Abstract
Pain is one of the most common manifestations in the postoperative stage and it has a detrimental effect on both sleep and patient satisfaction. Consequently, this integrative review seeks to identify the outcomes of pain management specifically concerning sleep quality and patient satisfaction among the patients receiving orthopedic surgeries. In a stepwise manner, peer-reviewed articles manually searched in four databases including Scopus, Science Direct, PubMed, and CINAML (Cumulated Index to Nursing and Allied Health Literature) published between 2019 and 2023 were selected. The current review finally encompassed 22 studies. The review elaborates and reaffirms the notion that pain after surgery is still a critical issue that impacts the quality of patients’ sleep as well as their overall satisfaction. Chronic sleep disturbance is generally linked with pain while other factors such as light exposure and hospital environment were found to influence sleep quality. It is thus crucial to develop clear multifaceted pain management guidelines that include patient-tailored pharmacological and non-pharmacological interventions aimed at helping patients recover better, sleep better, and be satisfied with the procedures and results.
Keywords: orthopedic surgery, postoperative care, patients satisfaction, sleep quality, pain management
Introduction and background
Pain is defined as an unpleasant experience that reduces the psychological and physical health of patients and has negative consequences such as discomfort, prolonged recovery, and the development of chronic pain [1,2]. About 300 million surgeries are performed for various reasons around the world annually [3]. However, pain after surgery is one of the most important complications that causes disability, long-term hospitalization, and financial burden [4-6]. Although protocols for postoperative pain management have evolved, pain remains an ongoing challenge to the medical community [7]. Studies indicate that pain management is affected by many factors such as gender, age, expectations before surgery, information given before surgery, type of anesthesia and medications given before surgery, and communication between staff and patients [8-10].
According to Kamphuis et al., sleep affects physical and mental health as it is considered one of the basic activities in a person's daily life [11]. Poor sleep quality is caused by several factors including psychological factors such as anxiety and stress, physical factors such as illness, severity of illness, and pain, and the hospital environment such as light and sound disturbances [12]. Sleep has an important role in inhibitory control of descending pain. Previous studies have also shown that high levels of pain after surgery, changes in behavior, and poor emotional health can lead to sleep disorders after surgery [13]. Sleep plays an important role in maintaining neuronal circuitry and maintaining overall health [14]. Various studies have found a bidirectional relationship between sleep disturbances, anxiety, and depression, suggesting that each contributes to development and is a consequence of the other [15]. The relationship between mood disorders, depression, and sleep quality remains unclear; however, sleep disturbances seem to be a risk factor for the development of depression. At the same time, depression and mood disorders are accompanied by sleep disturbances most of the time [16].
Patient satisfaction is a complex concept that is affected by many factors including economic, cultural, and social factors [17,18]. One of the pressing issues in the current field of medicine is patient satisfaction as it is an accepted measure of the quality of healthcare [19]. The overall level of patient satisfaction after anesthesia reported in different regions of the world ranges from 56.5% to 99.1% [20]. This creates large gaps between studies. Thus, this literature review focuses on postoperative pain management and its impact on sleep quality and patient satisfaction.
Review
Method
This literature review was conducted following a systematic approach. The search was conducted on four databases Scopus, Science Direct, PubMed, and CINAHL (Cumulated Index to Nursing and Allied Health Literature). Once the initial pool of literature was identified, the next step involved screening. Inclusion criteria were defined as articles (i) published in English, (ii) published between 2019 and 2023, and (iii) full-text articles following quantitative, qualitative, or mixed-method designs conducted on adult populations only.
