Abstract
Background
Ultraportable automated external defibrillators (AEDs) are a new generation of defibrillators that are small, lightweight, easy to carry on one’s person, and affordable for personal and home use. They offer the opportunity to increase AED availability in case of out-of-hospital cardiac arrest (OHCA) and therefore improve outcomes.
We aimed to review evidence supporting the potential effect on outcomes and the performance of these ultraportable AEDs.
Methods
We searched Ovid Medline, Embase and Cochrane databases from 2012 to July 4th, 2024 to identify any studies related to ultraportable AED. The population was adult and children with OHCA who were treated with an ultra-portable AED. All outcomes were accepted. We limited study designs to randomized controlled trials and non-randomized studies. Data charting was done by the primary author using standardized data abstraction forms.
Results
The search strategy identified 54 studies (Pubmed = 26, Embase = 28, with 19 duplicates). We included three articles in the final review. One study was a medico-economic simulation study including 600,000 simulated patients, one is the study protocol of cluster randomized trial of providing ultraportable AEDs to first responders and one is an abstract with preliminary results of this trial reporting 1805 community responders recruited, 903 allocated to ultraportable AED. No studies to date have reported patient outcomes.
Conclusion
This review found no evidence of ultraportable AED device performance, clinical or safety outcomes. There is an urgent need for further research to determine the safety and effectiveness of ultraportable AEDs.
Keywords: Cardiopulmonary resuscitation, Heart arrest, AED
Introduction
Early defibrillation is associated with a large increase in survival from out-of-hospital cardiac arrest (OHCA).1, 2, 3, 4 If defibrillation occurs within 3 to 5 min of collapse, survival rates as high as 50–70% have been reported.3, 4 Emergency medical services (EMS) response time rarely allows defibrillation to occur in such a short time.5 To date, public access defibrillation (PAD) programs are ineffective on their own, with low rates of OHCA patients receiving defibrillation by bystanders.6 A paradigm shift in automatic external defibrillator (AED) deployment is needed to improve outcomes.7, 8
Current strategies to decrease time to defibrillation in OHCA include using drones to delivery the AEDs and use of community volunteer responders dispatched by mobile apps to perform early bystander CPR and defibrillation.9, 10, 11 Recently, several companies have started advertising “ultraportable” AEDs for personal use by lay people or equipping community volunteer responders. They advocate that, compared to standard AEDs, these devices offer a lower cost and weight, allowing for easier portability and availability in homes, where most OHCAs occur. However, these devices may be limited to a certain number of shocks and lower energy outputs (e.g., restricted to up to 20 shocks and a maximum of 85 J).
We aimed to review evidence supporting the potential effect on patient outcomes and the performance of ultraportable AEDs.
Methods
Arksey and O’Malley’s methodological steps for scoping reviews, with the refinements proposed by Levac were followed to develop the protocol and conduct this review.12, 13
The international database of prospectively registered systematic reviews in health and social care (PROSPERO), Medline, google scholar, and open science framework were checked to confirm that no systematic, scoping, or narrative reviews on a similar topic have been published.
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR)14 (Supplement A). The review process followed the written protocol (Supplement B) and applied data screening steps and a standard data abstraction form available on Covidence.15 Our scoping review comprised of the following steps:
Identifying the research question
The research question was: In adults and children who are in cardiac arrest outside of a hospital does the use of an ultra-portable AED improve patient outcomes?
Identifying relevant studies
The search strategy was developed with assistance from an information specialist from University of Toronto. Key search terms and the search strategy are provided in Supplement C.
After review from the ILCOR BLS Task Force, the search strategy was run on July 4th, 2024. Articles for review were obtained through Ovid MEDLINE(R), EMBASE and Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials from 2012 to July 4th, 2024. We did not search grey literature. Since ultraportable AED are relatively new devices we limited the search to start from 2012.
Study selection
Table 1 explains the eligibility criteria for selecting appropriate articles for this review. The population was adults and children with OHCA who were treated with an ultra-portable AED. All outcomes were accepted. We limited study designs to randomized controlled trials (RCTs) and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies, conference abstracts and trial protocols).
Table 1.
