RESUME
Introduction: La polyarthrite rhumatoïde (PR) est souvent associée à des comorbidités notamment cardio-vasculaires. Les patients atteints de PR sont plus enclins à l’inactivité physique que la population générale. But: Notre étude visait à évaluer l'activité physique (AP) chez les patients atteints de PR et les obstacles qui l'influençaient parmi les caractéristiques de la PR.Méthodes: Nous avons mené une étude transversale sur 120 patients. Les comorbidités, les caractéristiques des patients, l’activité de la PR et son retentissement fonctionnel (Health Assessment Questionnaire (HAQ)) ont été évalués. L'AP a été évaluée par la version courte de l’International Physical Activity Questionnaire (IPAQ-S). Les facteurs influençant l'AP ont été analysés.Résultats: L'âge moyen était 56,1±10,1 ans avec un sex-ratio de 0,14. Les comorbidités notées étaient: hypertension artérielle (30,7%), diabète (18,4%) et obésité ou surpoids (71,1%). L’activité de la maladie était modérée à élevée chez 55,6% des patients. Le HAQ moyen était 0,9±0,6.La moyenne du score IPAQ-S continu était 4226,02±4703 MET-min/semaine. Le niveau d’activité physique (IPAQ-S catégorique) était faible chez 24,2% des patients, modéré chez 30,8% et élevé chez 45%.L'IPAQ-S continu était négativement corrélé avec l'âge (r=-0,18;p=0,045), l'âge de début de la maladie (r=-0,18;p=0,049) et le HAQ (r=-0,25;p=0,01). L'IPAQ-S catégorique était significativement associé au HAQ (p=0,03), l’hypertension artérielle (p=0,03) et la goutte (p=0,02).Conclusion: L’AP chez les patients atteints de PR peut apporter une amélioration significative de la qualité de vie et la fonction. Une AP régulière doit faire partie de la prise en charge de la PR.
ABSTRACT
Introduction: Rheumatoid arthritis (RA) is a chronic inflammatory disease frequently associated with comorbidities such as cardiovascular diseases. RA patients are more prone to physical inactivity than the general population. Aim: Our study aimed to evaluate physical activity (PA) in patients with RA and to assess barriers that influence it in RA characteristics. Methods: This was a cross sectional study of 120 RA patients. Comorbidities, patients’ characteristics, disease activity, function assessed by Health Assessment Questionnaire (HAQ), severity parameters, and extra-articular manifestations were assessed. PA was evaluated with the Short form of the International Physical Activity Questionnaire (IPAQ-S). Factors influencing PA were analyzed. Results: Mean age was 56.1±10.1 years and sex-ratio was 0.14. Screening for comorbidities showed that 30.7% of patients had hypertension, 18.4% had diabetes, and 71.1% were obese or overweight. Moderate to high disease activity was found in 55.6% of patients. Mean HAQ was 0.9±0.6. Evaluation of PA revealed that mean continuous IPAQ-S was 4226.02±4703 MET-min per week [0-24276]. Physical activity level (categorical IPAQ-S) was low in 24.2% of patients, moderate in 30.8%, and high in 45%. Continuous IPAQ-S was negatively correlated with age (r=-0.18,p=0.045), age of disease onset (r=-0.18,p=0.049), and HAQ (r=-0.25,p=0.01). Besides, categorical IPAQ-S was significantly associated with the presence of hypertension (p=0.03) and gout (p=0.02). Concerning RA parameters, categorical IPAQ-S was significantly associated with HAQ (p=0.03). Conclusion: Our study showed that PA in RA patients can provide significant improvement in terms of quality of life and function. In RA, regular PA should be part of disease management.
