Abstract
High sensitivity C-reactive protein (hsCRP) has been evaluated as a biomarker in stroke and relevant pathological diseases. While its predictive values in several pathological phenotypes have been confirmed, controversy exists among different studies. This review summarizes reports of the predictive values of hsCRP for the diagnosis, etiology, prognosis and mortality of stroke diseases. The current literature suggests that CRP expression is influenced by multiple factors, such as polymorphisms, the genomic backgrounds and gender. However, few reported studies analyzed data based on all these multiple factors. Future studies should focus on comprehensive analysis based on multiple factors.
Keywords: Atherosclerosis, High sensitivity C-reactive protein (hsCRP), Ischemic, Polymorphism, Predictability, Stroke
1. Introduction
Stroke is a major cerebrovascular disease threatening human health and life with high morbidity, disability and mortality [1]. According to the data from Global Burden of Disease Study [2], worldwide in 2010 there were an estimated 11,569,538 incident ischemic strokes and 5,324,997 events of incident hemorrhagic stroke; furthermore, 2,835,419 individuals died from ischemic stroke and 3,038,763 from hemorrhagic stroke. Stroke is the number cause of the death in several countries such as China [3]. Stroke was defined as a sudden onset of loss of global or focal cerebral function persisting for more than 24 h [4]. Biomarkers that predict the occurrence and outcome from ischemic stroke are critical for prevention and treatment. Serum biomarkers are considered to be the most valuable adjunct to routine clinical examination and imaging data [5]. Inflammation has an important role in the development of atherosclerosis and during the ischemic event. Inflammatory markers such as fibrinogen and hsCRP have been reported as a predictable marker for the stroke severity and outcome [6]. It has been reported that it is possible to use the increase in the concentration of acute phase reactants especially the hsCRP to help predict cerebrovascular mortality [7].
Human CRP (Pentraxin 1, Ptx1) is an acute phase reactant that is rapidly produced by the liver after tissue injury or infection [5,7]. CRP is a sensitive indicator of inflammation [8,9]. Although many inflammatory biomarkers have been reported to be useful in predicting clinical outcome after stroke, hsCRP remains one of the most widely used in clinical practice [8–12]. Increased hsCRP has been associated with the development of atherosclerosis, ischaemic attacks, hemorrhagic stroke, as well as disease outcomes [13–17]. Studies suggest that post-stroke inflammatory responses may exacerbate tissue damage after cerebral infarction and affect clinical outcomes [18,19]. Recent studies have shown that elevated hsCRP values independently predict the risk of future cardiovascular diseases and ischemic cerebrovascular diseases, including transient ischemic attack in the elderly [20–22]. After acute ischemic stroke (AIS), a sustained inflammatory response indicated by increased level of CRP has been reported in about 75% of patients. A strong and persistent inflammatory response is associated with a worse outcome. Moreover, CRP at discharge has been shown to be related to a 1-year outcome [23–25]. Recently, a meta-analysis suggested that elevated baseline hsCRP levels are independently associated with excessive ischemic stroke risk.
However, the physiologic role of CRP is not well understood; it potentially has anti-inflammatory properties as well as proinflammatory effects [26]. Inflammation may not only be the consequence of brain infarction, it may also contribute to ischemic damage. In addition, the role of inflammatory markers in predicting functional outcome in stroke remains controversial [27]. This review summarizes the data on the predictive value of hsCRP for ischemic stroke, analyzes the potential influence of CRP on functional outcomes, and identifies the critical issues that are important for the future studies.
2. CRP
CRP (protein CRP) is named because of its precipitation reaction with phosphocholine moiety of pneumococcal cell wall C-polysaccharide. According to the information on Ensembl data base (http://useast.ensembl.org/Homo_sapiens/Gene/Summary?db=core;g=ENSG00000132693;r=1:159712289-159714589), the CRP gene is located on human chromosome 1, between 159,712,289 and 159,714,589 bps. It has 7 transcripts, of which 5 encode proteins. Although the detailed functions of these protein variants are not fully known, the protein with 224 aa produced by the CRP-001transcriptis commonly known as the CRP protein. The protein is a member of the pentraxin family of proteins. The pentraxins are an ancient family of proteins with a unique architecture found as far back in evolution as the Horseshoe crab. CRP structure is strong phylogenetic conservation and high resistance to proteolysis [28]. Therefore, it is relative stable and easy to be measured.
Expression of CRP is regulated mainly at the transcriptional level by cytokines such as interleukin-1, interleukin-6, and tumor necrosis factor; among them, interleukin-6 is the primary circulating physiologic mediator [26]. Recent studies have examined the effects of IL-1β, the IL-1 receptor antagonist anakinra and the IL-6 receptor blocker tocilizumab on the regulation of expression of CRP [29]. An estimation suggests that inter-individual variation in blood CRP level is 35–40% heritable [30] and it is affected by gene polymorphisms. The expression of CRP is also influenced by environmental factors such as bacterial infection and injury. Plasma CRP concentrations increase rapidly and dramatically (100-fold or more) in response to tissue injury or inflammation. Therefore, high levels of CRP (10–1000 mg/L), are associated with serious infections or inflammatory diseases such as arthritis. The hsCRP, on the other hand, measures CRP in the low range, from 0.5 to 10 mg/L. At such range, the hsCRP test is used to identify low but persistent levels of inflammation. The hsCRP is more precise than standard CRP when measuring baseline concentrations. Induction of an hsCRP is rapid and its half-life is long enough in the blood for a steady time course. Therefore, plasma hsCRP is very useful for the diagnostic workup of inflammatory and infectious diseases [26].
3. HsCRP level in early diagnosis of stroke
At present, the diagnosis of stroke depends on clinical examination and neuro-imaging techniques [31]. It is critically important to identify effective biomarkers for the early diagnosis of acute stroke and to establish biological procedures for early diagnosis [5]. Early studies of different populations suggested that modest elevation of hsCRP is a predictor of future vascular events in apparently healthy individuals [32,33]. However, there are few data on the value of hsCRP for the early diagnosis of ischemic stroke.
In 2012, Youn et al. reported in the Keran population that higher hsCRP levels were associated with larger infarct volumes in AIS (Table 1) [26]. Their results suggest that elevated hsCRP levels may serve as a helpful serologic marker in the evaluation of the severity of AIS [34]. Kanai et al. investigated the reciprocal association between serum levels of hsCRP (Table 1) and intercellular adhesion molecule-1 (sICAM-1) and the risk of brain infarction in type 2 diabetic patients [18]. Their study suggests that both measurements of hsCRP and sICAM-1 levels are useful as a predictor of future stroke in diabetic subjects [34]. However, these studies are in Asian population. These findings have not been confirmed in the other regions such as US and European countries.