Summary of defined inclusion criteria for selecting articles.
| Population | In adults and children in out-of-hospital cardiac arrest |
| Intervention | the use of an ultra-portable / pocket AED |
| Comparison | |
| Outcomes | all outcomes were accepted |
| Study Design | Randomized controlled trials (RCTs) and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies) are eligible for inclusion. Non-peer reviewed studies, unpublished studies, conference abstracts and trial protocols are eligible for inclusion. Studies which describe the use of mobile AEDs associated with drone technology are excluded. |
| Timeframe | January 2012 − July 2024 |
All citations were uploaded into the Covidence website for screening and duplicates were removed. Included manuscripts described any studies related with ultraportable AED. Manuscripts that did not describe the use or the development of ultraportable AED and articles which described AEDs deliver by drones were excluded. We also excluded manuscripts that were not available in English.
First, two authors (GD, TN) reviewed all titles and abstracts against inclusion and exclusion criteria. For initial screening, limited exclusion criteria were employed to have broader inclusion. After initial screening, all potential eligible full texts were retrieved and further reviewed by two authors (GD, TN) against the same eligibility criteria. Additional citations were searched through hand search of the reference list of included studies following the initial review. Whenever there was uncertainty about a potentially eligible study, the final decisions were achieved by discussion and consensus.
Data extraction and charting the data
The primary author extracted the data using standardized data abstraction forms and guided by JBI (Joanna Briggs Institute) methodology.16 The following information was extracted for each included study: year and origin of publication, study design, population and number of included patients, intervention, comparator, outcome, if reported.
Collating, summarizing and reporting the results
An overview of all material reviewed was performed. The authors reviewed the outputs and developed a narrative summary describing the main results, qualities and limits of the evidence identified.
Results
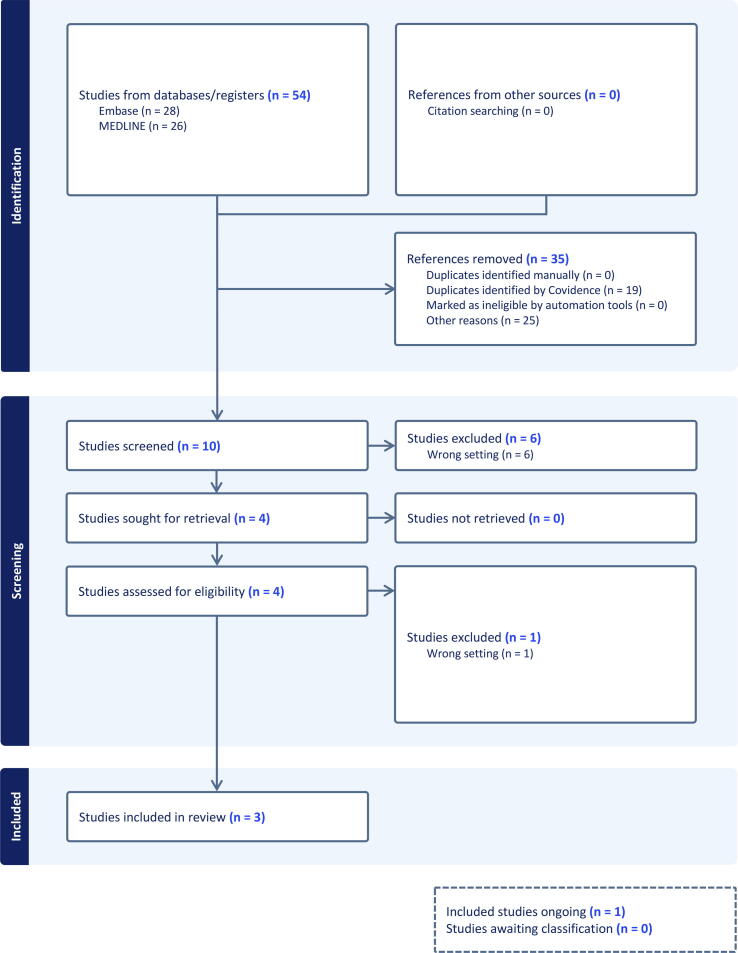
The search strategy identified 54 studies to screen (Pubmed = 26, Embase = 28, with 19 duplicates). We identified 4 articles for full-text review (Fig. 1). One was excluded due to wrong setting (standard AED).17 We included three articles in the final review.18, 19, 20 One study was a medico-economic simulation study, one is the study protocol of cluster randomized trial and one is an abstract with preliminary results of this trial (Table 2.). No papers reported on the potential effect on patient outcomes or the performance of ultra-portable AEDs.
