Abstract
Introduction
Chronic obstructive pulmonary disease (COPD) is a global health concern and a leading cause of morbidity and mortality worldwide. COPD action plans help patients manage exacerbations by recognizing symptoms early and taking necessary steps. We found our COPD written action plan difficult to understand, potentially affecting the patient’s ability to self-manage their COPD.
Aims
We aim to design a new COPD action plan to increase the knowledge scores of our patients during competency checks by 20%.
Methods
We employed the quality improvement methodology of needs analysis and root cause analysis and used a Pareto chart to identify the top four contributory factors to an ineffective COPD action plan. These include being too wordy, lacking pictorial illustrations, being only available in a single language (English), and too much medical jargon. Using the prioritization matrix to assess possible solutions, the team decided to implement a pictorial COPD action plan. After two cycles of Plan-Do-Study-Act, the final pictorial COPD plan was compared with the original written action plan.
Results
Ten English-speaking COPD patients from our outpatient respiratory clinics were surveyed with the original action plan while 11 more were surveyed after the introduction of the pictorial action plan. There was an improvement in mean knowledge scores by 92.8% (t(19) = 6.67, p < 0.01, at 95% CI). Patient satisfaction rates also increased from 44% to 100%. Sixty-three percent (63.6%) of patients surveyed said they referred back to the pictorial action plan 3 months after being introduced to it.
Conclusion
Pictorially enhanced COPD action plans have been shown to improve our patients’ knowledge of COPD self-management.
Keywords: copd self management, pictorial action plan, copd action plan, written action plan, copd (chronic obstructive pulmonary disease)
Introduction
Chronic obstructive pulmonary disease (COPD) is a global health concern and a leading cause of morbidity and mortality worldwide. COPD imparts a significant economic burden, including both direct costs of healthcare resource utilization and indirect costs of lost work productivity [1,2]. It is the tenth leading cause of death in Singapore [3].
COPD action plans help patients manage exacerbations through early recognition of symptoms and taking necessary steps, such as administering antibiotics and oral corticosteroids [4]. These plans have been proven effective in Cochrane reviews [5].
Materials and methods
COPD action plan
In the 2022 Cochrane review of self-management interventions in patients with COPD, the COPD action plan was mentioned to be associated with improvements in health-related quality of life, as well as reductions in respiratory-associated admissions and emergency department (ED) admissions [6].
These self-management interventions frequently rely on the patient's capability to recognize an exacerbation and initiate the action plan. As a result, the success of any action plan-based strategy would be primarily reliant on the patient’s comprehension and ability to become an effective self-manager.
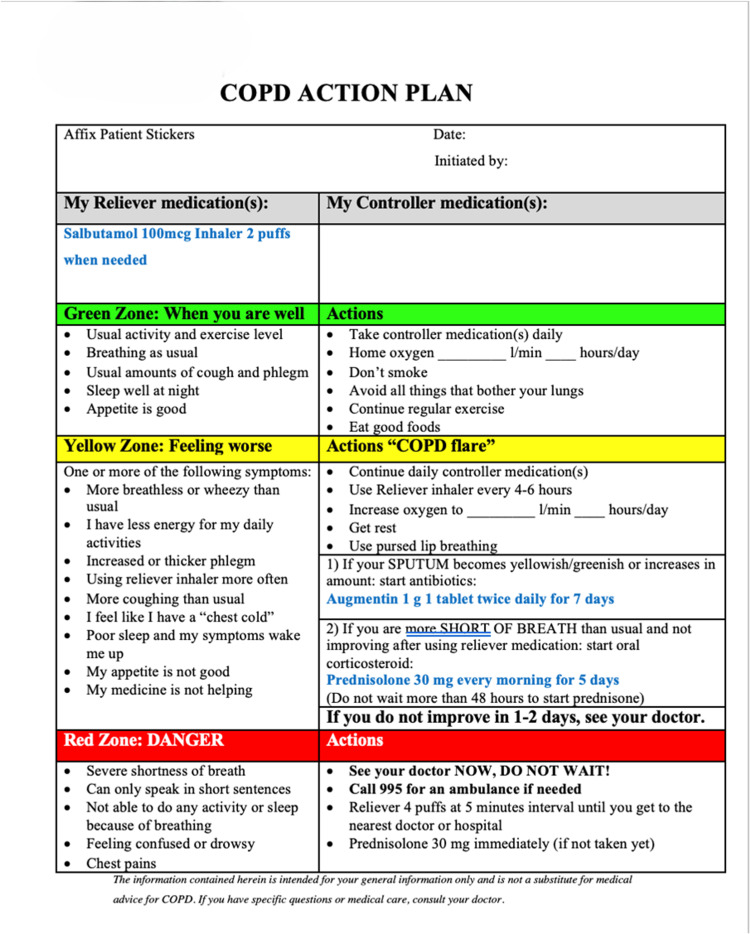
Our hospital has an established COPD action plan (Figure 1), which is adapted from both the American Lung Association [7] and the Canadian Thoracic Society [8]. These action plans are given out to our COPD patients by doctors and respiratory specialist nurses. We have received feedback from quite several patients and their caregivers that our current COPD action is difficult to understand. This could negatively impact our patient’s ability to manage exacerbations effectively, leading to poor clinical outcomes. Therefore, we decided to enhance our action plan to ensure that it is easy to comprehend [9].