1. INTRODUCTION
Physical activity (PA) is defined as any bodily movement produced by skeletal muscles that result in energy expenditure (1). Under this broad concept, activities relating to leisure time, exercise, sports, locomotion, and work must be considered parts of PA.Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease. The main features of this disease are inflammatory peripheral arthritis and joint destruction leading to pain, functional limitation, and deformity. On the other hand, comorbidities are common among patients with RA, particularly those associated with mental health and cardio-vascular diseases (2).All of these effects, in addition to sarcopenia, contribute together to a decreased physical function and quality of life (2). PA has positive effects on comorbidities, pain, function, general well-being, and reduced mortality in general population (3–5). PA is increasingly promoted for patients with RA and strongly recommended (6). However, adherence to regular PA remains low. Identifying the barriers to PA is a key element to understanding PA behavior in RA. The determinants of PA are patient- related factors or environmental factors in the general population. In RA, there are also disease-related factors. For a better understanding of the relation between PA and RA, we aimed to evaluate the PA level in RA patients and to assess the impact of disease-related factors on PA among patients with RA.
2. METHODES
Study design
In this cross-sectional study, we recruited a sample of 120 patients with RA, who were scheduled for regular follow-ups in an outpatients and inpatients clinic in the rheumatology department in a 12-month period between May 2021 and April 2022.Subjects were eligible for this study if their ages were 18 years or older, who they had been diagnosed with RA according to the ACR/EULAR 2010 criteria, and able to walk, with no restriction for comorbidities
Participants
Socio-demographic data (age, gender, education level), comorbidities (diabetes, hypertension, dyslipidemia, obesity, coronary heart disease, gout, peripheral vessel disease, chronic obstructive pulmonary disease (COPD)), habits (smoking), and anthropometric measurements (body mass index (BMI)) were evaluated in all patients. Normal BMI was defined as per the World Health Organization as 18.5–24.9 kg/m2, overweight as 25–29.9 kg/m2, and obesity as ≥30 kg/m2.We collected the specific RA data : disease duration, age at disease onset, the presence of an atlantoaxial subluxation or a coxitis, and treatments (corticosteroids, conventional synthetic DMARDs (csDMARDs), biologic DMARDs (bDMARDs), pain intensity using the Visual Analog Scale (VAS), and disease activity via swollen and tender joint count and Disease Activity Score using 28 joints (DAS28-CRP) (a composite score for the evaluation of disease activity in RA (7), interpreted as follows: Remission <2.6, Low Disease Activity [2.6-3.1[, Moderate Disease Activity [3.1-5.1[, and High Disease Activity >=5.1). Physical function and disability were assessed by health assessment questionnaire (HAQ), a quantitative patient-reported outcome instrument designed to assess health-related quality of life and disability in RA patients (8). Laboratory tests included complete blood count, immunologic data and C-reactive protein (CRP) (mg/L) were also recorded.
Physical activity assessment
Self-reported levels of PA were collected hrough the International Short form of the Physical Activity Questionnaire (IPAQ-S) and were analyzed through the number of metabolic equivalent of task (MET) minutes per week (energy expended while performing various activities throughout the whole week) (9). To calculate MET minutes per week, the MET value given (e.g., walking= 3.3,) was multiplied by the minutes; the activity was carried out and again by the number of days that activity was undertaken. For example, if someone reports walking for 50 minutes 3 days a week then the total MET minutes for that activity is 3.3x50x3=495 MET-min per week. The levels of PA were categorized as low, moderate and high following the IPAQ scoring protocol (10):- Low PA level: patients who do not meet criteria for categories Moderate and High PA levels- Moderate PA level: patients with one of the following three criteria: • 3 or more days of vigorous activity of at least 20 minutes per day OR • 5 or more days of moderate-intensity activity or walking of at least 30 minutes per day OR• 5 or more days of any combination of walking, moderate-intensity or vigorous intensity activities achieving a minimum of at least 600 MET-min/week.- High PA level: patients with one of the following two criteria: • Vigorous-intensity activity on at least 3 days and accumulating at least 1500 MET-minutes/week OR• 7 or more days of any combination of walking, moderate-intensity or vigorous intensity activities achieving a minimum of at least 3000 MET-minutes/ week
Statistical analysis
Data were managed and analyzed with the software IBM SPSS Statistics version 11.5.Clinical and demographic findings were expressed as mean values ± standard deviation (SD) for continuous variables and as frequencies and percentages for categorical variables. Patients were divided into three groups: low PA, moderate PA, and high PA. Comparisons between these three groups were made with the chi-square test or Fisher’s exact test (categorical variables) and the Mann–Whitney test (continuous variables). The level of statistical significance was set at 5% (p<0.05) in all tests.
