Abstract
Objective:
This study aimed to provide a comprehensive overview of the global burden of esophageal cancer (EC) and determine the temporal trends and factors influencing changes in the global burden.
Methods:
The latest incidence and mortality data for EC worldwide were obtained from GLOBALCAN 2022. The mortality and disability-adjusted life years (DALYs) rates for EC from 1990–2019 were sourced from the 2019 Global Burden of Diseases. Trends in EC mortality and DALYs attributable to 11 risk factors or clusters of risk were analyzed using the joinpoint regression model. The trends in age-related EC burden were assessed using a decomposition approach.
Results:
An estimated 511,054 new cases of EC were diagnosed in 2022 with 445,391 deaths worldwide. Approximately 75% of cases and deaths occurred in Asia. Nearly 50% of global EC deaths and DALYs were attributed to tobacco use in men in 2019, while 20% were attributed to high body mass index (BMI) in women. From 1990–2019, EC deaths and DALYs attributable to almost all risk factors had declining trends, while EC deaths and DALYs attributed to high BMI in men had upward trends. The age-related EC burden exhibited an upward trend driven by population growth and aging, which contributed to 307.4 thousand deaths and 7.2 million DALYs due to EC.
Conclusions:
The EC burden remains substantial worldwide. Effective tobacco and obesity control measures are critical for addressing the risk-attributable burden of EC. Population growth and aging pose challenges for EC prevention and control efforts.
Keywords: Esophageal cancer, incidence, mortality, disability-adjusted life years, risk factors, aging, trends
Introduction
Esophageal cancer (EC) is ranked as the 11th most common cancer and the 7th leading cause of cancer-related deaths worldwide1. Contributors to the EC burden include modifiable and non-modifiable risk factors2,3. Modifiable risk factors for EC include behavioral factors, such as smoking, alcohol consumption, and dietary habits, as well as metabolic factors, such as obesity3–7. EC is also associated with non-modifiable risk factors, such as aging. Trends in the EC burden are influenced by demographic shifts. Population aging contributes, in part, to the age-related burden of EC2,8. Monitoring these trends and understanding the contributors to the EC burden on a global scale is essential for the development and adaptation of targeted cancer prevention and control strategies, as well as for the rational allocation of public health resources.
Therefore, this study aimed to provide a comprehensive overview of the global burden of EC based on data from GLOBALCAN 20221,9, and to investigate the temporal trends and contributors influencing changes in the EC burden based on the comprehensive data from the 2019 Global Burden of Diseases study10. This study sought to offer insights into the adjustment and optimization of EC prevention and control policies.
Materials and methods
Data source
The global incidence and mortality rates for EC in 2022 were extracted from the GLOBOCAN 2022 database1,9. Age-standardized incidence rates (ASIRs) and age-standardized mortality rates (ASMRs) per 100,000 person-years were calculated based on the 1966 Segi-Doll World standard population11. GLOBALCAN 2022 is a project established by the International Agency for Research on Cancer, which enabled a comprehensive assessment of the cancer burden for 2022 in 185 countries or territories across 36 cancer types categorized by gender and age group. This assessment is based on the collection, aggregation, and estimation of national cancer registry data. The methodology adopted for estimating the incidence and mortality at the national level is described in detail elsewhere9,12. In brief, incidence and mortality rates were initially obtained from national or sub-national cancer registries for the most recent years and short-term prediction models were used to project the corresponding rates for 2022. In cases for which no reliable cancer registry data were available, incidence or mortality rates from neighboring countries were applied to estimate national incidence or mortality rates within the country.
The mortality and disability-adjusted life years (DALYs) rates for EC with population data from 1990–2019 were obtained from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 201910. The corresponding age-standardized rates were calculated using the GBD world population10. The GBD 2019 analysis provided a comprehensive evaluation of the global burden attributed to 369 diseases and injuries across 204 countries and territories. GBD 2019 conducted a systematic and scientifically rigorous assessment utilizing published, publicly accessible, and contributed data on disease and injury incidence, prevalence, and mortality rates. This meticulous analysis encompassed a thorough examination of a mutually exclusive and collectively exhaustive list of diseases and injuries. Access to all data relevant to this study is available to the public through the Global Health Data Exchange website (http://healthdata.org/).
The International Classification of Diseases (ICD-10) system was applied to define EC under the diagnosis codes, C15-C15.913.
Statistical analysis
Profiles of EC incidence and mortality in 2022
The number, crude rates, and age-standardized rates of EC incidence and mortality in 2022 were obtained from GLOBALCAN2022 by gender (both genders combined, and male and female separately), world regions, and four-tier human development index (HDI) regions1. The ASIR and ASMR were calculated using the 1966 Segi-Doll World Standard population for all ages11.
Trends in the modifiable risk-attributable EC burden from 1990–2019
The EC burden attributable to modifiable risk factors was assessed in terms of deaths and DALYs. Gender-specific deaths and DALYs rates, along with age-standardized rates for all age groups, were provided by the GBD 2019 dataset10. The age-standardized mortality and DALYs rates for all ages of EC attributable risk factors from 1990–2019 were extracted by gender (both genders combined, and male and female separately), GBD regions, and five-tier socio-demographic index regions. The age-standardized mortality and DALYs rates for EC attributable risk factors were calculated using the GBD standard population structure.
The hierarchy of risk factors for EC, according to the GBD comparative risk assessment, is as follows: level 0 includes all risk factors combined; level 1 encompasses behavioral and metabolic risk factors; level 2 includes 4 specific risks or clusters of risks [alcohol use, tobacco use, dietary risks, and high body mass index (BMI)]; and level 3 is comprised of 4 specific risks or clusters of risks (chewing tobacco, smoking, a diet low in fruits, and a diet low in vegetables)3. Table S1 is a comprehensive list of risk factors by hierarchy.
