Abstract
Introduction
An estimated one billion people globally are currently suffering from hypertension. Prevention and management of hypertension are suboptimal especially in low- and middle-income countries leading to increased complications and deaths. With increased mobile phone coverage globally, this study aims to review mobile health technologies used for the prevention and management of hypertension.
Methods
We conducted a literature search on electronic databases using identified keywords involving “hypertension”, “mobile health technology” and their synonyms. Snowballing technique was also used. Papers were screened at two levels by independent reviewers. The targets were studies published in peer-reviewed journals reporting mobile health interventions for hypertension prevention and management. Only primary research studies published in English from January 2017 to April 2024 were included. Google Forms were used to extract the data along with other characteristics, and selected articles were categorised into: mobile application, web-based solutions, and Short Message Service (SMS) and other offline solutions.
Result
The search yielded 184 articles, and 44 studies were included in the review. Most (n = 26) were randomised control trials. Twenty-two studies (22) focused only on mobile applications solutions, 12 on SMS and other offline mHealth, 5 web-based solutions, and 5 combined more than one type of mobile health technology. The United States of America had the majority of studies (n = 17), with 6 studies from other American countries, 11 from Asia and nine from Europe, while only one from Africa. A total of 36 studies reported that mobile health technology significantly improved hypertension care through reduced blood pressure, improved adherence to follow-up visits and medications, and lifestyle changes. SMS and offline mHealth strategies have also demonstrated effectiveness in promoting self-management and reducing racial disparities in hypertension care.
Conclusion
Mobile health technology has the potential to play a significant role in the prevention and management of hypertension. However, there is a need for mobile health solutions for hypertension prevention and management in African countries and other developing countries. Integrating mHealth into primary healthcare delivery would also go a long way in strengthening patient care and reducing the burden on healthcare systems.
Keywords: Digital health, hypertension, healthcare, eHealth
Introduction
It is estimated that approximately one billion people worldwide suffer from hypertension. 1 Approximately 80% of these problems are seen in low- and middle-income countries. 2 It is predicted that by 2025, one in every three people will be suffering from hypertension. 3 Complications of uncontrolled hypertension include chronic kidney disease, cerebrovascular accident, cardiomyopathy, and heart failure. These complications are, however, preventable through adequate management. This is cost effective and improves outcome. Expensive interventions, such as cardiac bypass surgery and dialysis, may be required when hypertension is poorly managed. Although antihypertensive drugs are effective and lifestyle adjustments have a positive impact on blood pressure, hypertension control rates are still far from ideal. 4 One of the best ways to manage hypertension is by self-management, which encourages people with the condition to take more responsibility for their own health. 5
Researchers and healthcare professionals have been inspired to explore the various features and applications of technology since its emergence in the healthcare system in order to enhance illness management and prevention. Following these efforts, mobile health technology (mHealth) has been noted to have the potential to facilitate and optimise patients’ self-management. 6 Previously, mobile health interventions focused on voice or text-based short messaging services (SMS), but the growing accessibility and usability of smartphone applications have enabled a considerable increase in the number of mobile applications that can be used to modify health behaviour. 7 The proliferation of mobile health (mHealth) care devices and software has greatly expanded self-care capabilities across the health care spectrum. 1 The increase in smartphone devices over the past few decades has been rapid. 8 This sharp rise in smartphone usage is mirrored by a surge in mobile applications that provide health services and information.9,10
This study aims to review mobile health technologies used for the prevention and management of hypertension.
Methodology
We carried out a scoping review to map relevant literature in the field of mHealth and its utilisation in the care of hypertension. This study design was favoured as Munn et al. 11 highlighted scoping reviews as the more useful approach for reviewing evidence rapidly in novel or emerging topics, under which mHealth falls, as well as identification and analysis of knowledge gaps to inform future questions about the field. The review was done following the five-stage framework developed by Arksey and O'Malley, 12 which consists of the stages outlined below:
Identification of the research question
We were interested in assessing mobile health technologies in the prevention and management of hypertension.
Identification of relevant studies
We conducted a literature search on electronic databases including MEDLINE, PubMed, PubMed Central, Google Scholar, and Scopus using a combination of keywords involving “hypertension”, “mobile health technology” and their synonyms identified from previous studies. The search strings are shown below in Table 1. Snowballing technique was also used by screening the bibliographies of identified papers for other relevant studies. Only articles published in peer-reviewed scientific journals were considered for review.
Table 1.
Search strategy.
| Hypertension | AND | Mobile health technology | Inclusion |
|---|---|---|---|
| Hypertension, elevated/raised/high blood pressure/diastolic blood pressure/systolic blood pressure/BP | mHealth/m-health/m health, mobile health technology, mobile phones/cell phone, text message, mobile application, eHealth/e-health/website/web/web-based/website-based/online/internet | Publications in English, hypertension interventions focused on prevention and/or management of A, and specifically, interventions offered using mHealth technologies. |
Study selection
The title and abstracts of the search results were screened by two independent reviewers. Conflicts were resolved through team consensus. Inclusion criteria included: (1) papers published in peer-reviewed journals reporting mobile health interventions for hypertension prevention and management, (2) papers published in English language, (3) publications from January 2017 to August 2022 (time of search conduction), (4) only primary research studies. The exclusion criteria were: (1) papers published in other languages, (2) papers focusing on other non-communicable diseases, including pregnancy-induced hypertensive disorders, (3) papers published before January 2017 or after August 2022, (4) all types of reviews. The time window was chosen in order to avoid outdated data, likely to be of less relevance or obsolete in a rapidly evolving field like mHealth, thus improving the accuracy of results.
The full manuscripts of the selected papers were screened for data extraction by eight reviewers and final decision for inclusion. The papers were shared among the eight reviewers divided into four pairs, with members of each pair working together to screen assigned manuscripts. Conflicts between them were resolved by an independent ninth reviewer who oversaw the whole process.
