Abstract
A healthy diet prevents overweight problems and hypertension. We investigated the associations of a healthy diet with the body mass index (BMI) and blood pressure (BP) in early childhood. In the GECKO birth cohort, height, weight, and BP were measured at 5 and 10 years of age. Diet was evaluated at 3 years using three diet scores: the Dietary Approaches to Stop Hypertension (DASH), the Mediterranean Diet Score (MDS), and the Lifelines Diet Score (LLDS). Linear and logistic regression models assessed the associations of diet scores with the BMI and BP. Of the 1077 children included, 10.8% were overweight or obese at 5 years. That number was 16.5% at 10 years. In addition, 34.5% had elevated BP at 5 years. That number was 23.9% at 10 years. Higher DASH, MDS, and LLDS, which indicate healthier diets, were all associated with lower BMI z-scores at 10 years of age. Higher DASH is related to lower overweight risk at 10 years. None of the diet scores were associated with BP or elevated BP at either 5 or 10 years. Also, in an overweight subset, diet was not related to BP. A healthy diet in early childhood is related to children being less overweight but not having lower BP at 10 years of age.
Keywords: DASH, MDS, LLDS, childhood BP, childhood BMI
1. Introduction
Childhood hypertension and overweight problems are global public health issues leading to long-term cardiovascular risk [1]. The global prevalence in children and adolescents was 4.0% for hypertension [2], 9.7% for prehypertension [2], and 14.8% for overweight problems [3]. Although many cohort studies show that hypertension, being overweight, or an increasing BMI trajectory during childhood predicts adulthood hypertension and cardiovascular diseases (CVD) [4,5]; intervention studies from early childhood are limited. Lifestyle and dietary consultations were reported by several studies to slightly contribute to improved cardiovascular health beginning from childhood, but few studies directly proved that long-term intervention or treatment of cardiovascular risk factors in childhood reduces the future risk of cardiovascular events [5]. It suggests the importance of early childhood in view of primordial prevention of CVD, which warrants additional focus.
A healthy diet is recommended by guidelines to prevent or reverse hypertension in adults and children, but the impact of different dietary patterns in children needs more research [6,7]. The Dietary Approaches to Stop Hypertension (DASH) diet was designed to decrease blood pressure (BP) and was shown to be effective in adults [7,8,9,10,11]. The Mediterranean diet, first studied in Greece and Southern Italy during the 1960s, improves the overall cardiometabolic risk profile and is associated with lower BP in adults [9,10,12]. The Lifelines Diet Score (LLDS) is a recently established diet score representing a dietary pattern adhering to the 2015 Dutch Dietary Guidelines [13]. It discriminated well between people with widely different intakes [13]. Higher LLDS scores, reflecting a healthier diet, were associated with lower BP, lower metabolic risk, and lower all-cause mortality in adults [14,15].
The associations of DASH and the Mediterranean Diet Score (MDS) with blood pressure or hypertension in childhood are inconsistent across studies, while the association between LLDS and BP in childhood has not yet been investigated. DASH was associated with lower BP and a lower prevalence of hypertension by cross-sectional and longitudinal studies in children and adolescents—healthy or ill [16,17,18,19,20,21,22]. DASH is effective in short-term and long-term clinical trials for decreasing BP in adolescents 10 to 18 years of age [23,24,25]. However, absent or opposite associations between DASH and childhood BP are also reported by cross-sectional and longitudinal studies [26,27,28,29]. Similarly, associations of the MDS with BP and hypertension were inconsistent in children and adolescents, indicating beneficial (2 cross-sectional studies), non-beneficial (1 cross-sectional study), and non-significant (3 cross-sectional studies and 1 longitudinal study) associations [30,31,32,33,34,35]. In contrast, a more consistent benefit of the MDS on BP in childhood was found in short-term and long-term clinical trials [36,37]. So far, there is limited research on LLDS and BP. Although higher LLDS values were associated with lower BP in adults, the relation with BP in children and adolescents has not yet been studied.
Similarly, well-known risk factors for hypertension—the BMI, being overweight, and obesity—and their association with diets have been investigated in many studies [38]. DASH has been associated with lower levels of the BMI [22] and weight gain [39], as well as people being less overweight or obese [16,40] and metabolically unhealthy obesity [29] in children older than 5 years in cross-sectional and longitudinal studies. In contrast, a few studies reported no association between DASH and the BMI or weight gain [20,25,41,42]. Similarly, the MDS was associated with lower levels of the BMI [34,36] and BMI gain [43], as well as people being less overweight or obese [34,37,44] in cross-sectional, longitudinal, and intervention studies, with a few studies showing inconsistent results [35,41,42,45]. So far, the only study on the LLDS in children showed that a higher LLDS is associated with a lower 7-year increase (from 3 to 10 years) in weight gain [46]. Further associations between the LLDS and BMI/obesity at other ages in childhood have not been reported.
Despite the existence of a large volume of studies that have assessed the influence of dietary patterns on BP and the BMI ranging from middle childhood to puberty, studies investigating this question in preschoolers younger than 5 years are limited. To fill this knowledge gap, we conducted a study from early to middle childhood to investigate the following three questions: (1) Is poor diet quality at 3 years related to a higher BMI and being overweight or obese at 5 and 10 years of age? (2) Is a poor diet quality at 3 years related to higher blood pressure and hypertension at 5 and 10 years of age? (3) Does the BMI influence the association between diet and blood pressure, and if so, how? We hypothesized that poor diet quality at 3 years of age may increase BP level and hypertension risk at 5 and 10 years of age and that the association depends on the BMI.
2. Materials and Methods
2.1. Study Design and Population
The GECKO Drenthe cohort study is a birth cohort focusing on early risk factors for the development of obesity in children. This cohort follows two-thirds of the children born in 1 year during 2006–2007 in Drenthe, a northern province in the Netherlands [47]. The children and their parents have been followed up during regular visits to the Well Baby Clinics during the first 4 years of life and thereafter via the school health services at 5/6 and 10/11 years [47]. The inclusion and exclusion criteria in the present study are shown in the flowchart (Figure S1). Among the 2842 active participants with informed consent in the GECKO cohort, 1077 individuals were included in the final analyses. The results of the attrition analysis are in the footnote of Figure S1. The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Medical Ethics Committee of the University Medical Center Groningen. Written informed consent was obtained from parents. The cohort is registered at www.birthcohorts.net.
2.2. Outcomes
The main outcomes of interest were systolic blood pressure (SBP), diastolic blood pressure (DBP), elevated BP, BMI, and overweight issues.
BP at the age of 5–6 and 10–11 years was measured by trained preventive child healthcare nurses in 3 consecutive measurements with a digital automatic BP monitor (Omron M3 intellisense, OMRON Healthcare Co., Minato City, Japan). The child was sitting for 5 min before the BP was measured. The means of SBP and DBP were calculated from the 3 measurements and adjusted for cuff size where necessary. According to the 2017 Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents, elevated BP was defined as ≥the age-, height- and sex-specific 90th percentile (or 120/80, whichever was lower), while hypertension was defined as ≥the age-, height- and sex-specific 95th percentile (or 130/80 whichever was lower) [48].
Height and weight at the ages of 5–6 and 10–11 years were measured by trained preventive child healthcare nurses according to standardized protocols, as described previously [49], using electronic scales without shoes or heavy clothing. BMI (kg/m2) was calculated at 5 and 10 years of age. The age- and sex- standardized BMI z-score was calculated using Growth Analyser software 3.5 (Dutch Growth Research Foundation, Rotterdam, The Netherlands), with the 1997 Dutch Growth study as the reference population [50]. According to the Extended International Obesity Task Force (IOTF) Body Mass Index Cutoffs from 2012, overweight, including obesity, was defined as BMI z-scores above 1.310 SD for boys and 1.244 SD for girls, while obesity was defined as BMI z-scores above 2.288 SD for boys and above 2.192 SD for girls [51].
2.3. Determinants
Dietary data over the past 4 weeks were collected using a food frequency questionnaire (FFQ) specific for children at 3 years of age. The FFQ was developed according to the Dutch National Food Consumption Survey 1997–1998 [52]. The FFQ contained 71 food products, with frequency categories from “never” to “6–7 times a week”. The units of the amounts were portions or common household measures. Parents were asked to measure the volume of glasses and cups used for different beverages. Verified and validated FFQ data were processed to calculate the daily intake of each food product (amount in portions ×portion size × weighting value/sum of weighting values × correction factor ×frequency/7 = daily intake in grams per day), after which daily energy and nutrient intake were calculated based on the Dutch food composition database (NEVO) of 2011 [53] (daily intake in gram per day × the amounts of energy and nutrients for per unit of each food product). The reliability of reported dietary intake was assessed using the Goldberg cutoff method and relied on the ratio of reported energy intake and basal metabolic rate [54,55,56]. Children with an energy intake/basal metabolic rate ratio below 0.87 or above 2.75 (N = 91) were excluded to limit bias through under- or over-reporting [54]. For more details, refer to TNO report V8643: Food frequency questionnaire on energy intake of children 2–12 years old: Verification and calculation procedures.
