Abstract
Objective:
Characterize college student COVID-19 behaviors and attitudes during the early pandemic.
Participants:
Students on two university campuses in Wisconsin.
Methods:
Surveys administered in September and November 2020.
Results:
Few students (3–19%) participated in most in-person activities during the semester, with eating at restaurants as the exception (72–80%) and attending work (35%) and parties (33%) also reported more frequently. The majority wore masks in public (94–99%), but comparatively fewer (42%) did so at parties. Mask-wearing at parties decreased from September to November (p < 0.05). Students attending parties, or consuming more alcohol, were less concerned and more likely to take COVID-19-associated risks.
Conclusions:
Students were motivated to adhere to COVID-19 prevention measures but gathered socially. Though there was frequent public masking, mask-wearing at parties declined in November and may represent pandemic fatigue. High-yield strategies for decreasing viral spread may include changing masking social norms and engaging with students about creative risk-reduction strategies.
Keywords: SARS-CoV-2, COVID-19, Universities, college campuses, college students, physical distancing, mask-wearing
Introduction
SARS-CoV-2, the virus that causes Coronavirus Disease 2019 (COVID-19), caused many universities in the United States to switch to virtual learning for the 2020 spring semester. Some college students returned to campus in August and September of 2020, coinciding with increasing COVID-19 cases among adolescents and young adults.1,2 As many activities typical of college life, including congregate living, in-person classes, extracurricular activities, and socialization in small and large groups, are known to potentiate COVID-19 spread, universities adopted various prevention approaches during the fall 2020 semester.3 Universal mask-wearing and physical distancing, strategies that prevent the spread of COVID-19 and were recommended for everyone in public, were also recommended for institutes of higher education.4–6 In July 2020, an executive order for a statewide face covering requirement was issued in Wisconsin, and was in place for the course of the fall semester.1
To date, the growing literature about COVID-19 and college campuses has explored the dynamics of viral spread7,8 and regular testing of students.9,10 Other studies have reported on the effects of the pandemic on student mental health11, alcohol12 and substance use, as well as attitudes toward COVID-19 vaccination.13 While knowledge and behavior toward COVID-19 has been investigated in the general U.S. population14, investigations that characterize university students’ attitudes and behaviors during the early pandemic months are limited. This study aimed to investigate and characterize these in the fall of 2020, when students at two universities in Wisconsin had just returned to campus after spring closing, and again at the end of the semester. This also represents a period before COVID-19 vaccination was available, when mitigation strategies such as masking and physical distancing were key tools in reducing spread of the virus. The students in this study were surveyed about activities, such as in-person class attendance, work and community work, extracurricular and social activities, as well as behaviors and attitudes related to COVID-19 (mask-wearing, mask-use types, and concern about contracting COVID-19). Since a subset of students were surveyed and both times, behaviors and attitudes could be compared at the start and end of the semester. We hypothesized that students who were more concerned about COVID-19 might be more likely to engage in mitigation behaviors.
Methods
Students at two universities in two different cities in Wisconsin were invited by email to complete surveys as a component of a larger serology investigation offered by a collaboration between the universities and the Centers for Disease Control and Prevention during September 1–11, 2020 and November 9–14, 2020. A subset of participants on each campus completed the survey at both timepoints. University A’s population is over 30,000 undergraduate students, while University B’s population is over 15,000 undergraduates.
At University A, all students in on-campus dormitory housing were invited to participate; at University B, students from both on-campus housing and from the population of students affiliated with sororities or fraternities were recruited to complete the surveys at the same time they participated in serology testing events. Students could participate in the end of semester survey independent of participation at the start of semester. Both universities allowed students to return to campus in person during the fall 2020 semester and instituted similar precautions against COVID-19 regarding universal masking in public, social distancing in public spaces, and made on-campus SARS-CoV-2 testing available. At University A, there were 6,164 students registered with campus housing; at University B, there were 2,187 students living in dorms and approximately 850 students from specific dorms were targeted by email to participate.
At University A, the surveys were completed electronically via Qualtrics; at University B, students answered the surveys in-person on paper. Questions about demographics, exposure history (“how many times have you been exposed”; “since the beginning of the semester, did you have any exposure to someone with confirmed COVID-19 infection?”), intended behaviors, frequency of substance use, and medical history were asked at the start of the semester; the end of semester survey was similar and included questions about reported behaviors, and additional items about COVID-19 attitudes and personal prevention practices over the semester.
Start and end of semester data were analyzed separately. We tested whether the null hypothesis was true—that there were no differences in frequencies of reported attitudes by select characteristics—for the end of the semester responses using chi-squared tests or Fisher’s exact test if there were cells with n < 5, based on a significance level of p < 0.05. For the cohort of students participating at both timepoints, start and end of semester survey responses were compared; McNemar’s test was used to compare whether the percentage of students answering activity and mask-wearing frequency questions changed from the start to the end of the semester, with statistical significance set at p < 0.05. Activity participation were dichotomous yes/no responses, and for mask-wearing and physician distancing answers were all/ most vs. some/rarely/never. Analyses were completed in SAS (version 9.4 software; SAS Institute).
