Abstract
PURPOSE
This cone-beam computed tomography (CBCT) study aimed to analyze the anatomical characteristics of alveolar bone at mandibular first molar (MFM) and their implications for immediate implant placement surgery.
MATERIALS AND METHODS
100 patients with 140 MFMs were reviewed retrospectively. We first performed a 3D reconstruction of the patient’s CBCT data to determine a reference plane with ideal implant placement and orientation. The following parameters of MFM region were analyzed: mesial-distal socket size (MD-SS), buccal-lingual socket size (BL-SS), root furcation fornix to inferior alveolar nerve (IAN) distance (RF-I), interradicular bone thickness (IRB), mesial/distal root apex to the IAN distance (MRA-I/DRA-I), thickness of the buccal/lingual bone of the mesial root (MR-B/MR-L), thickness of the buccal/lingual bone of the distal root (DR-B/DR-L).
RESULTS
The MD-SS of MFM was 8.74 ± 0.76 mm, and the BL-SS was 8.26 ± 0.72 mm. The MR-B, DR-B was 1.01 ± 0.40 mm and 1.14 ± 0.50 mm, and the difference was statistically significant (P = .001). The values of the MR-L, DR-L were 2.71 ± 0.78 mm and 3.09 ± 0.73 mm, and the difference was also statistically significant (P < .001). The mean distance of RF-I was 15.68 ± 2.13 mm, and the MRA-I was 7.06 ± 2.22 mm, which was greater than that of DRA-I (6.48 ± 2.30 mm, P < .001). The IRB at 2 mm, 4 mm apical from the furcation fornix, and at apex level was 2.81 ± 0.50 mm, 3.30 ± 0.62 mm, and 4.44 ± 1.02 mm, respectively.
CONCLUSION
There is relatively sufficient bone mass in interradicular bone in height, but an adequate width is lacking for the bone between the mesial and distal root after the extraction of the MFM for immediate implantation. The thickness of the MFM buccal bone is relative thin, especially for the mesial root.
Keywords: Mandibular first molar, Immediate implant placement, Cone-beam computed tomography, Anatomical analysis
INTRODUCTION
Due to the high long-term success and survival rates, dental implant-supported dentures are becoming a preferred choice for increasing numbers of patients with missing teeth.1 Currently, according to the timing of implant placement, implantation surgery is divided into immediate, early and delayed implantation.2 Compared with early and delayed implantation, immediate dental implant placement is generally characterized by the implantation of dental implants in the fresh extraction socket at the time of tooth extraction, which greatly shortens the time of missing teeth for patients.3 However, due to the limitations of anatomical conditions, wound closure and other factors, immediate implant placement is mostly used in anterior teeth or single-rooted premolars in the clinic, while multirooted molars are relatively rarely used.
The mandibular first molar is the first permanent tooth to erupt and has the most powerful masticatory function. The loss of the first molar caused by various factors, such as caries, will greatly affect the masticatory function of patients.4,5 In general, after the extraction of the molars, it is necessary to wait 3 months for the healing of the socket, and then perform delayed implant surgery. However, for mandibular first molars with vertical fracture or a residual root and residual crown without acute or chronic inflammation, immediate implantation may be a good choice.
Considering that the mandibular first molar plays a major role in maintaining normal masticatory function and dentofacial harmony,6 it is of great significance to repair it as soon as possible. However, as described above, the performance of immediate dental implant placement is associated with certain risks and technical sensitivity for mandibular molars because of the multi-roots and the existence of the inferior alveolar nerve.7,8 Only by fully understanding the relevant anatomical characteristics and parameters of mandibular first molars can we achieve good results in the immediate implant surgery of molars, which is also beneficial for improving safety and reducing the incidence of complications.
Although there have been studies focusing on the alveolar bone anatomy of the mandibular first molar related to immediate dental implant placement, these studies have limitations. Some studies focus on relevant parameters which are not comprehensive. For example, some studies only focus on the alveolar bone mass and do not pay attention to the relationship between the position of the extraction sockets and inferior alveolar nerve (IAN).9 Limited studies performed the analysis of alveolar bone around mandibular first molar with ideal implant placement and orientation,7,8,10 and it is certain that these data obtained may weaken the guiding significance for the clinic. In addition, no research has paid attention to the difference between the thickness of the buccal and lingual bone of mesial and distal root after the extraction of the mandibular first molar. On the whole, to ensure the success and safety of immediate dental implant placement in mandibular first molar, the alveolar bone mass around the mandibular first molar, the distance between the key anatomical point and IAN, the size of the alveolar socket and thickness of the buccal/lingual bone of the mesial/distal root after tooth extraction are both extremely important.