A recent search was further carried out by two reviewers using similar keywords to seek out more recent studies between time of original search (August 2022) and time of final submission (April 2024). Obtained studies were screened in full by the two reviewers, with conflicts being resolved by a third reviewer.
Quality assessment
The quality assessment was done using the CASP Critical Appraisal Tools.13–15 This is due to the fact that it has checklists for different study designs. Data was extracted by three reviewers using Google Sheet (Supplemental material).
Data charting
The data was extracted using online Google Forms and included variables such as year of publication, country of study, study design, type of mobile health technology, aim of study, key findings, significance of mHealth, study limitations and final decision on inclusion. The data extracted was subsequently exported into an excel sheet for cleaning, sorting and synthesising.
Collating, summarising and reporting the findings
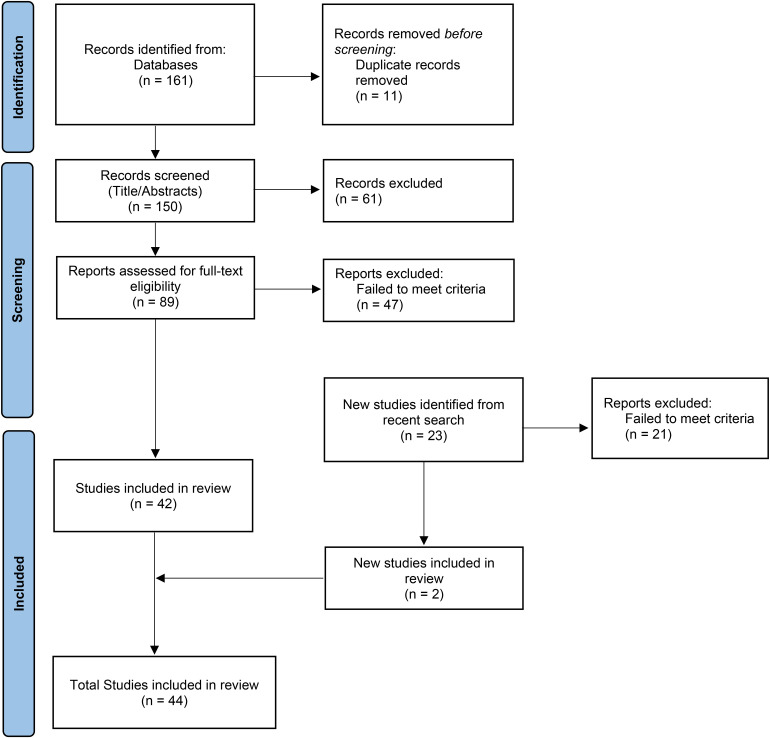
The data was categorised based on the mobile health technology used, that is, (1) SMS and other offline solutions, (2) mobile application solutions, and (3) web-based solutions. Other characteristics were also analysed, allowing us to clearly explore the different mHealth approaches, as well as to identify possible gaps. Figure 1 illustrates the process of identifying relevant papers for inclusion in data extraction and final synthesis.
Figure 1.
Flow diagram illustrating the article selection process.
Source: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.
Results
A total of 44 studies were included in this review (Table 2). The selected studies were grouped into three categories based on the type of the mobile health technology. A total of 22 studies4,16–36 focused on only mobile applications solutions, 1237–48 on SMS and other offline mHealth, five49–53 web-based solutions only, and five54–58 combined more than one type of mobile health technology.
Table 2.
Review of digital health intervention for hypertension management.
| S/N | First author surname (year of publication) | Country of intervention | Study design | Type of digital health intervention | Name of intervention | Did the digital intervention improve hypertension care? |
|---|---|---|---|---|---|---|
| 1. | Yeung, D. L. (2017) | United States of America | Case–control study | Web-based | Barcoded educational flashcard video | Yes, significantly |
| 2. | Yin, B. D. (2021) | China | Case–control study | Mobile application | Hypertension management platform of the chronic disease management application (APP) | Yes, significantly |
| 3. | Agnihothri, S. (2021) | United States of America | Cohort study | Web-based | N/A | Yes, significantly |
| 4. | Chandrasekhar, A. (2018) | United States of America | Cohort study | Mobile application | N/A | No, there was no difference from control |
| 5. | Ciemins, E. L. (2018) | United States of America | Cohort study | Mobile application | Bluetooth low energy technology | Yes, significantly |
| 6. | Gazit, T. (2021) | United States of America | Cohort study | Mobile application | Bluetooth-enabled BP monitor (Zewa UAM-910BT, Zewa UAM-900 T, or A&D UA-651BLE BP cuffs) paired with a smartphone app | Yes, but not statistically significant |
| 7. | Janssen, M. K. (2021) | United States of America | Cohort study | SMS and other offline mHealth | Heart safe motherhood. | Yes, significantly |
| 8. | Mao, A. Y. (2017) | United States of America | Cohort study | Mobile application | Vida health | Yes, significantly |
| 9. | Triebwasser, J. E. (2020) | United States of America | Cohort study | SMS and other offline mHealth | Heart safe motherhood | Yes, significantly |
| 10. | Zhong, D. (2020) | China | Cohort study | Web based | CrowdOS | Yes, significantly |
| 11. | Garner, S. L. (2020) | India | Cross sectional Study | Mobile application | N/A | Yes, significantly |
| 12. | Golbus, J. R. (2021) | United States of America | cross sectional study | Mobile application | MyDataHelps | Yes, significantly |
| 13. | Kaplan, A. L. (2017) | Israel | cross sectional study | Mobile application | Hello Heart | Yes, significantly |
| 14. | Langford, A. T. (2019) | United States of America | cross sectional study | Mobile application | Health Information National Trends Survey (HINTS) | Yes, significantly |
| 15. | Garner, S. L. (2021) | Hong Kong | Mixed-methods | Mobile application | N/A | Yes, significantly |
| 16. | Grant, S. (2019) | United Kingdom | Qualitative study | SMS and other offline mHealth, Web based, Data management | N/A | Yes, significantly |
| 17. | Morrissey, E. C. (2018) | Ireland | Qualitative study | Mobile application | MIBP | Yes, significantly |
| 18. | Schoenthaler, A. (2020) | United States of America | Qualitative study | Mobile application | The mHealth intervention was built by Radiant Point Technologies using Microsoft's Models, Views, and Controllers Entity Framework as the development environment for the intervention. The intervention consists of an administrative interface for creating user accounts and exporting data and a patient portal for entering information (eg, user profile, questionnaires) and completing activity modules | Yes, significantly |
| 19. | Andersson, U. (2021) | Sweden | Randomised control trial | Web-based | CQ | Yes, significantly |
| 20. | Araya, R. (2021) | Brazil, Peru | Randomised control trial | Mobile application | N/A | Yes, significantly |