This work was reviewed by ethical review boards at both universities, CDC, and the Wisconsin Department of Health Services, and was determined to be non-research as public health surveillance under federal law and CDC policy. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.2
Results
In total, 1,519 students participated in September (1,315 from University A; 204 from University B) and 844 students participated in November (631 from University A; 213 from University B). Of these, 237 students answered the survey at both timepoints (Figure 1). Students in September and November identified predominantly as female (60.3% and 66.8%), freshman (80.4% and 72.0%), and as White persons (86.1% and 85.3%), and as non-Hispanic or Latino (88.4% and 80.8%). More than half (61.0% in September; 58.9% in November) originated from Wisconsin. The majority (92.7% in September; 89.1% in November) lived on campus. About one-third of students surveyed had loans supporting their tuition (35.5% in September; 33.5% in November), most had a parent with a college degree or higher (78.1%; 72.4%), and approximately one-third were employed (33.2%; 37.7%). In September, 261 (19.4%) reported an underlying medical condition3; 155 students (23.4%) reported an underlying medical condition in November.
Figure 1.
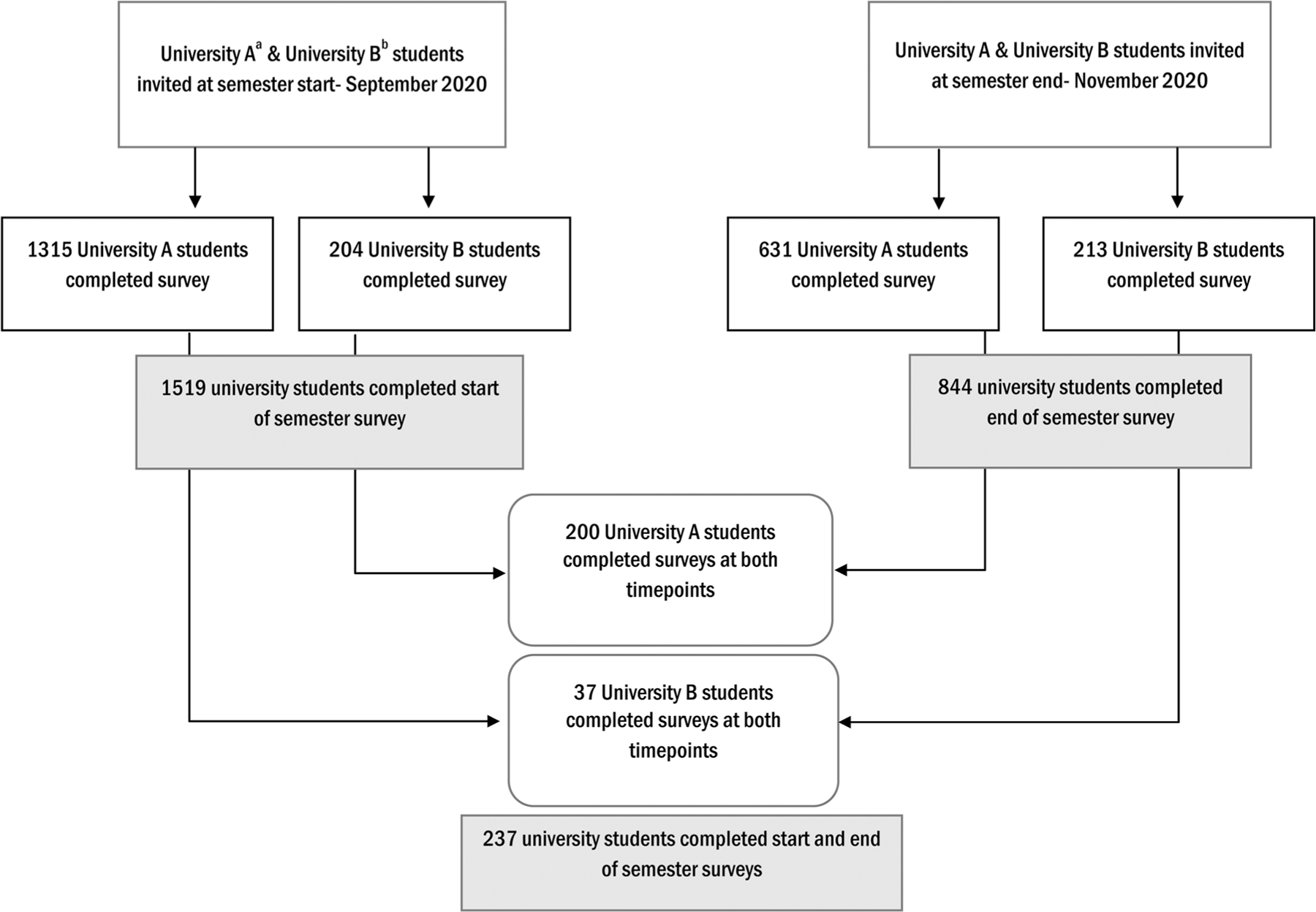
Flow of survey data collected at University A and University B in September and November 2020.aAt University A, 6,164 students were registered in on-campus dorms at start of semester and invited to participate.bAt University B, 2,187 students were registered in on-campus dorms at start of semester and approximately 850 of those in three of the dorms were invited to participate.
In September, a minority of students (207, 17.5%) reported a history of exposure to COVID-19 since January 2020. In November, more than half of students (454, 58.1%) reported a history of exposure during the semester; 437 (52.0% of participants) reported more than one exposure since January 2020 (Table 1).
Table 1.