Therefore, in this retrospective cone-beam computed tomography (CBCT) study, we carried out a comprehensive analysis of the above problems and parameters of mandibular first molars. To provide more clinically realistic data, we first determined an ideal restoration-oriented implant direction on CBCT and then evaluated the anatomical parameters of the mandibular molar region to facilitate safe and effective immediate implant placement surgery. Our study aimed to provide database guidance to dentists.
MATERIALS AND METHODS
The study protocol was approved by the Ethics Committee of the Chinese PLA General Hospital (Approval Number: S2022-347-01). From January 2021 to December 2023, 100 patients with 140 mandibular first molars were included in the current study. All of the included patients were scheduled to undergo implant restoration in the Oral Implant Department of Chinese PLA General Hospital. The imaging data of mandibular first molars were extracted from the preoperative CBCT of the patients.
-
The inclusion criteria are as follows:
Patients between the ages of 20 and 60 years;
At least one mandibular first molar with a root divided into mesial root and distal root;
No severe malocclusion, severe periapical inflammation, or obvious root resorption; no severe alveolar bone resorption (the level of the alveolar bone must be above the root furcation fornix);
No obvious elongation or inclination of the mandibular first molar.
-
The exclusion criteria are as follows:
Patients who had undergone or were currently undergoing orthodontic treatment;
The anatomical structure was not clearly observed, or IAN canal could not be clearly identified by CBCT images;
Age less than 20 years or greater than 60 years;
Presence of tumors or large-scale cysts in the target area.
Serious periodontal disease or other reasons leading to alveolar bone resorption blew the root furcation fornix.
CBCT images of all subjects were acquired with a Newtom 5G scanner (QR SRL, Verona, Italy) using an enhanced scanning protocol and the following parameters: 110 kVp, mA automatically determined by the initial scout exposure, field of view 12 cm × 8 cm, and exposure time 4.8 s. The images were reconstructed with a voxel size of 0.3 mm. Image analysis software (NNT Viewer, Version 5.3; NewTom, Verona, Italy) was used to measure related metrics.
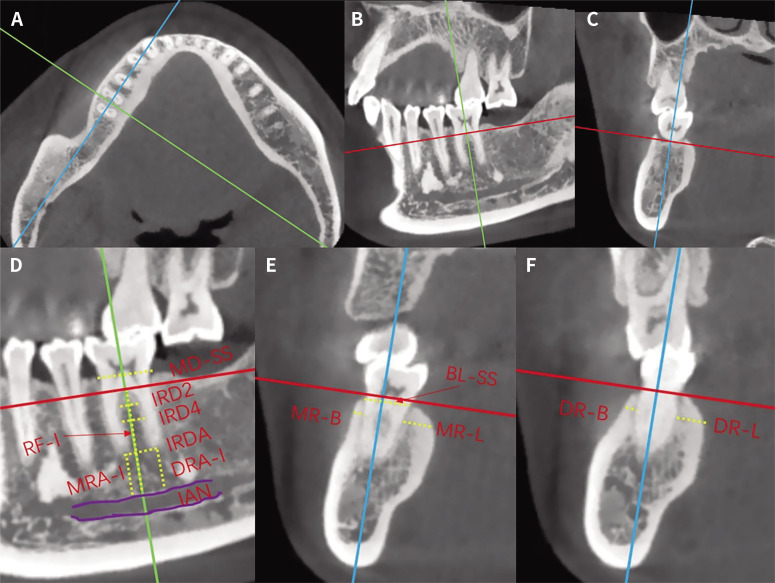
Before parameter measurement, 3D reconstruction of the patient’s CBCT data was performed to determine the reference planes in the ideal implant position and orientation. As shown in Figure 1, the green line represents the coronal plane, and the green line passes through the center of the crown of the mandibular first molar in the bucco-lingual upward direction, which is also parallel to the long axis of the mandibular first molar in the mesial-distal direction; the blue line represents the sagittal plane, and the reference line is perpendicular to the green line, which is also parallel to the long axis of the mandibular first molar in the bucco-lingual direction; and red represents the horizontal plane, which is parallel to the patient’s occlusal plane and perpendicular to the green and blue lines.