Figure 1. Sengkang General Hospital’s original COPD action plan.
Adapted from the American Lung Association and the Canadian Thoracic Society [7,8]
COPD: chronic obstructive pulmonary disease
Context
This quality improvement (QI) initiative was carried out at the Sengkang General Hospital Respiratory Medicine Department to improve our COPD action plan. A multidisciplinary QI team was established to investigate and carry out a QI project using the Institute for Healthcare Improvement's (IHI) Plan-Do-Study-Act (PDSA) framework. The framework involves a four-stage cyclic process for implementing and refining improvements. The team consisted of specialist nurses, pharmacists, senior residents, and consultants from the respiratory medicine department.
Needs analysis
To gain a better understanding of the attitudes and opinions of doctors, nurses, pharmacists, patients, and their caregivers regarding the current action plan, we conducted a needs analysis. This involved distributing questionnaires (Table 1) to all the relevant stakeholders. They consist of four questions meant to assess whether the respondents feel that the COPD action plan is important, if the current action plan is difficult to understand, if there is a need to improve it, and lastly, some of the factors that have contributed to an ineffective COPD action plan.
Table 1. Sample of a Needs Analysis questionnaire.
COPD: chronic obstructive pulmonary disease
| Strongly disagree | Disagree | Agree | Strongly Agree | ||
| 1. | The COPD action plan is important to help improve self-management knowledge among our patients | ||||
| 2. | The current COPD action plan is difficult to understand | ||||
| 3. | There is a need to improve our current COPD action plan | ||||
| 4. | What are some of the contributory factors to an ineffective COPD action plan? | | |||
We collected a total of 40 responses (Table 2) from 9 patients and their caregivers, 14 doctors, 5 nurses, and 12 pharmacists. Our needs analysis showed that most of the respondents strongly agree (n=25, 62.5%) that the COPD action plan is important to help improve the self-management knowledge of patients. Sixty-two point five percent (62.5%) of responses agree or strongly agree that there is a need to improve it.
Table 2. Responses from the Needs Analysis questionnaire.
COPD: chronic obstructive pulmonary disease
| Overall Response (n=40) | |||||||
| Strongly Disagree n (%) | Disagree n (%) | Agree n (%) | Strongly Agree n (%) | ||||
| 1 | The COPD action plan is important to help improve self-management knowledge among our patients | 1 (2.5) | 0 (0) | 14 (35) | 25 (62.5) | ||
| 2 | The current COPD action plan is difficult to understand | 1 (2.5) | 21 (52.5) | 14 (35) | 4 (10) | ||
| 3 | There is a need to improve our current COPD action plan | 2 (5) | 13 (32.5) | 19 (47.5) | 6 (15) | ||
| Response from pharmacists, nurses, and doctors (n=31) | |||||||
| Strongly Disagree n (%) | Disagree n (%) | Agree n (%) | Strongly Agree n (%) | ||||
| 1 | The COPD action plan is important to help improve self-management knowledge among our patients | 1 (3.2) | 0 (0) | 13 (41.9) | 17 (54.8) | ||
| 2 | The current COPD action plan is difficult to understand | 1 (3.2) | 19 (61.3) | 9 (29.0) | 2 (6.5) | ||
| 3 | There is a need to improve our current COPD action plan | 2 (6.5) | 11 (35.5) | 15 (48.4) | 3 (9.7) | ||
| Response from patients (n=9) | |||||||
| Strongly Disagree n (%) | Disagree n (%) | Agree n (%) | Strongly Agree n (%) | ||||
| 1 | The COPD action plan is important to help improve self-management knowledge among our patients | 0 (0) | 0 (0) | 1 (11.1) | 8 (88.9) | ||
| 2 | The current COPD action plan is difficult to understand | 0 (0) | 2 (22.2) | 5 (55.6) | 2 (22.2) | ||
| 3 | There is a need to improve our current COPD action plan | 0 (0) | 2 (22.2) | 4 (44.4) | 3 (33.3) | ||
It is interesting to note that 52.5% of our respondents do not find our current action plan difficult to understand. However, when the data is analyzed according to the various subgroups, there is a difference of opinions between our patients and healthcare staff. The majority of the patients (n=7, 77.8%) agree or strongly agree that the action plan is difficult to understand while only a small proportion (n=11, 35.5%) of our healthcare professionals (doctors, nurses, pharmacists) felt the same way.
