Abstract
Background
Depression, anxiety, and stress are the commonly encountered mental health conditions among medical students. Overseas environment may add additional burden to the existing environment. However, comparison of the rate and associated factors of depression, anxiety, stress among domestic and overseas students has not been attempted in Bangladesh. We aimed to assess the rate and associated factors of depression, anxiety, stress among domestic and overseas medical students in the country.
Methods
This cross‐sectional study was conducted among 360 undergraduate medical students in 2021. Data were collected by self‐reporting instruments by a stratified random sampling method by the Depression, Anxiety, and Stress Scale‐21 scale. Bivariable and multivariable binary logistic regression analyses were done by computing crude odds ratio and adjusted odds ratio with 95% confidence interval to identify the associated factors.
Results
Among the 360 undergraduate medical students, 181 were domestic and 179 overseas ones. 44.8% of domestic students reported depressive symptoms, 45.3% reported anxiety symptoms, and 33.1% reported stress. On the other hand, half of overseas students experienced depression (50.3%) and anxiety (52.5%), and 41.3% experienced stress. Female medical students were found vulnerable for developing depression, anxiety, and stress than males.
Conclusions
The study revealed higher rates of depression, anxiety, and stress among overseas undergraduate medical students enrolled in a private medical school of Bangladesh. Private medical college authorities could consider special services for overseas students to ensure adequate psychosocial support.
Keywords: anxiety, Bangladesh, depression, international students, medical students, stress
1. INTRODUCTION
Nowadays, mental health challenges among undergraduate students are a pressing global concern. Young adults between 18 and 24 years of age are at higher risk of mental disorders, including major depressive disorder, anxiety, and psychiatric comorbidities. 1 , 2 , 3 In recent years, undergraduate medical students have been reported as one of the most vulnerable groups who are experiencing mental health problems. 4 , 5 A large body of literature shows higher levels of psychological distress among medical students and residents. 5 , 6 , 7 , 8 Medical students initially exhibit better mental health compared to their nonmedical peers, but they experience a decline in mental well‐being during medical training. 9 , 10 , 11 The method of medical education and training can directly lead to psychological distress among medical students. 9
People with poor mental health tend to experience lower levels of physical and mental well‐being. Depression can be caused by various factors, such as genetics, social context, psychological predispositions, and life events, often triggered by adverse experiences. 12 It significantly influences a person's thoughts, decisions, and behaviors. 12 , 13 Anxiety is, on the other hand, related to fear and manifests as a future‐oriented mood state consisting of a complex cognitive, affective, physiological, and behavioral response system associated with preparation for anticipated events or situations perceived as threats. 14 Chronic stress emerges as a significant risk factor for depression and anxiety. 15 , 16 A longitudinal study reported a rise in the level of stress and depression in second‐year medical students compared to when entering medical school. 17 Medical students are exposed to numerous stressors that may affect their mental health, such as exam anxiety, excessive course load, poor social support, financial strain, sleep deprivation, and personal life events. 18 , 19 , 20 Psychological distress can adversely influence medical students, including compromised academic performance, diminished competency, increased likelihood of medical errors, dropping out of medical school, and suicidal ideation and attempts. 9 , 21
In Bangladesh, depression and anxiety are the commonly recognized mental health issues affecting university and medical students. 22 , 23 , 24 , 25 , 26 , 27 A good number of overseas students, especially from India (Kashmir), and Nepal are being admitted to medical colleges in Bangladesh. Maintaining good mental health is important for medical students to improve learning, reduce burnout, and enhance the quality of patient care. It is enormously important to investigate the burden and associated sociodemographic determinants of commonly occurring mental health conditions like depression, anxiety, and stress for developing coping strategies. Despite the evident need for targeted interventions, there is a dearth of research, comparing the burden and associated factors of depression, anxiety, and stress among domestic and overseas medical students in Bangladesh. Therefore, this study was undertaken to assess and compare the rate and associated sociodemographic factors of depression, anxiety, and stress among domestic and overseas undergraduate medical students of a medical college in Bangladesh.
2. METHODS
2.1. Study design and participants
The current cross‐sectional study was conducted among undergraduate medical students enrolled at Tairunnessa Memorial Medical College (a private medical college, established in 1995), located in Tongi, Gazipur, Bangladesh. Students enrolled in 2021 from first year to fifth year were recruited for the study.
2.2. Sampling strategy
Probability sampling was used to calculate the sample size of this study. The minimum required sample size for this study was calculated using a single population proportion formula, , where n = desired sample size, z = standard normal deviate = 1.96 at 95% confidence interval, p = prevalence of depression among medical college students in Bangladesh = 39.1%, 28 and e = margin of error = 5%. The calculated sample size was 366. Assuming a nonresponse rate of 5%, we aimed to approach a total of 386 students for interviews. Although the 386 randomly selected students were approached, 17 of them refused to participate in the study. Furthermore, nine interviews were excluded from the 369 interviews conducted due to incomplete information, and we finally analyzed the data of 360 respondents.
We used a stratified random sampling method for this study, where stratification was done on student type (domestic and overseas) and student level (first year, second year, third year, fourth year, and fifth year). First, we allocated the sample equally between domestic and overseas students. The total sample was then proportionately allocated based on the number of students in each year.
2.3. Data collection procedure
Data were collected by self‐reporting instruments. We prepared the questionnaire in Bangla for domestic students and in English for international students. As per the list, we distributed the questionnaire and collected after their responses.
2.4. Measures
2.4.1. Sociodemographic variables
The study collected information on the following sociodemographic variables: sex (male or female), age (≤20 years or 21–26 years), student type (overseas or domestic), student level (first year, second year, third year, fourth year, or fifth year), religion (Muslim or Hindu/Christian/Buddhist), marital status (ever married or unmarried), family type (nuclear or joint), monthly family income (≤70,000 BDT, 71,000 to 149,000 BDT, or 150,000 + BDT), residence type (urban or rural), and smoking status (smoker or nonsmoker).
2.4.2. Depression, anxiety, and stress scale
This study used the Depression, Anxiety, and Stress Scale (DASS‐ 21) to assess depression, anxiety, and stress among undergraduate medical students. This 21‐item scale has three subscales: depression subscale, anxiety subscale, and stress subscale with 7 items per subscale, where participants are asked to rate their reaction to each item over the past week on a 4‐point scale (0 = Did not apply to me at all, 1 = Applied to me to some degree, or some of the time, 2 = Applied to me to a considerable degree or a good part of time, and 3 = Applied to me very much or most of the time). 29 Scores for each subscale are calculated by adding the scores of relevant items in the specific subscale and multiplying by 2. Scores ≥14, ≥10, and ≥19 were used to indicate the presence of depression, anxiety, and stress, respectively. 30 The reliability of the DASS‐21 was tested by Cronbach's alpha. The overall Cronbach's α of this scale was 0.91, and the Cronbach's α of the depression, anxiety, and stress subscales was 0.82, 0.85, and 0.82, respectively. However, we used the previously validated Bangla version of the DASS‐21 for our data collection for native students and English version for overseas students. 31 Furthermore, we evaluated participants' distress statusbased on three psychiatric symptoms: depression, anxiety, and stress. Participants who had at least one of these three psychiatric symptoms were categorized as those having distress. On the other hand, those who experienced none of these symptoms were considered non‐distressed.