Fig. 1. Reference plane determination and measurement parameters. (A) Horizontal-sectional slice, (B) Sagittal-sectional slice, (C) Coronal-sectional slice, (D) Measurement parameters in the sagittal section, (E) Measurement parameters in the coronal section of the mesial root, (F) Measurement parameters of the coronal section of the distal root. The green line represents the coronal plane; the blue line represents the sagittal plane; and red represents the horizontal plane, which is parallel to the patient’s occlusal plane. The purple line represents the border of the inferior alveolar nerve. The yellow dotted line indicates the measured parameters. MD-SS: mesial-distal socket size; BL-SS: buccal-lingual socket size; RF-I: root furcation fornix to inferior alveolar nerve distance; IRB2/IRB4: the interradicular alveolar bone thickness at 2/4 mm apical from the furcation fornix; IRBA: the interradicular alveolar bone thickness between the mesial and distal root apex; MRA-I/DRA-I: mesial/distal root apex to the inferior alveolar nerve distance; MR-B/MR-L: thickness of the buccal/lingual bone of the mesial root at 2 mm apical from the alveolar crest; DR-B/DR-L: thickness of the buccal/lingual bone of the distal root at 2 mm apical from the alveolar crest.
The following measurement parameters closely related to the immediate implantation of mandibular first molars were analyzed (Fig. 1):
The mesial-distal socket size (MD-SS): the mesial-distal extraction socket size at the alveolar bone crest level.
Buccal-lingual socket size (BL-SS): the buccal-lingual extraction socket size at the alveolar bone crest level. The longest distance between the buccal and lingual alveolar crest of the mandibular first molar in the coronal plane was measured.
Root furcation fornix to inferior alveolar nerve distance (RF-I): the shortest bone height from the root furcation fornix to the IAN in the vertical direction. A line segment parallel to the vertical reference line was drawn from the highest point of alveolar bone at the root furcation fornix to the mandibular canal.
Interradicular bone thickness (IRB): the thickness of the alveolar bone at different positions of the interradicular bone. Specifically, based on the RF-I line segment, the interradicular alveolar bone thicknesses at 2 mm (IRB2), 4 mm (IRB4) apical from the furcation fornix, and at the apex (IRBA) level were measured. Measurements of the thickness need to be taken perpendicular to the RF-I.
Mesial/distal root apex to the IAN distance (MRA-I/DRA-I): the shortest bone height from the mesial/distal root apex to the IAN canal in the vertical direction. A line segment parallel to the vertical reference line was drawn from the apex of the mesial root to the mandibular canal.
Thickness of the buccal/lingual bone of the mesial root (MR-B, MR-L): The thickness of the buccal/lingual bone of the mesial root was measured at 2 mm apical from the mesial root’s buccal and lingual alveolar crest, respectively. Measurements of the thickness need to be taken perpendicular to the blue line, as shown in Figure 1E and F.
Thickness of the buccal/lingual bone of the distal root (DR-B, DR-L): The thickness of the buccal and lingual bone of the distal root was measured at 2 mm apical from the distal root’s buccal and lingual alveolar crest, respectively. The measurement method is the same as that used for MR-B and MR-L.
SPSS 19.0 software (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. The mean and standard deviation (SD) were calculated for all of the measurements. Student’s t test was used for statistical analyses for the comparison between the left and right molar or the male and female. The paired t test was used for the comparison between mesial and distal roots, including the MRA-I vs DRA-I, MR-B vs DR-B, etc. If the data did not meet the conditions of the Student’s t-test, the Mann-Whitney U-test was be used. P < .05 was considered statistically significant.
RESULTS
A total of 100 patients were included in this study, including 54 males and 46 females, all of whom were of Han nationality; the mean age was 40.15 ± 10.38 years. A total of 140 mandibular first molars were analyzed, including 75 left mandibular first molars and 65 right mandibular first molars.
The measurement of the MD-SS and BL-SS showed that the average values at the crest level were 8.74 ± 0.76 mm and 8.26 ± 0.72 mm, respectively (Table 1). The difference between MD-SS values for the left and right mandibular first molars was not statistically significant (P = .81). The difference between BL-SS values for the left and right mandibular first molars was of no statistically significance (P = .27).
Table 1. The extraction socket size of the mandibular first molar.
| Teeth | N | MD-SS | BL-SS |
|---|---|---|---|
| Total | 140 | 8.74 ± 0.76 | 8.26 ± 0.72 |
| Left mandibular first molar | 75 | 8.73 ± 0.75 | 8.19 ± 0.70 |
| Right mandibular first molar | 65 | 8.74 ± 0.78 | 8.34 ± 0.73 |
N: number of the teeth; MD-SS: mesial-distal socket size; BL-SS: buccal-lingual socket size.