Search Outcome
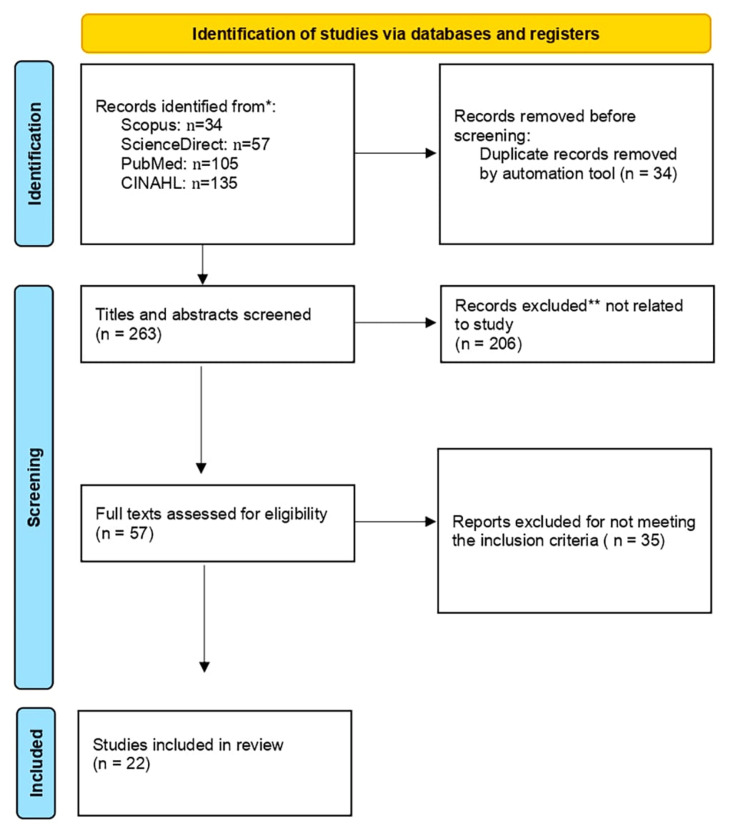
The keywords used for the search were “postoperative pain”, "sleep quality", and "patient satisfaction" by using different combinations of Boolean operators. Only original research articles were included. Further filtering was applied to reach the search results presented in Figure 1.
Figure 1. PRISMA flow diagram.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Articles not related to the topic were excluded after reviewing titles and abstracts and only related articles are mentioned herein. All articles related to orthopedic surgeries that resulted from the search were reviewed. To our knowledge and according to the search results, none of the studies reported sleep quality and patient satisfaction together in relation to postoperative pain. This makes this review the first to address these factors together.
Data Abstraction
From the 22 that were included in the final literature review, the following data were abstracted and inserted into Table 1: author and year of publication, purpose of the study, country, sample size, design, and main findings. The process of selecting the final 22 studies is outlined in Figure and the studies are listed in Table 1.
Table 1. List of studies identified through search in different databases.
| Author | Purpose | Country | Sample Size | Design | Main Findings |
| Kulpatcharapong et al. (2020) [12] | To assess the prevalence and factors related to poor sleep quality in hospital patients. | Thailand | 96 | Observational analytic study | High prevalence of poor sleep quality among hospitalized patients, with improvements during the stay; light exposure and pain were key factors. |
| Song et al. (2020) [13] | To study how surgery timing affects anesthetic needs, postoperative sleep, and pain. | China | 84 | Comparative study | Evening surgeries required fewer anesthetics but resulted in more sleep disruption compared to daytime surgeries. |
| Fetene et al. (2022) [20] | To investigate perioperative surgical patient satisfaction and its predictors in three Ethiopian hospitals. | Ethiopia | 411 | Multicenter cross-sectional study | Overall low satisfaction with perioperative anesthesia services. |
| Mouch et al. (2020) [21] | To investigate hospital sleep quality, disruptions, and aids for improvement. | United States | 195 | Mixed-method sequential explanatory study | Most patients have poor sleep quality during recovery from elective surgery, with many disruptions being modifiable. |
| Shakya et al. (2019) [22] | To examine zolpidem's effect on postoperative sleep quality, pain relief, and life quality in hip surgery patients. | China | 160 | Randomized double-blind controlled trial | Zolpidem improved pain relief, early mobility, reduced anxiety and depression, and enhanced overall perioperative experience and satisfaction. |
| Fu et al. (2022) [23] | To explore tramadol's impact on postoperative mood, anxiety, and sleep. | China | 200 | Randomized controlled trial | Tramadol effectively improved mood and sleep post-surgery, supporting its use in postoperative pain management. |
| Xiao et al. (2022) [24] | To evaluate preoperative zolpidem's impact on analgesia use and postoperative pain. | China | 88 | Randomized prospective study | Preoperative zolpidem reduced intraoperative analgesic use and postoperative pain. |
| Lee et al. (2022) [25] | To compare intermittent epidural bolus injections versus continuous injections for nighttime pain and sleep quality. | Korea | 76 | Comparative study | Intermittent epidural bolus injections reduced nighttime pain and improved sleep quality more effectively than continuous injections. |
| Shen et al. (2021) [26] | To assess improved perioperative sleep's effect on pain, analgesic use, nausea and vomiting after knee or hip surgery. | Australia | 1285 | Systematic review and meta-analysis | Better perioperative sleep significantly reduced early postoperative pain and analgesic consumption without increasing nausea and vomiting. |
| Luo et al. (2019) [27] | To explore the correlation between preoperative sleep quality and postoperative outcomes in joint arthroplasty patients. | China | 994 | Prospective cohort study | Better preoperative sleep quality improved postoperative pain threshold, reduced pain scores and analgesic use, and shortened hospital stays. |