The DASH score was calculated according to the European ALPHABET Consortium (for pregnant women) [57] and LifeCycle Data Harmonization Protocol 2018 (for pregnant women and children older than 5 years of age) [58], containing 8 food groups (Table S1). Daily intake of each food group and sodium was ranked into quintiles and given positive or reverse scores (from 0 to 4), summing up to a total score that ranged from 0 to 32.
The MDS was calculated according to the Identification and Prevention of Dietary- and Lifestyle-Induced Health Effects in Children and Infants Study (IDEFICS) (for children) [59], containing 7 food groups (Table S1). The daily intakes in grams/1000 kcal of each food group and the ratio of saturated to unsaturated fats were expressed as a dichotomous ranking including high adherence (1) and low adherence (0), summing up to a total score that ranged from 0 to 7. High adherence to MDS was defined as an MDS higher than 3.
The LLDS was calculated based on 29 systematic reviews regarding associations of diet with chronic diseases, which the Dutch Health Council evaluated in the process of the development of the 2015 Dutch dietary guidelines (for adults) [13]. The daily intake in grams/1000 kcal of 11 instead of 12 food groups, excluding coffee for children, were calculated from FFQ data and expressed in a quintile ranking of the sum of daily intakes of each product (valued as 0 to 4), summing up to a total score ranging from 0 to 44 (Table S1). A higher DASH score, MDS, or LLDS represents better diet quality.
2.4. Statistical Analyses
The associations of diet scores with continuous outcomes (SBP, BDP, BMI z-score) at 5 and 10 years were assessed using linear regressions and with dichotomous outcomes (elevated BP, overweight including obesity) at 5 and 10 years using logistic regressions. Diet scores were included in each model separately, both as continuous variables and categorical variables. As categorical determinants, DASH and LLDS were expressed in quintiles, with the highest quintile (best diet quality) as the reference level, while MDS was expressed as a dichotomy of high and low adherence. In the analyses, potential confounders were added to the crude model (model 1) in 3 steps (model 2, model 3, and model 4). In model 2, we adjusted for important basic covariates that affect outcome measurement, including age, sex, and height in the BP/elevated BP model and age and sex in the BMI/overweight model. In model 3, we additionally included socio-economic factors. To avoid overfitting, we only included one socio-economic factor with the largest coefficient based on the result of univariate models; these were maternal education level in the BP/elevated BP model and paternal education level in the BMI/overweight model. In model 4, we included any smoking during pregnancy, a common risk factor that may affect our outcomes based on existing evidence [60,61]. All tests were 2-sided, and p < 0.05 was used as the cutoff for statistical significance. Analyses were conducted using R version 4.0.5 and IBM SPSS Statistics 28 (SPSS, Chicago, IL, USA).
For the first research question, we investigate the associations between diet scores at 3 years of age and the BMI/overweight problems, including obesity at 5 and 10 years of age. For the second research question, we investigate the associations between diet scores at 3 years of age and BP/elevated BP at 5 and 10 years of age. For the third research question, we investigated the association of BMI z-score with BP and the associations of diet scores at 3 years of age with BP/elevated BP at 5 and 10 years of age only in children overweight including obesity at baseline (3 years of age). Considering the primary role of sodium in regulating BP and to avoid overestimated weight of sodium in the DASH pattern, we also investigated DASH without sodium instead of DASH as the determinant in the associations with BP/hypertension in sensitivity analyses.
3. Results
3.1. Demographic Characteristics
In total, a maximum of 1077 participants were included in the analysis (see flowchart Figure S1). Table 1 shows the characteristics of the study participants. Ages at outcome measurements were 5.83 (5.58, 6.00) and 10.58 (10.25, 10.83) years, and 48.7% of the participants were female.
Table 1.
Participant characteristics.
| General Characteristics | N = 1077 | |
|---|---|---|
| Sex (female), n (%) | 524 (48.7%) | |
| Age at food frequency questionnaire (years), median (IQR) | 3.08 (3.02, 3.16) | |
| Age at outcomes measurement 1 (years), median (IQR) | 5.83 (5.58, 6.00) | |
| Age at outcomes measurement 2 (years), median (IQR) | 10.58 (10.25, 10.83) | |
| Maternal education level within one year of birth, n (%) | High 423 (39.7%) | |
| Medium 357 (33.5%) | ||
| Low 285 (26.8%) | ||
| Paternal education level within one year of birth, n (%) | High 338 (32.4%) | |
| Medium 288 (27.6%) | ||
| Low 416 (39.9%) | ||
| Any smoking during pregnancy, n (%) | 118 (11.0%) | |
| Maternal history of hypertension, n (%) | 109 (10.3%) | |
| Maternal prepregnancy BMI (kg/m2), median (IQR) | 23.81 (21.61, 26.76) | |
| Determinants | N = 1077 | |
| DASH score at 3 years of age, median (IQR) | 16 (13, 19) | |
| MDS at 3 years of age, median (IQR) | 4 (3, 5) | |
| LLDS at 3 years of age, median (IQR) | 21 (17, 26) | |
| Outcomes | 5 years of age (N = 971) | 10 years of age (N = 959) |
| SBP (mm Hg), median (IQR) | 103.33 (98.00, 109.00) | 107.19 (101.86, 113.38) |
| DBP (mm Hg), median (IQR) | 61.67 (57.00, 66.33) | 63.50 (58.33, 68.00) |
| Elevated BP (including hypertension), n (%) | 293 (34.5%) | 217 (23.9%) |
| Hypertension, n (%) | 180 (21.2%) | 121 (13.3%) |
| BMI z-score (SD), median (IQR) | 0.21 (−0.31, 0.71) | 0.12 (−0.49, 0.91) |
| Overweight (including obesity), n (%) | 105 (10.8%) | 158 (16.5%) |
| Obesity, n (%) | 17 (1.8%) | 29 (3.0%) |
3.2. Diet Scores and BMI/Overweight Issues
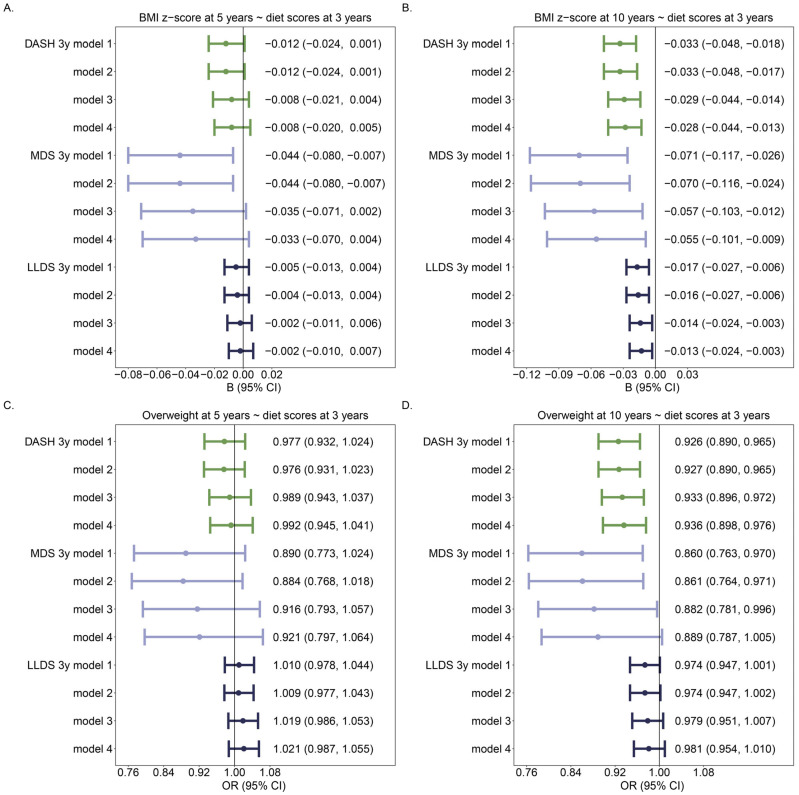
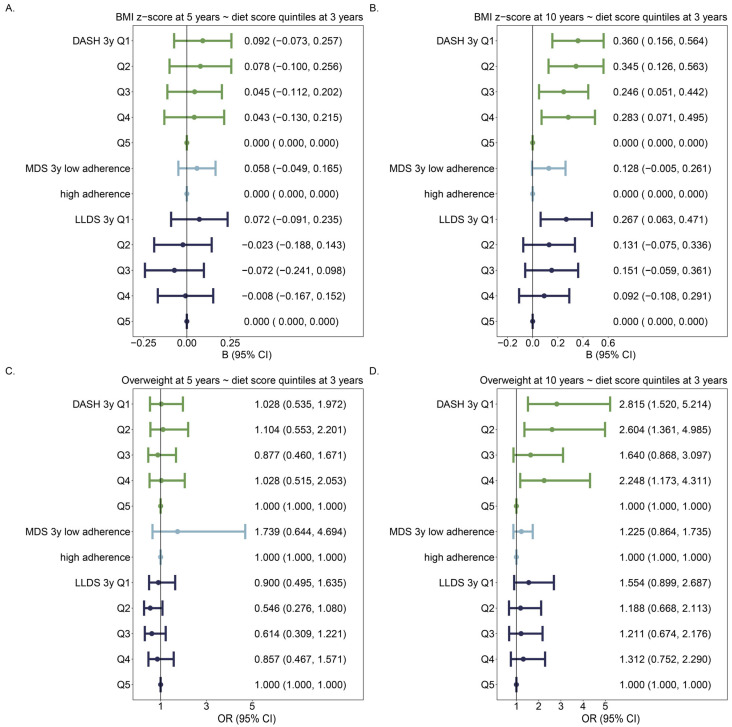
Overall, a better diet quality was related to a lower BMI and being less overweight or obese, mostly at 10 years of age (Figure 1B,D). An increase in any of the 3 diet scores on a continuous scale (DASH, MDS, and LLDS) at 3 years of age of 1 point was associated with a lower BMI z-score at 10 years of age (Figure 1B). In addition, an increase in DASH or MDS at 3 years of age was associated with lower overweight risk at 10 years of age (Figure 1D). However, when diet scores were assessed as categorical variables, the strongest associations were found for the DASH score (Figure 2).
