Abstract
Sexually transmitted infections (STIs) caused by bacterial pathogens Chlamydia trachomatis, Neisseria gonorrhoeae, and Treponema pallidum present significant public health challenges. These infections profoundly impact reproductive health, leading to pelvic inflammatory disease, infertility, and increased susceptibility to other infections. Prevention measures, including antibiotic treatments, are limited by the often-asymptomatic nature of these infections, the need for repetitive and continual screening of sexually active persons, antibiotic resistance for gonorrhea, and shortages of penicillin for syphilis. While vaccines exist for viral STIs like human papillomavirus (HPV) and hepatitis B virus (HBV), there are no vaccines available for bacterial STIs. This review examines the immune responses in the female genital tract to these bacterial pathogens and the implications for developing effective vaccines against bacterial STIs.
Keywords: sexually transmitted infections (STIs), Chlamydia trachomatis, Neisseria gonorrhoeae, Treponema pallidum, immunology, T cells, B cells, vaccines, bacterial pathogens, reproductive health
1. Introduction
Sexually transmitted infections (STIs) are a significant public health burden, both in the United States and worldwide [1]. Direct impacts of STIs on sexual and reproductive health include stigmatization, pelvic inflammatory disease (PID), pregnancy complications, infertility, and increased susceptibility to cervical cancer and HIV. In the United States in 2018, there were an estimated 68 million STIs and 26 million new infections. Bacterial STIs, including chlamydia, gonorrhea, and syphilis, accounted for 4 million, 1.6 million, and 146,000 infections, respectively, and contributed to over USD 1 billion in direct medical costs [2]. Nearly half of these STIs occurred in young people (ages 15–24) and care for women with STIs represented nearly 75% of all non-HIV STI-related medical costs.
Increased prevention measures are important to combat the STI epidemic. Bacterial STIs are curable with antibiotics. However, shortages of penicillin amid rising syphilis rates and antibiotic resistance to gonorrheal infections are increasing problems [3]. Further, most bacterial STIs are asymptomatic, limiting the number of people who seek antibiotic treatment and increasing transmission of the pathogens [2]. Current preventive measures include condom use and increased diagnostic surveillance. While vaccines have been developed against the viral STIs human papillomavirus (HPV) and hepatitis B virus (HBV), there are no vaccines against bacterial STI pathogens. Designing and implementing effective vaccines against bacterial STIs is a major research effort and depends heavily on our understanding of the immune response to these pathogens in the female genital tract. In this review, we will discuss the pathogens that cause bacterial STIs, adaptive and innate immunity to these pathogens, current vaccine strategies, and existing gaps in knowledge and implications for vaccine design (Table 1).
Table 1.
A summary of immune responses to and vaccine progress against bacterial STIs.
| Disease [Pathogen] | Symptoms of Female Genital Tract Infection | Immune Evasion Mechanisms | Protective Immune Responses | Experimental Models | Vaccine Development |
|---|---|---|---|---|---|
| Chlamydia [Chlamydia trachomatis] |
Lower genital tract discharge, dysuria, dyspareunia, urethritis, menstrual irregularities, PID; long term complications include chronic pelvic pain, infertility, ectopic pregnancy, adverse pregnancy outcomes Often asymptomatic Mother to child transmission during birth can cause neonatal conjunctivitis and pneumonia |
Evades recognition in intracellular niche [4] Can persist within inclusion in a low metabolic state [4] Multiple molecular mechanisms of epithelial cell invasion [4] Inhibition of neutrophil functions [5] Responses to natural infection are skewed toward Th2 in humans, supporting antibody production which is not associated with long-term protective immunity [6,7,8] |
IFNγ-mediated tryptophan depletion in humans restricts chlamydial growth and replication [9] CD4+ Th1 and Th17 responses associated with reduced reinfection in humans [6,8] |
Mice, guinea pigs, non-human primates, koalas [10,11] | Recombinant MOMP vaccine adjuvanted with CAF01 in Phase 1 human clinical trials (NCT02787109, NCT03926728) [12,13,14] Several preclinical vaccine candidates using MOMP, CPAF, PmpG recombinant proteins with an emphasis on Th1-inducing adjuvants [15,16,17] |
| Gonorrhea [Neisseria gonorrhoeae] |
Lower genital tract discharge, dysuria, dyspareunia, urethritis, menstrual irregularities, PID; long term complications include chronic pelvic pain, infertility, ectopic pregnancy, adverse pregnancy outcomes Often asymptomatic Disseminated infections can lead to sepsis, skin rash, arthritis, endocarditis, meningitis Mother to child transmission during birth can cause ocular or disseminated infection |
Antigenic and phase variation [18] Induces IL-10 and regulatory T cells that suppresses antibody responses [19] Inhibits complement deposition and blocks activation of complement [20,21] Epitope masking by IgA1 protease [22] Natural infection in mice drives Th17 and neutrophil responses, which N. gonorrhoeae resists, while suppressing protective Th1 responses [23,24] |
CD4+ Th1 responses associated with protection in mice [25] | Antibiotic-treated mice, humanized mice [26,27,28] Controlled human infection model (CHIM) [29] |
Phase 2 and Phase 4 human clinical trials evaluating efficacy of currently licensed meningococcal vaccine 4CMenB (Bexsero, GSK) against N. gonnorrhoea infections (NCT04722003, NCT04094883) [30,31] OMV-based vaccine in Phase1/2 human clinical trials (NCT05630859) Pre-clinical studies evaluating OMV-based vaccines in mice and determining candidate antigens for recombinant protein vaccines [32,33] |
| Syphilis [Treponema pallidum] |
Primary stage: chancre at infection site Secondary stage: skin lesions, fever, fatigue, rash, muscle aches, weight loss, headaches, hair loss and swollen lymph nodes Tertiary stage: neurological and cardiovascular complications, seizures, deafness, and vision problems including blindness Congenital syphilis: severe outcomes in newborns including prematurity, low birth weight, pneumonia, rash, neurologic disease, and bone abnormalities |
Ability to remain dormant for long periods Antigenic variation [34] |
CD4+ Th1 IFNγ-mediated recruitment of macrophages [35] Macrophage mediated opsonophagocytosis and killing [36,37] |
Rabbits are most widely used [38] Recent development of mouse and in vitro models [39,40] |
Pre-clinical studies identifying potential target antigens for recombinant protein vaccines [35,41] |
2. Bacterial STIs of the Female Genital Tract
2.1. Chlamydia
Chlamydia trachomatis is a Gram-negative obligate intracellular bacterium and the causative agent of chlamydial infections. Serovars A–C cause conjunctival infections of the eye, D–K cause the most common urogenital tract infections in the US, and L1–L3 cause lymphogranuloma venereum (LGV), a mucosally invasive infection [42]. C. trachomatis has a unique biphasic developmental cycle in which infectious elementary bodies [EBs) invade host epithelial cells, form an inclusion in which they transition to reticulate bodies for replication, and transition back to EBs for cell lysis or extrusion for cell attachment and re-initiation of the cycle [4]. C. trachomatis urogenital infections are detected in almost twice the number of women as men in the US [43], likely due to increased screening in women [44]. Up to 70% of C. trachomatis genital tract infections in women, and up to 50% in men, are asymptomatic. Symptomatic infections present with vaginal and/or urethral discharge, painful urination, dyspareunia, lower abdominal or pelvic pain in women, and testicular pain associated with epididymitis in men. Due its more invasive nature, LGV can induce severe proctitis from rectal infection, rectal strictures, and painful lymphadenopathy from lymph node invasion. Infections can also spread from infected mothers to newborns at the time of delivery, causing neonatal conjunctivitis and pneumonia. Antibiotic treatment with doxycycline or azithromycin is effective and antibiotic resistance is rare [45]. However, many asymptomatic infections are untreated and can last up to 4 years [46], resulting in continued asymptomatic transmission contributing to high prevalence of infections. Despite the high rate of asymptomatic infection, up to 40% of untreated infections in women ascend to involve the upper genital tract, causing damaging immunopathology which may lead to PID and reproductive sequelae including chronic pelvic pain, pregnancy complications, and infertility [42].
2.2. Gonorrhea
Neisseria gonorrhoeae is a Gram-negative diplococcus bacterium and the causative agent of urogenital gonorrheal infections. The organism infects epithelial cells and has virulence factors that allow it to survive inside infiltrating neutrophils via resistance to antimicrobial components in neutrophil granules [47]. Its genome, and the outer membrane proteins it encodes, is highly variable, allowing for immune evasion and complicating diagnostics, antibiotic treatment, and vaccine development [48,49]. Gonorrheal infections in the US are most prevalent among men and most infections are asymptomatic [43]. Urogenital symptoms are similar to those reported above for chlamydial infections. Approximately 10% of women with gonorrhea infections develop PID from infections that ascend to the upper genital tract with potential for consequent reproductive morbidities, as described with chlamydial infection [50]. Unlike chlamydial infections, which remain restricted to the mucosa, gonorrheal infections can disseminate through the bloodstream and result in bacterial sepsis with skin rash and multifocal arthritis, septic arthritis of single joints, endocarditis, and rarely, meningitis and hepatitis. Gonococcal infection can also be transmitted to newborns during delivery from an infected mother and can lead to severe neonatal ocular infection or disseminated infection as seen in adults. Ceftriaxone is the recommended antibiotic treatment and is highly effective [45]. However, antibiotic resistance is a growing concern for gonorrheal infections, as ~50% of isolates from infections in the US in 2022 were estimated to be resistant to at least one antibiotic [43], emphasizing the need for preventive vaccine development.
2.3. Syphilis
Treponema pallidum is a spirochete and is the causative agent of syphilis infections. The organism infects the epithelium and replicates inside tissues, inducing damaging inflammation [51]. Primary syphilis typically presents as a solitary, painless chancre at the site of infection, usually the genitals, anus, or mouth [52,53]. The chancre appears approximately 3 weeks after exposure and heals spontaneously within 3–6 weeks if untreated. Secondary syphilis occurs weeks to months after the initial infection and is characterized by systemic dissemination of the bacterium. Common clinical manifestations include a diffuse rash that often involves the palms and soles, skin lesions, and swollen lymph nodes. Other symptoms can include fever, fatigue, sore throat, and hair loss. Syphilis infections are sexually transmissible at this stage. Upon resolution, symptoms typically subside during latent syphilis and infections can only be detected during this stage by serologic testing. Tertiary syphilis can develop years to decades after the initial infection. It is characterized by large, destructive lesions affecting the skin, bones, and other tissues, heart problems, and neurosyphilis. Neurosyphilis can present at any stage but is more common in tertiary syphilis, manifesting as muscle weakness, coordination issues, seizures, deafness, and blindness [52,53]. Syphilis can also be passed from mother to child, causing congenital infections which are associated with fetal demise, prematurity, low birth weight, pneumonia, rash, neurologic disease, and bone abnormalities [54,55].
Of the three bacterial STIs discussed in this review, syphilis is the least prevalent in the US. In 2022, the Centers for Disease Control reported 207,255 cases of syphilis, 59,016 (28%) of which were primary and secondary syphilis cases [43]. Cases of syphilis have increased rapidly in recent years, with an increase of 17.3% from 2021 to 2022 [43]. A proportional increase in cases of congenital syphilis infections has also been observed [43,54], emphasizing the need for improved treatment and prevention measures. Penicillin is effective against syphilis infections [45], but asymptomatic untreated infections are common, and the organism can remain latent for long periods of time, increasing the risk of transmission.
3. B Cells and Antibody-Mediated Immunity
The primary role of B cells in the immune response against STIs and other pathogens is to secrete antibodies. Naïve B cells encounter antigens that are recognized by the B cell surface receptor. With stimulation by follicular dendritic cells and help from T cells, B cells form germinal centers in draining lymph nodes and undergo affinity maturation and class switching. B cells replicate and develop into short-lived immunoglobulin-secreting plasmablasts, memory B cells, or long-lived plasma cells. Memory B cells are long-lived antigen-specific B cells that are poised to recall and respond upon antigen re-exposure. Long-lived plasma cells home to the bone marrow and secrete antibodies that can last in circulation for years to a lifetime [56].
The five classes of antibody (IgA, IgD, IgE, IgG, and IgM) differ in their effector functions, anatomical distribution, and protection against different pathogens. IgG is the most abundant antibody class in the bloodstream and is involved in systemic immunity via neutralization, opsonophagocytosis, and antibody-dependent cellular cytotoxicity (ADCC).
3.1. IgG and Chlamydia Infection
3.1.1. Neutralization
Neutralization is the mechanism by which an antibody recognizes and binds to surface antigens on the pathogen, thereby blocking the ability of the pathogen or a secreted toxin to attach and interact with host cells. Although antibody-mediated neutralization of C. trachomatis has been demonstrated in vitro [57], this organism enters the host cell by a multitude of mechanisms including non-receptor–ligand-mediated pinocytosis [58]. There is also a panoply of bacterial surface ligand–host cell receptor-mediated interactions that enhance chlamydial invasion of host epithelial cells [59], serving as an effective evasion mechanism to thwart antibody neutralization. Female mouse models of chlamydial genital infection have revealed that IgG antibodies specific for the chlamydial major outer membrane protein (MOMP) that led to neutralization in vitro lowered the burden but failed to protect against C. trachomatis genital tract infection in mice [60,61].
3.1.2. Opsonophagocytosis
Opsonophagocytosis is the coating of a pathogen with antibodies that allows phagocytic cell FcRs to target the pathogen for destruction. Mouse model studies have revealed that chlamydia-specific antibody interactions with phagocytic cells can limit infectious burden when interferon gamma (IFNγ) is present [62,63,64,65]. Antibodies opsonize extracellular chlamydial elementary bodies by binding to a specific antigen epitope via Fab domains. The free Fc domain binds to immune effector cells, leading to opsonophagocytosis, and enhanced bacterial killing.
IFNγ upregulates phagocytic cell FcR expression and is required to enhance chlamydial opsonophagocytosis [66]. Naglak et al. reported that depletion of neutrophils and CD4+ T cells led to a chronic infection of significantly greater burden than in mice depleted of CD4+ T cells alone [67]. However, C. trachomatis can resist neutrophil opsonophagocytosis and killing by chlamydial protease-like activity factor (CPAF), which suppresses oxidative bursts, interferes with chemical-mediated activation, and prevents neutrophil extracellular trap (NET) formation [5]. Using B-cell deficient mice that had resolved a primary infection and were subsequently depleted of CD4+ T cells, they showed that transfer of Fab fragments from immune mice failed to provide any protection against chlamydial challenge infection, demonstrating that antibody-mediated protection is dependent on IgG with intact Fc [67].
3.1.3. Antibody-Dependent Cellular Cytotoxicity (ADCC)
Antibody-dependent cellular cytotoxicity (ADCC) is a third mechanism whereby antibodies mediate pathogen killing. It typically involves natural killer (NK) cell recognition of antibody-opsonized cells expressing non-self-antigens, but can also involve other myeloid cells. NK cells bind the Fc portions of antibodies and trigger the release of cytotoxic molecules, killing the infected target cell. Although NK cell depletion prolongs primary murine chlamydial infection, it leads to a shift towards a Th2 response [68], and depletion of NK cells during secondary infection has no effect on time to resolution in the B cell-deficient, CD4-depleted challenge model [67]. However, combined depletion of NK cells and CD4 T cells led to enhanced burden over CD4 depletion alone [67].
In vitro studies show that anti-chlamydial antibodies can increase both macrophage killing of infected epithelial cells and macrophage inhibition of productive growth of chlamydiae in co-cultures [69]. Anti-chlamydial antibodies can also boost antigen presentation, thereby augmenting protective memory T cell responses active during repeat infections [69]. Despite these protective mechanisms, B cells are exceedingly rare in the female genital tract, making up less than 1% of leukocytes in healthy cervical tissue compared to T cells that make up ~35% of leukocytes [70]. Some B cells in the cervix have been shown to form follicle-like structures that are closely associated with aggregates of T cells, while other CD38+ immunoglobulin-producing B cells are scattered among the lamina propria of the cervix and vagina [71]. IgG antibody produced by circulating B cells that transudates into genital secretions is a primary source of B cell-derived protection against pathogens of the female genital tract.