Trends in age-standardized mortality and DALYs rates attributable to these risk factors were assessed using the joinpoint regression model, implemented with joinpoint regression software (version 5.0.2) produced by the US National Cancer Institute14. The average annual percentage change (AAPC) from 1990–2019 was estimated to quantify changes in ASMRs and age-standardized DALYs rates (ASDRs) for EC. A P < 0.05 was considered statistically significant.
Trends in the non-modifiable age-related EC burden from 1990–2019
EC has been classified as an age-related disease with incidence rates among adults (≥ 25 years of age) exhibiting a quadratic increase with age, as indicated by the GBD study2. The number and crude mortality and DALYs rates for EC in 1990 and 2019 were extracted by gender (both genders combined, and male and female separately), age (25–95 years in 5-year increments and 95+ years), GBD regions, and 5-tier socio-demographic index regions. The corresponding age-standardized rates were calculated using the GBD standard population structure10. The age-related burden of EC encompasses the sum of all deaths and DALYs among adults (≥ 25 years of age). The changes in age-related EC deaths and DALYs from 1990–2019 were decomposed into 4 non-modifiable components (size of the adult population, age structure of the adult population, disease incidence or prevalence, and case fatality and disease severity). The deaths and DALYs associated with each of these four components contribute to the total changes in the age-related EC burden between 1990 and 2019. The decomposition of these four components is presented in the equation below:
In the equation, a represents the age group and y represents the year. The methodology for this analysis has been detailed elsewhere2,15–17. Additionally, we calculated the percentage change in deaths and DALYs attributable to the four components relative to the absolute deaths and DALYs in 1990. The ASMR and ASDR for EC in 1990 and 2019 were calculated using the GBD World Standard population for ages ≥ 25 years10.
All other analyses were performed using R (version 4.3.0). This study used only publicly available summary-level statistics and did not involve identifiable individual information.
Results
Profiles of EC incidence and mortality in 2022
Table 1 presents the global and regional incidence and mortality rates of EC for 2022 for both genders combined and separately for men and women. An estimated 511,054 new cases of EC were diagnosed globally with 365,225 in males and 145,829 in females. Additionally, 445,391 deaths from EC were estimated with 318,433 in males and 126,958 in females. Regionally, approximately 75% of both cases and deaths were estimated to occur in Asia, a significantly higher proportion than in any other continent. The ASIR and ASMR for EC were highest in Asia for both genders combined with an ASIR of 6.20/100,000 and an ASMR of 5.30/100,000. The lowest ASIR and ASMR were reported in Latin America and the Caribbean (2.40/100,000 and 2.20/100,000, respectively). The highest ASIR and ASMR for men were also reported in Asia (9.30/100,000 and 7.90/100,000, respectively) and the lowest ASIR and ASMR for men were reported in Latin America and the Caribbean (4.00/100,000 and 3.80/100,000, respectively). Conversely, women had the highest ASMR in Africa (2.90/100,000) and the lowest ASMR in North America (0.86/100,000). In contrast to other regions, the ASIR and ASMR for both genders were higher in Eastern Asia, Eastern Africa, South Africa, South Central Asia, and Northern Europe. The peak ASIR and ASMR were reported in Eastern Asia for males (12.20/100,000 and 9.70/100,000, respectively), while the peak ASIR and ASMR for females occurred in Eastern Africa (6.30/100,000 and 6.00/100,000, respectively).