Table 1.
Potential clinical applications of hsCRP level reported in literature.
| Studies | Phenotype | CRP changes | Effect and/or description |
|---|---|---|---|
| Xie et al. [13] | Atherosclerosis | Significantly high | Patients with ICAO (internal carotid artery occlusion), MCAO (middle cerebral artery occlusion) and ICAO + MCAO had significantly higher serum hsCRP concentrations |
| Youn et al. [26] | Early diagnosis | High | Serve as a helpful serologic marker in the evaluation of the severity of AIS |
| Kanai et al. [34] | >0.83 mg/L | Measurement the risk of brain infarction in type 2 diabetic patients | |
| Li et al. [48] | Death risk | High | Independent predictor of long-term mortality after ischemic stroke in a Chinese sample |
| Chan et al. [52] | >3.4 mg/L | Most significant independent predictor of both short- and long-term mortality after stroke | |
| Huang et al. [50] | >3.0 mg/L | Elevated plasma hsCRP independently predicted risk of all-cause death within 3 months after acute IS in Chinese patients | |
| Makita et al. [12] | High | CRP levels can be used to predict future ischemic stroke and mortality in Japanese men from the general population, independently from traditional cardiovascular risk factors | |
| Tu et al. [49] | High | Independent predictors of short-term outcome and mortality after AIS | |
| Elkind et al. [53] | High | Increase with stroke severity and may be associated with mortality to a greater degree than recurrence | |
| Liu et al. [58] | Etiological subtypes of IS | >6.96 mg/L | Different among the subtypes and were the highest in CE(cardioembolism), followed by LAA(large-artery atherosclerosis) and SAA (small-artery occlusion) |
| Ozkan et al. [27] | Prognosis | >0.5 mg/dL | Predict functional disability 3 months after stroke onset |
| Gong et al. [60] | >3.0 mg/L | Elevated hsCRP independently predicts 1-year poor outcome in acute stroke | |
| Park et al. [74] | High | hsCRP levels, along with MMP-9, TIMP-1 may be useful in the diagnosis of ischemic stroke patients | |
| Yeh et al. [40] | High | Serum level of hsCRP during both acute and convalescent phases was significantly and independently predictive of 90-day MANE (major adverse neurological event) | |
| Youn et al. [26] | Higher | Reflecting a large volume of infarct, may serve as a helpful serologic marker in the evaluation of severity of acute ischemic stroke | |
| Roudbary et al. [17] | Hemorrhagic stroke | Average About 10.7906 mg/L | hsCRP level is increase in patients with Ischemic infarct dramatically but not in hemorrhagic stroke which might be considered as a usefully adjunct method for determining type of stroke in patients with cerebrovascular problems |
4. HsCRP in the prediction of atherosclerosis—artery stenosis or occlusion
Ischaemic stroke accounts for 70–80% of all cases of stroke [35]. Ischaemic stroke is mainly caused by atherosclerosis and thrombotic obstruction of cerebral blood flow (Table 1) [36,37]. Atherosclerosis, as a complex and systemic disease, may unequally induce intracranial stenosis, which may in turn impose the limitation of particular inflammatory mediator in describing atherosclerosis [38,39]. Middle cerebral artery stenosis is also associated with advanced age, hypertension, diabetes mellitus and hyperlipidaemia. The risk of stroke increases with the prevalence of atherosclerosis. Therefore, identification of biomarkers for atherosclerosis—artery stenosis or occlusion is essential for the early prevention of stroke. Considerable studies have already shown that an elevated serum CRP level reflects an increased tendency for plaque rupture and a high atherosclerotic burden [13,32,33,40–42].
In 2011, Whiteley et al. showed that higher levels of hsCRP, along with IL-6 and fibrinogen measured after stroke onset in 817 patients are significantly associated with increased incidence of occlusive vascular events and vascular death, as well as nonvascular causes of death after stroke [43]. In a prospectively study of intracranial large artery atherosclerosis progression in 25 of 75 patients using transcranial Doppler follow-up during a median follow-up time of 23 months, Arenillas et al. reported that hsCRP and plasminogen activator inhibitor-1 measured 3 months after onset of ischemic stroke are highly predictive of intracranial large artery atherosclerosis progression [44]. Similarly, Yoshida et al. showed that CRP, along with IL-6 and protein-conjugated acrolein (PC-Acro) is the risk factor for carotid atherosclerosis [45]. In a study on the transcription levels of ABCA1, ABCG1 and SR–BI and plasma CRP in Chinese populations with various risk factors for atherosclerosis, Li et al. reported that circulating CRP was increased almost in all the risk populations except in males [46]. Similarly, hsCRP and Lp-PLA2 was found to improve ischemic stroke risk prediction in the Atherosclerosis Risk in Communities study [47].
At the same time, there are also negative reports. In a study of the association between inflammatory biomarkers and progression of intracranial large artery stenosis after ischemic stroke, Shimizu and colleagues reported that the Cox proportional hazard analysis did not show a significant association between hsCRP and intracranial large artery atherosclerosis progression. The authors concluded that, because the effects of inflammatory factors may continuously affect the vessel walls during the post stroke period, the biomarkers may be more predictive in the chronic rather than the acute stage of stroke and may be important for ILA progression [41]. In a study of the influence of polyvascular atherothrombotic disease on stroke patient prognosis, its relation with inflammatory markers and the progression of atherothrombotic disease, Blanco et al. found a non-significant trend to higher hsCRP levels in patients with vascular recurrences [19]. The authors explained that this is possibly because the calculation of the sample size was based on incorrect assumptions regarding IL-6 levels [42].
The above data suggest that the hsCRP is associated with the progression of atherosclerosis and possibly with artery stenosis or occlusion. The failure to detect significant relationship between hsCRP and the progression of atherosclerosis may be due to limited sample size.
5. hsCRP and death risk
An early risk assessment of the severity of disease and prognosis using biomarkers is pivotal for optimized care and the allocation of healthcare resources [48]. The predictability of death risk for the stroke patients by hsCRP has been evaluated extensively (Table 1). Current research indicated that expression of hsCRP can be used to predict mortality from as short as three months to as long as 5 year.