2.5. Statistical analysis
All statistical analyses were performed using Stata version 17. Frequencies and percentages were used to describe the sociodemographic characteristics of the study sample. Bivariable and multivariable binary logistic regression analyses were done by computing crude odds ratio (COR) and adjusted odds ratio (AOR) with 95% confidence interval (CI) to identify the factors associated with depression, anxiety, and stress among undergraduate medical students. All variables were entered into the multivariable logistic regression analyses. Model fitness was checked using the Hosmer‐Lemeshow test for depression, anxiety, stress, and distress, which had a p‐value of 0.93, 0.51, 0.19, and 0.32, respectively. These values are greater than a p‐value of 0.05, indicating that all these models were fitted to our data. 32 The multicollinearity of the independent variables was also checked by observing the standard errors (SEs) of regression coefficients in the logistic regression analyses. In this study, the SEs of regression coefficients in the models for depression, anxiety, and stress were less than 5.0, which indicates that there was no multicollinearity between the independent variables. 33 All statistics were tested using a two‐sided test, and p‐value of <0.05 was considered statistically significant.
2.6. Ethical considerations
Ethical clearance was taken from the Institutional Ethical Review Board (IERB) of Tairunnessa Memorial Medical College, Gazipur (TMMC/2024/01). Informed written consent was taken before collecting the data.
3. RESULTS
3.1. Sociodemographic characteristics of the respondents
A total of 360 undergraduate medical students, comprising 181 domestic and 179 overseas ones participated in this study. Among domestic students, 65.2% were female, whereas 54.7% of overseas students were male. The majority of students—both domestic (58.0%) and overseas (55.9%) were 21 years of age or younger. The largest portion of domestic respondents were from the first year (26.5%), followed by third year (25.4%). Similarly, among overseas respondents, first‐year students claimed the highest percentage (24.6%), followed by third‐year students (24.0%). The vast majority of both domestic (95.0%) and overseas (93.9%) students were Muslims. Over 90.0% of the respondents were unmarried, with a slightly higher percentage of domestic students (95.6%) than overseas students (92.7%). 84.0% of domestic students belonged to nuclear families compared to 74.3% of overseas students (Table 1). The highest share of both domestic (44.8%) and overseas (69.3%) students claimed that their monthly family income was 150,000 BDT or more. The majority of both domestic (70.7%) and overseas (53.6%) students came from urban areas. About 4.0% of domestic students were smokers, whereas the smoking rate among overseas students (11.7%) was more than double that of domestic students.
Table 1.
Sociodemographic characteristics of the respondents.
| Variable | Overall (n = 360) | Domestic (n = 181) | Overseas (n = 179) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Sex | ||||||
| Male | 161 | 44.7 | 63 | 34.8 | 98 | 54.7 |
| Female | 199 | 55.3 | 118 | 65.2 | 81 | 45.3 |
| Age | ||||||
| ≤21 years | 205 | 56.9 | 105 | 58.0 | 100 | 55.9 |
| 22–26 years | 155 | 43.1 | 76 | 42.0 | 79 | 44.1 |
| Student level | ||||||
| First year | 92 | 25.6 | 48 | 26.5 | 44 | 24.6 |
| Second year | 64 | 17.8 | 36 | 19.9 | 28 | 15.6 |
| Third year | 89 | 24.7 | 46 | 25.4 | 43 | 24.0 |
| Fourth year | 53 | 14.7 | 30 | 16.6 | 23 | 12.8 |
| Fifth year | 62 | 17.2 | 21 | 11.6 | 41 | 22.9 |
| Religion | ||||||
| Muslim | 340 | 94.4 | 172 | 95.0 | 168 | 93.9 |
| Hindu/Christian/Buddhist | 20 | 5.6 | 9 | 5.0 | 11 | 6.1 |
| Marital status | ||||||
| Ever married | 21 | 5.8 | 8 | 4.4 | 13 | 7.3 |
| Unmarried | 339 | 94.2 | 173 | 95.6 | 166 | 92.7 |
| Family type | ||||||
| Nuclear | 285 | 79.2 | 152 | 84.0 | 133 | 74.3 |
| Joint | 75 | 20.8 | 29 | 16.0 | 46 | 25.7 |
| Monthly family income | ||||||
| ≤70,000 BDT | 48 | 13.3 | 32 | 17.7 | 16 | 8.9 |
| 71,000–149,000 BDT | 107 | 29.7 | 68 | 37.6 | 39 | 21.8 |
| ≥150,000 BDT | 205 | 56.9 | 81 | 44.8 | 124 | 69.3 |
| Residence type | ||||||
| Urban | 224 | 62.2 | 128 | 70.7 | 96 | 53.6 |
| Rural | 136 | 37.8 | 53 | 29.3 | 83 | 46.4 |
| Smoking status | ||||||
| Smoker | 29 | 8.1 | 8 | 4.4 | 21 | 11.7 |
| Nonsmoker | 331 | 91.9 | 173 | 95.6 | 158 | 88.3 |
3.2. Rate of depression, anxiety, and stress
Figure 1 presents the rate of depression, anxiety, and stress among domestic and overseas undergraduate medical students. According to the figure, 44.8% of domestic students reported depressive symptoms, 45.3% reported anxiety symptoms, and one‐third (33.1%) reported stress. On the other hand, half of overseas students (50.3%) experienced depression, 52.5% experienced anxiety, and 41.3% experienced stress.
Figure 1.
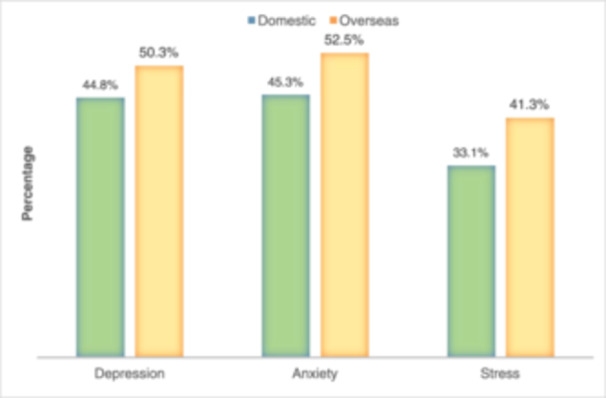
Rate of depression, anxiety, and stress among undergraduate medical students.
3.3. Factors associated with depression
Table 2 demonstrates the bivariable and multivariable associations between sociodemographic factors and depression among domestic and overseas undergraduate medical students. According to the bivariable analysis results, female sex (p = 0.025), age: 22–26 years (p = 0.007), student level: fourth year (p = 0.002), student level: fifth year (p = 0.004), and monthly family income: ≤70,000 BDT (p = 0.003) were associated with depression among domestic students. The multivariable analysis results reveal that female domestic students were at 2.62 times higher risk of having depressive symptoms than male domestic students (95% CI: 1.2–5.7). Fourth‐year and fifth‐year domestic students were respectively 3.96 (95% CI: 1.3–12.3) and 4.31(95% CI: 1.1–16.2) times more likely to experience depressive symptoms compared to their third‐year counterparts. Domestic students whose monthly family income was ≤70,000 BDT had 4.2‐fold higher odds of reporting depressive symptoms compared to those whose monthly family income was ≥150,000 BDT (95% CI: 1.5–11.8).
