Abstract
Background
Objective assessment of skills after training is essential for safe implementation of lung point-of-care ultrasound (POCUS). In low-and middle-income countries (LMIC) there is a need for assessment tools without onsite experts to scale up POCUS access. Our objective is to develop a web-based assessment tool and evaluate trainees across different countries and at different time points after initial lung POCUS training.
Methods
We adapted the objective and validated lung ultrasound score (LUS-OSAUS) to a web-based tool with quiz and practical skills test. Trainees were evaluated after a short (4-day) standardized lung POCUS training and were classified in distinct groups according to (i) their geographical location (Benin vs. South-Africa) and (ii) time elapsed since training (Benin 0 months vs. Benin 6 months). The Benin 6 months group had minimal continuous education. Skills test images were read by two blinded experts. We report the overall success rates and then compare these rates based on location and timing since training, using the Fischer’s exact test.
Results
A total of 35 out of 43 participants completed the online LUS-OSAUS quiz and skills test. The overall success rate was 0.84 (95%CI 0.80–0.88), with lower success rates for “correct depth” 0.54 (0.37–0.71), “correct assessment of pleura” 0.63 (0.45–0.79) and “conclusion” 0.71 (0.54–0.85). There were no differences based on location, with respective rates of 0.86 (0.80–0.92) and 0.83 (0.75–0.91) (p-value = 0.125) for Benin and South Africa at 0 months, respectively. Similarly, there were no differences according to timing with success rates of 0.86 (0.80–0.92) and 0.82 (0.72–0.93) (p-value = 0.563) for Benin at 0 months and 6 months, respectively.
Conclusion
Web-based objective and structured assessment of lung POCUS skills in LMIC following a short-standardized training is feasible and has a good overall success rate with consistent results across regions and up to 6 months after training given minimal continuous education. Overall, technical and POCUS-based clinical conclusion skills are the most difficult to acquire.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-05925-x.
Keywords: LUS-OSAUS; Lung POCUS; Low- and middle- income countries; Training, quality control
Background
Point-of-care ultrasonography (POCUS) of the lungs is increasingly used as a first-line imaging tool to manage patients with respiratory symptoms [1]. With the advent of portable and affordable devices, POCUS has become particularly attractive to low- and middle-income countries (LMICs), as these tools overcome typical imaging barriers such as the absence of radiology services or high patient fee [2–5].
However, insufficiently or inadequately trained physicians might harm patients through inaccurate diagnoses or inappropriate use of POCUS. Recently, POCUS was labeled as a potential major health technology hazard by the Joint Commission on Accreditation of Healthcare Organizations and the Emergency Care Research Institute, emphasizing the risks of adopting the tool without essential precautions such as validated training [6, 7]. For each subspecialty, including lung POCUS, ensuring adequate training programs and standardized skills assessment are key to develop its safe and effective use. While training efforts are progressing in high-income countries, with at least 35% of US medical schools integrating POCUS in their curriculum [8], LMICs often lack formal training, onsite experts, and early exposure in undergraduate and postgraduate curricula [9, 10]. Web-based solutions are already readily used in emergency medicine residency programs and can be interesting in LMIC to overcome the initial need of local experts [11]. The significant heterogeneity among existing lung POCUS courses, along with deficits in skill evaluation, necessitates research involving theoretical and practical assessments after training. To address this gap, a lung ultrasound objective structured assessment of technical skills (LUS-OSAUS) score was developed in 2016 [12] and validated in 2020 for medical undergraduate students in Europe [13]. Our objective is (i) to adapt the LUS-OSAUS score for web-based application in resource-limited settings and (ii) evaluate trainees across various countries and at two distinct time points (immediately after initial training and after a 6-month period) after a standardized short lung POCUS training.
Methods
Web-based LUS-OSAUS tool development adapted to LMICs
The LUS-OSAUS score was adapted to an online quiz tool and practical skills test with content adjusted to align with LMIC epidemiology. The LUS-OSAUS score evaluates the trainee’s expertise according to 6 areas (test indication, systematic lung ultrasound examination, technical skills, interpretation of lung ultrasound findings, documentation and conclusion), which were strictly maintained. Accross these 6 areas, 17 items are included [12]. The original items were slightly modified to make the quiz questions more fluent. Our adapted LUS-OSAUS tool has 6 areas and 18 items (summarized in Table 1, overview of minor modifications to the original score are available in appendix Table 1).
Table 1.