Figure 1.
Associations of diet scores (per unit) are continuous with BMI z-score and overweight including obesity: (A) Association between diet scores at 3 years of age and BMI z-score at 5 years of age; (B) Association between diet scores at 3 years of age and BMI z-score at 10 years of age; (C) Association between diet scores at 3 years of age and overweight at 5 years of age; (D) Association between diet scores at 3 years of age and being overweight at 10 years of age. For each diet score, there were 4 models: Model 1: Crude model; Model 2: model 1 + age + sex; Model 3: model 2 + paternal education level; Model 4: model 3 + any smoking during pregnancy. The number of individuals was 971 in 5y models, and 959 in 10y models. Different colors identify different diet scores.
Figure 2.
Associations of diet scores in categories with BMI z-score and weight problems including obesity: (A–D) are the same as Figure 1. Diet scores are expressed as categorical variables in the models, with the best diet quality as the reference category. Associations of each category of diet scores are compared with that of the reference (best) category, adjusting for age, sex, paternal education level, and any smoking during pregnancy. The number of individuals was 971 in 5y models and 959 in 10y models. Different colors identify different diet scores.
Sensitivity analyses showed that DASH without sodium was not associated with BMI z-score at 5 years of age [B and 95%CI, model 4: −0.002 (−0.014, 0.010)], whereas the sodium score [median and range were 2 (0, 4), higher score represent lower sodium intake in mg per day] associated with lower BMI z-score at 5 years of age [B and 95%CI, model 4: −0.049 (−0.086, −0.012)]. Both DASH without sodium and isolated sodium score were associated with lower BMI z-score at 10 years of age [model 4 of DASH without sodium: B and 95%CI were −0.018 (−0.033, −0.002), model 4 of sodium score −0.056 (−0.104, −0.008)]. These results are consistent with our main analyses, which found that DASH was associated with a lower BMI z-score at 10 years but not at 5 years. It seems that sodium in DASH played a more important role than other food groups in the association of DASH on BMI z-score.
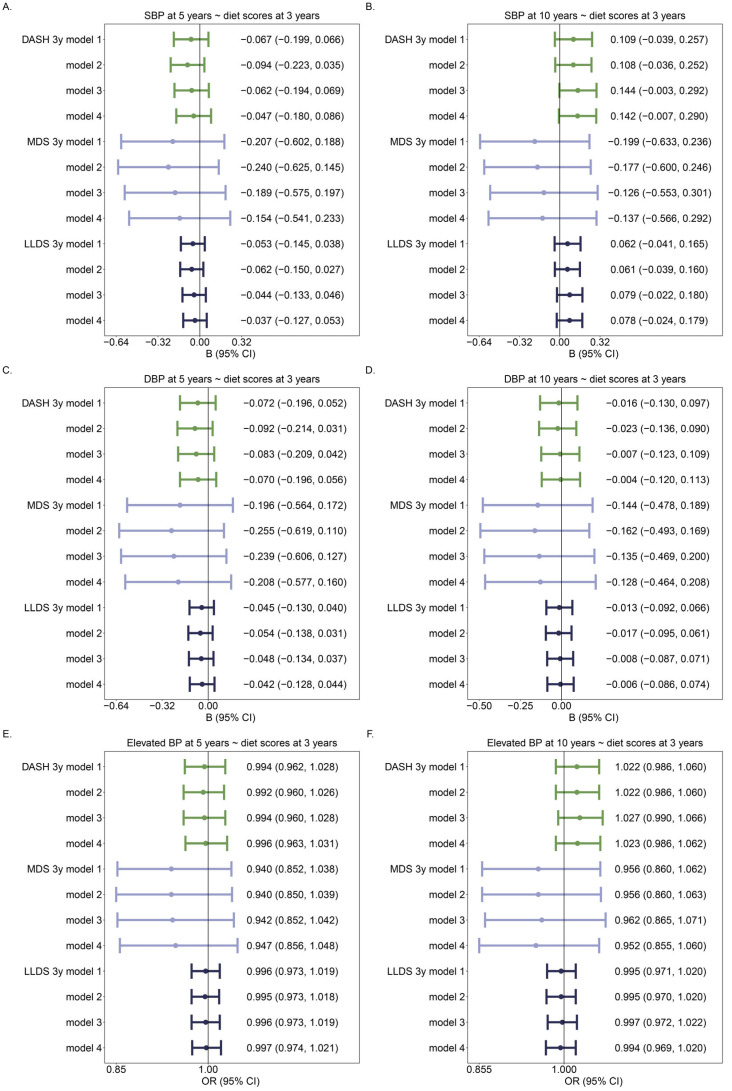
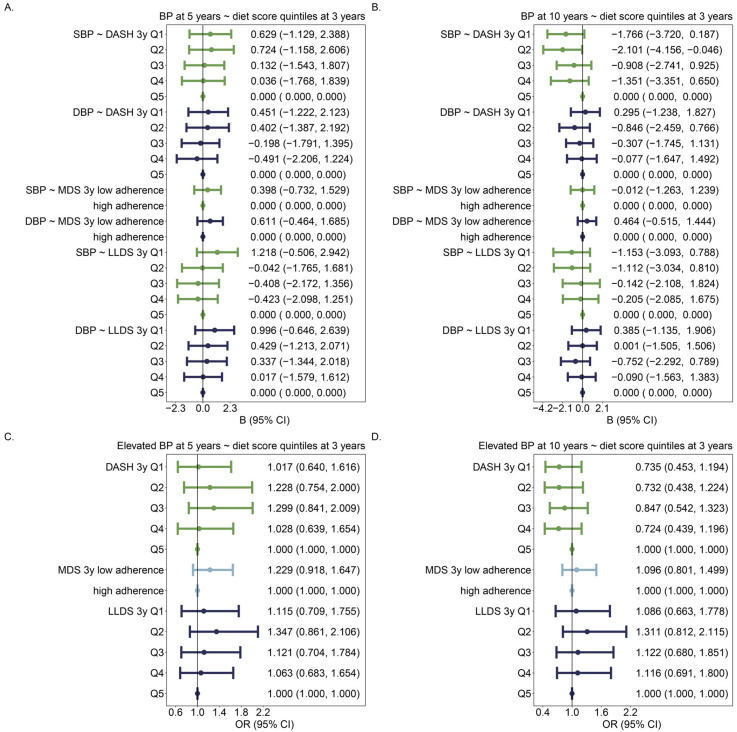
3.3. Diet Scores and BP/Elevated BP
As shown in Figure 3, none of the 3 diet scores were associated with SBP, DBP, or elevated BP at 5 or 10 years of age. Similarly, no significant associations were observed in quintiles of DASH or LLDS with BP or elevated BP at 5 or 10 years of age compared with the reference quintile, indicating the best diet quality, except the 2nd DASH quintile, indicating a relatively poor diet quality, which had a borderline significant association with lower SBP at 10 years of age (Figure 4). In the sensitivity analysis, neither DASH without sodium nor the isolated sodium score was associated with SBP or DBP at 5 or 10 years of age.
Figure 3.