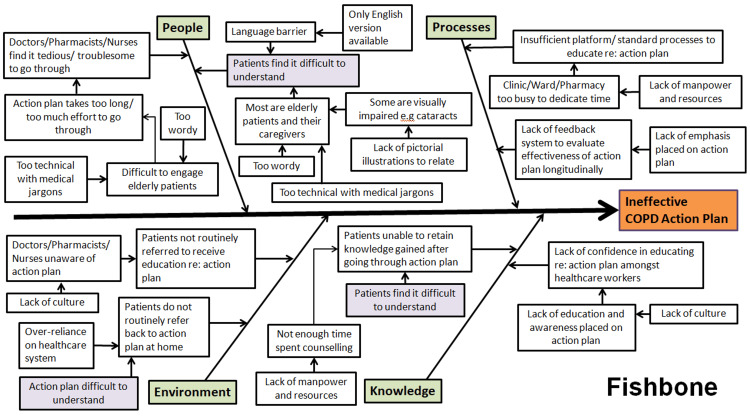
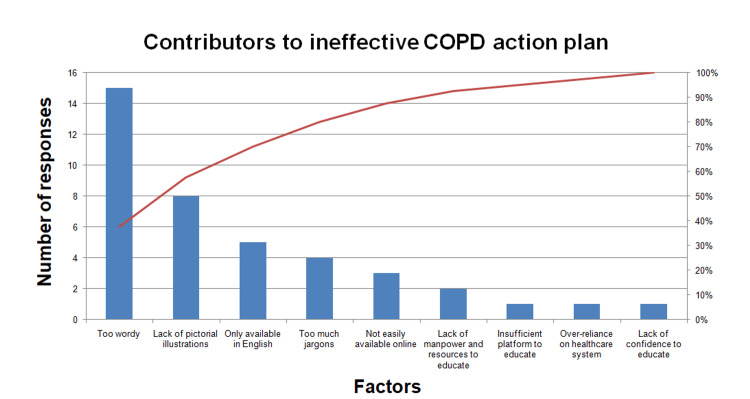
Assessment of problems
A root cause analysis was first performed by the QI team to identify factors that contributed to an ineffective COPD action plan. A Fishbone diagram was constructed to list the People, Environment, Processes, and Knowledge factors (Figure 2). Next, the team ran a Pareto chart (Figure 3) using responses from our stakeholders to identify the most important contributory factors to an ineffective COPD action plan. The Pareto chart is based on the Pareto principle, which states that about 80% of the outcome comes from 20% of its inputs. Hence, taking 80% of the responses we obtained from the Needs Questionnaire as a cut-off, we managed to identify the top four contributory factors. These include being too wordy, lack of pictorial illustrations, availability only in a single language (English), and too much medical jargon.
Figure 2. Fishbone cause-and-effect analysis.
Image credit: The authors
COPD: chronic obstructive pulmonary disease
Figure 3. Pareto chart.
Image credit: The authors
After identifying the top four contributory factors, the QI team came together to brainstorm various intervention options. These ideas were placed in a Prioritization Matrix (Table 3) and assessed based on their reliability, effectiveness, feasibility, affordability, and sustainability. Ultimately, the option of having a pictorially augmented COPD action plan obtained the highest score in our assessment and therefore, was chosen to be our primary intervention for the project.