| Boye Larsen et al. (2021) [28] | To examine the relationship between preoperative sleep quality, pain, anxiety, depression and chronic postoperative pain after joint arthroplasty. | Denmark | 185 | Secondary analysis of a randomized controlled trial | Poor preoperative sleep correlated with higher pain, anxiety, and depression, leading to worse chronic postoperative pain outcomes. |
| Liu et al. (2023) [29] | To assess postoperative pain management efficacy in China and identify factors contributing to suboptimal pain control. | China | 26193 | Cross-sectional study | Almost half of the patients experienced moderate-to-severe pain post-surgery; high rate of opioid use was reported. |
| Berkowitz et al. (2019) [30] | To measure the link between patient-reported satisfaction, regret, and clinical outcomes. | United States | 9953 | Retrospective study | Significant link between clinical outcomes and satisfaction; postoperative pain had the most impact on satisfaction and regret. |
| Peng et al. (2019) [31] | To implement a comprehensive perioperative pain management program and assess its impact on recovery and satisfaction. | China | 361 | Controlled pilot study | Stratified pain management based on risk assessment improved pain control and postoperative recovery. |
| Garvey et al. (2021) [32] | To evaluate postoperative opioid use after arthroscopic rotator cuff repair. | United States | 117 | Prospective cohort study | Effective pain control achieved with a multimodal approach after arthroscopic rotator cuff repair. |
| Terro et al. (2022) [33] | To present the results of a novel approach to laparoscopic cholecystectomy for potential adoption. | Saudi Arabia | 125 | Retrospective study | High satisfaction with pain control and cosmetic outcomes following the new laparoscopic cholecystectomy method. |
| Yunus et al. (2020) [34] | To report on perceptions and satisfaction with postoperative pain management in emergency surgeries. | Nigeria | 891 | Prospective study | Low satisfaction with pain management in emergency surgeries. |
| Belay Bizuneh et al. (2020) [35] | To assess patient satisfaction with postoperative pain management and identify associated factors. | Ethiopia | 43 | Cross-sectional study | Low satisfaction with pain management; key factors included ASA status and immediate postoperative pain presence. |
| Xu et al. (2024) [36] | To compare outcomes of patients discharged with opioid versus opioid-free pain management after surgery. | New Zealand | 4273 | International multicenter cohort study | Opioid prescriptions at discharge did not improve satisfaction but increased healthcare visits due to side effects. |
| Stambough et al. (2021) [37] | To identify factors influencing the number of postoperative narcotic refills requested after joint arthroplasty. | United States | 438 | Retrospective cohort study | More narcotic refills did not correlate with improved satisfaction; preoperative opioid and benzodiazepine use predicted prolonged narcotic use. |
| Benavent et al. (2020) [38] | To examine patient satisfaction with pain management using an opioid prescription protocol after hand surgery. | United States | 100 | Prospective survey | Patients took fewer opioids than prescribed; higher pain scores were linked to lower satisfaction with opioid use. |
| Alema et al. (2023) [39] | To evaluate determinants of patient satisfaction with postoperative pain management in a specialized Ethiopian hospital. | Ethiopia | 144 | Cross-sectional study | Highlighted the need for in-depth studies on satisfaction and the inclusion of non-pharmaceutical pain management strategies. |
Results
Characteristics of the Reviewed Studies
The reviewed studies encompass a diverse range of methodologies and focus areas related to postoperative pain, sleep quality, and patient satisfaction with pain management. A total of 22 studies were selected based on stringent inclusion criteria. These studies employed various research designs, including explanatory sequential mixed-method, analytic observational, prospective randomized controlled trials, systematic reviews, and meta-analyses. The sample sizes of the studies ranged from 43 to 26,193 participants, and they were conducted across multiple countries, including the United States, China, Australia, Ethiopia, and Denmark. The primary focus of these studies varied, but they all explored aspects of postoperative pain management, its impact on sleep quality, and patient satisfaction.