Adapted LUS-OSAUS score with 6 areas and 18 items
| Area (n = 6) | Item (n = 18) | ||
|---|---|---|---|
| Indication | |||
| Indication: evaluates the indication for lung ultrasound, suggests focused questions | |||
| Systematic lung ultrasound examination | |||
| Performs lung ultrasound systematically | |||
| Performs lung ultrasound on the basis of a focused question and places patient accordingly | |||
| Technical skills | |||
| Correct choice of transducer/preset | |||
| Correct depth | |||
| Correct gain | |||
| Saves images correctly | |||
| Labels anatomical position correctly | |||
| Interpretability of the images | |||
| Findings | |||
| Correct assessment of pleura | |||
| Correct assessment of B-lines | |||
| Correct assessment of consolidations | |||
| Correct assessment of pleural effusion | |||
| Correct assessment of diaphragm | |||
| Correct assessment of M-mode | |||
| Correct assessment of whether ultrasound-guided thoracentesis is safe | |||
| Documentation | |||
| Documents findings in patient’s chart | |||
| Conclusion | |||
| Able to make a diagnosis on the basis of lung ultrasound findings and able to integrate lung ultrasound findings with patient’s history | |||
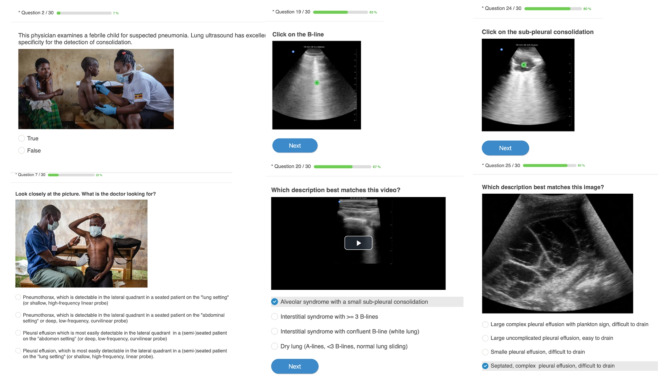
To assess these 18 items, we developed a 30-questions online quiz (Fig. 1, full quiz available in appendix Table 2) and 5 practical challenges (appendix Table 3). The 5 practical challenges consisted of capturing and uploading 5 s videos of the curtain sign in the right and left lateral quadrants, anterior lung sliding in M-mode, a 5 cm depth view of the pleural line and a posterior view of the pleural-line. Each challenge was evaluated for preset (or choice of probe), depth, gain, interpretability of the image, saving and labelling. The practical challenges were scored by 2 independent and certified remote LUS readers. A third reader was asked to grade in case of disagreement between the first two readers. All readers were blinded for the participant’s characteristics.
Fig. 1.
Example of online quiz questions adapted to a low-resource setting and based on the LUS-OSAUS score (available in a French and English version)
Appendix table 4 shows the link between the evaluated items, the online quiz questions and practical challenges. The original score evaluated every item on a scale of 1 to 5. With the adapted score, every question of the quiz was rated as correct (1 point) or not (0 point) and each item was evaluated through 1 to 5 questions. Every practical challenge (5 challenges) allowed to assess 6 items and were evaluated as passed (1 point per item and per challenge) or not (0 point). Participants could earn a maximum of 30 points for correctly answering online quiz questions and 30 points for successfully completing practical challenges. This added up to a maximum of 60 points achievable per participant. Since each item is evaluated through 1 to 5 questions, we defined an item as acquired based on a minimal percentage of correct answers per item: (n-1)/n (where n represents the number of questions for a single item) [14]. Levels of success were categorized as follows: good if the proportion of trainees who succeeded was ≥ 0.80, moderate if the proportion ranged from 0.70 to 0.79 and low if it was < 0.70.
Material used
The online quiz questions were developed using a platform to create interactive learning assessments (ProProfs®). For the practical challenges, participants were provided with an ultrasound on a chip POCUS device (Butterfly IQ ®). Test videos were recorded and uploaded on a secured cloud system and anonymized for the grading readers.