Table 3. Prioritization matrix.
| Weight of each attribute (1 ~ 9) | 6 | 7 | 8 | 3 | 6 | 30 | ||
| 12% | 23% | 27% | 23% | 20% | 100% | 100% | ||
| Type of option (Project’s potential changes) | Reliability | Effective | Feasible | Low cost | Sustainable | Score | Score mark | |
| Options | Pictorial action plan | 8 | 8 | 9 | 5 | 9 | 8 | |||||||| |
| Increase clinic consult time to educate the action plan | 3 | 7 | 1 | 1 | 2 | 3 | || | |
| Create QR code/digitalize action plan | 5 | 5 | 8 | 3 | 5 | 6 | ||||| | |
| Translate to different languages | 8 | 8 | 9 | 5 | 8 | 8 | ||||||| | |
| Interactive video action plan | 5 | 5 | 6 | 3 | 4 | 5 | |||| |
QI objective
A pictorially augmented COPD action plan was chosen to better engage our COPD patients. By designing and developing a new action plan, we aim to increase the knowledge scores of our patients during competency checks by 20% over a 10-month period.
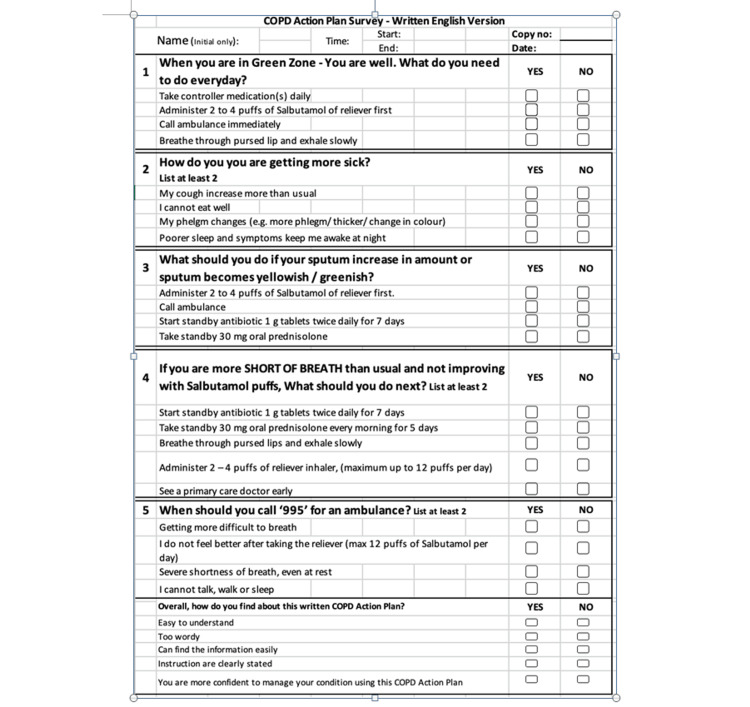
Data collection and analysis
Data collection was conducted at two different time frames, first using the existing COPD action plan, followed by using the newly developed COPD action plan. Both action plans were issued to our patients by the respiratory specialist nurse during outpatient clinic follow-ups. After going through the contents of the action plan, patients would undertake a five-question competency check (Figure 4) to assess their understanding of COPD self-management via structured questioning. We allocated 2 points for each question. Patients got 1 point if they managed to list one correct answer, and 2 points if they managed to list at least two correct answers and above. Knowledge scores were then derived after tabulating the total number of points obtained. At the end of the survey, patients were also asked about how satisfied they were with the action plan.
Figure 4. COPD action plan competency checklist.
Adapted from: [15]
COPD: chronic obstructive pulmonary disease
Three months after administration of the pictorial COPD action plan, our patients received a phone call from our QI team to check back on the utilization rates of the action plan.
The above data were de-identified and securely stored in a password-encrypted Microsoft Excel-based database (Microsoft Corporation, Redmond, WA, US). It was subsequently shared with the QI team for data analysis.