Associations of diet scores (per unit) in continuous with BP and elevated BP: (A,C) Association between diet scores at 3 years of age and BP at 5 years of age; (B,D) Association between diet scores at 3 years of age and BP at 10 years of age; (E) Association between diet scores at 3 years of age and elevated BP at 5 years of age; (F) Association between diet scores at 3 years of age and elevated BP at 10 years of age. For each diet score, there were 4 models: Model 1: Crude model; Model 2: model 1 + age + sex + height; Model 3: model 2 + maternal education level; Model 4: model 3 + any smoking during pregnancy. The number of individuals was 857 in 5y models and 908 in 10y models. Different colors identify different diet scores.
Figure 4.
Associations of diet scores in categories with BP and elevated BP: (A) Association between diet scores at 3 years of age and BP at 5 years of age; (B) Association between diet scores at 3 years of age and BP at 10 years of age; (C) Association between diet scores at 3 years of age and elevated BP at 5 years of age; (D) Association between diet scores at 3 years of age and elevated BP at 10 years of age. Diet scores are expressed as categorical variables in the models, with the best diet quality as the reference category. Associations of each category of diet scores are compared with that of the reference (best) category, adjusting for age, sex, height, maternal education level, and any smoking during pregnancy. The number of individuals was 857 in 5y models and 908 in 10y models. Different colors identify SBP/DBP (A,B) or different diet scores (C,D).
3.4. Role of BMI in the Association between Diet Scores and BP
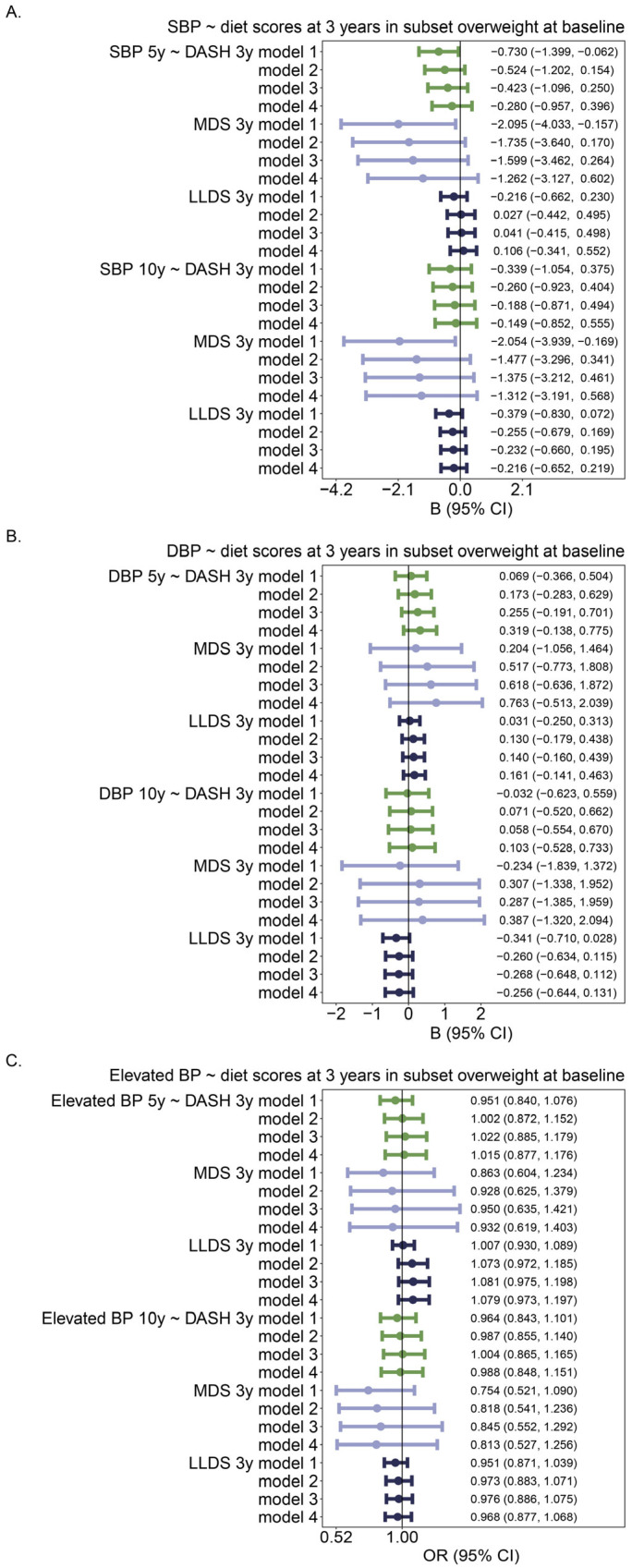
Since blood pressure was related to a higher BMI (in the model adjusted for age, sex, height, maternal education level, any smoking during pregnancy, BSBP~BMI = 2.092, BDBP~BMI = 1.513 at 5 years, and 1.479, 1.044 at 10 years, all p < 0.001), we hypothesized that diet may have more impact on blood pressure in children with a compromised metabolic profile, e.g., in children with overweight including obesity. Therefore, we related diet to BP outcomes in an overweight (including obesity) subset of all children. Figure 5 shows that the associations between diet scores and BP in the overweight subset were similar as in all children: in children who were overweight at baseline (3 years of age), DASH and MDS were associated with lower SBP at 5 years only in the crude model, whereas MDS associated with lower SBP at 10 years only in the crude model.
Figure 5.
Associations between diet score (per unit) and BP/elevated BP in children who were overweight or obese at baseline (3 years of age). The number of individuals was 62 in the 5y model and 65 in the 10y model. For each diet score, there were 4 models: Model 1: Crude model; Model 2: model 1 + age + sex + height; Model 3: model 2 + maternal education level; Model 4: model 3 + any smoking during pregnancy. (A). Association between diet scores at 3 years of age and SBP at 5 and 10 years of age. (B). Association between diet scores at 3 years of age and DBP at 5 and 10 years of age; (C). Association between diet scores at 3 years of age and elevated BP at 5 and 10 years of age. Different colors identify different diet scores.
4. Discussion
In the present study, we found that a healthy diet quality at 3 years of age relates to a lower BMI z-score and a lower risk of being overweight or obese but not to BP outcomes at 10 years of age. What is more, no association between diet quality and BP outcomes was found in a subset of children who are overweight or obese.
4.1. Diet Scores and BMI/Overweight Issues
We found associations of DASH and MDS with lower BMI z-score (and DASH also with fewer overweight issues) at 10 years of age. Previous longitudinal studies at similar ages showed both consistent [39] and inconsistent [41,42] results compared with the present study and reported no associations [35,41,42] more often than significant associations [43].
The association we found in the present study between a higher LLDS and a lower BMI z-score at 10 years of age is consistent with our previous study linking LLDS with a lower gain of weight and overweight incidence over a 7-year follow-up in childhood [46]. Our results indicated that a good diet quality at 3 years of age could benefit the BMI as shown over a 7-year follow-up in childhood. It could be explained by a sustained adherence to a healthy dietary pattern during childhood, based on the evidence that family diet and diet in early life were associated with diet at a later stage [62]. Alternatively, the dietary pattern at 3 years of age itself may have a long-term effect on the BMI z-score and on being overweight or obese at 10 years of age. The underlying mechanisms of dietary patterns as a whole decreasing BMI have not been well investigated, but the mechanisms may include reducing hunger, caloric restriction, and stimulation of dietary adherence [63]. Another thing that should be taken into consideration is that the prevalence of overweight or obese children in the present study was lower than that in European children in other studies, for example, 19.0% at preschool age in the ToyBox study [64]. One possible explanation is that the participants in the present study were children with normal birth outcomes, who were supposed to have a lower BMI z-score and overweight risk than children with poor birth outcomes. Sampling bias could explain the lower overweight prevalence at 10 years but not at 5 years in the present study because, according to our test, there was no sample bias at 5 years. So, we also suggested other explanations, including lower estimates due to the IOTF cutoffs.
In the present study, the associations of diet scores with the BMI z-score and with being overweight or obese were more significant at 10 years of age than at 5 years of age. One explanation might be that, for some individuals, the condition of being overweight was not yet developed at 5 years of age but was developed at 10 years of age. In addition, the childhood BMI has a curvilinear relation with age instead of a linear relation [51], leading to a relatively complex trajectory of associations.
Although the associations of diet scores, BMI z-scores, and being overweight or obese did not always show consistent trends from the 1st quintile to the 4th quintile, the 1st quintile indicating the poorest diet quality of DASH and LLDS was always the category with the strongest association with a higher BMI z-score and overweight incidence at 10 years of age. Overall, there is a convincing association between poor diet quality and being overweight.