| 21. | Bengtsson, U. (2018) | Sweden | Randomised control trial | Web-based | N/A | Yes, but not statistically significant |
| 22. | Bolmsjö, B. B. (2020) | Sweden | Randomised control trial | SMS and other offline mHealth | N/A | Yes, but not statistically significant |
| 23. | Bozorgi, A. (2021) | Iran | Randomised control trial | Mobile application | N/A | Yes, significantly |
| 24. | Buis, L. (2017) | United States of America | Randomised control trial | SMS and other offline mHealth | BPMED | Yes, but not statistically significant |
| 25. | Gong, K. (2020) | China | Randomised control trial | Mobile application | Yan Fu app | Yes, significantly |
| 26. | He, J. (2017) | Argentina | Randomised control trial | SMS and other offline mHealth | N/A | Yes, significantly |
| 27. | Ionov, M. V. (2020) | Russia | Randomised control trial | Mobile application, Web based | STRIDE BP | Yes, significantly |
| 28. | Jahan, Y. (2020) | Bangladesh | Randomised control trial | SMS and other offline mHealth | N/A | Yes, significantly |
| 29. | Kario, K. (2021) | Japan | Randomised control trial | Mobile application | HERB Mobile | Yes, significantly |
| 30. | Liu, F. (2023) | China | Randomised control trial | Mobile application | Blood Pressure Assistant | Yes, significantly |
| 31. | Márquez Contreras, E. (2019) | Spain | Randomised control trial | Mobile application | AlerHTA APP | Yes, significantly |
| 32. | Morawski, K. (2018) | United States of America | Randomised control trial | Mobile application | Medisafe app | Yes, but not statistically significant |
| 33. | Persell, S. D. (2020) | United States of America | Randomised control trial | Mobile application | HPCP coaching app | No, there was no difference from control |
| 34. | Sarfo, FS. (2019) | Ghana | Randomised control trial | Mobile application | N/A | Yes, significantly |
| 35. | Schroeder, E. B. (2019) | United States of America | Randomised control trial | SMS and other offline mHealth | N/A | Yes, significantly |
| 36. | Sookrah, R. (2019) | United States of America | Randomised control trial | SMS and other offline mHealth | IVR-T | Yes, significantly |
| 37. | Tobe, S. W. (2019) | Canada | Randomised control trial | SMS and other offline mHealth, mobile application, web-based, data management | SAS software | Yes, significantly |
| 38. | Varleta, P. (2017) | Chile | Randomised control trial | SMS and other offline mHealth | N/A | Yes, significantly |
| 39. | Villarreal, V. (2018) | Panama | Randomised control trial | Mobile application, web-based | PHP, Modern View Controller(MVC) | Yes, significantly |
| 40. | Yardley, L. (2022) | United Kingdom | Randomised control trial | Mobile application | HOME BP | Yes, significantly |
| 41. | Yatabe, J. (2021) | Japan | Randomised control trial | Mobile application, web-based | DASH mobile, online video content, TASMINH4 | Yes, significantly |
| 42. | Yeates, K. (2017) | Canada | Randomised control trial | SMS and other offline mHealth | None | Yes, significantly |
| 43. | Zahr, R. S. (2019) | United States of America | Randomised control trial | SMS and other offline mHealth | N/A | Yes, but not statistically significant |
| 44. | Zhai, P. (2020) | China | Randomised control trial | SMS and other offline mHealth | N/A | Yes, significantly |
Most (n = 26) of the selected studies4,20–26,28,29,37,38,40–47,49,53,54,56–58 were randomised control trials. Other study designs found were cohort studies (n = 8),30–33,39,48,51,52 qualitative studies (n = 3),18,19,55 and other observational studies (n = 7).16,17,27,34–36,50
Most of the studies19,20,23,30–34,36,39,41,42,44,47,48,50,52 were conducted in the United States of America (n = 17). There were six studies21,38,45,46,54,57 from other American countries, 114,16,22,25,27,29,35,37,40,51,56 from Asia, and nine17,18,24,26,43,49,53,55,58 from Europe. Only one study 28 was conducted in Africa.
A total of 36 studies4,16–19,21,22,24–31,34–40,42,45–48,50–58 reported that mobile health technology improved hypertension care significantly, while the remaining (n = 8)20,23,32,33,41,43,44,49 showed no statistically significant improvements. All studies (n = 5)54–58 that combined more than one type of digital technology significantly improved hypertension care. Improvement of hypertension care included reduced blood pressure (systolic or diastolic), improved adherence to follow-up visits, increased literacy, lifestyle changes and other prevention and management measures of hypertension in adults, Table 2.
Discussion
Interventions using Mobile application technology
Mobile applications (apps) and other mobile health (mHealth) interventions have been promoted as promising strategies to aid in the self-management of hypertension and other chronic conditions. 24 By offering reminders for taking medication and ordering refills, monitoring biometric findings, providing information, and facilitating social interactions that offer support and encouragement, these systems support long-term management of these conditions. Of the papers reviewed in this study that focused on mobile application technology as a digital health intervention and fulfilled the inclusion criteria (n = 26),4,16–36,54,56–58 only four20,23,32,33 reported no statistical improvement in hypertension care. Studies that showed improvement included 12 randomised control trials,4,21,22,24–26,28,29,54,56–58 thus offering high enough level of evidence on the benefits of this form of intervention.