3.1.4. FcRn Transcytosis
IgG can be transported from the apical to the basolateral surface of mucosal epithelial cells and into the tissue through transcytosis. The neonatal Fc receptor (FcRn) is found throughout the mucosal tissues of mammals, including on epithelial, endothelial, and antigen-presenting cells [72]. FcRn binds to IgG antibodies under acidic conditions (pH 5–6.5) and releases them at neutral pH (pH 7.4). This allows FcRn to transport IgG antibodies both into and out of the lumen of the male and female reproductive tracts, depending on the pH [73,74].
Whether or not transcytosing antibodies exacerbate or inhibit chlamydia infection in vitro is dependent upon antibody specificity [75]. IgG specifically targeting chlamydial MOMP increased FcRn-dependent uptake and translocation of chlamydial elementary bodies in polarized male epididymal epithelia. In contrast, FcRn-internalized IgG, which targets a chlamydial inclusion membrane protein, IncA, led to reduced in vitro infection. Further, it has been shown that additional inclusion membrane proteins that are cytoplasmic facing can be bound by intracellular IgG, and microinjection of an anti-Inc (CT229) antibody into infected cells inhibited chlamydial infection [76,77].
3.2. IgA and Chlamydia Infection
Secretory IgA (SIgA) is found predominantly in mucosal secretions and functions to neutralize pathogens by blocking their attachment to mucosal epithelial cells and by preventing their entry into tissues. In human cervical mucus, IgG predominates over IgA in abundance, which directly contrasts with other typical external secretions, such as saliva, tears, milk, and intestinal fluids, in which SIgA is the dominant isotype [78,79]. Although IgA is known to protect against a variety of mucosal pathogens [80], IgA-deficient mice resolve primary and secondary chlamydial genital infections similarly to IgA-sufficient mice [81]. It is possible that any contribution from IgA is masked by redundancy and high levels of IgG transcytosed via FcRn.
3.3. Chlamydia Antibody in Humans
Human data support a role for antibodies in limiting chlamydial burden but not reinfection. A majority of C. trachomatis-infected women and at least 50% of men develop detectable levels of anti-C. trachomatis serum IgG and IgA [82]. Additionally, C. trachomatis-specific IgG and IgA antibodies were more frequently found in female genital tract secretions when compared to serum [83]. Despite this, rates of repeat infections are high [84,85,86,87], failing to support a role for C. trachomatis-specific antibodies in resistance to reinfection.
We analyzed the relationship of serum anti-C. trachomatis IgG determined by microimmunofluorescence (MIF) assay to whole EBs in a cohort of 225 young women who were highly sexually exposed to C. trachomatis, with 83% being seropositive at enrollment [6]. Although we found an inverse relationship of antibody titers with cervical chlamydial burden as determined by quantitative PCR, there was no relationship determined between antibody titer and detection of endometrial chlamydial infection, indicating that antibodies failed to limit risk for upper genital tract infection and potential for reproductive sequelae. We also determined that both serum and cervical anti-C. trachomatis IgG correlated with increased risk of incident infection, with hazard ratios increasing 3.6-fold and 22.6-fold with each unit of serum and cervical IgG, respectively [6]. We went further and used a whole-proteome C. trachomatis array to screen serum samples for IgG to specific chlamydial proteins but were unable to identify protein-specific antibody responses that correlated with reduced risk of reinfection [7]. In contrast, in this same cohort, we determined that increased frequencies of chlamydial antigen-specific IFNγ-producing CD4 T cells were associated with reduced risk of reinfection [88]. Women with the highest anti-chlamydial antibody responses may be Th2-skewed, resulting in inadequate IFNγ and cell-mediated responses that are key for protection. Indeed, several studies correlate high titers of serum anti-chlamydial IgG with complications of infection [89,90,91]. As opposed to other mucosal pathogens, where antibodies in mucosal secretions function as a first line of defense [92], data from human studies of chlamydial genital tract infection fail to support a role for antibodies in the limitation of spread of infection to the upper genital tract in persons with a uterus, or acquisition of infection regardless of gender.
3.4. Antibody in Gonorrhea Infection
N. gonorrhoeae has a remarkable ability to modify its surface antigens, which differ not only between strains but also within the same strain over time. The organism also practices phase variation, which allows it to switch between phenotypic states rapidly and reversibly, altering expression of surface proteins over time [18]. Both mechanisms make it extremely difficult for antibody responses elicited by a primary gonorrhea infection to protect against a secondary infection [32]. These aspects, and the consideration that multiple other species of Neisseria also possess gonococcal antigens, further complicate serological studies in humans. Even so, both antibody and cell-mediated cytokine responses to documented, uncomplicated gonococcal infection are weak and wane after only a few weeks in both women and men [93,94]. Low levels of gonococcal antibody have been partially explained by the manipulation of the immune response by N. gonorrhoeae. One way N. gonorrhoeae suppresses antibody responses is by inducing IL-10-producing type 1 regulatory T cells. In a mouse model, these cells contributed significantly to the suppression of adaptive immunity, whereas their absence allowed antibody responses to develop [19]. N. gonorrhoeae encodes an IgA1 protease that masks epitopes by cleaving antigen-bound IgA [22]. It also has multiple mechanisms to evade complement, including sialylation of lipooligosaccharides (LOS) to prevent recognition by complement components [20] and binding of factor H and C4b-binding protein (C4BP) via surface proteins such as factor H binding protein (fHbp) and PorB to inhibit complement activation [21]. Between surface antigen variation and humoral immune evasion, it is not surprising that infections fail to elicit protective immunity upon re-exposure.
3.5. Antibody in Syphilis Infection
IgG and IgM against T. pallidum proteins have been detected in experimentally infected rabbits [95,96] and in humans with primary, secondary, and late-stage syphilis [97]. Partial immunity to T. pallidum challenge was conferred by adoptive transfer of immune serum in experimental infection of rabbits and hamsters [98,99], with the main mechanism of protection being antibody opsonization and induction of phagocytosis and killing by macrophages [35,36,37]. However, T. pallidum isolates from humans had varied capacities for binding opsonic antibodies, suggesting a potential evasion mechanism [100]. The high rates of syphilis reinfection despite detection of T. pallidum specific antibodies in previously infected persons indicates ineffective antibody-mediated protection is induced after natural infections. Specifically, antigenic variation of T. pallidum surface protein TprK can evade antibody-mediated immunity [34].
4. T Cell-Mediated Immunity
T cells encounter peptide antigens in the context of major histocompatibility complex (MHC) molecules on the surface of antigen-presenting cells such as dendritic cells, macrophages, and B cells. Activated T cells proliferate and differentiate into effector T cells which contribute to pathogen elimination. The main role of CD4+ T-helper cells is to secrete cytokines that are crucial for activating and regulating both innate and adaptive immune responses [101]. T-helper 1 (Th1) cells secrete IFNγ, TNFα, TNF, and IL-2, and contribute to elimination of viruses and intracellular bacteria by activating macrophage phagocytosis and enhancing CD8+ T cell cytotoxicity. Th2 cells secrete IL-4, IL-5, IL-13, and IL-10 and contribute to defense against extracellular pathogens and secreted toxins by stimulating B cells to produce antibodies and recruiting and activating eosinophils and mast cells. Th17 cells are highly plastic and secrete IL-17, IL-21, and IL-22 to promote inflammation and recruitment of neutrophils to the site of infection. Th17 cells give rise to long-lived resident memory T cells that are essential for protection against various mucosal pathogens [102], including STIs, but can also be pathogenic. T follicular helper (Tfh) cells secrete cytokines such as IL-21 and IL-4 and are specialized in providing help to B cells in the germinal centers of secondary lymphoid organs, in turn promoting antibody class switching, affinity maturation, and the generation of long-lived plasma cells and memory B cells [101]. Regulatory T (Treg) cells produce IL-10 and TGF, functioning as important negative regulators of the immune response to prevent over-activation and unchecked inflammation. CD8+ cytotoxic T lymphocytes (CTL) recognize and directly kill infected cells displaying foreign antigens by releasing cytotoxic granules containing perforin and granzymes or by inducing apoptosis in target cells through the Fas-Fas ligand pathway.
4.1. T Cells and Chlamydia Infection
Studies have shown that SCID, RAG-1−/−, TCRα−/−, CD4−/−, and MHCII−/− mice display delayed or failed resolution of chlamydial primary infections, while MHCI-deficient (b2M−/−), B cell-deficient (μMT), and CD8−/− mice resolve infection with comparable kinetics to wild-type, demonstrating that CD4+ T cells are key mediators of chlamydial host defense [62,103,104,105,106]. Gene-knockout, antibody depletion, and adoptive transfer studies in mice indicate Th1 cells and their defining production of IFNγ are key mediators for resolving primary infections [10,107,108]. However, this mechanism may be independent of expression of T-bet, the transcription factor that putatively defines Th1 cells [109]. CD8-derived IFNγ can also contribute to resolution of C. trachomatis infection in mice [110]. In humans, IFNγ mediates C. trachomatis killing by inducing indoleamine-2,3-dioxygenase (IDO) production in epithelial cells, which catabolizes tryptophan, thereby starving C. trachomatis of this essential nutrient (Figure 1) [9]. In mice epithelial cells, however, IFNγ induces expression of p47 GTPases, but not IDO, demonstrating host infection tropism and defining an important difference to consider when utilizing mouse models of chlamydia infection [111].
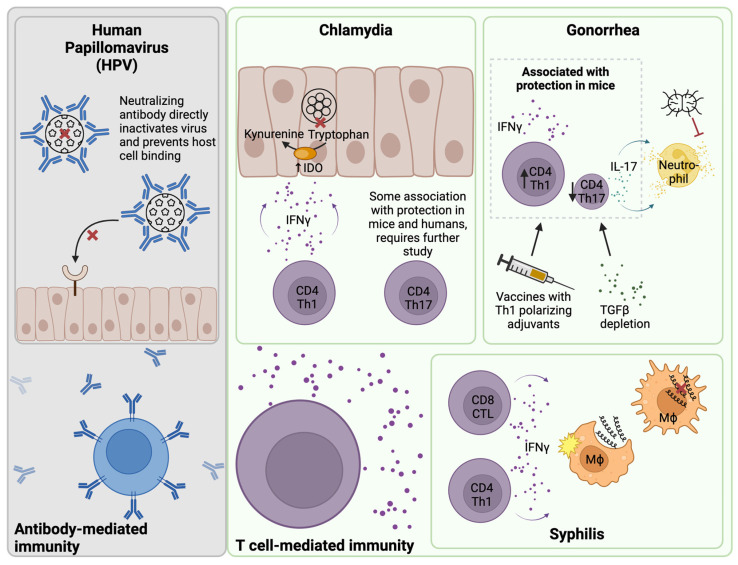
Figure 1.
T cell-mediated immunity for bacterial STIs of the female genital tract. Immunity to human papillomavirus (HPV) is mediated by a neutralizing antibody, which directly inactivates the virus and prevents the virus from binding to and entering host epithelial cells. In contrast, evidence points toward T cell-mediated immunity for bacterial STIs of the female genital tract including chlamydia, gonorrhea, and syphilis. In the context of chlamydia infection, CD4 Th1 cells are an abundant source of IFNγ. IFNγ induces epithelial cells to upregulate indoleamine 2,3-dioxygenase (IDO), which starves chlamydia of the essential nutrient tryptophan by metabolizing it to kynurenine. CD4 Th17 cells are also associated with protection in mice and humans, but further study is required. Gonorrhea induces a strong Th17 response, which supports neutrophil influx. This Th17 response is favorable for gonorrhea survival because the organism can resist neutrophil killing both intracellularly and extracellularly. Immunization with vaccines containing Th1-polarizing adjuvants or depletion of TGFβ in mice results in suppression of Th17 responses and induction of Th1 responses, which are associated with greater protection. In the context of syphilis infection, IFNγ from T cells and innate cells supports recruitment and activation of macrophages, which phagocytose and mediate killing of the organism. Created with Biorender.
Adoptive transfer of a chlamydia-specific Th2 clone did not protect against murine genital challenge and T cells displayed reduced trafficking to the genital mucosa [112]. Th17 cells can be protective or pathogenic in contexts of infection and disease [113,114]. One study found that blocking IFNγ signaling promoted tissue damage by greatly enhancing chlamydia-specific Th17 responses [115]. Another study found that IL-17 supported neutrophil influx, a major contributor to chlamydial pathology, but also protective Th1 responses during murine chlamydial infection [116]. IL-17 was not required for infection resolution [116]. We detected both chlamydia-specific IFNγ and IL-17-producing CD4+ T cells in C. trachomatis-exposed adolescents and adults [88,117]. Increased frequencies of Th1 and Th17 cells were also found to be associated with reduced reinfection in a highly exposed cohort of C. trachomatis-infected women, while increased frequencies of Th2 cells were found to be associated with increased reinfection over time [8]. Together, these results suggest that Th1 responses drive protective immunity to C. trachomatis, while Th2 responses are not protective, and the role of Th17 responses requires further study (Figure 1).
4.2. T Cells and Gonorrhea Infection
Studies in mice have shown that N. gonorrhoeae genital tract infection drives a Th17 cytokine profile and suppresses Th1 or Th2 responses through the induction of TGFβ [23]. This immune evasion strategy results in recruitment of neutrophils, which N. gonorrhoeae resists both intracellularly and extracellularly [24]. Indeed, TGFβ depletion in mice resulted in suppressed Th17 responses and enhanced Th1 and Th2 responses to N. gonorrhoeae infection, which were associated with increased protection against subsequent challenge (Figure 1) [25]. Two of the characteristic cytokines produced by Th17 cells are IL-17 and IL-22. Interestingly, IL-17 depletion resulted in prolonged gonorrheal infection in mice [118] while IL-22 depletion resulted in accelerated clearance [119], demonstrating divergent roles for these two Th17 effectors in the context of gonorrheal immunity. Studies in gonococcal-infected humans found increased IL-17, IL-23, and IFNγ in serum [120], which suggests that Th17 responses are also activated in humans. In summary, strong evidence exists for Th1 cells to play a role in protection for both chlamydial and gonococcal infections, and recent data suggest Th17-lineage cells may contribute to resistance to chlamydial reinfection and may be involved in resolution of gonococcal infection.
4.3. T Cells and Syphilis Infection
Experimental infection of male rabbits with T. pallidum subsp. pallidum elicited a CD4+ Th1-dominant response in testicular lesions [121,122]. Detection of high levels of IL-2, IFNγ, and IL-12 alongside low levels of IL-4, IL-5, and IL-13 transcripts by RT-PCR in primary and secondary human lesion biopsies also support a Th1 profile [123]. CD8+ T cells have also been detected in syphilis lesions in humans [124]. Salazar et al. reported that CD4 and CD8 T cells from blister fluid of males and females with secondary syphilis expressed higher levels of CCR5, a mucosal homing marker, and CD45RO, a marker of T cell memory, than T cells in peripheral blood [125]. The relative contributions of T cell subsets to protection against syphilis infection is unclear, although it is generally thought that production of IFNγ by innate cells and CD4 or CD8 T cells is important for recruiting and activating macrophages, which facilitate T. pallidum killing (Figure 1) [35,41]. Further, many of the rabbit model studies of T cell responses were limited to evaluation of male testicular lesions, and studies in the context of the female genital tract are very limited.
4.4. Resident Memory T Cells in the Female Genital Tract
Most activated T cells undergo apoptosis after resolution of a primary immune response to a specific pathogen, but some differentiate into memory cells, which persist in the periphery and quickly respond to subsequent encounters with the same pathogen. Central memory T (TCM) cells primarily reside in secondary lymphoid organs, where they serve as a long-term reservoir of antigen-specific T cells, remaining poised to proliferate and differentiate into effector cells capable of trafficking to the site of infection upon reactivation [126]. They typically express high levels of the lymph node-homing receptor CD62L (L-selectin) and the chemokine receptor CCR7, which facilitate their migration and retention within secondary lymphoid organs. Effector memory T (TEM) cells lack CD62L and CCR7 expression, circulating between peripheral blood and mucosal tissues, where they are primed to respond immediately to reactivation.