Characteristics of students who participated in COVID-19 surveys at two universities in Wisconsin—fall 2020.
| Characteristic | Semester start* No. (%) | Semester end* No. (%) | Students completing survey at both start and end, No. (%) |
|---|---|---|---|
| Total | 1,519 | 844 | 237 |
| Sex5 | |||
| Male | 595 (39.2%) | 277 (33.1%) | 68 (28.7%) |
| Female | 916 (60.4%) | 560 (66.8%) | 169 (71.3%) |
| Other | 5 (0.3%) | 1 (0.1%) | 0 (0.0%) |
| Age, median (IQR) | 18 (18,18) | 18 (17,19) | 18 (18, 18) |
| Class year6 | |||
| Freshman | 1,221 (80.4%) | 601 (72.0%) | 194 (81.9%) |
| Sophomore | 136 (9.0%) | 110 (13.2%) | 18 (7.6%) |
| Junior | 86 (5.7%) | 55 (6.6%) | 9 (3.8%) |
| Senior | 71 (4.7%) | 64 (7.7%) | 16 (6.8%) |
| Grad student | 4 (0.3%) | 5 (0.6%) | 0 (0.0%) |
| Race | |||
| White | 1,308 (86.1%) | 720 (85.3%) | 169 (71.3%) |
| Black | 24 (1.6%) | 14 (1.7%) | 0 (0.0%) |
| Asian | 100 (6.6%) | 57 (6.8%) | 13 (5.5%) |
| Other races | 87 (5.7%) | 53 (6.3%) | 55 (23.2%) |
| Ethnicity | |||
| Hispanic/Latino | 89 (5.9%) | 43 (5.1%) | 12 (5.1%) |
| Non-Hispanic/Latino | 1,342 (88.4%) | 718 (85.1%) | 175 (73.8%) |
| Not specified or missing | 88 (5.8%) | 83 (9.8%) | 50 (21.1%) |
| Home state 7 | |||
| Wisconsin | 923 (61.0%) | 497 (58.9%) | 150 (63.3%) |
| Other/International | 590 (39.0%) | 347 (41.1%) | 87 (36.7%) |
| Housing location8 | |||
| On campus | 1,407 (92.7%) | 746 (89.1%) | 225 (94.9%) |
| Off campus | 84 (5.5%) | 74 (8.8%) | 9 (3.8%) |
| Sorority or fraternity | 27 (1.8%) | 17(2.0%) | 3 (1.3%) |
| Tuition source9 | |||
| Tuition supported by loans | 538 (35.5%) | 283 (33.5%) | 84 (35.6%) |
| Tuition supported by scholarship | 752 (49.6%) | 357 (42.3%) | 122 (51.7%) |
| Parent with college degree10 | 1,186 (78.1%) | 611 (72.4%) | 167 (70.5%) |
| Employed11 | 504 (33.2%) | 316 (37.7%) | 88 (37.1%) |
| Any underlying medical condition12 | 261 (19.4%) | 155 (23.4%) | 35 (17.7%) |
| Reported exposure to COVID-19 | |||
| Ever since January 2020 | 265 (17.5%) | – | 54 (22.8%) |
| Over course of semester (August-November 2020)13 | – | 454 (58.1%) | 124 (54.6%) |
| Exposed twice or more times since January 202014 | – | 437 (52.0%) | 115 (48.5%) |
At the end of the semester, the majority reported attending few or no classes in person during the semester (87.0%, Table 2). However, while most students also reported eating in and outside restaurants (80.1% and 72.5%), a minority reported participating in sports teams (11.3%), theater/music (2.6%), and work or community work (34.7%). One-third (278 students; 32.9%) reported attending house or dormitory parties, 140 students (16.6%) went to bars, and 90 students (10.7%) went to sorority/fraternity parties. Virtually all students reported owning cloth masks (98.2%), half owned surgical masks (53.4%) and 15.1% owned N-95 masks. In November, students reported wearing masks all or most of the time in public (shopping: 99.2%, in class: 99.2%, between class: 79.5%, in residence hallways: 91.9%, during extracurricular activities: 82.4% and, dining: 94.3%). At social events and parties, however, just 278 students (41.6%) reported mask wearing all or most of the time, and a similar proportion (260 students; 38.9%) reported wearing a mask not much or never at parties.
Table 2.