RESULTS
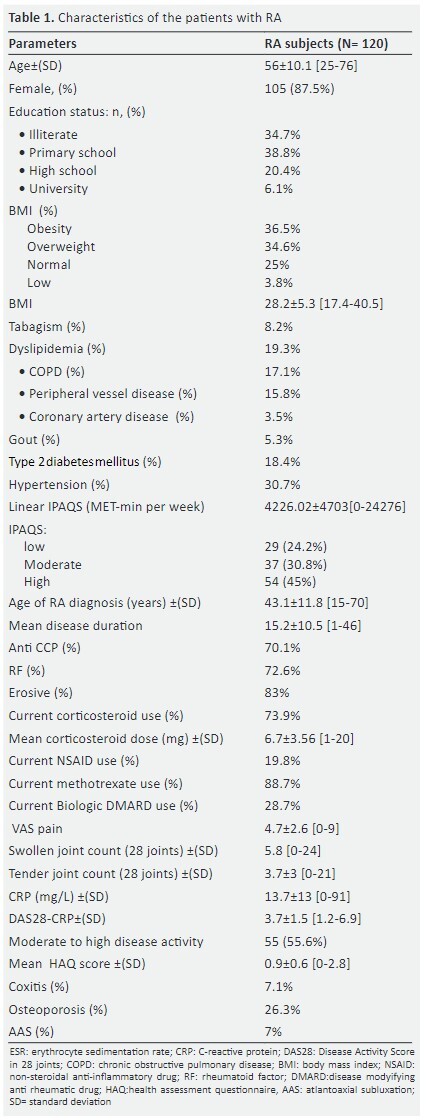
The study group consisted of 120 patients with RA. Mean age was 56.1±10.1 years and sex ratio (Male/Female) was 0.14. A screening of comorbidities showed that 71.1% of patients were obese or overweight and 30.7% had hypertension (Table 1).Mean age at the time of the RA diagnosis was 43.1±11.8 years and mean disease duration was 15.2±10.5 years [1-46]. RA was erosive in 83% of patients and seropositive 72.6% of cases. Mean DAS28-CRP was 3.7±1.5 [1.2-6.9]; 55.6% of patients had moderate to high disease activity. Mean HAQ was 0.9±0.6 [0-2.8]. Characteristics of RA patients are shown in table 1.
Physical activity assessment
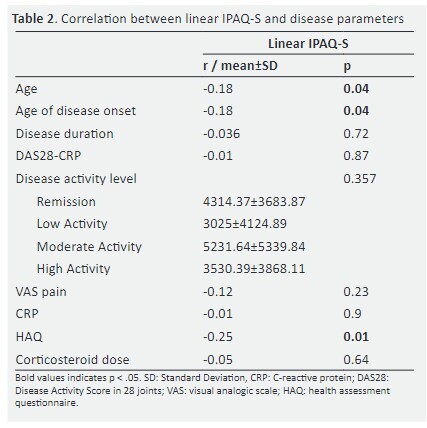
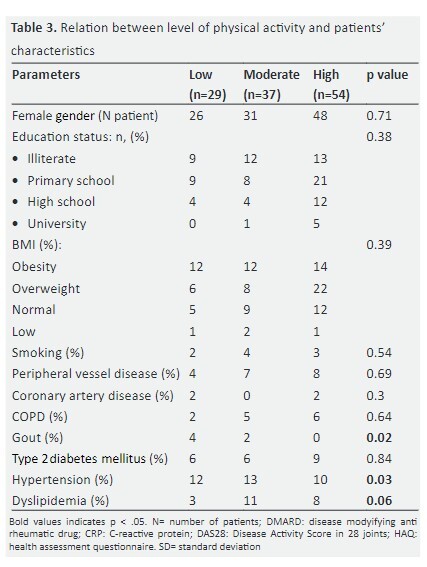
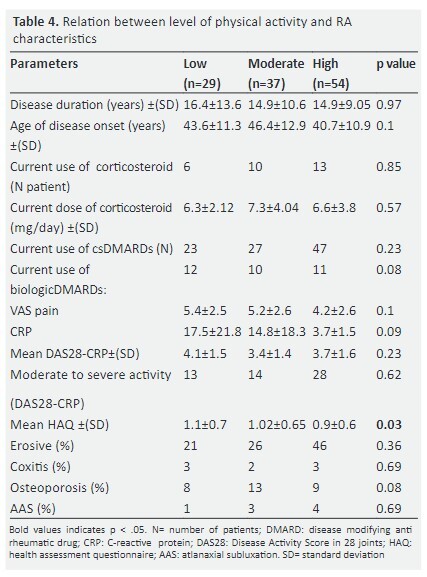
The evaluation of PA revealed that mean linear IPAQ-S was 4226.02±4703 MET-min per week [0-24276]. Based on IPAQ-S, PA level was considered low in 24.2% of patients, moderate in 30.8%, and high in 45% (Table1). The continuous IPAQ-S Was negatively correlated with age (r=-0.18, p=0.045), age of disease onset (r=-0.18, p=0.049), and functional assessment (HAQ) (r= -0.25, p=0.01) (Table 2). The categorical IPAQ-S IPAQ-S was divided in low, moderate or high PA and was significantly associated with patients’ related comorbidities (table 3). The presence of hypertension, gout, and dyslipidemia were associated with low PA, respectively: p=0.03; p=0.02, and p=0.06. Concerning the association between the categorical IPAQ-S and disease related-factors, PA level was low in RA patients with higher HAQ (p=0.03) (table4).
DISCUSSION
Our work evaluated the relationship between PA and RA, specifically the impact of joint inflammation, function impairment, and pain on the PA behavior in patients with this chronic rheumatic disease. This study evaluated PA levels of 120 patients through the IPAQ-S, and concluded that less than one third of our population had a low PA level. In fact, the continuous IPAQ-S was 4226.02±4703 MET-min per week ; PA level was low in 24.2% of patients, moderate in 30.8%, and high in 45%. IPAQ-S is considered the cheapest and easiest way to quickly compile PA data from a large number of people providing an assessment of PA by domains in patients with rheumatic diseases (11–13). IPAQ-S is a formal consensus for defining or describing levels of PA based on self–report population surveys. Although IPAQ-S has already been employed in clinical osteoarthritis trials, recently, this tool was used to evaluate PA patterns in inflammatory joint disorders such as RA. However, this score is a self-reporting and therefore subjective tool for PA assessment, possibly leading to an overestimation of PA level (14). Other alternatives to obtain an accurate measurement of PA can be used. They consist of assessing the total daily energy expenditure, such as the doubly-labeled water technique (15) or calorimetry (16), but these procedures are expensive and cumbersome.The precise measurement of PA is the key to study its association with diseases, but the assessment of PA is complex and it is conditioned by a balance between accuracy and ease of use (16). In RA, the central