Resident memory T (TRM) cells are a subset of TEM that do not circulate but are retained in mucosal tissues and barrier sites. TRM cells contribute to frontline defense in both mice and humans against a variety of mucosal pathogens [127,128]. TRM cells are classically defined by expression of CD69, which inhibits the sphingosine-1 phosphate receptor (S1PR), a molecule required for egress from tissues or secondary lymphoid organs to the circulation [129,130,131].
Studies have documented TRM cells in the genital tracts of healthy women [132,133]. CD8 T cells predominated in the vagina while CD4 T cells predominated in the ectocervix and endocervix [132]. CD4 and CD8 T cells in the genital tract were primarily effector memory T cells as evidenced by lack of CD45RA and CCR7 [132,133]. CD4 and CD8 TRM cells in the female genital tract expressed higher levels of the following markers than CD4 and CD8 T cells in peripheral blood: CD69 and CD103, putative markers of TRM cells; PD-1, a marker upregulated on T effector cells in peripheral and mucosal tissues [134]; and CCR5, an important factor for healthy barrier immunity in the genital tract [135,136]. CD4 TRM cells expressed lower levels of CD103 than their CD8 counterparts [133], but CD69+CD103+ CD4 TRM cells were still detected across the vagina, ectocervix, and endocervix [132], with higher frequencies detected in the vagina. However, most CD4 TRM cells in all three tissues were CD69+CD103− [132]. Of note, CD69−CD103− T cells from genital tract tissues were transcriptionally distinct from CD69−CD103− T cells from peripheral blood, by demonstrating enrichment of cell migration and localization pathways [133]. A recent study showed that TRM cells are not only distinct between blood and mucosal sites, but are also distinct between different mucosal tissues in the same individuals including lung, skin, and jejunum [137]. Pattacini et al. aligned gene expression of cervicovaginal TRM cells with a previously published dataset comparing gene signatures of human spleen and lung tissues [134], and found both gene expression signatures that were common and unique to cervicovaginal TRM cells [133]. These findings support the further study of TRM cells in the female genital tract.
This review focuses on immunity to bacterial STIs, but much of the foundational work regarding TRM cells in the context of STIs of the female genital tract comes from studies of herpes simplex virus (HSV) in mice and humans [138,139,140,141,142,143,144,145,146]. Work in the contexts of human papillomavirus (HPV) and cervical cancer [147,148,149], lymphocytic choriomeningitis virus (LCMV) [147,148,149], and human immunodeficiency virus (HIV) [150,151,152,153,154,155,156,157] has also demonstrated the importance of TRM cells in the female genital tract in the context of viral infections. While CD8+ TRM cells are key antiviral effectors [158], CD4+ TRM cells are likely the main contributors to defense against bacterial STIs such as chlamydia.
Before the term TRM cells was coined, clusters of T cells were reported in genital tract tissues of chlamydia-infected convalescent mice [159], in chlamydia-infected macaques [160], and in cervical and endometrial samples from women with C. trachomatis infections [161,162]. Early studies also demonstrated the importance of IFNγ and T cell contact with epithelial cells for nitric oxide-mediated killing of Chlamydia in the female genital tract of mice [163,164]. Additionally, T cells migrating to the female mouse genital tract following chlamydial infection were mostly CD4+ and expressed increased mucosal homing molecules LFA-1 (CD11a) and α4β7 [165,166].
Studies in more recent years have investigated the role of chlamydia-specific TRM cells elicited by vaccination in mice. Stary et al. showed that intranasal or intrauterine but not subcutaneous immunization of female mice with UV-inactivated C. trachomatis (UV-Ct) complexed with charge-switching synthetic adjuvant particles (cSAP) induced CD4 TRM cells in the genital tract, with increased expression of IFNγ, TNFα, and IL-2 that rapidly expanded upon challenge, resulting in accelerated bacterial clearance and reduced oviduct pathology [108]. Two “waves” of protective T cells were induced, including TRM cells retained in the genital tract after mucosal immunization and circulating effector cells that were quickly recruited to the genital tract following challenge. The circulating memory subset contributed to the overall recall response, but its protective role was suboptimal in the absence of TRM cells, as evidenced by parabiotic mouse experiments. Importantly, mucosal immunization of mice with unadjuvanted UV-Ct exacerbated infection via induction of FoxP3+ CD4 regulatory T cells, demonstrating that vaccine platforms and adjuvants are important considerations for effective vaccine design. Nguyen et al. detected IFNγ- and IL-17-producing TRM cells in female genital tracts of C. trachomatis-challenged mice that had been immunized subcutaneously with CAF01-adjuvanted variable domain 4 (VD4) of the major outer membrane protein (MOMP) [167]. The same group found that simultaneous subcutaneous and intrauterine immunization with the same vaccine was required to elicit CD4 Th1 and Th17 TRM pre-challenge [168]. Notably, nearly 40% of Th17 TRM co-expressed IL-17 and IFNγ by 14 days post-infection, suggesting that Th17 cells may contribute to IFNγ-mediated protection against chlamydial infection. Overall, it has been shown that mucosal vaccines elicit CD4 TRM cells in the genital tracts of mice and that these cells likely contribute to accelerated resolution of chlamydial infection upon challenge. Further research is needed to elucidate genital tract TRM cells’ responses after natural chlamydial infection, both in mouse models and in human cohorts.
Notably, studies of resident memory T cells in the context of gonorrhea or syphilis infection have not been reported in either mice or humans but will be important for understanding their contributions to infection resolution with these pathogens.
5. Innate Lymphocyte-Mediated Immunity
Although not a part of the trained adaptive response, the role of innate lymphocytes in protection against bacterial STIs is worth mentioning.
5.1. NK Cells
Upon pathogen recognition, natural killer (NK) cells release cytotoxic granules containing perforin and granzymes, inducing apoptosis in the target cell. They also secrete IFNγ and TNFα, which are important effectors and regulators of downstream immune responses. An early study reported that NK cells were recruited to the female genital tracts of mice as early as 12 h post-infection with C. muridarum, and that depletion of NK cells resulted in reduced IFNγ and a Th2-skewed immune response [68]. Later studies corroborated that depletion of NK cells exacerbated C. muridarum infection in mice and further demonstrated that IFNγ from NK cells promotes IL-12 production by dendritic cells, which then supports a strong Th1 response [169]. Depletion of NK cells also impaired production of IFNγ by memory T cells in respiratory C. muridarum infection [170]. These studies suggest that the early presence of NK cells and their production of IFNγ could both directly inhibit chlamydial growth by tryptophan depletion [9] and support Th1 responses associated with chlamydial protection [107].
5.2. Helper Innate Lymphoid Cells (ILCs)
Helper innate lymphoid cells (ILCs) recognize pathogens through Toll-like receptors (TLRs) and pattern recognition receptors (PRRs) and secrete effector cytokines that modulate the downstream immune response like T-helper cells. They are present in lymphoid and non-lymphoid tissues, but are most abundant in mucosal tissues, where they play an important role in pathogen defense against lung and gut pathogens [171]. ILCs are present in the female genital tracts of healthy humans and mice and are dominated by the ILC3 subtype [172,173]. ILC3s produce IL-17 and IL-22 and express transcription factors including RORγt, RORα, and HIF1, which inhibit their plasticity toward ILC1s, which express T-bet, in conjunction with Aiolos and Bcl6 [174]. The contribution of ILCs to protection against STIs of the female genital tract is largely unknown. Initial studies have found that ILCs accumulate in the oviducts of mice infected with C. muridarum [175] and that transfer of ILC3-like cells to the mouse colon prevents gastrointestinal colonization by C. muridarum [176]. The contribution of ILCs in the context of gonorrhea or syphilis infection is unknown. Significant further study will be required to elucidate the protective capacity of ILCs in the context of bacterial STIs of the female reproductive tract.
5.3. Mucosal-Associated Invariant T (MAIT) Cells
Mucosal-associated invariant T (MAIT) cells are a population of unconventional innate-like T cells that have unusual specificity for microbial riboflavin-derivative antigens presented by the MHCI-like protein MR1 [177]. They are defined by surface expression of the semi-invariant T cell receptor Vα7.2 and high expression of C-type lectin CD161. They can be activated by TCR-dependent and TCR-independent mechanisms, secrete cytokines including IFNγ, TNFα, IL-17, and IL-22, and are involved in defense against a variety of mucosal pathogens [178]. Gibbs et al. were the first to report MAIT cells in the human female genital tract [179]. MAIT cells were present in the endometrium, endocervix, transformation zone, and ectocervix, as were MR-1+ antigen-presenting cells. MAIT cells accounted for ~1.0% of T cells in the endometrium, ~1.8% of T cells in the cervix, and ~2.1% of T cells in the blood. CD8+CD4− MAIT cells predominated over CD4+ and CD8−CD4− MAIT cells in all three tissues. MAIT cells isolated from the genital tract produced IL-17- and IL-22-biased responses upon ex vivo stimulation with E. coli [179]. Bister et al. detected MAIT cells in the endometrium of healthy pre- and postmenopausal women, and in decidua from healthy women in first-trimester pregnancies [180]. They showed that endometrial MAIT cells had an activated tissue-resident phenotype by higher expression of CD69, CD103, CD38, HLA-DR, and PD-1 than peripheral blood MAIT cells. Between pairs of monozygotic twins, frequencies of peripheral blood MAIT cells were similar, while frequencies of endometrial MAIT cells varied, suggesting that the migration of MAIT cells to mucosal tissues is influenced by environmental factors. Profiling of endometrial tissue before and after uterus transplantation showed that endometrial MAIT cells were transiently tissue resident, being replaced by MAIT cells that expressed recipient HLA molecules [180]. While this study showed that decidual MAIT cells from healthy women responded to ex vivo stimulation with N. gonorrhoeae by expressing CD107a and secreting granzyme B, IFNγ, and TNFα [180], the role of MAIT cells in the in vivo context of STIs of the female genital tract has yet to be elucidated.
6. Implications for Vaccine Design
Repeated infections are common for chlamydia, gonorrhea, and syphilis [181,182,183,184], which is evidence for weak acquired natural immunity in humans. This is a major challenge for vaccine development, requiring careful consideration of vaccine platforms, immunogenic antigens, and adjuvants to elicit protective immunity not elicited by the pathogens themselves.
Although acquired immunity from natural infections is weak, there is some evidence for it in the cases of chlamydia and syphilis. For example, prevalence of C. trachomatis infection was inversely correlated with increasing age, lower chlamydial burdens were reported in repeat infections, and resistance to reinfection was increased in women who cleared a C. trachomatis infection without antibiotic treatment [85,185,186]. We also found that women who had continued exposure after an initial C. trachomatis infection but did not experience reinfection over one year had distinct immune profiles, including increased frequencies of CD4 TCM Th1 and Th17 in peripheral blood compared to women who experienced repeat infections [8]. People who became reinfected with syphilis were more likely to have asymptomatic infections and had reduced levels of IL-10 [187,188]. There is no documented evidence of acquired immunity to gonorrhea infections.
The fact that natural infections do not elicit protective immunity in humans creates a challenge for implementing effective vaccines. In fact, natural infections with chlamydia and gonorrhea demonstrate a level of immune evasion by skewing responses toward non-protective phenotypes. Chlamydia infection, for example, drives strong Th2 immunity and antibody responses in humans that are not correlated with protection [6,8,189], whereas Th1 responses are strongly associated with protection in mice and humans but are less frequent in infected individuals [8,88,107]. Similarly, gonorrhea infection drives Th17 responses and depresses Th1/Th2 responses, increasing influx of neutrophils that gonorrhea has mechanisms to resist [23,24]. Traditional vaccines elicit neutralizing antibody responses, which has proven highly effective for some pathogens including HPV (Figure 1). However, antibodies are not associated with protection against chlamydia, and gonorrhea has known mechanisms of antibody evasion, so vaccines that elicit strong T cell-mediated immunity are important for effective protection against bacterial STIs.
While vaccines against chlamydia, gonorrhea, and syphilis are not yet available, there is significant progress being made toward that goal.
6.1. Chlamydia Vaccines
Animal models have been essential for chlamydial vaccine research, offering insights into the infection process, immune response, and potential vaccine efficacy before human trials [10,11]. The most used models include mice, guinea pigs, non-human primates, and koalas. Mice, and the murine pathogen Chlamydia muridarum, are the most widely used model system for in vivo studies of pathogenesis, immunity, and preclinical evaluation of vaccine efficacy thanks to their relatively low cost and wide range of genetic backgrounds and immunological reagents. Guinea pigs and minipigs have genital tract anatomy more like humans than mice, and also serve as important models to evaluate candidate vaccine efficacy. Non-human primates, such as Cynomolgus and Rhesus macaques, closely mimic human genetics and reproductive physiology, making them ideal for studying transmission, immune response, and long-term protection against human genital infections. Koalas, natural hosts for Chlamydia pecorum, provide unique insights into vaccine responses in a naturally susceptible population. Together, these models have contributed to a comprehensive understanding of chlamydial infection and vaccine development.
The first large placebo-controlled human C. trachomatis vaccine trials were completed in the 1960s [190,191,192,193,194,195]. They evaluated protection against ocular trachoma with intramuscularly delivered whole-cell vaccines and found short-lived and, in some cases, strain-specific protection. Since then, there has been significant progress in the field toward vaccine development [196].
One chlamydia vaccine is currently being tested in clinical trials. The first Phase 1 clinical trial (NCT02787109) in healthy women evaluated immunization with CTH522, a recombinant version of the major outer membrane protein (MOMP) from C. trachomatis, formulated with either the liposome-based cationic adjuvant formulation CAF01 or aluminum hydroxide. Three doses of vaccine were delivered intramuscularly (i.m.) followed by two intranasal (i.n.) doses. The study found that both vaccines were safe and immunogenic, and that the CAF01 formulation elicited higher IgG titers, enhanced mucosal antibody responses, and more consistent cell-mediated immune responses than the aluminum hydroxide formulation [12]. Another recently completed Phase 1 trial (NCT03926728) in healthy men and women evaluated a vaccine consisting of three i.m. doses of CTH522-CAF01 or CTH522-CAF09b followed by intradermal or topical ocular administration of CTH522. The study found that both formulations were safe and immunogenic, and that ocular IgA was induced by a topical ocular booster [13,14]. Future clinical trials will evaluate the protective efficacy of CTH522-based vaccines against both ocular and urogenital C. trachomatis infections.
Many other candidate vaccines are in the preclinical development phase in animal models and have been recently reviewed [15,16]. Primary infection of mice with virulent or attenuated C. muridarum provides sterilizing but short-lived immunity against subsequent challenge [10,197,198]. MOMP is the most popular protein target for candidate vaccines, as it makes up approximately 60% of the protein mass of the chlamydial outer membrane [199]. However, monomeric MOMP is challenging to purify from cells. Chlamydial protease-like activation factor (CPAF) and polymorphic outer membrane proteins (Pmp) are other immunogenic proteins that have demonstrated protection against chlamydial challenge in mice [200,201,202,203,204,205,206]. It is also increasingly evident that adjuvants that support Th1 immunity and mucosal routes of immunization may be required for optimal protection [17,108,167,168,207,208].
6.2. Gonorrhea Vaccines
Preclinical testing of N. gonorrhoeae vaccines has been limited by the difficulty of adapting studies of the human-restricted pathogen to animal models [26,27]. However, treating female mice with estradiol to extend estrus and antibiotics to suppress the overgrowth of commensal flora allows colonization of the genital tract with N. gonorrhoeae [28], and such models have improved the ability to study N. gonorrhoeae biology and immunity in vivo. Limitations to these models still exist since N. gonorrhoeae uses human-specific receptors for adherence and invasion pathways, some of which can be addressed by using humanized transgenic mice [209,210]. The N. gonorrhoeae-controlled human infection model (Ng CHIM) is also a valuable model for studying gonorrheal pathogenesis and immunity, but it is only used for male urethral infection due to risk of pathogen ascension in the female genital tract [29]. The mouse and Ng CHIM models are both useful in studies of correlates of immunity and vaccine testing.