Standardized training content and trainee groups
The initial training was the same for all participants and consisted of a 4-hour lung ultrasound theory session, a 2-hour small group (max 4 participants) training on a healthy volunteer, a 6-hour small group (max 4 participants) on hospitalized patients and a 2-hour recapulative session, spread over 4 days (appendix Fig. 1). Trainers were Swiss LUS experts. Trainees were classified in three distinct groups based on their geographical location and the timing since their initial training. The first group (Benin 0 months) consisted of 18 West-African health care professionals trained at the National University Hospital for Tuberculosis and Lung Diseases in Cotonou, Benin in February 2022 and was evaluated immediately after training. The second group (South-Africa 0 months) consisted of 17 South-African physicians trained at the district-level public hospital of Tintswalo, Acornhoek, Mpumalanga Province in April 2022 and was also evaluated immediately after training. The third group (Benin 6 months) consisted of 8 physicians working in the National Teaching Hospital for Tuberculosis and Lung Diseases in Cotonou, Benin and were trained in September 2021. Since their initial training, this group had weekly 1-hour voluntary POCUS case meetings and on-demand POCUS supervision for selected cases. Participants were evaluated six months after their initial training, in March 2022.
Statistical evaluation
We report the overall success rates of all participants (percentage of points obtained out of a total of 60 points), as well as success rates by LUS-OSAUS area (N = 6) and by individual items (N = 18).
To assess differences by region and by time elapsed since training, we analyze and compare the success rates overall, by area and by item between Benin 0 months and South Africa 0 months as well as between Benin 0 months and Benin 6 months, respectively, using the Fischer’s exact test. All statistical analyses are performed using the STATA statistics software package, version 17.0.
Results
A total of 35 out of 43 trainees completed and uploaded the LUS-OSAUS quiz and skills test and are part of the analysis. No participant was previously certified in ultrasonography. However, the groups showed some differences in terms of previous lung POCUS practice as summarized in Table 2. In the Benin 0 months group, 5 (31%) already practiced unsupervised lung ultrasound before the skills assessment (3 practiced daily and 2 on a weekly basis in the last 6 months) without previous standardized training. In the South Africa group, all participants were novices. In the Benin 6-month group, 6 trainees (86%) had daily unsupervised practice of lung ultrasound during the time between training and assessment.
Table 2.
Summary of group characteristics. * with quiz and skills completed and uploaded
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| Benin 0 months | South Africa 0 months | Benin 6 months | |
| Date of training | February 2022 | April 2022 | September 2021 |
| Number of participants | 18 | 17 | 8 |
| Number of participants included in the analysis* | 16 | 12 | 7 |
| Previous lung POCUS practice | |||
| Daily | 3 | 0 | 6 |
| Weekly | 2 | 0 | 0 |
| Monthly | 0 | 0 | 0 |
| Never | 11 | 12 | 1 |
The overall success rate was 0.84 (95%CI 0.80–0.88). The two areas that exhibited the highest levels of success (≥ 0.80) are “indication of lung POCUS”, with a score of 1 (95% CI 0.90-1), and “documentation of findings”, with a score of 0.91 (95% CI 0.77–0.98). The areas with a moderate level of success (0.70–0.79) are “findings on lung POCUS”, with a score of 0.77 (95% CI 0.60–0.90) and “conclusion”, with a score of 0.71 (95% CI 0.54–0.85). The area with the lowest level of success (< 0.70) is “technical skills” with a score of 0.66 (95% CI 0.48–0.81). Among the 18 items, a majority (14/18, 78%) exhibited the highest levels of success (≥ 0.80), with maximum scores achieved by assessment of pleural effusion, B-lines, and indication of lung POCUS. Two items had a moderate level of success (0.70–0.79): “correct choice of transducer/preset” with a score of 0.71 (95% CI 0.54–0.85) and “conclusion” also with a score of 0.71 (95% CI 0.54–0.85). Two items had the lowest level of success (< 0.70): “correct depth” with a score of 0.54 (0.37–0.71) and “correct assessment of pleura” with a score of 0.63 (0.45–0.79). Although the depth choice was often incorrect, there was a high level of success on “interpretability of the images” at 0.80 (95%CI 0.63–0.92).