Reported activities and attitudes of students who participated in COVID-19 surveys at the semester’s end at two universities in Wisconsin- fall 2020
| In-person activity or attitude | Students reporting at semester end, No. (%) |
|---|---|
| Total participants | 844 |
| Class attendance in person15 | |
| All/most/half | 109 (13.0%) |
| Few/none | 730 (87.0%) |
| Ate in person at a restaurant | 676 (80.1%) |
| Ate outside at a restaurant | 612 (72.5%) |
| Work and/or community work | 293 (34.7%) |
| Sports team | 95 (11.3%) |
| Religious service | 82 (9.7%) |
| House/dorm party | 278 (32.9%) |
| Sorority/fraternity event | 156 (18.5%) |
| Sorority/fraternity party | 90 (10.7%) |
| Bar | 140 (16.6%) |
| Theater/music | 22 (2.6%) |
| Substance use | |
| Typically consume 3 or more drinks on average16 | 383 (50.5%) |
| Frequency of drinking on typical occasion17 | |
| Weekly or more | 413 (49.3%) |
| Less than weekly | 194 (23.2%) |
| Never | 231 (27.6%) |
| Vape or use electronic cigarettes18 | 153 (18.3%) |
| Smoke tobacco19 | 61 (7.3%) |
| COVID-19 level of concern20 | |
| Very concerned | 170 (20.2%) |
| Somewhat concerned | 372 (44.3%) |
| I was a little concerned | 215 (25.6%) |
| I wasn’t concerned at all | 83 (9.9%) |
| Reported COVID-19 preventive actionst | |
| I did everything I could to avoid infection | 224 (26.7%) |
| I was careful most of the time but not all the time | 533 (63.5%) |
| I took on risks on several occasions | 80 (9.5%) |
| I was trying to get infected | 3 (0.4%) |
| Mask ownership | |
| Cloth mask | 829 (98.2%) |
| Surgical mask | 451 (53.4%) |
| N-95 mask | 127 (15.1%) |
| Mask-wearing frequency by activity21 | |
| Shopping | 836 |
| All or most of the time | 829 (99.2%) |
| Half | 5 (0.6%) |
| Not much or never | 2 (0.2%) |
| In class | 627 |
| All or most of the time | 622 (99.2%) |
| Half | 0 (0.0%) |
| Not much or never | 5 (0.8%) |
| Between class | 726 |
| All or most of the time | 577 (79.5%) |
| Half | 83 (11.4%) |
| Not much or never | 66 (9.1%) |
| In residence hallways | 741 |
| All or most of the time | 675 (91.9%) |
| Half | 32 (4.3%) |
| Not much or never | 34 (4.6%) |
| Extracurriculars | 604 |
| All or most of the time | 498 (82.4%) |
| Half | 61 (10.1%) |
| Not much or never | 45 (7.5%) |
| Dining | 785 |
| All or most of the time | 740 (94.3%) |
| Half | 42 (5.4%) |
| Not much or never | 3 (0.4%) |
| Social events and parties | 669 |
| All or most of the time | 278 (41.6%) |
| Half | 131 (19.6%) |
| Not much or never | 260 (38.9%) |
Despite a range of attitudes about the level of concern regarding contraction of COVID-19 at the end of semester (very concerned: 20.2%, somewhat concerned: 44.3%, a little concerned: 25.6%, not concerned at all: 9.9%), student-reported preventive actions reflected that the majority did either everything they could to avoid infection (26.7%), or were careful most of the time: (63.5%) (Table 2).
A comparison of selected characteristics by level of concern and reported personal prevention strategy showed that a level of concern about COVID-19 varied significantly by party attendance- 24.6% of those who did not attend parties were very concerned about COVID-19 compared to those who attended parties (12.1%, p < 0.05); 32.9% of those not attending parties did everything they could to avoid infection compared to 15.2% of party attendees (p < 0.05). Among students who reported that they typically consumed more than three drinks on days they consumed alcohol, a smaller proportion (13.8%) was very concerned about COVID-19, compared with those consuming less than three drinks (25.6%, p < 0.05). Among students who reported mask-wearing all or most of the time at social parties and events, 27.0% were slightly or not concerned at all about COVID-19, while among students who masked not much or never at parties, 50.4% reported being slightly or not concerned about COVID-19 (p < 0.05). Of those who reported physical distancing all or most of the time in public, 4.4% reported taking risks on several occasions or more risks, while among those who physically distanced in public half the time or less, 21.1% reported taking more risks (p < 0.05) (Table 3).