At least two studies have evaluated the value of hsCRP for predicting the risk of early death of stroke patients. In a prospective study of 189 patients with AIS who were admitted within 24 h after the onset of symptoms, Tu et al. measured short-term functional outcome by the modified Rankin scale (mRS), 90 days after admission. They concluded that hsCRP was independent predictor of short-term outcome and mortality (Table 1) after AIS [49]. Huang et al. (Table 1) found that elevated plasma hsCRP independently predicted risk of all-cause death within 3 months after acute stroke in Chinese patients. Compared with low hsCRP, patients with high hsCRP (>3 mg/L) (Table 1) had a significantly higher rate of all-cause death (0.71% vs. 10.00%; p < 0.001) at 3 months after stroke onset [50]. Their study suggests that the level of hsCRP is a better predictor of risk of death than for disease relapse. These studies suggest that shortly after the onset of AIS, increased CRP levels may reflect an accompanying inflammatory reaction. Elevated CRP levels may reflect the extent of brain injury. Therefore, the elevated level of hsCRP can predict the risk of early death of stroke patients.
Li and Liu prospectively studied one year outcomes in 374 patients with ischemic stroke who were admitted within 24 h after the onset of symptoms. They measured serum levels of PCT, hsCRP and NIH stroke scale of the patients at the time of admission. Clinical follow-up was performed at 1 year. Their data showed that hsCRP on admission was independent predictor of 1 year mortality with an adjusted hazard ratio of 15.37 (95% confidence interval [CI], 3.25–41.08) [48].
Several prospective studies have demonstrated that high hsCRP was an independent predictor of long-term mortality in patients with stroke. Idicula et al. (Table 1) prospectively studied 498 patients with ischemic stroke who were admitted within 24 h after the onset of symptoms [51]. Their investigation indicated that elevated hsCRP concentration was an independent predictor of long-term mortality over a period of 2.5 years after ischemic stroke (p = 0.002). Their results also suggested that hsCRP concentration was also an independent predictor of short-term mortality after supratentorial intracerebral hemorrhage [51]. From a prospective cohort study, Makita et al. (Table 1) found that baseline serum hsCRP level was an independent predictor for future ischemic stroke and all-cause mortality in apparently healthy Japanese men. In their study, the mean follow-up period was 2.7 years [12].
The 5-year is the longest reported follow-up period. Chan et al. [52] investigated biomarkers of various pathophysiologic pathways including hsCRP with mortality in stroke patients (Table 1). During the 5-year follow-up, the mortality was 37.0% (34 out of 92). Authors concluded that hsCRP was the most significant independent predictor of both short- and long-term mortality after stroke. Mitchell et al. [53] admitted 467 patients with first ischemic stroke; at 5-year follow-up, they concluded that hsCRP was associated with risk of death. Similarly, several other reports have suggested that increased hsCRP level is associated with high risk of death stroke patients with variety of mortality rate. These studies included Hartmann et al. (41.0% mortality rate) [54], Whiting et al. (60.0% mortality rate) [55], Kammersgaard et al. (58.4%) [56], and Putaala et al. (10.7%) [57].
At present, hsCRP is probably the only independent prognostic factors in predicting both short- and long-term mortality.
6. Application in etiological subtypes of ischemics stroke
Like many known disease, ischemic stroke is a group of diseases with many different etiologies. At present, precise etiological classification depends heavily on the results of auxiliary examination. However, most of these examinations are difficult to complete at the early onset of a stroke because of the emergency nature of the disease. Based on the TOAST etiology classification system, ischemic stroke is divided into five categories (Table 1): largeartery atherosclerosis (LAA), cardioembolism (CE), small-artery occlusion (SAA), stroke of other determined etiology (SOE), and stroke of undetermined etiology (SUE) [58,59]. As hsCRP levels vary in apparently healthy population and in stroke patients, it might be a useful marker for the ischemic stroke classification. Liu et al. found that hsCRP and D-dimer levels were significantly different among the subtypes and were the highest in CE (cardioembolism). Using the data, hsCRP > 6.96 mg/L was classified as the CE subtype, with a sensitivity of 41% and a specificity of 74% [58]. The authors suggested that using a combination of hsCRP and DD may improve the diagnostic accuracy of CE in the acute phase [58]. Future studies on this aspect will improve the classification of the of stroke subtypes.
7. hsCRP and prognosis
CRP levels strongly correlate with stroke severity and independently predict mortality and stroke recurrence in AIS patients (Table 1) [60], but only hsCRP is an independent predictor for unfavorable outcome [61]. The level of hsCRP can predict the severity of AIS patients. By examining the level of hsCRP in 316 patients with AIS, Luo et al. found that elevated CRP level can reflect the severity of AIS [61].
The different time points of blood sampling for the measurement of hsCRP levels are also studied. Yeh et al. studies the hsCRP levels during both acute and convalescent phases of 160 patients [27]. They found that Hs-CRP levels during both acute phase and convalescent phase of IS were significantly and independently predictive of 90-day major adverse neurological event (MANE) [27]. Authors also found that circulating level of hsCRP at 48 h was better than the level at day 21 after acute IS for predictive of 90-day MANE [27]. Their finding supports the validity of using serum hsCRP level in predicting clinical outcome in patients with and without IS regardless of the timing for blood sampling [27].
During the subacute phase of stroke, hsCRP values are associated with the level of functional disability. Song et al. examined the hsCRP level in a total of 309 patients with first-ever stroke within 24 h after symptom onset [62]. The hsCRP measurements were made at admission and on the seventh hospital day. Their study showed that both hsCRP values on admission and on the seventh hospital day were significantly correlated with modified Rankin Scale (mRS) scores obtained at 4 times after the onset of stroke. Authors suggest that hsCRP values on the subacute phase have sufficient value as predictors of the prognosis of functional disability after first-ever stroke [62].
However, the prognostic value of hsCRP on stroke has its limitations. Elkind et al. found that, after adjusting for confounders, hsCRP was not associated with risk of recurrent stroke or recurrent stroke, myocardial infarction, or vascular death but was associated with risk of death [53]. In a study to investigate the association between the progression of silent cerebral infarction (SCI) and levels of soluble adhesion molecules and high-sensitivity C-reactive protein (hsCRP) in type 2 diabetic patients, Kawamura et al. reported that hsCRP was not associated with the progression of SCI. By examining the hsCRP and ferritin levels of 62 patients prospectively within 48 h after onset of ischemic stroke, Ozkan et al. (Table 1) reported that neither hsCRP nor ferritin levels could predict functional disability 3 months after stroke onset [27].