Fig. 1.
PRISMA flowchart. EBM: Evidence-based medicine. Embase: Excerpta Medica Database.
Table 2.
Summary of results.
| Study Details | Study Design | Population | Intervention | Comparator(s) | Outcome measure |
|---|---|---|---|---|---|
| Shaker, 2022; 9 | Economic analysis | 600,000 simulated patients at low, moderate, and high-riskfor SCA | SMall AED for Rapid Treatment of SCA (SMART) strategy | No SMART strategy | At a 1.6% SCA annual risk, SMART strategy was associated with $95,251/QALY (societal perspective) and $100,797/QALY (healthcare perspective). At a 3.5% SCA annual risk, SMART strategy was associated with $53,925/QALY (societal perspective) and and $59,672/QALY (healthcare perspective). SMART prevented 1,762 fatalities across risk strata (1.59% fatality relative risk reduction across groups). |
| Todd, 2023; 16 | Cluster-randomised controlled trial − Study protocol | Sample size calculation of 714 (357 per arm) | Community responder dispatched with GoodSAM app equipped with an ultraportable AED | Community responder not equipped with AED | Primary outcome will be survival to 30 days.Aim to detect a 7% increase in survival (9% to 16%) |
| Todd, 2023; 19 | Cluster randomized intervention −preliminary trial results (abstract) | 1805 community responders recruited, 903 allocated to CellAED | Community responder dispatched with GoodSAM app equipped with an ultraportable defibrillator (CellAED) n = 903 | Community responder not equipped with AED | Unfinished study. 1,788 alerts to CellAED participants, 104 arriving before EMS. |
AED: Automated External Defibrillator, QALY: Quality Adjusted Life Year, SCA: Sudden Cardiac Death.
Health-economic simulation study (n = 1)
A health-economic analysis modeled the impact of a SMall AED for Rapid Treatment of a Sudden Cardiac Arrest (SMART) strategy on a simulated patient database (n = 600,000) at low, moderate, and high-risk for OHCA.20 Their results suggest that a SMART approach to prevent fatalities related to OHCA is cost-effective in patients with elevated sudden cardiac arrest risk (annual cardiac arrest risk > 1.5%). They described a smartphone-enabled pocket AED, but as a simulation study, they estimated the performance of the device from conventional AED studies, which limited the applicability of the results to ultraportable AEDs.
Real world studies with use of ultraportable AED (n = 2)
In two papers, Todd et al. presented the study protocol and preliminary results of the First Responder Shock (FIRST) cluster randomized trial.18, 19 FIRST aims to examine if providing frequently responding volunteer community responders with an ultraportable AED can increase OHCA survival at 30-days.18, 19 In their abstract 1,788 alerts have been sent to CellAED participants, with 104 responders arriving before EMS. No data on the performance of the device or patient outcomes were reported.
Discussion
Ultraportable AEDs are a new generation of defibrillators that offer an opportunity to enhance public access defibrillation and community volunteer responder programs, increase home AED availability with potential to improve patient outcomes. However, in this review we found no evidence of device efficacy or real-world evidence of their use or impact.
The use of AEDs by trained lay responders in community-based PAD programs has been shown to increase survival after sudden cardiac arrest. When sudden cardiac arrest is witnessed and an AED is immediately available impressive survival with favorable neurologic outcome results have been reported.3, 4, 21 Programs to develop layperson-enacted CPR-response plan by adding AEDs and AED training can increase the number of survivors of OHCA in public locations.22 Unfortunately, the large majority of cardiac arrest occur at home, and to date access to home AED has not been shown to be associated with improved outcomes.23
Bystander CPR before EMS arrival has increased in industrialized countries and can be observed up to 70% of OHCA. Despite these improvements, community defibrillation rates usually remain low (less than 10%).24 In a systematic review and meta-analysis, Squizzato et al. observed that dispatching citizen first responders using mobile phone technologies is associated with an increase of AED use.25 The strategy assessed in the FIRST trial to improve volunteer community’ability to provide early defibrillation is novel.18 Volunteer community responders alerted using mobile apps could, in addition to providing early CPR, be the carriers of small, affordable AED and decrease time to first shock. A recent RCT and observational research shows AED use does not improve when responders are sent to retrieve an AED on the way to the scene.26 Further research is required to explore if the widespread deployment of ultraportable AED to volunteer community responders will increase AED use before EMS arrival on scene and translate to improved patient outcomes.