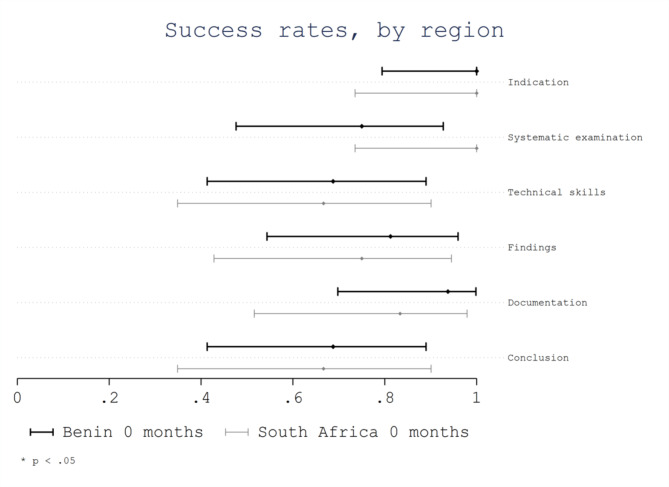
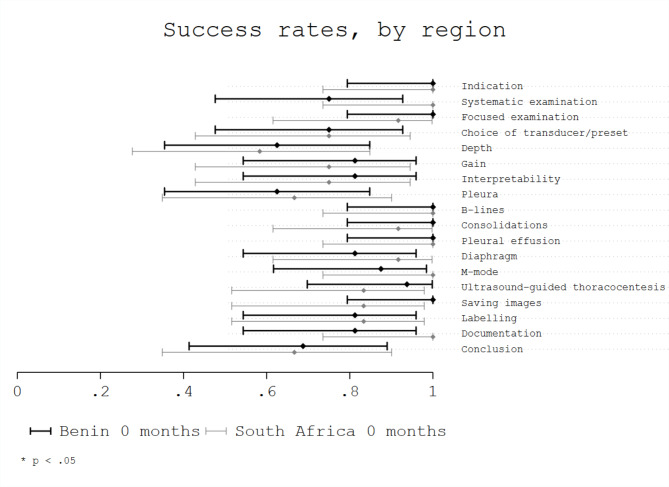
Considering geographical region (Benin 0 months vs. South Africa 0 months), no significant differences were observed, with respective overall success rates of 0.86 (95%CI 0.80–0.92) for Benin 0 months and 0.83 (95%CI 0.75–0.91) for South Africa 0 months (p = 0.13). No significant differences were observed in the success rates of evaluated areas based on the region (Fig. 2). However, trainees from Benin showed a non-significant lower success rate for the area “systematic examination” with a score of 0.75 (95% CI 0.48–0.93) compared with trainees from South Africa with a score of 1.0 (95% CI 0.74-1.0; p = 0.11). No significant differences were observed in the success rates of evaluated items based on the region (Fig. 3).
Fig. 2.
Success rate per area by region
Fig. 3.
Success rate per item by region
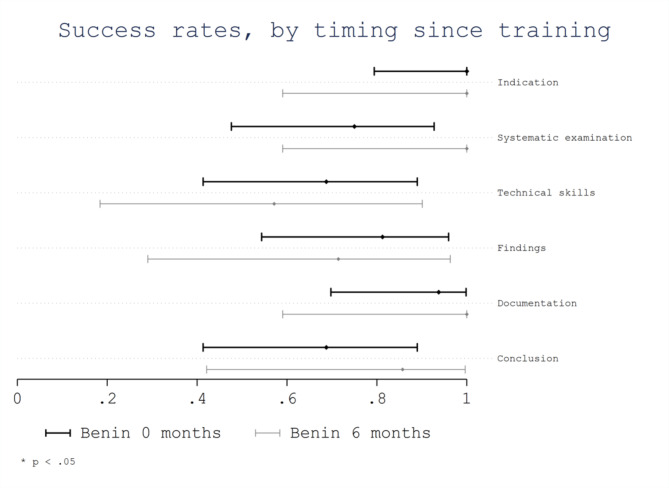
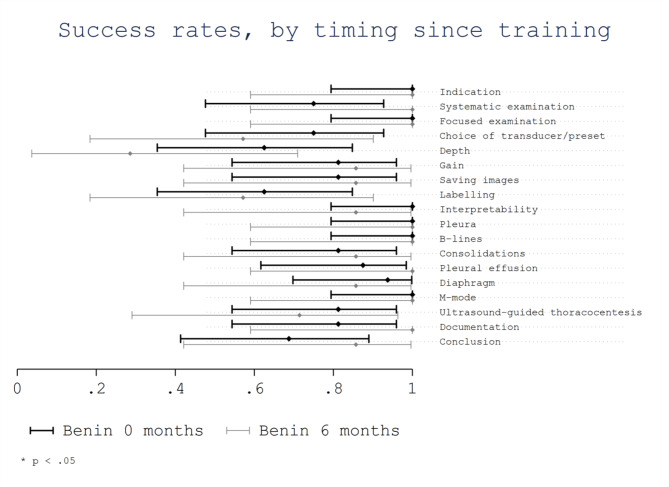
Considering time elapsed since training (Benin 0 months vs. Benin 6 months) no significant differences were observed. The overall success rate was 0.86 (95%CI 0.80–0.92) for Benin 0 months and 0.82 (95%CI 0.72–0.93) for Benin 6 months (p = 0.56). No significant differences were observed in the success rates of evaluated areas (Fig. 4). However, trainees from Benin 0 months showed a non-significant lower success rate for the area “systematic examination” with a score of 0.75 (95% CI 0.48–0.93) compared with trainees from Benin 6 months with a score of 1.0 (95% CI 0.59-1.0; p = 0.27). In addition, trainees from Benin 0 months showed a non-significant lower success rate for the area “conclusion” with a score of 0.69 (95% CI 0.41–0.89) compared with trainees from Benin 6 months with a score of 0.86 (95% CI 0.42-1.0; p = 0.62). No significant differences were observed in the success rates of evaluated items based on the time since training, although trainees from Benin 0 months showed a non-significant higher success rate for some scanning technical skills as the “correct choice of transducer/preset”, the “correct depth” and the “labelling of anatomical position” (Fig. 5).