Plan-Do-Study-Act (PDSA)
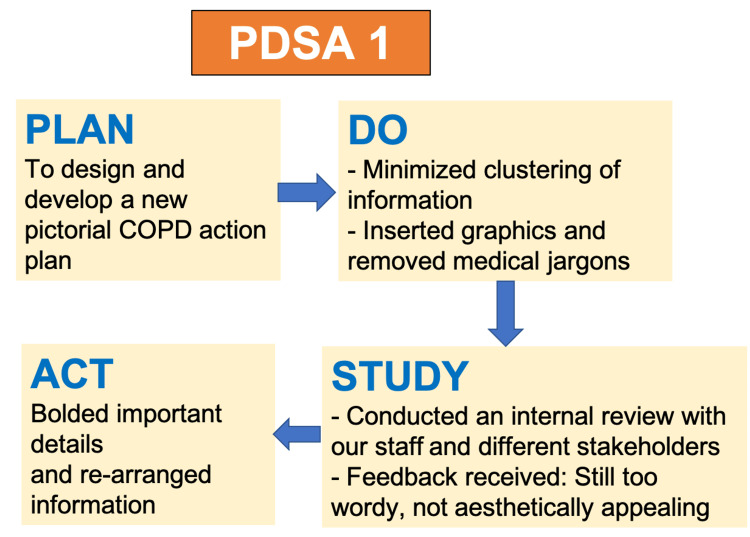
A total of two PDSA cycles were carried out.
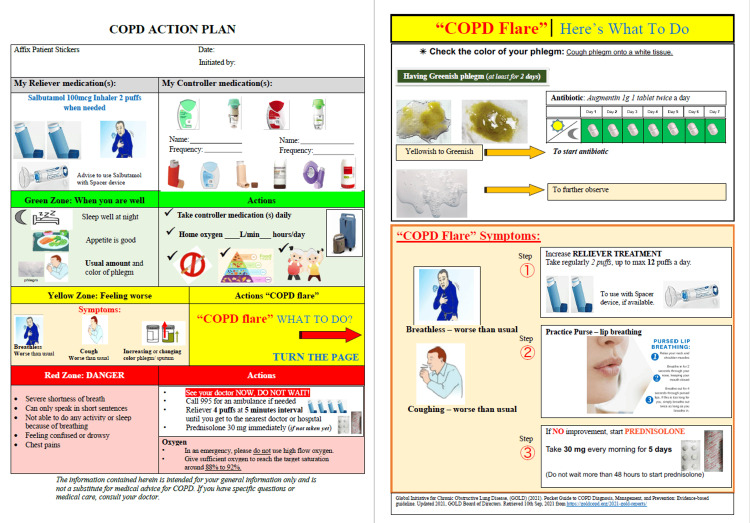
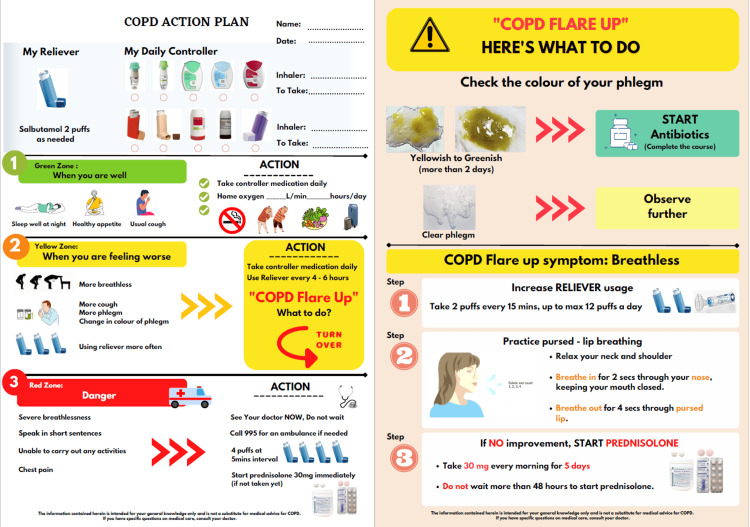
During the first PDSA cycle (Figure 5), we minimized the clustering of information by removing medical jargon. We also inserted relevant graphics (Figure 6). Afterward, the QI team also conducted an internal review within the respiratory department and the various stakeholders to evaluate the comprehensibility of the action plan. The feedback we received was that the action plan was still too wordy and important points were not emphasized. To address these concerns, we rearranged information in the action plan and important details were highlighted in bold (Figure 7).
Figure 5. PDSA Cycle 1.