Postoperative Pain and Sleep Quality
The reviewed studies consistently indicate that postoperative pain significantly affects sleep quality in patients recovering from surgery. Mouch et al. found that most patients do not sleep well while recovering from elective surgery with most sleep disruptions being modifiable [21]. Similarly, Kulpatcharapong et al. highlighted a high prevalence of poor sleep quality in hospitalized patients which was partly improved during hospitalization [12]. Factors such as light exposure and pain were significant contributors to poor sleep quality. Studies by Shakya et al. [22], Fu et al. [23], and Xiao et al. [24] focused on pharmacological interventions to improve sleep quality and manage pain. Shakya et al. demonstrated that zolpidem, a sedative, can relieve pain, increase early range of motion and muscle strength, reduce perioperative anxiety and depression, and improve perioperative experience and satisfaction. Similarly, Fu et al. found that intravenous analgesia using tramadol effectively improved postoperative depression and sleep status in women undergoing abdominal endoscopic surgery [23]. Xiao et al. reported that improving preoperative sleep quality with zolpidem reduced intraoperative analgesic use and postoperative pain [24].
Lee et al. [25] and Shen et al. [26] investigated different pain management techniques and their impact on sleep quality. Lee et al. observed that programmed intermittent epidural bolus injections were more effective in reducing nighttime pain and improving sleep quality compared to continuous epidural injections [25]. Shen et al. conducted a systematic review and meta-analysis that confirmed improved perioperative sleep could significantly reduce pain levels at the early stage after total knee or hip arthroplasty (TKA or THA), decreasing analgesic drug consumption without increasing the incidence of postoperative nausea and vomiting [26].
Timing of surgery and its impact on sleep quality and pain was explored by Song et al., who reported that evening operations required lower dosages of anesthetic drugs but greater sleep disruption occurred when anesthesia and surgery were performed at night [13]. Luo et al. highlighted that better sleep quality before the operation improves pain threshold decreases pain score and analgesic consumption and reduces the length of stay (LOS) [27]. Studies by Boye et al. [28] and Liu et al. [29] examined the broader implications of sleep quality on pain and overall recovery. Boye et al. noted that patients with poor preoperative sleep have higher preoperative pain intensities and higher levels of pain, catastrophizing anxiety and depression [28]. Liu et al. reported that almost half of the patients suffered from moderate-to-severe pain after surgery in China with a high rate of systemic opioid use [29].
Patient Satisfaction with Postoperative Pain Management
Patient satisfaction with pain management is influenced by various factors including the effectiveness of pain control methods and the management of side effects. Berkowitz et al. found a strong association between patients' clinical outcomes and their satisfaction with postoperative pain being a critical determinant [30]. As reported by several researchers, personalized pain management approach has a role in increasing patient satisfaction. In a study by Peng et al., it was shown that a stratified approach to pain management through risk assessment enhanced the efficacy of analgesics thereby improving postoperative recovery and patient satisfaction [31]. Satisfactory pain control was achieved by Garvey et al. with a multimodal approach in patients following arthroscopic rotator cuff repair in 2021 [32]. The postoperative satisfaction of the patient with pain control and cosmetic appearance in a new approach to laparoscopic cholecystectomy was very much beyond expectation as unraveled by Terro et al. [33]. On the other hand, patient satisfaction seems very low in some regions based on studies conducted by Yunus et al. [33], Liu et al. [29], and Belay Bizuneh et al. [35], calling for improved standards in the current pain management protocols. Yunus et al. [34] noted dissatisfaction in pain management specifically among subjects who had gone through emergency surgeries while Belay Bizuneh et al. [35] reported low levels of satisfaction influenced by other factors such as American Society of Anesthesiologists (ASA) status and the presence of pain immediately after operation.