Fig. 4.
Success rate per area by timing elapsed since training
Fig. 5.
Success rate per item by timing elapsed since training
Discussion
Web-based objective and structured assessment of theoretical and practical lung POCUS skills in low-resource settings is feasible and revealed a good overall success rate of 0.84 (95%CI 0.80–0.88) after a short 4-day training. In line with our findings, previous studies on learning curves of various POCUS domains showed that lung POCUS is indeed a relatively easy skill to acquire [15, 16]. To reach basic technical competence, it is estimated that 5 to 25 supervised lung POCUS exams are necessary [16–19]. The following items appear the most challenging: (1) setting the correct depth, (2) correct assessment of the normal pleura and (3) POCUS based clinical conclusions.
First, it is important to note that even within a context of longitudinal (e.g., 6 months) lung POCUS learning programs correct depth and axis of the probe remain challenging [15, 16]. Depth is particularly important in assessing the lower lung quadrants allowing to correctly visualize the diaphragm to make a clear distinction between thorax and abdomen. A study after short (4.5 h) training of respiratory therapists, showed that the lower lung quadrants are more challenging to evaluate (98.4 ± 1.8% of upper lung zone images were interpretable versus 91.3 ± 9.5% of lower lung zone images were interpretable) [20].
Second, our study also points out that trainees have particular difficulties with recognizing normal pleura as opposed to the facility to recognize B-lines and pleural effusions. After a 4-day training on the BLUE-protocol in Italy, internal medicine residents as compared to experienced sonographers performed “excellent” for the recognition of B-lines and pleural effusion ((with kappas of 0.90 (0.88–0.92) and 0.82 (0.81–0.83) respectively). However, similar to our findings, recognition of the normal lung was more challenging with a kappa of 0.65 (0.61–0.69) [21]. A recent study showed that after a very short 1.5 h training for ICU nurses, the normal pleura and lung sliding are also significantly more challenging to recognize as compared to the B-line pattern (0.34 (0.24–0.48) correct interpretation versus 0.88 (0.76–0.92) respectively) [22]. Our participants tend to err on the side of seeing pathology. For instance, Z-lines which are small subpleural artefacts seen in 80% of the normal population [23], are mistakenly taken for subpleural consolidations (overinterpretation). In specific settings where subtle pleural lesions are important for diagnosis (e.g., diagnosis of pulmonary tuberculosis), 50.8% of inter reader mismatches are between normal pleura and subpleural lesions of less than 1 cm [24]. Training in this setting is reportedly more time-intensive requiring on-site presence of a skilled trainer over a longer period of time [25].
Third, trainees had difficulties integrating POCUS findings into clinical-decision making. This skill tends to improve with practice as shown by a tendency to better performance 6 months after training. This is consistent with a study in Rwanda where learners had better thoracic POCUS integration skills 58-weeks post training. However, in this study, training course was intensive with frequent follow-up training [26] A study in Ghana using clinical vignettes to assess the skill of integrating cardiopulmonary POCUS findings found a stable performance 9–11 months after a short initial training. This might be because of a focus on cardiac and abdominal POCUS (83% and 92% of participants with weekly practice respectively) as compared to lung POCUS (78% weekly practice) [27].
Regarding timing after initial training, success rates remained high after 6 months including minimal continuous education as described above. The overall consistency of POCUS skills after short (1.5 h to 4 day) training courses over time aligns with previous research in low- [25, 27] as well as high-income countries [20, 28, 29].
To improve lung POCUS skills over time, additional continuous ultrasound training including direct supervision and targeted ultrasound rounds lead to significantly better results [29–31]. However, current limited opportunities in LMIC for supervised practice have been identified as an important barrier [32, 33]. This barrier might be partly overcome with remote supervision applications and artificial intelligence (AI) support [25, 34]. We further suggest that besides technical skills, continuous training should also give particular attention to integrating POCUS findings into clinical decision-making.