Image credit: The authors
PDSA: Plan-Do-Study-Act
Figure 6. First edition of the pictorial COPD action plan.
Image credit: The authors
COPD: chronic obstructive pulmonary disease
Figure 7. Revised edition of pictorial COPD action plan.
Image credit: The authors
COPD: chronic obstructive pulmonary disease
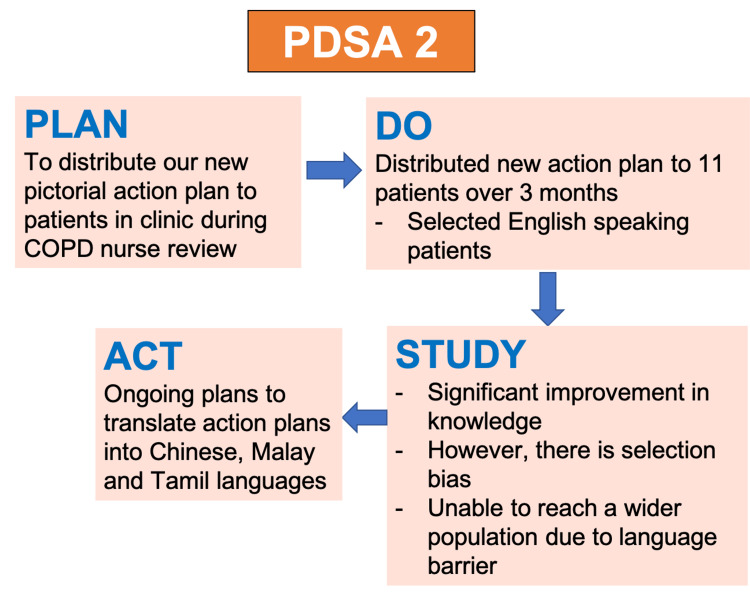
During the second PDSA cycle (Figure 8), we managed to distribute our revised pictorial COPD action plan to 11 English-speaking COPD patients who came to our outpatient respiratory clinic. This was carried out across three months from March to May 2022. As mentioned previously, we would conduct a competency check (Figure 4) after explaining the contents of the action plan to evaluate how much our patients have understood and retained the information. We then compared the knowledge scores we obtained from patients before and after the pictorial action plan was implemented (more details in the "Results" section). During the "study" phase of our PDSA cycle, the QI team recognized that even though there was a significant improvement in knowledge scores, we only targeted English-speaking patients. We were unable to reach a wider audience, as our action plan was only available in English. Hence, there are ongoing plans to translate our action plan into the Chinese, Malay, and Tamil languages.
Figure 8. PDSA cycle 2.
Image credit: The authors
PDSA: Plan-Do-Study-Act
Results
Ten English-speaking COPD patients from the outpatient respiratory clinic agreed to be surveyed after administering the original COPD action plan while 11 patients were surveyed after distributing the revised COPD action plan.
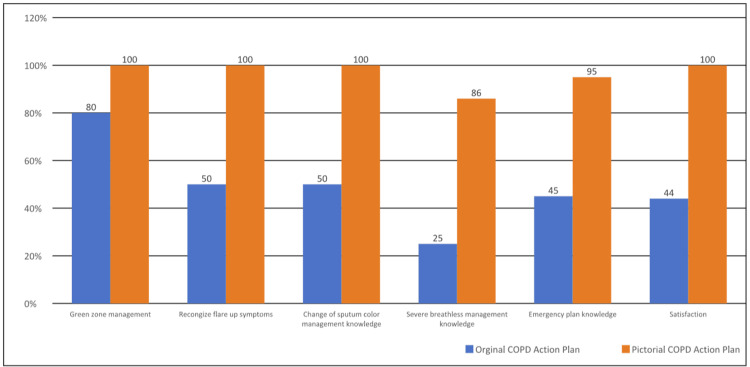
With the original COPD action plan, the mean knowledge score obtained from the competency check was 5/10 (n = 10). After receiving the revised plan, the mean knowledge score was 9.64/10 (n = 11). This amounted to an overall improvement of 92.8%, (t (19) = 6.67, p < 0.01, at 95% CI) (1-tailed t-test). Further analysis of the data revealed that the greatest improvement in scores was seen in questions related to recognizing exacerbations and how to manage them.