4.2. Diet Scores and BP/Elevated BP
The lack of association between DASH and BP in the present study is consistent with several cross-sectional studies and longitudinal studies in children. Previous cross-sectional and longitudinal studies with a 4-year follow-up in children older than 6 years showed no benefit of DASH on BP, even though an association between DASH and cardiometabolic biomarkers had been observed [26,27]. However, observational studies with longer follow-ups, for example, 6-year [22] and > 10-year [19] follow-ups, found associations between DASH and lower BP. In line with this, associations between DASH and lower BP were found in intervention studies using either short-term (for example, 6-week [23] and 10-week [24]) or long-term follow-up (6 month [25]) in children with underlying diseases including metabolic syndrome [23], hemophilia [24], and elevated BP [25]. As for the association between MDS and BP, both significant [30,31] and absent [31,32,34] associations of MDS with lower BP or lower odds ratio of elevated BP in children were found in cross-sectional studies, with absences of associations being more predominant. A previous longitudinal study in adolescents of multiple ethnicities showed no association of MDS with BP [35], which is consistent with the present study. However, consistent associations were found in MDS intervention studies of 4 weeks [37] and 12 months [36]. To our knowledge, the present study is the first one to investigate the association of LLDS with BP in children. Although it is inconsistent with the study in adults showing that adherence to the highest tertile of LLDS is associated with lower SBP, the present study provides a novel perspective on this association in very early childhood.
One reason why diet quality was not related to BP outcomes in young children may be related to the mechanisms by which diet can affect blood pressure. Short-term effects may relate to a high intake of sodium, which increases BP, while a high intake of potassium [65], magnesium [66], and calcium [67] decreases BP both in the short- and long-term [68,69,70,71,72]. Short-term interventions of diet patterns decrease BP in adults and overweight children [73,74], but some of them are only effective in the short term but not in the long term [75,76]. It may be that we have not been able to detect a short-term effect of high salt intake because the day-to-day variation is high, and the FFQ captures dietary habits over the longer term. Long-term mechanisms include vascular remodeling and arterial stiffness, which take time to develop and may not occur yet in children, as opposed to elderly adults [77]. In that case, the 7-year follow-up in childhood in the present study is not long enough to observe the effects on the development of hypertension. To summarize, short-term effects of diet on decreasing BP are more often reported and more consistent than long-term effects [76,77]. Although we have not observed a long-term association (2-year or 7-year follow-up), there might be an unmeasured short-term association. Alternatively, changes in blood pressure may take a long time to manifest in response to dietary changes. On the other hand, the sampling methodology could partly account for variability in results and possible associations. To exclude prenatal factors as probable confounders relating to childhood BP in previous studies, we excluded children with premature birth or low birth weight. It made the present study focus on the major research questions but, at the same time, excluded possible associations of diet quality with BP through, or when interacting with, prenatal factors.
4.3. Role of BMI in Relationship between Diet and BP/Elevated BP
The association of the BMI with BP in the present study is in line with most previous studies, which found obese children were at higher risk of developing hypertension with multiple mechanisms potentially contributing, including activation of the renin–angiotensin–aldosterone system and the sympathetic nervous system, vascular dysfunction, other mineralocorticoid activity, and reduced kidney function [78,79]. However, we found no evidence of a stronger relationship between diet quality and BP in overweight children.
4.4. Strengths and Limitations
The present study has several strengths. First, our study has quite a long follow-up (from 3 years old to 10 years old), which is rare in previous studies in children. We investigated the associations of diet scores at 3 years with outcomes at both 5 years (preschoolers) and 10 years of age (middle childhood). Second, we highlight the significance of dietary analysis at the pattern level. Investigating diet quality as a whole instead of isolated nutrients is more important because the former is based on dietary recommendations and considers the imbalances among diet components. Third, 3 diet scores are investigated in the present study, supplying 3 different evaluation criteria of the diet quality of the same diet profile at the same time. In addition, the association of LLDS (a relatively newly established diet score) with BP in childhood has not been studied previously.
The limitations of the present study are as follows. First, the conclusion is not causal due to the observational design. Second, although many covariates have been included in our adjustments, residual confounding effects from unmeasured or unknown covariates cannot be completely ruled out. We have not adjusted physical activity in our models, but in a previous study in the same population, no association of early physical activity with BMI outcomes or BP outcomes was found [80]. We exclude individuals with adverse pregnancy outcomes at the start, so we have not included pregnancy outcomes as covariates. Third, the BP is the mean of three measurements in one visit instead of in separate visits; the same is true for the BMI measurements, so the definition of elevated BP/hypertension and overweight problems/obesity should be considered with caution as they are no clinical definitions. Fourth, only 1077 individuals who have normal birth outcomes among the whole cohort (N = 2842, including individuals with incomplete data, premature birth, or low birth weight) were included in the present study, which might have led to some bias.: The relationships between diet quality and BP or the BMI might be different for the participants with normal birth outcomes and the excluded participants who have poor birth outcomes. As a result, care should be taken when trying to extrapolate our results to other populations including participants with poor birth outcomes. Fifth, the MDS and LLDS calculations adapted to our population at a very young age, but the adaption to children of DASH should be taken into consideration. Although all three diet scores were based on an FFQ and a data process manual specific to children, the DASH calculation used food group criteria for pregnant women and school-aged children, with a daily intake in servings per day instead of adjusting for total energy intake. Differently, although the LLDS calculation was based on criteria for adults, we have excluded the coffee group in order to incorporate children’s diets, and the daily intake, which was adjusted for total energy intake, made up for the intake amount difference with adults. We suggested a further study assessing the accurate adaption of DASH to children younger than 5 years of age. Sixth, the FFQ data could have recall bias even though the data are validated. Under- or over-reporting has been excluded by the Goldberg cutoff method and relied on the ratio of reported energy intake and basal metabolic rate.
5. Conclusions
In conclusion, a better diet quality at 3 years of age relates to a lower BMI but not a lower BP at 10 years of age. These results were confirmed in overweight children and for elevated BP. Our findings suggest that a healthy diet in early childhood may prevent overweight problems in middle childhood, but the effect on BP needs further study with a longer follow-up.
Acknowledgments
This research is based on the GECKO (Groningen Expert Center for Kids With Obesity) Drenthe study. The authors are grateful to the families who took part in the GECKO Drenthe study, the midwives, gyneacologists, nurses, and the general practitioners and all health professionals at the Preventive Child Healthcare Drenthe for their help in the recruitment and the measurements, and the GECKO Drenthe study team.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/nu16162634/s1. Table S1: Food groups of the 3 diet scores; Figure S1: Flowchart detailing participant inclusion and exclusion.
Author Contributions
Q.W.: Formal analysis, Investigation, Methodology, Data curation, Writing—original draft, Writing—review and editing; T.X.: Writing—review and editing; X.H.: Writing—review and editing, Supervision; H.S.: Conceptualization, Validation, Writing—review and editing, Supervision, Resources, Project administration; E.C.: Conceptualization, Validation, Data curation, Writing—review and editing, Supervision, Resources, Project administration. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Medical Ethics Committee of the University Medical Center Groningen. Approval code: METc 2005/260. Approval date: 3rd April 2006.
Informed Consent Statement
Parents signed the informed consent form for all children included in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the Confidentiality Statement of Gecko Drenthe Cohort.