Following the COVID-19 pandemic which highlighted the shortcomings of conventional medical care and the need for telemedicine, 59 new chances to care for patients with cardiac problems remotely have been made possible by mobile phones, especially smartphones. In the past, telemedicine called for giving patients specialised monitoring equipment to use at home. However, mobile apps and wearable technology offer enormous potential for monitoring health through calls, texts, data recording, highly portable peripheral devices, and activity monitoring, which may find utility for novel models of healthcare delivery that are affordable, accessible, and patient-centred. 52
This can be accomplished by integrating healthcare into daily life through the delivery and collection of health information and services in a convenient, accessible, and interactive manner. 60 The use of a physician-supervised mobile health app was strongly linked to better health outcomes (reduced BP). For individuals with high levels of severity, the improvement was notable. 52 As a result, using an mHealth app can help a healthcare system be proactive (especially with regard to a silent killer like hypertension) and vastly enhance the quality of care. 61
A wide variety of applications were utilised in the reviewed studies with novel apps like MIBP employing user-centred interventions focused on self-BP monitoring, physical activity, reduced sodium intake, and medication adherence to improve hypertensive care. 18 Another study by Contreras et al., made use of an app, AlerTHA, on hypertensive patients’ mobile phones to enhance BP control and pharmacological therapy adherence via health education and reminder of appointments. 24 Social media platforms have also shown to be crucial with a study in China demonstrating how WeChat app, through health education, health promotion, group chats, and blood pressure monitoring, help patients lower blood pressure and improve the effectiveness of self-management.61,62
Additional benefits have also been described when blood pressure telemonitoring is offered under the supervision of healthcare personnel.62,63 The effective treatment of hypertension requires self-management, and with the development of mobile technologies, mHealth assists in the management of hypertension. 64 Also, it was noted that patients’ medication adherence and self-management behaviours had improved when mobile app was used to control patients’ hypertension. 25 According to Li et al., 64 the most effective mobile apps integrate customised messages, interactive communication, and complex features.
In order to motivate patients to engage in healthy behaviours and embrace healthy lifestyles, mobile applications that contain gamification aspects, such as prizes and challenges, are also available.65,66
Interventions using short message service technology (or other offline mHealth strategies)
Eleven37–40,42,45–48,54,55 out of 14 papers reviewed with focus on SMS and other offline mHealth interventions (n = 14)37–48,54,55 improved hypertension management significantly. Most of the papers were randomised controlled trials (n = 8).37,38,40,42,45–47,54 Most studies39,42,47,48 were conducted in the United States of America (n = 4).
The self-management and control of chronic illnesses, including hypertension and diabetes, have benefited from the usage of Short Message Service (SMS), chatbots, and other offline mHealth techniques that communicate mostly through short texts in telecommunications.62,67
SMS has been shown to be effective in reminding patients to take their daily meds at a low cost with high results. 68 In fact, it has been a significant source of patient–physician monitoring for brief and rapid communication, especially in difficult-to-reach places. SMS is a remarkable mHealth intervention in the treatment of hypertension that helps prevention of disruption of daily routines, preference for natural therapies, anxiety about side effects, forgetfulness, and inconvenience. 19
More specifically, SMS has made it possible to monitor and evaluate clinical and behavioural outcomes of patients as this brief messaging and offline technique improves patients’ adherence as a form of reminder for the control and management of blood pressure. 64
In order to achieve quality health delivery while keeping patient care in mind, offline mHealth strategies have indeed been helpful in minimising racial disparities. 39 Additionally, it has given healthcare professionals the chance to spend time caring for other patients by reducing the number of unnecessary hospital visits by patients managing hypertension. Due to the present shortage of healthcare professionals, mHealth technology has been supporting the need to prioritise scheduling more patients in order to ensure that they can receive high-quality care. 69
Interventions using web-based or websites
A total of 10 papers49–58 reviewed included web-based technology as its intervention to improve hypertension management. Only one 49 study reported no significant improvement in hypertension care. A total of six papers49,53,54,56–58 were randomised controlled trials. Two (2) studies were conducted in the United States of America50,52 and Sweden49,53 while a paper each from Russia, 58 Canada, 54 Panama, 57 China, 51 Japan, 56 and United Kingdom. 55
Sam Liu et al. conducted a randomised controlled trial to show the significance of expert-driven web-based interventions compared to the self-guided interventions. 70 This study reported a greater systolic blood pressure reduction among the expert-driven group when compared to the control group. However, systolic blood pressure reduction did not significantly differ between user- and expert-driven. A self-monitoring automated electronic sphygmomanometer was studied in relation to the usual care of routine clinic visits in Taiwan. 71 The intervention group also reported a significant decrease in the overall defined daily dose of medications and a significant improvement in health-related quality of life in comparison with the control. 71 Villarreal et al., developed a platform which is an integrated form of mobile application and a web-based application called AmIHealth. 57 The mobile application is the main platform for patient interaction which allows the recording and storing of vital signs of patients in a local database, while the web application obtains data from the mobile application when there is internet connectivity. Doctors can then have access to and follow up on the records of their patients from the web application thereby allowing for the generation of a prevention plan more appropriate to each patient.