pathology is in the synovial membrane. The main manifestation of the disease is joint limitation. This, in addition to the fact that most RA patients also suffer from muscle loss, which contributes to decreased physical function and quality of life. Consequently, it has been assumed that RA patients are less active than the general population because of such joint manifestations. Besides, recent data suggest that disease activity influences negatively PA in RA patients (12, 17). In our study, the statistical analysis revealed that the continuous IPAQ-S was negatively correlated with age (r= -0.18, p=0.045), age of disease onset (r= -0.18, p=0.049), and functional assessment (HAQ) (r= -0.25, p=0.01) but there was no significant correlation with DAS28-CRP, CRP level, pain (VAS), erosions, or treatment. However, some studies indicated that PA levels have an inverse relationship with disease activity (as assessed by DAS28 or Simple Disease Activity Index (SDAI)) in RA patients (12,17–19). In these studies, accelerometry was sufficiently sensitive to detect PA changes related with disease activity both in RA patients who showed clinical improvements in response to treatment (17) and in patients who suffered from a disease flare (12). An additional factor that might have contributed to this inactivity tendency stems from recommendations, classically given by physicians, which restrict exercise due to concerns that excessive PA might aggravate both joint inflammation (9) and pain (10), and accelerate joint damage in RA patients. However, currently, evidence suggests that exercise has no deleterious effects either on disease activity or on joint damage (20, 21) and improves muscle strength in RA (22). A recent Spanish review supported the evidence of favoring the prescribing of PA for RA patients than there is against (23). Regular exercise with a moderate to high
352 level of intensity has proven to be effective in improving muscle strength and cardiovascular fitness in patients with chronic illnesses, including RA (20,24–26). A part from providing general health gains, also yield disease-specific benefits such as reduced pain, improved muscle function, and delayed onset of disability (21,27–29), without deleterious effects on joint (20, 21). In this regard, recently it has been suggested that RA patients who are physically active before clinical disease onset presented with a milder disease, both in terms of inflammation, pain, and function (30).In healthy populations, there is an inverse relationship between PA and cardiovascular risk factors such as BMI, body composition (increased whole body fat and visceral fat) (31), and blood lipid levels (32). Although different studies on the relationships between PA, BMI, fat mass, and lipid levels in RA populations have yielded controversial data (12, 33, 34). In our study, the presence of some comorbidities such as hypertension, gout, and dyslipidemia were associated with low PA, respectively: p=0.03; p=0.02 and p=0.06. The evidence clearly suggests that PA improves the cardiovascular risk profile in RA patients (12 , 24, 35). Among other factors contributing to physical inactivity, sarcopenia was associated