Abstract
Hydatid cyst disease, caused by the larval stage of Echinococcus granulosus, is a parasitic infection endemic in many regions, including South Asia. We present a case of a 36-year-old South Asian female with concurrent liver and peritoneal hydatid cysts, emphasizing the diagnostic challenges and management complexities associated with this condition. The patient presented with abdominal pain, nausea, and decreased appetite, and imaging studies revealed characteristic cystic lesions in the liver and peritoneum. Initial medical management with albendazole was followed by surgical excision due to inadequate response to therapy. Postoperative care included prophylactic albendazole to prevent recurrence. This case highlights the importance of a multidisciplinary approach involving medical therapy and surgical intervention tailored to the individual patient's needs and disease presentation.
Keywords: surgical management, peritoneal cyst, liver cyst, echinococcus granulosus, hydatid cyst
Introduction
Hydatid cyst disease, caused by the larval stage of the tapeworm Echinococcus granulosus, remains a significant public health concern in endemic regions worldwide, including South Asia. The parasite's life cycle involves canines as definitive hosts and herbivores as intermediate hosts, with humans incidentally becoming infected through ingestion of parasite eggs via contaminated food, water, or direct contact with infected animals [1]. Echinococcosis primarily affects the liver (70%) and lungs (20%), though it can manifest in any organ or tissue, termed as extrahepatic or extrapulmonary hydatid disease [2]. Intra-abdominal involvement, particularly in the peritoneum, is less common but can occur due to rupture or dissemination of hepatic cysts or direct infestation through the gastrointestinal tract [3].
Clinical manifestations of hydatid cyst disease vary widely from asymptomatic cysts discovered incidentally on imaging to symptomatic presentations such as abdominal pain, nausea, vomiting, and obstructive symptoms depending on the cyst's location, size, and complications [4]. Diagnosis relies on a combination of clinical suspicion, imaging studies (e.g., ultrasound, computed tomography), and serological tests (e.g., enzyme-linked immunosorbent assay) to confirm the presence of cystic lesions and identify specific antibodies against Echinococcus antigens [5]. Treatment strategies encompass medical therapy with benzimidazoles (e.g., albendazole, mebendazole) to reduce cyst viability and size, coupled with surgical intervention for large, symptomatic, or complicated cysts such as those causing mass effect, rupture, or secondary bacterial infection [6]. Surgical options range from cystectomy or pericystectomy to more conservative approaches like cyst puncture-aspiration-injection-reaspiration (PAIR) in select cases [7]. Given the chronicity and potential for recurrence, postoperative management includes long-term pharmacotherapy with albendazole to prevent cyst recurrence and close monitoring through imaging and serological testing to assess treatment efficacy and detect early relapse [8].
Case presentation
A 36-year-old South Asian female presented with a six-month history of intermittent abdominal pain localized to the right side. The pain was insidious in onset, gradually worsening, and non-radiating. She also reported nausea and decreased appetite but denied fever, vomiting, trauma, or significant medical history. On physical examination, her abdomen appeared scaphoid with a centrally placed umbilicus. There were no palpable masses, tenderness, guarding, or rigidity noted upon abdominal examination.