The average values of MR-B, DR-B, MR-L and DR-L of the extraction socket were shown in Table 2. The thickness of the buccal/lingual bone of the distal root at 2 mm apical from the alveolar crest was thicker than that of the mesial root, corresponding to a statistically significant difference (P = .001 for MR-B vs DR-B, P < .001 for the MR-L vs DR-L).
Table 2. Thickness of the buccal/lingual bone of the roots at 2 mm apical from the alveolar crest.
| Root | TB | TL |
|---|---|---|
| MR | 1.01 ± 0.40 | 2.71 ± 0.78 |
| DR | 1.14 ± 0.50* | 3.09 ± 0.73# |
MR: mesial root; DR: distal root; TB: thickness of the buccal bone; TL: thickness of the lingual bone. *: P < .05 compared with the MR-B; #: P < .05 compared with the MR-L.
As shown in Table 3, in the ideal three-dimensional orientation of implant placement, the mean RF-I distance was 15.68 ± 2.13 mm. The frequency distribution of RF-I measurements is shown in the Table 4, with 83.57% of teeth having RF-I values between 12.1 mm and 18.0 mm. In a total of 97.86% of the mandibular first molars, this distance was greater than 12.0 mm. The mean MRA-I of the mandibular first molar was 7.06 ± 2.22 mm, the MRA-I value of teeth accounts for the largest proportion in 6.1 – 8.0 mm, which is 36.43% (Table 5); while the largest proportion of DRA-I values was between 6.1 – 8.0 mm, as high as 32.14% (Table 5). The distal root apex was closer to the IAN compared to the mesial root, the difference was statistically significant (P < .001).
Table 3. Distance to the IAN and available bone thickness measurements.
| Parameter | Mean ± SD | Minimum value | Maximum value |
|---|---|---|---|
| RF-I | 15.68 ± 2.13 | 9.8 | 21.7 |
| MRA-I | 7.06 ± 2.22 | 2.2 | 14.3 |
| DRA-I | 6.48 ± 2.30 | 1.4 | 12.9 |
| IRB2 | 2.81 ± 0.50 | 1.6 | 4.0 |
| IRB4 | 3.30 ± 0.62 | 2.1 | 5.1 |
| IRBA | 4.44 ± 1.02 | 1.9 | 7.5 |
RF-I: root furcation fornix to inferior alveolar nerve distance; MRA-I/DRA-I: mesial/distal root apex to the inferior alveolar nerve distance; IRB2/IRB4: the interradicular alveolar bone thickness at 2 mm, 4 mm apical from the furcation fornix; IRBA: the interradicular alveolar bone thickness between the mesial and distal root apex.
Table 4. Frequency distribution of the RF-I.
| Range | N | Ratio (%) |
|---|---|---|
| ≤ 10.0 | 1 | 0.71 |
| 10.1 ‒ 12.0 | 2 | 1.43 |
| 12.1 ‒ 14.0 | 34 | 24.29 |
| 14.1 ‒ 16.0 | 45 | 32.14 |
| 16.1 ‒ 18.0 | 38 | 27.14 |
| 18.1 ‒ 20.0 | 15 | 10.71 |
| > 20.0 | 5 | 3.57 |
| Total | 140 | 100 |
Table 5. Frequency distribution of the root apex to the IAN measurements.
| Range | MRA-I | DRA-I | ||
|---|---|---|---|---|
| N | Ratio (%) | N | Ratio (%) | |
| ≤ 2.0 | 0 | 0.00 | 2 | 1.43 |
| 2.1 ‒ 4.0 | 12 | 8.57 | 21 | 15.00 |
| 4.1 ‒ 6.0 | 31 | 22.14 | 37 | 26.43 |
| 6.1 ‒ 8.0 | 51 | 36.43 | 45 | 32.14 |
| 8.1 ‒ 10.0 | 33 | 23.57 | 25 | 17.86 |
| > 10.0 | 13 | 9.29 | 10 | 7.14 |
| Total | 140 | 100 | 140 | 100 |
MRA-I/DRA-I: mesial/distal root apex to the inferior alveolar nerve distance
The average values of IRB2, IRB4 and IRBA for the width of interradicular bone were shown in Table 3. The frequency distribution of IRB2, IRB4 and IRBA was shown in the Table 6. For the IRB2 and IRB4, 95.71% and 86.43% of teeth had values between 2 – 4 mm, respectively; while the IRA value of mandibular first molars was mainly concentrated in 3 – 6 mm, accounting for 87.86%. In this study, not all of the bone widths between the root apexes were greater than IRB4; specifically, there were 5 teeth with an IRB4 width equal to that of IRBA, while there were 13 teeth with an IRBA width less than those of IRB4.