with low PA levels (36). In fact, physical inactivity is one of the factors leading to sarcopenia with sarcopenia itself exacerbating physical inactivity. However, our work has some limitations: first, the evaluation of IPAQ-S is limited by subjectivity and less precision, but it is accessible, cheap, and the easiest way to quickly compile PA data from a large number of people providing an assessment of PA by domains. Second, there was no control group to see if there was a significant difference between RA patients and general population.
4. CONCLUSION
Our study showed that low PA levels in RA are associated with functional impairment and comorbidities. In RA, regular PA should be part of disease management. Health professionals must support and motivate RA patients by helping them to cope with the disease in a positive way and convince them to be more physically active to take
References
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep Wash DC 1974. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- Hill J, Harrison J, Christian D, et al. The prevalence of comorbidity in rheumatoid arthritis: a systematic review and meta-analysis. Br J Community Nurs. 2022 May 2;27(5):232–241. doi: 10.12968/bjcn.2022.27.5.232. [DOI] [PubMed] [Google Scholar]
- Almeida OP, Khan KM, Hankey GJ, Yeap BB, Golledge J, Flicker L. 150 minutes of vigorous physical activity per week predicts survival and successful ageing: a population-based 11-year longitudinal study of 12 201 older Australian men. Br J Sports Med. 2014 Feb;48(3):220–225. doi: 10.1136/bjsports-2013-092814. [DOI] [PubMed] [Google Scholar]
- Orrow G, Kinmonth AL, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012 Mar 26;344:e1389. doi: 10.1136/bmj.e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenson KR, Wen F, Herring AH. Associations of Accelerometry-Assessed and Self-Reported Physical Activity and Sedentary Behavior With All-Cause and Cardiovascular Mortality Among US Adults. Am J Epidemiol. 2016 Nov 1;184(9):621–632. doi: 10.1093/aje/kww070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters MJL, Symmons DPM, McCarey D, et al. EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis. 2010 Feb;69(2):325–331. doi: 10.1136/ard.2009.113696. [DOI] [PubMed] [Google Scholar]
- Van der Heijde DM, van ’t Hof MA, van Riel PL, et al. Judging disease activity in clinical practice in rheumatoid arthritis: first step in the development of a disease activity score. Ann Rheum Dis. 1990 Nov;49(11):916–920. doi: 10.1136/ard.49.11.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980 Feb;23(2):137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011 Oct 21;8:115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IPAQ scoring protocol International Physical Activity Questionnaire. 2023. [[cited 2023 Jun 25]]. https://sites.google.com/view/ipaq/score