Non-adherence to medications has been found to be a remarkable cause of treatment failures, increasing mortality, and costing about $100b every year.25,72 A prospective study was carried out by Yeung et al. involving 68 patients with the aim of investigating the effectiveness of low-health literacy educational interventions such as paper flashcards and quick response coded online videos in improving medication adherence in patients using heart failure, hypertension, and diabetes medications. 50 The study reported that 88% of patients were satisfied with the educational intervention and would recommend it to family and friends. 50 Web-based intervention can allow patients to take an active role in the management of their hypertension. For instance, a randomised control trial using an interactive web-based system conducted showed that people who made use of the web system had a good understanding of how their blood pressure was affected by their lifestyle and are inspired to live a healthy lifestyle. 53
Limitations of mHealth
mHealth, despite its benefits and ease of use, is however not void of limitations. A major one noted during this review was the fact that hypertension status was self-reported by the patients in a number of studies, thus giving way for over- or underreporting, as well as patient recording errors.25,34,61 A wide variability was also noted among participants with varied literacy and health literacy levels. 16 High attrition rate was also noted as a major challenge among participants due to changes in location, as well as forgetfulness. 25
Of the interventions using web-based or websites and Short Message Service Technology (or other offline mHealth strategies), no limitation was specifically mentioned or stated for any improvement yet. These could be due to limited publications yet in mHealth and digital health in the prevention and management of hypertension.
Limitations of study
This scoping review has some limitations. First, the search period was narrow. This is because of the rapid advancement of digital health technology and a high number of available studies in recent years. Also, the scoping review did not include some databases such as Cochrane database and conference proceedings. The CASP critical appraisal tools used for risk assessment do not have a standardised scoring of quality of study. However, it was chosen because of the availability of checklists for different study designs.
Conclusion
In conclusion, this review shows the potential of mHealth in improving hypertension prevention and management globally including the low- and middle-income countries. It shows the need to combine digital health technologies to achieve better outcomes. It shows the need for more mHealth interventions in Africa to prevent and manage hypertension.
Supplemental Material
Supplemental material, sj-xlsx-1-dhj-10.1177_20552076241277172 for Mobile health technologies in the prevention and management of hypertension: A scoping review by Abdulhammed Opeyemi Babatunde, Deborah Abisola Ogundijo, Abdul-Gafar Olayemi Afolayan, Olutola Vivian Awosiku, Zainab Opeyemi Aderohunmu, Mayowa Sefiu Oguntade, Uthman Hassan Alao, Abdulrahman Ololade Oseni, Abdulqudus Abimbola Akintola and Olanrewaju Adams Amusat in DIGITAL HEALTH
Acknowledgements
The authors appreciate Dimaji A. Olawuyi and all members and volunteers of the SmileBuilders Initiative for the support in conducting the research.
Footnotes
Consent for publication: All authors provided consent to publication.
Contributorship: AOB and OAA conceptualised and designed the study. ZOA and DAO performed the literature search. DAO, AGO, OVA, ZOA, MSO, AOO, OAA, AAA screened and reviewed articles for inclusion. DAO, OVA, AGO, AAA, AOB, ZOA wrote the first draft of the manuscript. UHA, AGO, AOB did the final literature review, proofreading and copyediting. All authors reviewed the manuscript and approved for submission.
Data availability: Available upon request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Abdulhammed Opeyemi Babatunde https://orcid.org/0000-0002-3648-5340
Abdul-Gafar Olayemi Afolayan https://orcid.org/0009-0001-3843-271X
Abdulqudus Abimbola Akintola https://orcid.org/0000-0003-0789-1216
Supplemental material: Supplemental material for this article is available online.
References
- 1.Alessa T, Hawley MS, Hock ESet al. et al. Smartphone Apps to support self-management of hypertension: review and content analysis. JMIR mHealth uHealth [Internet] 2019. May 1 [cited 2024 Apr 1]; 7: e13645. Available from: /pmc/articles/PMC6658295/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vedanthan R, Bernabe-Ortiz A, Herasme OI, et al. Innovative approaches to hypertension control in low- and middle-income countries. Cardiol Clin [Internet] 2017. Feb 1 [cited 2024 Apr 1]; 35: 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation [Internet] 2019. Mar 5 [cited 2024 Apr 1]; 139: e56–528. [DOI] [PubMed] [Google Scholar]
- 4.Bozorgi A, Hosseini H, Eftekhar H, et al. The effect of the mobile “blood pressure management application” on hypertension self-management enhancement: a randomized controlled trial. Trials [Internet] 2021. Dec 1 [cited 2024 Apr 1]; 22: 413. Available from: https://pubmed.ncbi.nlm.nih.gov/34167566/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shahaj O, Denneny D, Schwappach A, et al. Supporting self-management for people with hypertension: a meta-review of quantitative and qualitative systematic reviews. J Hypertens [Internet] 2019. [cited 2024 Apr 1]; 37: 264–279. [DOI] [PubMed] [Google Scholar]
- 6.Kluge EHW. Framework considerations. Electron Heal Rec 2020. Jan 1: 105–133. [Google Scholar]
- 7.McKay FH, Cheng C, Wright A, et al. Evaluating mobile phone applications for health behaviour change: a systematic review. J Telemed Telecare [Internet] 2018. Jan 1 [cited 2024 Apr 1]; 24: 22–30. [DOI] [PubMed] [Google Scholar]
- 8.Barnes SJ, Pressey AD, Scornavacca E. Mobile ubiquity: understanding the relationship between cognitive absorption, smartphone addiction and social network services. Comput Human Behav 2019; 90: 246–258. [Google Scholar]
- 9.Zhang L, Hua K, Wang H, et al. Sentiment analysis on reviews of Mobile users. Procedia Comput Sci 2014; 34: 458–465. [Google Scholar]
- 10.Rivera J, McPherson A, Hamilton J, et al. Mobile apps for weight management: a scoping review. JMIR mHealth UHealth [Internet] 2016. Jul 1 [cited 2024 Apr 1]; 4: e5115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol [Internet] 2018. Nov 19 [cited 2024 Apr 14]; 18: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arksey H, O’malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol [Internet] 2005. [cited 2024 Apr 14]; 8: 19–32. [Google Scholar]
- 13.Critical Appraisal Skills Programme [Internet]. CASP Randomised Control Trial Checklist. 2021 [cited 2024 Jul 1]. Available from: https://casp-uk.net/checklists/casp-rct-randomised-controlled-trial-checklist.pdf.