Table 3.
Self-reported characteristics at the end of the semester at two universities in Wisconsin by student COVID-19 concern and personal prevention behaviors- fall 2020.
| Characteristic | COVID-19 Concern (No., row %) | COVID-19 Personal Prev ention (No., row %) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total students No. | Very concerned | Somewhat concerned | Only slightly concerned/I was not concerned at all | p-value22 | I did everything I could to avoid infection | I was careful most of the time, not all the time | I took risks on several occasions OR more frequent risks | p-valuev | |
| Party attendance23 | 840 | <0.05 | <0.05 | ||||||
| Attended parties | 296 | 36 (12.1%) | 123 (41.6%) | 137 (46.3%) | 45 (15.2%) | 192 (64.9%) | 59 (19.9%) | ||
| Did not attend parties | 544 | 134 (24.6%) (24.6%) | 249 (45.8%) | 161 (29.6%) | 179 (32.9%) | 341 (62.7%) | 24 (4.4%) | ||
| Alcohol consumption amount24 | 758 | <0.05 | |||||||
| Typically consume 3 or more drinks | 383 | 53 (13.8%) | 173 (45.2%) | 157 (41.0%) | 262 (68.4%) | 50 (13.1%) | 71 (18.5%) | <0.05 | |
| Consume less than 3 drinks | 223 | 57 (25.6%) | 98 (43.9%) | 68 (30.5%) | 64 (28.7%) | 151 (67.7%) | 8 (3.6%) | ||
| N/A | 152 | 43 (28.3%) | 68 (44.7%) | 41 (27.0%) | 79 (52.0%) | 71 (46.7%) | 2 (1.3%) | ||
| Wears mask at social events25 | 838 | <0.05 | |||||||
| All or most of the time | 278 | 68 (24.5%) | 135 (48.6%) | 75 (27.0%) | 109 (39.2%) | 162 (58.3%) | 7 (2.5%) | <0.05 | |
| Half the time | 131 | 27 (20.6%) | 50 (38.2%) | 54 (41.2%) | 13 (9.9%) | 105 (80.2%) | 13 (9.9%) | ||
| Not much or never | 260 | 21 (8.1%) | 108 (41.5%) | 131 (50.4%) | 24 (9.2%) | 176 (67.7%) | 60 (23.1%) | ||
| N/A | 169 | 54 (32.0%) | 78 (46.2%) | 37 (21.9%) | 77 (45.6%) | 89 (52.7%) | 3 (1.8%) | ||
| Physical distancing26 in public27 | 830 | <0.05 | |||||||
| All or most | 565 | 135 (23.9%) | 270 (47.8%) | 160 (28.3%) | 191 (33.8%) | 349 (61.8%) | 25 (4.4%) | <0.05 | |
| Half | 233 | 32 (13.7%) | 94 (40.3%) | 107 (45.9%) | 31 (13.3%) | 156 (67.0%) | 46 (19.7%) | ||
| Not much or never | 32 | 2 (6.3%) | 5 (15.6%) | 25 (78.1%) | 0 (0.0%) | 22 (68.8%) | 10 (31.3%) | ||
A subset of 237 students responded to the survey at both timepoints, and McNemar’s test was applied to compare whether there was a change between the proportions of students intending to participate in an activity/behavior (on the September survey) and those reporting activities/ behaviors (November survey). Overall, students planned to participate in more in-person activities during the semester than they actually reported at the end of the semester (Figure 2A); specifically, a larger percentage planned to work or do community work (64.1% in September; 33.3% in November, p < 0.05), participate in sports teams (35.9%; 11.8%, p < 0.05), and attend sorority/fraternity events (27.4%; 21.5%, p < 0.05). A larger proportion of students also reported physical distancing4 in public all or most of the time in September (72.8%) compared to physical distancing in November (62.5%, p < 0.05). In this group, consistent with the overall sample of students, mask-wearing all or most of the time was reported by the majority across all public activities (shopping, dining, extracurricular, in-person class) in both September and November, with the exception of social events and parties. At the start of the semester, 66.3% of students planned to wear masks all or most of the time at parties; by November, 38.1% reported wearing masks all or most of the time (p < 0.05). (Figure 2B, Supplemental Table).
Figure 2.
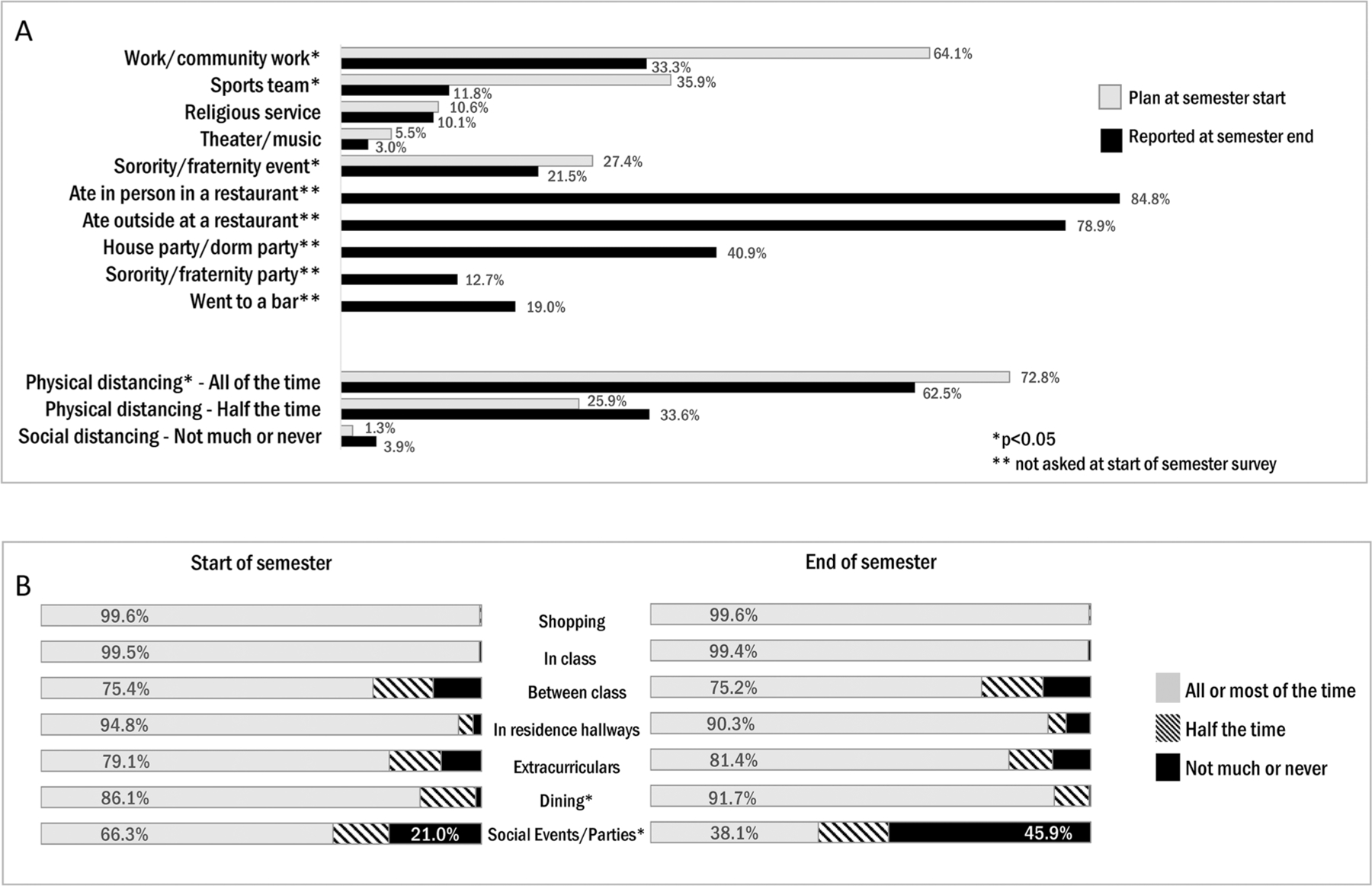
Comparison of intended and reported behaviors at the start of semester within cohort answering survey at two timepoints.A) Planned and reported activities and planned and reported frequency of physical distancing in public. B) Mask-wearing by activity start and end of semester.