8. CRP and hemorrhageic stroke
Studies so far indicate that hsCRP is not a predictive marker for hemorrhagic stroke. Roudbary et al. assessed the concentration of hsCRP in patients with documented ischemic and hemorrhagic stroke in the first 24 h of the onset of symptoms [17]. Their study revealed that types of stroke were related to elevated hsCRP levels [17]. Serum level of hsCRP (Table 1) in ischemic patients was 18.92 ± 11.28 and in hemorrhagic group was 2.65 ± 1.70. This difference was statistically significant (p < 0.0001) [17]. They concluded that hsCRP level is increased in patients with ischemic but not in hemorrhagic stroke, which may make it a useful adjunctive method for determining type of stroke. At present other markers, but not hsCRP, are potentially used in the diagnosis of hemorrhagic stroke.
9. Other neurological and related conditions
In addition its prediction value in the stroke, hsCRP has also been investigated for its prediction values in stroke relevant diseases. Wersching et al. examined 447 community-dwelling and stroke-free individuals from the Systematic Evaluation and Alteration of Risk Factors for Cognitive Health (SEARCH) Study. They found that serum CRP is linked to cerebral microstructural integrity and cognitive function [63]. Song et al. examined 212 patients with de novo Parkinson’s disease (PD), 253 patients with acute ischemic cerebrovascular disease and 119 healthy subjects and investigated the differences in hsCRP among these 3 groups. Their results suggested that elevated hsCRP might have a clinical value as a risk factor for Parkinson’s disease [15]. In a study of CRP and lipid levels in women Everett et al. found that hsCRP associated more closely with ischemic stroke than with CHD. They suggested that concomitant evaluation of lipid levels and hsCRP may improve risk assessment for stroke as well as CHD [11]. These and many other studies have indicated that hsCRP is associated with large number of diseases and disorders. Currently, the mechanistic linkages between CRP and these diseases are not completely understood.
10. CRP polymorphism influence the level of hsCRP
Like many other genes, the expression level of CRP is influenced by its polymorphism [64] (Fig. 1). Polymorphism of CRP has been investigated in different ethnic groups and different diseases. Sheu et al. [65] measured CRP concentrations and investigated 6 polymorphisms of CRP gene in 369 Chinese men. They found that CRP 1009A>G genotypes and associated haplotypes were associated with lower fasting serum hsCRP concentrations in a group of elderly Chinese men. Liu et al. [66] then investigated the potential association of the CRP gene + 1444C/T polymorphism with symptomatic carotid artery stenosis. They found that CRP + 1444 CC genotype is a risk factor for >70% carotid artery stenosis. The serum CRP level was associated with the presence of carotid stenosis.
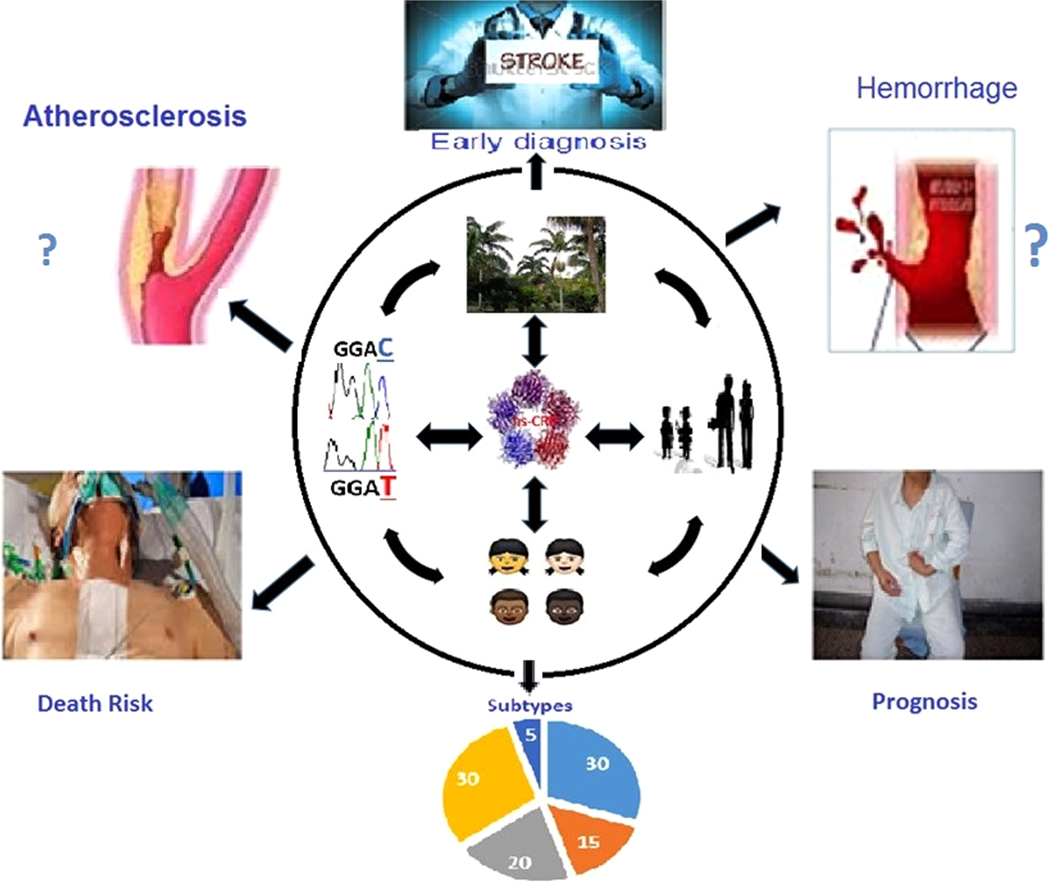
Fig. 1.
Multiple factors determine the prediction function of hsCRP on stroke phenotypes. Level of hsCRP is influenced by its gene polymorphism, genomic background of the ethnic groups, gender and it interacts with environment. These multiple factors interact each other to eventually determine the level of hsCRP. Accordingly, the level of hsCRP achieves its values in whether it predicts different disease phenotypes.