Table 2.
Bivariable and multivariable logistic regression analysis of sociodemographic factors associated with depression among domestic and overseas medical students.
| Overall depression | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Present | Absent | Domestic students (n = 181) | Overseas students (n = 179) | ||||||||
| Variable | n (%) | n (%) | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value | |
| Sex | |||||||||||
| Female | 110 (55.3) | 89 (44.7) | 2.1 (1.1–3.9) | 0.025 | 2.6 (1.2–5.7) | 0.016 | 2.3 (1.3–4.3) | 0.006 | 2.6 (1.3–5.4) | 0.009 | |
| Male | 61 (37.9) | 100 (62.1) | Reference | Reference | Reference | Reference | |||||
| Age | |||||||||||
| 22–26 years | 71 (45.8) | 84 (54.2) | 2.3 (1.3–4.2) | 0.007 | 1.1 (0.4–3.3) | 0.837 | 0.34 (0.2–0.6) | <0.001 | 0.5 (0.2–1.3) | 0.153 | |
| ≤21 years | 100 (48.8) | 105 (51.2) | Reference | Reference | Reference | ||||||
| Student level | |||||||||||
| First year | 52 (56.5) | 40 (43.5) | 1.2 (0.5–2.9) | 0.620 | 1.1 (0.4–3.2) | 0.884 | 4.3 (1.2–7.8) | 0.002 | 4.0 (1.1–15.2) | 0.030 | |
| Second year | 26 (40.6) | 38 (59.4) | 1.0 (1.4–33.6) | 0.945 | 0.79 (0.3–2.5) | 0.695 | 1.3 (1.1–8.7) | 0.631 | 0.7 (0.9–11.5) | 0.080 | |
| Fourth year | 29 (54.7) | 24 (45.3) | 4.8 (1.8–13.0) | 0.002 | 3.96 (1.3–12.3) | 0.018 | 0.7 (0.3–2.9) | 0.460 | 0.8 (0.3–3.5) | 0.925 | |
| Fifth year | 30 (48.4) | 32 (51.6) | 5.2 (1.7–16.0) | 0.004 | 4.3 (1.1–16.3) | 0.031 | 0.7 (0.3–1.8) | 0.479 | 1.1 (0.3–3.5) | 0.907 | |
| Third year | 34 (38.2) | 55 (61.8) | Reference | Reference | Reference | Reference | |||||
| Religion | |||||||||||
| Muslim | 159 (46.8) | 181 (53.2) | 1.7 (0.4–6.9) | 0.484 | 0.9 (0.2–4.4) | 0.928 | 0.2 (0.1– 1.0) | 0.048 | 0.3 (0.1–1.4) | 0.118 | |
| Hindu/Christian/Buddhist | 12 (60.0) | 8 (40.0) | Reference | Reference | Reference | Reference | |||||
| Marital status | |||||||||||
| Ever married | 9 (42.9) | 12 (57.1) | 0.7 (0.2–3.1) | 0.674 | 1.3 (0.3–6.4) | 0.722 | 0.8 (0.3–2.6) | 0.758 | 1.03 (0.3–3.8) | 0.968 | |
| Unmarried | 162 (47.8) | 177 (52.2) | Reference | Reference | Reference | Reference | |||||
| Family type | |||||||||||
| Nuclear | 143 (50.2) | 142 (49.8) | 1.00 (0.5– 2.2) | 0.993 | 1.1 (0.5–2.9) | 0.784 | 2.7 (1.3–5.4) | 0.006 | 3.6 (1.5–9.0) | 0.005 | |
| Joint | 28 (37.3) | 47 (62.7) | Reference | Reference | Reference | Reference | |||||
| Monthly family income | |||||||||||
| ≤70,000 BDT | 33 (68.8) | 15 (31.3) | 3.9 (1.6–9.8) | 0.003 | 4.2 (1.5–11.8) | 0.006 | 1.3 (0.5–3.7) | 0.639 | 1.3 (0.4–4.4) | 0.693 | |
| 71,000–149,000 BDT | 41 (38.3) | 66 (61.7) | 0.6 (0.3–1.2) | 0.176 | 0.6 (0.3–1.2) | 0.135 | 1.0 (0.5–2.0) | 0.889 | 1.1 (0.5–2.4) | 0.905 | |
| 150,000 + BDT | 97 (47.3) | 108 (52.7) | Reference | Reference | Reference | Reference | |||||
| Residence type | |||||||||||
| Urban | 113 (50.4) | 111 (49.6) | 1.3 (0.7–2.8) | 0.373 | 1.0 (0.4–2.1) | 0.908 | 1.5 (0.9–2.8) | 0.157 | 1.4 (0.7–2.9) | 0.371 | |
| Rural | 58 (42.6) | 78 (57.4) | Reference | Reference | Reference | Reference | |||||
| Smoking status | |||||||||||
| Smoker | 16 (55.2) | 13 (44.8) | 0.7 (0.2–3.2) | 0.674 | 0.8 (0.2–4.5) | 0.836 | 1.6 (0.9–2.9) | 0.195 | 3.8 (1.2–11.9) | 0.022 | |
| Nonsmoker | 155 (46.8) | 176 (53.2) | Reference | Reference | Reference | Reference | |||||
Note: Bold values indicate significant results.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio.
On the other hand, there was a bivariate association between female sex (p = 0.006), age: 22–26 years (p < 0.001), student level: first year (p = 0.002), Muslim religion (p = 0.048), and nuclear family type (p = 0.006) and depression among overseas students. The multivariable analysis results also show that female overseas students were 2.60 times more likely to develop depressive symptoms compared to their male counterparts (95% CI: 1.3–5.4). Overseas first‐year students were at 4.0 times higher risk of experiencing depression than overseas third‐year students (95% CI: 1.1–15.2). Overseas students from a nuclear family were 3.6 times more likely to develop depression compared to those from a joint family (95% CI: 1.5–9.0). The results also show that overseas students who smoked were 3.8 times more likely to report depressive symptoms than those who did not smoke (95% CI: 1.2–11.9).
3.4. Factors associated with anxiety
Table 3 presents the bivariable and multivariable associations between sociodemographic factors and anxiety among domestic and overseas undergraduate medical students. The bivariable analysis results show that female sex (p = 0.008), age: 22–26 years (p = 0.010), student level: fourth year (p = 0.002), and student level: fifth year (p = 0.001) were associated with anxiety among domestic students. The multivariable analysis results show that female domestic students were at 2.4 times higher risk of experiencing anxiety symptoms than their male counterparts (95% CI: 1.1–5.2). Fourth‐year and fifth‐year domestic students were respectively 3.8 (95% CI: 1.2–11.6) and 6.4 (95% CI: 1.6–25.6) times more likely to develop anxiety symptoms compared to third‐year domestic students.