Discussion
At two universities during the fall 2020 semester of the COVID-19 pandemic, students reported low in-person participation in typical college activities, frequent mask-wearing in public spaces, and motivation to adhere to preventive measures delineated by university and public health leadership in Wisconsin. Despite this, the decreased frequency of reported physical distancing and mask-wearing at social events at the end of the semester highlights the challenge of implementing mitigation measures in social settings among young people, as well as potential pandemic fatigue. Despite prevention strategies by the universities, and state policy aimed at decreasing spread, many students reported exposure, and both universities experienced COVID-19 outbreaks following student arrival on campus.15,16 While most students did not attend in-person class nor participate in other usual college activities – likely in part because universities offered limited in-person options—some students gathered socially and reported activities known to be highest-risk for COVID-19 transmission.17,18
Masks are a key component to decrease community COVID-19 spread5,19; observational studies have demonstrated that mask use on university campuses was higher in locations where masks were mandated compared to other spaces,20,21 but information about college student masking behaviors in nonpublic venues has been limited.22 This report found that students were mostly adherent to mask-wearing policies in public locations, which may have been in part due to state and university universal masking policies.17 However, the frequency of mask-wearing was comparatively lower for social gatherings and parties, which are more likely to be private gatherings. Notably, adherence to mask-wearing at social gatherings worsened by the end of the semester; among those surveyed in both September and November, the proportion reporting not masking at social events rose from 21% to 46%. Young adults may have felt peer pressure not to wear a mask in social settings, specifically.23 This report also found that students who reported higher risk behaviors (for example, greater amount of alcohol consumption) were less concerned about COVID-19 and also were more likely to report taking COVID-19 related risks. Similarly, those with less frequent mask-wearing at parties, and less frequent physical distancing in public reported a higher likelihood of engaging in behaviors that increased risk for contracting COVID-19. Binge-drinking behavior may be correlated with other risk-taking behaviors with negative consequences24; therefore, applying risk-reduction approaches that already exist on campus may be one strategy toward targeting behaviors more likely to increase risk of contracting COVID-19. Importantly, because there was also a correlation between reporting lower risk behaviors, more concern about COVID-19, and higher likelihood to engage in personal prevention practices to avoid infection, it appears that there is not a large knowledge gap – i.e. students were able to identify when they were engaging in risky behavior related to COVID-19. Therefore, focused efforts to reach students that may participate in higher risk behaviors through behavioral or environmental modifications, such as outdoor college-sponsored gatherings as opposed to indoor events, or other creative approaches25,26, might be more effective than informational campaigns.
Notably, comparing responses among the group who answered surveys at the start and the end of the semester, the proportion of respondents who physically distanced in public all or most of the time decreased from 73% to 62%; together with the smaller proportion who wore masks at social events by the end of semester, this suggests COVID-19 pandemic fatigue, a term that WHO defined as the expected and natural response to a prolonged public health crisis.27 Combatting COVID-19 pandemic fatigue and continuing to support students’ psychological well-being28 may result in improved prevention efforts on college campuses.
COVID-19 prevention is challenging on university campuses, where the young adult population has also been known to contribute to case increases in communities.15,23 Model-based evaluations found that a mandatory mask-wearing policy and extensive physical distancing would prevent most infections among students and faculty.29,30 How can universities best encourage these behaviors on campuses? The data from this analysis show that while high-risk activities (social gatherings, and less frequent mask-wearing at these events) occurred during fall 2020, it also showed students realized when they took COVID-19 related risks. While high-risk activities should be avoided as much as possible4, if students plan to participate in such events, a risk-reduction approach—mask-wearing, holding events that are small, outside or in well-ventilated spaces, encouraging receipt of COVID-19 vaccination31—to the greatest extent possible may reduce the spread of infection. This would be similar to strategies used to discourage other high-risk behaviors among young people and may work best.32 Creative, peer-led campaigns to shift social norms among students and capitalizing on delivering public health information via social media may be most effective in this population.33,34 Several studies found that students’ who received more social support reported better mental health and well-being35 and less alcohol consumption.36 As a group of public health experts stated in an open letter to university leadership in October 2020, engaging students in these public health interventions on university campuses may be the most effective approach to ensuring overall health and well-being for students and their communities.37
There are several limitations to this report. First, participants may have been particularly interested in learning their immunity status and therefore opted to take the survey, as the survey invitation was coupled with one to participate in serology testing. Given the non-representative nature of students completing the survey, selection bias may have occurred. Approximately 10–20% of students invited opted to participate and a direct comparison of demographics or other characteristics to the general, on-campus, University population is not possible. Second, the population participating was majority non-Hispanic White, female, and in the freshmen class, limiting generalizability to all U.S. university students; however, the subset of students surveyed at both timepoints, representing the start and end of semester groups, had closely comparable demographics and other survey responses to the overall start and end participating populations. Third, these findings are self-reported measures of behaviors and attitudes, as well as events that may be subject to incomplete recall. Survey participants were not given strict definitions of ‘COVID-19 exposure’. Social desirability bias may have influenced students’ responses to question related to COVID-19 prevention behaviors and the activities that they participated in. Additionally, these were not validated surveys. Fourth, responses from both universities were combined and no weighting was used to account for non-independence of responses within each university. Last, students’ self-rated prevention behaviors and risk-taking frequencies may have been influenced by past infection with COVID-19, and this was not accounted for in the investigation.