Kettunen et al. investigated 5 polymorphisms and measured CRP concentration of hsCRP in men in a Finnish middle-aged study population. They found that CRP gene allelic variation is associated with CRP levels in both sexes and with one carotid artery elasticity parameter (SI) in men in a population-based Finnish cohort of middle-aged subjects [64]. Assayag genotyped the −757T>C CRP gene SNP and determined the concentration of serum CRP, the intima-media thickness (IMT) of the common carotid artery and the existence of plaque/s in 612 apparently healthy men and women aged 66 ± 10 years in Israel [67]. Their study provided evidence that CRP-757C allele of CRP gene is associated with carotid atherosclerosis, independently of traditional vascular risk factors.
By studying the C1444T polymorphism of CRP 75 in consecutive patients with a first-ever cerebral ischemic event attributable to symptomatic intracranial atherosclerotic disease (ICAD) [68], Arenillas et al. suggested that presence of the T allele within the CRP gene C1444T polymorphism is associated with a higher risk of further ischemic events in symptomatic ICAD patients.
Polymorphisms in other locations in the genome are also found to influence the level of hsCRP. Bernardo et al. investigated the Influence of the CD14 C260T promoter polymorphism on C-reactive protein levels in patients with coronary artery disease [69]. Their finding indicated that homozygosis status of the T allele was independently associated with hsCRP levels and suggested that T homozygotes of this functional polymorphism are at increased ischemic risk.
However, there are negative reports suggest there is no association of polymorphisms of CRP with disease. Ghattaset al reported that CRP 1059G/C gene variation influences plasma CRP levels. Conversely, this polymorphism was not associated with the risk for acute myocardial infarction in an Egyptian population [70]. Huang assessed the potential genetic determinants for serum hsCRP levels in a cohort with well-controlled nondiabetic hypertension. They reported that CRP genotype had a limited effect on serum hsCRP levels in subjects with well-controlled hypertension; suggesting that the impacts of clinical rather than genetic determinants influence serum hsCRP levels for cardiovascular risk stratification in this intermediate-risk Chinese Taiwanese cohort [71].
These results above probably are the results of variation of function of the polymorphism, different ethnic genetic backgrounds, and potential gene-environmental interaction.
11. Ethnic difference on the prediction values of hsCRP
The predictive value of hsCRP may vary among different ethnic groups (Fig. 1). At present, data on the early diagnosis based on the expression level of hsCRP are all from Asian population [26,34]. The reports on prediction values on diagnosis of disease recurrence and major adverse neurological events are also from Asian population [27,61,62]. Although the prediction of death rate is well recognized among all ethnic groups, two studies that reported the prediction values of hsCRP on the risk of early death of stroke patients are all from Asian [49,50]. It is not clear whether it is true that some polymorphism are only associated with men [64,65] while others are associated with both sexes, and some of the polymorphism do not have prediction values. The values of hsCRP expression level for the prediction of atherosclerosis—artery stenosis or occlusion have been recognized in a variety of ethnic groups. However, there is a possibility that it predicts different phenotypes in different populations [35–47]. Therefore, it is most likely that the level of hsCRP and its predication values on variety of stroke phenotypes are influenced by the ethnic genome background.
12. Summary and future direction
It is clear that hsCRP has an important role in the prognosis and risk factor prediction in stroke diseases, including long term and short time death risk, early diagnosis, prediction of etiological subtypes, and prognosis (Table 2). CRP is potentially valuable for the prediction of atherosclerosis (Table 2). Its value on the prediction is unknown for on idiopathic Parkinson’s disease, cerebral microstructural integrity and cognitive function, and Hemorrhage. Reports on its predictive value on functional disability, Cognitive decline in late midlife, and genetic influence are controversial (Table 2).
Table 2.
Predictive values of CRP on different phenotypes.
| Valuable | Potentially valuable | Unknown value | Controversial |
|---|---|---|---|
| 1. Death risk [12,48–50,52–57] | Atherosclerosis [13,46] | 1. Idiopathic Parkinson’s disease [15] | 1. Cognitive decline in late midlife [78] |
| 2. Etiological subtypes [58,59] | 2. Cerebral microstructural integrity and cognitive function [63] | 2. Genetic determinants influence [71] | |
| 3. Early diagnosis [26,34] | 3. Functional disability [62,79–81] | ||
| 4. Prognosis [26,27,40,60,74] | 3. Hemorrhage [17] |
CRP expression and its predictive value are influenced by gene polymorphisms [65], the genomic backgrounds of different racial groups [26,27,35,46,50], sex and the environment (Fig. 1). Therefore it is important to consider these factors when evaluating the predictive value of hsCRP on stroke phenotypes in the future studies. These factors may also contribute to the controversial differences between studies in the value of hsCRP. Based on the current report, hsCRP can be used in early diagnosis of stroke, prediction of atherosclerosis—artery stenosis or occlusion, death risk, and etiological subtypes of ischemic stroke.
In addition, hsCRP may be a valuable marker for some cerebrovascular relevant diseases, but further investigation is necessary. For example, the value of hsCRP levels as risk factors for the initiation of Parkison’s disease [15]. Interestingly, in the prediction of stroke prognosis, lesion volume and all of the evaluated biochemical parameters are not deterministic factors [72].
In many studies, hsCRP has been investigated together with other biomarkers. In order to increase the sensitivity and specificity of diagnosis, the combination of multi-biomarkers may be necessary [5,27,34,41,47–49,53,58,62,73–75]. These markers may together with hsCRP predict risk in different stages of the stroke and/or phenotypes. For example, recent observations suggest that measurement of serum MMP-9, TIMP-1, and hsCRP levels may be useful in the diagnosis and management of ischemic stroke patients providing a more feasible blood biomarker index [74]. Recently, the association between cerebrovascular disease and adhesion molecules has received much attention. A study suggests that sICAM-1 levels may be a potential marker for silent cerebral infarction, which may lead to future stroke and vascular dementia, and that this marker could be useful in monitoring disease progression and as a surrogate marker in treatment studies [75,76].
Lowering CRP levels may be of value in stroke patients or those with other relevant diseases. It has been reported that statin therapy significantly alters serum hsCRP level in patient after acute ischemic stroke [14]. While more studies may be necessary to determine whether statins improve the clinical outcome among patients with AIS with elevated CRP levels [26], statins should be given as early as possible in patients with acute ischemic stroke, especially those with high hsCRP concentrations [14].
Quick and accurate detection methods for CRP levels should be developed. For example, a real-time, on-line and low-cost widerange -CRP assay is a reasonable alternative to the Behring Dade hsCRP method in acute stroke/transient ischemic attack patients [77].
There are several important questions regarding the role of CRP polymorphisms. It is important to understand whether polymorphisms affect the expression level or function of the CRP, whether the altered level of CRP reflect the risk level in stroke disease, and whether single plays a key role or multiple polymorphisms act together.