- 14.Critical Appraisal Skills Programme [Internet]. CASP Cohort Study Checklist. 2018 [cited 2024 Jul 1]. Available from: https://casp-uk.net/checklists/casp-cohort-studies-checklist-fillable.pdf.
- 15.Critical Appraisal Skills Programme [Internet]. CASP qualitative checklist. 2018 [cited 2024 Jul 1]. Available from: https://casp-uk.net/checklists/casp-qualitative-studies-checklist.pdf.
- 16.Garner SL, Wong CL, Young P, et al. Mobile health to improve hypertension and diabetes health literacy among Asian Indian migrants to Hong Kong. Comput Inform Nurs [Internet] 2021. Apr 10 [cited 2024 Apr 6]; 40: 269–277. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan AL, Cohen ER, Zimlichman E. Improving patient engagement in self-measured blood pressure monitoring using a mobile health technology. Heal Inf Sci Syst [Internet] 2017. Dec 1 [cited 2024 Apr 6]; 5: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrissey EC, Casey M, Glynn LG, et al. Smartphone apps for improving medication adherence in hypertension: patients’ perspectives. Patient Prefer Adherence [Internet] 2018. May 14 [cited 2024 Apr 6]; 12: 813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schoenthaler A, Leon M, Butler M, et al. Development and evaluation of a tailored mobile health intervention to improve medication adherence in black patients with uncontrolled hypertension and Type 2 diabetes: pilot randomized feasibility trial. JMIR mHealth uHealth [Internet] 2020. Sep 1 [cited 2024 Apr 6]; 8: e17135. Available from: https://pubmed.ncbi.nlm.nih.gov/32965230/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morawski K, Ghazinouri R, Krumme A, et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med [Internet] 2018. Jun 1 [cited 2024 Apr 6]; 178: 802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Araya R, Menezes PR, Claro HG, et al. Effect of a digital intervention on depressive symptoms in patients with comorbid hypertension or diabetes in Brazil and Peru: two randomized clinical trials. JAMA [Internet] 2021. May 11 [cited 2024 Apr 6]; 325: 1852–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gong K, Yan YL, Li Y, et al. Mobile health applications for the management of primary hypertension: a multicenter, randomized, controlled trial. Medicine (Baltimore) [Internet] 2020. Apr 30 [cited 2024 Apr 6]; 99: E19715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Persell SD, Peprah YA, Lipiszko D, et al. Effect of home blood pressure monitoring via a smartphone hypertension coaching application or tracking application on adults with uncontrolled hypertension: a randomized clinical trial. JAMA Netw Open [Internet] 2020. Mar 2 [cited 2024 Apr 6]; 3: E200255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Márquez Contreras E, Márquez Rivero S, Rodríguez García E, et al. Specific hypertension smartphone application to improve medication adherence in hypertension: a cluster-randomized trial. Curr Med Res Opin [Internet] 2019. Jan 2 [cited 2024 Apr 6]; 35: 167–173. [DOI] [PubMed] [Google Scholar]
- 25.Liu F, Song T, Yu P, et al. Efficacy of an mHealth App to support patients’ self-management of hypertension: randomized controlled trial. J Med Internet Res [Internet] 2023. [cited 2024 Apr 15] 25: e43809. Available from: /pmc/articles/PMC10762623/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yardley L, Morton K, Greenwell K, et al. Digital interventions for hypertension and asthma to support patient self-management in primary care: the DIPSS research programme including two RCTs. Program Grants Appl Res [Internet] 2022. [cited 2024 Apr 15]; 10. Available from: https://www.ncbi.nlm.nih.gov/books/NBK587710/. [PubMed] [Google Scholar]
- 27.Yin BD, Tu DH, Yang Net al. et al. The application effect of internet technology on managing patients with hypertension in a medical center: a prospective case-control study. Medicine (Baltimore) [Internet] 2021. Dec 17 [cited 2024 Apr 6]; 100: E28027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sarfo FS, Treiber F, Gebregziabher M, et al. Phone-based intervention for blood pressure control among Ghanaian stroke survivors: a pilot randomized controlled trial. Int J Stroke [Internet] 2019. Aug 1 [cited 2024 Apr 15]; 14: 630–638. [DOI] [PubMed] [Google Scholar]
- 29.Kario K, Nomura A, Harada N, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J [Internet] 2021. Oct 10 [cited 2024 Apr 15]; 42: 4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mao AY, Chen C, Magana C, et al. A Mobile phone-based health coaching intervention for weight loss and blood pressure reduction in a national payer population: a retrospective study. JMIR mHealth UHealth [Internet] 2017. Jun 8 [cited 2024 Apr 6]; 5: e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ciemins EL, Arora A, Coombs NC, et al. Improving blood pressure control using smart technology. Telemed J E Health [Internet] 2018. Mar 1 [cited 2024 Apr 6]; 24: 222–228. [DOI] [PubMed] [Google Scholar]
- 32.Gazit T, Gutman M, Beatty AL. Assessment of hypertension control among adults participating in a Mobile technology blood pressure self-management program. JAMA Netw Open [Internet] 2021. Oct 1 [cited 2024 Apr 6]; 4: e2127008–e2127008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chandrasekhar A, Kim CS, Naji M, et al. Smartphone-based blood pressure monitoring via the oscillometric finger-pressing method. Sci Transl Med [Internet] 2018. Mar 7 [cited 2024 Apr 6]; 10: eaap8674. Available from: https://pubmed.ncbi.nlm.nih.gov/29515001/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Langford AT, Solid CA, Scott E, et al. Mobile phone ownership, health apps, and tablet use in US adults with a self-reported history of hypertension: cross-sectional study. JMIR mHealth UHealth [Internet] 2019. Jan 14 [cited 2024 Apr 6]; 7: e12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garner SL, George CE, Young P, et al. Effectiveness of an mHealth application to improve hypertension health literacy in India. Int Nurs Rev [Internet] 2020. Dec 1 [cited 2024 Apr 6]; 67: 476–483. [DOI] [PubMed] [Google Scholar]