Table 1.
Age-standardized incidence and mortality rates of esophageal cancer by world regions and four-tier HDI, 2022
| Region | Incidence | Mortality | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Both genders | Male | Female | Both genders | Male | Female | |||||||||||||
|
| ||||||||||||||||||
| Case | CIRa | ASIRb | Case | CIR | ASIR | Case | CIR | ASIR | Case | CMRc | ASMRd | Case | CMR | ASMR | Case | CMR | ASMR | |
| World | 511,054 | 6.50 | 5.00 | 365,225 | 9.20 | 7.60 | 145,829 | 3.70 | 2.60 | 445,391 | 5.70 | 4.30 | 318,433 | 8.00 | 6.50 | 126,958 | 3.30 | 2.20 |
| Continent | ||||||||||||||||||
| Africa | 29,965 | 2.10 | 3.60 | 16,722 | 2.40 | 4.30 | 13,243 | 1.90 | 3.00 | 28,276 | 2.00 | 3.50 | 15,765 | 2.20 | 4.20 | 12,511 | 1.80 | 2.90 |
| Latin America and the Caribbean | 20,366 | 3.10 | 2.40 | 15,493 | 4.70 | 4.00 | 4,873 | 1.40 | 0.98 | 18,895 | 2.80 | 2.20 | 14,466 | 4.40 | 3.80 | 4,429 | 1.30 | 0.88 |
| North America | 21,888 | 5.90 | 2.90 | 17,045 | 9.20 | 4.80 | 4,843 | 2.60 | 1.20 | 19,116 | 5.10 | 2.40 | 15,298 | 8.30 | 4.20 | 3,818 | 2.00 | 0.86 |
| Asia | 382,892 | 8.20 | 6.20 | 273,705 | 11.50 | 9.30 | 109,187 | 4.80 | 3.40 | 329,803 | 7.10 | 5.30 | 235,426 | 9.90 | 7.90 | 94,377 | 4.20 | 2.80 |
| Europe | 53,513 | 7.20 | 3.30 | 40,516 | 11.20 | 5.70 | 12,997 | 3.40 | 1.30 | 47,212 | 6.30 | 2.80 | 35,963 | 10.00 | 4.90 | 11,249 | 2.90 | 1.00 |
| Oceania | 2,430 | 5.60 | 3.30 | 1,744 | 8.00 | 5.10 | 686 | 3.10 | 1.60 | 2,089 | 4.80 | 2.70 | 1,515 | 6.90 | 4.30 | 574 | 2.60 | 1.30 |
| HDI | ||||||||||||||||||
| Very HDI country | 107,524 | 6.60 | 3.10 | 81,713 | 10.10 | 5.30 | 25,811 | 3.10 | 1.30 | 88,639 | 5.40 | 2.50 | 68,136 | 8.40 | 4.30 | 20,503 | 2.50 | 0.95 |
| High HDI country | 261,867 | 9.50 | 6.10 | 194,596 | 14.00 | 9.70 | 67,271 | 4.90 | 2.80 | 222,730 | 8.10 | 5.10 | 165,904 | 11.90 | 8.20 | 56,826 | 4.20 | 2.20 |
| Medium HDI country | 112,931 | 5.00 | 5.30 | 73,332 | 6.30 | 7.00 | 39,599 | 3.60 | 3.60 | 106,923 | 4.70 | 5.00 | 69,656 | 6.00 | 6.70 | 37,267 | 3.40 | 3.40 |
| Low HDI country | 28,588 | 2.40 | 4.30 | 15,485 | 2.50 | 4.90 | 13,103 | 2.20 | 3.70 | 26,967 | 2.20 | 4.10 | 14,645 | 2.40 | 4.70 | 12,322 | 2.10 | 3.50 |
| Region | ||||||||||||||||||
| Eastern Africa | 17,936 | 3.80 | 7.60 | 9,817 | 4.20 | 9.10 | 8,119 | 3.40 | 6.30 | 16,933 | 3.60 | 7.20 | 9,255 | 4.00 | 8.70 | 7,678 | 3.30 | 6.00 |
| Middle Africa | 2,617 | 1.40 | 2.90 | 1,676 | 1.80 | 3.90 | 941 | 0.99 | 2.00 | 2,480 | 1.30 | 2.80 | 1,562 | 1.60 | 3.80 | 918 | 0.96 | 2.00 |
| Northern Africa | 3,231 | 1.30 | 1.40 | 1,772 | 1.40 | 1.60 | 1,459 | 1.20 | 1.20 | 3,126 | 1.20 | 1.40 | 1,718 | 1.30 | 1.60 | 1,408 | 1.10 | 1.20 |
| South Africa | 3,621 | 5.20 | 6.30 | 2,098 | 6.20 | 8.50 | 1,523 | 4.30 | 4.60 | 3,321 | 4.80 | 5.90 | 1,947 | 5.70 | 8.20 | 1,374 | 3.90 | 4.20 |
| Western Africa | 2,560 | 0.60 | 1.20 | 1,359 | 0.64 | 1.30 | 1,201 | 0.57 | 1.20 | 2,416 | 0.57 | 1.20 | 1,283 | 0.60 | 1.30 | 1,133 | 0.54 | 1.10 |
| Caribbean | 1,758 | 4.00 | 2.80 | 1,319 | 6.10 | 4.60 | 439 | 2.00 | 1.30 | 1,625 | 3.70 | 2.60 | 1,230 | 5.70 | 4.20 | 395 | 1.80 | 1.10 |
| Central America | 1,959 | 1.10 | 0.97 | 1,427 | 1.60 | 1.60 | 532 | 0.57 | 0.46 | 1,755 | 0.96 | 0.86 | 1,301 | 1.40 | 1.40 | 454 | 0.48 | 0.39 |