Acknowledgments
Role of the funder/sponsor
The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Funding/support
This work was partially supported by funding from The First Hospital of Qiqihar City, Heilongjiang Province, PR China and the National Natural Science Foundation of China (Project 81372996 to YJ), P.R. China. Support was also received from an unrestricted grant from Research to Prevent Blindness (New York, NY). The funding organization had no role in the design or conduct of this research.
Footnotes
Conflict of interest disclosures
No conflicting relationship exists for any author.
References
- [1].Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology 2013;81:264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health 2013;1:e259–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Liu L, Wang D, Wong KS, et al. Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 2011;42:3651–4. [DOI] [PubMed] [Google Scholar]
- [4].Yip HK, Tsai TH, Lin HS, et al. Effect of erythropoietin on level of circulating endothelial progenitor cells and outcome in patients after acute ischemic stroke. Crit Care 2011;15:R40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jia L, Hao F, Wang W, et al. Circulating miR-145 is associated with plasma high-sensitivity C-reactive protein in acute ischemic stroke patients. Cell Biochem Funct 2015;33:314–9. [DOI] [PubMed] [Google Scholar]
- [6].Vibo R, Kõrv J, Roose M, et al. Acute phase proteins and oxidised low-density lipoprotein in association with ischemic stroke subtype, severity and outcome. Free Radic Res 2007;41:282–7. [DOI] [PubMed] [Google Scholar]
- [7].Yoldas T, Gonen M, Godekmerdan A, et al. The serum high-sensitive C reactive protein and homocysteine levels to evaluate the prognosis of acute ischemic stroke. Mediators Inflamm 2007;2007:15929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Tsai NW, Chang WN, Shaw CF, et al. The value of leukocyte adhesion molecules in patients after ischemic stroke. J Neurol 2009;256:1296–302. [DOI] [PubMed] [Google Scholar]
- [9].Vila N, Castillo J, Davalos A, et al. Levels of antiinflammatory cytokines and neurological worsening in acute ischemic stroke. Stroke 2003;34:671–5. [DOI] [PubMed] [Google Scholar]
- [10].Frijns CJ, Kappelle LJ. Inflammatory cell adhesion molecules in ischemic cerebrovascular disease. Stroke 2002;33:2115–22. [DOI] [PubMed] [Google Scholar]
- [11].Everett BM, Kurth T, Buring JE, et al. The relative strength of C-reactive protein and lipid levels as determinants of ischemic stroke compared with coronary heart disease in women. J Am Coll Cardiol 2006;48:2235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Makita S, Nakamura M, Satoh K, et al. Serum C-reactive protein levels can be used to predict future ischemic stroke and mortality in Japanese men from the general population. Atherosclerosis 2009;204:234–8. [DOI] [PubMed] [Google Scholar]
- [13].Xie D, Deng L, Liu XD, et al. Role of high sensitivity C-reactive protein and other risk factors in intracranial and extracranial artery occlusion in patients with ischaemic stroke. J Int Med Res 2015;43:711–7. [DOI] [PubMed] [Google Scholar]
- [14].Tsai NW, Lee LH, Huang CR, et al. The association of statin therapy and high-sensitivity C-reactive protein level for predicting clinical outcome in acute non-cardioembolic ischemic stroke. Clin Chim Acta 2012;413:1861–5. [DOI] [PubMed] [Google Scholar]
- [15].Song IU, Kim JS, Chung SW, et al. Is there an association between the level of high-sensitivity C-reactive protein and idiopathic Parkinson’s disease? A comparison of Parkinson’s disease patients, disease controls and healthy individuals. Eur Neurol 2009;62:99–104. [DOI] [PubMed] [Google Scholar]
- [16].Chang CY, Chen JY, Ke D, et al. Plasma levels of lipophilic antioxidant vitamins in acute ischemic stroke patients: correlation to inflammation markers and neurological deficits. Nutrition 2005;21:987–93. [DOI] [PubMed] [Google Scholar]
- [17].Roudbary SA, Saadat F, Forghanparast K, et al. Serum C-reactive protein level as a biomarker for differentiation of ischemic from hemorrhagic stroke. Acta Med Iran 2011;49:149–52. [PubMed] [Google Scholar]
- [18].Samson Y, Lapergue B, Hosseini H. Inflammation and ischaemic stroke: current status and future perspectives. Rev Neurol (Paris) 2005;161:1177–82. [DOI] [PubMed] [Google Scholar]
- [19].Huang J, Upadhyay UM, Tamargo RJ. Inflammation in stroke and focal cerebral ischemia. Surg Neurol 2006;66:232–45. [DOI] [PubMed] [Google Scholar]
- [20].Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest 2003;111:1805–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Winbeck K, Poppert H, Etgen T, et al. Prognostic relevance of early serial C-reactive protein measurements after first ischemic stroke. Stroke 2002;33:2459–64. [DOI] [PubMed] [Google Scholar]
- [22].Rosenson RS, Koenig W. High-sensitivity C-reactive protein and cardiovascular risk in patients with coronary heart disease. Curr Opin Cardiol 2002;17:325–31. [DOI] [PubMed] [Google Scholar]
- [23].Di Napoli M, Papa F, Bocola V. Prognostic influence of increased C-reactive protein and fibrinogen levels in ischemic stroke. Stroke 2001;32:133–8. [DOI] [PubMed] [Google Scholar]
- [24].Muir KW, Weir CJ, Alwan W, et al. C-reactive protein and outcome after ischemic stroke. Stroke 1999;30:981–5. [DOI] [PubMed] [Google Scholar]
- [25].Di Napoli M, Papa F, Bocola V. C-reactive protein in ischemic stroke: an independent prognostic factor. Stroke 2001;32:917–24. [DOI] [PubMed] [Google Scholar]
- [26].Youn CS, Choi SP, Kim SH, et al. Serum highly selective C-reactive protein concentration is associated with the volume of ischemic tissue in acute ischemic stroke. Am J Emerg Med 2012;30:124–8. [DOI] [PubMed] [Google Scholar]
- [27].Ozkan AK, Yemisci OU, Saracgil Cosar SN, et al. Can high-sensitivity C-reactive protein and ferritin predict functional outcome in acute ischemic stroke? A prospective study. Top Stroke Rehabil 2013;20:528–36. [DOI] [PubMed] [Google Scholar]