Xu et al. [36] and Stambough et al. [37] explored the implications of opioid use on patient satisfaction. Xu et al. noted that opioid prescribing at surgical discharge is not associated with reduced patient satisfaction but with increased risk of presentation to healthcare due to side effects [36]. Stambough et al. added that more postoperative narcotic refills after total joint arthroplasty do not improve patient satisfaction and preoperative opioid and benzodiazepine use are associated with prolonged narcotic use [37]. Benavent et al. reported that patients consumed fewer opioid pills than prescribed and those who took more opioid pills had higher pain scores and lower satisfaction [38]. Similarly, Alema et al. highlighted the need for future in-depth studies on patient satisfaction and the lack of inclusiveness of non-pharmaceutical interventions in pain management strategies [39]. Fetene et al. found that overall patient satisfaction toward perioperative anesthesia service was low, indicating room for improvement in pain management practices [20].
Discussion
The integrative review shows the critical interaction of postoperative pain management, sleep quality, and patient satisfaction. Effective postoperative pain management is essential not just for pain relief but also for sound sleep quality, which is critical for better recovery and well-being of patients.
Postoperative Pain and Sleep Quality
A number of studies have shown that poorly managed postoperative pain disrupts sleep quality to a great extent. For example, Mouch et al. [21] and Kulpatcharapong et al. [12] revealed that postoperatively, pain and other modifiable factors such as light exposure may contribute to poor sleep quality. These observations are in line with more general literature that posits that pain can disrupt sleep and can bring about fragmented and less restorative sleep. Earlier studies by Chou et al. demonstrated that postoperative pain can cause poor quality of sleep, which in turn can encourage sensitivity to pain and thus create a circular pattern of poor sleep and hyperalgesia [40].
Pharmacological treatments have shown positive results in both conditions. Studies by Shakya et al. [22] and Fu et al. [23] have already proved that zolpidem or tramadol can improve sleep quality and concomitantly reduce pain. Such a dual benefit will be significant because restorative sleep might accelerate the process of healing while at the same time reducing the overall perception of pain as suggested by Tang et al. [41]. Enhancing preoperative sleep has demonstrated effectiveness in reducing postoperative pain as a programmed intermittent epidural bolus injection strategy during surgery works to reduce postoperative pain. These two strategies underline an all-encompassing approach to pain management from the preoperative, intraoperative, and postoperative phases. Non-pharmacologic approaches including cognitive behavioral therapy for insomnia (CBT-I) have been proven effective in managing sleep disturbances among patients suffering from chronic pain and therefore may offer an edge in the postoperative period among the same patients [41].
Satisfaction with Pain Management
Patient satisfaction is an outcome dependent on the methods of control management of side effects and personalization of strategies used for pain. According to Berkowitz et al., the link between clinical outcomes and patient satisfaction stands strong meaning effective pain management remains a crucial determinant of patient satisfaction [30]. This finding supports the study by Rahmqvist and Bara, who found that pain management quality is directly proportional to overall patient satisfaction within hospital settings [42]. Effective action regarding the personalization of pain management strategies has been reflected as a point that increases levels of patient satisfaction in several studies. For example, Peng et al. showed that a stratified approach to pain management developed from risk assessment levels increased analgesic success levels and postoperative recovery increasing patient satisfaction [31]. Effective pain management was successful using a multimodal method in patients after arthroscopic rotator cuff repair as seen in the study by Garvey et al. [32]. These findings agree with those of Chou et al., who also put forward multimodal analgesia as the optimal choice for adequate pain control because it reduces the intensity of pain and the use of opioids [40].
Nevertheless, as shown in various studies, patient satisfaction with pain management is still rated at a low level in several areas. Yunus et al. [34] and Liu et al. [29] found significant inadequacies in the satisfaction of patients from pain management. Both studies showed the necessity for developing universal protocols for the management of pain which could be implemented in various healthcare settings. According to Gan et al. [43], despite achievements that have been made in pain management after surgery there are too many cases in which patients feel inadequate anesthesia. Of particular significance is that opioid use impacts the satisfaction of the patient. Most of such patients are discharged with an opioid prescription that increases the risk of side effects which reduces patient satisfaction. This calls for balanced strategies in pain management with minimal use of opioids in favor of multimodal approaches in the management of pain. Hill et al. support this showing that reducing opioid prescriptions does not compromise pain control and can improve overall patient satisfaction [44].