| South America | 16,649 | 3.80 | 2.80 | 12,747 | 5.90 | 4.80 | 3,902 | 1.80 | 1.10 | 15,515 | 3.50 | 2.60 | 11,935 | 5.50 | 4.50 | 3,580 | 1.60 | 1.00 |
| North America | 21,888 | 5.90 | 2.90 | 17,045 | 9.20 | 4.80 | 4,843 | 2.60 | 1.20 | 19,116 | 5.10 | 2.40 | 15,298 | 8.30 | 4.20 | 3,818 | 2.00 | 0.86 |
| Eastern Asia | 248,384 | 15.40 | 7.60 | 186,824 | 22.70 | 12.20 | 61,560 | 7.70 | 3.40 | 203,035 | 12.60 | 5.90 | 153,056 | 18.60 | 9.70 | 49,979 | 6.30 | 2.50 |
| Southeastern Asia | 15,108 | 2.20 | 2.00 | 12,147 | 3.60 | 3.40 | 2,961 | 0.87 | 0.70 | 14,334 | 2.10 | 1.90 | 11,535 | 3.40 | 3.20 | 2,799 | 0.82 | 0.66 |
| South Central Asia | 114,956 | 5.60 | 5.80 | 72,433 | 6.80 | 7.30 | 42,523 | 4.30 | 4.20 | 108,482 | 5.30 | 5.50 | 68,712 | 6.50 | 6.90 | 39,770 | 4.00 | 4.00 |
| Western Asia | 4,444 | 1.50 | 1.70 | 2,301 | 1.50 | 1.80 | 2,143 | 1.60 | 1.60 | 3,952 | 1.40 | 1.50 | 2,123 | 1.40 | 1.70 | 1,829 | 1.30 | 1.30 |
| Eastern Europe | 17,102 | 5.90 | 3.20 | 13,690 | 10.00 | 6.10 | 3,412 | 2.20 | 0.95 | 15,551 | 5.30 | 2.80 | 12,590 | 9.20 | 5.60 | 2,961 | 1.90 | 0.79 |
| Western Europe | 17,325 | 8.80 | 3.80 | 13,101 | 13.50 | 6.10 | 4,224 | 4.20 | 1.70 | 14,801 | 7.50 | 2.90 | 11,198 | 11.60 | 4.90 | 3,603 | 3.60 | 1.20 |
| Southern Europe | 6,440 | 4.30 | 1.80 | 4,995 | 6.70 | 3.10 | 1,445 | 1.90 | 0.66 | 5,605 | 3.70 | 1.50 | 4,356 | 5.90 | 2.50 | 1,249 | 1.60 | 0.50 |
| Northern Europe | 12,646 | 11.80 | 5.00 | 8,730 | 16.50 | 7.60 | 3,916 | 7.20 | 2.60 | 11,255 | 10.50 | 4.10 | 7,819 | 14.80 | 6.40 | 3,436 | 6.30 | 2.10 |
| Australia-New Zealand | 2,151 | 7.00 | 3.30 | 1,554 | 10.10 | 5.10 | 597 | 3.80 | 1.60 | 1,828 | 5.90 | 2.70 | 1,341 | 8.70 | 4.30 | 487 | 3.10 | 1.10 |
| Melanesia | 249 | 2.20 | 3.30 | 161 | 2.70 | 4.30 | 88 | 1.60 | 2.30 | 233 | 2.00 | 3.10 | 147 | 2.50 | 4.10 | 86 | 1.50 | 2.30 |
| Polynesia | 21 | 3.00 | 2.70 | 20 | 5.70 | 5.20 | 1 | 0.29 | 0.27 | 19 | 2.70 | 2.40 | 18 | 5.10 | 4.70 | 1 | 0.29 | 0.27 |
| Micronesia | 9 | 1.60 | 1.50 | 9 | 3.20 | 3.00 | 0 | 0.00 | 0.00 | 9 | 1.60 | 1.50 | 9 | 3.20 | 3.00 | 0 | 0.00 | 0.00 |
HDI, human development index. aCIR, crude rate of incidence (per 100,000); bASIR, age-standardized incidence rate (per 100,000) was calculated using the Segi world standard population; cCMR, crude rate of mortality (per 100,000); dASMR, age-standardized mortality rate (per 100,000) was calculated using the Segi world standard population.
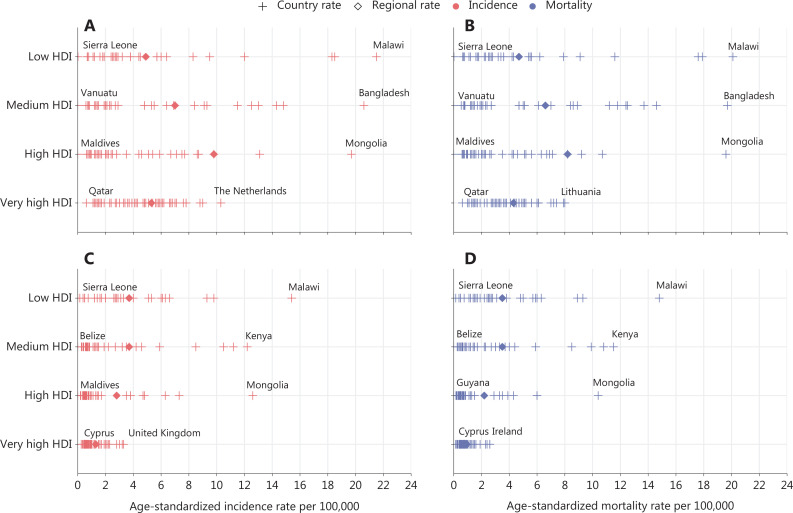
Figure 1 illustrates the country-level EC incidence and mortality rates by the 4-tier HDI in 2022. EC incidence patterns based on the 4-tier HDI differed between males and females. The ASIR and ASMR increased with decreasing HDI levels for women, ranging from 1.30/100,000 and 0.95/100,000 in countries with a very high HDI to 3.70/100,000 and 3.50/100,000 in countries with a low HDI. However, among men, the highest ASIR and ASMR were both reported in countries with a high HDI (9.70/100,000 and 8.20/100,000, respectively). Countries with a low HDI had the lowest ASIR (4.90/100,000), while countries with a very high HDI had the lowest ASMR (4.30/100,000).
Figure 1.
Country-level esophageal cancer incidence and mortality rates by four-tier HDI, 2022. (A) Country-level esophageal cancer incidence rates for males. (B) Country-level esophageal cancer mortality rates for males. (C) Country-level esophageal cancer incidence rates for females. (D) Country-level esophageal cancer mortality rates for females. HDI, human development index.