This review highlights the lack of available data on the effectiveness and safety of such devices. Device registration with regulatory authorities alone does not provide evidence of device performance in real-world settings. As the success of defibrillation is related to several factors including shock energy, transthoracic impedance, defibrillator pad size and anatomical location, diagnostic accuracy for shockable rhythms and the duration the person has been in cardiac arrest. Clinical research is required to demonstrate the clinical efficacy of ultraportable AEDs.
Limitations
This scoping review has some limitations that should be considered when interpreting the findings. This review focused on peer-reviewed studies and excluded gray literature which may have restricted the number of included studies. We limited our review to include only publications which had an English language abstract available. As such, it is possible that we missed studies published in other languages and not translated.
Conclusion
This review found no evidence of ultraportable AED device performance, clinical or safety outcomes. There is an urgent need for further research to determine the safety and effectiveness of ultraportable AEDs.
Disclosure statement
The authors declared no conflict of interest related to this work. GDP is an Editor and JEB an Editorial Board Member of Resuscitation. GDP is Editor-in-Chief, JEB an Editor and KD and TO are Editorial Board Members of Resuscitation Plus.
Funding details
This Scoping review was funded by the American Heart Association, on behalf of The International Liaison Committee on Resuscitation (ILCOR). None of the authors received payment from this funding source to complete this scoping review. JB receives a Fellowship by the National Heart Foundation of Australia.
CRediT authorship contribution statement
G. Debaty: Writing – original draft, Visualization, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. GD. Perkins: Writing – review & editing, Visualization, Validation, Methodology, Investigation, Data curation, Conceptualization. K.N. Dainty: Writing – review & editing, Methodology, Investigation, Conceptualization. T. Norii: Writing – review & editing, Visualization, Investigation, Data curation, Conceptualization. T.M. Olasveengen: Writing – review & editing, Visualization, Validation, Supervision, Methodology, Conceptualization. J.E. Bray: Writing – review & editing, Validation, Supervision, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Acknowledgments
The authors would like to sincerely thank Julie Waddick, Health Science Librarian at North York General Hospital, Toronto, Canada, for her help with developing the search strategy.
The authors acknowledge the contributions of the non-author ILCOR BLS Task Force Members: Julie Considine, Sung Phil Chung, Vihara Dassanayak, Maya Dewan, Bridget Dicker, Fredrik Folke, Carolina Malta Hansen, Takanari Ikeyama, Nicholas J. Johnson, Siobhán Masterson, Chika Nishiyama, Ziad Nehme, Giuseppe Ristagno, George Lucas, Peter Morley, Tetsuya Sakamoto, Christopher M. Smith, Michael Smyth, Christian Vaillancourt.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100739.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Nakashima T., Noguchi T., Tahara Y., et al. Public-access defibrillation and neurological outcomes in patients with out-of-hospital cardiac arrest in Japan: a population-based cohort study. Lancet. 2019;394:2255–2262. doi: 10.1016/S0140-6736(19)32488-2. [DOI] [PubMed] [Google Scholar]
- 2.Kitamura T., Kiyohara K., Iwami T. Public-access defibrillation in Japan. N Engl J Med. 2017;376:e12. doi: 10.1056/NEJMc1700160. [DOI] [PubMed] [Google Scholar]
- 3.Caffrey S.L., Willoughby P.J., Pepe P.E., Becker L.B. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–1247. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 4.Valenzuela T.D., Roe D.J., Nichol G., Clark L.L., Spaite D.W., Hardman R.G. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 5.Gold L.S., Fahrenbruch C.E., Rea T.D., Eisenberg M.S. The relationship between time to arrival of emergency medical services (EMS) and survival from out-of-hospital ventricular fibrillation cardiac arrest. Resuscitation. 2010;81:622–625. doi: 10.1016/j.resuscitation.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Nishiyama C., Kiguchi T., Okubo M., et al. Three-year trends in out-of-hospital cardiac arrest across the world: Second report from the international liaison committee on resuscitation (ILCOR) Resuscitation. 2023;186 doi: 10.1016/j.resuscitation.2023.109757. [DOI] [PubMed] [Google Scholar]
- 7.Brent C.M., Cheskes S., Castrén M., Brooks S.C. Wolf creek XVII part 5: mobile AEDs. ResuscitationPlus. 2023;16 doi: 10.1016/j.resplu.2023.100500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brooks S.C., Clegg G.R., Bray J., et al. Optimizing outcomes after out-of-hospital cardiac arrest with innovative approaches to public-access defibrillation: A scientific statement from the international liaison committee on resuscitation. Resuscitation. 2022;172:204–228. doi: 10.1016/j.resuscitation.2021.11.032. [DOI] [PubMed] [Google Scholar]
- 9.Schierbeck S., Hollenberg J., Nord A., et al. Automated external defibrillators delivered by drones to patients with suspected out-of-hospital cardiac arrest. Eur Heart J. 2022;43:1478–1487. doi: 10.1093/eurheartj/ehab498. [DOI] [PubMed] [Google Scholar]
- 10.Pollack R.A., Brown S.P., Rea T., et al. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation. 2018;137:2104–2113. doi: 10.1161/CIRCULATIONAHA.117.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ringh M., Rosenqvist M., Hollenberg J., et al. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 12.Levac D., Colquhoun H., O'Brien K.K. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 14.Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 15.Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org.