There are multiple gonorrheal vaccines in clinical trials. Of note, the US Food and Drug Administration (FDA) granted fast-track designation to GSK’s generalized modules for membrane antigen (GMMA)-based Neisseria Gonorrhoeae GMMA (NgG) vaccine in 2023. GMMA vaccines use genetically modified Gram-negative bacterial pathogens to overproduce outer membrane vesicles (OMV), which are usually produced at relatively low amounts, increasing yield and reducing LPS endotoxicity for upscaled production [30]. The currently ongoing clinical trial (NCT05630859) is a Phase 1/2 trial to evaluate safety and efficacy. Phase 1 was completed with positive safety results and Phase 2 is ongoing, so the immunogenicity and efficacy of the vaccine is yet to be determined. Most other completed and ongoing clinical trials are focused on evaluating the cross-protective efficacy of the currently licensed meningococcal group B vaccine 4CMenB (Bexsero, GSK) against N. meningitidis and have been reviewed recently [31,211]. 4CMenB is composed of (1) fHbp variant 1.1 (subfamily B) fused to the genome-derived Neisseria antigen (GNA) 2091; (2) Neisseria adhesin A (NadA); (3) Neisserial heparin binding antigen (NHBA) peptide 2 fused to GNA1030; and (4) the MeNZB vaccine, composed of N. meningitidis OMVs from a strain isolated in New Zealand containing porin A (PorA) P1.4. Although not all these antigens are homologous to N. gonorrhoeae, NHBA is 68.8% identical, and many of the New Zealand-strain OMV proteins share >90% homology [212], providing opportunity for cross-protection. Serum from Bexsero-immunized people contained antibodies that recognized gonorrheal antigens [213]. Real-world evidence of 4CMenB efficacy against gonorrheal infection includes a study in Canada that found estimated risk reduction of 59% [214], a study in the US that reported vaccine efficacy of 40% [215], and a study in South Australia that found vaccine efficacy of 33% [216]. Recently completed clinical trials (NCT04722003, NCT04094883) evaluated the systemic and local immune responses against N. gonorrhoeae following 4CMenB vaccination, but published results are not yet available. These studies will be important to identify correlates of immunity and to improve vaccines targeted against N. gonorrhoeae infections. Studies in mice showed that 4CMenB vaccination accelerated clearance and reduced N. gonorrhoeae bacterial burden in the female genital tract and elicited vaginal IgG and IgA. However, T cell responses against N. gonorrhoeae elicited by 4CMenB vaccination have yet to be evaluated in mice or humans and are needed considering protection against N. gonorrhoeae in mice is associated with the Th1 immune response [25]. Indeed, intravaginal vaccination of mice with an experimental N. gonorrhoeae OMV vaccine and coadministration of IL-12 generated IFNγ-producing CD4 T cells and accelerated bacterial clearance following N. gonorrhoeae challenge [33]. Investigation of potential recombinant antigens for N. gonorrhoeae subunit vaccines is also ongoing [32].
6.3. Syphilis Vaccines
Syphilis vaccine research is also limited by the lack of in vitro and animal model systems to study T. pallidum. In vitro culture of the organism was first reported in 2018 [39]. Studies of T. pallidum pathogenesis and immunity are primarily conducted in rabbits [38], but immunological reagents are severely lacking for this model system. Non-human primates and hamsters have also been used to model T. pallidum infection [217,218], but these studies are limited. A C57BL/6 model was recently discovered and has potential to be a useful tool for future immunological research, but infected mice lack clinical manifestations [40].
Heat- or penicillin-inactivated T. pallidum was shown to provide partial protection in rabbits [219]. However, the fragility of the T. pallidum outer membrane and the lack, until recently, of in vitro models for production of large quantities of organisms for use in vaccines has limited their study. Experimental DNA vaccines have demonstrated attenuated lesions and decreased bacterial burden in rabbit models [220,221,222], and experimental recombinant protein vaccines have demonstrated some success as well (recently reviewed in [223]). So far, none of these vaccines have moved forward to human trials, but the recent advances in in vitro culture and animal models will be important tools for future immunological evaluation of candidate vaccines.
7. Conclusions
Prevalence of bacterial sexually transmitted infections (STIs) chlamydia, gonorrhea, and syphilis is inversely proportional to the occurrence of symptoms. These infections not only impact sexually active adolescents and adults but also pose serious risks to newborns through mother to child transmission. Current public health interventions include use of barrier methods, doxycycline post-exposure prophylaxis for men who have sex with men (MSM), and increased diagnostic surveillance and reporting [45], but effective vaccines are not available for disease prevention. A significant challenge in understanding immunity to these infections is that natural infection does not confer strong protective immunity, as these pathogens have developed mechanisms to evade both innate and adaptive host immune responses. This review focuses on adaptive immunity, but innate immune evasion by these pathogens has been reviewed elsewhere [32,224,225,226]. These immune evasion mechanisms underscore the importance of generating protective T cell responses with effective vaccines. Recent advances in understanding the quality of cellular responses needed, such as CD4 Th1 responses for C. trachomatis and N. gonorrhoeae, and the availability of Th1-inducing adjuvants, offer hope for the development of effective vaccines. Additionally, the establishment of models for testing syphilis vaccines represents a critical step forward. These aspects together, as summarized in Table 1, demonstrate that continued research into the immunological mechanisms is essential for continued vaccine development.
Author Contributions
Conceptualization, K.S.Y. and T.D.; writing, writing—original draft preparation, K.S.Y. and T.D.; writing—review and editing, K.S.Y. and T.D.; visualization, K.S.Y.; supervision, T.D. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This work was supported by the National Institute of Allergy and Infectious Diseases through U19AI144181 and R01AI170959. K.S.Y. received funding from UNC STI/HIV T32 postdoctoral training grant AI007001 and The American Association of Immunologists Intersect Fellowship Program for Computational Scientists and Immunologists.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Zheng Y., Yu Q., Lin Y., Zhou Y., Lan L., Yang S., Wu J. Global Burden and Trends of Sexually Transmitted Infections from 1990 to 2019: An Observational Trend Study. Lancet Infect. Dis. 2022;22:541–551. doi: 10.1016/S1473-3099(21)00448-5. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control . Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States, 2018. NCHHSTP Newsroom; CDC; Atlanta, GA, USA: 2018. [Google Scholar]
- 3.Nelson R. Syphilis Rates Soar in the USA Amid Penicillin Shortage. Lancet. 2023;402:515. doi: 10.1016/S0140-6736(23)01665-3. [DOI] [PubMed] [Google Scholar]
- 4.Bastidas R.J., Elwell C.A., Engel J.N., Valdivia R.H. Chlamydial Intracellular Survival Strategies. Cold Spring Harb. Perspect. Med. 2013;3:a010256. doi: 10.1101/cshperspect.a010256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajeeve K., Das S., Prusty B.K., Rudel T. Chlamydia Trachomatis Paralyses Neutrophils to Evade the Host Innate Immune Response. Nat. Microbiol. 2018;3:824–835. doi: 10.1038/s41564-018-0182-y. [DOI] [PubMed] [Google Scholar]
- 6.Russell A.N., Zheng X., O’Connell C.M., Taylor B.D., Wiesenfeld H.C., Hillier S.L., Zhong W., Darville T. Analysis of Factors Driving Incident and Ascending Infection and the Role of Serum Antibody in Chlamydia trachomatis Genital Tract Infection. J. Infect. Dis. 2016;213:523–531. doi: 10.1093/infdis/jiv438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu C., Hufnagel K., O’Connell C.M., Goonetilleke N., Mokashi N., Waterboer T., Tollison T.S., Peng X., Wiesenfeld H.C., Hillier S.L., et al. Reduced Endometrial Ascension and Enhanced Reinfection Associated with Immunoglobulin G Antibodies to Specific Chlamydia trachomatis Proteins in Women at Risk for Chlamydia. J. Infect. Dis. 2022;225:846–855. doi: 10.1093/infdis/jiab496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yount K.S., Kollipara A., Liu C., Zheng X., O’Connell C.M., Bagwell B., Wiesenfeld H.C., Hillier S.L., Darville T. Unique T Cell Signatures Are Associated with Reduced Chlamydia trachomatis Reinfection in a Highly Exposed Cohort. bioRxiv. 2023 bioRxiv: 2023.08.02.551709. [Google Scholar]
- 9.Beatty W.L., Belanger T.A., Desai A.A., Morrison R.P., Byrne G.I. Tryptophan Depletion as a Mechanism of Gamma Interferon-Mediated Chlamydial Persistence. Infect. Immun. 1994;62:3705–3711. doi: 10.1128/iai.62.9.3705-3711.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rank R.G., Whittum-Hudson J.A. Protective Immunity to Chlamydial Genital Infection: Evidence from Animal Studies. J. Infect. Dis. 2010;201((Suppl. S2)):S168–S177. doi: 10.1086/652399. [DOI] [PubMed] [Google Scholar]
- 11.Clercq E.D., Kalmar I., Vanrompay D. Animal Models for Studying Female Genital Tract Infection with Chlamydia Trachomatis. Infect. Immun. 2013;81:3060–3067. doi: 10.1128/IAI.00357-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abraham S., Juel H.B., Bang P., Cheeseman H.M., Dohn R.B., Cole T., Kristiansen M.P., Korsholm K.S., Lewis D., Olsen A.W., et al. Safety and Immunogenicity of the Chlamydia Vaccine Candidate Cth522 Adjuvanted with Caf01 Liposomes or Aluminium Hydroxide: A First-in-Human, Randomised, Double-Blind, Placebo-Controlled, Phase 1 Trial. Lancet Infect. Dis. 2019;19:1091–1100. doi: 10.1016/S1473-3099(19)30279-8. [DOI] [PubMed] [Google Scholar]
- 13.Olsen A.W., Rosenkrands I., Jacobsen C.S., Cheeseman H.M., Kristiansen M.P., Dietrich J., Shattock R.J., Follmann F. Immune Signature of Chlamydia Vaccine Cth522/Caf®01 Translates from Mouse-to-Human and Induces Durable Protection in Mice. Nat. Commun. 2024;15:1665. doi: 10.1038/s41467-024-45526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pollock K.M., Borges Á.H., Cheeseman H.M., Rosenkrands I., Schmidt K.L., Søndergaard R.E., Day S., Evans A., McFarlane L.R., Joypooranachandran J., et al. An Investigation of Trachoma Vaccine Regimens by the Chlamydia Vaccine Cth522 Administered with Cationic Liposomes in Healthy Adults (Chlm-02): A Phase 1, Double-Blind Trial. Lancet Infect. Dis. 2024;24:829–844. doi: 10.1016/S1473-3099(24)00147-6. [DOI] [PubMed] [Google Scholar]
- 15.de la Maza L.M., Darville T.L., Pal S. Chlamydia Trachomatis Vaccines for Genital Infections: Where Are We and How Far Is There to Go? Expert. Rev. Vaccines. 2021;20:421–435. doi: 10.1080/14760584.2021.1899817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borges Á.H., Follmann F., Dietrich J. Chlamydia Trachomatis Vaccine Development—A View on the Current Challenges and How to Move Forward. Expert. Rev. Vaccines. 2022;21:1555–1567. doi: 10.1080/14760584.2022.2117694. [DOI] [PubMed] [Google Scholar]
- 17.Poston T.B. Advances in Vaccine Development for Chlamydia trachomatis. Pathog. Dis. 2024:ftae017. doi: 10.1093/femspd/ftae017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stern A., Brown M., Nickel P., Meyer T.F. Opacity Genes in Neisseria Gonorrhoeae: Control of Phase and Antigenic Variation. Cell. 1986;47:61–71. doi: 10.1016/0092-8674(86)90366-1. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y., Liu W., Russell M.W. Suppression of Host Adaptive Immune Responses by Neisseria Gonorrhoeae: Role of Interleukin 10 and Type 1 Regulatory T Cells. Mucosal Immunol. 2014;7:165–176. doi: 10.1038/mi.2013.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J.J., Zhou D., Mandrell R.E., Griffiss J.M. Effect of Exogenous Sialylation of the Lipooligosaccharide of Neisseria Gonorrhoeae on Opsonophagocytosis. Infect. Immun. 1992;60:4439–4442. doi: 10.1128/iai.60.10.4439-4442.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ngampasutadol J., Ram S., Gulati S., Agarwal S., Li C., Visintin A., Monks B., Madico G., Rice P.A. Human Factor H Interacts Selectively with Neisseria Gonorrhoeae and Results in Species-Specific Complement Evasion. J. Immunol. 2008;180:3426–3435. doi: 10.4049/jimmunol.180.5.3426. [DOI] [PubMed] [Google Scholar]
- 22.Pohlner J., Halter R., Beyreuther K., Meyer T.F. Gene Structure and Extracellular Secretion of Neisseria Gonorrhoeae Iga Protease. Nature. 1987;325:458–462. doi: 10.1038/325458a0. [DOI] [PubMed] [Google Scholar]
- 23.Liu Y., Islam E.A., Jarvis G.A., Gray-Owen S.D., Russell M.W. Neisseria Gonorrhoeae Selectively Suppresses the Development of Th1 and Th2 Cells, and Enhances Th17 Cell Responses, through TGF-β-Dependent Mechanisms. Mucosal Immunol. 2012;5:320–331. doi: 10.1038/mi.2012.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palmer A., Criss A.K. Gonococcal Defenses against Antimicrobial Activities of Neutrophils. Trends Microbiol. 2018;26:1022–1034. doi: 10.1016/j.tim.2018.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y., Russell M.W. Diversion of the Immune Response to Neisseria Gonorrhoeae from Th17 to Th1/Th2 by Treatment with Anti-Transforming Growth Factor β Antibody Generates Immunological Memory and Protective Immunity. mBio. 2011;2:e00095-11. doi: 10.1128/mBio.00095-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Girgis M.M., Christodoulides M. Vertebrate and Invertebrate Animal and New In Vitro Models for Studying Neisseria Biology. Pathogens. 2023;12:782. doi: 10.3390/pathogens12060782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rice P.A., Shafer W.M., Ram S., Jerse A.E. Neisseria Gonorrhoeae: Drug Resistance, Mouse Models, and Vaccine Development. Annu. Rev. Microbiol. 2017;71:665–686. doi: 10.1146/annurev-micro-090816-093530. [DOI] [PubMed] [Google Scholar]
- 28.Jerse A.E. Experimental Gonococcal Genital Tract Infection and Opacity Protein Expression in Estradiol-Treated Mice. Infect. Immun. 1999;67:5699–5708. doi: 10.1128/IAI.67.11.5699-5708.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waltmann A., Duncan J.A., Pier G.B., Cywes-Bentley C., Cohen M.S., Hobbs M.M. Experimental Urethral Infection with Neisseria Gonorrhoeae. Curr. Top. Microbiol. Immunol. 2022 doi: 10.1007/82_2021_250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mancini F., Micoli F., Necchi F., Pizza M., Berlanda Scorza F., Rossi O. GMMA-Based Vaccines: The Known and the Unknown. Front. Immunol. 2021;12:715393. doi: 10.3389/fimmu.2021.715393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruiz García Y., Sohn W.Y., Seib K.L., Taha M.K., Vázquez J.A., de Lemos A.P.S., Vadivelu K., Pizza M., Rappuoli R., Bekkat-Berkani R. Looking Beyond Meningococcal B with the 4CMenB Vaccine: The Neisseria Effect. NPJ Vaccines. 2021;6:130. doi: 10.1038/s41541-021-00388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russell M.W., Jerse A.E., Gray-Owen S.D. Progress toward a Gonococcal Vaccine: The Way Forward. Front. Immunol. 2019;10:2417. doi: 10.3389/fimmu.2019.02417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Y., Hammer L.A., Liu W., Hobbs M.M., Zielke R.A., Sikora A.E., Jerse A.E., Egilmez N.K., Russell M.W. Experimental Vaccine Induces Th1-Driven Immune Responses and Resistance to Neisseria Gonorrhoeae Infection in a Murine Model. Mucosal Immunol. 2017;10:1594–1608. doi: 10.1038/mi.2017.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Addetia A., Tantalo L.C., Lin M.J., Xie H., Huang M.-L., Marra C.M., Greninger A.L. Comparative Genomics and Full-Length Tprk Profiling of Treponema Pallidum Subsp. Pallidum Reinfection. PLOS Neglected Trop. Dis. 2020;14:e0007921. doi: 10.1371/journal.pntd.0007921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ávila-Nieto C., Pedreño-López N., Mitjà O., Clotet B., Blanco J., Carrillo J. Syphilis Vaccine: Challenges, Controversies and Opportunities. Front. Immunol. 2023;14:1126170. doi: 10.3389/fimmu.2023.1126170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baker-Zander S.A., Lukehart S.A. Macrophage-Mediated Killing of Opsonized Treponema Pallidum. J. Infect. Dis. 1992;165:69–74. doi: 10.1093/infdis/165.1.69. [DOI] [PubMed] [Google Scholar]
- 37.Hawley K.L., Cruz A.R., Benjamin S.J., La Vake C.J., Cervantes J.L., LeDoyt M., Ramirez L.G., Mandich D., Fiel-Gan M., Caimano M.J., et al. IFNγ Enhances Cd64-Potentiated Phagocytosis of Treponema Pallidum Opsonized with Human Syphilitic Serum by Human Macrophages. Front. Immunol. 2017;8:1227. doi: 10.3389/fimmu.2017.01227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baker-Zander S., Sell S. A Histopathologic and Immunologic Study of the Course of Syphilis in the Experimentally Infected Rabbit. Demonstration of Long-Lasting Cellular Immunity. Am. J. Pathol. 1980;101:387–414. [PMC free article] [PubMed] [Google Scholar]
- 39.Edmondson D.G., Hu B., Norris S.J. Long-Term In Vitro Culture of the Syphilis Spirochete Treponema Pallidum Subsp. Pallidum. mBio. 2018;9:e01153-18. doi: 10.1128/mBio.01153-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lu S., Zheng K., Wang J., Xu M., Xie Y., Yuan S., Wang C., Wu Y. Characterization of Treponema Pallidum Dissemination in C57bl/6 Mice. Front. Immunol. 2020;11:577129. doi: 10.3389/fimmu.2020.577129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lithgow K.V., Cameron C.E. Vaccine Development for Syphilis. Expert. Rev. Vaccines. 2017;16:37–44. doi: 10.1080/14760584.2016.1203262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Connell C.M., Ferone M.E. Chlamydia Trachomatis Genital Infections. Microb. Cell. 2016;3:390–403. doi: 10.15698/mic2016.09.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control Sexually Transmitted Infections Surveillance: National Overview of Stis. [(accessed on 26 July 2024)];2022 Available online: https://www.cdc.gov/std/statistics/2022/overview.htm.