As we enter the third year of the COVID-19 pandemic, community levels vary in the United States.38 Continuing to encourage prevention measures against the spread of COVID-19 amidst the high-risk, in-person interactions that are possible on college campuses, and in the context of potential COVID-19 pandemic fatigue, will be critical.
Supplementary Material
Acknowledgments
We wish to thank Fatima Abdirizak, Rodel Desamu-Thorpe, Monique Foster, Clint Morgan, David Payne, Tarah Somers, Jeanne Ruff, John Paul Bigouette, Marie Killerby for their contributions.
Funding
This work was part of a public health investigation and was funded by the Centers for Disease Control and Prevention.
Footnotes
This work was authored as part of the Contributor’s official duties as an Employee of the United States Government and is therefore a work of the United States Government. In accordance with 17 USC. 105, no copyright protection is available for such works under US Law.
See e.g., 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
Conditions reported were asthma/reactive airway disease, cancer, cardiovascular disease, chronic lung disease, Crohn’s disease, fibromyalgia, hypertension, immunosuppressive condition or therapy, kidney disorder, liver disorder, obesity, transplant history
Survey question asked about “social distancing” defined in parentheses as “separation of minimum of 6 feet from others”
3 students did not reply at start of semester; 6 students did not reply at end of semester
9 students did not reply at end of semester
6 students did not reply at start of semester; 7 students did not reply at end of semester
1 student did not reply at start of semester
Students could select more than one source of tuition. 4 students did not reply to this question at start of semester
5 students did not reply at end of semester
This combined variable was derived from list of underlying medical conditions with option to select “yes”, “no” or “unknown”. 171 students did not reply at start of semester; 178 students did not reply at end of semester.
62 students did not reply at end of semester; 10 of these were in the cohort of students answering at both time points (third column)
4 students did not reply at end of semester
5 students did not reply to this question
86 students did not reply to this question
6 students did not reply to this question
8 students did not reply to this question
9 students did not reply to this question
4 students did not reply to this question
No. for each individual activity reflects the number of students participating in activity (those who answered N/A were eliminated from total)
p-values were calculated using χ2 tests
4 students did not reply to this question
86 students did not reply to this question
6 students did not reply to this question
Physical distancing = separation of minimum of 6 feet from others
14 students did not reply to this question Abbreviation: N/A = not applicable
Conflict of interest disclosure
The authors have no conflicts of interest to report. The authors confirm that the research presented in this article met the ethical guidelines, including adherence to the legal requirements, of the United States of America. This work was reviewed by ethical review boards at both universities, CDC, and the Wisconsin Department of Health Services, and was determined to be non-research as public health surveillance under federal law and CDC policy. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.
Publisher's Disclaimer: Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the CDC.
References
- 1.Salvatore PP, Sula E, Coyle JP, et al. Recent increase in COVID-19 cases reported among adults aged 18–22 Years—United States, May 31–September 5, 2020. MMWR Morb Mortal Wkly Rep 2020;69(39):1419–1424. doi: 10.15585/mmwr.mm6939e4.[ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boehmer TK, DeVies J, Caruso E, et al. Changing age distribution of the COVID-19 pandemic—United States, May-August 2020. MMWR Morb Mortal Wkly Rep 2020;69(39):1404–1409. doi: 10.15585/mmwr.mm6939e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walke HT, Honein MA, Redfield RR. Preventing and responding to COVID-19 on college campuses. JAMA 2020;324(17):1727– 1728. doi: 10.1001/jama.2020.20027/JAMA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. https://www.cdc.gov/coronavirus/2019-ncov/community/colleges-universities/considerations.html .