Table 3.
Bivariable and multivariable logistic regression analysis of sociodemographic factors associated with anxiety among domestic and overseas medical students.
| Overall anxiety | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Present | Absent | Domestic students (n = 181) | Overseas students (n = 179) | |||||||
| Variable | n (%) | n (%) | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value |
| Sex | ||||||||||
| Female | 114 (57.3) | 85 (42.7) | 2.4 (1.3–4.5) | 0.008 | 2.4 (1.1–5.2) | 0.024 | 2.4 (1.3–4.4) | 0.005 | 3.1 (1.5–6.5) | 0.003 |
| Male | 62 (38.5) | 99 (61.5) | Reference | Reference | Reference | Reference | ||||
| Age | ||||||||||
| 22–26 years | 72 (46.5) | 83 (53.5) | 2.2 (1.2–4.0) | 0.010 | 1.2 (0.4–3.6) | 0.703 | 0.3 (0.2–0.6) | <0.001 | 0.5 (0.2–1.4) | 0.164 |
| ≤21 years | 104 (50.7) | 101 (49.3) | Reference | Reference | Reference | |||||
| Student level | ||||||||||
| First year | 51 (55.4) | 41 (44.6) | 1.3 (0.5–3.0) | 0.608 | 1.3 (0.4–3.8) | 0.653 | 3.6 (1.4–9.0) | 0.002 | 3.6 (1.2–11.1) | 0.026 |
| Second year | 31 (48.4) | 33 (51.6) | 1.6 (0.7–4.1) | 0.293 | 1.5 (0.5–4.6) | 0.483 | 1.4 (0.5– 3.6) | 0.631 | 0.8 (0.2–2.5) | 0.669 |
| Fourth year | 29 (54.7) | 24 (45.3) | 4.6 (1.7–12.2) | 0.002 | 3.8 (1.2–11.6) | 0.020 | 0.7 (0.2–1.9) | 0.460 | 0.8 (0.2–2.5) | 0.775 |
| Fifth year | 30 (48.4) | 32 (51.6) | 7.3 (2.2–23.9) | 0.001 | 6.4 (1.6–25.6) | 0.008 | 0.5 (0.2–1.3) | 0.479 | 0.8 (0.2–2.5) | 0.643 |
| Third year | 35 (39.3) | 54 (60.7) | Reference | Reference | Reference | Reference | ||||
| Religion | ||||||||||
| Muslim | 166 (48.8) | 174 (51.2) | 3.0 (0.6–15.1) | 0.173 | 2.3 (0.4–13.0) | 0.354 | 0.4 (0.1–1.5) | 0.179 | 0.5 (0.1–2.4) | 0.410 |
| Hindu/Christian/Buddhist | 10 (50.0) | 10 (50.0) | Reference | Reference | Reference | Reference | ||||
| Marital status | ||||||||||
| Ever married | 11 (52.4) | 10 (47.6) | 1.2 (0.3–5.0) | 0.785 | 2.2 (0.5–10.0) | 0.331 | 1.1 (0.3–3.3) | 0.920 | 1.3 (0.3–4.8) | 0.729 |
| Unmarried | 165 (48.7) | 174 (51.3) | Reference | Reference | Reference | Reference | ||||
| Family type | ||||||||||
| Nuclear | 144 (50.3) | 141 (49.5) | 1.0 (0.5–2.3) | 0.955 | 1.2 (0.5–3.1) | 0.670 | 1.8 (0.9–3.6) | 0.079 | 2.2 (0.9–5.2) | 0.079 |
| Joint | 32 (42.7) | 43 (57.3) | Reference | Reference | Reference | Reference | ||||
| Monthly family income | ||||||||||
| ≤70,000 BDT | 31 (64.6) | 17 (35.4) | 2.0 (0.9–4.6) | 0.110 | 1.7 (0.7–4.4) | 0.279 | 2.2 (0.7–6.7) | 0.165 | 2.3 (0.6–8.1) | 0.211 |
| 71,000–149,000 BDT | 46 (43.0) | 61 (57.0) | 0.7 (0.4–1.3) | 0.272 | 0.5 (0.3–1.2) | 0.123 | 1.2 (0.6–2.4) | 0.675 | 1.3 (0.6–3.0) | 0.557 |
| 150,000 + BDT | 99 (48.3) | 106 (51.7) | Reference | Reference | Reference | Reference | ||||
| Residence type | ||||||||||
| Urban | 115 (51.3) | 109 (48.7) | 1.0 (0.5–2.3) | 0.955 | 1.1 (0.5–2.4) | 0.814 | 1.3 (0.7–2.3) | 0.438 | 1.2 (0.6–2.6) | 0.568 |
| Rural | 61 (44.9) | 75 (55.1) | Reference | Reference | Reference | Reference | ||||
| Smoking status | ||||||||||
| Smoker | 18 (62.1) | 11 (37.9) | 0.4 (0.1–2.0) | 0.254 | 0.4 (0.1–2.4) | 0.323 | 3.3 (1.2–9.4) | 0.027 | 6.8 (2.0–23.1) | 0.002 |
| Nonsmoker | 158 (47.7) | 173 (52.3) | Reference | Reference | Reference | Reference | ||||
Note: Bold values indicate significant results.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio.
The bivariable analysis results also exhibit that female sex (p = 0.005), age: 22–26 years (p < 0.001), student level: first year (p = 0.002), and smoking status: smoker (p = 0.027) were associated with anxiety among overseas students. It is evident from the multivariable analysis results that female overseas students were at 3.1 times increased risk of developing anxiety compared to male overseas students (95% CI: 1.5–6.5). Overseas first‐year students were 3.6 times more likely to have anxiety symptoms than overseas third‐year students (95% CI: 1.2–11.1). Overseas students who smoked had a 6.8 times higher chance of experiencing anxiety symptoms than their nonsmoking counterparts (95% CI: 2.0–23.1).
3.5. Factors associated with stress
Table 4 shows the bivariable and multivariable associations between sociodemographic factors and stress among domestic and overseas undergraduate medical students. As suggested by the bivariable analysis results, female sex (p = 0.024), age: 22–26 years (p = 0.002), student level: fourth year (p = 0.042), student level: fifth year (p < 0.001), and monthly family income: ≤70,000 BDT (p = 0.020) were associated with stress among domestic students. According to the multivariable analysis results, female domestic students were 2.6 times more likely to report stress than their male counterparts (95% CI: 1.1–6.1). Fifth‐year domestic students had a 7.4 times higher chance of experiencing stress compared to third‐year domestic students (95% CI: 1.9–29.3). Domestic students whose monthly family income was ≤70,000 BDT were 2.8 times more likely to develop stress than those whose monthly family income was ≥150,000 BDT (95% CI: 1.1–7.5).
Table 4.