No significant difference in success rate was found based on geographic region (South-Africa vs. Benin). Globally, online lung POCUS training has gained substantial momentum in recent years [28, 35]. These consistent outcomes across regions are encouraging for the potential and broader applicability of this web-based evaluation tool for LMICs.
Finally, collaborative efforts involving the academic and the private sector, governments and NGOs are crucial to establish longitudinal training programs where needed, ensure quality control including AI support and promote safe and sustainable adoption of lung POCUS in LMIC [25, 36, 37].
Limitations
The participants in our study might not accurately represent all healthcare professionals learning in low-income practice environments. Those who subscribed for training expressed a personal interest in gaining ultrasound skills and sometimes traveled far for this training. As a result, the performance of this specific group might not be applicable to a wider range of healthcare professionals. Additionally, limitations include the small number of participants involved in the study, their heterogeneity (some with previous experience) and difficulties with connectivity or informatics (8 out of 43 trainees could not fully upload their test). The small number of participants in each group (based on geographical regions and timing since training) provide limited power for comparison. Another limitation is linked to the group definition” timing after training”. Indeed, we did not follow up longitudinally the same group of trainees, but compared two different groups of trainees according to the timing elapsed since training.
Conclusion
Web-based objective and structured assessment of lung POCUS skills in LMIC following a short standardized training is feasible and showed a good overall success rate among trainees with consistent results across regions and up to 6 months after training given minimal continuous education. Overinterpretation is an important beginner’s mistake and the acquisition of technical and integrative clinical skills can be challenging. Continuous training modules can improve technical skills and should also give particular attention to the integration of POCUS findings in clinical-decision making. Collaborative efforts are needed for further standardization of lung POCUS training curricula and validation in LMIC.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors wish to acknowledge Ginette Makpemikpa, Aboudou Hada, Frédéric Alovokpinhou and Brice Guendehou for their contribution to the onsite training sessions.
Abbreviations
- AI
Artificial intelligence
- ICU
Intensive care unit
- LMIC
Low- and middle-income countries
- LUS
Lung ultrasound
- LUS-OSAUS
Lung ultrasound objective and structured assessment ultrasound score
- NGO
Non-governmental organization
- POCUS
Point-of-care-ultrasound
- USA
United States of America
Author contributions
V.S. designed the training program, online quiz and skills test. I.C. collected and analyzed the dataset together with statistical expert J.B. V.S. and I.C. wrote the first draft. MA.H., J.DT., PA.M., E.G., G.A. and T.B. reviewed the training program design and course content, online quiz and skills test. PA.W. and N.B.B. conceptualized the study and did the final manuscript review.
Funding
The training program is supported by the Lausanne University Hospital Humanitarian Fund and the Butterfly Network Global Health Program.
Open access funding provided by University of Lausanne
Data availability
The links to course content and online quiz are available in the appendix. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval and informed consent was waived by the research committee of the university of Parakou, Benin.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Veronique Suttels and Ines Chichignoud contributed equally to this work.
References
- 1.Buda N, Mendrala K, Skoczyński S, Pasquier M, Mazur P, Garcia E, et al. Basics of point-of-care Lung Ultrasonography. N Engl J Med. 2023;389(21):e44. 10.1056/NEJMvcm2108203 [DOI] [PubMed] [Google Scholar]
- 2.Buonsenso D, De Rose C. Implementation of lung ultrasound in low- to middle-income countries: a new challenge global health? Eur J Pediatr. 2021:1–8. [DOI] [PMC free article] [PubMed]
- 3.Yadav H, Shah D, Sayed S, Horton S, Schroeder LF. Availability of essential diagnostics in ten low-income and middle-income countries: results from national health facility surveys. Lancet Glob Health. 2021;9(11):e1553–60. 10.1016/S2214-109X(21)00442-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart KA, Navarro SM, Kambala S, Tan G, Poondla R, Lederman S, et al. Trends in Ultrasound Use in Low and Middle Income countries: a systematic review. Int J MCH AIDS. 2020;9(1):103–20. 10.21106/ijma.294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suttels V, Du Toit JD, Fiogbé AA, Wachinou AP, Guendehou B, Alovokpinhou F, et al. Point-of-care ultrasound for tuberculosis management in Sub-saharan Africa-a balanced SWOT analysis. Int J Infect Dis. 2022;123:46–51. 10.1016/j.ijid.2022.07.009 [DOI] [PubMed] [Google Scholar]
- 6.Castro G. Top 10 health technology hazards for 2020. Oakbrook Terrace, IL : The Joint Commission, January 3, 2020 (https://www.jointcommission.org/en/resources/news-and-multimedia/blogs/dateline-tjc/2020/01/top-10-health-technology-hazards-for-2020/. opens in new tab).