Profile and trends in the risk-attributable EC burden
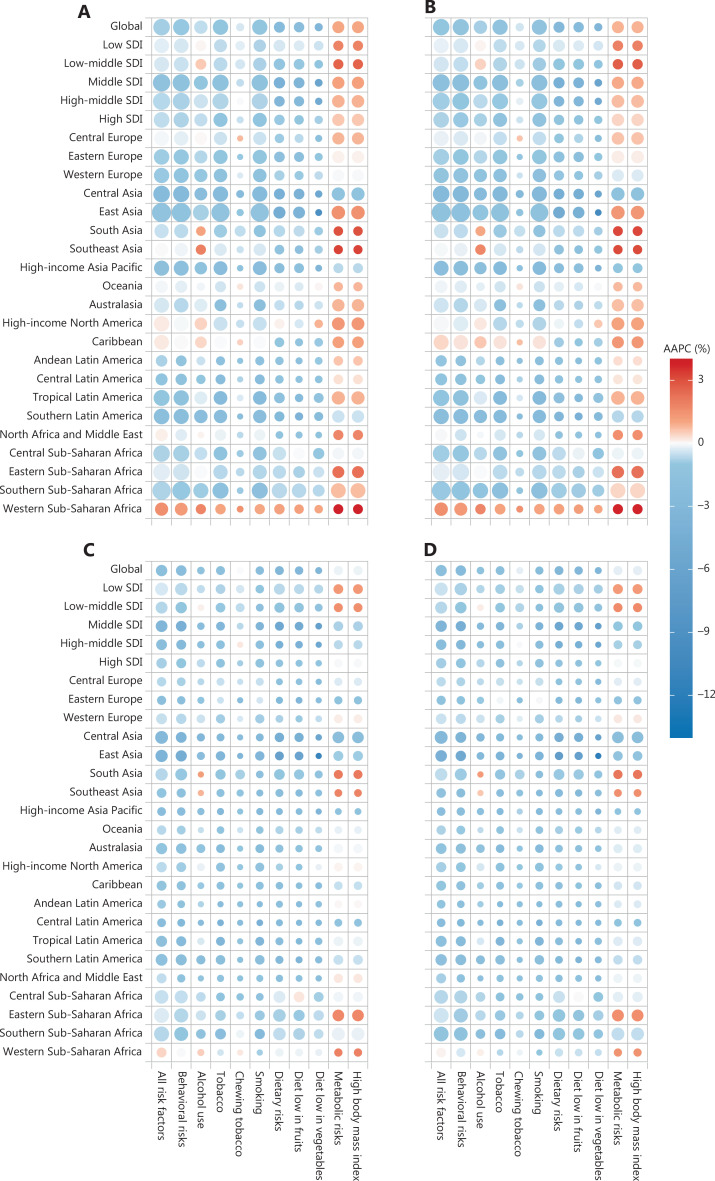
Figure 2, and Tables S2 and S3 illustrate the profiles and trends in risk-attributable deaths and DALYs for EC based on the SDI and GBD regions from 1990–2019. An estimated 339,546 EC deaths (68.2% of EC deaths) and 8,098,678 DALYs (69.4% of EC DALYs) were attributed to all risk factors in 2019. At level 2 of the risk factor hierarchy, nearly 50% of the global EC deaths and DALYs in men were attributed to tobacco use, while 20% were attributed to high BMI in women.
Figure 2.
Trends in risk for esophageal cancer incidence mortality and DALY rates for esophageal cancer by SDI and GBD regions, 1990–2019. The size of the point indicates a logarithmic transformation after normalization to age-standardized mortality and DALY rates. The color of the point indicates the average annual percent change of age-standardized mortality and DALY rates. (A) Trends in risk-attributable age-standardized mortality rates for males. (B) Trends in risk-attributable age-standardized DALY rates for males. (C) Trends in risk-attributable age-standardized mortality rates for females. (D) Trends in risk-attributable age-standardized DALY rates for females. DALY, disability-adjusted life-years; SDI, socio-demographic index; GBD, global burden of diseases; AAPC, average annual percent change.
In 2019 the leading level 2 risk factor globally for attributable EC deaths in males was tobacco (smoking and chewing), which accounted for 194.5 thousand deaths (53.2% of male EC deaths), followed by alcohol use, which accounted for 103.8 thousand deaths (28.4% of male EC deaths). The third largest level 2 risk factor for EC attributable deaths among males in 2019 was high BMI, with 65.5 thousand deaths (17.9% of male EC deaths), followed by dietary risks (a diet low in fruits and vegetables), accounting for 45.7 thousand deaths (12.5% of male EC deaths). However, there were significant differences between attributable deaths in males and females. In women, the level 2 risk factor ranking was high BMI, tobacco, dietary risks, and alcohol use, accounting for 18.4%, 16.3%, 15.2%, and 7.3% of female EC deaths in 2019, respectively. When considering DALYs, the ranking and proportion of DALYs attributed to each risk factor were similar to deaths. Tobacco ranked first for males and a high BMI was the leading cause for females with respect to attributable DALYs, accounting for 4.6 million and 0.5 million DALYs, respectively.
From 1990–2019, EC deaths and DALYs attributable to all risk factors exhibited a declining trend globally, except for deaths and DALYs attributed to a high BMI in men, which demonstrated an AAPC of 0.99% and 0.84% for ASMR and ASDR, respectively. For both men and women, esophageal cancer deaths and DALYs attributable to tobacco, alcohol, and dietary factors decreased in most regions. In contrast, deaths and DALYs attributable to a high BMI increased, especially in low-middle SDI regions. Notably, EC deaths and DALYs attributable to each risk factor increased among men in Western sub-Saharan Africa, and deaths and DALYs attributable to alcohol use also increased in South and Southeast Asia.