Table 6. Frequency distribution of the available bone thickness parameters.
| Range | IRB2 | IRB4 | IRBA | |||
|---|---|---|---|---|---|---|
| N | Ratio (%) | N | Ratio (%) | N | Ratio (%) | |
| ≤ 2.0 | 6 | 4.29 | 0 | 0 | 1 | 0.71 |
| 2.1 ‒ 3.0 | 87 | 62.14 | 55 | 39.29 | 9 | 6.43 |
| 3.1 ‒ 4.0 | 47 | 33.57 | 66 | 47.14 | 40 | 28.57 |
| 4.1 ‒ 5.0 | 0 | 0 | 17 | 12.14 | 50 | 35.71 |
| 5.1 ‒ 6.0 | 0 | 0 | 2 | 1.43 | 33 | 23.57 |
| > 6.0 | 0 | 0 | 0 | 0 | 7 | 5.00 |
| Total | 140 | 100 | 140 | 100 | 140 | 100 |
IRB2/IRB4: the interradicular alveolar bone thickness at 2 mm, 4 mm apical from the furcation fornix; IRBA: the interradicular alveolar bone thickness between the mesial and distal root apex.
A total of 72 male mandibular first molars and 68 female mandibular first molars were included in this study, the relevant statistical results are in Table 7. The measurement of the MD-SS and BL-SS showed that the average values of the male is larger than the female, which is of statistical significance (P = .000 and 0.003, respectively). For the mesial root, the average value of MR-B of the extraction socket in the male is thicker than the female (P = .008), while the average value of MR-L for the male is thinner than the female (P = .006). However, for the distal root, there is no statistical difference in the thickness of the buccal and lingual bone plate. For the parameters about distance to the IAN measurements, all of the results showed that the RF-I, MRA-I and DRA-I for the male was greater than the female, and the difference was statistically significant. Besides, The IRB2, IRB4 and IRBA for the width of interradicular bone between the male and female are all of no statistical significance.
Table 7. Results of the related parameters grouped by gender.
| Parameters | Mean ± SD | P values | |
|---|---|---|---|
| Male | Female | ||
| MD-SS | 8.99 ± 0.72 | 8.47 ± 0.71 | .000 |
| BL-SS | 8.43 ± 0.70 | 8.07 ± 0.68 | .003 |
| MR-B | 1.11 ± 0.45 | 0.90 ± 0.31 | .008* |
| MR-L | 2.54 ± 0.80 | 2.89 ± 0.71 | .006 |
| DR-B | 1.18 ± 0.51 | 1.11 ± 0.48 | .413 |
| DR-L | 2.99 ± 0.80 | 3.19 ± 0.65 | .056* |
| RF-I | 16.46 ± 2.10 | 14.85 ± 1.85 | .000 |
| MRA-I | 7.84 ± 2.28 | 6.22 ± 1.82 | .000 |
| DRA-I | 7.27 ± 2.31 | 5.63 ± 1.98 | .000 |
| IRB2 | 2.73 ± 0.48 | 2.88 ± 0.50 | .074 |
| IRB4 | 3.26 ± 0.63 | 3.34 ± 0.61 | .439 |
| IRBA | 4.46 ± 1.06 | 4.41 ± 0.97 | .744 |
MD-SS: mesial-distal socket size; BL-SS: buccal-lingual socket size; MR-B/MR-L: thickness of the buccal/lingual bone of the mesial root at 2 mm apical from the alveolar crest; DR-B/DR-L: thickness of the buccal/lingual bone of the distal root at 2 mm apical from the alveolar crest; RF-I: root furcation fornix to inferior alveolar nerve distance; MRA-I/DRA-I: mesial/distal root apex to the inferior alveolar nerve distance; IRB2/IRB4: the interradicular alveolar bone thickness at 2 mm, 4 mm apical from the furcation fornix; IRBA: the interradicular alveolar bone thickness between the mesial and distal root apex. *: Results from the Mann-Whitney U-test.