- 7.Prager R, Wu D, Garber G, Finestone PJ, Zang C, Aslanova R, et al. Medico-legal risks of point-of-care ultrasound: a closed-case analysis of Canadian Medical Protective Association medico-legal cases. Ultrasound J. 2024;16(1):16. 10.1186/s13089-024-00364-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Díaz-Gómez JL, Mayo PH, Koenig SJ. Point-of-Care Ultrasonography. N Engl J Med. 2021;385(17):1593–602. 10.1056/NEJMra1916062 [DOI] [PubMed] [Google Scholar]
- 9.Ali N, Soomar SM, Waheed S. Point-of-care ultrasound training in low-income countries: a need of time. Ann Med Surg (Lond). 2023;85(4):1356–7. 10.1097/MS9.0000000000000397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wachira J, Matheka DM, Masheti SA, Githemo GK, Shah S, Haldeman MS, et al. A training program for obstetrics point-of-care ultrasound to 514 rural healthcare providers in Kenya. BMC Med Educ. 2023;23(1):922. 10.1186/s12909-023-04886-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amini R, Adhikari S, Fiorello A. Ultrasound competency assessment in emergency medicine residency programs. Acad Emerg Med. 2014;21(7):799–801. 10.1111/acem.12408 [DOI] [PubMed] [Google Scholar]
- 12.Skaarup SH, Laursen CB, Bjerrum AS, Hilberg O. Objective and structured Assessment of Lung Ultrasound competence. A Multispecialty Delphi Consensus and Construct Validity Study. Annals Am Thorac Soc. 2017;14(4):555–60. 10.1513/AnnalsATS.201611-894OC [DOI] [PubMed] [Google Scholar]
- 13.Di Pietro S, Mascolo M, Falaschi F, Brambilla W, Ruzga R, Mongodi S, et al. Lung-ultrasound objective structured assessment of technical skills (LUS-OSAUS): utility in the assessment of lung-ultrasound trained medical undergraduates. J Ultrasound. 2021;24(1):57–65. 10.1007/s40477-020-00454-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thorndike RL, Angoff WH. Education ACo. Educational Measurement: American Council on Education; 1971. [Google Scholar]
- 15.Breunig M, Hanson A, Huckabee M. Learning curves for point-of-care ultrasound image acquisition for novice learners in a longitudinal curriculum. Ultrasound J. 2023;15(1):31. 10.1186/s13089-023-00329-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blehar DJ, Barton B, Gaspari RJ. Learning curves in emergency ultrasound education. Acad Emerg Med. 2015;22(5):574–82. 10.1111/acem.12653 [DOI] [PubMed] [Google Scholar]
- 17.Arbelot C, Dexheimer Neto FL, Gao Y, Brisson H, Chunyao W, Lv J, et al. Lung Ultrasound in Emergency and critically ill patients: number of supervised exams to Reach Basic competence. Anesthesiology. 2020;132(4):899–907. 10.1097/ALN.0000000000003096 [DOI] [PubMed] [Google Scholar]
- 18.Russell FM, Ferre R, Ehrman RR, Noble V, Gargani L, Collins SP, et al. What are the minimum requirements to establish proficiency in lung ultrasound training for quantifying B-lines? ESC Heart Fail. 2020;7(5):2941–7. 10.1002/ehf2.12907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stolz LA, Stolz U, Fields JM, Saul T, Secko M, Flannigan MJ, et al. Emergency Medicine Resident Assessment of the emergency Ultrasound milestones and current training recommendations. Acad Emerg Med. 2017;24(3):353–61. 10.1111/acem.13113 [DOI] [PubMed] [Google Scholar]
- 20.Young A, Wu D, Myslik F, Burke D, Stephens M, Arntfield R. Acquisition and retention of lung ultrasound skills by respiratory therapists: a curriculum for respiratory therapists. Can J Respir Ther. 2023;59:26–32. 10.29390/cjrt-2021-077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mozzini C, Fratta Pasini AM, Garbin U, Cominacini L. Lung ultrasound in internal medicine: training and clinical practice. Crit Ultrasound J. 2016;8(1):10. 10.1186/s13089-016-0048-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mongodi S, Arioli R, Quaini A, Grugnetti G, Grugnetti AM, Mojoli F. Lung ultrasound training: how short is too short? Observational study on the effects of a focused theoretical training for novice learners. BMC Med Educ. 2024;24(1):166. 10.1186/s12909-024-05148-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134(1):117–25. 10.1378/chest.07-2800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suttels V et al. Diagnostic performance of thoracic point-of-care ultrasound for pulmonary tuberculosis - the TrUST cohort (unpublished data – 2024).