Profile and trends in the age-related EC burden
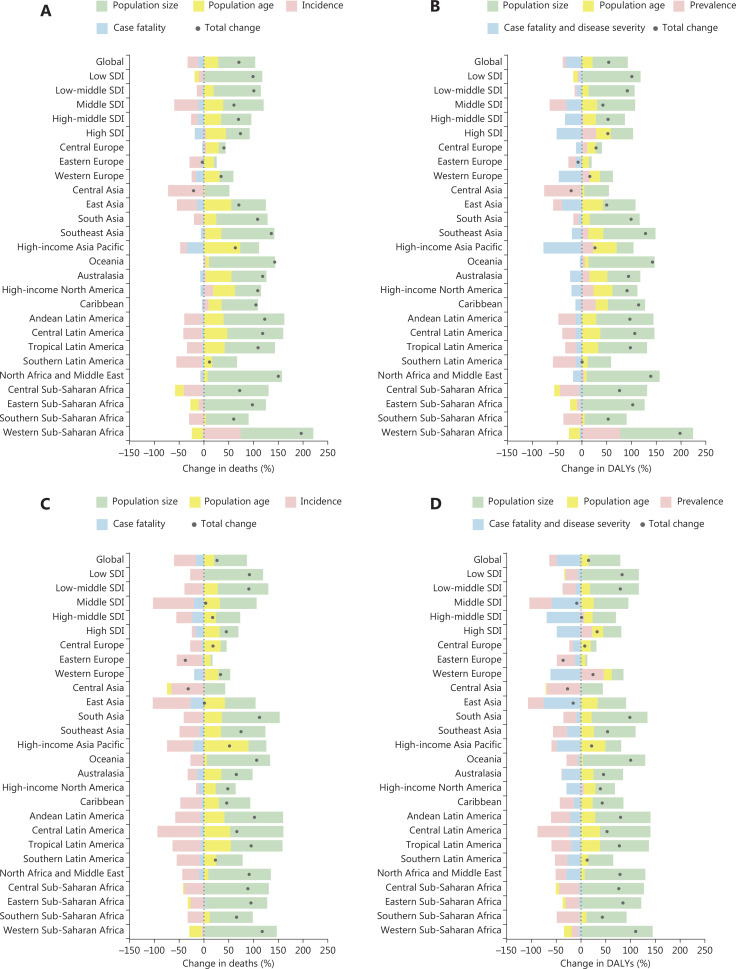
Figure 3, and Tables S4 and S5 depict the profile and trends in age-related deaths and DALYs for EC based on the SDI and GBD regions from 1990–2019. There were an estimated 497.7 thousand age-related EC deaths in 2019, which was defined as deaths occurring in adults ≥ 25 years of age, with 365.4 thousand deaths in males and 132.3 thousand deaths in females. Additionally, there were 11.6 million age-related EC DALYs with 8.8 million DALYs in males and 2.8 million DALYs in females.
Figure 3.
Decomposition of changes in age-related deaths and DALYs due to esophageal cancer between 1990 and 2019, by SDI and GBD regions. (A) Decomposition of changes in age-related deaths for males. (B) Decomposition of changes in age-related DALYs for males. (C) Decomposition of changes in age-related deaths for females. (D) Decomposition of changes in age-related DALYs for females. DALYs, disability-adjusted life-years; SDI, socio-demographic index; GBD, global burden of diseases.
The change in global age-related deaths and DALYs for EC were 56.1% and 42.3% of the absolute level in 1990, respectively. Decomposition analysis revealed that the contributors to the increased age-related EC burden during this time period were the adult population growth and population aging. Conversely, the decrease in case fatality rate and disease severity, as well as the incidence and prevalence of age-related EC, led to a decrease in age-related EC deaths and DALYs globally. The magnitude of change in age-related EC deaths in men across the SDI associated with population growth showed a decline ranging from 117.8% in countries with a low SDI to 47.9% in countries with a high SDI, while the magnitude of the change associated with the case fatality rate increased, ranging from −1.2% to −18.5.%. The change in age-related EC DALYs associated with population growth and population aging showed similar trends to deaths. In regions with a low SDI, population aging contributed to a decline in age-related EC deaths and DALYs in males with a −8.8% and −9.0% change, respectively. Age-related EC deaths in women showed almost no growth (3.6%) and DALYs decreased (−8.6%) in regions with a middle SDI, which were largely attributable to decreased incidence and prevalence. In regions with a high-middle SDI, age-related EC deaths and DALYs increased slightly in females (17.5% and 1.2%, respectively).
Discussion
This study presents the 2022 global incidence and mortality rates for EC by world region and HDI, and provides a comprehensive analysis of trends in risk-attributable and age-related EC deaths and DALYs by SDI and GBD regions from 1990–2019. The findings of this study provide an overview of the global epidemiology of EC and the changing patterns of attributable burden. These updated estimates of the global burden of EC provide crucial evidence for prioritizing policy-making and the development and acceleration of cancer control initiatives aimed at reducing the current and future burden of EC.
Approximately 511,100 new EC cases and 445,400 deaths occurred in 2022 with considerable variation across countries and regions. Approximately 75% of cases and deaths occurred in Asia, where 59.2% of the world’s population resides. The EC burden in the Asian regions is disproportionately greater than the corresponding population. EC primarily consists of two epidemiologically and pathologically distinct subtypes that share the same anatomic location [esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC)]18. High ASIRs and ASMRs were reported in Eastern Asia and Eastern Africa, which could be related to the predominant distribution of ESCC in Asia and Africa, with ESCC being the most prevalent histologic type of EC19. While ESCC was predominantly observed in Asian and African countries, EAC was predominantly found in countries in Europe and North America20. The burden of EC differs widely among countries and populations due to variations in risk factors and subtype distribution21. The main risk factors for EAC include obesity and metabolic syndrome, while the main risk factors for ESCC are more likely to be overconsumption of alcohol, dietary habits, such as low intake of fruits and vegetables, hot beverages, and pickled foods, and lower socioeconomic status7,18,22–29. Significant differences in the burden of EC between genders, with a greater burden in males, may be attributed to both biological differences and environmental factors. These factors include higher exposure to occupational risks, elevated levels of social stress, and unhealthy lifestyles among males. Gender disparities in the burden of EC may arise from the differential distribution of exposure factors between the genders.