Conclusions
The current review emphasizes the need to create and implement effective and all-inclusive pain management protocols that will decrease the intensity of pain, improve sleep quality, and assure the satisfaction of the patient. The implementation of such protocols is likely to result in better postoperative outcomes, reduced hospital stays, and overall improved patient experience. Healthcare providers can significantly improve their quality of care for postoperative patients when the interconnection of pain, sleep, and satisfaction is addressed.
Future research should build and implement comprehensive protocols for managing pain that look at the multi-facets of pain and its effects on sleep quality and satisfaction. In this way, it is necessary to have protocols that combine the pharmacological and non-pharmacological interventions according to the needs of each patient. More studies should be done to look at how improved sleep might have long-term consequences relative to the postoperative recovery and satisfaction of patients. The level of postoperative care offered across regions will be standardized if the application of the standard guidelines in managing pain becomes a reality in all areas through the training of health workers involved in care delivery and monitoring. With such training, there will be improvements in the general quality of care.
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Omar M. Alqaisi, Suhair Al-Ghabeesh
Acquisition, analysis, or interpretation of data: Omar M. Alqaisi, Suhair Al-Ghabeesh
Drafting of the manuscript: Omar M. Alqaisi, Suhair Al-Ghabeesh
Critical review of the manuscript for important intellectual content: Omar M. Alqaisi, Suhair Al-Ghabeesh
Supervision: Suhair Al-Ghabeesh
References
- 1.Improving the management of post-operative acute pain: priorities for change. Meissner W, Coluzzi F, Fletcher D, et al. Curr Med Res Opin. 2015;31:2131–2143. doi: 10.1185/03007995.2015.1092122. [DOI] [PubMed] [Google Scholar]
- 2.Barriers to effective pain management in cancer patients from the perspective of patients and family caregivers: a qualitative study. Al-Ghabeesh SH, Bashayreh IH, Saifan AR, Rayan A, Alshraifeen AA. Pain Manag Nurs. 2020;21:238–244. doi: 10.1016/j.pmn.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 3.Topical ambroxol for the treatment of neuropathic pain. An initial clinical observation. Kern KU, Weiser T. Schmerz. 2015;29:0–96. doi: 10.1007/s00482-015-0060-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.No evidence of real progress in treatment of acute pain, 1993-2012: scientometric analysis. Correll DJ, Vlassakov KV, Kissin I. J Pain Res. 2014;7:199–210. doi: 10.2147/JPR.S60842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Recent advances in postoperative pain management. Vadivelu N, Mitra S, Narayan D. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2844689/ Yale J Biol Med. 2010;83:11–25. [PMC free article] [PubMed] [Google Scholar]
- 6.Evaluating and identifying predictors of emotional well-being in nursing students in Jordan: a cross-sectional study. Al-Sagarat AY, al Hadid LA, Tapsell A, Moxham L, Al Barmawi M, Khalifeh AH. Adv Ment Health. 2022;20:242–252. [Google Scholar]
- 7.Multifactorial preoperative predictors for postcesarean section pain and analgesic requirement. Pan PH, Coghill R, Houle TT, et al. Anesthesiology. 2006;104:417–425. doi: 10.1097/00000542-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 8.The impact of preoperative information on state anxiety postoperative pain and satisfaction with pain management. Sjöling M, Nordahl G, Olofsson N, et al. Patient Educ Couns. 2003;51:169–176. doi: 10.1016/s0738-3991(02)00191-x. [DOI] [PubMed] [Google Scholar]
- 9.Patient satisfaction with postoperative pain management--effect of preoperative factors. Niemi-Murola L, Pöyhiä R, Onkinen K, Rhen B, Mäkelä A, Niemi TT. Pain Manag Nurs. 2007;8:122–129. doi: 10.1016/j.pmn.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Assessment of nutritional status in the critically Ill. Narayan SK, Gudivada KK, Krishna B. Indian J Crit Care Med. 2020;24:0–6. doi: 10.5005/jp-journals-10071-23617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poor sleep as a potential causal factor in aggression and violence. Kamphuis J, Meerlo P, Koolhaas JM, Lancel M. Sleep Med. 2012;13:327–334. doi: 10.1016/j.sleep.