- [28].Kathariya R, Jain H, Gujar D, et al. Pentraxins as key disease markers for periodontal diagnosis. Dis Markers 2013;34:143–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ridker PM. From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection. Circ Res 2016;118:145–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hage FG, Szalai AJ. C-reactive protein gene polymorphisms, C-reactive protein blood levels, and cardiovascular disease risk. J Am Coll Cardiol 2007;50:1115–22. [DOI] [PubMed] [Google Scholar]
- [31].Tan JR, Tan KS, Koo YX, et al. Blood microRNAs in low or no risk ischemic stroke patients. Int J Mol Sci 2013;14:2072–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kitagawa K. Cerebral vessel disease and inflammatory process. Brain Nerve 2009;61:1061–8. [PubMed] [Google Scholar]
- [33].Di Napoli M, Schwaninger M, Cappelli R, et al. Evaluation of C-reactive protein measurement for assessing the risk and prognosis in ischemic stroke: a statement for health care professionals from the CRP Pooling Project members. Stroke 2005;36:1316–29. [DOI] [PubMed] [Google Scholar]
- [34].Kanai A, Kawamura T, Umemura T, et al. Association between future events of brain infarction and soluble levels of intercellular adhesion molecule-1 and C-reactive protein in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract 2008;82:157–64. [DOI] [PubMed] [Google Scholar]
- [35].Bonita R, Mendis S, Truelsen T, et al. The global stroke initiative. Lancet Neurol 2004;3:391–3. [DOI] [PubMed] [Google Scholar]
- [36].Gorelick PB. Stroke prevention therapy beyond antithrombotics: unifying mechanisms in ischemic stroke pathogenesis and implications for therapy: an invited review. Stroke 2002;33:862–75. [DOI] [PubMed] [Google Scholar]
- [37].Liu LH, Chia LG. The causes of ischemic stroke in patients under 45 years of age. Zhonghua Yi Xue Za Zhi (Taipei) 1993;52:314–8. [PubMed] [Google Scholar]
- [38].Akins PT, Pilgram TK, Cross DT 3rd, et al. Natural history of stenosis from intracranial atherosclerosis by serial angiography. Stroke 1998;29:433–8. [DOI] [PubMed] [Google Scholar]
- [39].Koenig W. High-sensitivity C-reactive protein and atherosclerotic disease: from improved risk prediction to risk-guided therapy. Int J Cardiol 2013;168:5126–34. [DOI] [PubMed] [Google Scholar]
- [40].Yeh KH, Tsai TH, Chai HT, et al. Comparison of acute versus convalescent stage high-sensitivity C-reactive protein level in predicting clinical outcome after acute ischemic stroke and impact of erythropoietin. J Transl Med 2012;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Shimizu K, Shimomura K, Tokuyama Y, et al. Association between inflammatory biomarkers and progression of intracranial large artery stenosis after ischemic stroke. J Stroke Cerebrovasc Dis 2013;22:211–7. [DOI] [PubMed] [Google Scholar]
- [42].Blanco M, Sobrino T, Montaner J, et al. Stroke with polyvascular atherothrombotic disease. Atherosclerosis 2010;208:587–92. [DOI] [PubMed] [Google Scholar]
- [43].Whiteley W, Jackson C, Lewis S, et al. Association of circulating inflammatory markers with recurrent vascular events after stroke: a prospective cohort study. Stroke 2011;42:10–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Arenillas JF, Alvarez-Sabín J, Molina CA, et al. Progression of symptomatic intracranial large artery atherosclerosis is associated with a proinflammatory state and impaired fibrinolysis. Stroke 2008;39:1456–63. [DOI] [PubMed] [Google Scholar]
- [45].Yoshida M, Higashi K, Kobayashi E, et al. Correlation between images of silent brain infarction, carotid atherosclerosis and white matter hyperintensity, and plasma levels of acrolein, IL-6 and CRP. Atherosclerosis 2010;211:475–9. [DOI] [PubMed] [Google Scholar]
- [46].Li C, Guo R, Lou J, et al. The transcription levels of ABCA1, ABCG1 and SR-BI are negatively associated with plasma CRP in Chinese populations with various risk factors for atherosclerosis. Inflammation 2012;35:1641–8. [DOI] [PubMed] [Google Scholar]
- [47].Nambi V, Hoogeveen RC, Chambless L, et al. Lipoprotein-associated phospholipase A2 and high-sensitivity C-reactive protein improve the stratification of ischemic stroke risk in the Atherosclerosis Risk in Communities (ARIC) study. Stroke 2009;40:376–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Li YM, Liu XY. Serum levels of procalcitonin and high sensitivity C-reactive protein are associated with long-term mortality in acute ischemic stroke. J Neurol Sci 2015;352:68–73. [DOI] [PubMed] [Google Scholar]
- [49].Tu WJ, Zhao SJ, Liu TG, et al. Combination of high-sensitivity C-reactive protein and homocysteine predicts the short-term outcomes of Chinese patients with acute ischemic stroke. Neurol Res 2013;35:912–21. [DOI] [PubMed] [Google Scholar]
- [50].Huang Y, Jing J, Zhao XQ, et al. High-sensitivity C-reactive protein is a strong risk factor for death after acute ischemic stroke among Chinese. CNS Neurosci Ther 2012;18:261–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Idicula TT, Brogger J, Naess H, et al. Admission C-reactive protein after acute ischemic stroke is associated with stroke severity and mortality: the ‘Bergen stroke study’. BMC Neurol 2009;9:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Chan CP, Jiang HL, Leung LY, et al. Multiple atherosclerosis-related biomarkers associated with short- and long-term mortality afterstroke. Clin Biochem 2012;45:1308–15. [DOI] [PubMed] [Google Scholar]
- [53].Elkind MS, Tai W, Coates K, et al. High-sensitivity C-reactive protein, lipoprotein-associated phospholipase A2, and outcome after ischemic stroke. Arch Intern Med 2006;166:2073–80. [DOI] [PubMed] [Google Scholar]
- [54].Hartmann A, Rundek T, Mast H, et al. Mortality and causes of death after first ischemic stroke: the Northern Manhattan Stroke Study. Neurology 2001;57:2000–5. [DOI] [PubMed] [Google Scholar]