Bivariable and multivariable logistic regression analysis of sociodemographic factors associated with stress among domestic and overseas undergraduate medical students.
| Overall stress | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Present | Absent | Domestic students (n = 181) | Overseas students (n = 179) | ||||||||
| Variable | n (%) | n (%) | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value | |
| Sex | |||||||||||
| Female | 89 (44.7) | 110 (55.3) | 2.2 (1.1–4.5) | 0.024 | 2.6 (1.1–6.1) | 0.016 | 2.5 (1.3–4.5) | 0.004 | 2.4 (1.2–4.7) | 0.015 | |
| Male | 45 (28.0) | 116 (72.0) | Reference | Reference | Reference | Reference | |||||
| Age | |||||||||||
| 22–26 years | 59 (38.1) | 96 (61.9) | 2.7 (1.5–5.2) | 0.002 | 1.3 (0.4–4.3) | 0.634 | 0.4 (0.2–0.8) | 0.009 | 0.8 (0.3–2.3) | 0.666 | |
| ≤21 years | 75 (36.6) | 130 (63.4) | Reference | Reference | Reference | ||||||
| Student level | |||||||||||
| First year | 37 (40.2) | 55 (59.8) | 0.8 (0.3–2.2) | 0.720 | 0.8 (0.2–2.7) | 0.681 | 3.3 (1.4–7.9) | 0.008 | 3.4 (1.2–9.7) | 0.021 | |
| Second year | 24 (37.5) | 40 (62.5) | 1.2 (0.5–3.3) | 0.691 | 1.1 (0.3–3.7) | 0.944 | 2.1 (0.8–5.5) | 0.144 | 1.6 (0.5–4.9) | 0.403 | |
| Fourth year | 24 (45.3) | 29 (54.7) | 2.8 (1.0–7.5) | 0.042 | 2.0 (0.6–6.1) | 0.243 | 1.6 (0.6–4.5) | 0.381 | 1.5 (0.4–5.4) | 0.504 | |
| Fifth year | 24 (38.7) | 38 (61.3) | 8.0 (2.5–25.5) | <0.001 | 7.4 (1.9–29.3) | 0.005 | 0.6 (0.2–1.6) | 0.278 | 0.7 (0.2–2.4) | 0.570 | |
| Third year | 25 (28.1) | 64 (71.9) | Reference | Reference | Reference | Reference | |||||
| Religion | |||||||||||
| Muslim | 125 (36.8) | 215 (63.2) | 1.8 (0.4–8.9) | 0.480 | 1.2 (0.2–7.0) | 0.858 | 0.4 (0.1–1.4) | 0.133 | 0.5 (0.1–1.9) | 0.284 | |
| Hindu/Christian/Buddhist | 9 (45.0) | 11 (55.0) | Reference | Reference | Reference | Reference | |||||
| Marital status | |||||||||||
| Ever married | 7 (33.3) | 14 (66.7) | 01.2 (0.3–5.3) | 0.789 | 2.7 (0.6–13.5) | 0.220 | 0.6 (0.2–2.1) | 0.425 | 0.8 (0.2–3.1) | 0.707 | |
| Unmarried | 127 (37.5) | 212 (62.5) | Reference | Reference | Reference | Reference | |||||
| Family type | |||||||||||
| Nuclear | 110 (38.6) | 175 (61.4) | 1.1 (0.5–2.6) | 0.792 | 1.5 (0.5–4.4) | 0.433 | 1.7 (0.8–3.3) | 0.165 | 1.6 (0.7–3.7) | 0.259 | |
| Joint | 24 (32.0) | 51 (68.0) | Reference | Reference | Reference | Reference | |||||
| Monthly family income | |||||||||||
| ≤70,000 BDT | 28 (58.3) | 20 (41.7) | 2.7 (1.2–6.3) | 0.020 | 2.8 (1.1–7.5) | 0.036 | 2.6 (0.9–7.5) | 0.088 | 2.6 (0.8–8.8) | 0.115 | |
| 71,000–149,000 BDT | 31 (29.0) | 76 (71.0) | 0.7 (0.3–1.4) | 0.248 | 0.5 (0.2–1.2) | 0.115 | 1.0 (0.5–2.0) | 0.906 | 1.0 (0.4–2.2) | 0.922 | |
| ≥150,000 BDT | 75 (36.6) | 130 (63.4) | Reference | Reference | Reference | Reference | |||||
| Residence type | |||||||||||
| Urban | 85 (38.0) | 139 (62.1) | 1.6 (0.8–3.2) | 0.217 | 1.1 (0.5–2.6) | 0.861 | 1.0 (0.5–1.7) | 0.834 | 0.8 (0.4–1.7) | 0.644 | |
| Rural | 49 (36.0) | 87 (64.0) | Reference | Reference | Reference | Reference | |||||
| Smoking status | |||||||||||
| Smoker | 13 (44.8) | 16 (55.2) | 1.2 (0.3–5.3) | 0.789 | 1.7 (0.3–8.4) | 0.533 | 1.3 (0.5–3.3) | 0.535 | 2.0 (0.7–5.9) | 0.284 | |
| Nonsmoker | 121 (36.6) | 210 (63.4) | Reference | Reference | Reference | Reference | |||||
Note: Bold values indicate significant results.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio.
The bivariable analysis results also reveal that female sex (p = 0.004), age: 22–26 years (p = 0.009), and student level: first year (p = 0.008) were associated with stress among overseas students. It is found from the multivariable analysis results that female overseas students were 2.4 times more likely to develop stress compared to their male counterparts (95% CI: 1.2–4.7). Overseas first‐year students were at 3.4 times higher risk of having stress than overseas third‐year students (95% CI: 1.2–9.7).
3.6. Factors associated with distress
Table 5 shows the bivariable and multivariable associations between sociodemographic factors and distress among domestic and overseas undergraduate medical students. The bivariable analysis results show that age: 22–26 years (p = 0.049), student level: fourth year (p = 0.023) and fifth year (p = 0.005), and monthly family income: ≤70,000 BDT (0.019) were associated with distress among domestic students. On the other hand, the multivariable analysis results display that fifth‐year domestic students were 8.7 times more likely to feel distressed (95% CI: 1.6–48.3; third‐year‐reference year).
Table 5.