- 36.Golbus JR, Pescatore NA, Nallamothu BK, et al. Wearable device signals and home blood pressure data across age, sex, race, ethnicity, and clinical phenotypes in the Michigan predictive activity & clinical trajectories in health (MIPACT) study: a prospective, community-based observational study. Lancet Digit Heal [Internet] 2021. Nov 1 [cited 2024 Apr 6]; 3: e707–e715. [DOI] [PubMed] [Google Scholar]
- 37.Jahan Y, Rahman MM, Faruque ASG, et al. Awareness development and usage of mobile health technology among individuals with hypertension in a rural community of Bangladesh: randomized controlled trial. J Med Internet Res [Internet] 2020. Dec 1 [cited 2024 Apr 7]; 22: e19137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He J, Irazola V, Mills KT, et al. Effect of a community health worker–led multicomponent intervention on blood pressure control in low-income patients in Argentina: a randomized clinical trial. JAMA [Internet] 2017. Sep 19 [cited 2024 Apr 7]; 318: 1016–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Triebwasser JE, Janssen MK, Hirshberg Aet al. et al. Successful implementation of text-based blood pressure monitoring for postpartum hypertension. Pregnancy Hypertens [Internet] 2020. Oct 1 [cited 2024 Apr 7]; 22: 156–159. [DOI] [PubMed] [Google Scholar]
- 40.Zhai P, Hayat K, Ji W, et al. Efficacy of text messaging and personal consultation by pharmacy students among adults with hypertension: randomized controlled trial. J Med Internet Res [Internet] 2020. May 20 [cited 2024 Apr 15]; 22: e16019. Available from: /pmc/articles/PMC7270845/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buis L, Hirzel L, Dawood RM, et al. Text messaging to improve hypertension medication adherence in African Americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR mHealth UHealth [Internet] 2017. Feb 1 [cited 2024 Apr 7]; 5: e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schroeder EB, Moore K, Manson SM, et al. An interactive voice response and text message intervention to improve blood pressure control among individuals with hypertension receiving care at an urban Indian Health Organization: Protocol and baseline characteristics of a pragmatic randomized controlled trial. JMIR Res Protoc 2019; 8: e11794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bolmsjö BB, Wolff M, Nymberg VM, et al. Text message-based lifestyle intervention in primary care patients with hypertension: a randomized controlled pilot trial. Scand J Prim Health Care [Internet] 2020. [cited 2024 Apr 7]; 38: 300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zahr RS, Anthony CA, Polgreen PM, et al. A texting-based blood pressure surveillance intervention. J Clin Hypertens (Greenwich) [Internet] 2019. Oct 1 [cited 2024 Apr 7]; 21: 1463–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yeates K, Campbell N, Maar MA, et al. The effectiveness of text messaging for detection and management of hypertension in indigenous people in Canada: protocol for a randomized controlled trial. JMIR Res Protoc [Internet] 2017. Dec 19 [cited 2024 Apr 7]; 6: e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Varleta P, Acevedo M, Akel C, et al. Mobile phone text messaging improves antihypertensive drug adherence in the community. J Clin Hypertens [Internet] 2017. Dec 1 [cited 2024 Apr 7]; 19: 1276–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sookrah R, Dhowtal JD, Nagowah SD. A DASH diet recommendation system for hypertensive patients using machine learning. 2019 7th Int Conf Inf Commun Technol ICoICT 2019 [Internet]. 2019. Jul 1 [cited 2024 Apr 7]; Available from: https://www.researchgate.net/publication/335863523_A_DASH_Diet_Recommendation_System_for_Hypertensive_Patients_Using_Machine_Learning [Google Scholar]
- 48.Janssen MK, Demmers S, Srinivas SK, et al. Implementation of a text-based postpartum blood pressure monitoring program at 3 different academic sites. Am J Obstet Gynecol MFM [Internet] 2021. Nov 1 [cited 2024 Apr 7]; 3: 100446. Available from: https://pubmed.ncbi.nlm.nih.gov/34329800/ [DOI] [PubMed] [Google Scholar]
- 49.Bengtsson U, Kjellgren K, Hallberg I, et al. Patient contributions during primary care consultations for hypertension after self-reporting via a mobile phone self-management support system. Scand J Prim Health Care [Internet] 2018. Jan 2 [cited 2024 Apr 9]; 36: 70–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yeung DL, Alvarez KS, Quinones ME, et al. Low-health literacy flashcards & mobile video reinforcement to improve medication adherence in patients on oral diabetes, heart failure, and hypertension medications. J Am Pharm Assoc (2003) [Internet] 2017. Jan 1 [cited 2024 Apr 9]; 57: 30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhong D, Yian Z, Lanqing W, et al. Continuous blood pressure measurement platform: a wearable system based on multidimensional perception data. IEEE Access 2020; 8: 10147–10158. [Google Scholar]
- 52.Agnihothri S, Cui L, Rajan B, et al. Mobile health application usage and quality of care at a hypertension clinic: an observational cohort study. J Hypertens [Internet] 2021. Nov 1 [cited 2024 Apr 9]; 39: 2265–2271. [DOI] [PubMed] [Google Scholar]