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Sleep quality of hospitalized patients, contributing factors, and prevalence of associated disorders. Kulpatcharapong S, Chewcharat P, Ruxrungtham K, et al. Sleep Disord. 2020;2020:8518396. doi: 10.1155/2020/8518396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Comparison of morning and evening operation under general anesthesia on intraoperative anesthetic requirement, postoperative sleep quality, and pain: a randomized controlled trial. Song B, Li Y, Teng X, Li X, Yang Y, Zhu J. Nat Sci Sleep. 2020;12:467–475. doi: 10.2147/NSS.S257896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sleep deprivation and neurological disorders. Bishir M, Bhat A, Essa MM, et al. Biomed Res Int. 2020;2020:5764017. doi: 10.1155/2020/5764017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Alvaro PK, Roberts RM, Harris JK. Sleep. 2013;36:1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sleep patterns and the risk for unipolar depression: a review. Wiebe ST, Cassoff J, Gruber R. Nat Sci Sleep. 2012;4:63–71. doi: 10.2147/NSS.S23490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patient satisfaction with peri-operative anesthesia care and associated factors at two National Referral Hospitals: a cross sectional study in Eritrea. Andemeskel YM, Elsholz T, Gebreyohannes G, Tesfamariam EH. BMC Health Serv Res. 2019;19:669. doi: 10.1186/s12913-019-4499-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patient satisfaction with perioperative care among patients having orthopedic surgery in a university hospital. Jlala HA, Caljouw MA, Bedforth NM, Hardman JG. Local Reg Anesth. 2010;3:49–55. doi: 10.2147/lra.s11381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patient satisfaction. Prakash B. J Cutan Aesthet Surg. 2010;3:151–155. doi: 10.4103/0974-2077.74491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perioperative patient satisfaction and its predictors following surgery and anesthesia services in North Shewa, Ethiopia. A multicenter prospective cross-sectional study. Fetene MB, Bayable SD, Wendimu ES, Belehu KD, Almaw AA, Dula PK, Bejiga BZ. Ann Med Surg (Lond) 2022;76:103478. doi: 10.1016/j.amsu.2022.103478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sleep patterns and quality among inpatients recovering from elective surgery: a mixed-method study. Mouch CA, Baskin AS, Yearling R, Miller J, Dossett LA. J Surg Res. 2020;254:268–274. doi: 10.1016/j.jss.2020.04.032. [DOI] [PubMed] [Google Scholar]
- 22.Prospective randomized controlled study on improving sleep quality and impact of zolpidem after total hip arthroplasty. Shakya H, Wang D, Zhou K, Luo ZY, Dahal S, Zhou ZK. J Orthop Surg Res. 2019;14:289. doi: 10.1186/s13018-019-1327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Effects of intravenous analgesia using tramadol on postoperative depression state and sleep quality in women undergoing abdominal endoscopic surgery: a randomized controlled trial. Fu M, Chen S, Xu R, et al. Drug Des Devel Ther. 2022;16:1289–1300. doi: 10.2147/DDDT.S357773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The effect of improving preoperative sleep quality on perioperative pain by zolpidem in patients undergoing laparoscopic colorectal surgery: a prospective, randomized study. Xiao Z, Long B, Zhao Z. Pain Res Manag. 2022;2022:3154780. doi: 10.1155/2022/3154780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Comparison of programmed intermittent epidural bolus injection and continuous epidural injection in controlling nighttime pain and improving sleep quality after thoracotomy. Lee SS, Baek JH, Park SJ, Kim HJ, Kim HY, Byeon GJ. Medicine (Baltimore) 2022;101:0. doi: 10.1097/MD.0000000000031684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Improved perioperative sleep quality or quantity reduces pain after total hip or knee arthroplasty: a systematic review and meta-analysis. Shen SP, Wang YJ, Zhang Q, Qiang H, Weng XS. Orthop Surg. 2021;13:1389–1397. doi: 10.1111/os.12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Preoperative sleep quality affects postoperative pain and function after total joint arthroplasty: a prospective cohort study. Luo ZY, Li LL, Wang D, Wang HY, Pei FX, Zhou ZK. J Orthop Surg Res. 2019;14:378. doi: 10.1186/s13018-019-1446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The association between sleep quality, preoperative risk factors for chronic postoperative pain and postoperative pain intensity 12 months