DISCUSSION
With the development and maturity of technology and materials, immediate implant placement surgery has achieved similar high implant survival rates to those of delayed implant placement.11,12 For immediate implantation, several factors are of key importance and differ from those related to delayed implant placement.13,14 First, minimally invasive tooth extraction is needed. After the tooth is extracted, the remaining alveolar bone should be preserved as much as possible to create favorable conditions for subsequent implant surgery. Second, the implant must have good primary stability. For most immediate implant placement surgeries, the amount of available alveolar bone remaining at the ideal implant location is one of the key factors associated with good primary implant stability. Third, the wound must be closed. Conventionally, since implants are inserted immediately after tooth extraction, a temporary restoration or healing abutment is routinely needed to help close the wound. In addition, free connective tissue autografts have also been used in achieving wound closure. Finally, care should be taken to avoid injuring relevant important anatomical structures during immediate implant surgery. Therefore, it is of great significance to understand the relationship between different teeth and surrounding bone tissues and important anatomical structures. To achieve good results in the immediate implantation of mandibular first molars, we analyzed the above points in the current study. Moreover, to provide practical data for the clinic, we carried out a series of measurements based on an ideal restoration-oriented implant direction.
We first analyzed the extraction socket size of mandibular first molars. The measurements of the MD-SS and BL-SS showed that the average values were 8.74 ± 0.76 mm and 8.26 ± 0.72 mm, respectively, which means that the size of the extraction socket is significantly larger than that of conventional implants and healing abutments. When the mandibular first molar is implanted immediately, there will be a gap around the upper part of the implant, which may require filling with bone substitution material.9 However, case reports have shown that osseointegration of an implant placed immediately in the first molar extraction site is possible without having to graft the gap around the implant,15,16 but there is currently a lack of evidence from well-designed clinical RCTs for validation. Moreover, the determination of how to close the wound also needs to be made before surgery. The extraction socket sizes in our study were larger than those of another related study, in which the extraction socket sizes were 8.77 mm (mesial-distal) and 7.76 mm (buccal-lingual), which were slightly smaller than our results in the buccal-lingual direction.10 This may be related to the different measurement methods and populations. In a study of Saudi Arabians, the extraction socket size of mandibular first molars was 9.32 mm × 8.89 mm.17
Minimally invasive tooth extraction can be used to preserve the surrounding tissue as much as possible. However, the thickness of the buccal bone of the mandibular first molars roots was very thin, and the average values of MR-B and DR-B were 1.01 ± 0.40 mm and 1.14 ± 0.50 mm, respectively. In addition, 51.43% of mesial roots and 37.86% of distal roots had buccal plate thicknesses less than 1 mm. Studies have shown that postoperative bone loss can be significantly reduced when the buccal bone plate is intact,18 suggesting that extra attention should be paid to protecting the thin buccal bone wall of the mandibular first molar during tooth extraction. The thickness of the lingual bone wall was significantly larger than that of the buccal bone wall, and the difference was statistically significant in the mesial and distal roots. Protection of the lingual plate is also critical. Therefore, it is necessary to carefully observe the patient’s CBCT before surgery to provide guidance for minimally invasive tooth extraction. Our findings are consistent with those of previous studies.10 To the best of our knowledge, most of the previous studies only observed the thickness of the buccal and lingual bone at the mesial root, while we analyzed both the mesial and distal roots of the mandibular first molar.
Immediate implantation of mandibular first molars mainly relies on the interradicular bone and the bone between the root apex and the mandibular neural canal to obtain the primary stability of the implant. Our results show that the widest bone is at the level of the root apex, namely, the value of IRBA, with an average of 4.44 ± 1.02 mm. However, it is only slightly larger than that of conventional 4-mm-diameter implants, and 35.71% of the mandibular first molars this value is less than 4.0 mm. Of course, the value of IRBA is mainly related to the separation angle of the tooth’s mesial and distal roots. This result suggests that the choice of implant diameter should be carefully evaluated. A meta-analysis indicated that the use of implants smaller than 5 mm in diameter for immediate implant placement in molars resulted in higher survival rates and less bone loss.18 In addition, care should be taken when preparing the implant cavity to prevent bone damage and loss caused by the swing of the bur. In clinical surgery, implant bed preparation before tooth extraction may be a better option.19,20 From the root furcation fornix to the inferior alveolar nerve, the average height was 15.68 mm. Moreover, in a total of 97.86% of the mandibular first molars, this distance was greater than 12.0 mm, which was sufficient for the use of a standard 10-mm-long implant for the patient. We also found that the RF-I for the male was greater than the female, but the average values in two groups were both more than 14 mm.