There was a significant improvement in patient satisfaction rates from 44% to 100% (Figure 9). During the 3-month callback, the majority of our patients, 7 out of 11 (63.6%) said they referred back to the new pictorial action plan at home when they were unwell. Out of these seven patients, three of them recognized the need to take a standby course of antibiotics and corticosteroids. These patients improved clinically and did not have to visit the ED to seek medical attention. The remaining patients who did not self-administer treatment or did not refer back to the action plan stated that they had no exacerbations throughout those three months.
Figure 9. Percentage improvement in knowledge scores before and after the implementation of the pictorial COPD action plan.
Image credit: The authors
COPD: chronic obstructive pulmonary disease
Discussion
COPD action plans have empowered patients to self-manage their conditions. Studies have shown that these action plans improve dyspnoea, decrease respiratory and all cause-related hospitalizations, and increase health-related quality of life [9,10]. Therefore, it is crucial that patients understand the action plan and are willing to use them when necessary.
Pictorially augmented action plans have been used for asthma in various studies [11,12]. They have exhibited benefits in asthma control and health-related quality of life, especially in the illiterate population [13]. A recent study done in Malaysia, which has a similar racial demographic to Singapore, found that pictorial asthma action plans were associated with better asthma control and cost savings in primary care patients [14]. For COPD, there was one small study, which evaluated the comprehensibility of pictorial COPD action plans by employing techniques of guessability and translucency. The study was conducted in a London hospital with 21 adult participants, and the investigators found pictorial action plans to be easily understood [15]. Other than that, our literature review revealed that there was still a lack of similar studies looking at pictorial action plans specifically for COPD patients.
A quality improvement methodology was used to assess the effectiveness of the original COPD action plan in a local context. The problem was evaluated using various QI tools such as the Needs Analysis, Fishbone diagram, Pareto chart, and subsequent Prioritization Matrix. We found a pictorially augmented COPD action plan to be a promising intervention. Upon implementation of our pictorial action plan using PDSA cycles, the data of our QI project showed a statistically significant improvement in knowledge scores between groups who have, and who have not received the new action plan. We achieved our aim of increasing the knowledge scores of our patients during competency checks by 20% over 10 months. A majority of the patients also referred back to our action plan at home.
In the future, we hope to further investigate the clinical impact of a pictorially augmented COPD action plan and to determine if this intervention translates to clinically relevant outcomes such as a decrease in the frequency of ED visits and hospitalization rates.
Limitations
Our study was limited by a small sample size, as it was carried out during the COVID pandemic. There were also potential biases in patient selection and feedback since only English-speaking patients and caregivers were recruited, and the majority of our stakeholders who participated in the Needs Analysis were healthcare professionals. We also recognized that our study had a short follow-up period of three months. Hence, we were unable to draw meaningful conclusions on the long-term impact of our project, specifically with regard to the frequency of COPD exacerbations and healthcare utilization of our patients.
However, we hope that our QI project serves as a primer to future larger-scale studies on pictorial COPD action plans. Furthermore, we expect that the benefits of these action plans will be further validated in upcoming studies.
Sustainability
Our hospital has replaced the existing COPD action plan with the new pictorial version. This new version has been translated into Mandarin, and we are working on translating it into other languages. To help widen our reach and increase accessibility to our COPD action plan, we have uploaded the soft copy version onto the hospital intranet to allow for easy access by other healthcare professionals. The team is also working on creating an application or QR code link to a webpage for easy reference by patients. We also plan to extend our action plan to other hospitals and the primary healthcare setting.
Conclusions
Pictorially enhanced COPD action plans have been shown to improve our patients’ COPD self-management knowledge. More studies are needed to assess the clinical relevance of this intervention. In the long run, we hope to empower more patients with the skills to self-manage their COPD condition at home.
Acknowledgments
The datasets generated and analyzed during the current study are available from Jonathan Ye (corresponding author).