- 44.Thompson E.L., Griner S.B., Galvin A.M., Lowery A.D., Lewis M.A. Correlates of Sti Testing among Us Young Adults: Opportunities for Prevention. Prev. Sci. 2021;22:216–226. doi: 10.1007/s11121-020-01179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Workowski K.A., Bachmann L.H., Chan P.A., Johnston C.M., Muzny C.A., Park I., Reno H., Zenilman J.M., Bolan G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm. Rep. 2021;70:1–187. doi: 10.15585/mmwr.rr7004a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Molano M., Meijer C.J., Weiderpass E., Arslan A., Posso H., Franceschi S., Ronderos M., Muñoz N., van den Brule A.J. The Natural Course of Chlamydia Trachomatis Infection in Asymptomatic Colombian Women: A 5-Year Follow-Up Study. J. Infect. Dis. 2005;191:907–916. doi: 10.1086/428287. [DOI] [PubMed] [Google Scholar]
- 47.Johnson M.B., Criss A.K. Resistance of Neisseria Gonorrhoeae to Neutrophils. Front. Microbiol. 2011;2:77. doi: 10.3389/fmicb.2011.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Snyder L.A.S., Butcher S.A., Saunders N.J. Comparative Whole-Genome Analyses Reveal over 100 Putative Phase-Variable Genes in the Pathogenic Neisseria spp. Microbiology. 2001;147:2321–2332. doi: 10.1099/00221287-147-8-2321. [DOI] [PubMed] [Google Scholar]
- 49.Belcher T., Rollier C.S., Dold C., Ross J.D.C., MacLennan C.A. Immune Responses to Neisseria Gonorrhoeae and Implications for Vaccine Development. Front. Immunol. 2023;14:1248613. doi: 10.3389/fimmu.2023.1248613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Unemo M., Seifert H.S., Hook E.W., 3rd, Hawkes S., Ndowa F., Dillon J.R. Gonorrhoea. Nat. Rev. Dis. Primers. 2019;5:79. doi: 10.1038/s41572-019-0128-6. [DOI] [PubMed] [Google Scholar]
- 51.Peeling R.W., Mabey D., Kamb M.L., Chen X.-S., Radolf J.D., Benzaken A.S. Syphilis. Nat. Rev. Dis. Primers. 2017;3:17073. doi: 10.1038/nrdp.2017.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brown D.L., Frank J.E. Diagnosis and Management of Syphilis. Am. Fam. Physician. 2003;68:283–290. [PubMed] [Google Scholar]
- 53.Whiting C., Schwartzman G., Khachemoune A. Syphilis in Dermatology: Recognition and Management. Am. J. Clin. Dermatol. 2023;24:287–297. doi: 10.1007/s40257-022-00755-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McDonald R., O’Callaghan K., Torrone E., Barbee L., Grey J., Jackson D., Woodworth K., Olsen E., Ludovic J., Mayes N., et al. Vital Signs: Missed Opportunities for Preventing Congenital Syphilis—United States, 2022. MMWR Morb. Mortal. Wkly. Rep. 2023;72:1269–1274. doi: 10.15585/mmwr.mm7246e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thean L., Moore A., Nourse C. New Trends in Congenital Syphilis: Epidemiology, Testing in Pregnancy, and Management. Curr. Opin. Infect. Dis. 2022;35:452–460. doi: 10.1097/QCO.0000000000000875. [DOI] [PubMed] [Google Scholar]
- 56.Amanna I.J., Slifka M.K. Mechanisms That Determine Plasma Cell Lifespan and the Duration of Humoral Immunity. Immunol. Rev. 2010;236:125–138. doi: 10.1111/j.1600-065X.2010.00912.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Caldwell H.D., Perry L.J. Neutralization of Chlamydia Trachomatis Infectivity with Antibodies to the Major Outer Membrane Protein. Infect. Immun. 1982;38:745–754. doi: 10.1128/iai.38.2.745-754.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hybiske K., Stephens R.S. Mechanisms of Chlamydia Trachomatis Entry into Nonphagocytic Cells. Infect. Immun. 2007;75:3925–3934. doi: 10.1128/IAI.00106-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bastidas R.J., Valdivia R.H. The Emerging Complexity of Chlamydia Trachomatis Interactions with Host Cells as Revealed by Molecular Genetic Approaches. Curr. Opin. Microbiol. 2023;74:102330. doi: 10.1016/j.mib.2023.102330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Su H., Parnell M., Caldwell H.D. Protective Efficacy of a Parenterally Administered Momp-Derived Synthetic Oligopeptide Vaccine in a Murine Model of Chlamydia Trachomatis Genital Tract Infection: Serum Neutralizing Igg Antibodies Do Not Protect against Chlamydial Genital Tract Infection. Vaccine. 1995;13:1023–1032. doi: 10.1016/0264-410X(95)00017-U. [DOI] [PubMed] [Google Scholar]
- 61.Cotter T.W., Meng Q., Shen Z.L., Zhang Y.X., Su H., Caldwell H.D. Protective Efficacy of Major Outer Membrane Protein-Specific Immunoglobulin a (Iga) and Igg Monoclonal Antibodies in a Murine Model of Chlamydia Trachomatis Genital Tract Infection. Infect. Immun. 1995;63:4704–4714. doi: 10.1128/iai.63.12.4704-4714.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morrison S.G., Su H., Caldwell H.D., Morrison R.P. Immunity to Murine Chlamydia Trachomatis Genital Tract Reinfection Involves B Cells and Cd4(+) T Cells but Not Cd8(+) T Cells. Infect. Immun. 2000;68:6979–6987. doi: 10.1128/IAI.68.12.6979-6987.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morrison S.G., Morrison R.P. Resolution of Secondary Chlamydia Trachomatis Genital Tract Infection in Immune Mice with Depletion of Both Cd4+ and Cd8+ T Cells. Infect. Immun. 2001;69:2643–2649. doi: 10.1128/IAI.69.4.2643-2649.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morrison S.G., Morrison R.P. A Predominant Role for Antibody in Acquired Immunity to Chlamydial Genital Tract Reinfection. J. Immunol. 2005;175:7536–7542. doi: 10.4049/jimmunol.175.11.7536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Naglak E.K., Morrison S.G., Morrison R.P. IFNγ Is Required for Optimal Antibody-Mediated Immunity against Genital Chlamydia Infection. Infect. Immun. 2016;84:3232–3242. doi: 10.1128/IAI.00749-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schiff D.E., Rae J., Martin T.R., Davis B.H., Curnutte J.T. Increased Phagocyte Fc Gammari Expression and Improved Fc Gamma-Receptor-Mediated Phagocytosis after In Vivo Recombinant Human Interferon-Gamma Treatment of Normal Human Subjects. Blood. 1997;90:3187–3194. doi: 10.1182/blood.V90.8.3187. [DOI] [PubMed] [Google Scholar]
- 67.Naglak E.K., Morrison S.G., Morrison R.P. Neutrophils Are Central to Antibody-Mediated Protection against Genital Chlamydia. Infect. Immun. 2017;85:e00409-17. doi: 10.1128/IAI.00409-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tseng C.T., Rank R.G. Role of NK Cells in Early Host Response to Chlamydial Genital Infection. Infect. Immun. 1998;66:5867–5875. doi: 10.1128/IAI.66.12.5867-5875.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moore T., Ananaba G.A., Bolier J., Bowers S., Belay T., Eko F.O., Igietseme J.U. Fc Receptor Regulation of Protective Immunity against Chlamydia Trachomatis. Immunology. 2002;105:213–221. doi: 10.1046/j.0019-2805.2001.01354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Trifonova R.T., Lieberman J., van Baarle D. Distribution of Immune Cells in the Human Cervix and Implications for Hiv Transmission. Am. J. Reprod. Immunol. 2014;71:252–264. doi: 10.1111/aji.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Johansson E.L., Rudin A., Wassén L., Holmgren J. Distribution of Lymphocytes and Adhesion Molecules in Human Cervix and Vagina. Immunology. 1999;96:272–277. doi: 10.1046/j.1365-2567.1999.00675.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roopenian D.C., Akilesh S. FcRn: The Neonatal Fc Receptor Comes of Age. Nat. Rev. Immunol. 2007;7:715–725. doi: 10.1038/nri2155. [DOI] [PubMed] [Google Scholar]
- 73.Knee R.A., Hickey D.K., Beagley K.W., Jones R.C. Transport of Igg across the Blood-Luminal Barrier of the Male Reproductive Tract of the Rat and the Effect of Estradiol Administration on Reabsorption of Fluid and Igg by the Epididymal Ducts. Biol. Reprod. 2005;73:688–694. doi: 10.1095/biolreprod.105.041079. [DOI] [PubMed] [Google Scholar]
- 74.Li Z., Palaniyandi S., Zeng R., Tuo W., Roopenian D.C., Zhu X. Transfer of Igg in the Female Genital Tract by Mhc Class I-Related Neonatal Fc Receptor (Fcrn) Confers Protective Immunity to Vaginal Infection. Proc. Natl. Acad. Sci. USA. 2011;108:4388–4393. doi: 10.1073/pnas.1012861108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Armitage C.W., O’Meara C.P., Harvie M.C., Timms P., Blumberg R.S., Beagley K.W. Divergent Outcomes Following Transcytosis of Igg Targeting Intracellular and Extracellular Chlamydial Antigens. Immunol. Cell Biol. 2014;92:417–426. doi: 10.1038/icb.2013.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hackstadt T., Scidmore-Carlson M.A., Shaw E.I., Fischer E.R. The Chlamydia Trachomatis Inca Protein Is Required for Homotypic Vesicle Fusion. Cell Microbiol. 1999;1:119–130. doi: 10.1046/j.1462-5822.1999.00012.x. [DOI] [PubMed] [Google Scholar]
- 77.Rzomp K.A., Moorhead A.R., Scidmore M.A. The Gtpase Rab4 Interacts with Chlamydia Trachomatis Inclusion Membrane Protein Ct229. Infect. Immun. 2006;74:5362–5373. doi: 10.1128/IAI.00539-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kutteh W.H., Prince S.J., Hammond K.R., Kutteh C.C., Mestecky J. Variations in Immunoglobulins and Iga Subclasses of Human Uterine Cervical Secretions around the Time of Ovulation. Clin. Exp. Immunol. 1996;104:538–542. doi: 10.1046/j.1365-2249.1996.36742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brandtzaeg P. Mucosal Immunity in the Female Genital Tract. J. Reprod. Immunol. 1997;36:23–50. doi: 10.1016/S0165-0378(97)00061-2. [DOI] [PubMed] [Google Scholar]
- 80.Perez-Lopez A., Behnsen J., Nuccio S.-P., Raffatellu M. Mucosal Immunity to Pathogenic Intestinal Bacteria. Nat. Rev. Immunol. 2016;16:135–148. doi: 10.1038/nri.2015.17. [DOI] [PubMed] [Google Scholar]
- 81.Morrison S.G., Morrison R.P. The Protective Effect of Antibody in Immunity to Murine Chlamydial Genital Tract Reinfection Is Independent of Immunoglobulin A. Infect. Immun. 2005;73:6183–6186. doi: 10.1128/IAI.73.9.6183-6186.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Woodhall S.C., Gorwitz R.J., Migchelsen S.J., Gottlieb S.L., Horner P.J., Geisler W.M., Winstanley C., Hufnagel K., Waterboer T., Martin D.L., et al. Advancing the Public Health Applications of Chlamydia Trachomatis Serology. Lancet Infect. Dis. 2018;18:e399–e407. doi: 10.1016/S1473-3099(18)30159-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Albritton H.L., Kozlowski P.A., Lillis R.A., McGowin C.L., Siren J.D., Taylor S.N., Ibana J.A., Buckner L.R., Shen L., Quayle A.J. A Novel Whole-Bacterial Enzyme Linked-Immunosorbant Assay to Quantify Chlamydia Trachomatis Specific Antibodies Reveals Distinct Differences between Systemic and Genital Compartments. PLoS ONE. 2017;12:e0183101. doi: 10.1371/journal.pone.0183101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Batteiger B.E., Fraiz J., Newhall W.J., Katz B.P., Jones R.B. Association of Recurrent Chlamydial Infection with Gonorrhea. J. Infect. Dis. 1989;159:661–669. doi: 10.1093/infdis/159.4.661. [DOI] [PubMed] [Google Scholar]
- 85.Batteiger B.E., Tu W., Ofner S., Van Der Pol B., Stothard D.R., Orr D.P., Katz B.P., Fortenberry J.D. Repeated Chlamydia Trachomatis Genital Infections in Adolescent Women. J. Infect. Dis. 2010;201:42–51. doi: 10.1086/648734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Blythe M.J., Katz B.P., Batteiger B.E., Ganser J.A., Jones R.B. Recurrent Genitourinary Chlamydial Infections in Sexually Active Female Adolescents. J. Pediatr. 1992;121:487–493. doi: 10.1016/S0022-3476(05)81812-8. [DOI] [PubMed] [Google Scholar]
- 87.Brunham R.C., Kimani J., Bwayo J., Maitha G., Maclean I., Yang C., Shen C., Roman S., Nagelkerke N.J., Cheang M., et al. The Epidemiology of Chlamydia Trachomatis within a Sexually Transmitted Diseases Core Group. J. Infect. Dis. 1996;173:950–956. doi: 10.1093/infdis/173.4.950. [DOI] [PubMed] [Google Scholar]
- 88.Russell A.N., Zheng X., O‘Connell C.M., Wiesenfeld H.C., Hillier S.L., Taylor B.D., Picard M.D., Flechtner J.B., Zhong W., Frazer L.C., et al. Identification of Chlamydia trachomatis Antigens Recognized by T Cells From Highly Exposed Women Who Limit or Resist Genital Tract Infection. J Infect Dis. 2016;214:1884–1892. doi: 10.1093/infdis/jiw485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ness R.B., Soper D.E., Richter H.E., Randall H., Peipert J.F., Nelson D.B., Schubeck D., McNeeley S.G., Trout W., Bass D.C., et al. Chlamydia Antibodies, Chlamydia Heat Shock Protein, and Adverse Sequelae after Pelvic Inflammatory Disease: The PID Evaluation and Clinical Health (Peach) Study. Sex. Transm. Dis. 2008;35:129–135. doi: 10.1097/OLQ.0b013e3181557c25. [DOI] [PubMed] [Google Scholar]
- 90.Tiitinen A., Surcel H.M., Halttunen M., Birkelund S., Bloigu A., Christiansen G., Koskela P., Morrison S.G., Morrison R.P., Paavonen J. Chlamydia Trachomatis and Chlamydial Heat Shock Protein 60-Specific Antibody and Cell-Mediated Responses Predict Tubal Factor Infertility. Hum. Reprod. 2006;21:1533–1538. doi: 10.1093/humrep/del014. [DOI] [PubMed] [Google Scholar]
- 91.El Hakim E.A., Gordon U.D., Akande V.A. The Relationship between Serum Chlamydia Antibody Levels and Severity of Disease in Infertile Women with Tubal Damage. Arch. Gynecol. Obs. 2010;281:727–733. doi: 10.1007/s00404-009-1225-7. [DOI] [PubMed] [Google Scholar]