- 53.Andersson U, Bengtsson U, Ranerup A, et al. Patients and Professionals as Partners in Hypertension Care: Qualitative Substudy of a Randomized Controlled Trial Using an Interactive Web-Based System Via Mobile Phone. J Med Internet Res [Internet] 2021. Jun 1 [cited 2024 Apr 9]; 23: e26143. Available from: https://pubmed.ncbi.nlm.nih.gov/34081021/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tobe SW, Yeates K, Campbell NRC, et al. Diagnosing hypertension in indigenous Canadians (DREAM-GLOBAL): a randomized controlled trial to compare the effectiveness of short message service messaging for management of hypertension: main results. J Clin Hypertens [Internet] 2019. Jan 1 [cited 2024 Apr 9]; 21: 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grant S, Hodgkinson J, Schwartz C, et al. Using mHealth for the management of hypertension in UK primary care: an embedded qualitative study of the TASMINH4 randomised controlled trial. Br J Gen Pract [Internet] 2019. Sep 1 [cited 2024 Apr 9]; 69: e612–e620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yatabe J, Yatabe MS, Ichihara A. The current state and future of internet technology-based hypertension management in Japan. Hypertens Res [Internet] 2021. Mar 1 [cited 2024 Apr 7]; 44: 276–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Villarreal V, Nielsen M, Samudio M. Sensing and storing the blood pressure measure by patients through a platform and mobile devices. Sensors (Switzerland) [Internet] 2018. Jun 3 [cited 2024 Apr 7]; 18: 1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ionov MV, Zhukova OV, Yudina YS, et al. Value-based approach to blood pressure telemonitoring and remote counseling in hypertensive patients. Blood Press [Internet] 2021. [cited 2024 Apr 7]; 30: 20–30. [DOI] [PubMed] [Google Scholar]
- 59.Kallas D, Sandhu N, Gandilo C, et al. Use of digital health technology in heart failure and diabetes: a scoping review. J Cardiovasc Transl Res [Internet] 2023. Jun 1 [cited 2024 Apr 11]; 16: 526–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Haleem A, Javaid M, Singh RPet al. et al. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sensors Int [Internet] 2021. Jan 1 [cited 2024 Apr 11]; 2: 100117. Available from: https://pubmed.ncbi.nlm.nih.gov/34806053/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen X, Zhou X, Li H, et al. The value of WeChat application in chronic diseases management in China. Comput Methods Programs Biomed 2020. Nov 1; 196: 105710. [DOI] [PubMed] [Google Scholar]
- 62.Arshed M, Zakar R, Umer MF, et al. Efficacy of mHealth and education-led peer counseling for patients with hypertension and coronary artery disease in Pakistan: study protocol for a double-blinded pragmatic randomized-controlled trial with factorial design. Trials [Internet] 2023. Dec 1 [cited 2024 Apr 15]; 24. Available from: https://pubmed.ncbi.nlm.nih.gov/37424031/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alzahrani SA, Muammar MB, Muammar AB, et al. The adoption and acceptance of mHealth interventions for self-management of hypertension among adult patients: a systematic review. Cureus [Internet] 2022. Nov 16 [cited 2024 Apr 11]; 14. Available from: https://www.cureus.com/articles/123879-the-adoption-and-acceptance-of-mhealth-interventions-for-self-management-of-hypertension-among-adult-patients-a-systematic-review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li R, Liang N, Bu Fet al. et al. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis. JMIR mHealth uHealth [Internet] 2020. Mar 1 [cited 2024 Apr 11]; 8. Available from: https://pubmed.ncbi.nlm.nih.gov/32217503/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Edwards EA, Lumsden J, Rivas C, et al. Gamification for health promotion: systematic review of behaviour change techniques in smartphone apps. BMJ Open [Internet] 2016. [cited 2024 Apr 11]; 6: e012447. Available from: https://pubmed.ncbi.nlm.nih.gov/27707829/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kassavou A, Wang M, Mirzaei V, et al. The association between smartphone app-based self-monitoring of hypertension-related behaviors and reductions in high blood pressure: systematic review and meta-analysis. JMIR mHealth uHealth [Internet] 2022. Jul 1 [cited 2024 Apr 15]; 10. Available from: /pmc/articles/PMC9328789/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wheeler TS, Michael Vallis T, Giacomantonio NBet al. et al. Feasibility and usability of an ontology-based mobile intervention for patients with hypertension. Int J Med Inform [Internet] 2018. Nov 1 [cited 2024 Apr 11]; 119: 8–16. [DOI] [PubMed] [Google Scholar]
- 68.Haramiova Z, Stasko M, Hulin M, et al. The effectiveness of daily SMS reminders in pharmaceutical care of older adults on improving patients’ adherence to antihypertensive medication (SPPA): study protocol for a randomized controlled trial. [DOI] [PMC free article] [PubMed]
- 69.World Health Organization. Global strategy on human resources for health: Workforce 2030. WHO [Internet]. 2020 [cited 2024 Apr 11];64. Available from: https://www.who.int/hrh/resources/global_strategy_workforce2030_14_print.pdf?ua=1.
- 70.Liu S, Brooks D, Thomas SG, et al. Effectiveness of user- and expert-driven web-based hypertension programs: an RCT. Am J Prev Med [Internet] 2018. Apr 1 [cited 2024 Apr 11]; 54: 576–583. [DOI] [PubMed] [Google Scholar]
- 71.Kao CW, Chen TY, Cheng SM, et al. A web-based self-titration program to control blood pressure in patients with primary hypertension: randomized controlled trial. J Med Internet Res [Internet] 2019. Dec 1 [cited 2024 Apr 11]; 21: e15836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Van Dulmen S, Sluijs E, Van Dijk L, et al. Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res [Internet] 2007. Apr 17 [cited 2024 Apr 11]; 7: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-dhj-10.1177_20552076241277172 for Mobile health technologies in the prevention and management of hypertension: A scoping review by Abdulhammed Opeyemi Babatunde, Deborah Abisola Ogundijo, Abdul-Gafar Olayemi Afolayan, Olutola Vivian Awosiku, Zainab Opeyemi Aderohunmu, Mayowa Sefiu Oguntade, Uthman Hassan Alao, Abdulrahman Ololade Oseni, Abdulqudus Abimbola Akintola and Olanrewaju Adams Amusat in DIGITAL HEALTH