In our study, the distance from the mesial and distal root apex to the IAN was 7.06 mm and 6.84 mm, respectively, in the ideal restoration-oriented implant direction. Immediate implantation in the anterior region generally requires at least 4 – 5 mm of bone at the apex to provide primary stability. For mandibular first molars, our study shows that the bone volume at the apex of the implant can also meet the requirement that the lower end of the implant be 4 mm in the bone, and there is a safe distance of 2 mm from the mandibular neural canal. Therefore, theoretically, for mandibular first molars that cannot be preserved and are without obvious bone resorption around the root and the periodontal tissue, due to recent longitudinal fracture or severe caries, the bone height is usually sufficient for the immediate implantation. These results are also similar to those of previous studies,10 with the distinction that our results showed that the distal root apex was closer to the mandibular neural canal, which may be due to the difference in the measurement axis. Moreover, our study showed that both the mesial and distal root apices of the female were closer to the IAN than the male. Our study only focused on the vertical distance from mesial/distal root apex to the IAN. When performing the immediate dental implant placement surgery, more attention should also be paid to the alveolar bone mass and density, especially the teeth with asymptomatic apical periodontitis. It has been proven that the immediate placement of implants into the extraction sockets with asymptomatic apical periodontitis did not lead to an increased rate of complications and rendered an equally favorable type of tissue integration.21 However, if the inflammation leads to bone destruction, even if the height of MRA-I and DRA-I are sufficient, the initial stability of the implant may be insufficient, and will lead to failure of treatment.
Our current study also has certain limitations. First, we only included double-rooted mandibular first molars, so the relevant findings may not be applicable to patients with variable roots. Second, this study is focused on the Chinese population, and it is not clear whether there are differences between different ethnic groups. Third, the age distribution of patients is wide, and we cannot deny that patients of different ages may have different bone conditions. Finally, there are also limitations in the design of the research. The current research is designed as a single-center survey, and the source and the number of samples are limited. Although we include 100 patients and 140 teeth, considering individual anatomical variations and different periodontal states and other confounding factors (such as the degree of bifurcation of the root, the degree of bending of the root, and the absorption of alveolar bone) will directly affect the accuracy of results. These shortcomings and limitations need to be further validated and addressed in future studies.
CONCLUSION
According to our current research results, for the immediate implantation of mandibular first molars, there seems to be relatively sufficient bone mass in interradicular bone in height, but an adequate width is lacking for the bone between the mesial and distal root after the extraction of the teeth. The thickness of the mandibular first molar buccal bone is relative thin, especially for the mesial root, and it indicates that more attention may be paid to protect it during extraction to avoid bone defects. There are differences in anatomical features related to alveolar bone around mandibular first molars between males and females. Therefore, before implantation, the patient’s CBCT should be carefully analyzed to ensure the success and safety of immediate dental implant placement in mandibular first molar. However, clinical trial’s better design with larger sample size is required to validate the current findings.
Footnotes
This research was supported by the Military Health Care Project (22BJZ22) and Beijing Natural Science Foundation (L222109).
References
- 1.Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs) Clin Oral Implants Res. 2007;18(Suppl 3):97–113. doi: 10.1111/j.1600-0501.2007.01439.x. [DOI] [PubMed] [Google Scholar]
- 2.Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017;73:84–102. doi: 10.1111/prd.12170. [DOI] [PubMed] [Google Scholar]
- 3.Blanco J, Carral C, Argibay O, Liñares A. Implant placement in fresh extraction sockets. Periodontol 2000. 2019;79:151–167. doi: 10.1111/prd.12253. [DOI] [PubMed] [Google Scholar]
