10.1016/j.rbmo.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 164.Bourdon M., Santulli P., Oliveira J., Marcellin L., Maignien C., Melka L., Bordonne C., Millisher A.E., Plu-Bureau G., Cormier J., et al. Focal adenomyosis is associated with primary infertility. Fertil. Steril. 2020;114:1271–1277. doi: 10.1016/j.fertnstert.2020.06.018. [DOI] [PubMed] [Google Scholar]
- 165.Shi J., Wu Y., Li X., Gu Z., Zhang C., Yan H., Dai Y., Leng J. Effects of localization of uterine adenomyosis on clinical features and pregnancy outcome. Sci. Rep. 2023;13:14714. doi: 10.1038/s41598-023-40816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wang Y., Yi Y.C., Guu H.F., Chen Y.F., Kung H.F., Chang J.C., Chen L.Y., Chuan S.T., Chen M.J. Impact of adenomyosis and endometriosis on IVF/ICSI pregnancy outcome in patients undergoing gonadotropin-releasing hormone agonist treatment and frozen embryo transfer. Sci. Rep. 2023;13:6741. doi: 10.1038/s41598-023-34045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Huang B.S., Seow K.M., Tsui K.H., Huang C.Y., Lu Y.F., Wang P.H. Fertility outcome of infertile women with adenomyosis treated with the combination of a conservative microsurgical technique and GnRH agonist: Long-term follow-up in a series of nine patients. Taiwan. J. Obstet. Gynecol. 2012;51:212–216. doi: 10.1016/j.tjog.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 168.Chang W.H., Wang K.C., Lee N.R., Huang N., Su W.H., Chao H.T., Yen M.S., Fuh J.L., Wang P.H. Reproductive performance of severely symptomatic women with uterine adenomyoma who wanted preservation of the uterus and underwent combined surgical-medical treatment. Taiwan. J. Obstet. Gynecol. 2013;52:39–45. doi: 10.1016/j.tjog.2013.01.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.