- [55].Whiting R, Shen Q, Hung WT, et al. Predictors for 5-year survival in a prospective cohort of elderly stroke patients. Acta Neurol Scand 2011;124:309–16. [DOI] [PubMed] [Google Scholar]
- [56].Kammersgaard LP, Olsen TS. Cardiovascular risk factors and 5-year mortality in the Copenhagen Stroke Study. Cerebrovasc Dis 2006;21:187–93. [DOI] [PubMed] [Google Scholar]
- [57].Putaala J, Curtze S, Hiltunen S, et al. Causes of death and predictors of 5-year mortality in young adults after first-ever ischemic stroke: the Helsinki Young Stroke Registry. Stroke 2009;40:2698–703. [DOI] [PubMed] [Google Scholar]
- [58].Liu LB, Li M, Zhuo WY, et al. The role of hs-CRP, D-dimer and fibrinogen in differentiating etiological subtypes of ischemic stroke. PLoS One 2015;10: e0118301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41. [DOI] [PubMed] [Google Scholar]
- [60].Gong X, Zou X, Liu L, et al. Prognostic value of inflammatory mediators in 1-year outcome of acute ischemic stroke with middle cerebral artery stenosis. Mediat Inflamm 2013;2013:850714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Luo Y, Wang Z, Li J, et al. Serum CRP concentrations and severity of ischemic stroke subtypes. Can J Neurol Sci 2012;39:69–73. [DOI] [PubMed] [Google Scholar]
- [62].Song IU, Kim YD, Kim JS, et al. Can high-sensitivity C-reactive protein and plasma homocysteine levels independently predict the prognosis of patients with functional disability after first-ever ischemic stroke. Eur Neurol 2010;64:304–10. [DOI] [PubMed] [Google Scholar]
- [63].Wersching H, Duning T, Lohmann H, et al. Serum C-reactive protein is linked to cerebral microstructural integrity and cognitive function. Neurology 2010;74:1022–9. [DOI] [PubMed] [Google Scholar]
- [64].Kettunen T, Eklund C, Kähönen M, et al. Polymorphism in the C-reactive protein (CRP) gene affects CRP levels in plasma and one early marker of atherosclerosis in men: The Health 2000 Survey. Scand J Clin Lab Invest 2011;71:353–61. [DOI] [PubMed] [Google Scholar]
- [65].Sheu WH, Chen YD, Yu CY, et al. C-reactive protein gene polymorphism 1009A>G is associated with serum CRP levels in Chinese men: a TCVGHAGE study. Clin Chim Acta 2007;382:117–23. [DOI] [PubMed] [Google Scholar]
- [66].Liu ZZ, Ding XR, Zheng HG, et al. Study on the association of the CRP gene +1444C/T polymorphism with symptomatic carotid artery stenosis. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2009;26:435–8. [PubMed] [Google Scholar]
- [67].Ben Assayag E, Shenhar-Tsarfaty S, Bova I, et al. Association of the −757T>C polymorphism in the CRP gene with circulating C-reactive protein levels and carotid atherosclerosis. Thromb Res 2009;124:458–62. [DOI] [PubMed] [Google Scholar]
- [68].Arenillas JF, Massot A, Alvarez-Sabín J, et al. C-reactive protein gene C1444T polymorphism and risk of recurrent ischemic events in patients with symptomatic intracranial atherostenoses. Cerebrovasc Dis 2009;28:95–102. [DOI] [PubMed] [Google Scholar]
- [69].Bernardo E, Angiolillo DJ, Ramírez C, et al. Influence of the CD14 C260T promoter polymorphism on C-reactive protein levels in patients with coronary artery disease. Am J Cardiol 2006;98:1182–4. [DOI] [PubMed] [Google Scholar]
- [70].Ghattas MH, Abo-Elmatty DM, El-Eraki AZ. C-reactive protein 1059G/C gene polymorphism, C-reactive protein levels and acute myocardial infarction. J Cardiovasc Med (Hagerstown) 2012;13:716–9. [DOI] [PubMed] [Google Scholar]
- [71].Huang CC, Chung CM, Leu HB, et al. Genetic variation in C-reactive protein in ethnic Chinese population in Taiwan. Eur J Clin Invest 2013;43:449–56. [DOI] [PubMed] [Google Scholar]
- [72].Varoglu AO, Kuyucu M, Demir R, et al. Prognostic values of lesion volume and biochemical markers in ischemic and hemorrhagic stroke: a stereological and clinical study. Int J Neurosci 2009;119:2206–18. [DOI] [PubMed] [Google Scholar]
- [73].Umemura T, Kawamura T, Sakakibara T, et al. Association of soluble adhesion molecule and C-reactive protein levels with silent brain infarction in patients with and without type 2 diabetes. Curr Neurovasc Res 2008;5:106–11. [DOI] [PubMed] [Google Scholar]
- [74].Park SY, Kim MH, Kang SY, et al. Inflammatory marker expression and its implication in Korean ischemic stroke patients. Korean J Lab Med 2007;27:197–204. [DOI] [PubMed] [Google Scholar]
- [75].Kawamura T, Umemura T, Kanai A, et al. Soluble adhesion molecules and C-reactive protein in the progression of silent cerebral infarction in patients with type 2 diabetes mellitus. Metabolism 2006;55:461–6. [DOI] [PubMed] [Google Scholar]
- [76].Zhou Y, Han W, Gong D, et al. Hs-CRP in stroke: a meta-analysis. Clin Chim Acta 2016;453:21–7. [DOI] [PubMed] [Google Scholar]
- [77].Shenhar-Tsarfaty S, Ben Assayag E, et al. Wide-range C-reactive protein efficacy in acute ischemic stroke patients. Acta Neurol Scand 2006;114:29–32. [DOI] [PubMed] [Google Scholar]
- [78].Singh-Manoux A, Dugravot A, Brunner E, et al. Interleukin-6 and C-reactive protein as predictors of cognitive decline in late midlife. Neurology 2014;83:486–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Taheraghdam A, Aminnejad S, Pashapour A, et al. Is there a correlation between hs-CRP levels and functional outcome of Ischemic Stroke? Pak J Med Sci 2013;29:166–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Song IU, Kim JS, Kim YI, et al. Relationship between high-sensitivity C-reactive protein and clinical functional outcome after acute ischemic stroke in a Korean population. Cerebrovasc Dis 2009;28:545–50. [DOI] [PubMed] [Google Scholar]
- [81].Bunevicius A, Kazlauskas H, Raskauskiene N, et al. Ischemic stroke functional outcomes are independently associated with C-reactive protein concentrations and cognitive outcomes with triiodothyronine concentrations: a pilot study. Endocrine 2014;45:213–20. [DOI] [PubMed] [Google Scholar]