- 5.Brooks JT, Butler JC. Effectiveness of mask wearing to control community spread of SARS-CoV-2. JAMA 2021;325(10):998–999. JAMA doi: 10.1001/jama.2021.1505/J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strong social distancing measures in the united states reduced The COVID-19 growth rate. Health Affairs. 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- 7.Hamer DH, White LF, Jenkins HE, et al. Assessment of a COVID-19 control plan on an urban university campus during a second wave of the pandemic. JAMA Netw Open. 2021;4(6):e2116425. doi: 10.1001/jamanetworkopen.2021.16425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson SS, Jackson KC, Mietchen MS, Sbai S, Schwartz EJ, Lofgren ET. Excess risk of COVID-19 to university populations resulting from in-person sporting events. IJERPH. 2021;18(16):8260. doi: 10.3390/ijerph18168260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rennert L, McMahan C, Kalbaugh CA, et al. Surveillance-based informative testing for detection and containment of SARS-CoV-2 outbreaks on a public university campus: an observational and modelling study. Lancet Child Adolesc Health. 2021;5(6):428–436. doi: 10.1016/S2352-4642(21)00060–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schultes O, Clarke V, Paltiel AD, Cartter M, Sosa L, Crawford FW. COVID-19 testing and case rates and social contact among residential college students in Connecticut during the 2020–2021 academic year. JAMA Netw Open. 2021;4(12):e2140602. doi: 10.1001/jamanetworkopen.2021.40602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Copeland WE, McGinnis E, Bai Y, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2021;60(1):134–141.e2. doi: 10.1016/j.jaac.2020.08.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fruehwirth JC, Gorman BL, Perreira KM. The effect of social and stress-related factors on alcohol use among college students during the covid-19 pandemic. J Adolesc Health. 2021;69(4):557–565. doi: 10.1016/j.jadohealth.2021.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graupensperger S, Abdallah DA, Lee CM. Social norms and vaccine uptake: college students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine 2021;39(15):2060–2067. doi: 10.1016/j.vaccine.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Health Surveill. 2020;6(2):e19161. doi: 10.2196/19161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pray IW, Kocharian A, Mason J, Westergaard R, Meiman J. Trends in outbreak-associated cases of COVID-19—Wisconsin, March– November 2020. MMWR Morb Mortal Wkly Rep 2021;70(4):114–117. doi: 10.15585/mmwr.mm7004a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leidner AJ, Barry V, Bowen VB, et al. Opening of large institutions of higher education and county-level COVID-19 incidence— United States, July 6–September 17, 2020. MMWR Morb Mortal Wkly Rep 2021;70(1):14–19. doi: 10.15585/mmwr.mm7001a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guy GP Jr., Lee FC, Sunshine G, CDC Public Health Law Program, et al. Association of state-issued mask mandates and allowing on-premises restaurant dining with county-level COVID-19 case and death growth rates—United States, March 1–December 31, 2020. MMWR Morb Mortal Wkly Rep 2021;70(10):350–354. doi: 10.15585/mmwr.mm7010e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sami S, Turbyfill CR, Daniel-Wayman S, et al. Community transmission of SARS-CoV-2 associated with a local bar opening event—Illinois, February 2021. MMWR Morb Mortal Wkly Rep ePub: 5 April 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/masking-science-sars-cov2.html .
- 20.Barrios LC, Riggs MA, Green RF, et al. Observed Face Mask Use at Six Universities - United States, September-November 2020. MMWR Morb Mortal Wkly Rep Feb 12 2021;70(6):208–211. doi: 10.15585/mmwr.mm7006e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hutchins HJ, Wolff B, Leeb R, et al. COVID-19 Mitigation Behaviors by Age Group - United States, April-June 2020. MMWR Morb Mortal Wkly Rep 2020;69(43):1584–1590. doi: 10.15585/mmwr.mm6943e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen AK, Hoyt LT, Dull B. A Descriptive Study of COVID-19-Related Experiences and Perspectives of a National Sample of College Students in Spring 2020. J Adolesc Health. 2020;67(3):369–375. doi: 10.1016/j.jadohealth.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilson RF, Sharma AJ, Schluechtermann S, et al. Factors influencing risk for COVID-19 exposure among young adults aged 18–23 years—Winnebago County, Wisconsin, March-July 2020. MMWR Morb Mortal Wkly Rep 2020;69(41):1497–1502. doi: 10.15585/mmwr.mm6941e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krieger H, Young CM, Anthenien AM, Neighbors C. The epidemiology of binge drinking among college-age individuals in the United States. Alcohol Res 2018;39(1):23–30. [PMC free article] [PubMed] [Google Scholar]
- 25.https://www.cdc.gov/coronavirus/2019-ncov/community/colleges-universities/considerations.html Accessed 3/22/2022.
- 26.Lederer AM, Hoban MT, Lipson SK, Zhou S, Eisenberg D. More than inconvenienced: the unique needs of U.S. college students during the COVID-19 pandemic. Health Educ Behav 2021;48(1):14–19. doi: 10.1177/1090198120969372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. https://apps.who.int/iris/bitstream/handle/10665/335820/WHO-EURO-2020-1160-40906-55390-eng.pdf .
- 28. https://healthymindsnetwork.org/wp-content/uploads/2020/07/Healthy_Minds_NCHA_COVID_Survey_Report_FINAL.pdf .
- 29.Losina E, Leifer V, Millham L, et al. College campuses and COVID-19 mitigation: clinical and economic value. Ann Intern Med 2021;174(4):472–483. doi: 10.7326/M20-6558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goyal R, Hotchkiss J, Schooley RT, De Gruttola V, Martin NK. Evaluation of SARS-CoV-2 transmission mitigation strategies on a university campus using an agent-based network model. Clin Infect Dis 2021; doi: 10.1093/cid/ciab037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. https://www.acha.org/ACHA/About/ACHA_News/ACHA_Recommends_COVID-19_Vaccination_Requirements_for_Fall_2021.aspx .
- 32. https://www.acha.org/documents/resources/guidelines/ACHA_Considerations_for_Reopening_IHEs_for_Spring_2021.pdf .
- 33.Andrews JL, Foulkes L, Blakemore S-J. Peer influence in adolescence: public-health implications for COVID-19. Trends Cogn Sci 2020;24(8):585–587. doi: 10.1016/j.tics.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chesser A, Drassen Ham A, Keene Woods N. Assessment of COVID-19 knowledge among university students: implications for future risk communication strategies. Health Educ Behav. 2020 2020;47(4):540–543. [DOI] [PubMed] [Google Scholar]
- 35.Graupensperger S, Benson AJ, Kilmer JR, Evans MB. Social (Un) distancing: teammate interactions, athletic identity, and mental health of student-athletes during the COVID-19 pandemic. J Adolesc Health. 2020;67(5):662–670. doi: 10.1016/j.jadohealth.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav 2020;110(110):106527. doi: 10.1016/j.addbeh.2020.106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. https://www.insidehighered.com/views/2020/10/15/university-leaders-should-take-more-humane-approach-students-during-covid-19 .
- 38. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