EC is a complex, multifactorial disease influenced by various risk factors, which can be broadly categorized into behavioral, environmental, metabolic, and genetic factors. Behavioral risk factors include smoking, alcohol consumption, and dietary factors, including the consumption of pickled foods, a low intake of fruits and vegetables, and consumption of hot drinks. Smoking is the leading attributable risk factor for EC, accounting for 40.8% of all EC deaths. The proportion of EC deaths attributable to smoking is highest among men, representing 51.2% of all male EC deaths. This disparity may be associated with the substantially higher prevalence of smoking among men, which is often > 10-fold that among women in many Asian countries30. Dietary factors also significantly contribute to the risk of EC. Studies have demonstrated that the consumption of pickled foods and hot foods increases the risk of EC 2.10- and 1.90-fold, respectively31,32. This finding is further evidenced by the increased prevalence of EC in regions where such dietary habits are common, particularly in developing countries in Asia32. Environmental risk factors for EC include exposure to radiation and bitumen33. However, attributable deaths due to environmental risk factors were not analyzed due to the low prevalence in the population and the lack of sufficient data. Metabolic factors, especially obesity, have a crucial role in the development of EAC. Obese individuals have been shown to have a higher risk of EAC, with an odds ratio of approximately 1.5027. Biologically, visceral obesity may contribute to the pathogenesis of EAC by directly influencing the development of gastroesophageal reflux disease and Barrett’s esophagus. Moreover, visceral obesity can affect the progression of EAC through mechanisms independent of reflux, involving adipokines, growth factors, insulin resistance, and alterations in the microbiome26. Over the past four decades, there has been a significant increase in the global prevalence of obesity. Previous studies have reported a corresponding increase in the incidence of EAC, which may partly reflect the obesity epidemic34. The increasing trends in obesity are theorized to be significant contributors to the increased incidence of EAC. The global obesity epidemic may lead to a shift in the pathologic distribution pattern of EC35.
Demographic characteristics significantly influence the EC burden. As a chronic, non-communicable, age-related disease, changes in the population size and age structure can drive the burden of EC. The United Nations General Assembly declared 2021–2030 the United Nations Decade of Healthy Aging with an aim to foster global collaborative efforts to promote longer and healthier lives36. With increasing life expectancy, the pace of population aging is accelerating more rapidly than in previous times. Between 2015 and 2050, the proportion of the world’s population ≥ 60 years of age is projected to nearly double, increasing from 12% to 22%36. Greater than 90% of EC deaths occur in individuals > 50 years of age, with individuals > 70 years of age accounting for approximately 50% of all EC deaths37. Both incidence and mortality from EC are higher in older populations, and population aging contributes to an increased disease burden from EC. Our findings indicate that 24.1% and 18.5% of the increases in EC deaths and DALYs, respectively, between 1990 and 2019 were attributed to population aging. Population aging is thus poised to pose a significant challenge to the prevention and control of EC. Trends in the burden of EC are also influenced by economic development and advances in medical technology. With economic development and social progress, the population has witnessed rapid growth, leading to an increase in population size38. This growth in population size also contributes to the burden of EC. Our study found that 72.3% and 69.4% of the increases in EC deaths and DALYs, respectively, over the last three decades were attributed to population growth. In contrast, advances in medical technology have reduced the EC fatality rate, thereby mitigating the burden of EC.
This study had several notable strengths. Our study utilized representative data from GLOBALCAN 2022 and GBD 2019, which facilitated a comprehensive and systematic analysis of the profiles, trends, and contributors to the global burden of EC. However, there were also limitations to consider. First, our analysis was restricted to a limited number of risk factors, as described above. Second, cancer statistics inherently have a lag, and therefore only trends from 1990–2019 could be analyzed in this study.
Conclusions
This study aimed to provide a comprehensive understanding of the global burden of EC. The burden of EC remains substantial and shows an upward trend worldwide, particularly in males. Effective measures to control tobacco use and obesity are critical for addressing the risk-attributable burden of EC. Population growth and aging pose challenges for EC prevention and control efforts.
Supporting Information
Acknowledgements
We would like to express our gratitude to the staff of the International Agency for Research on Cancer and the Institute for Health Metrics and Evaluation, as well as their collaborators for compiling and making these valuable data publicly available.
Funding Statement
This study was funded by the National Natural Science Foundation of China (Grant No. 82273721) and Capital’s Funds for Health Improvement and Research (Grant No. 2024-1G-4023). The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Conflict of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the analysis: Yi Teng, Wanqing Chen.
Collected the data: Yi Teng.
Contributed data or analysis tools: Yi Teng.
Performed the analysis: Yi Teng.
Wrote the paper: Yi Teng, Changfa Xia, Maomao Cao, Fan Yang, Xinxin Yan, Siyi He, Mengdi Cao, Shaoli Zhang, Qianru Li, Nuopei Tan, Jiachen Wang, Wanqing Chen.
Data availability statement
All data used in this study are publicly available from the Global Cancer Observatory (GCO) [https://gco.iarc.fr] and the Global Burden of Disease Study 2019 [https://vizhub.healthdata.org/gbd-results/].