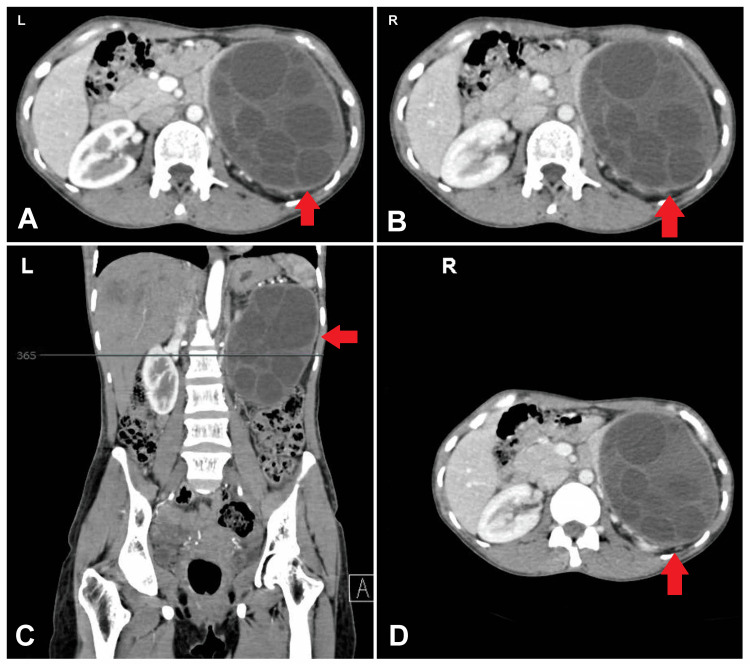
Initial investigations including routine blood tests were within normal limits. Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis revealed two significant findings: a well-defined cystic lesion with folded membranes in segment 7 of the liver, and a large cystic lesion with multiple daughter cysts located in the peritoneal cavity near the gastrosplenic region. The latter cyst measured 9.8 x 10.8 x 13.7 cm and was compressing the left kidney and the tail of the pancreas, closely abutting the splenic and left renal vessels (Figures 1A-1D).
Figure 1. (A-D) CECT abdomen shows cyst measured 9.8 x 10.8 x 13.7 cm and was compressing the left kidney and the tail of the pancreas, closely abutting the splenic and left renal vessels.
CECT: Contrast-enhanced computed tomography
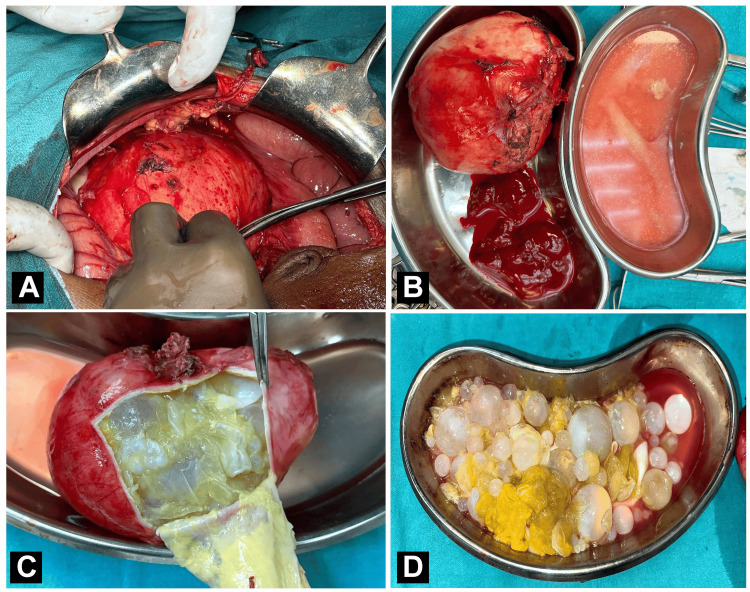
During the surgical procedure for excision of peritoneal and liver hydatid cysts, a midline vertical incision was made extending from the xiphisternum to 2 cm below the umbilicus. Careful layer-by-layer dissection of the peritoneum followed, ensuring meticulous attention to avoid damage to underlying structures. A large, approximately 13x12x6 cm hydatid cyst was identified within the lesser sac, densely adherent to the omentum, tail of the pancreas, transverse colon, and splenic hilum. The cyst was carefully dissected and mobilized along with its blood supply vessels, which were ligated and cut. Additionally, a 5x5 cm hydatid cyst located in segment 8 of the liver, containing daughter cysts, was excised using a cruciate incision and subjected to pericystectomy (Figures 2A-2D). Post-procedure, a thorough wash with 20% cetrimide-soaked saline was administered to prevent infection. The operation proceeded uneventfully, with no incidences of anaphylaxis reported.
Figure 2. (A) Intraoperative image of the peritoneal hydatid cyst procedure, (B) excised specimen of peritoneal hydatid cyst, and (C, D) peritoneal hydatid cyst showing daughter hydatid cyst.