Conflicts of Interest
The authors declare no conflict of interest. The authors declare that the GECKO Drenthe birth cohort received funding from Hutchison Whampoa Ltd., Hong Kong. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Funding Statement
The GECKO Drenthe birth cohort was funded by an unrestricted grant of Hutchison Whampoa Ltd., Hong Kong and supported by the University of Groningen, Well Baby Clinic Foundation Icare, Noordlease, Paediatric Association Of The Netherlands, Youth Preventive Health Care Drenthe, the European Union’s Horizon 2020 research and innovation programme (LIFECYCLE, grant agreement No 733206, 2016), and Foundation Vrienden Beatrix Kinderziekenhuis, Groningen, The Netherlands. Qihua Wang was financially supported by a grant from the China Scholarship Council (file No. 202106780015). The funders had no role in study design, data collection and analysis, manuscript writing, or decision to publish.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Morton K., Heindl B., Clarkson S., Bittner V. Primordial Prevention of Atherosclerotic Cardiovascular Disease: A review of the literature. J. Cardiopulm. Rehabil. Prev. 2022;42:389–396. doi: 10.1097/HCR.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 2.Song P., Zhang Y., Yu J., Zha M., Zhu Y., Rahimi K., Rudan I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019;173:1154–1163. doi: 10.1001/jamapediatrics.2019.3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang X., Liu J., Ni Y., Yi C., Fang Y., Ning Q., Shen B., Zhang K., Liu Y., Yang L., et al. Global Prevalence of Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2024:e241576. doi: 10.1001/jamapediatrics.2024.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kibret K.T., Strugnell C., Backholer K., Peeters A., Tegegne T.K., Nichols M. Life-course trajectories of body mass index and cardiovascular disease risks and health outcomes in adulthood: Systematic review and meta-analysis. Obes. Rev. 2024;25:e13695. doi: 10.1111/obr.13695. [DOI] [PubMed] [Google Scholar]
- 5.Raitakari O., Pahkala K., Magnussen C.G. Prevention of atherosclerosis from childhood. Nat. Rev. Cardiol. 2022;19:543–554. doi: 10.1038/s41569-021-00647-9. [DOI] [PubMed] [Google Scholar]
- 6.Steinberger J., Daniels S.R., Hagberg N., Isasi C.R., Kelly A.S., Lloyd-Jones D., Pate R.R., Pratt C., Shay C.M., Towbin J.A., et al. Cardiovascular Health Promotion in Children: Challenges and Opportunities for 2020 and Beyond: A Scientific Statement From the American Heart Association. Circulation. 2016;134:e236–e255. doi: 10.1161/CIR.0000000000000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Appel L.J., Moore T.J., Obarzanek E., Vollmer W.M., Svetkey L.P., Sacks F.M., Bray G.A., Vogt T.M., Cutler J.A., Windhauser M.M., et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 8.Sacks F.M., Obarzanek E., Windhauser M.M., Svetkey L.P., Vollmer W.M., McCullough M., Karanja N., Lin P.H., Steele P., Proschan M.A., et al. Rationale and design of the Dietary Approaches to Stop Hypertension trial (DASH). A multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann. Epidemiol. 1995;5:108–118. doi: 10.1016/1047-2797(94)00055-X. [DOI] [PubMed] [Google Scholar]
- 9.Liang S., Mijatovic J., Li A., Koemel N., Nasir R., Toniutti C., Bell-Anderson K., Skilton M., O’Leary F. Dietary Patterns and Non-Communicable Disease Biomarkers: A Network Meta-Analysis and Nutritional Geometry Approach. Nutrients. 2022;15:76. doi: 10.3390/nu15010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowell O.R., Mistry N., Deighton K., Matu J., Griffiths A., Minihane A.M., Mathers J.C., Shannon O.M., Siervo M. Effects of a Mediterranean diet on blood pressure: A systematic review and meta-analysis of randomized controlled trials and observational studies. J. Hypertens. 2021;39:729–739. doi: 10.1097/HJH.0000000000002667. [DOI] [PubMed] [Google Scholar]
- 11.Filippou C.D., Tsioufis C.P., Thomopoulos C.G., Mihas C.C., Dimitriadis K.S., Sotiropoulou L.I., Chrysochoou C.A., Nihoyannopoulos P.I., Tousoulis D.M. Dietary Approaches to Stop Hypertension (DASH) Diet and Blood Pressure Reduction in Adults with and without Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2020;11:1150–1160. doi: 10.1093/advances/nmaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis C., Bryan J., Hodgson J., Murphy K. Definition of the Mediterranean Diet; a Literature Review. Nutrients. 2015;7:9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vinke P.C., Corpeleijn E., Dekker L.H., Jacobs D.R., Jr., Navis G., Kromhout D. Development of the food-based Lifelines Diet Score (LLDS) and its application in 129;369 Lifelines participants. Eur. J. Clin. Nutr. 2018;72:1111–1119. doi: 10.1038/s41430-018-0205-z. [DOI] [PubMed] [Google Scholar]
- 14.Khadem A., Shiraseb F., Mirzababaei A., Ghaffarian-Ensaf R., Mirzaei K. Association of Lifelines Diet Score (LLDS) and metabolically unhealthy overweight/obesity phenotypes in women: A cross-sectional study. BMC Womens Health. 2022;22:374. doi: 10.1186/s12905-022-01957-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vinke P.C., Navis G., Kromhout D., Corpeleijn E. Associations of Diet Quality and All-Cause Mortality across Levels of Cardiometabolic Health and Disease: A 7.6-Year Prospective Analysis from the Dutch Lifelines Cohort. Diabetes Care. 2021;44:1228–1235. doi: 10.2337/dc20-2709. [DOI] [PubMed] [Google Scholar]
- 16.Asghari G., Yuzbashian E., Mirmiran P., Hooshmand F., Najafi R., Azizi F. Dietary Approaches to Stop Hypertension (DASH) Dietary Pattern Is Associated with Reduced Incidence of Metabolic Syndrome in Children and Adolescents. J. Pediatr. 2016;174:178–184.e171. doi: 10.1016/j.jpeds.2016.03.077. [DOI] [PubMed] [Google Scholar]
- 17.Najafi A., Faghih S., Hojhabrimanesh A., Najafi M., Tangestani H., Atefi M., Teymouri M., Salehi M., Kamali M., Amanat S., et al. Greater adherence to the dietary approaches to stop hypertension (DASH) dietary pattern is associated with lower blood pressure in healthy Iranian primary school children. Eur. J. Nutr. 2018;57:1449–1458. doi: 10.1007/s00394-017-1423-1. [DOI] [PubMed] [Google Scholar]
- 18.Cohen J.F.W., Lehnerd M.E., Houser R.F., Rimm E.B. Dietary Approaches to Stop Hypertension Diet; Weight Status; and Blood Pressure among Children and Adolescents: National Health and Nutrition Examination Surveys 2003-2012. J. Acad. Nutr. Diet. 2017;117:1437–1444.e1432. doi: 10.1016/j.jand.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 19.Moore L.L., Bradlee M.L., Singer M.R., Qureshi M.M., Buendia J.R., Daniels S.R. Dietary Approaches to Stop Hypertension (DASH) eating pattern and risk of elevated blood pressure in adolescent girls. Br. J. Nutr. 2012;108:1678–1685. doi: 10.1017/S000711451100715X. [DOI] [PubMed] [Google Scholar]
- 20.Ducharme-Smith K., Caulfield L.E., Brady T.M., Rosenstock S., Mueller N.T., Garcia-Larsen V. Higher Diet Quality in African-American Adolescents Is Associated with Lower Odds of Metabolic Syndrome: Evidence from the NHANES. J. Nutr. 2021;151:1609–1617. doi: 10.1093/jn/nxab027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zafarmand M.H., Spanjer M., Nicolaou M., Wijnhoven H.A.H., van Schaik B.D.C., Uitterlinden A.G., Snieder H., Vrijkotte T.G.M. Influence of Dietary Approaches to Stop Hypertension-Type Diet; Known Genetic Variants and Their Interplay on Blood Pressure in Early Childhood: ABCD Study. Hypertension. 2020;75:59–70. doi: 10.1161/HYPERTENSIONAHA.118.12292. [DOI] [PubMed] [Google Scholar]
- 22.Krijger J.A., Nicolaou M., Nguyen A.N., Voortman T., Hutten B.A., Vrijkotte T.G. Diet quality at age 5-6 and cardiovascular outcomes in preadolescents. Clin. Nutr. ESPEN. 2021;43:506–513. doi: 10.1016/j.clnesp.2021.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Saneei P., Hashemipour M., Kelishadi R., Rajaei S., Esmaillzadeh A. Effects of recommendations to follow the Dietary Approaches to Stop Hypertension (DASH) diet v. usual dietary advice on childhood metabolic syndrome: A randomised cross-over clinical trial. Br. J. Nutr. 2013;110:2250–2259. doi: 10.1017/S0007114513001724. [DOI] [PubMed] [Google Scholar]