- 4.Baik UB, Jung JY, Jung HJ, Kim YJ, Chae HS, Park KS, Vaid NR, Nanda R. Alveolar bone changes after molar protraction in young adults with missing mandibular second premolars or first molars. Angle Orthod. 2022;92:64–72. doi: 10.2319/022321-147.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saber AM, Altoukhi DH, Horaib MF, El-Housseiny AA, Alamoudi NM, Sabbagh HJ. Consequences of early extraction of compromised first permanent molar: a systematic review. BMC Oral Health. 2018;18:59. doi: 10.1186/s12903-018-0516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ADA Division of Communications; Journal of the American Dental Association; ADA Council on Scientific Affairs. For the dental patient. Tooth eruption: the permanent teeth. J Am Dent Assoc. 2006;137:127. doi: 10.14219/jada.archive.2006.0031. [DOI] [PubMed] [Google Scholar]
- 7.Chrcanovic BR, de Carvalho Machado V, Gjelvold B. Immediate implant placement in the posterior mandible: a cone beam computed tomography study. Quintessence Int. 2016;47:505–514. doi: 10.3290/j.qi.a36008. [DOI] [PubMed] [Google Scholar]
- 8.Haj Yahya B, Chaushu G, Hamzani Y. Computed tomography for the assessment of the potential risk after implant placement in fresh extraction sites in the posterior mandible. J Oral Implantol. 2021;47:2–8. doi: 10.1563/aaid-joi-D-18-00227. [DOI] [PubMed] [Google Scholar]
- 9.Sayed AJ, Shaikh SS, Shaikh SY, Hussain MA, Tareen SUK, Awinashe V. Influence of inter-radicular septal bone quantity in primary stability of immediate molar implants with different length and diameter placed in mandibular region. a cone-beam computed tomography-based simulated implant study. J Pharm Bioallied Sci. 2021;13(Suppl 1):S484–S491. doi: 10.4103/jpbs.JPBS_818_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Padhye NM, Shirsekar VU, Bhatavadekar NB. Three-dimensional alveolar bone assessment of mandibular first molars with implications for immediate implant placement. Int J Periodontics Restorative Dent. 2020;40:e163–e167. doi: 10.11607/prd.4614. [DOI] [PubMed] [Google Scholar]
- 11.Garcia-Sanchez R, Dopico J, Kalemaj Z, Buti J, Pardo Zamora G, Mardas N. Comparison of clinical outcomes of immediate versus delayed placement of dental implants: a systematic review and meta-analysis. Clin Oral Implants Res. 2022;33:231–277. doi: 10.1111/clr.13892. [DOI] [PubMed] [Google Scholar]
- 12.Donos N, Asche NV, Akbar AN, Francisco H, Gonzales O, Gotfredsen K, Haas R, Happe A, Leow N, Navarro JM, Ornekol T, Payer M, Renouard F, Schliephake H. Impact of timing of dental implant placement and loading: Summary and consensus statements of group 1-The 6th EAO Consensus Conference 2021. Clin Oral Implants Res. 2021;32(Suppl 21):85–92. doi: 10.1111/clr.13809. [DOI] [PubMed] [Google Scholar]
- 13.Becker W. Immediate implant placement: diagnosis, treatment planning and treatment steps/or successful outcomes. J Calif Dent Assoc. 2005;33:303–310. [PubMed] [Google Scholar]
- 14.Lee W. Immediate implant placement in fresh extraction sockets. J Korean Assoc Oral Maxillofac Surg. 2021;47:57–61. doi: 10.5125/jkaoms.2021.47.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saltzburg N, Kang P. Observed healing of an immediately placed implant in a molar site without bone replacement graft or primary closure. Compend Contin Educ Dent. 2020;41:326–330. [PubMed] [Google Scholar]
- 16.Gober DD, Fien MJ. Flapless extraction socket healing around an immediate implant placed into a mandibular molar site without the use of regenerative materials: a case report. Int J Periodontics Restorative Dent. 2016;36:e26–e32. doi: 10.11607/prd.2516. [DOI] [PubMed] [Google Scholar]
- 17.Sayed AJ, Shaikh SS, Shaikh SY, Hussain MA. Inter radicular bone dimensions in primary stability of immediate molar implants - a cone beam computed tomography retrospective analysis. Saudi Dent J. 2021;33:1091–1097. doi: 10.1016/j.sdentj.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ragucci GM, Elnayef B, Criado-Cámara E, Del Amo FS, Hernández-Alfaro F. Immediate implant placement in molar extraction sockets: a systematic review and meta-analysis. Int J Implant Dent. 2020;6:40. doi: 10.1186/s40729-020-00235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rebele SF, Zuhr O, Hürzeler MB. Pre-extractive interradicular implant bed preparation: case presentations of a novel approach to immediate implant placement at multirooted molar sites. Int J Periodontics Restorative Dent. 2013;33:89–96. doi: 10.11607/prd.1444. [DOI] [PubMed] [Google Scholar]
- 20.Scarano A. Traditional postextractive implant site preparation compared with pre-extractive interradicular implant bed preparation in the mandibular molar region, using an ultrasonic device: a randomized pilot study. Int J Oral Maxillofac Implants. 2017;32:655–660. doi: 10.11607/jomi.5342. [DOI] [PubMed] [Google Scholar]
- 21.Crespi R, Capparé P, Crespi G, Lo Giudice G, Gastaldi G, Gherlone E. Immediate implant placement in sockets with asymptomatic apical periodontitis. Clin Implant Dent Relat Res. 2017;19:20–27. doi: 10.1111/cid.12422. [DOI] [PubMed] [Google Scholar]