Based on these imaging findings suggestive of hydatid cysts, the patient was initiated on medical management with albendazole (400 mg) for six weeks. However, follow-up ultrasound indicated no reduction in the size of the cysts, necessitating a surgical approach. The patient underwent an uneventful operative procedure for excision of the hydatid cysts in the liver and peritoneal cavity. Postoperatively, she received antibiotics, and analgesics, and was prescribed a prophylactic regimen of albendazole (400 mg PO BD for 21 days per cycle) to prevent recurrence of the parasitic infection.
The patient tolerated the surgical procedure well and was advised on postoperative care, including maintaining local hygiene at the suture site and avoiding heavy lifting. Regular follow-ups were scheduled to monitor her recovery and ensure treatment effectiveness. This case highlights the diagnostic challenges and management complexities associated with hydatid cyst disease, emphasizing the importance of a multidisciplinary approach involving medical therapy and surgical intervention tailored to the individual patient's needs and disease presentation.
Discussion
Hydatid cyst disease, caused by the larval stage of E. granulosus, remains a significant public health concern in endemic regions such as South Asia. This parasitic infection commonly affects the liver and occasionally spreads to other organs, including the peritoneum, lungs, and rarely the brain or bones [1]. The clinical presentation of hydatid cyst disease varies widely, ranging from asymptomatic cysts incidentally detected on imaging to severe complications such as rupture, infection, or compression of adjacent structures [9]. In our case, a 36-year-old South Asian female presented with symptoms consistent with liver and peritoneal involvement of hydatid cysts, including abdominal pain, nausea, and decreased appetite. Radiological imaging, particularly CECT, played a crucial role in confirming the diagnosis by identifying characteristic cystic lesions with daughter cysts, typical of hydatid disease [10].
Treatment strategies for hydatid cyst disease depend on several factors, including cyst size, location, and the presence of complications. Medical therapy with benzimidazoles like albendazole or mebendazole is often initiated to reduce cyst viability and prevent recurrence, although complete resolution of cysts through medical management alone can be challenging [6]. Surgical intervention remains the cornerstone for large or complicated cysts, as in our case, where the inadequate response to medical therapy and the risk of compressive symptoms necessitates surgical excision [11]. Surgical management of hydatid cysts aims to achieve complete cyst removal while minimizing the risk of intraoperative spillage and subsequent anaphylactic reactions. Postoperative care includes the administration of anthelmintics to prevent recurrence, as evidenced by our patient's prophylactic albendazole regimen [12]. Long-term follow-up is essential to monitor for recurrence or complications post-surgery, underscoring the chronic nature of this parasitic infection. The challenges in managing hydatid cyst disease are compounded by diagnostic delays, variability in cyst presentation, and the potential for cyst recurrence even after apparently successful treatment. Multidisciplinary collaboration involving infectious disease specialists, radiologists, and surgeons is crucial for optimal patient outcomes, ensuring timely diagnosis, appropriate treatment selection, and comprehensive postoperative care [13].
Conclusions
In conclusion, the case of hydatid cyst disease in our South Asian female patient underscores the diagnostic challenges and therapeutic complexities associated with this parasitic infection. The presentation involving both hepatic and peritoneal cysts highlights the varied clinical manifestations and the need for a multidisciplinary approach to management. While medical therapy with albendazole was initially attempted, surgical excision became necessary due to inadequate response and the risk of complications from cyst growth and compression of adjacent structures. Postoperative care, including prophylactic albendazole administration, aimed at preventing recurrence, reflects the chronic nature of hydatid disease and the importance of long-term follow-up. This case emphasizes the significance of timely diagnosis, individualized treatment strategies, and comprehensive postoperative management to optimize outcomes in patients with hydatid cyst disease.