- 16.Shaeri S., Considine J., Dainty K.N., Olasveengen T.M., Morrison L.J. Accuracy of etiological classification of out-of-hospital cardiac arrest: A scoping review. Resuscitation. 2024;198 doi: 10.1016/j.resuscitation.2024.110199. [DOI] [PubMed] [Google Scholar]
- 17.Shen C.P., Freed B.C., Walter D.P., et al. Convolution neural network algorithm for shockable arrhythmia classification within a digitally connected automated external defibrillator. J Am Heart Assoc. 2023;12 doi: 10.1161/JAHA.122.026974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Todd V., Dicker B., Okyere D., et al. A study protocol for a cluster-randomised controlled trial of smartphone-activated first responders with ultraportable defibrillators in out-of-hospital cardiac arrest: The First Responder Shock Trial (FIRST) Resusc Plus. 2023;16 doi: 10.1016/j.resplu.2023.100466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Todd V, Dicker B, Okyere D, et al. The First Responder Shock Trial (FIRST): Can we improve cardiac arrest survival by providing community responders with ultraportable automated external defibrillators? Heart, Lung and Circulation. 2023; 32.
- 20.Shaker M.S., Abrams E.M., Oppenheimer J., et al. Estimation of health and economic benefits of a small automatic external defibrillator for rapid treatment of sudden cardiac arrest (SMART): A cost-effectiveness analysis. Front Cardiovasc Med. 2022;9 doi: 10.3389/fcvm.2022.771679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page R.L., Joglar J.A., Kowal R.C., et al. Use of automated external defibrillators by a U.S Airline. New England Journal of Medicine. 2000;343:1210–1216. doi: 10.1056/NEJM200010263431702. [DOI] [PubMed] [Google Scholar]
- 22.Hallstrom A.P., Ornato J.P., Weisfeldt M., et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 23.Bardy G.H., Lee K.L., Mark D.B., et al. Home use of automated external defibrillators for sudden cardiac arrest. N Engl J Med. 2008;358:1793–1804. doi: 10.1056/NEJMoa0801651. [DOI] [PubMed] [Google Scholar]
- 24.Marijon E., Narayanan K., Smith K., et al. The Lancet Commission to reduce the global burden of sudden cardiac death: a call for multidisciplinary action. Lancet. 2023;402:883–936. doi: 10.1016/S0140-6736(23)00875-9. [DOI] [PubMed] [Google Scholar]
- 25.Scquizzato T., Belloni O., Semeraro F., et al. Dispatching citizens as first responders to out-of-hospital cardiac arrests: a systematic review and meta-analysis. Eur J Emerg Med. 2022;29:163–172. doi: 10.1097/MEJ.0000000000000915. [DOI] [PubMed] [Google Scholar]
- 26.Morin F., Douillet D., Lamhaut L., Fadel M., Savary D. Deployment of “super lay-rescuers” equipped with AED to improve OHCA survival: An innovative partnership between emergency medical service, city hall and a mobile application in France. Resuscitation. 2022;176:51–52. doi: 10.1016/j.resuscitation.2022.05.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.