Bivariable and multivariable logistic regression analysis of sociodemographic factors associated with distress among domestic and overseas undergraduate medical students.
| Overall distress | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Present | Absent | Domestic students (n = 181) | Overseas students (n = 179) | |||||||
| Variable | n (%) | n (%) | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value | COR (95% CI) | p‐Value | AOR (95% CI) | p‐Value |
| Sex | ||||||||||
| Female | 139 (69.8) | 60 (30.2) | 1.8 (0.9–3.3) | 0.072 | 1.7 (0.8–3.6) | 0.156 | 1.9 (1.0–3.7) | 0.047 | 1.8 (0.9–3.9) | 0.119 |
| Male | 93 (57.8) | 68 (42.2) | Reference | Reference | Reference | Reference | ||||
| Age | ||||||||||
| 22– 26 years | 95 (61.3) | 60 (38.7) | 1.9 (1.0–3.5) | 0.049 | 1.0 (0.3–2.7) | 0.950 | 0.3 (0.2–0.6) | <0.001 | 0.4 (0.1–1.2) | 0.088 |
| ≤21 years | 137 (66.8) | 68 (33.2) | Reference | Reference | Reference | |||||
| Student level | ||||||||||
| First year | 65 (70.7) | 27 (29.3) | 1.1 (0.5–2.4) | 0.840 | 0.9 (0.3–2.6) | 0.897 | 8.7 (2.6–28.6) | <0.001 | 9.9 (2.4–41.6) | 0.002 |
| Second year | 42 (65.6) | 22 (34.4) | 1.4 (0.6–3.4) | 0.453 | 1.1 (0.4–3.3) | 0.834 | 2.6 (0.9–7.4) | 0.072 | 1.8 (0.5–6.1) | 0.338 |
| Fourth year | 38 (71.7) | 15 (28.3) | 3.3 (1.2–9.2) | 0.023 | 2.8 (0.9–9.0) | 0.078 | 1.6 (0.6–4.6) | 0.360 | 2.6 (0.7–9.6) | 0.143 |
| Fifth year | 41 (66.1) | 21 (33.9) | 9.5 (2.0–45.5) | 0.005 | 8.7 (1.6–48.3) | 0.013 | 1.0 (0.4–2.4) | 0.988 | 2.1 (0.7–6.6) | 0.217 |
| Third year | 46 (51.7) | 43 (48.3) | Reference | Reference | Reference | Reference | ||||
| Religion | ||||||||||
| Muslim | 220 (64.7) | 120 (35.3) | 3.4 (0.8–14.0) | 0.093 | 2.4 (0.5–11.6) | 0.273 | 0.4 (0.1–2.1) | 0.310 | 0.9 (0.2–5.2) | 0.909 |
| Hindu/Christian/Buddhist | 12 (60.0) | 8 (40.0) | Reference | Reference | Reference | Reference | ||||
| Marital status | ||||||||||
| Ever married | 12 (57.1) | 9 (42.9) | 0.6 (0.1–2.6) | 0.505 | 1.1 (0.2–5.1) | 0.889 | 0.8 (0.2–2.4) | 0.629 | 1.0 (0.3–3.7) | 0.960 |
| Unmarried | 220 (64.9) | 119 (35.1) | Reference | Reference | Reference | Reference | ||||
| Family type | ||||||||||
| Nuclear | 190 (66.7) | 95 (33.3) | 1.1 (0.5–2.6) | 0.744 | 1.4 (0.6–3.6) | 0.464 | 2.2 (1.1–4.4) | 0.028 | 2.8 (1.2–6.7) | 0.018 |
| Joint | 42 (56.0) | 33 (44.0) | Reference | Reference | Reference | Reference | ||||
| Monthly family income | ||||||||||
| ≤70,000 BDT | 40 (83.3) | 8 (16.7) | 3.5 (1.2–10.1) | 0.019 | 3.0 (0.9–9.3) | 0.055 | 2.1 (0.6–7.9) | 0.255 | 2.1 (0.5–9.2) | 0.316 |
| 71,000–149,000 BDT | 60 (56.1) | 47 (43.9) | 0.7 (0.4–1.3) | 0.269 | 0.6 (0.3–1.3) | 0.178 | 0.9 (0.4–1.9) | 0.744 | 0.7 (0.3–1.8) | 0.511 |
| ≥150,000 BDT | 132 (64.4) | 73 (35.6) | Reference | Reference | Reference | Reference | ||||
| Residence type | ||||||||||
| Urban | 148 (66.1) | 76 (33.9) | 1.3 (0.7–2.5) | 0.402 | 1.0 (0.5–2.3) | 0.920 | 1.2 (0.7–2.3) | 0.500 | 0.9 (0.4–1.9) | 0.782 |
| Rural | 84 (61.8) | 52 (38.2) | Reference | Reference | Reference | Reference | ||||
| Smoking status | ||||||||||
| Smoker | 19 (65.5) | 10 (34.5) | 0.4 (0.1–1.6) | 0.173 | 0.4 (0.1–2.1) | 0.294 | 1.6 (0.6–4.6) | 0.374 | 3.0 (0.9–10.3) | 0.078 |
| Nonsmoker | 213 (64.4) | 118 (35.6) | Reference | Reference | Reference | Reference | ||||
Note: Bold values indicate significant results.
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio.
The bivariable analysis results also exhibit that female sex (p = 0.047), age: 22–26 years (p < 0.001), student level: first year (p < 0.001), and nuclear family type (p = 0.028) were associated with distress among overseas students. According to the multivariable analysis results, first‐year overseas students were 9.9 times more likely to develop distress (95% CI: 2.4–41.6; third year‐reference year). Overseas students from nuclear families were at 2.8 times greater risk of distress than those from joint families (95% CI: 1.2–6.7).
4. DISCUSSION
The mental health and psychosocial well‐being of medical students are critical aspects of their overall academic success, professional development, and personal fulfillment. 34 Medical education is rigorous, demanding, and often stressful, placing significant pressure on students to excel academically while navigating the complexities of clinical training and patient care across the globe, and Bangladesh has no exception. 35 However, the mental health of medical students, domestic or overseas, has garnered increasing attention due to the demanding nature of their studies and the unique sociodemographic context of the country. 36 The present study identified higher prevalence of depression, anxiety and stress in overseas students than domestic students. These results are in line with the previous research conducted on the prevalence of mental health issues in Bangladesh, which have consistently highlighted elevated levels of depression, anxiety, and stress among medical students. 24 , 37 , 38 These mental health issues can have profound implications for students’ well‐being, academic performance, and future professional success. 39
Stress is an omnipresent challenge faced by medical students in Bangladesh, with academic stressors, clinical responsibilities, and personal pressures contributing to heightened stress levels. 38 Medical students often experience stress related to the volume and complexity of coursework, the demands of clinical rotations, long working hours, and exposure to human suffering and illness. Additionally, personal stressors, such as financial worries, family expectations, and lack of work‐life balance further compound the stress experienced by medical students. All these are not only experienced by domestic students but also by overseas medical students. Overseas medical students face unique stressors and challenges associated with studying abroad. Adapting to a new cultural and educational environment, adjusting to life away from home, and navigating language barriers can contribute to feelings of isolation, loneliness, and stress among overseas students. 40
Study results also showed gender differences in depression, anxiety, and stress that is endorsed by the previous research. 41 , 42 Societal norms and gender roles surrounding femininity, including the pressure to balance academic success with traditional roles as caregivers and homemakers, may contribute to heightened levels of psychological distress among female medical students. Moreover, relationship between study year, age, and mental health outcomes may vary throughout their academic journey. 25 In the early years of medical school, students often experience adjustment issues related to the transition from pre‐medical education to the rigorous demands of the medical curriculum. The first year, in particular, may be characterized by stressors such as academic workload, adjustment to new learning environments, and social integration challenges. As students' progress throughtheir medical education, the intensity and complexity of coursework typically increase, potentially leading to heightened levels of stress, anxiety, and depression in later study years. 43 Clinical rotations and clerkships in the later years of medical school may introduce additional stressors, including long working hours, patient care responsibilities, and high‐stakes examinations.