after knee and hip arthroplasty. Boye Larsen D, Laursen M, Simonsen O, Arendt-Nielsen L, Petersen KK. Br J Pain. 2021;15:486–496. doi: 10.1177/20494637211005803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Postoperative pain-related outcomes and perioperative pain management in China: a population-based study. Liu Y, Xiao S, Yang H, et al. Lancet Reg Health West Pac. 2023;39:100822. doi: 10.1016/j.lanwpc.2023.100822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The impact of complications and pain on patient satisfaction. Berkowitz R, Vu J, Brummett C, Waljee J, Englesbe M, Howard R. Ann Surg. 2021;273:1127–1134. doi: 10.1097/SLA.0000000000003621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stratified pain management counseling and implementation improving patient satisfaction: a prospective, pilot study. Peng LH, Min S, Jin JY, Wang WJ. Chin Med J (Engl) 2019;132:2812–2819. doi: 10.1097/CM9.0000000000000540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Satisfactory pain management with minimal opioid use after arthroscopic rotator cuff repair. Garvey KD, Lowenstein NA, Piana LE, Arant KR, Chang Y, Matzkin EG. Arthrosc Sports Med Rehabil. 2021;3:0–7. doi: 10.1016/j.asmr.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.A retrospective cohort report of single-incision laparoscopic cholecystectomies in Saudi Arabia: postoperative outcomes and patient satisfaction. Terro K, Baroudi M, Alsaoud R, Sabbah BN, Abunimer A, Abduljawad S, Al-Shanafey S. Ann Med Surg (Lond) 2022;81:104245. doi: 10.1016/j.amsu.2022.104245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Postoperative pain management in emergency surgeries: a one-year survey on perception and satisfaction among surgical patients. Yunus AA, Ugwu EM, Ali Y, Olagunju G. Niger J Surg. 2020;26:42–47. doi: 10.4103/njs.NJS_18_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Assessment of patient's satisfaction and associated factors regarding postoperative pain management at the University of Gondar Compressive Specialized Hospital, Northwest Ethiopia. Belay Bizuneh Y, Fitiwi Lema G, Yilkal Fentie D, Woldegerima Berhe Y, Enyew Ashagrie H. Pain Res Manag. 2020;2020:8834807. doi: 10.1155/2020/8834807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Impact of opioid-free analgesia on pain severity and patient satisfaction after discharge from surgery: multispecialty, prospective cohort study in 25 countries. Br J Surg. 2024;111 doi: 10.1093/bjs/znad421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Narcotic refills and patient satisfaction with pain control after total joint arthroplasty. Stambough JB, Hui R, Siegel ER, Edwards PK, Barnes CL, Mears SC. J Arthroplasty. 2021;36:454–461. doi: 10.1016/j.arth.2020.07.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patient satisfaction and opioid use with a postoperative opioid protocol after common hand procedures. Benavent KA, Altschul ND, Lincoln LF, Chruscielski CM, Kennedy KF, Earp BE. J Hand Surg Glob Online. 2020;2:191–195. doi: 10.1016/j.jhsg.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patients' satisfaction with post-operative pain management in Ayder Comprehensive Specialized Hospital, Ethiopia: a cross-sectional study. Alema NM, Asgedom SW, Welegebrial BG, et al. Pan Afr Med J. 2023;45:94. doi: 10.11604/pamj.2023.45.94.22563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Postoperative sleep disruptions: a potential catalyst of acute pain? Chouchou F, Khoury S, Chauny JM, Denis R, Lavigne GJ. Sleep Med Rev. 2014;18:273–282. doi: 10.1016/j.smrv.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 41.Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. Tang NK, Wright KJ, Salkovskis PM. J Sleep Res. 2007;16:85–95. doi: 10.1111/j.1365-2869.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- 42.Patient characteristics and quality dimensions related to patient satisfaction. Rahmqvist M, Bara AC. Int J Qual Health Care. 2010;22:86–92. doi: 10.1093/intqhc/mzq009. [DOI] [PubMed] [Google Scholar]
- 43.Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Curr Med Res Opin. 2014;30:149–160. doi: 10.1185/03007995.2013.860019. [DOI] [PubMed] [Google Scholar]
- 44.An educational intervention decreases opioid prescribing after general surgical operations. Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ Jr. Ann Surg. 2018;267:468–472. doi: 10.1097/SLA.0000000000002198. [DOI] [PubMed] [Google Scholar]