- Metsios GS, Stavropoulos-Kalinoglou A, Treharne GJ, et al. Disease activity and low physical activity associate with number of hospital admissions and length of hospitalisation in patients with rheumatoid arthritis. [Jun 29];Arthritis Res Ther. 2011 13(3):R108. doi: 10.1186/ar3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Hernández V, Ferraz-Amaro I, Díaz-González F. Influence of disease activity on the physical activity of rheumatoid arthritis patients. [Apr];Rheumatol Oxf Engl. 2014 53(4):722–731. doi: 10.1093/rheumatology/ket422. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. [Aug];Med Sci Sports Exerc. 2003 35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Adams SA, Matthews CE, Ebbeling CB, et al. The effect of social desirability and social approval on self-reports of physical activity. [Feb 15];Am J Epidemiol. 2005 161(4):389–398. doi: 10.1093/aje/kwi054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerterp KR. Assessment of physical activity: a critical appraisal. [Apr];Eur J Appl Physiol. 2009 105(6):823–828. doi: 10.1007/s00421-009-1000-2. [DOI] [PubMed] [Google Scholar]
- Warren JM, Ekelund U, Besson H, et al. Assessment of physical activity - a review of methodologies with reference to epidemiological research: a report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. [Apr];Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol. 2010 17(2):127–139. doi: 10.1097/HJR.0b013e32832ed875. [DOI] [PubMed] [Google Scholar]
- Prioreschi A, Hodkinson B, Tikly M, McVeigh JA. Changes in physical activity measured by accelerometry following initiation of DMARD therapy in rheumatoid arthritis. [May];Rheumatol Oxf Engl. 2014 53(5):923–926. doi: 10.1093/rheumatology/ket457. [DOI] [PubMed] [Google Scholar]
- Prioreschi A, Hodkinson B, Avidon I, Tikly M, McVeigh JA. The clinical utility of accelerometry in patients with rheumatoid arthritis. [Sep];Rheumatol Oxf Engl. 2013 52(9):1721–1727. doi: 10.1093/rheumatology/ket216. [DOI] [PubMed] [Google Scholar]
- Prioreschi A, Hodkinson B, Avidon I, Tikly M, McVeigh JA. The clinical utility of accelerometry in patients with rheumatoid arthritis. [Sep];Rheumatol Oxf Engl. 2013 52(9):1721–1727. doi: 10.1093/rheumatology/ket216. [DOI] [PubMed] [Google Scholar]
- de Jong Z, Munneke M, Kroon HM, et al. Long-term follow-up of a high-intensity exercise program in patients with rheumatoid arthritis. Clin Rheumatol. 2009 Jun;28(6):663–671. doi: 10.1007/s10067-009-1125-z. [DOI] [PubMed] [Google Scholar]
- Plasqui G. The role of physical activity in rheumatoid arthritis. Physiol Behav. 2008 May 23;94(2):270–275. doi: 10.1016/j.physbeh.2007.12.012. [DOI] [PubMed] [Google Scholar]
- Van den Ende CH, Breedveld FC, le Cessie S, Dijkmans BA, de Mug AW, Hazes JM. Effect of intensive exercise on patients with active rheumatoid arthritis: a randomised clinical trial. Ann Rheum Dis. 2000 Aug;59(8):615–621. doi: 10.1136/ard.59.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Hernández MV, Díaz-González F. Role of physical activity in the management and assessment of rheumatoid arthritis patients. Reumatol Clin. 2017;13(4):214–220. doi: 10.1016/j.reuma.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Stavropoulos-Kalinoglou A, Metsios GS, Veldhuijzen van Zanten JJJCS, Nightingale P, Kitas GD, Koutedakis Y. Individualised aerobic and resistance exercise training improves cardiorespiratory fitness and reduces cardiovascular risk in patients with rheumatoid arthritis. Ann Rheum Dis. 2013 Nov;72(11):1819–1825. doi: 10.1136/annrheumdis-2012-202075. [DOI] [PubMed] [Google Scholar]
- Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009 May 20;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- De Jong Z, Munneke M, Zwinderman AH, et al. Is a long-term high-intensity exercise program effective and safe in patients with rheumatoid arthritis? Results of a randomized controlled trial. Arthritis Rheum. 2003 Sep;48(9):2415–2424. doi: 10.1002/art.11216. [DOI] [PubMed] [Google Scholar]
- Hurkmans E, van der Giesen FJ, Vliet Vlieland TP, Schoones J, Van den Ende ECHM. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. 2009 Oct 7;2009(4):CD006853. doi: 10.1002/14651858.CD006853.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurkmans E, van der Giesen FJ, Vliet Vlieland TP, Schoones J, Van den Ende ECHM. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. 2009 Oct 7;2009(4):CD006853. doi: 10.1002/14651858.CD006853.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabbaj SE, Rkain H, Benslama I, et al. Physical Activity and Rheumatoid Arthritis: Results from QUEST-RA Moroccan Study. Ann Rheum Dis. 2013 Jun 1;72(Suppl 3):A607–A607. [Google Scholar]
- Sandberg MEC, Wedrén S, Klareskog L, et al. Patients with regular physical activity before onset of rheumatoid arthritis present with milder disease. Ann Rheum Dis. 2014 Aug;73(8):1541–1544. doi: 10.1136/annrheumdis-2014-205180. [DOI] [PubMed] [Google Scholar]
- Bann D, Kuh D, Wills AK, et al. Physical activity across adulthood in relation to fat and lean body mass in early old age: findings from the Medical Research Council National Survey of Health and Development, 1946-2010. Am J Epidemiol. 2014 May 15;179(10):1197–1207. doi: 10.1093/aje/kwu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panagiotakos DB, Pitsavos C, Chrysohoou C, et al. Effect of leisure time physical activity on blood lipid levels: the ATTICA study. Coron Artery Dis. 2003 Dec;14(8):533–539. doi: 10.1097/00019501-200312000-00003. [DOI] [PubMed] [Google Scholar]
- Stavropoulos-Kalinoglou A, Metsios GS, Smith JP, et al. What predicts obesity in patients with rheumatoid arthritis? An investigation of the interactions between lifestyle and inflammation. Int J Obes 2005. 2010 Feb;34(2):295–301. doi: 10.1038/ijo.2009.220. [DOI] [PubMed] [Google Scholar]
- Elkan AC, Håkansson N, Frostegård J, Hafström I. Low level of physical activity in women with rheumatoid arthritis is associated with cardiovascular risk factors but not with body fat mass--a cross sectional study. BMC Musculoskelet Disord. 2011 Jan 14;12:13. doi: 10.1186/1471-2474-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metsios GS, Stavropoulos-Kalinoglou A, Panoulas VF, et al. Association of physical inactivity with increased cardiovascular risk in patients with rheumatoid arthritis. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Card Rehabil Exerc Physiol. 2009 Apr;16(2):188–194. doi: 10.1097/HJR.0b013e3283271ceb. [DOI] [PubMed] [Google Scholar]
- Moschou D, Krikelis M, Georgakopoulos C, et al. Sarcopenia in Rheumatoid arthritis. A narrative review. J Frailty Sarcopenia Falls. 2023 Mar 1;8(1):44–52. doi: 10.22540/JFSF-08-044. [DOI] [PMC free article] [PubMed] [Google Scholar]