Students from lower SES backgrounds may encounter additional stressors related to financial constraints, limited access to resources, and lack of social support, which can exacerbate feelings of anxiety and depression. 44 , 45 Conversely, students from higher SES backgrounds may have access to greater support networks and coping resources, buffering them against the adverse effects of stress. Although smoking has been noted as important vulnerable factor for mental disorder, we found it as a risk for depression and anxiety among overseas students. This observation warrants further studies among domestic undergraduate medical students. Among domestic medical students in Bangladesh, the demanding nature of medical education, coupled with high levels of academic pressure and competition, may lead some students to turn to smoking as a maladaptive coping mechanism for managing stress and anxiety. 46 On the contrary, overseas medical students engage in smoking behavior as a response to stress and anxiety arising from transition to a new cultural and academic environment, coupled with homesickness and social isolation. Research suggests that domestic and overseas medical students who smoke may be at increased risk of experiencing symptoms of depression and anxiety. 47 Smoking behavior may exacerbate existing mental health issues or serve as a form of self‐medication to alleviate psychological distress. Additionally, social factors, such as peer pressure and exposure to smoking within social circles, may contribute to the initiation and maintenance of smoking habits among medical students.
4.1. Implications of the study
The present study sheds light on the complex interplay between various sociodemographic factors and mental health outcomes within the context of Bangladesh. Factors such as socioeconomic status, gender, and age can interact with each other to influence an individual's susceptibility to depression, anxiety, and stress. By acknowledging these intersecting factors, healthcare providers and policymakers can develop more nuanced and inclusive approaches to supporting student mental health. It is important to consider that most of the risk factors identified in this study have been known beforehand among undergraduate medical students. This study replicated the findings and made a comparison between domestic and overseas students.
The findings of this study have implications for the broader medical community in Bangladesh. Medical professionals are not immune to mental health challenges, and addressing the well‐being of medical students is essential for fostering a resilient and empathetic healthcare workforce. By prioritizing student mental health, medical colleges can cultivate a culture of support, empathy, and self‐care within the medical community, ultimately improving patient care and outcomes.
4.2. Limitation
To the best of the authors' knowledge, this is the first attempt to compare the psychological burden and associated factors in terms of depression, anxiety, and stress among Bangladeshi and international students. However, several limitations should be considered while generalizing the study results. First, the study was conducted in a single private medical school in Bangladesh. So, the inclusion of other medical schools from different parts of the country may reveal a different scenario. Second, DASS‐21 is a screening tool. Therefore, the psychological burden may be different if diagnostic interviews or diagnostic tools are used. Third, data were collected through a self‐reporting approach which may be a source of bias considering the over‐ and under‐estimation of psychological distress.
5. CONCLUSIONS
The study revealed higher rates of depression, anxiety, and stress among overseas undergraduate medical students enrolled in a private medical school of Bangladesh. Implementing targeted interventions and support systems can mitigate the negative impacts of mental health problems on medical students. Medical schools should implement measures, such as mental health awareness programs, accessible counseling, peer support groups, and stress management workshops to help students, especially overseas ones overcome psychological distress. However, further studies can be conducted to measure the issues more precisely.
AUTHOR CONTRIBUTIONS
Md Khayrul Islam: Conceptualization; methodology; investigation; data curation; supervision; project administration; writing—original draft; writing—review and editing. Md Golam Kibria: Writing—original draft; writing—review and editing; formal analysis; data curation. Rizwana Amin: Writing—original draft; writing—review and editing. Tasnia Ishaque Sharna: Data curation; writing—original draft; writing—review and editing. Samsun Nahar: Writing—original draft; writing—review and editing; data curation. S. M. Yasir Arafat: Writing—original draft; writing—review and editing.
CONFLICT OF INTEREST STATEMENT
Arafat, S.M. Yasir is an Editorial Board member of Health Science Reports. and a coauthor of this article. To minimize bias, they were excluded from all editorial decision‐making related to the acceptance of this article for publication.
TRANSPARENCY STATEMENT
The lead author S. M. Yasir Arafat affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ACKNOWLEDGMENTS
The authors have no funding to report.
Islam MK, Kibria MG, Amin R, Sharna TI, Nahar S, Arafat SMY. Rate and sociodemographic correlates of depression, anxiety, and stress among domestic and overseas medical students: a cross‐sectional observation from a private medical college in Bangladesh. Health Sci Rep. 2024;7:e70024. 10.1002/hsr2.70024
DATA AVAILABILITY STATEMENT
Data will be provided on query to the corresponding author. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Peng P, Hao Y, Liu Y, et al. The prevalence and risk factors of mental problems in medical students during COVID‐19 pandemic: A systematic review and meta‐analysis. J Affect Disord. 2023;321:167‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention (CDC) . Vital signs: current cigarette smoking among adults aged ≥18 years with mental illness ‐ United States, 2009‐2011. MMWR Morb Mortal Wkly Rep. 2013;62(5):81‐87. [PMC free article] [PubMed] [Google Scholar]
- 3. Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:21‐27. [DOI] [PubMed] [Google Scholar]
- 4. Cuttilan AN, Sayampanathan AA, Ho RC. Mental health issues amongst medical students in Asia: a systematic review [2000−2015]. Ann Transl Med. 2016;4(4):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abdulghani HM, AlKanhal AA, Mahmoud ES, Ponnamperuma GG, Alfaris EA. Stress and its effects on medical students: a cross‐sectional study at a college of medicine in Saudi Arabia. J Health Popul Nutr. 2011;29(5):516‐522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pokhrel NB, Khadayat R, Tulachan P. Depression, anxiety, and burnout among medical students and residents of a medical school in Nepal: a cross‐sectional study. BMC Psychiatry. 2020;20(1):298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross‐sectional study. Med Educ. 2005;39(6):594‐604. [DOI] [PubMed] [Google Scholar]
- 8. Pacheco JP, Giacomin HT, Tam WW, et al. Mental health problems among medical students in Brazil: a systematic review and meta‐analysis. Rev Brasil Psiquiatria. 2017;39(4):369‐378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jafari N, Loghmani A, Montazeri A. Mental health of medical students in different levels of training. Int J Prev Med. 2012:S107‐S112. [PMC free article] [PubMed] [Google Scholar]
- 10. Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80:1613‐1622. [DOI] [PubMed] [Google Scholar]
- 11. Miller PM, Surtees PG. Psychological symptoms and their course in first‐year medical students as assessed by the Interval General Health Questionnaire (I‐GHQ). Br J Psychiatry. 1991;159:199‐207. [DOI] [PubMed] [Google Scholar]