References
- 1.Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229–63. doi: 10.3322/caac.21834. [DOI] [PubMed] [Google Scholar]
- 2.Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. 2019;4:e159–67. doi: 10.1016/S2468-2667(19)30019-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thrift AP. Global burden and epidemiology of Barrett oesophagus and oesophageal cancer. Nat Rev Gastroenterol Hepatol. 2021;18:432–43. doi: 10.1038/s41575-021-00419-3. [DOI] [PubMed] [Google Scholar]
- 5.Tarazi M, Chidambaram S, Markar SR. Risk factors of esophageal squamous cell carcinoma beyond alcohol and Ssoking. Cancers (Basel) 2021;13:1009. doi: 10.3390/cancers13051009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheikh M, Poustchi H, Pourshams A, Etemadi A, Islami F, Khoshnia M, et al. Individual and combined effects of environmental risk factors for esophageal cancer based on results from the Golestan Cohort Study. Gastroenterology. 2019;156:1416–27. doi: 10.1053/j.gastro.2018.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qin X, Jia G, Zhou X, Yang Z. Diet and esophageal cancer risk: an umbrella review of systematic reviews and meta-analyses of observational studies. Adv Nutr. 2022;13:2207–16. doi: 10.1093/advances/nmac087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solary E, Abou-Zeid N, Calvo F. Ageing and cancer: a research gap to fill. Mol Oncol. 2022;16:3220–37. doi: 10.1002/1878-0261.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferlay J, Ervik M, Lam F, Laversanne M, Colombet M, Mery L, et al. Global cancer observatory: cancer today (version 1.1) Lyon, France: International Agency for Research on Cancer; 2024. [Google Scholar]
- 10.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doll R, Payne P, Waterhouse J. Cancer incidence in five continents - a technical report. 1st ed. Berlin: Springer; 1966. [Google Scholar]
- 12.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. 2nd ed. Geneva: World Health Organization; 2004. [Google Scholar]
- 14.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 15.Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl) 2022;135:584–90. doi: 10.1097/CM9.0000000000002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C, Chang Y, Ren J, Wu Z, Zheng Y, Luo Z, et al. Modifiable risk-attributable and age-related burden of lung cancer in China, 1990-2019. Cancer. 2023;129:2871–86. doi: 10.1002/cncr.34850. [DOI] [PubMed] [Google Scholar]
- 17.GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smyth EC, Lagergren J, Fitzgerald RC, Lordick F, Shah MA, Lagergren P, et al. Oesophageal cancer. Nat Rev Dis Primers. 2017;3:17048. doi: 10.1038/nrdp.2017.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Melina A, Isabelle S, Jacques F, David F. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015;64:381. doi: 10.1136/gutjnl-2014-308124. [DOI] [PubMed] [Google Scholar]
- 20.Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: risk factors, screening and endoscopic treatment in western and eastern countries. World J Gastroenterol. 2015;21:7933–43. doi: 10.3748/wjg.v21.i26.7933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morgan E, Soerjomataram I, Rumgay H, Coleman HG, Thrift AP, Vignat J, et al. The global landscape of esophageal squamous cell carcinoma and esophageal adenocarcinoma incidence and mortality in 2020 and projections to 2040: new estimates from GLOBOCAN 2020. Gastroenterology. 2022;163:649–58.e2. doi: 10.1053/j.gastro.2022.05.054. [DOI] [PubMed] [Google Scholar]
- 22.Yuan S, Chen J, Ruan X, Sun Y, Zhang K, Wang X, et al. Smoking, alcohol consumption, and 24 gastrointestinal diseases: Mendelian randomization analysis. Elife. 2023;12:e84051. doi: 10.7554/eLife.84051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014;371:836–45. doi: 10.1056/NEJMra1314704. [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez GM, DePuy D, Aljehani M, Bien J, Lee JSH, Wang DH, et al. Trends in epidemiology of esophageal cancer in the US, 1975-2018. JAMA Netw Open. 2023;6:e2329497. doi: 10.1001/jamanetworkopen.2023.29497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maomao C, He L, Dianqin S, Siyi H, Xinxin Y, Fan Y, et al. Current cancer burden in China: epidemiology, etiology, and prevention. Cancer Biol Med. 2022;19:1121–38. doi: 10.20892/j.issn.2095-3941.2022.0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elliott JA, Reynolds JV. Visceral obesity, metabolic syndrome, and esophageal adenocarcinoma. Front Oncol. 2021;11:627270. doi: 10.3389/fonc.2021.627270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi EK, Park HB, Lee KH, Park JH, Eisenhut M, van der Vliet HJ, et al. Body mass index and 20 specific cancers: re-analyses of dose-response meta-analyses of observational studies. Ann Oncol. 2018;29:749–57. doi: 10.1093/annonc/mdx819. [DOI] [PubMed] [Google Scholar]
- 28.Chen Q, Zhuang H, Liu Y. The association between obesity factor and esophageal caner. J Gastrointest Oncol. 2012;3:226–31. doi: 10.3978/j.issn.2078-6891.2012.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abnet CC, Arnold M, Wei WQ. Epidemiology of esophageal squamous cell carcinoma. Gastroenterology. 2018;154:360–73. doi: 10.1053/j.gastro.2017.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mackay J, Amos A. Women and tobacco. Respirology. 2003;8:123–30. doi: 10.1046/j.1440-1843.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- 31.Yan B, Zhang L, Shao Z. Consumption of processed and pickled food and esophageal cancer risk: a systematic review and meta-analysis. Bull Cancer. 2018;105:992–1002. doi: 10.1016/j.bulcan.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 32.Andrici J, Eslick GD. Hot food and beverage consumption and the risk of esophageal cancer: a meta-analysis. Am J Prev Med. 2015;49:952–60. doi: 10.1016/j.amepre.2015.07.023. [DOI] [PubMed] [Google Scholar]
- 33.International Agency for Research on Cancer. List of classifications by cancer sites with sufficient or limited evidence in humans. Lyon, France: International Agency for Research on Cancer; 2023. [Google Scholar]
- 34.Kroep S, Lansdorp-Vogelaar I, Rubenstein JH, Lemmens VE, van Heijningen EB, Aragonés N, et al. Comparing trends in esophageal adenocarcinoma incidence and lifestyle factors between the United States, Spain, and the Netherlands. Am J Gastroenterol. 2014;109:336–43. doi: 10.1038/ajg.2013.420. quiz 35, 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7:231–40. doi: 10.1016/S2213-8587(19)30026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. Ageing and health. Geneva: World Health Organization; 2022. [Google Scholar]
- 37.Lin L, Li Z, Yan L, Liu Y, Yang H, Li H. Global, regional, and national cancer incidence and death for 29 cancer groups in 2019 and trends analysis of the global cancer burden, 1990-2019. J Hematol Oncol. 2021;14:197. doi: 10.1186/s13045-021-01213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.United Nations. World population prospects 2022. New York, United States: United Nations; 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used in this study are publicly available from the Global Cancer Observatory (GCO) [https://gco.iarc.fr] and the Global Burden of Disease Study 2019 [https://vizhub.healthdata.org/gbd-results/].