- 92.Chen K., Magri G., Grasset E.K., Cerutti A. Rethinking Mucosal Antibody Responses: Igm, Igg and Igd Join Iga. Nat. Rev. Immunol. 2020;20:427–441. doi: 10.1038/s41577-019-0261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hedges S.R., Mayo M.S., Mestecky J., Hook E.W., 3rd, Russell M.W. Limited Local and Systemic Antibody Responses to Neisseria Gonorrhoeae during Uncomplicated Genital Infections. Infect. Immun. 1999;67:3937–3946. doi: 10.1128/IAI.67.8.3937-3946.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hedges S.R., Sibley D.A., Mayo M.S., Hook E.W., 3rd, Russell M.W. Cytokine and Antibody Responses in Women Infected with Neisseria Gonorrhoeae: Effects of Concomitant Infections. J. Infect. Dis. 1998;178:742–751. doi: 10.1086/515372. [DOI] [PubMed] [Google Scholar]
- 95.Lukehart S.A., Baker-Zander S.A., Sell S. Characterization of the Humoral Immune Response of the Rabbit to Antigens of Treponema Pallidum after Experimental Infection and Therapy. Sex. Transm. Dis. 1986;13:9–15. doi: 10.1097/00007435-198601000-00003. [DOI] [PubMed] [Google Scholar]
- 96.Leader B.T., Hevner K., Molini B.J., Barrett L.K., Van Voorhis W.C., Lukehart S.A. Antibody Responses Elicited against the Treponema Pallidum Repeat Proteins Differ during Infection with Different Isolates of Treponema Pallidum subsp. Pallidum. Infect. Immun. 2003;71:6054–6057. doi: 10.1128/IAI.71.10.6054-6057.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Baker-Zander S.A., Hook E.W., 3rd, Bonin P., Handsfield H.H., Lukehart S.A. Antigens of Treponema Pallidum Recognized by Igg and Igm Antibodies during Syphilis in Humans. J. Infect. Dis. 1985;151:264–272. doi: 10.1093/infdis/151.2.264. [DOI] [PubMed] [Google Scholar]
- 98.Bishop N.H., Miller J.N. Humoral Immunity in Experimental Syphilis. I. The Demonstration of Resistance Conferred by Passive Immunization. J. Immunol. 1976;117:191–196. doi: 10.4049/jimmunol.117.1.191. [DOI] [PubMed] [Google Scholar]
- 99.Schell R.F., Chan J.K., Le Frock J.L. Endemic Syphilis: Passive transfer of Resistance with Serum and Cells in Hamsters. J. Infect. Dis. 1979;140:378–383. doi: 10.1093/infdis/140.3.378. [DOI] [PubMed] [Google Scholar]
- 100.Cruz A.R., Ramirez L.G., Zuluaga A.V., Pillay A., Abreu C., Valencia C.A., La Vake C., Cervantes J.L., Dunham-Ems S., Cartun R., et al. Immune Evasion and Recognition of the Syphilis Spirochete in Blood and Skin of Secondary Syphilis Patients: Two Immunologically Distinct Compartments. PLoS Negl. Trop. Dis. 2012;6:e1717. doi: 10.1371/journal.pntd.0001717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dong C. Cytokine Regulation and Function in T Cells. Annu. Rev. Immunol. 2021;39:51–76. doi: 10.1146/annurev-immunol-061020-053702. [DOI] [PubMed] [Google Scholar]
- 102.Amezcua Vesely M.C., Pallis P., Bielecki P., Low J.S., Zhao J., Harman C.C.D., Kroehling L., Jackson R., Bailis W., Licona-Limon P., et al. Effector T(H)17 Cells Give Rise to Long-Lived T(Rm) Cells That Are Essential for an Immediate Response against Bacterial Infection. Cell. 2019;178:1176–1188.e15. doi: 10.1016/j.cell.2019.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yang X., Hayglass K.T., Brunham R.C. Different Roles Are Played by Alpha Beta and Gamma Delta T Cells in Acquired Immunity to Chlamydia Trachomatis Pulmonary Infection. Immunology. 1998;94:469–475. doi: 10.1046/j.1365-2567.1998.00549.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Morrison R.P., Feilzer K., Tumas D.B. Gene Knockout Mice Establish a Primary Protective Role for Major Histocompatibility Complex Class Ii-Restricted Responses in Chlamydia Trachomatis Genital Tract Infection. Infect. Immun. 1995;63:4661–4668. doi: 10.1128/iai.63.12.4661-4668.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Magee D.M., Igietseme J.U., Smith J.G., Bleicker C.A., Grubbs B.G., Schachter J., Rank R.G., Williams D.M. Chlamydia Trachomatis Pneumonia in the Severe Combined Immunodeficiency (SCID) Mouse. Reg. Immunol. 1993;5:305–311. [PubMed] [Google Scholar]
- 106.Su H., Feilzer K., Caldwell H.D., Morrison R.P. Chlamydia Trachomatis Genital Tract Infection of Antibody-Deficient Gene Knockout Mice. Infect. Immun. 1997;65:1993–1999. doi: 10.1128/iai.65.6.1993-1999.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Perry L.L., Feilzer K., Caldwell H.D. Immunity to Chlamydia Trachomatis Is Mediated by T Helper 1 Cells through Ifn-Gamma-Dependent and -Independent Pathways. J. Immunol. 1997;158:3344–3352. doi: 10.4049/jimmunol.158.7.3344. [DOI] [PubMed] [Google Scholar]
- 108.Stary G., Olive A., Radovic-Moreno A.F., Gondek D., Alvarez D., Basto P.A., Perro M., Vrbanac V.D., Tager A.M., Shi J., et al. A Mucosal Vaccine against Chlamydia Trachomatis Generates Two Waves of Protective Memory T Cells. Science. 2015;348:aaa8205. doi: 10.1126/science.aaa8205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rixon J.A., Depew C.E., McSorley S.J. Th1 Cells Are Dispensable for Primary Clearance of Chlamydia from the Female Reproductive Tract of Mice. PLoS Pathog. 2022;18:e1010333. doi: 10.1371/journal.ppat.1010333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lampe M.F., Wilson C.B., Bevan M.J., Starnbach M.N. Gamma Interferon Production by Cytotoxic T Lymphocytes Is Required for Resolution of Chlamydia Trachomatis Infection. Infect. Immun. 1998;66:5457–5461. doi: 10.1128/IAI.66.11.5457-5461.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nelson D.E., Virok D.P., Wood H., Roshick C., Johnson R.M., Whitmire W.M., Crane D.D., Steele-Mortimer O., Kari L., McClarty G., et al. Chlamydial IFN-γ Immune Evasion Is Linked to Host Infection Tropism. Proc. Natl. Acad. Sci. USA. 2005;102:10658–10663. doi: 10.1073/pnas.0504198102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hawkins R.A., Rank R.G., Kelly K.A. A Chlamydia Trachomatis-Specific Th2 Clone Does Not Provide Protection against a Genital Infection and Displays Reduced Trafficking to the Infected Genital Mucosa. Infect. Immun. 2002;70:5132–5139. doi: 10.1128/IAI.70.9.5132-5139.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Khader S.A., Gaffen S.L., Kolls J.K. Th17 Cells at the Crossroads of Innate and Adaptive Immunity against Infectious Diseases at the Mucosa. Mucosal Immunol. 2009;2:403–411. doi: 10.1038/mi.2009.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Paroli M., Caccavale R., Fiorillo M.T., Spadea L., Gumina S., Candela V., Paroli M.P. The Double Game Played by Th17 Cells in Infection: Host Defense and Immunopathology. Pathogens. 2022;11:1547. doi: 10.3390/pathogens11121547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Vicetti Miguel R.D., Harvey S.A.K., LaFramboise W.A., Reighard S.D., Matthews D.B., Cherpes T.L. Human Female Genital Tract Infection by the Obligate Intracellular Bacterium Chlamydia Trachomatis Elicits Robust Type 2 Immunity. PLoS ONE. 2013;8:e58565. doi: 10.1371/journal.pone.0058565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Scurlock A.M., Frazer L.C., Andrews C.W., Jr., O’Connell C.M., Foote I.P., Bailey S.L., Chandra-Kuntal K., Kolls J.K., Darville T. Interleukin-17 Contributes to Generation of Th1 Immunity and Neutrophil Recruitment during Chlamydia Muridarum Genital Tract Infection But Is Not Required for Macrophage Influx or Normal Resolution of Infection. Infect. Immun. 2011;79:1349–1362. doi: 10.1128/IAI.00984-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Barral R., Desai R., Zheng X., Frazer L.C., Sucato G.S., Haggerty C.L., O’Connell C.M., Zurenski M.A., Darville T. Frequency of Chlamydia Trachomatis-Specific T Cell Interferon-Gamma and Interleukin-17 Responses in Cd4-Enriched Peripheral Blood Mononuclear Cells of Sexually Active Adolescent Females. J. Reprod. Immunol. 2014;103:29–37. doi: 10.1016/j.jri.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Feinen B., Jerse A.E., Gaffen S.L., Russell M.W. Critical Role of Th17 Responses in a Murine Model of Neisseria Gonorrhoeae Genital Infection. Mucosal Immunol. 2010;3:312–321. doi: 10.1038/mi.2009.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Feinen B., Russell M.W. Contrasting Roles of IL-22 and IL-17 in Murine Genital Tract Infection by Neisseria Gonorrhoeae. Front. Immunol. 2012;3:11. doi: 10.3389/fimmu.2012.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gagliardi M.C., Starnino S., Teloni R., Mariotti S., Dal Conte I., Di Carlo A., Stefanelli P. Circulating Levels of Interleukin-17a and Interleukin-23 Are Increased in Patients with Gonococcal Infection. FEMS Immunol. Med. Microbiol. 2011;61:129–132. doi: 10.1111/j.1574-695X.2010.00759.x. [DOI] [PubMed] [Google Scholar]
- 121.Leader B.T., Godornes C., VanVoorhis W.C., Lukehart S.A. Cd4+ Lymphocytes and Gamma Interferon Predominate in Local Immune Responses in Early Experimental Syphilis. Infect. Immun. 2007;75:3021–3026. doi: 10.1128/IAI.01973-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lukehart S.A., Baker-Zander S.A., Lloyd R.M., Sell S. Characterization of Lymphocyte Responsiveness in Early Experimental Syphilis. Ii. Nature of Cellular Infiltration and Treponema Pallidum Distribution in Testicular Lesions. J. Immunol. 1980;124:461–467. doi: 10.4049/jimmunol.124.1.461. [DOI] [PubMed] [Google Scholar]
- 123.Van Voorhis W.C., Barrett L.K., Koelle D.M., Nasio J.M., Plummer F.A., Lukehart S.A. Primary and Secondary Syphilis Lesions Contain Mrna for Th1 Cytokines. J. Infect. Dis. 1996;173:491–495. doi: 10.1093/infdis/173.2.491. [DOI] [PubMed] [Google Scholar]
- 124.van Voorhis W.C., Barrett L.K., Nasio J.M., Plummer F.A., Lukehart S.A. Lesions of Primary and Secondary Syphilis Contain Activated Cytolytic T Cells. Infect. Immun. 1996;64:1048–1050. doi: 10.1128/iai.64.3.1048-1050.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Salazar J.C., Cruz A.R., Pope C.D., Valderrama L., Trujillo R., Saravia N.G., Radolf J.D. Treponema Pallidum Elicits Innate and Adaptive Cellular Immune Responses in Skin and Blood during Secondary Syphilis: A Flow-Cytometric Analysis. J. Infect. Dis. 2007;195:879–887. doi: 10.1086/511822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sallusto F., Lenig D., Förster R., Lipp M., Lanzavecchia A. Two Subsets of Memory T Lymphocytes with Distinct Homing Potentials and Effector Functions. Nature. 1999;401:708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 127.Lange J., Rivera-Ballesteros O., Buggert M. Human Mucosal Tissue-Resident Memory T Cells in Health and Disease. Mucosal Immunol. 2022;15:389–397. doi: 10.1038/s41385-021-00467-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Morris S.E., Farber D.L., Yates A.J. Tissue-Resident Memory T Cells in Mice and Humans: Towards a Quantitative Ecology. J. Immunol. 2019;203:2561–2569. doi: 10.4049/jimmunol.1900767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Matloubian M., Lo C.G., Cinamon G., Lesneski M.J., Xu Y., Brinkmann V., Allende M.L., Proia R.L., Cyster J.G. Lymphocyte Egress from Thymus and Peripheral Lymphoid Organs Is Dependent on S1P Receptor 1. Nature. 2004;427:355–360. doi: 10.1038/nature02284. [DOI] [PubMed] [Google Scholar]
- 130.Shiow L.R., Rosen D.B., Brdicková N., Xu Y., An J., Lanier L.L., Cyster J.G., Matloubian M. Cd69 Acts Downstream of Interferon-Alpha/Beta to Inhibit S1p1 and Lymphocyte Egress from Lymphoid Organs. Nature. 2006;440:540–544. doi: 10.1038/nature04606. [DOI] [PubMed] [Google Scholar]
- 131.Mackay L.K., Braun A., Macleod B.L., Collins N., Tebartz C., Bedoui S., Carbone F.R., Gebhardt T. Cutting Edge: Cd69 Interference with Sphingosine-1-Phosphate Receptor Function Regulates Peripheral T Cell Retention. J. Immunol. 2015;194:2059–2063. doi: 10.4049/jimmunol.1402256. [DOI] [PubMed] [Google Scholar]
- 132.Woodward Davis A.S., Vick S.C., Pattacini L., Voillet V., Hughes S.M., Lentz G.M., Kirby A.C., Fialkow M.F., Gottardo R., Hladik F., et al. The Human Memory T Cell Compartment Changes across Tissues of the Female Reproductive Tract. Mucosal Immunol. 2021;14:862–872. doi: 10.1038/s41385-021-00406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pattacini L., Woodward Davis A., Czartoski J., Mair F., Presnell S., Hughes S.M., Hyrien O., Lentz G.M., Kirby A.C., Fialkow M.F., et al. A Pro-Inflammatory Cd8+ T-Cell Subset Patrols the Cervicovaginal Tract. Mucosal Immunol. 2019;12:1118–1129. doi: 10.1038/s41385-019-0186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kumar B.V., Ma W., Miron M., Granot T., Guyer R.S., Carpenter D.J., Senda T., Sun X., Ho S.-h., Lerner H., et al. Human Tissue-Resident Memory T Cells Are Defined by Core Transcriptional and Functional Signatures in Lymphoid and Mucosal Sites. Cell Rep. 2017;20:2921–2934. doi: 10.1016/j.celrep.2017.08.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Woodward Davis A.S., Roozen H.N., Dufort M.J., DeBerg H.A., Delaney M.A., Mair F., Erickson J.R., Slichter C.K., Berkson J.D., Klock A.M., et al. The Human Tissue-Resident CCR5+ T Cell Compartment Maintains Protective and Functional Properties during Inflammation. Sci. Transl. Med. 2019;11:eaaw8718. doi: 10.1126/scitranslmed.aaw8718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hladik F., Lentz G., Delpit E., McElroy A., McElrath M.J. Coexpression of Ccr5 and Il-2 in Human Genital but Not Blood T Cells: Implications for the Ontogeny of the Ccr5+ Th1 Phenotype. J. Immunol. 1999;163:2306–2313. doi: 10.4049/jimmunol.163.4.2306. [DOI] [PubMed] [Google Scholar]