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: QinHao Jonathan Ye, Yiting Tang, Hsiao Peng Toh, Kiran Sharma, Jessica Tan, Gan Liang Tan
Acquisition, analysis, or interpretation of data: QinHao Jonathan Ye, Yiting Tang, Hsiao Peng Toh, Kiran Sharma, Jessica Tan, Gan Liang Tan
Drafting of the manuscript: QinHao Jonathan Ye, Yiting Tang, Kiran Sharma
Critical review of the manuscript for important intellectual content: QinHao Jonathan Ye, Hsiao Peng Toh, Kiran Sharma, Jessica Tan, Gan Liang Tan
References
- 1.Mortality by cause for eight regions of the world: Global Burden of Disease Study. Murray CJ, Lopez AD. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 2.Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Murray CJ, Lopez AD. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health Singapore. Principal cause of death. [ Nov; 2023 ];https://www.moh.gov.sg/resources-statistics/singapore-health-facts/principal-causes-of-death 2022 2023:3–2023. [Google Scholar]
- 4.Action plans for COPD: strategies to manage exacerbations and improve outcomes. Jalota L, Jain VV. Int J Chron Obstruct Pulmon Dis. 2016;11:1179–1188. doi: 10.2147/COPD.S76970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Action plans for chronic obstructive pulmonary disease. Turnock AC, Walters EH, Walters JA, Wood-Baker R. Cochrane Database Syst Rev. 2005;4:0. doi: 10.1002/14651858.CD005074.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Self-management interventions for people with chronic obstructive pulmonary disease. Schrijver J, Lenferink A, Brusse-Keizer M, Zwerink M, van der Valk PD, van der Palen J, Effing TW. Cochrane Database Syst Rev. 2022;1:0. doi: 10.1002/14651858.CD002990.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Lung Association. My COPD action plan. [ Nov; 2023 ]. 2022. https://www.lung.org/getmedia/c7657648-a30f-4465-af92-fc762411922e/FY22-ALA-COPD-Action-Plan-with-QR-codes.pdf https://www.lung.org/getmedia/c7657648-a30f-4465-af92-fc762411922e/FY22-ALA-COPD-Action-Plan-with-QR-codes.pdf
- 8.My COPD action plan. Patient's copy. The Canadian Thoracic Society (CTS) [ Nov; 2023 ]. 2022. https://cts-sct.ca/wp-content/uploads/2018/03/4915_THOR_COPDActionPlanUpdate_Editable_Eng_v006.pdf https://cts-sct.ca/wp-content/uploads/2018/03/4915_THOR_COPDActionPlanUpdate_Editable_Eng_v006.pdf
- 9.(Cost-)effectiveness of self-treatment of exacerbations in patients with COPD: 2 years follow-up of a RCT. Zwerink M, Kerstjens HA, van der Palen J, van der Valk P, Brusse-Keizer M, Zielhuis G, Effing T. Respirology. 2016;21:497–503. doi: 10.1111/resp.12697. [DOI] [PubMed] [Google Scholar]
- 10.Self-management interventions including action plans for exacerbations versus usual care in patients with chronic obstructive pulmonary disease. Lenferink A, Brusse-Keizer M, van der Valk PD, et al. Cochrane Database Syst Rev. 2017;8:0. doi: 10.1002/14651858.CD011682.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Use of a low-literacy written action plan to improve parent understanding of pediatric asthma management: a randomized controlled study. Yin HS, Gupta RS, Mendelsohn AL, et al. J Asthma. 2017;54:919–929. doi: 10.1080/02770903.2016.1277542. [DOI] [PubMed] [Google Scholar]
- 12.The development and comprehensibility of a pictorial asthma action plan. Roberts NJ, Mohamed Z, Wong PS, Johnson M, Loh LC, Partridge MR. Patient Educ Couns. 2009;74:12–18. doi: 10.1016/j.pec.2008.07.049. [DOI] [PubMed] [Google Scholar]
- 13.The effectiveness of a pictorial asthma action plan for improving asthma control and the quality of life in illiterate women. Pur Ozyigit L, Ozcelik B, Ozcan Ciloglu S, Erkan F. J Asthma. 2014;51:423–428. doi: 10.3109/02770903.2013.863331. [DOI] [PubMed] [Google Scholar]
- 14.Feasibility of supported self-management with a pictorial action plan to improve asthma control. Sazlina SG, Lee PY, Cheong AT, et al. NPJ Prim Care Respir Med. 2022;32:34. doi: 10.1038/s41533-022-00294-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evaluation of a paper and electronic pictorial COPD action plan. Roberts NJ, Partridge MR. Chron Respir Dis. 2011;8:31–40. doi: 10.1177/1479972310382245. [DOI] [PubMed] [Google Scholar]