- 25.Fentress M, Henwood PC, Maharaj P, Mitha M, Khan D, Jackpersad R, et al. Thoracic ultrasound for TB diagnosis in adults and children. Public Health Action. 2022;12(1):3–6. 10.5588/pha.21.0072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henwood PC, Mackenzie DC, Rempell JS, Douglass E, Dukundane D, Liteplo AS, et al. Intensive point-of-care ultrasound training with long-term follow-up in a cohort of Rwandan physicians. Trop Med Int Health. 2016;21(12):1531–8. 10.1111/tmi.12780 [DOI] [PubMed] [Google Scholar]
- 27.Osei-Ampofo M, Tafoya MJ, Tafoya CA, Oteng RA, Ali H, Becker TK. Skill and knowledge retention after training in cardiopulmonary ultrasound in Ghana: an impact assessment of bedside ultrasound training in a resource-limited setting. Emerg Med J. 2018;35(11):704–7. 10.1136/emermed-2018-207716 [DOI] [PubMed] [Google Scholar]
- 28.Schott CK, LoPresti CM, Boyd JS, Core M, Haro EK, Mader MJ, et al. Retention of Point-of-care Ultrasound skills among practicing Physicians: findings of the VA National POCUS Training Program. Am J Med. 2021;134(3):391–e98. 10.1016/j.amjmed.2020.08.008 [DOI] [PubMed] [Google Scholar]
- 29.Matthews L, Contino K, Nussbaum C, Hunter K, Schorr C, Puri N. Skill retention with ultrasound curricula. PLoS ONE. 2020;15(12):e0243086. 10.1371/journal.pone.0243086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelm DJ, Ratelle JT, Azeem N, Bonnes SL, Halvorsen AJ, Oxentenko AS, et al. Longitudinal Ultrasound Curriculum improves Long-Term Retention among Internal Medicine residents. J Grad Med Educ. 2015;7(3):454–7. 10.4300/JGME-14-00284.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rominger AH, Gomez GAA, Elliott P. The implementation of a longitudinal POCUS curriculum for physicians working at rural outpatient clinics in Chiapas, Mexico. Crit Ultrasound J. 2018;10(1):19. 10.1186/s13089-018-0101-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Veronique S, Sofia Guedes Da C, Elena G, Thomas B, Mary-Anne H, Gildas A, et al. Barriers and facilitators to implementation of point-of-care lung ultrasonography in a tertiary centre in Benin: a qualitative study among general physicians and pneumologists. BMJ Open. 2023;13(6):e070765. 10.1136/bmjopen-2022-070765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah S, Santos N, Kisa R, Mike Maxwell O, Mulowooza J, Walker D, et al. Efficacy of an ultrasound training program for nurse midwives to assess high-risk conditions at labor triage in rural Uganda. PLoS ONE. 2020;15(6):e0235269. 10.1371/journal.pone.0235269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evangelista A, Galuppo V, Méndez J, Evangelista L, Arpal L, Rubio C, et al. Hand-held cardiac ultrasound screening performed by family doctors with remote expert support interpretation. Heart. 2016;102(5):376–82. 10.1136/heartjnl-2015-308421 [DOI] [PubMed] [Google Scholar]
- 35.Eke OF, Henwood PC, Wanjiku GW, Fasina A, Kharasch SJ, Shokoohi H. Global point-of-care ultrasound education and training in the age of COVID-19. Int J Emerg Med. 2021;14(1):12. 10.1186/s12245-021-00338-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frija G, Salama DH, Kawooya MG, Allen B. A paradigm shift in point-of-care imaging in low-income and middle-income countries. EClinicalMedicine. 2023;62:102114. 10.1016/j.eclinm.2023.102114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abrokwa SK, Ruby LC, Heuvelings CC, Bélard S. Task shifting for point of care ultrasound in primary healthcare in low- and middle-income countries-a systematic review. EClinicalMedicine. 2022;45:101333. 10.1016/j.eclinm.2022.101333 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The links to course content and online quiz are available in the appendix. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.