- 137.Poon M.M.L., Caron D.P., Wang Z., Wells S.B., Chen D., Meng W., Szabo P.A., Lam N., Kubota M., Matsumoto R., et al. Tissue Adaptation and Clonal Segregation of Human Memory T Cells in Barrier Sites. Nat. Immunol. 2023;24:309–319. doi: 10.1038/s41590-022-01395-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Iijima N., Iwasaki A. A Local Macrophage Chemokine Network Sustains Protective Tissue-Resident Memory Cd4 T Cells. Science. 2014;346:93–98. doi: 10.1126/science.1257530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Shin H., Iwasaki A. A Vaccine Strategy Protects against Genital Herpes by Establishing Local Memory T Cells. Nature. 2012;491:463–467. doi: 10.1038/nature11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Shin H., Kumamoto Y., Gopinath S., Iwasaki A. Cd301b+ Dendritic Cells Stimulate Tissue-Resident Memory Cd8+ T Cells to Protect against Genital Hsv-2. Nat. Commun. 2016;7:13346. doi: 10.1038/ncomms13346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Koelle D.M., Dong L., Jing L., Laing K.J., Zhu J., Jin L., Selke S., Wald A., Varon D., Huang M.L., et al. Hsv-2-Specific Human Female Reproductive Tract Tissue Resident Memory T Cells Recognize Diverse Hsv Antigens. Front. Immunol. 2022;13:867962. doi: 10.3389/fimmu.2022.867962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Posavad C.M., Zhao L., Dong L., Jin L., Stevens C.E., Magaret A.S., Johnston C., Wald A., Zhu J., Corey L., et al. Enrichment of Herpes Simplex Virus Type 2 (Hsv-2) Reactive Mucosal T Cells in the Human Female Genital Tract. Mucosal Immunol. 2017;10:1259–1269. doi: 10.1038/mi.2016.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Peng T., Phasouk K., Bossard E., Klock A., Jin L., Laing K.J., Johnston C., Williams N.A., Czartoski J.L., Varon D., et al. Distinct Populations of Antigen-Specific Tissue-Resident Cd8+ T Cells in Human Cervix Mucosa. JCI Insight. 2021;6:e149950. doi: 10.1172/jci.insight.149950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Roychoudhury P., Swan D.A., Duke E., Corey L., Zhu J., Davé V., Spuhler L.R., Lund J.M., Prlic M., Schiffer J.T. Tissue-Resident T Cell-Derived Cytokines Eliminate Herpes Simplex Virus-2-Infected Cells. J. Clin. Investig. 2020;130:2903–2919. doi: 10.1172/JCI132583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Posavad C.M., Zhao L., Mueller D.E., Stevens C.E., Huang M.-L.W., Wald A., Corey L. Persistence of Mucosal T Cell Responses to Herpes Simplex Virus Type 2 (Hsv-2) in the Female Genital Tract. Mucosal Immunol. 2014;8:115–126. doi: 10.1038/mi.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mackay L.K., Stock A.T., Ma J.Z., Jones C.M., Kent S.J., Mueller S.N., Heath W.R., Carbone F.R., Gebhardt T. Long-Lived Epithelial Immunity by Tissue-Resident Memory T (Trm) Cells in the Absence of Persisting Local Antigen Presentation. Proc. Natl. Acad. Sci. USA. 2012;109:7037–7042. doi: 10.1073/pnas.1202288109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Beura L.K., Mitchell J.S., Thompson E.A., Schenkel J.M., Mohammed J., Wijeyesinghe S., Fonseca R., Burbach B.J., Hickman H.D., Vezys V., et al. Intravital Mucosal Imaging of Cd8+ Resident Memory T Cells Shows Tissue-Autonomous Recall Responses That Amplify Secondary Memory. Nat. Immunol. 2018;19:173–182. doi: 10.1038/s41590-017-0029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Schenkel J.M., Fraser K.A., Vezys V., Masopust D. Sensing and Alarm Function of Resident Memory Cd8⁺ T Cells. Nat. Immunol. 2013;14:509–513. doi: 10.1038/ni.2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Schenkel J.M., Fraser K.A., Beura L.K., Pauken K.E., Vezys V., Masopust D. Resident Memory Cd8 T Cells Trigger Protective Innate and Adaptive Immune Responses. Science. 2014;346:101–198. doi: 10.1126/science.1254536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Buggert M., Nguyen S., Salgado-Montes de Oca G., Bengsch B., Darko S., Ransier A., Roberts E.R., del Alcazar D., Brody I.B., Vella L.A., et al. Identification and Characterization of Hiv-Specific Resident Memory Cd8+ T Cells in Human Lymphoid Tissue. Sci. Immunol. 2018;3:eaar4526. doi: 10.1126/sciimmunol.aar4526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cantero-Pérez J., Grau-Expósito J., Serra-Peinado C., Rosero D.A., Luque-Ballesteros L., Astorga-Gamaza A., Castellví J., Sanhueza T., Tapia G., Lloveras B., et al. Resident Memory T Cells Are a Cellular Reservoir for Hiv in the Cervical Mucosa. Nat. Commun. 2019;10:4739. doi: 10.1038/s41467-019-12732-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Gibbs A., Buggert M., Edfeldt G., Ranefall P., Introini A., Cheuk S., Martini E., Eidsmo L., Ball T.B., Kimani J., et al. Human Immunodeficiency Virus-Infected Women Have High Numbers of Cd103-Cd8+ T Cells Residing Close to the Basal Membrane of the Ectocervical Epithelium. J. Infect. Dis. 2018;218:453–465. doi: 10.1093/infdis/jix661. [DOI] [PubMed] [Google Scholar]
- 153.Gupta P., Collins K.B., Ratner D., Watkins S.C., Naus G.J., Landers D.V., Patterson B.K. Memory Cd4+ T Cells Are the Earliest Detectable Human Immunodeficiency Virus Type 1 (Hiv-1)-Infected Cells in the Female Genital Mucosal Tissue during Hiv-1 Transmission in an Organ Culture System. J. Virol. 2002;76:9868–9876. doi: 10.1128/JVI.76.19.9868-9876.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Moylan D., Goepfert P.A., Kempf M.-C., Saag M.S., Richter H.E., Mestecky J.F., Sabbaj S. Diminished Cd103 (αEβ7) Expression on Resident T Cells from the Female Genital Tract of Hiv-Positive Women. Pathog. Immun. 2017;1:371–389. doi: 10.20411/pai.v1i2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Petitdemange C., Kasturi S.P., Kozlowski P.A., Nabi R., Quarnstrom C.F., Reddy P.B.J., Derdeyn C.A., Spicer L.M., Patel P.J., Legere T., et al. Vaccine Induction of Antibodies and Tissue-Resident Cd8+ T Cells Enhances Protection against Mucosal Shiv-Infection in Young Macaques. JCI Insight. 2019;4:e126047. doi: 10.1172/jci.insight.126047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Shacklett B.L. Mucosal Immunity in Hiv/Siv Infection: T Cells, B Cells and Beyond. Curr. Immunol. Rev. 2019;15:63–75. doi: 10.2174/1573395514666180528081204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Tan H.-X., Wheatley A.K., Esterbauer R., Jegaskanda S., Glass J.J., Masopust D., Rose R.D., Rose R.D., Kent S.J., Kent S.J. Induction of Vaginal-Resident Hiv-Specific Cd8 T Cells with Mucosal Prime–Boost Immunization. Mucosal Immunol. 2017;11:994–1007. doi: 10.1038/mi.2017.89. [DOI] [PubMed] [Google Scholar]
- 158.Iwasaki A. Antiviral Immune Responses in the Genital Tract: Clues for Vaccines. Nat. Rev. Immunol. 2010;10:699–711. doi: 10.1038/nri2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Morrison S.G., Morrison R.P. In Situ Analysis of the Evolution of the Primary Immune Response in Murine Chlamydia Trachomatis Genital Tract Infection. Infect. Immun. 2000;68:2870–2879. doi: 10.1128/IAI.68.5.2870-2879.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Van Voorhis W.C., Barrett L.K., Sweeney Y.T., Kuo C.C., Patton D.L. Repeated Chlamydia Trachomatis Infection of Macaca Nemestrina Fallopian Tubes Produces a Th1-Like Cytokine Response Associated with Fibrosis and Scarring. Infect. Immun. 1997;65:2175–2182. doi: 10.1128/iai.65.6.2175-2182.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kiviat N.B., Paavonen J.A., Wølner-Hanssen P., Critchlow C.W., Stamm W.E., Douglas J., Eschenbach D.A., Corey L.A., Holmes K.K. Histopathology of Endocervical Infection Caused by Chlamydia Trachomatis, Herpes Simplex Virus, Trichomonas Vaginalis, and Neisseria Gonorrhoeae. Hum. Pathol. 1990;21:831–837. doi: 10.1016/0046-8177(90)90052-7. [DOI] [PubMed] [Google Scholar]
- 162.Kiviat N.B., Wolner-Hanssen P., Eschenbach D.A., Wasserheit J.N., Paavonen J.A., Bell T.A., Critchlow C.W., Stamm W.E., Moore D.E., Holmes K.K. Endometrial Histopathology in Patients with Culture-Proved Upper Genital Tract Infection and Laparoscopically Diagnosed Acute Salpingitis. Am. J. Surg. Pathol. 1990;14:167–175. doi: 10.1097/00000478-199002000-00008. [DOI] [PubMed] [Google Scholar]
- 163.Igietseme J.U., Uriri I.M., Hawkins R., Rank R.G. Integrin-Mediated Epithelial-T Cell Interaction Enhances Nitric Oxide Production and Increased Intracellular Inhibition of Chlamydia. J. Leukoc. Biol. 1996;59:656–662. doi: 10.1002/jlb.59.5.656. [DOI] [PubMed] [Google Scholar]
- 164.Igietseme J.U. Molecular Mechanism of T-Cell Control of Chlamydia in Mice: Role of Nitric Oxide In Vivo. Immunology. 1996;88:1–5. doi: 10.1046/j.1365-2567.1996.d01-655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kelly K.A., Rank R.G. Identification of Homing Receptors That Mediate the Recruitment of Cd4 T Cells to the Genital Tract Following Intravaginal Infection with Chlamydia Trachomatis. Infect. Immun. 1997;65:5198–5208. doi: 10.1128/iai.65.12.5198-5208.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hawkins R.A., Rank R.G., Kelly K.A. Expression of Mucosal Homing Receptor Alpha4beta7 Is Associated with Enhanced Migration to the Chlamydia-Infected Murine Genital Mucosa In Vivo. Infect. Immun. 2000;68:5587–5594. doi: 10.1128/IAI.68.10.5587-5594.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Nguyen N., Olsen A.W., Lorenzen E., Andersen P., Hvid M., Follmann F., Dietrich J. Parenteral Vaccination Protects against Transcervical Infection with Chlamydia Trachomatis and Generate Tissue-Resident T Cells Post-Challenge. NPJ Vaccines. 2020;5:7. doi: 10.1038/s41541-020-0157-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Nguyen N., Guleed S., Olsen A.W., Follmann F., Christensen J.P., Dietrich J. Th1/Th17 T Cell Tissue-Resident Immunity Increases Protection, but Is Not Required in a Vaccine Strategy Against Genital Infection with Chlamydia trachomatis. Front. Immunol. 2021;12:790463. doi: 10.3389/fimmu.2021.790463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Jiao L., Gao X., Joyee A.G., Zhao L., Qiu H., Yang M., Fan Y., Wang S., Yang X. NK Cells Promote Type 1 T Cell Immunity through Modulating the Function of Dendritic Cells during Intracellular Bacterial Infection. J. Immunol. 2011;187:401–411. doi: 10.4049/jimmunol.1002519. [DOI] [PubMed] [Google Scholar]
- 170.Wang H., Li J., Dong X., Zhou X., Zhao L., Wang X., Rashu R., Zhao W., Yang X. NK Cells Contribute to Protective Memory T Cell Mediated Immunity to Chlamydia Muridarum Infection. Front. Cell Infect. Microbiol. 2020;10:296. doi: 10.3389/fcimb.2020.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Panda S.K., Colonna M. Innate Lymphoid Cells in Mucosal Immunity. Front. Immunol. 2019;10:861. doi: 10.3389/fimmu.2019.00861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Doisne J.M., Balmas E., Boulenouar S., Gaynor L.M., Kieckbusch J., Gardner L., Hawkes D.A., Barbara C.F., Sharkey A.M., Brady H.J., et al. Composition, Development, and Function of Uterine Innate Lymphoid Cells. J. Immunol. 2015;195:3937–3945. doi: 10.4049/jimmunol.1500689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Miller D., Motomura K., Garcia-Flores V., Romero R., Gomez-Lopez N. Innate Lymphoid Cells in the Maternal and Fetal Compartments. Front. Immunol. 2018;9:2396. doi: 10.3389/fimmu.2018.02396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Schroeder J.H., Howard J.K., Lord G.M. Transcription Factor-Driven Regulation of Ilc1 and Ilc3. Trends Immunol. 2022;43:564–579. doi: 10.1016/j.it.2022.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Barth S., Kirschnek S., Ortmann N., Tanriver Y., Häcker G. The Reaction of Innate Lymphoid Cells in the Mouse Female Genital Tract to Chlamydial Infection. Infect. Immun. 2021;89:e0080020. doi: 10.1128/IAI.00800-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.He Y., Xu H., Song C., Koprivsek J.J., Arulanandam B., Yang H., Tao L., Zhong G. Adoptive Transfer of Group 3-Like Innate Lymphoid Cells Restores Mouse Colon Resistance to Colonization of a Gamma Interferon-Susceptible Chlamydia muridarum Mutant. Infect. Immun. 2021;89:e00533-20. doi: 10.1128/IAI.00533-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Godfrey D.I., Koay H.F., McCluskey J., Gherardin N.A. The Biology and Functional Importance of Mait Cells. Nat. Immunol. 2019;20:1110–1128. doi: 10.1038/s41590-019-0444-8. [DOI] [PubMed] [Google Scholar]
- 178.Le Bourhis L., Martin E., Péguillet I., Guihot A., Froux N., Coré M., Lévy E., Dusseaux M., Meyssonnier V., Premel V., et al. Antimicrobial Activity of Mucosal-Associated Invariant T Cells. Nat. Immunol. 2010;11:701–708. doi: 10.1038/ni.1890. [DOI] [PubMed] [Google Scholar]
- 179.Gibbs A., Leeansyah E., Introini A., Paquin-Proulx D., Hasselrot K., Andersson E., Broliden K., Sandberg J.K., Tjernlund A. MAIT Cells Reside in the Female Genital Mucosa and Are Biased towards IL-17 and IL-22 Production in Response to Bacterial Stimulation. Mucosal Immunol. 2016;10:35–45. doi: 10.1038/mi.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bister J., Crona Guterstam Y., Strunz B., Dumitrescu B., Haij Bhattarai K., Özenci V., Brännström M., Ivarsson M.A., Gidlöf S., Björkström N.K. Human Endometrial Mait Cells Are Transiently Tissue Resident and Respond to Neisseria Gonorrhoeae. Mucosal Immunol. 2021;14:357–365. doi: 10.1038/s41385-020-0331-5. [DOI] [PubMed] [Google Scholar]
- 181.Hosenfeld C.B., Workowski K.A., Berman S., Zaidi A., Dyson J., Mosure D., Bolan G., Bauer H.M. Repeat Infection with Chlamydia and Gonorrhea among Females: A Systematic Review of the Literature. Sex. Transm. Dis. 2009;36:478–489. doi: 10.1097/OLQ.0b013e3181a2a933. [DOI] [PubMed] [Google Scholar]