Acknowledgments
I want to express my deep appreciation for the integral role of Artificial Intelligence (AI) in completing this research paper. The ChatGPT language model (OpenAI, San Francisco, CA) was employed to assist in the formulation of key arguments, structuring the content, and refining the language of our manuscript. It provided valuable insights and suggestions throughout the writing process, enhancing the overall coherence and clarity of the article. It was also utilized to assist in editing and rephrasing the work to ensure coherence and clarity in conveying the findings.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Srinivasa Reddy, Pankaj Gharde, Rajesh G. Gattani, Harshal Tayade, Darshana Tote, Nitesh Badwaik, Chahat Singh, Dheeraj P. Surya, Mihir Patil
Acquisition, analysis, or interpretation of data: Srinivasa Reddy, Pankaj Gharde, Rajesh G. Gattani, Harshal Tayade, Darshana Tote, Nitesh Badwaik, Chahat Singh, Dheeraj P. Surya, Mihir Patil
Drafting of the manuscript: Srinivasa Reddy, Pankaj Gharde, Rajesh G. Gattani, Harshal Tayade, Darshana Tote, Nitesh Badwaik, Chahat Singh, Dheeraj P. Surya, Mihir Patil
Critical review of the manuscript for important intellectual content: Srinivasa Reddy, Pankaj Gharde, Rajesh G. Gattani, Harshal Tayade, Darshana Tote, Nitesh Badwaik, Chahat Singh, Dheeraj P. Surya, Mihir Patil
Supervision: Srinivasa Reddy, Pankaj Gharde, Rajesh G. Gattani, Harshal Tayade, Darshana Tote, Nitesh Badwaik, Chahat Singh, Dheeraj P. Surya, Mihir Patil
References
- 1.Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Eckert J, Deplazes P. Clin Microbiol Rev. 2004;17:107–135. doi: 10.1128/CMR.17.1.107-135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Echinococcosis: a review. Moro P, Schantz PM. Int J Infect Dis. 2009;13:125–133. doi: 10.1016/j.ijid.2008.03.037. [DOI] [PubMed] [Google Scholar]
- 3.Diagnosis and treatment of uncomplicated hydatid cyst of the liver. Sayek I, Onat D. World J Surg. 2001;25:21–27. doi: 10.1007/s002680020004. [DOI] [PubMed] [Google Scholar]
- 4.Almulhim AM, John S. Treasure Island, FL: StatPearls Publishing; 2024. Echinococcus granulosus. [PubMed] [Google Scholar]
- 5.Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Brunetti E, Kern P, Vuitton DA. Acta Trop. 2010;114:1–16. doi: 10.1016/j.actatropica.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Albendazole in treatment of human cystic echinococcosis: 12 years of experience. Horton RJ. Acta Trop. 1997;64:79–93. doi: 10.1016/s0001-706x(96)00640-7. [DOI] [PubMed] [Google Scholar]
- 7.'No cyst, no echinococcosis': a scoping review update on the diagnosis of cystic echinococcosis after the issue of the WHO-IWGE Expert Consensus and current perspectives. Siles-Lucas M, Uchiumi L, Tamarozzi F. Curr Opin Infect Dis. 2023;36:333–340. doi: 10.1097/QCO.0000000000000941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clinical management of cystic echinococcosis: state of the art, problems, and perspectives. Junghanss T, da Silva AM, Horton J, Chiodini PL, Brunetti E. https://pubmed.ncbi.nlm.nih.gov/18784219/ Am J Trop Med Hyg. 2008;79:301–311. [PubMed] [Google Scholar]
- 9.Cystic hydatid disease: current trends in diagnosis and management. Sayek I, Tirnaksiz MB, Dogan R. Surg Today. 2004;34:987–996. doi: 10.1007/s00595-004-2830-5. [DOI] [PubMed] [Google Scholar]
- 10.Hydatid disease: radiologic and pathologic features and complications. Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Radiographics. 2000;20:795–817. doi: 10.1148/radiographics.20.3.g00ma06795. [DOI] [PubMed] [Google Scholar]
- 11.Percutaneous aspiration-injection-reaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Smego RA Jr, Bhatti S, Khaliq AA, Beg MA. Clin Infect Dis. 2003;37:1073–1083. doi: 10.1086/378275. [DOI] [PubMed] [Google Scholar]
- 12.Medical treatment of liver hydatidosis. Saimot AG. World J Surg. 2001;25:15–20. doi: 10.1007/s002680020003. [DOI] [PubMed] [Google Scholar]
- 13.Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. https://pubmed.ncbi.nlm.nih.gov/8789923/ Bull World Health Organ. 1996;74:231–242. [PMC free article] [PubMed] [Google Scholar]