- 24.Mahdavi A., Mohammadi H., Foshati S., Shokri-Mashhadi N., Clark C.C.T., Moafi A., Rouhani M.H. Effects of the dietary approach to stop hypertension (DASH) diet on blood pressure; blood glucose; and lipid profile in adolescents with hemophilia: A randomized clinical trial. Food Sci. Nutr. 2021;9:145–153. doi: 10.1002/fsn3.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Couch S.C., Saelens B.E., Khoury P.R., Dart K.B., Hinn K., Mitsnefes M.M., Daniels S.R., Urbina E.M. Dietary Approaches to Stop Hypertension Dietary Intervention Improves Blood Pressure and Vascular Health in Youth With Elevated Blood Pressure. Hypertension. 2021;77:241–251. doi: 10.1161/HYPERTENSIONAHA.120.16156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aljahdali A.A., Peterson K.E., Cantoral A., Ruiz-Narvaez E., Tellez-Rojo M.M., Kim H.M., Hebert J.R., Wirth M.D., Torres-Olascoaga L.A., Shivappa N., et al. Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis. Nutrients. 2022;14:896. doi: 10.3390/nu14040896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eloranta A.M., Schwab U., Venalainen T., Kiiskinen S., Lakka H.M., Laaksonen D.E., Lakka T.A., Lindi V. Dietary quality indices in relation to cardiometabolic risk among Finnish children aged 6-8 years—The PANIC study. Nutr. Metab. Cardiovasc. Dis. 2016;26:833–841. doi: 10.1016/j.numecd.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Bricarello L.P., de Moura Souza A., de Almeida Alves M., Retondario A., Fernandes R., Santos de Moraes Trindade E.B., Zanette Ramos Zeni L.A., de Assis Guedes de Vasconcelos F. Association between DASH diet (Dietary Approaches to Stop Hypertension) and hypertension in adolescents: A cross-sectional school-based study. Clin. Nutr. ESPEN. 2020;36:69–75. doi: 10.1016/j.clnesp.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Rahimi H., Yuzbashian E., Zareie R., Asghari G., Djazayery A., Movahedi A., Mirmiran P. Dietary approaches to stop hypertension (DASH) score and obesity phenotypes in children and adolescents. Nutr. J. 2020;19:112. doi: 10.1186/s12937-020-00631-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mesas A.E., Jimenez-Lopez E., Martinez-Vizcaino V., Fernandez-Rodriguez R., Bizzozero-Peroni B., Garrido-Miguel M., Cavero-Redondo I., Lopez-Gil J.F. Are adherence to the Mediterranean diet and siesta individually or jointly associated with blood pressure in Spanish adolescents? Results from the EHDLA study. Front. Public Health. 2022;10:934854. doi: 10.3389/fpubh.2022.934854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garcia-Hermoso A., Vegas-Heredia E.D., Fernandez-Vergara O., Ceballos-Ceballos R., Andrade-Schnettler R., Arellano-Ruiz P., Ramirez-Velez R. Independent and combined effects of handgrip strength and adherence to a Mediterranean diet on blood pressure in Chilean children. Nutrition. 2019;60:170–174. doi: 10.1016/j.nut.2018.08.019. [DOI] [PubMed] [Google Scholar]
- 32.Cagiran Yilmaz F., Cagiran D., Ozcelik A.O. Adolescent Obesity and Its Association with Diet Quality and Cardiovascular Risk Factors. Ecol. Food Nutr. 2019;58:207–218. doi: 10.1080/03670244.2019.1580581. [DOI] [PubMed] [Google Scholar]
- 33.Agostinis-Sobrinho C., Santos R., Rosario R., Moreira C., Lopes L., Mota J., Martinkenas A., Garcia-Hermoso A., Correa-Bautista J.E., Ramirez-Velez R. Optimal Adherence to a Mediterranean Diet May Not Overcome the Deleterious Effects of Low Physical Fitness on Cardiovascular Disease Risk in Adolescents: A Cross-Sectional Pooled Analysis. Nutrients. 2018;10:815. doi: 10.3390/nu10070815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mistretta A., Marventano S., Antoci M., Cagnetti A., Giogianni G., Nolfo F., Rametta S., Pecora G., Marranzano M. Mediterranean diet adherence and body composition among Southern Italian adolescents. Obes. Res. Clin. Pract. 2017;11:215–226. doi: 10.1016/j.orcp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 35.Zhong V.W., Lamichhane A.P., Crandell J.L., Couch S.C., Liese A.D., The N.S., Tzeel B.A., Dabelea D., Lawrence J.M., Marcovina S.M., et al. Association of adherence to a Mediterranean diet with glycemic control and cardiovascular risk factors in youth with type I diabetes: The SEARCH Nutrition Ancillary Study. Eur. J. Clin. Nutr. 2016;70:802–807. doi: 10.1038/ejcn.2016.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cobos-Palacios L., Munoz-Ubeda M., Gallardo-Escribano C., Ruiz-Moreno M.I., Vilches-Perez A., Vargas-Candela A., Leiva-Gea I., Tinahones F.J., Gomez-Huelgas R., Bernal-Lopez M.R. Adipokines Profile and Inflammation Biomarkers in Prepubertal Population with Obesity and Healthy Metabolic State. Children. 2022;9:42. doi: 10.3390/children9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Macknin M., Stegmeier N., Thomas A., Worley S., Li L., Hazen S.L., Tang W.H.W. Three Healthy Eating Patterns and Cardiovascular Disease Risk Markers in 9 to 18 Year Olds With Body Mass Index >95%: A Randomized Trial. Clin. Pediatr. 2021;60:474–484. doi: 10.1177/00099228211044841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang X., Hu J., Huang S., Yang Z., Dong Y., Dong B., Ma J., Liang W. Exploring Overweight Risk Trajectories During Childhood and Their Associations With Elevated Blood Pressure at Late Adolescence: A Retrospective Cohort Study. Hypertension. 2022;79:1605–1613. doi: 10.1161/HYPERTENSIONAHA.121.18714. [DOI] [PubMed] [Google Scholar]
- 39.Berz J.P., Singer M.R., Guo X., Daniels S.R., Moore L.L. Use of a DASH food group score to predict excess weight gain in adolescent girls in the National Growth and Health Study. Arch. Pediatr. Adolesc. Med. 2011;165:540–546. doi: 10.1001/archpediatrics.2011.71. [DOI] [PubMed] [Google Scholar]
- 40.Golpour-Hamedani S., Mohammadifard N., Khosravi A., Feizi A., Safavi S.M. Dietary approaches to stop hypertension diet and obesity: A cross-sectional study of Iranian children and adolescents. ARYA Atheroscler. 2017;13:7–13. [PMC free article] [PubMed] [Google Scholar]
- 41.Bekelman T.A., Ringham B.M., Sauder K.A., Johnson S.L., Harrall K.H., Glueck D.H., Dabelea D. Adherence to index-based dietary patterns in childhood and BMI trajectory during the transition to adolescence: The EPOCH study. Int. J. Obes. 2021;45:2439–2446. doi: 10.1038/s41366-021-00917-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Monjardino T., Lucas R., Ramos E., Barros H. Associations between a priori-defined dietary patterns and longitudinal changes in bone mineral density in adolescents. Public Health Nutr. 2014;17:195–205. doi: 10.1017/S1368980012004879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martin-Calvo N., Chavarro J.E., Falbe J., Hu F.B., Field A.E. Adherence to the Mediterranean dietary pattern and BMI change among US adolescents. Int. J. Obes. 2016;40:1103–1108. doi: 10.1038/ijo.2016.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tognon G., Hebestreit A., Lanfer A., Moreno L.A., Pala V., Siani A., Tornaritis M., De Henauw S., Veidebaum T., Molnar D., et al. Mediterranean diet; overweight and body composition in children from eight European countries: Cross-sectional and prospective results from the IDEFICS study. Nutr. Metab. Cardiovasc. Dis. 2014;24:205–213. doi: 10.1016/j.numecd.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 45.Jennings A., Welch A., van Sluijs E.M., Griffin S.J., Cassidy A. Diet quality is independently associated with weight status in children aged 9-10 years. J. Nutr. 2011;141:453–459. doi: 10.3945/jn.110.131441. [DOI] [PubMed] [Google Scholar]
- 46.Vinke P.C., Luitjens M., Blijleven K.A., Navis G., Kromhout D., Corpeleijn E. Nutrition beyond the first 1000 days: Diet quality and 7-year change in BMI and overweight in 3-year old children from the Dutch GECKO Drenthe birth cohort. J. Dev. Orig. Health Dis. 2021;12:933–939. doi: 10.1017/S204017442000118X. [DOI] [PubMed] [Google Scholar]
- 47.L’Abee C., Sauer P.J., Damen M., Rake J.P., Cats H., Stolk R.P. Cohort Profile: The GECKO Drenthe study; overweight programming during early childhood. Int. J. Epidemiol. 2008;37:486–489. doi: 10.1093/ije/dym218. [DOI] [PubMed] [Google Scholar]
- 48.Flynn J.T., Kaelber D.C., Baker-Smith C.M., Blowey D., Carroll A.E., Daniels S.R., de Ferranti S.D., Dionne J.M., Falkner B., Flinn S.K., et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140:e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 49.Sijtsma A., Bocca G., L’Abee C., Liem E.T., Sauer P.J., Corpeleijn E. Waist-to-height ratio; waist circumference and BMI as indicators of percentage fat mass and cardiometabolic risk factors in children aged 3–7 years. Clin. Nutr. 2014;33:311–315. doi: 10.1016/j.clnu.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 50.Dutch Growth Research Foundation Growth Analyser: Innovative Healthcare Software Version 3.5. [(accessed on 3 July 2024)]. Available online: https://growthanalyser.org.