- 182.Cha S., Newman D.R., Rahman M., Peterman T.A. High Rates of Repeat Chlamydial Infections among Young Women-Louisiana, 2000–2015. Sex. Transm. Dis. 2019;46:52–57. doi: 10.1097/OLQ.0000000000000906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Newman D.R., Matthias J., Rahman M.M., Brantley A., Peterman T.A. Repeat Syphilis Among Hiv-Infected Men in Florida and Louisiana 2000–2018: Implications for Screening Recommendations. AIDS Patient Care STDS. 2021;35:435–440. doi: 10.1089/apc.2021.0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Hsu K.K., Molotnikov L.E., Roosevelt K.A., Elder H.R., Klevens R.M., DeMaria A., Jr., Aral S.O. Characteristics of Cases With Repeated Sexually Transmitted Infections, Massachusetts, 2014–2016. Clin. Infect. Dis. 2018;67:99–104. doi: 10.1093/cid/ciy029. [DOI] [PubMed] [Google Scholar]
- 185.Geisler W.M., Lensing S.Y., Press C.G., Hook E.W., 3rd Spontaneous Resolution of Genital Chlamydia Trachomatis Infection in Women and Protection from Reinfection. J. Infect. Dis. 2013;207:1850–1856. doi: 10.1093/infdis/jit094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Arno J.N., Katz B.P., McBride R., Carty G.A., Batteiger B.E., Caine V.A., Jones R.B. Age and Clinical Immunity to Infections with Chlamydia Trachomatis. Sex. Transm. Dis. 1994;21:47–52. doi: 10.1097/00007435-199401000-00010. [DOI] [PubMed] [Google Scholar]
- 187.Kenyon C., Tsoumanis A., Osbak K., Van Esbroeck M., Florence E., Crucitti T., Kestens L. Repeat Syphilis Has a Different Immune Response Compared with Initial Syphilis: An Analysis of Biomarker Kinetics in Two Cohorts. Sex. Transm. Infect. 2018;94:180–186. doi: 10.1136/sextrans-2017-053312. [DOI] [PubMed] [Google Scholar]
- 188.Kenyon C., Osbak K.K., Apers L. Repeat Syphilis Is More Likely to Be Asymptomatic in Hiv-Infected Individuals: A Retrospective Cohort Analysis with Important Implications for Screening. Open Forum Infect. Dis. 2018;5:ofy096. doi: 10.1093/ofid/ofy096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Darville T., Albritton H.L., Zhong W., Dong L., O’Connell C.M., Poston T.B., Quayle A.J., Goonetilleke N., Wiesenfeld H.C., Hillier S.L., et al. Anti-Chlamydia Igg and Iga Are Insufficient to Prevent Endometrial Chlamydia Infection in Women, and Increased Anti-Chlamydia Igg Is Associated with Enhanced Risk for Incident Infection. Am. J. Reprod. Immunol. 2019;81:e13103. doi: 10.1111/aji.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Nichols R.L., Bell S.D., Jr., Murray E.S., Haddad N.A., Bobb A.A. Studies on Trachoma. V. Clinical Observations in a Field Trial of Bivalent Trachoma Vaccine at Three Dosage Levels in Saudi Arabia. Am. J. Trop. Med. Hyg. 1966;15:639–647. doi: 10.4269/ajtmh.1966.15.639. [DOI] [PubMed] [Google Scholar]
- 191.Nichols R.L., Bell S.D., Jr., Haddad N.A., Bobb A.A. Studies on Trachoma. Vi. Microbiological Observations in a Field Trial in Saudi Arabia of Bivalent Rachoma Vaccine at Three Dosage Levels. Am. J. Trop. Med. Hyg. 1969;18:723–730. doi: 10.4269/ajtmh.1969.18.723. [DOI] [PubMed] [Google Scholar]
- 192.Grayston J.T., Woolridge R.L., Wang S.P., Yen C.H., Yang C.Y., Cheng K.H., Chang I.H. Field Studies of Protection from Infection by Experimental Trachoma Virus Vaccine in Preschool-Aged Children on Taiwan. Proc. Soc. Exp. Biol. Med. 1963;112:589–595. doi: 10.3181/00379727-112-28112. [DOI] [PubMed] [Google Scholar]
- 193.Woolridge R.L., Grayston J.T., Chang I.H., Cheng K.H., Yang C.Y., Neave C. Field Trial of a Monovalent and of a Bivalent Mineral Oil Adjuvant Trachoma Vaccine in Taiwan School Children. Am. J. Ophthalmol. 1967;63:1645–1650. doi: 10.1016/0002-9394(67)94158-X. [DOI] [PubMed] [Google Scholar]
- 194.Sowa S., Sowa J., Collier L.H., Blyth W.A. Trachoma Vaccine Field Trials in the Gambia. J. Hyg. 1969;67:699–717. doi: 10.1017/S0022172400042157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Dhir S.P., Agarwal L.P., Detels R., Wang S.P., Grayston J.T. Field Trial of Two Bivalent Trachoma Vaccines in Children of Punjab Indian Villages. Am. J. Ophthalmol. 1967;63:1639–1644. doi: 10.1016/0002-9394(67)94157-8. [DOI] [PubMed] [Google Scholar]
- 196.Mabey D.C., Hu V., Bailey R.L., Burton M.J., Holland M.J. Towards a Safe and Effective Chlamydial Vaccine: Lessons from the Eye. Vaccine. 2014;32:1572–1578. doi: 10.1016/j.vaccine.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.O’Connell C.M., Ingalls R.R., Andrews C.W., Jr., Scurlock A.M., Darville T. Plasmid-Deficient Chlamydia Muridarum Fail to Induce Immune Pathology and Protect against Oviduct Disease. J. Immunol. 2007;179:4027–4034. doi: 10.4049/jimmunol.179.6.4027. [DOI] [PubMed] [Google Scholar]
- 198.Riley M.M., Zurenski M.A., Frazer L.C., O’Connell C.M., Andrews C.W., Jr., Mintus M., Darville T. The Recall Response Induced by Genital Challenge with Chlamydia Muridarum Protects the Oviduct from Pathology But Not from Reinfection. Infect. Immun. 2012;80:2194–2203. doi: 10.1128/IAI.00169-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Caldwell H.D., Kromhout J., Schachter J. Purification and Partial Characterization of the Major Outer Membrane Protein of Chlamydia Trachomatis. Infect. Immun. 1981;31:1161–1176. doi: 10.1128/iai.31.3.1161-1176.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Proctor J., Stadler M., Cortes L.M., Brodsky D., Poisson L., Gerdts V., Smirnov A.I., Smirnova T.I., Barua S., Leahy D., et al. A TriAdj-Adjuvanted Chlamydia trachomatis Cpaf Protein Vaccine Is Highly Immunogenic in Pigs. Vaccines. 2024;12:423. doi: 10.3390/vaccines12040423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Murthy A.K., Li W., Guentzel M.N., Zhong G., Arulanandam B.P. Vaccination with the Defined Chlamydial Secreted Protein Cpaf Induces Robust Protection against Female Infertility Following Repeated Genital Chlamydial Challenge. Vaccine. 2011;29:2519–2522. doi: 10.1016/j.vaccine.2011.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Murphey C., Murthy A.K., Meier P.A., Neal Guentzel M., Zhong G., Arulanandam B.P. The Protective Efficacy of Chlamydial Protease-Like Activity Factor Vaccination Is Dependent Upon Cd4+ T Cells. Cell Immunol. 2006;242:110–117. doi: 10.1016/j.cellimm.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Cong Y., Jupelli M., Guentzel M.N., Zhong G., Murthy A.K., Arulanandam B.P. Intranasal Immunization with Chlamydial Protease-Like Activity Factor and Cpg Deoxynucleotides Enhances Protective Immunity against Genital Chlamydia Muridarum Infection. Vaccine. 2007;25:3773–3780. doi: 10.1016/j.vaccine.2007.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Pal S., Favaroni A., Tifrea D.F., Hanisch P.T., Luczak S.E.T., Hegemann J.H., de la Maza L.M. Comparison of the Nine Polymorphic Membrane Proteins of Chlamydia Trachomatis for Their Ability to Induce Protective Immune Responses in Mice against a C. Muridarum Challenge. Vaccine. 2017;35:2543–2549. doi: 10.1016/j.vaccine.2017.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Müller T., Becker E., Stallmann S., Waldhuber A., Römmler-Dreher F., Albrecht S., Mohr F., Hegemann J.H., Miethke T. Vaccination with the Polymorphic Membrane Protein a Reduces Chlamydia Muridarum Induced Genital Tract Pathology. Vaccine. 2017;35:2801–2810. doi: 10.1016/j.vaccine.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 206.Lanfermann C., Wintgens S., Ebensen T., Kohn M., Laudeley R., Schulze K., Rheinheimer C., Hegemann J.H., Guzmán C.A., Klos A. Prophylactic Multi-Subunit Vaccine against Chlamydia trachomatis: In Vivo Evaluation in Mice. Vaccines. 2021;9:609. doi: 10.3390/vaccines9060609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Yu H., Karunakaran K.P., Jiang X., Shen C., Andersen P., Brunham R.C. Chlamydia Muridarum T Cell Antigens and Adjuvants That Induce Protective Immunity in Mice. Infect. Immun. 2012;80:1510–1518. doi: 10.1128/IAI.06338-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Poston T.B., Girardi J., Polson A.G., Bhardwaj A., Yount K.S., Jaras Salas I., Trim L.K., Li Y., O’Connell C.M., Leahy D., et al. Viral-Vectored Boosting of Omcb- or Cpaf-Specific T-Cell Responses Fail to Enhance Protection from Chlamydia Muridarum in Infection-Immune Mice and Elicits a Non-Protective Cd8-Dominant Response in Naïve Mice. Mucosal Immunol. 2024 doi: 10.1016/j.mucimm.2024.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Muenzner P., Hauck C.R. Neisseria Gonorrhoeae Blocks Epithelial Exfoliation by Nitric-Oxide-Mediated Metabolic Cross Talk to Promote Colonization in Mice. Cell Host Microbe. 2020;27:793–808.e795. doi: 10.1016/j.chom.2020.03.010. [DOI] [PubMed] [Google Scholar]
- 210.Muenzner P., Bachmann V., Zimmermann W., Hentschel J., Hauck C.R. Human-Restricted Bacterial Pathogens Block Shedding of Epithelial Cells by Stimulating Integrin Activation. Science. 2010;329:1197–1201. doi: 10.1126/science.1190892. [DOI] [PubMed] [Google Scholar]
- 211.Ladhani S.N., White P.J., Campbell H., Mandal S., Borrow R., Andrews N., Bhopal S., Saunders J., Mohammed H., Drisdale-Gordon L., et al. Use of a Meningococcal Group B Vaccine (4cmenb) in Populations at High Risk of Gonorrhoea in the UK. Lancet Infect. Dis. 2024 doi: 10.1016/S1473-3099(24)00031-8. [DOI] [PubMed] [Google Scholar]
- 212.Marjuki H., Topaz N., Joseph S.J., Gernert K.M., Kersh E.N., Wang X. Genetic Similarity of Gonococcal Homologs to Meningococcal Outer Membrane Proteins of Serogroup B Vaccine. mBio. 2019;10:e01668-19. doi: 10.1128/mBio.01668-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Semchenko E.A., Tan A., Borrow R., Seib K.L. The Serogroup B Meningococcal Vaccine Bexsero Elicits Antibodies to Neisseria Gonorrhoeae. Clin. Infect. Dis. 2019;69:1101–1111. doi: 10.1093/cid/ciy1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Longtin J., Dion R., Simard M., Betala Belinga J.-F., Longtin Y., Lefebvre B., Labbé A.-C., Deceuninck G., De Wals P. Possible Impact of Wide-scale Vaccination Against Serogroup B Neisseria Meningitidis on Gonorrhea Incidence Rates in One Region of Quebec, Canada. Open Forum Infect. Dis. 2017;4:S734–S735. doi: 10.1093/ofid/ofx180.002. [DOI] [Google Scholar]
- 215.Abara W.E., Bernstein K.T., Lewis F.M.T., Schillinger J.A., Feemster K., Pathela P., Hariri S., Islam A., Eberhart M., Cheng I., et al. Effectiveness of a Serogroup B Outer Membrane Vesicle Meningococcal Vaccine against Gonorrhoea: A Retrospective Observational Study. Lancet Infect. Dis. 2022;22:1021–1029. doi: 10.1016/S1473-3099(21)00812-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Wang B., Giles L., Andraweera P., McMillan M., Almond S., Beazley R., Mitchell J., Ahoure M., Denehy E., Flood L., et al. 4cmenb Sustained Vaccine Effectiveness against Invasive Meningococcal B Disease and Gonorrhoea at Three Years Post Programme Implementation. J. Infect. 2023;87:95–102. doi: 10.1016/j.jinf.2023.05.021. [DOI] [PubMed] [Google Scholar]
- 217.Marra C.M., Castro C.D., Kuller L., Dukes A.C., Centurion-Lara A., Morton W.R., Lukehart S.A. Mechanisms of Clearance of Treponema Pallidum from the Csf in a Nonhuman Primate Model. Neurology. 1998;51:957–961. doi: 10.1212/WNL.51.4.957. [DOI] [PubMed] [Google Scholar]
- 218.Schell R.F., LeFrock J.L., Chan J.K., Bagasra O. LSH Hamster Model of Syphilitic Infection. Infect. Immun. 1980;28:909–913. doi: 10.1128/iai.28.3.909-913.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Metzger M., Michalska E., Podwińska J., Smogór W. Immunogenic Properties of the Protein Component of Treponema Pallidum. Br. J. Vener. Dis. 1969;45:299–304. doi: 10.1136/sti.45.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zheng K., Xu M., Xiao Y., Luo H., Xie Y., Yu J., Tan M., Li Y., Zhao F., Zeng T., et al. Immunogenicity and Protective Efficacy against Treponema Pallidum in New Zealand Rabbits Immunized with Plasmid DNA Encoding Flagellin. Emerg. Microbes Infect. 2018;7:177. doi: 10.1038/s41426-018-0176-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zhao F., Zhang X., Liu S., Zeng T., Yu J., Gu W., Zhang Y., Chen X., Wu Y. Assessment of the Immune Responses to Treponema Pallidum Gpd DNA Vaccine Adjuvanted with Il-2 and Chitosan Nanoparticles before and after Treponema Pallidum Challenge in Rabbits. Sci. China Life Sci. 2013;56:174–180. doi: 10.1007/s11427-012-4434-4. [DOI] [PubMed] [Google Scholar]
- 222.Zhao F., Wu Y., Zhang X., Yu J., Gu W., Liu S., Zeng T., Zhang Y., Wang S. Enhanced Immune Response and Protective Efficacy of a Treponema Pallidum Tp92 DNA Vaccine Vectored by Chitosan Nanoparticles and Adjuvanted with IL-2. Hum. Vaccines. 2011;7:1083–1089. doi: 10.4161/hv.7.10.16541. [DOI] [PubMed] [Google Scholar]
- 223.Xiong S., Liu Z., Zhang X., Huang S., Ding X., Zhou J., Yao J., Li W., Liu S., Zhao F. Resurgence of Syphilis: Focusing on Emerging Clinical Strategies and Preclinical Models. J. Transl. Med. 2023;21:917. doi: 10.1186/s12967-023-04685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Darville T. Pelvic Inflammatory Disease Due to Neisseria Gonorrhoeae and Chlamydia Trachomatis: Immune Evasion Mechanisms and Pathogenic Disease Pathways. J. Infect. Dis. 2021;224:S39–S46. doi: 10.1093/infdis/jiab031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Wang X., Wu H., Fang C., Li Z. Insights into Innate Immune Cell Evasion by Chlamydia Trachomatis. Front. Immunol. 2024;15:1289644. doi: 10.3389/fimmu.2024.1289644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Scurtu L.G., Jinga V., Simionescu O. Fascinating Molecular and Immune Escape Mechanisms in the Treatment of Stis (Syphilis, Gonorrhea, Chlamydia, and Herpes Simplex) Int. J. Mol. Sci. 2022;23:3550. doi: 10.3390/ijms23073550. [DOI] [PMC free article] [PubMed] [Google Scholar]