- 12. National Institute of Mental Health . What is depression? 2011. http://www.nimh.nih.gov/health/publications/depression/what-causes-depressio.shtml
- 13. Marcus M, Yasamy MT, Ommeren MV, et al. Depression: A Global Public Health Concern. Vol 1. Department of Mental Health and Substance Abuse, WHO; 2012:6‐8. http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf [Google Scholar]
- 14. Chand SP, Marwaha R. Anxiety. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK470361/ [PubMed] [Google Scholar]
- 15. Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, Halpert JA. Stressors and child and adolescent psychopathology: moving from markers to mechanisms of risk. Psychol Bull. 2003;129(3):447‐466. [DOI] [PubMed] [Google Scholar]
- 16. Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293‐319. [DOI] [PubMed] [Google Scholar]
- 17. Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students' depression at one medical school. Acad Med. 1997;72(6):542‐546. [DOI] [PubMed] [Google Scholar]
- 18. Tsegay L, Shumet S, Damene W, Gebreegziabhier G, Ayano G. Prevalence and determinants of test anxiety among medical students in Addis Ababa Ethiopia. BMC Med Educ. 2019;19:423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stewart SM, Lam TH, Betson CL, Wong CM, Wong AM. A prospective analysis of stress and academic performance in the first two years of medical school. Med Educ. 1999;33:243‐250. [DOI] [PubMed] [Google Scholar]
- 20. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354‐373. [DOI] [PubMed] [Google Scholar]
- 21. Tyssen R, Vaglum P, Grønvold NT, Ekeberg O. Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord. 2001;64(1):69‐79. [DOI] [PubMed] [Google Scholar]
- 22. Sadiq MS, Morshed NM, Rahman W, Chowdhury NF, Arafat S, Mullick M. Depression, anxiety, stress among postgraduate medical residents: a cross sectional observation in Bangladesh. Iran J Psychiatry. 2019;14(3):192‐197. [PMC free article] [PubMed] [Google Scholar]
- 23. Islam MA, Barna SD, Raihan H, Khan M, Hossain MT. Depression and anxiety among university students during the COVID‐19 pandemic in Bangladesh: A web‐based cross‐sectional survey. PLoS One. 2020;15(8):e0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hossain MM, Alam MA, Masum MH. Prevalence of anxiety, depression, and stress among students of Jahangirnagar University in Bangladesh. Health Sci Rep. 2022;5(2):e559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Faruk MO, Mamun MA, Siddique AB, et al. Risk factors for depression and anxiety disorders among Bangladeshi dental students: a cross‐sectional survey study. Int J Ment Health Addict. 2023;21(3):1501‐1514. [Google Scholar]
- 26. Jamilah A, Haque MI, Muhammad F, et al. Depression and associated factors among international students in a private university of Bangladesh. Glob Psychiatry. 2021;4(1):55‐61. [Google Scholar]
- 27. Kabir R, Isha SN, Chowdhury MTH, et al. Depression among the Non‐Native International Undergraduate Students Studying Dentistry in Bangladesh. Int J Environ Res Public Health. 2021;18(11):5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tareq SR, Likhon RA, Rahman SN, et al. Depression among medical students of Bangladesh. Mymensingh Med J. 2020;29(1):16‐20. [PubMed] [Google Scholar]
- 29. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335‐343. [DOI] [PubMed] [Google Scholar]
- 30. Roy N, Amin MB, Mamun MA, Sarker B, Hossain E, Aktarujjaman M. Prevalence and factors associated with depression, anxiety, and stress among people with disabilities during COVID‐19 pandemic in Bangladesh: a cross‐sectional study. PLoS One. 2023;18(7):e0288322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alim SMAHM, Mahbub‐E‐Kibria S, Islam MJ, et al. Translation of DASS 21 into bangla and validation among medical students. Bang J Psychiatry. 2014;28(2):67‐70. [Google Scholar]
- 32. Kibria MG, Kabir R, Rahman US, et al. Prevalence and factors associated with depression and anxiety among COVID‐19 survivors in Dhaka city. Front Psychiatry. 2024;15:1280245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chan YH. Biostatistics 202: logistic regression analysis. Singapore Med J. 2004;45(4):149‐153. [PubMed] [Google Scholar]
- 34. Chattu VK, Sahu PK, Seedial N, et al. Subjective well‐being and its relation to academic performance among students in medicine, dentistry, and other health professions. Educ Sci. 2020;10(9):224. [Google Scholar]
- 35. Al‐Bedaery R, Rosenthal J, Protheroe J, Reeve J, Ibison J. Primary care in the world of integrated care systems: education and training for general practice. Future Healthcare J. 2023;10(3):253‐258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jannatul H. Level of depression and anxiety among the students of University of Dhaka and Jahangirnagar University during Covid‐19 pandemic (Doctoral dissertation, Bangladesh Health Professions Institute, Faculty of Medicine, the University of Dhaka, Bangladesh). 2022.
- 37. Ashiq MAR, Gupta PS, Jubayer Biswas MAA, et al. Depression, anxiety, stress, and fear of COVID‐19 among Bangladeshi medical students during the first wave of the pandemic: a mixed‐methods study. Front Psychiatry. 2023;14:1142724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Biswas MAAJ, Hasan MT, Samir N, et al. The prevalence and associated factors of depressive symptoms among medical students in Bangladesh during the COVID‐19 pandemic: a cross‐sectional pilot study. Front Public Health. 2021;9:811345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hammoudi Halat D, Soltani A, Dalli R, Alsarraj L, Malki A. Understanding and fostering mental health and well‐being among university faculty: a narrative review. J Clin Med. 2023;12(13):4425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Iorga M, Soponaru C, Muraru ID, Socolov S, Petrariu FD. Factors associated with acculturative stress among International Medical Students. BioMed Res Int. 2020;2020:2564725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gao W, Ping S, Liu X. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J Affect Disord. 2020;263:292‐300. [DOI] [PubMed] [Google Scholar]
- 42. Curran E, Rosato M, Ferry F, Leavey G. Prevalence and factors associated with anxiety and depression in older adults: gender differences in psychosocial indicators. J Affect Disord. 2020;267:114‐122. [DOI] [PubMed] [Google Scholar]
- 43. Agyapong‐Opoku G, Agyapong B, Obuobi‐Donkor G, Eboreime E. Depression and anxiety among undergraduate health science students: a scoping review of the literature. Behav Sci. 2023;13(12):1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Buffel V, Wouters E, Cullati S, Tancredi S, Van Eeckert N, Van De Velde S. The relation between economic stressors and higher education students’ mental health during the initial outbreak of the COVID‐19 pandemic. Scand J Public Health. 2024;52(3):316‐328. [DOI] [PubMed] [Google Scholar]
- 45. Rahal D, Shaw ST, Stigler JW. Lower socioeconomic status is related to poorer emotional well‐being prior to academic exams. Anxiety Stress Coping. 2023;36(4):502‐518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jahrami H, AlKaabi J, Trabelsi K, et al. The worldwide prevalence of self‐reported psychological and behavioral symptoms in medical students: an umbrella review and meta‐analysis of meta‐analyses. J Psychosom Res. 2023;173:111479. [DOI] [PubMed] [Google Scholar]
- 47. Chkhaidze I, Maglakelidze N, Maglakelidze T, Khaltaev N. Prevalence of and factors influencing smoking among medical and non‐medical students in Tbilisi, Georgia. J Brasil Neumol. 2013;39(5):579‐584. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be provided on query to the corresponding author. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