- 51.Cole T.J., Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness; overweight and obesity. Pediatr. Obes. 2012;7:284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 52.Dutman A.E., Stafleu A., Kruizinga A., Brants H.A., Westerterp K.R., Kistemaker C., Meuling W.J., Goldbohm R.A. Validation of an FFQ and options for data processing using the doubly labelled water method in children. Public Health Nutr. 2011;14:410–417. doi: 10.1017/S1368980010002119. [DOI] [PubMed] [Google Scholar]
- 53.The National Institute for Public Health and the Environment (RIVM)/Netherlands Nutrition Centre . NEVO-Tabel: Dutch Nutrient Database 2011. NEVO; Hague, The Netherlands: 2011. [Google Scholar]
- 54.Black A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: Basal metabolic rate. A practical guide to its calculation; use and limitations. Int. J. Obes. Relat. Metab. Disord. 2000;24:1119–1130. doi: 10.1038/sj.ijo.0801376. [DOI] [PubMed] [Google Scholar]
- 55.Schofield W.N. Predicting basal metabolic rate; new standards and review of previous work. Hum. Nutr. Clin. Nutr. 1985;39((Suppl. S1)):5–41. [PubMed] [Google Scholar]
- 56.Sijtsma A., Corpeleijn E., Sauer P.J. Energy requirements for maintenance and growth in 3- to 4-year-olds may be overestimated by existing equations. J. Pediatr. Gastroenterol. Nutr. 2014;58:642–646. doi: 10.1097/MPG.0000000000000278. [DOI] [PubMed] [Google Scholar]
- 57.Aubert A.M., Forhan A., de Lauzon-Guillain B., Chen L.W., Polanska K., Hanke W., Jankowska A., Mensink-Bout S.M., Duijts L., Suderman M., et al. Deriving the Dietary Approaches to Stop Hypertension (DASH) Score in Women from Seven Pregnancy Cohorts from the European ALPHABET Consortium. Nutrients. 2019;11:2706. doi: 10.3390/nu11112706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vafeiadi M., Margetaki K., Stratakis N., Roumeliotaki T., Chatzi L., Charles M.-A., Dargent-Molina P., Lioret S., de Lauzon B., Heude B., et al. LifeCycle quality checks and protocol for harmonization of WP3.1.4: Lifestyle (WP3) 2018. [(accessed on 3 July 2024)]. Available online: https://lifecycle-project.eu/wp-content/uploads/2020/05/LifeCycle_Subtask_3.1.4_Harmonisation_Protocol_QControl.pdf.
- 59.Tognon G., Moreno L.A., Mouratidou T., Veidebaum T., Molnar D., Russo P., Siani A., Akhandaf Y., Krogh V., Tornaritis M., et al. Adherence to a Mediterranean-like dietary pattern in children from eight European countries. The IDEFICS study. Int. J. Obes. 2014;38((Suppl. S2)):S108–S114. doi: 10.1038/ijo.2014.141. [DOI] [PubMed] [Google Scholar]
- 60.Parada-Ricart E., Luque V., Zaragoza M., Ferre N., Closa-Monasterolo R., Koletzko B., Grote V., Gruszfeld D., Verduci E., Xhonneux A., et al. Effect of maternal smoking during pregnancy on child blood pressure in a European cohort. Sci. Rep. 2022;12:17308. doi: 10.1038/s41598-022-21337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li L., Peters H., Gama A., Carvalhal M.I., Nogueira H.G., Rosado-Marques V., Padez C. Maternal smoking in pregnancy association with childhood adiposity and blood pressure. Pediatr. Obes. 2016;11:202–209. doi: 10.1111/ijpo.12046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Małachowska A., Gębski J., Jeżewska-Zychowicz M. Childhood Food Experiences and Selected Eating Styles as Determinants of Diet Quality in Adulthood-A Cross-Sectional Study. Nutrients. 2023;15:2256. doi: 10.3390/nu15102256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chao A.M., Quigley K.M., Wadden T.A. Dietary interventions for obesity: Clinical and mechanistic findings. J. Clin. Investig. 2021;131:e140065. doi: 10.1172/JCI140065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Usheva N., Lateva M., Galcheva S., Koletzko B.V., Cardon G., De Craemer M., Androutsos O., Kotowska A., Socha P., Moreno L.A., et al. Breastfeeding and Overweight in European Preschoolers: The ToyBox Study. Nutrients. 2021;13:2880. doi: 10.3390/nu13082880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stone M.S., Martin B.R., Weaver C.M. Short-Term RCT of Increased Dietary Potassium from Potato or Potassium Gluconate: Effect on Blood Pressure, Microcirculation, and Potassium and Sodium Retention in Pre-Hypertensive-to-Hypertensive Adults. Nutrients. 2021;13:1610. doi: 10.3390/nu13051610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang X., Li Y., Del Gobbo L.C., Rosanoff A., Wang J., Zhang W., Song Y. Effects of Magnesium Supplementation on Blood Pressure: A Meta-Analysis of Randomized Double-Blind Placebo-Controlled Trials. Hypertension. 2016;68:324–333. doi: 10.1161/HYPERTENSIONAHA.116.07664. [DOI] [PubMed] [Google Scholar]
- 67.Luft F.C., Miller J.Z., Lyle R.M., Melby C.L., Fineberg N.S., McCarron D.A., Weinberger M.H., Morris C.D. The effect of dietary interventions to reduce blood pressure in normal humans. J. Am. Coll. Nutr. 1989;8:495–503. doi: 10.1080/07315724.1989.10720319. [DOI] [PubMed] [Google Scholar]
- 68.Huang L., Trieu K., Yoshimura S., Neal B., Woodward M., Campbell N.R.C., Li Q., Lackland D.T., Leung A.A., Anderson C.A.M., et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: Systematic review and meta-analysis of randomised trials. BMJ. 2020;368:m315. doi: 10.1136/bmj.m315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guyton A.C., Coleman T.G., Young D.B., Lohmeier T.E., DeClue J.W. Salt balance and long-term blood pressure control. Annu. Rev. Med. 1980;31:15–27. doi: 10.1146/annurev.me.31.020180.000311. [DOI] [PubMed] [Google Scholar]
- 70.Filippini T., Violi F., D’Amico R., Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int. J. Cardiol. 2017;230:127–135. doi: 10.1016/j.ijcard.2016.12.048. [DOI] [PubMed] [Google Scholar]
- 71.Dibaba D.T., Xun P., Song Y., Rosanoff A., Shechter M., He K. The effect of magnesium supplementation on blood pressure in individuals with insulin resistance; prediabetes; or noncommunicable chronic diseases: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2017;106:921–929. doi: 10.3945/ajcn.117.155291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Korhonen P., Tihtonen K., Isojärvi J., Ojala R., Ashorn U., Ashorn P., Tammela O. Calcium supplementation during pregnancy and long-term offspring outcome: A systematic literature review and meta-analysis. Ann. N. Y. Acad. Sci. 2022;1510:36–51. doi: 10.1111/nyas.14729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen A.K., Roberts C.K., Barnard R.J. Effect of a short-term diet and exercise intervention on metabolic syndrome in overweight children. Metabolism. 2006;55:871–878. doi: 10.1016/j.metabol.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 74.Roberts C.K., Vaziri N.D., Barnard R.J. Effect of diet and exercise intervention on blood pressure; insulin; oxidative stress; and nitric oxide availability. Circulation. 2002;106:2530–2532. doi: 10.1161/01.CIR.0000040584.91836.0D. [DOI] [PubMed] [Google Scholar]
- 75.Hodgson J.M., Zhu K., Lewis J.R., Kerr D., Meng X., Solah V., Devine A., Binns C.W., Woodman R.J., Prince R.L. Long-term effects of a protein-enriched diet on blood pressure in older women. Br. J. Nutr. 2012;107:1664–1672. doi: 10.1017/S0007114511004740. [DOI] [PubMed] [Google Scholar]
- 76.Jiang J., Liu M., Troy L.M., Bangalore S., Hayes R.B., Parekh N. Concordance with DASH diet and blood pressure change: Results from the Framingham Offspring Study (1991–2008) J. Hypertens. 2015;33:2223–2230. doi: 10.1097/HJH.0000000000000710. [DOI] [PubMed] [Google Scholar]
- 77.Miura K., Nakagawa H. Can dietary changes reduce blood pressure in the long term? Curr. Opin. Nephrol. Hypertens. 2005;14:253–257. doi: 10.1097/01.mnh.0000165892.05996.f1. [DOI] [PubMed] [Google Scholar]
- 78.Wuhl E. Hypertension in childhood obesity. Acta Paediatr. 2019;108:37–43. doi: 10.1111/apa.14551. [DOI] [PubMed] [Google Scholar]
- 79.Savica V., Bellinghieri G., Kopple J.D. The effect of nutrition on blood pressure. Annu. Rev. Nutr. 2010;30:365–401. doi: 10.1146/annurev-nutr-010510-103954. [DOI] [PubMed] [Google Scholar]
- 80.Wiersma R., Hartman E., Boezen H M., Corpeleijn E. Adiposity and high blood pressure during childhood: A prospective analysis of the role of physical activity intensity and sedentary time in the GECKO Drenthe cohort. Int. J. Environ. Res. Public Health. 2020;17:9526. doi: 10.3390/ijerph17249526. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the Confidentiality Statement of Gecko Drenthe Cohort.